Abstract
This article provides an overview of the main controversies in a number of key areas of breast cancer management. Relevant studies that have contributed to guide the treatment of this heterogeneous disease in the field of breast screening, surgery, chemotherapy and radiotherapy are highlighted. Mammography and ultrasound are the main methods of breast screening. MRI and tomosynthesis are emerging as new screening tools for a selected group of breast cancer patients. From a surgical perspective, oncoplastic techniques and neoadjuvant chemotherapy are improving cosmetic results in breast-conserving surgery. For high-risk patients, controversies still remain regarding prophylactic mastectomies. Finally, the appropriate management of the axilla continues evolving with the increasing role of radiotherapy as an alternative treatment to axillary dissection.
Keywords: breast cancer, breast cancer management, breast cancer update
Breast cancer is the most frequent cancer among women in the world with 1.7 million new cancer cases diagnosed in 2012 (25% of all cancers in woman). It is the most common cause of cancer death among women and the second most common cancer death in developed counties after lung cancer [1].
Early detection and improving treatments have been associated with a reduction in breast cancer mortality rate [2]. In the last decade, awareness of the heterogeneous nature of breast cancer through classical histopathological features has been refined by seminal papers using gene-expression profiling techniques [3,4]. Microarray-based gene-expression studies have shown that breast cancer consists of varying groups with distinct molecular features, risk factors, clinical presentation and response to adjuvant therapies [5,6]. The advent of new screening modalities, advances in surgery, radiotherapy and chemotherapy, has allowed a more individualized treatment for breast cancer patients.
This review provides an update in breast cancer management in the areas of screening, surgery, radiotherapy and rationalization for chemotherapy, highlighting the advances in breast cancer treatment.
Breast cancer screening (what are the controversies?)
Early breast cancer can be more effectively treated than advanced stages, when clinical signs and symptoms are present. Breast cancer screening allows detection of breast cancer in an asymptomatic phase and at an early stage. Different types of imaging and image-guided needle biopsies are used for breast screening.
Mammography
Mammography represents the mainstay of breast cancer screening. It has a 77–95% and 94–97% of sensitivity and specificity, respectively [7]. Mammographic screening is associated with a reduction in breast cancer mortality. A recent meta-analysis of eight large randomized controlled trials (RCTs) starting in the 1960s, showed a 19% reduction in the relative risk of breast cancer mortality [8]. However, risk reduction mortality varies according to the age of screening, with women in their 40s and 60s having relative reduction of 15 and 32%, respectively [9].
Screening recommendations vary by country and institution. For instance, in 2009 the US Preventive Services Task Force (USPSTF) updated its mammography recommendations to a biannually routine screening starting at age 50 years [10]. A study from the USA showed that screening mammography decreased slightly in women aged 40–49 years immediately after the USPSTF guidelines were published. However, the screening rate for this age group increased in the following 2 years [11]. Although these recommendations are followed by many European countries, as well as Australia, current guidelines from several USA organizations recommend yearly mammographic screening starting at age 40 years.
Even though mammographic screening has increased the detection of ductal carcinoma in situ (DCIS) and early invasive cancers, the rates of advanced cancer have not changed dramatically in the last three decades. The analysis of data from the Surveillence, Epidemiology and End Results (SEER) program of the National Cancer Institute for Breast Cancer Screening in the USA between 1976 and 2008, demonstrated an increase of 122 early breast cancers per 100,000 women. However, late-stage cancers decreased 8% in that period [12]. This supports the theory that mammography screening detects some cancers that would not progress to an invasive form.
Furthermore, a study by Autier et al. in Sweden showed that breast cancer mortality declined sharply during or soon after the implementation of screening. On retrospective assessment of the mortality rates of women in Sweden aged 40 years or older from 1972 to 2009, a decline in the annual rate of mortality was seen by 0.98% annually after screening had been commenced. The mortality rate declined from 68.4 to 42.8 per 100,000 [13]. More recently a study published by Foca et al. identified results that concurred with Autier et al. identifying a significant and stable decrease in the incidence of late-stage breast cancer from the third year after screening strategies had been implemented on an Italian population and onward with the incidence rate ratio decreasing and varying between 0.81 and 0.71 [14].
The natural history of DCIS is unclear. It has been considered a precursor lesion to invasive cancer, although current evidence of overdiagnosis is challenging this belief.
Overdiagnosis is an ongoing debate related to screening. Although there is no single definition for overdiagnosis, it can be understood as the diagnosis of a condition in an asymptomatic person that does not produce a net benefit for that patient [15]. Overdiagnosis is not misdiagnosis, but rather the concept of a cancer being diagnosed during a patient's lifetime that would not impact their life if not detected.
The existence of overdiagnosis due to mammographic screening is now widely accepted, however, the estimated rates of its occurrence are conflicting. A number of breast working groups have looked at this topic. According to a recent report from the International Agency for Research on Cancer (IARC), the best estimates for overdiagnosis include the differential in the cumulative probabilities of breast cancer detection in screened and unscreened women, after allowing for sufficient lead time. The estimate of overdiagnosis by the Euroscreen Working Group is 6.5% (1–10%) [16]. On assessment of the risks versus the benefit of screening, the European Working Group have concluded that there is still benefit from inviting women 50–69 years of age for screening.
Overtreatment of screen detected DCIS is one of the consequences of overdiagnosis. To date, there is no way to differentiate DCIS that will progress to an invasive cancer from that which will not. The LORIS trial (low-risk DCIS), a Phase III trial, will randomize women with low and intermediate grade of screen detected DCIS, to surgery or to active monitoring [17]. The results of this study will help to identify early breast cancer that can spare surgery.
Providing information about overdiagnosis and overtreatment to women who participate in breast screening programs will help them to make an informed decision about the time and frequency of their breast screening.
Breast ultrasound
The main indication for screening ultrasonography is for women with dense fibroglandular tissue in whom mammographic detection rates are lower. In the presence of dense breasts, the sensitivity of mammography for cancer detection can be as low as 30–48% [18,19]. Dense breasts are usually defined as having 50% or greater glandular tissue in mammography (American College of Radiology [ACR] category 3 and 4).
The ACR also recommends screening breast ultrasonography, in addition to mammography, in women with a high risk of developing breast cancer who cannot undergo MRI. High-risk women are those considered with a BRCA gene mutation or who are untested first-degree relatives of a BRCA carrier, a history of chest irradiation between the ages of 10–30 years for lymphomas and other tumors, and women with 20% or greater lifetime risk of breast cancer [20].
A multicenter study (ACRIN 6666 trial) evaluating screening ultrasound in women at elevated risk of breast cancer, showed that screening ultrasound identified 3.7 additional cancers per 1000 screens in this group [21]. Between 1995 and 2004, six studies were performed to evaluate screening ultrasonography in women of average risk of breast cancer. Across these six series, totaling 42,838 examinations, 150 additional cancers were identified only on breast ultrasound in 126 women, with 90% of these women having dense or heterogeneously dense parenchyma [22]. This supports the view that breast ultrasonography screening is a complementary tool that is more beneficial in women with high breast density.
What is the role of MRI?
Unlike mammography, no randomized trial has ever been conducted to evaluate whether MRI screening can reduce breast cancer mortality [23]. In high-risk patients for breast cancer, a combined mammography screening with MRI has a higher sensitivity compared with mammography alone (90–100% and 25–59%, respectively). However, a lower specificity is seen with the combined method (73–93%) [24]. On the basis of nine trial results, in 2007 the ACS recommended annual screening MRI as a supplement to annual screening mammography for women classified with a high risk of breast cancer [25].
In 2010, the Society of Breast Imaging and the American College of Radiology recommended annual mammography and MRI in BRCA 1/2 carriers starting at age 30 years. In women with 20% or higher lifetime risk of breast cancer, the same recommendation applies. Women with a history of chest irradiation should begin annual mammography and MRI screening 8 years after receiving the treatment but not before age 25 years. For women with a history of breast cancer (invasive cancer or DCIS), ovarian cancer, biopsy-proven lobular neoplasia (ALH or LCIS) or ADH, annual mammography and MRI should also be considered from the time of diagnosis [26].
Recently, an abbreviated protocol (AP) for breast cancer screening with MRI was evaluated in the University Hospital of Aechen in Germany [27]. The study was conducted in 443 women at mild-to-moderate increased risk of breast cancer. In the AP, radiologists read only the first postcontrast subtracted (FAST) and the maximum-intensity projection images, while in the full diagnostic protocol (FDP) all the images were read. The acquisition time of the AP was 3 min and the average time to read the protocol was 2.8 s compared with 17 min and 28 s for FDP, respectively.
The AP was equally effective as FDP finding 11 invasive breast cancers that had escaped detection on regular mammography. The screening accuracy of the AP was similar to that of an FDP, resulting in an additional cancer yield of 18.2 per 1000.
More studies are necessary to support FAST breast MRI as the standard method of breast cancer screening. So far, the evidence shows that FAST MRI screening is safe, accurate and can detect more cancers than mammography.
Digital breast tomosynthesis: a replacement for mammography?
Digital breast tomosynthesis (DBT) is a new imaging technology that produces 3D images with reconstruction into slices, which minimizes the effect of overlapping breast tissue, particularly in women with breast dense parenchyma. The addition of DBT to the standard two-view mammography significantly improves accuracy, mainly due to the reduction of false-positive interpretations [28,29].
A recent systematic review (2475 women from 11 studies) analyzing the validity of tomosynthesis for screening and diagnosis of breast cancer showed that the sensitivity and specificity of tomosynthesis ranged from 69 to 100% and from 54 to 100%, respectively. The authors also found that one-view tomosynthesis was not superior to two-view digital mammography and the evidence for superiority of two-view tomosynthesis was inconclusive [30].
At present, there is insufficient evidence to justify a change in breast screening from standard or digital mammography to DBT. Ongoing studies, such as the TOMMY trial (in the UK) and the Norwegian Oslo study will help to identify the future role of DBT in the detection of early-stage cancers and subtle lesions, particularly in women with dense breasts.
Advances in breast cancer surgery
Sentinel lymph node biopsy
In the last two decades, the development of sentinel lymph node biopsy (SLNB) has revolutionized the surgical management of the axilla in early-stage breast cancer. Numerous studies in the late 1990s and early 2000s compared SLNB with completion of axillary lymph node dissection (ALND). Across all these trials, the sensitivity of SLNB for node involvement ranged from 71 to 100% and the false-negative rate averaged 8.4% [31]. The results from six RCT showed no differences in terms of overall survival (OS), recurrence and disease-free survival (DFS) between SLNB and ALND [32–37]. The largest of these study reported an actuarial 8-year survival rate of 91.8 and 90.3% for ALND and SLNB alone, respectively [37].
In 2005, the American Society of Clinical Oncology supported the use of SLNB as an appropriate alternative staging to routine ALND for breast cancer patients with clinically negative axillary nodes. Moreover, completion of ALND was not required for patients with negative SLNB [31]. Although, ALND was mandatory for patients with positive SLNB, it was not clear at that time whether further nodal dissection improved survival. To answer this question, two RCTs randomly assigned patients with metastasis in SLNs to either completion of ALND or no ALND: ACOSOG Z0011 [38] and IBCSG 23-01 [39].
ACOSOG Z0011 randomly assigned 446 patients to SLNB with no further ALND and 445 to SLNB plus ALND. All patients had T1 or T2 tumors treated with lumpectomy and whole breast radiation therapy. At a median follow-up of 6.3 years, OS and DFS were not statistically significant between arms. It is important to mention that 97% of the patients received adjuvant systemic treatment, 70% had tumors ≤2 cm and more than 80% had a positive estrogen receptor, and thus this was a relatively good prognosis cohort of patients. Furthermore, it is likely that many patients received radiotherapy to the lower axilla.
The IBCSG 23-01 trial was designed for patients with sentinel node micrometastasis. This study enrolled 934 women with a primary breast tumor ≤5 cm from 27 institutions. At a median follow-up of 5 years, DFS and OS were similar among the SLNB and ALND groups (DFS: 87.8 and 84.4%, respectively, log-rank p = 0.16; OS: 97.5 and 97.6%, respectively, log-rank p = 0.73).
Both studies were noninferior in their design. Additionally, the ACOSOG Z0011 trial closed early because it failed to meet accrual targets. Despite this, the current ASCO guidelines recommend that women with one to two metastatic SLNs, who will undergo breast-conserving surgery (BCS) and whole-breast radiotherapy, can safely omit ALND [40].
There are several concerns with this recommendation including the lack of long-term follow-up data and also lack of standardization about radiotherapy fields. There is currently a lack of evidence regarding locoregional recurrence and survival data when it comes to poorer biology tumors. Emerging data from radiation trials such as MA-20 may in fact contradict the policy of not providing definitive radiotherapy/or surgery to the axillary node macrometastasis. It is also likely that the use of adjuvant systemic therapy will muddy the waters in relation to the utility of ALND.
Prophylactic mastectomy
Bilateral prophylactic mastectomy (BPM) is an option in high-risk women who desire to reduce their risk of developing breast cancer. Likewise, women who have unilateral breast cancer may consider contralateral prophylactic mastectomy (CPM) to prevent a second breast cancer. However, as a preventive measure, prophylactic mastectomy remains controversial.
Consideration for BPM has tended to focus on women at high risk as determined by the presence of mutations of BRCA 1 or 2 genes, which are associated with increased risk of breast cancer, or by statistical models of risk estimation, such as the Gail model [41]. A number of case series and retrospective cohort studies indicate that BPM reduces in approximately 90% the incidence of breast cancer in high-risk patients [42–44]. One of these studies, including 639 women at high and moderate risk of breast cancer, reported 81–94% reduction in the risk of dying from breast cancer following BPM after a median follow-up of 14 years [42].
For women who have been diagnosed with a primary breast cancer, several studies have demonstrated that CPM is effective in reducing the risk of contralateral breast cancer. A retrospective study of 745 women who underwent CPM showed a reduction of more than 90%, in breast cancer incidence [45]. Although some retrospective studies have reported a survival benefit after CPM [46,47], a recent Cochrane review concluded that there was limited evidence about whether, and for whom, CPM may actually improve survival [48].
Although, prophylactic mastectomy (PM) can reduce the risk of breast cancer, it does not completely eliminate the risk as not all breast tissue can be removed. One potential benefit from risk reducing surgery is the potential of preventing sequelae of a cancer diagnosis for the patient. This includes the potential of having to have chemotherapy if a high-risk breast cancer is diagnosed in the future. Although not eliminated, this risk is reduced in high-risk patients. It is essential that women who wish to undertake this procedure consider both the benefits and limitations of it, and weigh the risks and benefits of other alternatives, such as chemoprevention, close surveillance or oophorectomy.
When considering a mastectomy, there have been a number of significant breakthroughs in operative technique. These can be subdivided into approaches to the skin and replacement of the gland.
Skin sparing & nipple sparing mastectomy
Maintaining the skin envelop and potentially the nipple–areolar complex has allowed revolutionary outcomes in overall cosmetic results for patients undergoing these procedures. It is important to consider the technical challenges with these skin-preserving procedures based on the size of the breast, ptosis and comorbidities (diabetes, smoking, BMI).
Glandular replacement
After removing all visible breast tissue, replacement of the gland is either by using an implant or autologous techniques. Implant techniques are either one or two stage techniques (expander first and then later a definitive implant is placed). The use of acellular dermal matrix materials (cadaveric and animal derived) has enabled the placement of immediate subpectoral implants with inferior border coverage. The increasing use of lipomodeling techniques has also allowed for revision of any minor deformities associated with these procedures.
Autologous tissue reconstruction is recruited from the back (latissimus dorsi flap) or the abdomen (deep inferior epigastric perforator flap).
The choice between prosthetic or autologous techniques reflects patient factors (such as the size of glandular replacement required and the amount of autologous tissue available) and patient choice, weighing up morbidity and durability of the different procedures. Ultimately, the decision about the choice of reconstruction should involve an informed discussion of the available options together with a discussion of the pros and cons of each.
Surgical margins in BCS
Recent advances in the management of surgical margins in patients treated with breast-conserving therapy have been reported. In the last decade, there was awareness of the increased risk of local recurrence (LR) when surgical margins were positive [49–51], however, there was no consensus on what constituted an adequate negative margin in BCS. The lack of consensus on this topic reflected variations in the surgical management among different institutions and countries. As a consequence, re-excision to achieve wider clear margins was frequently performed, potentially affecting cosmetics results after BCS.
Recently, a multidisciplinary consensus panel [52] published guidelines for the management of surgical margins of patients with stage I and II invasive breast cancer, treated with breast conserving therapy. The guidelines are based on the results of a meta-analysis of 33 studies including 28,162 patients [53]. Positive margins, defined as ‘ink on tumor’, are associated with more than a twofold increase in the risk of ipsilateral breast tumor recurrence (IBTR). This increased risk in recurrence is not decreased by delivery of a radiation boost, systemic therapy (endocrine therapy, chemotherapy, biologic therapy) or favorable biology of the tumor. Therefore, re-excision of positive margins is always recommended. On the other hand, the practice of obtaining wider margins than ‘no ink on tumor’ does not significantly lower the risk of IBTR, and is currently not indicated. From a practical perspective, despite this consensus statement, re-excision of positive margins also depends upon whether the margin is a vertical or radial margin. Generally the surgeon would excise from pectoralis fascia to skin during a wide local excision (lumpectomy) and hence there is less of a tendency to reoperate for anterior or posterior margins even in the setting of positive margins.
A paradigm shift in BCS (oncological principles are important but so is cosmesis)
We have evolved from the belief that breast cancer was a local disease with larger operations leading to better outcomes. This period is best characterized by William Halsted with his classical description of a radical mastectomy, employing a tear-drop incision, removing the whole breast, pectoralis major and axillary contents after dividing the pectoralis minor with a skin graft for wound closure.
Studies from Veronesi's Milan Group [36] and Fisher's NSABP B-O6 [37] demonstrated equivalence of breast lumpectomy plus adjuvant radiotherapy and mastectomy alone. There was a trend toward poor cosmesis after radiotherapy had been completed.
Radiotherapy postsurgical procedures can be associated with a cosmetic deformity, especially when a potential seroma cavity fills and then adheres to the chest wall. This in itself defeats the purpose of breast conservation, which is to ensure the breast tissue looks like a breast without nipple deviation, deformity or asymmetry.
The surgical outcomes of patients who are candidates for breast conservation have improved with the advent of oncoplastic techniques. The integration of plastic surgical techniques into BCS has allowed surgeons to perform larger resections of breast tissue in patients who would otherwise have required mastectomy to achieve clear margins. Oncoplastic surgery (OPS) combines the principle of oncology with those of plastic surgery to optimize oncologic and cosmetic outcomes in patients who decide to conserve their breast.
Clough et al. [54] identified three components that are key for the oncoplastic approach to breast conserving therapy: the excision volume, the tumor location and the glandular density. The authors also proposed a classification based on the amount of breast tissue excised and the level of difficulty of the technique. A level I approach involves less than 20% of the breast volume being excised. The technique comprises dual plate mobilization, with removal of the tumor to pectoral fascia and reapproximation of breast tissue. Skin mobilization involves extensive undermining of the nipple with potential recentralization of the nipple–areola complex. In the level II approach, 20–50% of the breast volume is excised and reduction mammoplasty techniques are used for gland remodeling.
OPS procedures provide oncologic safety, low morbidity and good aesthetic outcomes). Local recurrence reported after OPS is low (between 0 and 7%) [55]. Additionally, in a multicentered study, a higher proportion of excellent aesthetic outcomes were found in patients who underwent OPS compared with patients with lumpectomy alone (p = 0.028) [56]. More studies are necessary to validate these results.
As oncoplastic techniques for BCS has gained acceptance, refinements of its indications, together with an adequate selection of patients and techniques, are critical to obtaining good outcomes.
Chemotherapy to improve BCS
The introduction of adjuvant chemotherapy in the 1970s represented a breakthrough in the management of breast cancer patients. Traditionally, neoadjuvant chemotherapy was used in an effort to improve the DFS in locally advanced breast cancer considered inoperable at the time of the initial presentation.
The use of neoadjuvant therapy is a powerful tool, alongside oncoplastic techniques, for offering women increasing options for breast conservation. In operable breast cancer, neoadjuvant chemotherapy also allows measuring in vivo response to systemic therapy. This response can be evaluated by clinical and pathological parameters.
The results of two large RCT have demonstrated that neoadjuvant systemic therapy increased significantly the rate of BCS over mastectomy [57,58]. Additionally, neoadjuvant treatment has been demonstrated to be as effective as adjuvant therapy in terms of DFS and OS in early breast cancer [59].
Pathologic complete response (pCR) is a useful tool to measure the effectiveness of neoadjuvant treatment. Although, there is no consensus about what constitutes a pCR, the most widely accepted definition is no residual invasive disease in breast and axillary lymph nodes [60]. Although pCR is associated with improved long-term survival outcomes, the use of this measure is as a surrogate end point.
Recent data from the ACOSOG Z1071 trial demonstrated that triple-negative and Her-2-positive breast cancers had the highest rates of pCR (38.2 and 45.4%, respectively; p <0.001) and BCS (46.8 and 43%, respectively; p = 0.019) after neoadjuvant chemotherapy compared with luminal tumors (pCR: 11.4%; BCS: 34.5%) [61].
How do we rationalize chemotherapy options?
One of the main areas of interest in oncological research is the accurate identification of patients who benefit from adjuvant treatments (responders) from those who do not (nonresponders). Multigene assays are currently being used in clinical practice to predict recurrence risk and guide decisions about adjuvant chemotherapy. Oncotype DX®, PAM50 and MammaPrint assays have been validated in retrospective studies.
Large prospective clinical trials are still in progress to further validate multigene assays. The TAILORx trial is a Phase III study for node-negative, estrogen receptor-positive breast cancer patients. It incorporates Oncotype DX recurrence score to randomize patients to hormone therapy alone or hormone therapy plus chemotherapy with an intermediate recurrence score. So far, this study has recruited approximately 7000 women at 900 sites in the USA and Canada. The RxPONDER trial includes the results of the Oncotype DX recurrence score to randomize node-positive breast cancer patients to receive tamoxifen, anastrozole, letrozole or exemestane with or without chemotherapy.
The MINDACT is another multicenter, prospective, Phase III randomized study that compares MammaPrint with Adjuvant! Online to select node-negative breast cancer patients for adjuvant chemotherapy. The randomization is as follows: if both methods classify the patient's risk of relapse as low, adjuvant chemotherapy is withheld; if both methods classify the patient's risk of relapse as high then chemotherapy is proposed; if the methods give discordant results, the patient is randomized to follow the clinical-pathological method (Adjuvant! Online) or to follow the genomic results (MammaPrint). The primary endpoint is to confirm that patients with low risk determined by MammaPrint, and high-risk determined by Adjuvant! Online, can safely spare chemotherapy without compromising survival.
Advances in the genomic field and the emerging data reflecting the heterogeneity of breast cancer disease are currently the focus of ongoing oncological research.
Advances in radiotherapy
Radiotherapy (RT) has improved local-regional control and overall survival of breast cancer patients after BCS [62–64]. A standard course of whole breast radiotherapy consists of 50–50.4 Gy delivered in 25 fractions followed by a 10–16 Gy boost to the tumor bed. The treatment is given 5 days per week, for 5–7 weeks.
New radiotherapy options after BCS
In the last decade, several alternative methods of radiotherapy have been developed to reduce the number of fractions and normal breast tissue exposed to RT. One of these new RT techniques is called hypofractionation, which is defined as the delivery of a larger radiation dose over a shorter period of time than standard RT. To date, three RCT (one from Canada and two from the UK) have demonstrated equivalent local control and cosmetic outcomes between hypofractionation and standard regimens [65–67]. Unfortunately patient selection criteria, doses and fractionation are not uniform among these trials, which has precluded the widespread acceptance of hypofractionation as a standard practice.
Accelerated partial breast irradiation (APBI) delivers high dose of radiation to the postsurgical cavity, sparing normal breast tissue from radiation. APBI can be delivered as brachytherapy, intraoperative radiotherapy and external beam conformal therapy. The ideal patient profile for APBI is still not clearly identified. To date, there are limited data on long-term outcomes with APBI and the best technique for its delivery. Recent reports from the American Society for Radiation Oncology (ASTRO) and the Groupe Européen de Curiethérapie-European Society for Therapeutic Radiology and Oncology (GEC-ESTRO) have suggested selection criteria for ‘suitable patients’ who could receive APBI outside of clinical trials. Currently, there are six ongoing Phase III trials to evaluate APBI.
The TARGIT-A trial is a prospective randomized noninferiority trial in women 45 years and older. Patients were randomized to targeted intraoperative radiotherapy (IORT) or whole breast external beam radiotherapy (EBRT). The predefined noninferiority margin was an absolute difference of 2.5% in the primary endpoint. All randomized patients were included in the intention-to-treat analysis. Nine hundred and ninety-six patients received IORT, whereas 1025 patients received EBRT. The 4-year data has demonstrated six recurrences in the intraoperative radiotherapy arm and five in the external beam arm. The Kaplan–Meier estimate of local recurrence in the conserved breast at 4 years was 1 × 20% (95% CI: 0 × 53 to 2 × 71) in the targeted intraoperative radiotherapy and 0 × 95% (0 × 39 to 2 × 31) in the external beam radiotherapy group (difference between groups 0 × 25%, −1 × 04 to 1 × 54; p = 0 × 41) [68].
Postmastectomy radiotherapy
Improvement in DFS and OS in women with positive axillary nodes with the addition of postmastectomy radiation (PMRT) has been demonstrated in three RCT [69–71]. In these trials, the ipsilateral chest wall and loco-regional lymph node were irradiated. Based on these studies, current guidelines [72,73] recommend postmastectomy radiotherapy for women with four or more positive axillary lymph nodes, but not for most women with node-negative disease.
Controversy remains for patients with one to three lymph nodes involved. Recent evidence has demonstrated that radiation is also beneficial in this group. A meta-analysis analyzed the results of 22 RCT for a total of 8315 patients who had mastectomy and axillary dissection [74]. Patients were randomly assigned to either RT to the chest wall and regional lymph nodes after surgery, or to no RT after surgery.
For 1314 women with one to three positive lymph nodes, RT reduced overall recurrence by 32%, (RR: 0.68; 95% CI: 0.57–0.82, 2; p = 0.00006), and breast cancer mortality by 20% (RR: 0.80; 95% CI: 0.67–0.95, 2; p = 0.01). These benefits were independent to those of adjuvant systemic therapy. For 700 women with axillary dissection and no positive lymph nodes, RT did not show significant effect on local-regional recurrence or breast cancer mortality. Until the results of new trials are available, data from this meta-analysis are the best evidence currently available to guide PMRT in breast cancer women.
Another controversial topic is radiation therapy to the internal mammary and supraclavicular lymph nodes. A meta-analysis of three randomized trials (French [n = 1334 patients], European-EORTC [n = 4004 patients], Canadian [n = 1832 patients], demonstrated that additional regional radiotherapy to the internal mammary and medial supraclavicular nodes statistically significantly improves DFS and overall survival in stage I–III breast cancer [75]. However, it is not yet the standard of care to irradiate the IM-MS lymph nodes irradiation of the internal mammary may be associated with cardiac and pulmonary toxicity. Therefore, the indication of radiotherapy to these nodes should balance potential toxicity versus benefits.
Radiotherapy as treatment for positive axillary nodes
EORTC AMAROS trial evaluated axillary RT as alternative treatment to axillary dissection (ALND) in breast cancer patients with positive lymph nodes [76]. The study included 4806 patients with T1–T2 invasive cancer. Out of the 1425 patients with positive sentinel nodes, 744 were assigned to ALND and 681 to axillary RT. Axillary recurrence at 5 years was 0.43 and 1.19% for patients who received ALND and RT, respectively. The results showed that both treatments are comparable with significantly less lymphedema in the axillary RT arm relative to the ALND arm (5-year incidence 11 vs 23%, respectively).
A newly randomized controlled trial will begin this year conducted by British researchers and the ANZBCTG, to evaluate axillary recurrence in women with early stage breast cancer and metastases in one or two sentinel nodes. Patients will be randomized to no axillary treatment, axillary treatment with axillary clearance or axillary radiotherapy (POSNOC). The hypothesis is that the treatment of residual disease in the axilla does not impact recurrence in early stage breast cancer patients who receive systemic adjuvant therapy.
Conclusion & future perspective
The understanding of the complex nature and biology of breast cancer is allowing multidisciplinary teams to make better decisions regarding treatment. The detection of breast cancer in an early stage has improved survival outcomes. However, evidence about overdiagnosis and overtreatment are challenging breast cancer screening programs. The recognition of early breast cancer, detected by screening, which will not progress to an advance disease, is key to select patients who would benefit from surveillance instead of surgery.
Advances in research relating to breast cancer surgery, such as the management of patients with positive axillary nodes are continually improving. So far, the evidence supports that some patients with early breast cancer and a limited number of positive lymph nodes may avoid axillary dissection without compromising recurrence or survival.
Oncoplastic techniques have improved the management of patients who undergo BCS. Excision volume, tumor location and glandular density are essential to determine the type of oncoplastic approach after BCS.
Increasing use of neoadjuvant chemotherapy has contributed to improved rates of BCS. The identification of breast cancer subtypes that respond better to neoadjuvant treatment is crucial to selecting suitable candidates.
Adjuvant chemotherapy represents an important component of breast cancer treatment. Currently, multigene assays are being used to predict risk of recurrence and select patients who can benefit from adjuvant chemotherapy. The results of ongoing trials will provide evidence to guide decisions regarding adjuvant therapy.
Radiotherapy treatment for breast cancer has also evolved. Postmastectomy radiation has improved outcomes in breast cancer patients with four or more positive lymph nodes. Although recent evidence has also shown benefits for patients with one to three positive axillary nodes after radiation therapy, controversies still remain regarding the management of this group.
Executive summary
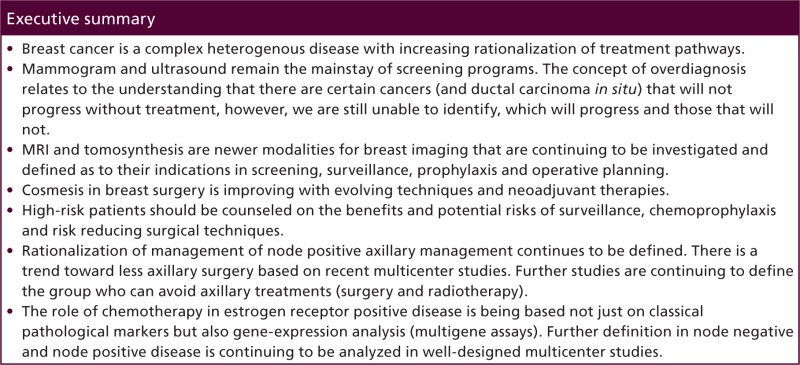
Breast cancer is a complex heterogenous disease with increasing rationalization of treatment pathways.
Mammogram and ultrasound remain the mainstay of screening programs. The concept of overdiagnosis relates to the understanding that there are certain cancers (and ductal carcinoma in situ) that will not progress without treatment, however, we are still unable to identify, which will progress and those that will not.
MRI and tomosynthesis are newer modalities for breast imaging that are continuing to be investigated and defined as to their indications in screening, surveillance, prophylaxis and operative planning.
Cosmesis in breast surgery is improving with evolving techniques and neoadjuvant therapies.
High-risk patients should be counseled on the benefits and potential risks of surveillance, chemoprophylaxis and risk reducing surgical techniques.
Rationalization of management of node positive axillary management continues to be defined. There is a trend toward less axillary surgery based on recent multicenter studies. Further studies are continuing to define the group who can avoid axillary treatments (surgery and radiotherapy).
The role of chemotherapy in estrogen receptor positive disease is being based not just on classical pathological markers but also gene-expression analysis (multigene assays). Further definition in node negative and node positive disease is continuing to be analyzed in well-designed multicenter studies.
Financial & competing interests disclosure
The authors have no relevant affiliations or financial involvement with any organization or entity with a financial interest in or financial conflict with the subject matter or materials discussed in the manuscript. This includes employment, consultancies, honoraria, stock ownership or options, expert testimony, grants or patents received or pending, or royalties.
No writing assistance was utilized in the production of this manuscript.
References
- Papers of special note have been highlighted as: • of interest
- 1.Ferlay J, Soerjomataram I, Dikshit R, et al. Cancer incidence and mortality worldwide: sources, methods and major patterns in GLOBOCAN 2012. Int. J. Cancer 136(5), e359–e386 (2015). [DOI] [PubMed] [Google Scholar]
- 2.Berry DA, Cronin KA, Plevritis SK, et al. Effect of screening and adjuvant therapy on mortality from breast cancer. N. Engl. J. Med. 353 (17), 1784–1792 (2005). [DOI] [PubMed] [Google Scholar]
- 3.Perou CM, Sorlie T, Eisen MB, et al. Molecular portraits of human breast tumours. Nature 406(6797), 747–752 (2000). [DOI] [PubMed] [Google Scholar]
- 4.Prat A, Perou CM. Deconstructing the molecular portraits of breast cancer. Mol. Oncol. 5(1), 5–23 (2011). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Sotiriou C, Pusztai L. Gene-expression signatures in breast cancer. N. Engl. J. Med. 360(8), 790–800 (2009). [DOI] [PubMed] [Google Scholar]
- 6.Weigelt B, Baehner FL, Reis-Filho JS. The contribution of gene expression profiling to breast cancer classification, prognostication and prediction: a retrospective of the last decade. J. Pathol. 220(2), 263–280 (2010). [DOI] [PubMed] [Google Scholar]
- 7.Humphrey LL, Helfand M, Chan BK, Woolf SH. Breast cancer screening: a summary of the evidence for the U.S. Preventive Services Task Force. Ann. Intern. Med. 137(5 Pt 1), 347–360 (2002). [DOI] [PubMed] [Google Scholar]
- 8.Gotzsche PC, Jorgensen KJ. Screening for breast cancer with mammography. Cochrane Database Syst. Rev. 6, CD001877 (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Pace LE, Keating NL. A systematic assessment of benefits and risks to guide breast cancer screening decisions. J. Am. Med. Assoc. 311(13), 1327–1335 (2014). [DOI] [PubMed] [Google Scholar]
- 10.Force USPST. Screening for breast cancer: U.S. Preventive Services Task Force recommendation statement. Ann. Intern. Med. 151(10), 716–726, W–236 (2009). [DOI] [PubMed] [Google Scholar]
- 11.Wang AT, Fan J, Van Houten HK, et al. Impact of the 2009 US Preventive Services Task Force guidelines on screening mammography rates on women in their 40s. PloS ONE 9(3), e91399 (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Bleyer A, Welch HG. Effect of three decades of screening mammography on breast-cancer incidence. N. Engl. J. Med. 367(21), 1998–2005 (2012). [DOI] [PubMed] [Google Scholar]
- 13.Autier P, Héry C, Haukka J, Boniol M, Byrnes G. Advanced breast cancer and breast cancer mortality in randomized controlled trials on mammography screening. J. Clin. Oncol. 27, 5919–5923 (2009). [DOI] [PubMed] [Google Scholar]
- 14.Foca F, Mancini S, Bucchi L, et al. Decreasing incidence of late-stage breast cancer after the introduction of organized mammography screening in Italy. Cancer 119 (11), 2022–2028 (2013). [DOI] [PubMed] [Google Scholar]
- 15.Carter SM, Rogers W, Heath I, Degeling C, Doust J, Barratt A. The challenge of overdiagnosis begins with its definition. Brit. Med. J. 350 h869 (2015). [DOI] [PubMed] [Google Scholar]
- 16.Lauby-Secretan B, Scoccianti C, Loomis D, et al. Breast-cancer screening – viewpoint of the IARC Working Group. N. Engl. J. Med. doi: 10.1056/NEJMsr1504363(2015) (Epub ahead of print). [DOI] [PubMed]
- 17.Francis A, Thomas J, Fallowfield L, et al. Addressing overtreatment of screen detected DCIS; the LORIS trial. Eur. J. Cancer 51(16), 2296–2303 (2015). [DOI] [PubMed] [Google Scholar]
- 18.Mandelson MT, Oestreicher N, Porter PL, et al. Breast density as a predictor of mammographic detection: comparison of interval- and screen-detected cancers. J. Natl Cancer Inst. 92(13), 1081–1087 (2000). [DOI] [PubMed] [Google Scholar]
- 19.Kolb TM, Lichy J, Newhouse JH. Comparison of the performance of screening mammography, physical examination, and breast US and evaluation of factors that influence them: an analysis of 27,825 patient evaluations. Radiologia 225(1), 165–175 (2002). [DOI] [PubMed] [Google Scholar]
- 20.Mainiero MB, Lourenco A, Mahoney MC, et al. ACR appropriateness criteria breast cancer screening. J. Am. Coll. Radiol. 10(1), 11–14 (2013). [DOI] [PubMed] [Google Scholar]
- 21.Berg WA, Zhang Z, Lehrer D, et al. Detection of breast cancer with addition of annual screening ultrasound or a single screening MRI to mammography in women with elevated breast cancer risk. J. Am. Med. Assoc. 307(13), 1394–1404 (2012). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Berg WA. Supplemental screening sonography in dense breasts. Radiol. Clin. North. Am. 2(5), 845–851, vi (2004). [DOI] [PubMed] [Google Scholar]
- 23.Feig S. Cost–effectiveness of mammography, MRI, and ultrasonography for breast cancer screening. Radiol. Clin. North Am. 48(5), 879–891 (2010). [DOI] [PubMed] [Google Scholar]
- 24.Warner E, Messersmith H, Causer P, Eisen A, Shumak R, Plewes D. Systematic review: using magnetic resonance imaging to screen women at high risk for breast cancer. Ann. Intern. Med. 148(9), 671–679 (2008). [DOI] [PubMed] [Google Scholar]
- 25.Saslow D, Boetes C, Burke W, et al. American Cancer Society guidelines for breast screening with MRI as an adjunct to mammography. CA. Cancer J. Clin. 57(2), 75–89 (2007). [DOI] [PubMed] [Google Scholar]
- 26.Lee CH, Dershaw DD, Kopans D, et al. Breast cancer screening with imaging: recommendations from the Society of Breast Imaging and the ACR on the use of mammography, breast MRI, breast ultrasound, and other technologies for the detection of clinically occult breast cancer. J. Am. Coll. Radiol. 7(1), 18–27 (2010). [DOI] [PubMed] [Google Scholar]
- 27.Kuhl CK, Schrading S, Strobel K, Schild HH, Hilgers RD, Bieling HB. Abbreviated breast magnetic resonance imaging (MRI): first postcontrast subtracted images and maximum-intensity projection-a novel approach to breast cancer screening with MRI. J. Clin. Oncol. 32(22), 2304–2310 (2014). [DOI] [PubMed] [Google Scholar]
- 28.Bernardi D, Ciatto S, Pellegrini M, et al. Prospective study of breast tomosynthesis as a triage to assessment in screening. Breast. Cancer. Res. Treat. 133(1), 267–271 (2012). [DOI] [PubMed] [Google Scholar]
- 29.Michell MJ, Iqbal A, Wasan RK, et al. A comparison of the accuracy of film-screen mammography, full-field digital mammography, and digital breast tomosynthesis. Clin. Radiol. 67(10), 976–981 (2012). [DOI] [PubMed] [Google Scholar]
- 30.Garcia-Leon FJ, Llanos-Mendez A, Isabel-Gomez R. Digital tomosynthesis in breast cancer: a systematic review. Radiologia 57(4), 333–343 (2014). [DOI] [PubMed] [Google Scholar]
- 31.Lyman GH, Giuliano AE, Somerfield MR, et al. American Society of Clinical Oncology guideline recommendations for sentinel lymph node biopsy in early-stage breast cancer. J. Clin. Oncol. 23(30), 7703–7720 (2005). [DOI] [PubMed] [Google Scholar]
- 32.Veronesi U, Paganelli G, Viale G, et al. A randomized comparison of sentinel-node biopsy with routine axillary dissection in breast cancer. N. Engl. J. Med. 349(6), 546–553 (2003). [DOI] [PubMed] [Google Scholar]
- 33.Mansel RE, Fallowfield L, Kissin M, et al. Randomized multicenter trial of sentinel node biopsy versus standard axillary treatment in operable breast cancer: the ALMANAC trial. J. Natl Cancer Inst. 98(9), 599–609 (2006). [DOI] [PubMed] [Google Scholar]
- 34.Zavagno G, De Salvo GL, Scalco G, et al. A Randomized clinical trial on sentinel lymph node biopsy versus axillary lymph node dissection in breast cancer: results of the Sentinella/GIVOM trial. Ann. Surg. 247(2), 207–213 (2008). [DOI] [PubMed] [Google Scholar]
- 35.Canavese G, Catturich A, Vecchio C, et al. Sentinel node biopsy compared with complete axillary dissection for staging early breast cancer with clinically negative lymph nodes: results of randomized trial. Ann. Oncol. 20(6), 1001–1007 (2009). [DOI] [PubMed] [Google Scholar]
- 36.Veronesi U, Viale G, Paganelli G, et al. Sentinel lymph node biopsy in breast cancer: ten-year results of a randomized controlled study. Ann. Surg. 251(4), 595–600 (2010). [DOI] [PubMed] [Google Scholar]
- 37.Krag DN, Anderson SJ, Julian TB, et al. Sentinel-lymph-node resection compared with conventional axillary-lymph-node dissection in clinically node-negative patients with breast cancer: overall survival findings from the NSABP B-32 randomised Phase 3 trial. Lancet Oncol. 11(10), 927–933 (2010). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Giuliano AE, Hunt KK, Ballman KV, et al. Axillary dissection vs no axillary dissection in women with invasive breast cancer and sentinel node metastasis: a randomized clinical trial. J. Am. Med. Assoc. 305(6), 569–575 (2011). [DOI] [PMC free article] [PubMed] [Google Scholar]
- •.Landmark paper comparing axillary surgery versus no surgery in node-positive disease that has been practice-changing in USA.
- 39.Galimberti V, Cole BF, Zurrida S, et al. Axillary dissection versus no axillary dissection in patients with sentinel-node micrometastases (IBCSG 23–01): a Phase 3 randomised controlled trial. Lancet Oncol. 14(4), 297–305 (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Lyman GH, Temin S, Edge SB, et al. Sentinel lymph node biopsy for patients with early-stage breast cancer: American Society of Clinical Oncology clinical practice guideline update. J. Clin. Oncol. 32(13), 1365–1383 (2014). [DOI] [PubMed] [Google Scholar]
- 41.Gail MH, Benichou J. Validation studies on a model for breast cancer risk. J. Natl Cancer Inst. 86(8), 573–575 (1994). [DOI] [PubMed] [Google Scholar]
- 42.Hartmann LC, Schaid DJ, Woods JE, et al. Efficacy of bilateral prophylactic mastectomy in women with a family history of breast cancer. N. Engl. J. Med. 340(2), 77–84 (1999). [DOI] [PubMed] [Google Scholar]
- 43.Meijers-Heijboer H, Van Geel B, Van Putten WL, et al. Breast cancer after prophylactic bilateral mastectomy in women with a BRCA1 or BRCA2 mutation. N. Engl. J. Med. 345(3), 159–164 (2001). [DOI] [PubMed] [Google Scholar]
- 44.Rebbeck TR, Friebel T, Lynch HT, et al. Bilateral prophylactic mastectomy reduces breast cancer risk in BRCA1 and BRCA2 mutation carriers: the PROSE study Group. J. Clin. Oncol. 22(6), 1055–1062 (2004). [DOI] [PubMed] [Google Scholar]
- 45.McDonnell SK, Schaid DJ, Myers JL, et al. Efficacy of contralateral prophylactic mastectomy in women with a personal and family history of breast cancer. J. Clin. Oncol. 19(19), 3938–3943 (2001). [DOI] [PubMed] [Google Scholar]
- 46.Herrinton LJ, Barlow WE, Yu O, et al. Efficacy of prophylactic mastectomy in women with unilateral breast cancer: a cancer research network project. J. Clin. Oncol. 23 (19), 4275–4286 (2005). [DOI] [PubMed] [Google Scholar]
- 47.Peralta EA, Ellenhorn JD, Wagman LD, Dagis A, Andersen JS, Chu DZ. Contralateral prophylactic mastectomy improves the outcome of selected patients undergoing mastectomy for breast cancer. Am. J. Surg. 180(6), 439–445 (2000). [DOI] [PubMed] [Google Scholar]
- 48.Lostumbo L, Carbine NE, Wallace J. Prophylactic mastectomy for the prevention of breast cancer. Cochrane Database Syst. Rev. (11), CD002748 (2010). [DOI] [PubMed] [Google Scholar]
- 49.Singletary SE. Surgical margins in patients with early-stage breast cancer treated with breast conservation therapy. Am. J. Surg. 184(5), 383–393 (2002). [DOI] [PubMed] [Google Scholar]
- 50.Morrow M, Strom EA, Bassett LW, et al. Standard for breast conservation therapy in the management of invasive breast carcinoma. CA. Cancer. J. Clin. 52(5), 277–300 (2002). [DOI] [PubMed] [Google Scholar]
- 51.Schwartz GF, Veronesi U, Clough KB, et al. Consensus conference on breast conservation. J. Am. Coll. Surg. 203(2), 198–207 (2006). [DOI] [PubMed] [Google Scholar]
- 52.Moran MS, Schnitt SJ, Giuliano AE, et al. Society of Surgical Oncology-American Society for Radiation Oncology consensus guideline on margins for breast-conserving surgery with whole-breast irradiation in stages I and II invasive breast cancer. J. Clin. Oncol. 32(14), 1507–1515 (2014). [DOI] [PubMed] [Google Scholar]
- •.Consensus group guidelines looking at management of invasive ductal carcinoma.
- 53.Houssami N, Macaskill P, Marinovich ML, Morrow M. The association of surgical margins and local recurrence in women with early-stage invasive breast cancer treated with breast-conserving therapy: a meta-analysis. Ann. Surg Oncol. 21(3), 717–730 (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Clough KB, Kaufman GJ, Nos C, Buccimazza I, Sarfati IM. Improving breast cancer surgery: a classification and quadrant per quadrant atlas for oncoplastic surgery. Ann. Surg. Oncol. 17(5), 1375–1391 (2010). [DOI] [PubMed] [Google Scholar]
- •.Summary description of oncoplastic techniques.
- 55.Franceschini G, Terribile D, Magno S, et al. Update on oncoplastic breast surgery. Eur. Rev. Med. Pharmacol. Sci. 16(11), 1530–1540 (2012). [PubMed] [Google Scholar]
- 56.Santos G, Urban C, Edelweiss MI, et al. Long-term comparison of aesthetical outcomes after oncoplastic surgery and lumpectomy in breast cancer patients. Ann. Surg Oncol. 22(8), 2500–2508 (2014). [DOI] [PubMed] [Google Scholar]
- 57.Fisher B, Brown A, Mamounas E, et al. Effect of preoperative chemotherapy on local-regional disease in women with operable breast cancer: findings from National Surgical Adjuvant Breast and Bowel Project B-18. J. Clin. Oncol. 15(7), 2483–2493 (1997). [DOI] [PubMed] [Google Scholar]
- 58.Bear HD, Anderson S, Smith RE, et al. Sequential preoperative or postoperative docetaxel added to preoperative doxorubicin plus cyclophosphamide for operable breast cancer: National Surgical Adjuvant Breast and Bowel Project Protocol B–27. J. Clin. Oncol. 24(13), 2019–2027 (2006). [DOI] [PubMed] [Google Scholar]
- 59.Mauri D, Pavlidis N, Ioannidis JPA. Neoad- juvant versus adjuvant systemic treatment in breast cancer: a meta-analysis. J. Natl Cancer. Inst. 97, 188–194 (2005). [DOI] [PubMed] [Google Scholar]
- 60.Cortazar P, Zhang L, Untch M, et al. Pathological complete response and long-term clinical benefit in breast cancer: the CTNeoBC pooled analysis. Lancet 384(9938), 164–172 (2014). [DOI] [PubMed] [Google Scholar]
- •.Meta-analysis looking at varying pathological complete responses with neoadjuvant therapies based on luminal subtypes.
- 61.Boughey JC, McCall LM, Ballman KV, et al. Tumor biology correlates with rates of breast-conserving surgery and pathologic complete response after neoadjuvant chemotherapy for breast cancer: findings from the ACOSOG Z1071 (Alliance) prospective multicenter clinical trial. Ann. Surg. 260(4), 608–614; discussion 614–606 (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Early Breast Cancer Trialists' Collaborative G, Darby S, McGale P, et al. Effect of radiotherapy after breast-conserving surgery on 10-year recurrence and 15-year breast cancer death: meta-analysis of individual patient data for 10,801 women in 17 randomised trials. Lancet 378 (9804), 1707–1716 (2011). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Fisher B, Anderson S, Bryant J, et al. Twenty-year follow-up of a randomized trial comparing total mastectomy, lumpectomy, and lumpectomy plus irradiation for the treatment of invasive breast cancer. N. Engl. J. Med. 347(16), 1233–1241 (2002). [DOI] [PubMed] [Google Scholar]
- 64.Veronesi U, Cascinelli N, Mariani L, et al. Twenty-year follow-up of a randomized study comparing breast-conserving surgery with radical mastectomy for early breast cancer. N. Engl. J. Med. 347(16), 1227–1232 (2002). [DOI] [PubMed] [Google Scholar]
- 65.Group ST, Bentzen SM, Agrawal RK, et al. The UK Standardisation of Breast Radiotherapy (START) Trial A of radiotherapy hypofractionation for treatment of early breast cancer: a randomised trial. Lancet Oncol. 9(4), 331–341 (2008). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Group ST, Bentzen SM, Agrawal RK, et al. The UK Standardisation of Breast Radiotherapy (START) Trial B of radiotherapy hypofractionation for treatment of early breast cancer: a randomised trial. Lancet 371(9618), 1098–1107 (2008). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Whelan TJ, Pignol JP, Levine MN, et al. Long-term results of hypofractionated radiation therapy for breast cancer. N. Engl J. Med. 362(6), 513–520 (2010). [DOI] [PubMed] [Google Scholar]
- 68.Vaidya JS, Joseph D, Tobias J, et al. Targeted intraoperative radiotherapy versus whole breast radiotherapy for breast cancer (TARGIT-A trial): an international, prospective, randomised, non-inferiority Phase 3 trial. Lancet 376(9735), 91–102 (2010) [DOI] [PubMed] [Google Scholar]
- 69.Overgaard M, Hansen PS, Overgaard J, et al. Postoperative radiotherapy in high-risk premenopausal women with breast cancer who receive adjuvant chemotherapy. Danish Breast Cancer Cooperative Group 82b Trial. N. Engl. J. Med. 337(14), 949–955 (1997). [DOI] [PubMed] [Google Scholar]
- 70.Overgaard M, Jensen MB, Overgaard J, et al. Postoperative radiotherapy in high-risk postmenopausal breast-cancer patients given adjuvant tamoxifen: Danish Breast Cancer Cooperative Group DBCG 82c randomised trial. Lancet 353(9165), 1641–1648 (1999). [DOI] [PubMed] [Google Scholar]
- 71.Ragaz J, Olivotto IA, Spinelli JJ, et al. Locoregional radiation therapy in patients with high-risk breast cancer receiving adjuvant chemotherapy: 20-year results of the British Columbia randomized trial. J. Natl Cancer Inst. 97(2), 116–126 (2005). [DOI] [PubMed] [Google Scholar]
- 72.Recht A, Edge SB, Solin LJ, et al. Postmastectomy radiotherapy: clinical practice guidelines of the American Society of Clinical Oncology. J. Clin. Oncol. 19 (5), 1539–1569 (2001). [DOI] [PubMed] [Google Scholar]
- 73.Truong PT, Olivotto IA, Whelan TJ, Levine M, Steering Committee on Clinical Practice Guidelines for The C, Treatment of Breast C. Clinical practice guidelines for the care and treatment of breast cancer: 16. Locoregional post-mastectomy radiotherapy. CMAJ 170(8), 1263–1273 (2004). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.EBCTCG, McGale P, Taylor C, et al. Effect of radiotherapy after mastectomy and axillary surgery on 10-year recurrence and 20-year breast cancer mortality: meta-analysis of individual patient data for 8135 women in 22 randomised trials. Lancet 383(9935), 2127–2135 (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Budach W, Kammers K, Boelke E, Matuschek C. Adjuvant radiotherapy of regional lymph nodes in breast cancer – a meta-analysis of randomized trials. Radiat. Oncol. 8, 267 (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Donker M, Van Tienhoven G, Straver ME, et al. Radiotherapy or surgery of the axilla after a positive sentinel node in breast cancer (EORTC 10981-22023 AMAROS): a randomised, multicentre, open-label, Phase 3 non-inferiority trial. Lancet Oncol. 15(12), 1303–1310 (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]