Abstract
Hawai‘i faces unique challenges to Electronic Health Record (EHR) adoption due to physician shortages, a widespread distribution of Medically Underserved Areas and Populations (MUA/P), and a higher percentage of small independent practices. However, research on EHR adoption in Hawai‘i is limited. To address this gap, this article examines the current state of EHR in Hawai‘i, the barriers to adoption, and the future of Health Information Technology (HIT) initiatives to improve the health of Hawai‘i's people. Eight focus groups were conducted on Lana‘i, Maui, Hawai‘i Island, Kaua‘i, Moloka‘i, and O‘ahu. In these groups, a total of 51 diverse health professionals were asked about the functionality of EHR systems, barriers to use, facilitators of use, and what EHRs would look like in a perfect world. Responses were summarized and analyzed based on constant comparative analysis techniques. Responses were then clustered into thirteen themes: system compatibility, loss of productivity, poor interface, IT support, hardware/software, patient factors, education/training, noise in the system, safety, data quality concerns, quality metrics, workflow, and malpractice concerns. Results show that every group mentioned system compatibility. In response to these findings, the Health eNet Community Health Record initiative — which allows providers web-based access to patient health information from the patient's provider network— was developed as a step toward alleviating some of the barriers to sharing information between different EHRs. The Medicare Access and CHIP Reauthorization Act of 2015 (MACRA) legislation will introduce a new payment model in 2017 that is partially based on EHR utilization. Therefore, more research should be done to understand EHR adoption and how this ruling will affect providers in Hawai‘i.
Keywords: Electronic health records, barriers, MACRA, community health record, physician workforce, Hawai‘i
Introduction
The passage of the Health Information Technology for Economic and Clinical Health (HITECH) Act in 20091 brought the implementation of electronic health records (EHRs) to the forefront of healthcare practice and delivery. In spite of the enormous promise of Health Information Technology (HIT) to benefit patients, reduce inefficiencies, and reduce costs for providers, it is still in the process of being realized.2 In February 2014, Hawai‘i's Office of the Governor published a report declaring HIT connectivity and capability, including EHR adoption, part of a six-point plan to address the future of healthcare in Hawai‘i.3,4 With initiatives such as telehealth, community care networks, and many other novel solutions, the report sets out the goal of achieving “better health, better healthcare, lower costs and reduced health disparities.”3
Attempts to develop rudimentary EHR systems (systems containing computerized records of patients' healthcare information) began across the United States (US) in the 1960s.5,6 By 1965, “at least 73 hospital and clinical information system projects and 28 projects for storage and retrieval of medical documents” were in the works.6 As these efforts were heavily constrained by technological limitations, paper records remained the standard for decades. Fast forward to the 21st century, when, despite radical advancements in digital technologies, paper records continue to be favored in many healthcare facilities. Thus, in 2009, the HITECH Act invested $29 billion to galvanize EHR adoption across the US.7 As a result, eligible professionals could apply for financial rewards through either the Medicare or Medicaid EHR incentive programs. 8–12 To qualify, providers are required to successfully demonstrate “meaningful use” of a certified EHR system by meeting three stages of progressively rigorous EHR objectives as determined by the Center for Medicare and Medicaid Services (CMS).8,13 Enrollment in the Medicare incentive program closed in 2014; however, providers could still enroll in the Medicaid incentive program until 2016.10–12
Against this backdrop, the adoption of EHRs became commonplace among various health providers by 2015—the year Medicare reimbursement penalties began for providers who failed to meet meaningful use requirements.9,11 On April 27th, 2016 a Notice of Proposed Rulemaking was released for the Medicare Access and CHIP Reauthorization Act of 2015 (MACRA).14 The current Medicare reimbursement model and meaningful use-associated penalties will be replaced by the Quality Payment Program (QPP), a new Medicare Part B reimbursement model consisting of the Merit-based Incentive Payment System (MIPS) and the Advanced Alternative Payment Model (APM).14,15 Instead of meaningful use criteria, EHR utilization will continue to be evaluated as part of the new Advancing Care Information (ACI) category of MIPS.16
Although EHRs are now mainstream, responses to EHR adoption initiatives are mixed. While 84% of EHR adopting physicians agreed “EHR use produces clinical benefits,”17 multiple challenges have also been identified, such as EHR interoperability, usability, and data security.18 In particular, physicians in Hawai‘i face their own compounding challenges to a smooth running healthcare system. These include (1) a growing physician shortage,19 (2) a widespread distribution of Medically Underserved Areas and Populations (MUA/P),20 and (3) a higher percentage of small-group practice models. 3
Healthcare in Hawai‘i is greatly impacted by a shortage of over 600 physicians as compared to the number of physicians across the US for a population the same size.19 By 2020, the shortage in Hawai‘i is expected to more than double to 1,600 physicians in demand.19 The second obstacle is a wide distribution of federally-designated MUA/P across the state. 20 These underserved areas and populations can cover entire islands and are common in rural areas far from the urban capital of Honolulu.20 The third challenge is that Hawai‘i's physician workforce is composed of many solo and smaller private practices,3 even though national trends have shifted toward the employed provider practice model.21 Historically, small group practices were responsible for a “significant portion of the care received by underserved and vulnerable individuals,”22 and the same trend is expected for underserved communities on the neighbor islands. Without the infrastructure of a supporting organization, it is difficult for small practices to adopt EHRs and avoid subsequent meaningful use penalties. According to one study, family medicine physicians in small practices and those among MUA/P were less likely to adopt an EHR compared to physicians in larger practices.23 In 2013, overall adoption of EHRs among office-based primary care providers in Hawai‘i was 9% higher than the nationally reported average in the same category.24 However, basic EHR adoption among office-based rural providers in Hawai‘i was 7% lower than the national average for the same group.24
In the face of new changes to HIT policies, it is unfortunate that there is very little literature specific to EHR adoption and utilization in Hawai‘i. Nationally, physicians have cited numerous barriers such as cost, loss of productivity, training, and the EHR selection process.17 In 2013, a collaborative study between the RAND Corporation and the American Medical Association found that EHRs “significantly worsen professional satisfaction for many physicians.”25 Although there are multiple reasons for the physician shortage in Hawai‘i, early physician retirement remains the biggest factor for workforce attrition.19 In a geographically isolated island state with a physician shortage, many underserved areas, and a trend toward small group practices, it is critically important to support Hawai‘i's physicians during their transition to EHR adoption.
To facilitate this process, the federal government funded the creation of Regional Extension Centers (RECs) across the nation to provide “technical assistance for individual and small provider practices, medical practices lacking resources to implement and maintain [EHRs], and those who provide primary care services in public and critical access hospitals, community health centers, and other settings that mostly serve those who lack adequate coverage or medical care.”26 This assistance is available locally through the Hawai‘i Health Information Exchange (Hawai‘i HIE), the official State Designated Entity for the creation of an interoperable health information exchange.27 Although REC assistance is available nationwide, numerous challenges to EHR implementation have still been noted in the literature.17,18 Through a series of focus groups, this study aims to better understand the current EHR landscape in Hawai‘i, identify the barriers to adoption of this health technology, and discuss its future role in Hawai‘i's medical community.
Methods
Facilitated focus groups were conducted in 2014 to explore health provider adoption of EHR and other associated health information technologies in Hawai‘i. Eight focus groups were held on six of the eight main Hawaiian Islands, including Lana‘i, Maui, Hawai‘i Island, Kaua‘i, Moloka‘i, and O‘ahu (West O‘ahu, Honolulu, and East O‘ahu). Healthcare providers and HIT experts known to the researchers in each region were invited to participate in a focus group that included a meal but no other incentive. Convenience sampling was used, and invitations were delivered by email and fax to provider offices. A total of 51 diverse professionals participated in the focus groups, including 26 physicians, 6 HIT professionals, 5 advanced practice registered nurses, 2 registered nurses, 2 staff members, 2 lawyers, and 1 participant from each of the following fields: physician assistant, case worker, nurse aid, nurse manager, office manager, hospice specialist, finance officer, and chief operating officer. The number of participants in each focus group ranged from 3–13 participants per group.
Facilitators asked open-ended questions to solicit discussion. These questions included use and functionality of EHR systems, barriers to use, facilitators of use, and what EHR would look like in a perfect world. Focus group responses were summarized and analyzed using constant comparative analysis for themes. The frequency of each focus groups discussing a specific theme was tabulated. All participants signed informed consent agreements and were invited to view and comment on a draft report of the findings. In June 2015, an interview with Hawai‘i HIE was conducted to verify the current state of EHR usage and upcoming health information technology initiatives in Hawai‘i. Marketing data from the Hawai‘i HIE Customer Relationship Management System was used as a proxy for EHR vendor usage across the state. Data from the ambulatory EHR market was considered as the closest representative of the research population of interest. This research was performed under University of Hawaii Committee on Human Subjects Institutional Review Board protocol 21832.
Results
Utilization of Electronic Health Records in Practice
Of the 42 actively practicing medical providers and staff who answered a focus group question about using an EHR, all but six had an active EHR. Of these six, three participants stated they did not have an EHR, and three had selected EHR software and were planning to go live with it soon. Attestation is the process of documenting the meaningful use of EHRs and whether their requirements are being fulfilled. Attestation was common to all providers implementing EHRs, although those in larger provider groups were less sure of the level of attestation their group had attained.
EHR Vendors in Hawai‘i
A total of 16 different EHR systems were used by those present in the eight focus groups. Two EHR systems were excluded from this study because the description did not translate to known software. The most commonly reported EHR systems among focus group participants were Epic and Allscripts, with 5 users each. GE Centricity, eClinicalWorks, Meditech, and Siemens followed with three users each (Table 1).
Table 1.
Comparison of Ambulatory EHR Vendors in Hawai‘i Ranked by Percent Market Share and Number of Focus Group Participants Using Each System
| EHR Software System | Percent Market Share | Number of Focus Group Participants |
| Epic | 18.30% | 5 |
| Allscripts/Team Praxis | 7.52% | 5 |
| GE Centricity | 13.96% | 3 |
| eClinicalWorks | 11.20% | 3 |
| Meditech | - | 3 |
| Siemens | - | 3 |
| Amazing Charts | 6.20% | 2 |
| RPMS - Indian Health Services | 1.20% | 2 |
| Practice Fusion | 1.31% | 1 |
| NextGen | 0.45% | 1 |
| gMed | 0.33% | 1 |
| Essentris Clinicomp | - | 1 |
| AHLTA | - | 1 |
| Legacy CHCS | - | 1 |
| Nuesoft Technologies | 10.80% | 0 |
| Vitera | 2.73% | 0 |
| eMDs | 2.70% | 0 |
| Aprima | 2.29% | 0 |
| SOAPWare Inc | 1.64% | 0 |
| Document Storage Systems | 1.53% | 0 |
| McKesson | 1.53% | 0 |
| Catalis | 0.65% | 0 |
| Keiser Computers | 0.65% | 0 |
| Chart Logic | 0.45% | 0 |
| Dr Chrono | 0.45% | 0 |
| Spring Medical Systems | 0.45% | 0 |
| AltaPoint Data Systems | 0.33% | 0 |
| MTBC (Medical Transcription Billing Corporation) | 0.33% | 0 |
| Netsmart | 0.33% | 0 |
| MDIntellesys Inc | 0.23% | 0 |
| ADP | 0.11% | 0 |
| Alere | 0.11% | 0 |
| Athena Health | 0.11% | 0 |
| Conceptual Mindworks | 0.11% | 0 |
| Data Tec Inc | 0.11% | 0 |
| DigiDMS | 0.11% | 0 |
| Health Fusion | 0.11% | 0 |
| MDSync | 0.11% | 0 |
| Other | 0.11% | 0 |
| SRSsoft | 0.11% | 0 |
| Unknown/No EHR System | 11.34% | 6 |
Percent market shares current as of 3/25/2015.
Most of the EHRs described among focus group participants had e-prescribing ability but lacked features to indicate outcomes at the pharmacy (eg, if the prescription was picked up or not). More than half of the EHRs could access labs electronically from at least one laboratory, but very few providers had the capability to order labs electronically. Consults and hospital discharges were more likely to be exchanged using faxes, with the exception of military and Epic systems. Most EHRs had, or will soon have, patient portals; however, usage varied widely due to both patient and provider factors. Billing was usually done through interfaced technology with a third party biller. Quality metrics could be collected by the EHRs, but reporting was done manually in some instances due to the number of different reporting requirements. It was evident that many providers still relied on paper communication as every group mentioned the use of fax machines.
Barriers to EHR Implementation
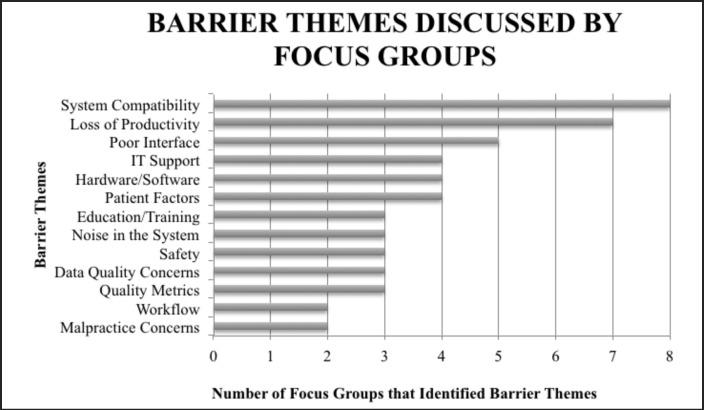
Focus group responses centered on thirteen identifiable barrier themes: system compatibility, loss of productivity, poor interface, IT support, hardware/software, patient factors, education/training, noise in the system, safety, data quality concerns, quality metrics, workflow, and malpractice concerns. Figure 1 presents the prevalence of these barrier themes across the focus groups.
Figure 1.
Number of Focus Groups that Identified Specific Barriers to the Electronic Health Record (EHR)
System compatibility was the only theme common to all eight focus groups. Within this theme, participants desired interoperability among different EHR systems and expressed frustration over the inability to engage in efficient health information exchange. Communication issues persisted between providers and hospitals. According to one provider, “You need to learn that all systems at the hospital and in the office don't communicate.” Some participants were unable to communicate even when using the same EHR vendor. Another participant stated, “If you have to go to a different hospital that has the same system, they can't necessarily communicate.”
Loss of productivity was mentioned as a barrier to EHR utilization by seven out of eight focus groups. Participants agreed that EHR usage took longer than documenting patient visits in a paper chart system. One participant stated, “A computer system doesn't make anything more efficient. When we use paper charts we realize how quick and easy paper is.”
Participants also identified poor user interfaces as a barrier. They were dissatisfied with data entry requirements and the number of “clicks” necessary to complete tasks. Participants described many EHR systems as “hard to read and confusing” and were frustrated by the hassles of juggling multiple windows in an EHR interface. Providers felt patient portal utilization, a core measure for meeting meaningful use requirements and receiving EHR incentives28, was hindered by various patient factors ranging from a lack of patient access to computers to the inability to bill for telehealth services for patients via email or phone. One provider from a rural area stated, “Only 60 percent of our patients have access to computers.”
Hardware and software concerns were mentioned by four of the eight focus groups. Participants were concerned about how quickly EHRs became outdated and the need for adequate IT support, especially in more rural areas. One participant stated, “By the time we have a good program, we are so out of date that the hardware doesn't work.” Capturing the need for IT support, another participant stated, “The difference now is that we can't support it locally like we used to. We have to call off island.”
In addition to concerns about maintaining adequate EHR systems, some providers questioned the integrity of EHR data and the potential perpetuation of errors through incomplete or repeated data entry. According to one participant, “I'm worried that if we just check off boxes, we don't know if people actually did the things that are checked…” In addition, some providers expressed dissatisfaction with the “signal to noise ratio” of EHR records. For example, “One progress note ends up being three pages. It's hard to draw out the basic information.”
Some healthcare providers were concerned about confidentiality, medical malpractice, quality metrics, and overall workflow. One participant commented, “From a patient perspective it is scary that all your info is in “the cloud.” What will happen if I apply for life insurance?” Mental health records in particular can contain sensitive information. Patients and providers desired the assurance of confidentiality during health information exchange and recommended allowing patients to opt-in or opt-out of sharing mental health records. Furthermore, some providers thought the additional information available in an EHR could potentially increase the likelihood of malpractice suits. One participant stated, “Obscure information is a treasure trove for attorneys when something goes wrong.”
Opinions about quality metrics programs were mixed. Dissatisfaction with insurance-based quality program technology stemmed from a lack of interconnectivity between systems, missed documentation, and requisite data entry. As one provider noted, “… the technology is not there.” Providers also described interrupted clinical workflows when using EHR. One participant stated, “EHR hurts flow, ability to code charts, and transmit charts to billing.”
HIT in a “Perfect World”
Focus group participants were not only able to identify barriers, but also provided ideas on what they would want from HIT. Suggestions included intelligent data output, a central data warehouse, inter-professional team support benefits, high security, improvement of patient care, lower cost, system interconnectivity, and a one-time sign in. Respondents described the need to minimize unnecessary effort by reducing duplicate tasks and eliminating “noise” in the patient record. Providers desired EHRs to be an asset to medical practice that improves patient care. Ideally, an EHR would “maximize time with the patient and get human direction back into medicine.” Additionally, “HIT should allow providers to retain independence and practice the way they want to.” Some participants believed HIT could improve patient care by being more patient-centered, including only essential information, and rewarding “service to the patient that improved health.” Reflecting the commonly identified system compatibility barrier, a desire for system interconnectivity, especially the ability to conduct health information exchange, was voiced by many providers. For instance, one participant stated, “I wish we were all on one system and could go into anyone's record and get all the info.” A suggestion was made for a one-time pass through option for providers to log in to one EHR system that will forward credentials to other systems and avoid redundant sign in efforts.
Linked to the desire for greater system interconnectivity were suggestions regarding uniformity of requirements, telemedicine/telehealth, a data warehouse, and many other desired features and functionalities. The suggestions included standards for mandatory immunization reports, a universal intake form, and a single “platform for quality metrics and pay for performance.” Although there was a mention of billing and liability concerns, focus group participants supported “telemedicine as a strategic initiative” for its practicality and ease of use. According to one participant, “[It] doesn't make sense to fly people all over if you can use telehealth.” Another participant stated, “Telehealth will be the key for chronic disease in the future. It's a no-brainer.” Participants also described the need for a “bucket approach” to a patient data warehouse or a “central data repository that can be queried”. One participant commented that it would “be asking less of providers if the technology were better and we could get all the info from one location.”
Focus group participants also shared many new, innovative ideas. Among them were ideas for a patient profile with risk factors and anticipatory guidance, the distribution of handouts in patients' native languages, a medication management tool, character recognition for identification of scanned lab results, and the ability to remotely prescribe.
Discussion
This study presents an overview of recent EHR utilization in Hawai‘i. While a great deal of frustration around EHR remains, the general sense of the participants is not only that EHR is here to stay, but also a hope that it will improve patient care in the future. The implementation and utilization of an EHR still seems to outweigh the relative ease of paper charts. Providers felt that it was worth the work to convert to EHRs and improvement discussions were lively. In the words of one focus group participant, “Done right, you can make it work.”
Many of the frustrations with EHR systems in Hawai‘i are echoed nationally. One of the first barriers to EHR adoption is choosing the right system. A national study conducted in 2011 found that both EHR adopters and non-adopters considered EHR selection to be within the top five barriers for EHR implementation.17 For small or solo practices, the full responsibility of researching and choosing an EHR can be a burden on the physician. One participant said, “Most developed countries have a single EHR system, why don't we?” Another participant was “tied to one product that was only used for a few years.” As of August 2013, out of close to 1,400 complete EHR systems certified for Stage 1 of meaningful use, only 21 complete systems were certified for 2014 Stage 2 requirements.29 The disparity between Stage 2 demands and a lack of Stage 2 meaningful use certified EHR vendor supply put providers in a difficult, costly dilemma. Based on certification status, providers who had adopted an EHR ineligible for Stage 2 of meaningful use attestation faced the difficult choice to either reinvest time and funds “to ‘rip and replace’ their existing EHR” or forfeit incentive payments and incur Medicare penalties. 29
While the focus group participants did not describe the selection as frustrating, they did describe the lack of functionality frustrating. One focus group participant mentioned, “A lot of what Medicare level 2 is asking us to do what our EHR can't do.” Another attendee said, “It's like running a race with shackles on if the EHR is not user-friendly. Most are sluggish and have limited capabilities.” Only 57% of rural Hawai‘i providers had achieved meaningful use compared to 73% of rural providers at the national level,24 which could be influenced by geographic isolation from Honolulu and the many MUA/P across the state.20
Reported EHR systems among focus group participants varied, but generally reflected commonality with state and national ambulatory EHR vendor data. According to the Office of the National Coordinator for Health Information Technology, the top five ambulatory EHR vendors nationally were Epic, Allscripts, eClinicalWorks, NextGen Healthcare, and GE Healthcare (Centricity) respectively for ambulatory EHR systems.30 These systems aligned with the four most frequently reported EHR systems among Hawai‘i focus group participants (Epic, Allscripts, GE Healthcare (Centricity), and eClinicalWorks; Table 1).30 However, there are exceptions to this trend. Nuesoft Technologies occupies 10.80% of the ambulatory EHR market in Hawai‘i, yet this vendor was not represented among focus group attendees (Table 1).
Percent market share data were unavailable for five of the EHRs utilized by focus group participants. Of these missing data, three of the systems were military or Veteran's Administration-based. The other two vendors, Meditech and Siemens (Cerner), are well represented in the hospital EHR market and are not likely to occupy a significant portion of the ambulatory market in Hawai‘i.31
Some physicians view the tedious process and cost factor of EHR implementation as a fruitless endeavor, especially those near retirement age. The upfront startup cost for an in-office EHR system was estimated to be $33K with a five-year total cost of ownership at about $48K.32 In 2013, EHR non-adoption was indicated by less than 10% of all physicians with 41% of this population composed of retiring physicians. 33 According to one provider, “I've only got a few more years until I retire. It's just not worth it.” More research is needed to develop effective solutions to convince those who are considering early retirement to stay in practice. In addition, the number of physicians retiring early may increase based on upcoming Medicare reimbursement changes in 201714, especially since Hawai‘i has the second oldest physician population in the nation.34 As a result, these reimbursement changes could create an extra burden for physicians who are older or in small practices, both of which are represented in greater numbers in Hawai‘i than the rest of the country.21
Under the meaningful use system, providers who did not meet meaningful use requirements would begin receiving an annually increasing 1% Medicare reimbursement readjustment in 2015. 9 The penalty would increase annually for each year of noncompliance with meaningful use regulations up to a maximum total deduction of 5%.9 However, this payment readjustment scale will be replaced by upcoming MACRA changes.14 Instead of attesting to meaningful use, eligible professionals will be evaluated by a four-part performance-based MIPS score, of which the ACI category currently comprises 25%.14,16 ACI includes EHR utilization with “emphasis on interoperability and information exchange.”16 Unlike meaningful use incentives, MACRA evaluates providers relative to other providers across the nation based on the MIPS score, and adjustments must be budget-neutral.14 In year one, participants may be subject to a range of +4% to −4% Medicare reimbursement adjustments based on their MIPS performance score with future adjustments increasing in magnitude: +/−5% in 2020, +/−7% in 2021, and +/− 9% in 2022 and beyond.14 Although the EHR utilization or ACI category will compose a fourth of the MIPS score in year one, it is unclear if this proportion will change and what role EHR utilization will play in the upcoming changes to Medicare reimbursement. What is clear is that it will likely result in a significant downward income adjustment for physicians without high-functioning EHRs.
Among focus group participants, decreased revenue or more specifically, productivity loss, was a highly discussed barrier. Higher costs for providers are ultimately linked to productivity loss and any reduction in patient volume ultimately translates to lost revenue. One participant stated, “You have to hire a new staff person to do all the scanning and printing.” Another said, “We're so busy that to go ahead and put in an EHR and slow down office practice would be difficult. We already spend enough time at our office.” Taking the appropriate steps to evaluate a practice's readiness for EHR conversion can facilitate a smoother transition and minimize unexpected challenges. Hawai‘i's high population of smaller physician practices means providers are less likely to have the support of larger organizations when managing EHR implementation.3 Thus, creating an EHR implementation strategy with stages of planning and evaluation can facilitate this process.27 One participant suggested to complete a “workflow pre-implementation” check and “recheck post-implementation.” It has been done, which is demonstrated by a rural Wisconsin physician. Through careful planning and local REC assistance, they transitioned to EHR without forfeiting patient volume.35 Other providers have a more difficult time with EHR implementation. As one provider stated, “We need EHR SWAT teams to start workflow analysis and fix it.” Technical assistance and education can greatly facilitate successful EHR adoption, especially in small practices.
Technical Barriers
A previous study demonstrated that eight or more technical support visits and at least nine months of EHR utilization were associated with quality improvement in “small primary care practices serving disadvantaged populations.”36 Education and training can help providers and staff use an EHR to its fullest potential. However, access to technical assistance is complicated for neighbor island providers. One attendee stated, “If we want to get trained we have to go to Honolulu. We have to bear the cost of bringing someone over to educate our office.” Although technical support is available, focus group participants reported that outsourcing EHR training and technical support from O‘ahu was resource intensive. Nevertheless, the importance of technical assistance to facilitate implementation and fulfill security requirements cannot be understated.
Data safety and confidentiality were major concerns for focus group participants. Some participants were particularly concerned about the confidentiality of sensitive mental health records. One provider stated, “My patients voice concern and I share their concern that easier IT access to patient mental health records by other providers may not be appropriately protected.” Furthermore, implementation of EHR in behavioral health settings is lower than other healthcare providers, and some mental health providers were ineligible for meaningful use financial incentives based on the setting of care.37–38 In order to meet meaningful use requirements, eligible professionals are required to conduct a mandatory security risk analysis at the time of EHR adoption and review the analysis each reporting period thereafter or sooner if changes occur.39 According to CMS, “doing a thorough and professional risk analysis that will stand up to a compliance review will require expert knowledge that could be obtained through services of an experienced outside professional.” 39 Focus group participants expressed hesitancy about the security of protected health information. To remain in compliance with security standards, providers can seek technical assistance from RECs to conduct security risk assessments.
One of the other challenges in EHR adoption in Hawai‘i is small group practices. Current five-year projections put the total cost of EHR implementation at $48K.32 This estimated amount can be much higher when considering the resources required to outsource training on the neighbor islands. There are even more costs associated with maintaining the EHR, upgrading systems, meeting meaningful use requirements, and conducting audits. Although workflow was only mentioned by two out of eight focus groups, the concept of workflow is interwoven into the other barriers. Previously, failure to meet meaningful use requirements meant that providers would be disqualified from incentive payments that could offset EHR costs in addition to receiving decreased Medicare reimbursements.9 It is still unclear how new MACRA changes will affect providers in small practices.
One of the greatest frustrations with EHRs identified by focus group participants was the lack of system compatibility. Providers desired interoperability and efficient health information exchange. Even though one provider “worked in a community that all had” the same EHR system, “they still didn't communicate.” Because of the proprietary nature of EHR systems, this is one of the greatest challenges facing healthcare effectiveness in the US. However, attendees had positive opinions about a centralized data warehouse.
Since these focus groups were conducted (2014), Hawai‘i HIE has made a major upgrade to the Health eNet Community Health Record (CHR).40 The CHR is a web-based dashboard, a way of querying the patient health information (PHI) from small physician practices, hospitals and other health care facilities through a secure web-based portal to gather relevant PHI into a front-porch style view. 40 In effect, the CHR acts as an intermediary for providers to access patient information through a central health information exchange portal that can be queried on patients who are seeking care. 40 This technology has potential for situations that may occur outside the typical ambulatory setting and require immediate medical care. Similar initiatives are in development across the country with the eventual goal of national interoperability.41 For example, partnerships may eventually allow providers to query another state's CHR to care for a traveling patient. This could be a valuable asset in providing timely emergent care for neighbor island patients treated on O‘ahu, as well as the high influx of tourists and short-term stay individuals in Hawai‘i.
Having the opportunity to utilize health information exchange through a medium like the CHR is especially important for care coordination efficiency. If a neighbor island patient travels to O‘ahu for specialist care (which happens often), these records must be shared with the individual's primary care provider for care coordination. When health information exchange is not readily accessible, one focus group participant described it as “… a wild goose chase to get records.” The ultimate goal for providers is to have an integrated EHR exchange system that is easy to use, efficient, and cost-effective. As of yet, complete interoperability is still a work in progress, but through initiatives like the CHR, it is not out of reach. Additional progress has been made with new collaborations among major hospital systems and key laboratory service groups. The CHR has great potential to advance health information exchange among all healthcare providers in Hawai‘i, even in rural areas.
Limitations of this study include the fact that focus group methodology does not allow for the input of all physicians in the state. Therefore data may not be reflective of all providers across the state. In addition, the participants were selected with convenience sampling, and may over represent some places of employment. Attendance was not consistent across all focus groups, possibly leading to overrepresentation of certain communities. Additionally, self-reported data may be influenced by the presence of colleagues in a group setting. Furthermore, statistics from the Office of National Coordinator for Health IT are based on providers enrolled in an REC. This population is likely to represent the vast majority of EHR adopters; but there may be some providers utilizing EHRs who are unaffiliated with an REC.
The technology industry is highly labile and significant changes may have occurred from the time data were collected until the writing of this article. Data from Hawai‘i HIE was current as of March 25, 2015, and the focus groups were conducted in 2014. The marketing data was generally representative of ambulatory providers in Hawai‘i. However, focus group attendees included professionals from many different settings, including those outside of ambulatory settings. For the purposes of clarity, the terms EHR and EMR were used interchangeably and recorded as EHR even if the participant said EMR. Term usage of EHR vs EMR was generally evenly divided.
Conclusion
While we cannot make generalizations about the entire provider population, this study offers a glimpse of the recent state of EHR utilization in Hawai‘i. In this era of continual technological progress, many challenges continue to exist at the intersection of technology and medicine. In the midst of increasing requirements and challenges, the enormous promise of HIT is closer to realization than ever before. For physicians in Hawai‘i, this means the recent transition to EHRs not only fulfills national mandates, but also promotes the future of Hawai‘i's health. The hope is that increasing HIT utilization, health information exchange, and EHR adoption will contribute to more efficient, coordinated care and better health outcomes.3 The many challenges during this transition period highlight the importance of adapting as health technology moves forward. The hope is that in the future providers will be equipped with better tools, such as the CHR, which will result in efficient health information exchange, well coordinated care, decreased health disparities, and ultimately a healthier Hawai‘i for future generations.
Future research examining changing attitudes toward the EHR, especially as compatibility improves, would provide new insight. Future studies could investigate the perspectives of small group practices adjusting to the MIPS criteria and how initiatives such as CHR will impact interoperability across the state. Furthermore, with the change from Meaningful Use 3 to MACRA incentives, physicians are not sure how rewards and penalties will be allocated. Research into physician satisfaction with reimbursement and support for EHRs will go a long way in ensuring successful implementation.
Acknowledgments
The authors would like to acknowledge the assistance of Christine Sakuda, Hawai‘i Health Information Exchange Executive Director, and Dr. Natalie Pagoria, Hawai‘i Health Information Exchange Associate Director of Provider Services, for their contribution to the preparation of this manuscript.
Conflict of Interest
None of the authors identify a conflict of interest.
References
- 1.Office of the National Coordinator for Health Information Technology. HITECH Programs & Advisory Committees. [June 4, 2016]. Available from: https://www.healthit.gov/policy-researchers-implementers/hitech-programs-advisory-committees.
- 2.Office of the National Coordinator for Health Information Technology, author. Benefits of Electronic Health Records (EHRs) [July 12, 2015]. Available from: http://www.healthit.gov/providers-professionals/benefits-electronic-health-records-ehrs.
- 3.The Hawai‘i Healthcare Project, author. State of Hawai‘i Healthcare Innovation Plan. 2014. Feb, [July 10, 2015]. Available from: http://www.hawaiihealthcareproject.org/index.php/resources/healthcare-innovation-plan.html.
- 4.Office of the Governor Releases Healthcare Transformation Plan [news release] Honolulu, HI: Office of the Governor of the State of Hawai‘i; 2014. Feb 27, [July 10, 2015]. Available from: http://www.hawaiihealthcareproject.org/images/pdf/pressreleases/RELEASE%20Healthcare%20Transformation%20Plan.pdf. [Google Scholar]
- 5.Office of the National Coordinator for Health Information Technology, author. What is an electronic health record (EHR)? [May 5, 2016]. Available from: https://www.healthit.gov/providers-professionals/faqs/what-electronic-health-record-ehr.
- 6.Institute of Medicine, author. The Computer-Based Patient Record: An Essential Technology for Health Care, Revised Edition. Washington, DC: National Academy Press; 1997. p. 111. [PubMed] [Google Scholar]
- 7.Blumenthal D. Wiring the Health System — Origins and Provisions of a New Federal Program. N Engl J Med. 2011;365(24):2323–2329. doi: 10.1056/NEJMsr1110507. [DOI] [PubMed] [Google Scholar]
- 8.Office of the National Coordinator for Health Information Technology, author. Health IT Regulations: Meaningful Use Regulations. [July 11, 2016]. Available from: https://www.healthit.gov/policy-researchers-implementers/meaningful-use-regulations.
- 9.Centers for Medicare and Medicaid Services, author. Medicare and Medicaid EHR Incentive Program Basics. [May 5, 2016]. Available from: https://www.cms.gov/regulations-and-guidance/legislation/ehrincentiveprograms/basics.html.
- 10.Office of the National Coordinator for Health Information Technology, author. EHR Incentives and Certification: EHR Incentive Payment Timeline. [May 6, 2016]. Available from: https://www.healthit.gov/providers-professionals/ehr-incentive-payment-timeline.
- 11.Centers for Medicare and Medicaid Services, author. Medicare Electronic Health Record Incentive Payments for Eligible Professionals. [July 12, 2016]. Available from: https://www.cms.gov/Regulations-and-Guidance/Legislation/EHRIncentivePrograms/Downloads/MLN_MedicareEHRProgram_TipSheet_EP.pdf.
- 12.Centers for Medicare and Medicaid Services, author. Medicaid Electronic Health Record Incentive Payments for Eligible Professionals. [July 12, 2016]. Available from: https://www.cms.gov/Regulations-and-Guidance/Legislation/EHRIncentivePrograms/Downloads/MLN_MedicaidEHRProgram_TipSheet_EP.pdf.
- 13.Office of the National Coordinator for Health Information Technology, author. EHR Incentives and Certification: How to Attain Meaningful Use. [May 6, 2016]. Available from: https://www.healthit.gov/providers-professionals/how-attain-meaningful-use.
- 14.Centers for Medicare and Medicaid Services, author. Quality Payment Program Fact Sheet. [May 2, 2016]. Available from: https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/Value-Based-Programs/MACRA-MIPS-and-APMs/NPRM-QPP-Fact-Sheet.pdf.
- 15.Centers for Medicare and Medicaid Services, author. MACRA RFI Posting “RFI on Physician Payment Reform” (CMS-3321-NC) External FAQ. [May 2, 2016]. Available from: https://innovation.cms.gov/Files/x/macra-faq.pdf.
- 16.Centers for Medicare and Medicaid Services, author. Advancing Care Information Fact Sheet. [May 2, 2016]. Available from: https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/Value-Based-Programs/MACRA-MIPS-and-APMs/Advancing-Care-Information-Fact-Sheet.pdf.
- 17.Jamoom EW, Patel V, Furukawa MF, King J. EHR Adopters vs. Non-adopters: Impacts of, barriers to, and federal initiatives for EHR adoption. Healthc (Amst) 2014;2(1):33–39. doi: 10.1016/j.hjdsi.2013.12.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Blumenthal D. Implementation of the Federal Health Information Technology Initiative. N Engl J Med. 2011;365(25):2426–2431. doi: 10.1056/NEJMsr1112158. [DOI] [PubMed] [Google Scholar]
- 19.Withy K, Dall T, Sakamoto D. Hawai‘i Physician Workforce Assessment 2010. Hawai'i J Med Public Health. 2012;71(4 Suppl 1):6–12. [PMC free article] [PubMed] [Google Scholar]
- 20.Belforte J, Carter J, Reinisch F, Zheng D. State of Hawai‘i Community Health Needs Assessment. Healthcare Association of Hawai‘i; 2013. Jul, [May 8, 2016]. Available from: http://hah.org/wp-content/uploads/2013/12/2013_state_chna.pdf. [Google Scholar]
- 21.Singleton T, Miller P. The Physician Employment Trend: What You Need to Know. Fam Pract Manag. 2015 Jul-Aug;22(4):11–15. [PubMed] [Google Scholar]
- 22.NORC at the University of Chicago, author. Briefing Paper: Understanding the Impact of Health IT in Underserved Communities and those with Health Disparities. 2010. Oct, [August 2, 2015]. Available from: https://www.healthit.gov/sites/default/files/pdf/hit-underserved-communities-health-disparities.pdf.
- 23.Xierali IM, Phillips RL, Green LA, Bazemore AW, Puffer JC. Factors influencing family physician adoption of electronic health records (EHRs) J Am Board Fam Med. 2013;26(4):388–393. doi: 10.3122/jabfm.2013.04.120351. [DOI] [PubMed] [Google Scholar]
- 24.Office of the National Coordinator for Health Information Technology, author. Health IT State Summary: Hawai‘i, Health IT State Summary. 2015. Feb, [June 23, 2015]. Available from: http://dashboard.healthit.gov/quickstats/widget/state-summaries/HI.pdf.
- 25.Friedberg MW, Chen PG, Van Busum KR, et al. Factors Affecting Physician Professional Satisfaction and Their Implications for Patient Care, Health Systems, and Health Policy. RAND Corporation. 2013. http://www.jstor.org/stable/10.7249/j.ctt5hhsc5. [PMC free article] [PubMed]
- 26.Office of the National Coordinator for Health Information Technology, author. Regional Extension Centers (RECs) [July 16, 2016]. Available from: https://www.healthit.gov/providers-professionals/rec-history.
- 27.Chin BJ, Sakuda CM. Transforming and Improving Health Care through Meaningful Use of Health Information Technology. Hawaii J Med Public Health. 2012;71(4 Suppl 1):50–55. [PMC free article] [PubMed] [Google Scholar]
- 28.Centers for Medicare and Medicaid Services, author. Eligible Professional Meaningful Use Core Measures, Measure 7 of 17. [July 17, 2016]. Available from: https://www.cms.gov/Regulations-and-Guidance/Legislation/EHRIncentivePrograms/downloads/Stage2_EPCore_7_PatientElectronicAccess.pdf.
- 29.Turney S. MGMA Letter to HHS Calling for Moratorium on Meaningful Use Penalties. Medical Group Management Association; 2013. Aug, [August 11, 2015]. Available from: http://www.mgma.com/WorkArea/DownloadAsset.aspx?id=1375260. [Google Scholar]
- 30.Office of the National Coordinator for Health Information Technology, author. Electronic Health Record Vendors Reported by Health Care Professionals Participating in the CMS EHR Incentive Programs and ONC Regional Extension Centers Program, Health IT Quick-Stat #30. [July 5, 2015]. Available from: dashboard.healthit.gov/quickstats/pages/FIG-Vendors-of-EHRs-to-Participating-Professionals.php.
- 31.Office of the National Coordinator for Health Information Technology, author. Electronic Health Record Vendors Reported by Hospitals Participating in the CMS EHR Incentive Programs, Health IT Quick-Stat #29. [July 19, 2016]. Available from: dashboard.healthit.gov/quickstats/pages/FIG-Vendors-of-EHRs-to-Participating-Hospitals.php.
- 32.Office of the National Coordinator for Health Information Technology, author. Frequently Asked Questions: How Much is This Going to Cost Me? [July 3, 2015]. Available from: http://www.healthit.gov/providers-professionals/faqs/how-much-going-cost-me.
- 33.Heisey-Grove D, Patel V. ONC Data Brief No. 21: Physician Motivations for Adoption of Electronic Health Records. Washington, DC: Office of the National Coordinator for Health Information Technology; 2014. [July 12, 2015]. Available from: http://www.healthit.gov/sites/default/files/oncdatabrief-physician-ehr-adoption-motivators-2014.pdf. [Google Scholar]
- 34.American Association of Medical Colleges Center for Workforce Studies, author. 2015 State Physician Workforce Data Book. [July 19, 2016]. Available from: http://members.aamc.org/eweb/upload/2015StateDataBook%20(revised).pdf.
- 35.Verdon DR. The EHR Project: How This Rural Practice Took Consistent Steps to Implement an EHR Without Loss of Patient Volume. 2013. Jun 25, [June 25, 2015]. Available from: http://medicaleconomics.modernmedicine.com/medical-economics/content/tags/ehr/ehr-project-interview-melissa-lucarelli-md. Medical Economics.
- 36.Ryan AM, Bishop TF, Shih S, Casalino LP. Small Physician Practices In New York Needed Sustained Help To Realize Gains In Quality From Use Of Electronic Health Records. Health Affairs. 2013;32(1):53–62. doi: 10.1377/hlthaff.2012.0742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.McGregor B, Mack D, Wrenn G, Shim RS, Holden K, Satcher D. Improving Service Coordination and Reducing Mental Health Disparities Through Adoption of Electronic Health Records. Psychiatric services (Washington, DC) 2015;66(9):985–987. doi: 10.1176/appi.ps.201400095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Office of the National Coordinator for Health Information Technology, author. Behavioral Health: Why Focus Health IT on Behavioral Health? [December 2, 2016]. Available from: https://www.healthit.gov/policy-researchers-implementers/behavioral-health.
- 39.Centers for Medicare and Medicaid Services, author. Security Risk Analysis Tip Sheet: Protect Patient Health Information. [May 6, 2016]. Available from: https://www.cms.gov/Regulations-and-Guidance/Legislation/EHRIncentivePrograms/Downloads/2016_SecurityRiskAnalysis.pdf.
- 40.Sakuda C. Lecture presented: Status of the Hawai‘i HIE and the Community Health Record at 2015 Health Workforce and IT Summit. Honolulu, HI: 2015. Sep 19, [Google Scholar]
- 41.Office of the National Coordinator for Health Information Technology, author. HITECH Programs & Advisory Committees: State Health Information Exchange Cooperative Agreement Program. [May 12, 2016]. Available from: https://www.healthit.gov/policy-researchers-implementers/state-health-information-exchange.