Abstract
Reduced bone mineral density is a strong risk factor for fracture. The WHO's definition of osteoporosis is based on bone mineral density measurements assessed by dual x-ray absorptiometry. Several on other techniques than dual x-ray absorptiometry have been developed for quantitative assessment of bone, for example, quantitative ultrasound and digital x-ray radiogrammetry. Some of these techniques may also capture other bone properties than bone mass that contribute to bone strength, for example, bone porosity and microarchitecture. In this article we give an update on technologies which are available for evaluation primarily of bone mass and bone density, but also describe methods which currently are validated or are under development for quantitative assessment of other bone properties.
Keywords: BMD, bone quality, DXA, DXR, osteoporosis, QCT, QUS
Bone is a mineralized connective tissue, and is comprised of 80% cortical (compact) and 20% trabecular (cancellous) bone. The load-bearing capacity of bone depends on the amount of bone (i.e., mass), the size, the spatial distribution of the bone mass (i.e., geometry and microarchitecture) and the intrinsic properties of the materials that form the bone [1,2]. Osteoporosis is a systemic skeletal disease characterized by low bone mass and microarchitectural deterioration of bone tissue with a consequent increase in bone fragility and susceptibility to fracture [3]. The consequences of fragility fracture are reduced quality of life and increased disability and mortality [4]. Fragility fractures in elderly individuals also cause substantial monetary costs and demand large health resources [5]. Due to the aging of the population worldwide, the number of fragility fractures related to osteoporosis will rise [6]. Thus, osteoporosis is a severe global health problem and a disease which needs to be diagnosed and treated properly. Low bone mass is part of the definition of osteoporosis, and assessment of bone mineral density (BMD) reflecting bone mass is the cornerstone in the diagnosis, risk prediction and monitoring of treatment with antiosteoporotic drugs [5]. BMD has been shown to account for up to 60–90% of the variation in bone strength [7,8].
From BMD to assessment of fracture risk
The WHO operational definition of osteoporosis is based on BMD measurement at the hip (femoral neck and total hip) and/or lumbar spine by dual x-ray absorptiometry (DXA). The definition of normal BMD, osteopenia and osteoporosis is based on DXA BMD cut-off values where the measured BMD values are compared with reference BMD values from young adult females and expressed in standard deviations (SD; T-score). The T-score cut-off for osteoporosis is a BMD value ≤−2.5 SD below the young female adult mean [3]. The operational definition has been refined by WHO with the femoral neck as the proposed standard measurement site, and the use of an international reference standard from young women (NHANES III study) for the calculation of the T-score for both men and women [5,9].
It is controversial to use devices other than DXA for assessment of osteoporosis. The National Osteoporosis Society (NOS) has in their 2011 practical guide “Peripheral x-ray absorptiometry in the management of osteoporosis” [10] emphasized that use of axial DXA is preferable, but acknowledges that the use of less expensive and more convenient methods for evaluation of BMD are appealing. NOS recommends that in centers using peripheral BMD measurements, a triage approach with two thresholds should be applied. The upper thresholds are set to identify those who with 90% certainty would fulfill the WHO criteria for osteoporosis, while the lower threshold have 90% certainly for a normal BMD [10]. Other guidelines such as those from the International Society for Clinical Densitometry (ISCD), National Osteoporosis Foundation (NOF) and American College of Rheumatology (ACR) also make a distinction between diagnostic classification and the use of BMD for fracture risk assessment.
For fracture risk assessment, there is an agreement that many techniques can be applied [11–14]. The guidelines point out that BMD from different devices cannot be directly compared, and T-scores from measurements other than DXA cannot be used for the WHO diagnostic classification. According to these guidelines, DXA is also preferred for treatment decisions. However, if central DXA cannot be performed, assessment of fracture risk can be done on the basis of peripheral measurements and/or clinical risk factors, and treatment can be initiated [13,15].
Several other methods than DXA have been developed to assess BMD, and an increase in fracture risk with declining BMD has been shown using various techniques both at central and peripheral sites [16]. Even though BMD influences fracture risk, many women with fracture do not have low BMD and many women with low BMD do not fracture [17,18].
Several risk prediction algorithms based on fracture risk factors have been developed to estimate future fracture probability [19]. Among these is the FRAX® developed by the WHO, based on individual models that integrate the risk associated with clinical risk factors as well as BMD at the femoral neck. FRAX is designed to estimate a 10-year probability of hip and major osteoporotic fracture among men and women, aged 40–90 years [20]. FRAX can be used with or without BMD. Models for fracture risk prediction have several limitations. For example, in the FRAX model, neither risk of falling nor previous falls are included. Other limitations are that FRAX does not consider the dose–response relationship for number of fractures, alcohol use, smoking, use of glucocorticoids, or low BMD at other sites [21]. On the other hand, it is not certain that more complicated models including more risk factors would give better fracture prediction. In a study by Ensrud and colleagues, including women over 65 years, simple models based on age and BMD alone, or age and fracture history alone predicted 10 year risk of hip, major osteoporotic and clinical fracture, just as good as the more complex FRAX model [22]. In a systematic review including available risk assessment tools for fractures published in 2013 by Rubin et al., complex tools did not perform better than more simple tools [23]. Type II diabetes mellitus is an example of a condition where DXA-BMD and FRAX underestimate the fracture risk, and where other features of bone quality might enhance the fracture prediction [24].
During recent years there has been an increased interest in studying other bone features contributing to bone strength than BMD, for example, finding methods to not only evaluate bone quantity but also bone quality such as bone geometry, microarchitecture and material properties.
In this article we give an update of technologies for assessment of BMD and bone quality.
Technologies for the assessment of BMD
Dual-energy x-ray absorptiometry
The DXA is the gold standard for diagnosis of osteoporosis according to WHO, and is also the method of choice for measurement of BMD in clinical trials [25–27] and observational studies [28,29]. Further, DXA-BMD at the femoral neck is used in the fracture risk assessment tool FRAX [30] which is implemented in several guidelines [5,13,31].
DXA measures the attenuation of x-ray beams with two different energies during radiation transmission. Bone mineral content (BMC) of a region is obtained, and DXA-BMD corresponds to the ratio between BMC and the scanned area. Since it is a 2D measure, larger bones may have higher BMD than smaller bones because of size. Further, DXA does not distinguish between cortical or trabecular bone. DXA can be applied both to measure central (e.g., spine and hip) and peripheral parts of the skeleton (e.g., heel and distal radius). DXA devices with additional laser, for example, DXL techniques are also available [32]. Development of new softwares has also made it possible to assess bone geometry, including hip structural analysis (HSA) and vertebral assessment (VFA) with DXA [2,33–35]. Software for evaluation of bone microarchitecture in the spine is also available. This is based on the analysis of the gray level variation present in the x-ray projected image, which reflects trabecular architecture and is referred to as trabecular bone score (TBS) [36].
Single energy x-ray absorptiometry
Single x-ray absorptiometry (SXA) applies the same principle as DXA, but only one energy beam is used for BMD assessment at the forearm and heel [35]. The tool, which is feasible to use, has been applied in population studies and thus useful in longitudinal studies of old cohort, but has been less used in clinical care [37].
Quantitative computed tomography
Similar to DXA, quantitative computed tomography (QCT) applies a photon absorptiometric technique, but in contrast, the x-ray source and the detector rotate around the subject, and thus permit generation of 3D images. A bone mineral phantom allows calibration of data and provides a volumetric measure of BMD independent of bone size. QCT can differentiate between cortical and trabecular bone and can be used at both central and peripheral skeletal sites [2,33–35]. There is, however, a lack of data validating the QCT method for fracture prediction although some parameters has been shown to be predictive for fracture [38,39]. A QCT device is also included in the list of devices that may be applied for BMD measurements in FRAX.
High resolution peripheral QCT (HRpQCT) is a refinement of QCT. This method has a higher spatial resolution and can be used for assessment of smaller areas at distal skeletal sites. The method can evaluate microarchitecture such as trabecular number, thickness and separation, cortical thickness and porosity [2,33–35].
Quantitative ultrasound
Quantitative ultrasound (QUS) measures velocity (speed of sound) and frequency-dependent attenuation (broadband ultrasound attenuation) and not BMD per se. The speed through bone and how fast energy is lost, depend both on BMD and microarchitectural qualities such as porosity and trabecular connectivity. Thus, this method gives a quantitative measure of bone density, however, not directly comparable to other densitometric tools. QUS is used for measurement at peripheral sites, for example, calcaneus, radius, metacarpal bones and tibia. Several of the developed devices are relatively small and may thus also be portable [2,33–35,40]. QUS measurements have been shown to be predictive for fracture at the same level as measurements by DXA [41,42].
QUS methods for spine are also developed [43], and there are ongoing studies using ultrasound for quantitative measurements of cortical bone at the femoral neck [44].
Radiographic absorptiometry
This method measures BMD in the phalanges by comparing the skeleton to a known reference wedge on radiographs giving BMD in arbitrary units [35]. Radiographic absorptiometry has been shown to be predictive of fractures [45]. An advantage is that portable devices are available [46]. The radiographic absorptiometry device may also be installed on regular x-ray equipment [47].
Conventional radiographs
Plain radiographs are widely available and can give information on bone structure and other aspect of structure and/or bone geometry including textural analysis, for example, at the hip but also at other sites [48,49].
Digital x-ray radiogrammetry (DXR) is a computer version of the traditional technique of radiogrammetry [50] and estimates cortical BMD from defined regions of interest in the second, third and fourth metacarpal bone in the hand. Based on geometrical equations, BMD is calculated from measurements of cortical thickness and bone width and further corrected for porosity and scaled to DXA. Porosity is derived from the area percentage of local intensity minima (hole) in the cortical part relative to the entire cortical area. DXR can be analyzed both from conventional x-rays and from digitized x-rays [51,52]. DXR-BMD has been shown to be predictive of fracture [53]. The potential for measuring porosity might be of importance in fracture risk assessment [54].
Other techniques using plain radiographs are mandible osteoporosis radiography measuring trabecular pattern and mandibular cortical width [55].
MRI
MRI uses a magnetic field and a series of radiofrequency pulses to generate a nonionizing 3D image based on hydrogen in water. Although it can be used for BMD measurements [56], it is mainly used for structural analyses. As there is low water content in bone, MRI gives indirect images of bone microarchitecture via measurements of the marrow and other soft tissues. High resolution MRI applies clinical magnetic resonance scanners combined with specially designed coils to improve resolution, and may be performed at distal sites [2,33–34,57].
Conclusion & future perspective
Features associated with bone quality including macro- and microarchitecture of both cortical and trabecular bone, and biochemical composition of bone tissue have up to now mostly been studied in animal studies or ex vivo. Techniques such as HR-QCT and HR-MRI, have enabled the assessment of the quality of bone also in vivo. These techniques provide information on microarchitecture. When combined with advanced image processing and computational approaches such as finite element analysis modeling techniques, they can be used for prediction of bone structural properties [58–61]. Also for the more traditional techniques DXA, US and DXR, new modes for use and evaluation of bone quality parameters are developed.
Cortical porosity is one of the bone features that have been studied in the last few years. Haversian channels and resorption cavities in cortical bone give rise to a porous bone tissue with pore diameters ranging from a few up to several hundred micrometers [62]. In an ex vivo study with micro CT, Ural et al. showed that intracortical porosity is a significant contributor to the fracture resistance of the bone [63]. Granke et al. observed that change in porosity is the major determinant of the variation of cortical bone elasticity in aged women [64]. Furthermore, Zebaze et al. explored porosity in cortical bone, and found large pores, resulting from intracortical remodeling, thinning the cortex from inside and leaving remnants that looked similar to trabecular bone. Cortical bone loss due to intracortical porosity is poorly captured by DXA [65]. In vivo studies have shown that postmenopausal women with osteopenia have higher cortical porosity at distal radius than women with normal BMD [66]. Age-related differences in cortical porosity, as detected by HR-pQCT, are more pronounced than differences in standard cortical metrics [67]. Cortical porosity is also associated with distal radius fracture [54,68].
There are emerging techniques for examining tissue composition such as infrared and Raman spectroscopy, providing information on the quality of the bone matrix. So far, these measurements have to be performed in bone biopsies [69,70].
Nuclear MRI (NMRI) or solid-state MRI can also be used to provide information on tissue composition. In vivo, the method is limited to analyses of finger, hand and wrist [10,14–15].
Bone turnover has usually been assessed by measuring markers in serum [71]. Recently imaging techniques for exploring bone turnover have been developed, such as dynamic fluorine-18 labeled sodium fluoride positron emission tomography (18F-NaF PET) that allows the quantitative assessment of regional bone formation by measuring the plasma clearance of fluoride to bone at any site in the skeleton [72].
Another measurement of bone strength shown to discriminate patients with fragility fracture is microindentation [73]. There is a relationship between resistance to indentation and mechanical properties influenced by both elastic and plastic behavior of bone tissue [74,75]. Methods for possible intraoperative information about bone strength are also developed such as transpedicular measurement of the peak breakaway torque [76].
Ultrasound has been applied for quantitative measurements, but new in vivo applicable methods permit measurements of fracture-relevant properties, for example, cortical thickness and stiffness at the distal radius and the proximal femur [77].
DXA, the cornerstone in BMD measurements, can also be used for assessment of other parameters than BMD, for example, HSA, VFA or lumbar spine texture analysis using TBS that can enhance fracture prediction [78,79]. A more proactive vertebral assessment is also advocated as in the NOF guidelines [13]. Vertebral assessment can be done on plain x-ray or from DXA [80,81].
There are major differences in precision for the various tools as listed in Table 1. What method and site to choose depends on whether the purpose is for diagnostic use, for fracture risk assessment or for follow-up assessment of bone changes.
Table 1.
Bone assessment techniques in vivo.
| Techniques | Site | Measurements | CV% | Pros | Cons | Ref. |
|---|---|---|---|---|---|---|
| Dual-energy x-ray absorptiometry DXA | Spine, hip, forearm | aBMD/HSA/VFA/TBS | 1–3/2–10†/2/2 | Many validation studies, diagnostics used in WHO definition (aBMD) Can measure several sites and several applications |
Areal measurements and not volumetric Do not distinguish cortical and trabecular bone |
[79,82–84] |
| Radiographic absorptiometry | Phalanx, metacarpals | BMD | 1–2 | Portable devices | No central measure possible | [82] |
| Quantitative computed tomography/high resolution QCT | Spine, hip, forearm | vBMD/microarchitecture | 2–4/1–8† | Separate cortical and trabecular bone Structure analysis Volume BMD can be more correct for very small or very large or obese |
Higher radiation than DXA Less validated |
[74] |
| Digital x-ray radiogrammetry | Metacarpals | ‡DXRBMD/porosity | 0.3–0.5/3§ | Use standard x-ray Low radiation High precision Can be used for historical x-rays |
No central measure possible | [54,85] |
| Quantitative ultrasound | Calcaneus | BUA, SOS | 1.5–4 | Portable devices No radiation |
[82] | |
| MRI | Spine, hip, forearm | Microarchitecture | 2–7† | Microarchitecture Volume and structure No radiation |
Higher costs and low availability Poor precision |
[74] |
| Positron emission tomography | Spine, hip | Bone turnover | 9–14 | Bone turnover | Higher radiation Higher costs and low availability |
[86] |
| Microindentation | Tibia | Hardness/strength | 8–15 | Direct measure of a bone property | Invasive Less validated Poor precision |
[73] |
Depending what parameter and/or site.
BMD estimated from other parameters.
Precision measured ex- vivo.
aBMD: Areal bone mineral density; BMD: Bone mineral density; BUA: Broadband ultrasound attenuation; CV: Coefficient of variation; DXA: Dual x-ray absorptiometry; DXR: Digital x-ray radiogrammetry; HSA: Hip structural analyses; QCT: Quantitative computed tomography; SOS: Speed of sound; TBS: Trabecular bone score; vBMD: Volume bone mineral density; VFA: Vertebral fracture assessment.
The advances in bone assessment technologies provide opportunities to reveal other bone properties contributing to bone strength than BMD. They can address the ‘microarchitectural deterioration’ aspect of the definition of osteoporosis as “…a systemic skeletal disease characterized by low bone mass and microarchitectural deterioration of bone tissue with a consequent increase in bone fragility and susceptibility to fracture” [3]. Moving from bone quantity to bone quality may, in the future, improve fracture prediction. This is of major importance to better identify patients at high risk of fracture and to reduce the burden of osteoporotic fractures in the future.
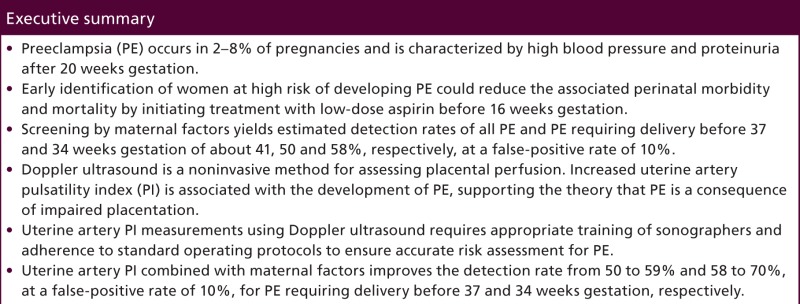
Executive summary
Bone mineral density measured by dual x-ray absorptiometry (DXA) is the cornerstone in diagnostics of osteoporosis according to the WHO criteria.
FRAX or other fracture risk assessment tools can be helpful with or without bone mineral density for fracture prediction.
Other densitometric techniques than DXA can be used for fracture prediction and/or prescreening.
- Bone quality features can improve identification of individuals at high risk. Methods for investigating bone quality in vivo are being developed:
-
-DXA: geometry, trabecular bone score;
-
-HRQCT: microarchitecture, cortical bone, including porosity;
-
-MRI: microarchitecture;
-
-Quantitative ultrasound: cortical thickness, stiffness of bone;
-
-Digital x-ray radiogrammetry: cortical porosity;
-
-Microindentation: hardness of bone.
-
-
Financial & competing interests disclosure
The authors have no relevant affiliations or financial involvement with any organization or entity with a financial interest in or financial conflict with the subject matter or materials discussed in the manuscript. This includes employment, consultancies, honoraria, stock ownership or options, expert testimony, grants or patents received or pending, or royalties.
No writing assistance was utilized in the production of this manuscript.
References
- Papersof special note have been highlighted as: • of interest
- 1.Christiansen BA, Bouxsein ML. Biomechanics of vertebral fractures and the vertebral fracture cascade. Curr. Osteoporosis Rep. 8(4), 198–204 (2010). [DOI] [PubMed] [Google Scholar]
- 2.Bouxsein ML, Seeman E. Quantifying the material and structural determinants of bone strength. Best. Pract. Res. Clin. Rheumatol. 23(6), 741–753 (2009). [DOI] [PubMed] [Google Scholar]
- 3.Assesment of fracture risk and its application to screening for postmenopausal osteoporosis. Technical report WHO (1994). www.who.int [PubMed]
- 4.Morin S, Lix LM, Azimaee M, Metge C, Caetano P, Leslie WD. Mortality rates after incident non-traumatic fractures in older men and women. Osteoporos. Int. 22(9), 2439–2448 (2011). [DOI] [PubMed] [Google Scholar]
- 5.Hernlund E, Svedbom A, Ivergard M, et al. Osteoporosis in the European Union: medical management, epidemiology and economic burden. A report prepared in collaboration with the International Osteoporosis Foundation (IOF) and the European Federation of Pharmaceutical Industry Associations (EFPIA). Arch. Osteoporosis 8(1–2), 136 (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- •.Update on the impact of osteoporosis.
- 6.IOF: Capture the fracture (2012). www.iofbonehealth.org
- •.Initiative to take action for those in high risk for fracture.
- 7.NIH Consensus Development Panel on Osteoporosis Prevention, Diagnosis, and Therapy. Osteoporosis prevention, diagnosis, and therapy. JAMA 285(6), 785–795 (2001). [DOI] [PubMed] [Google Scholar]
- 8.Ammann P, Rizzoli R. Bone strength and its determinants. Osteoporos. Int. 14(Suppl. 3), S13–S18 (2003). [DOI] [PubMed] [Google Scholar]
- 9.WHO Scientific group on the assessment of osteoporosis at primary care level. www.who.int/chp/topics/Osteoporosis.pdf
- 10.Patel R. Peripheral x-ray absorptiometry in the management of osteoporosis (2011). www.nos.org.uk
- 11.Hans DB, Shepherd JA, Schwartz EN, et al. Peripheral dual-energy x-ray absorptiometry in the management of osteoporosis: the 2007 ISCD Official Positions. J. Clin. Densitom. 11(1), 188–206 (2008). [DOI] [PubMed] [Google Scholar]
- 12.Schousboe JT, Shepherd JA, Bilezikian JP, Baim S. Executive summary of the 2013 International Society for Clinical Densitometry Position Development Conference on bone densitometry. J. Clin. Densitom. 16(4), 455–466 (2013). [DOI] [PubMed] [Google Scholar]
- 13.Cosman F, De Beur SJ, Leboff MS, et al. Clinician's guide to prevention and treatment of osteoporosis. Osteoporos. Int. 25(10), 2359–2381 (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.ACR. Position bonedensity measurements. www.rheumatology.org
- 15.NICE. Osteoporosis secondary prevention including strontium ranelate. http://guidance.nice.org.uk/TA161
- 16.Marshall D, Johnell O, Wedel H. Meta-analysis of how well measures of bone mineral density predict occurrence of osteoporotic fractures. BMJ 312(7041), 1254–1259 (1996). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Siris ES, Chen YT, Abbott TA, et al. Bone mineral density thresholds for pharmacological intervention to prevent fractures. Arch. Intern. Med. 164(10), 1108–1112 (2004). [DOI] [PubMed] [Google Scholar]
- 18.Oyen J, Rohde GE, Hochberg M, Johnsen V, Haugeberg G. Low-energy distal radius fractures in middle-aged and elderly women-seasonal variations, prevalence of osteoporosis, and associates with fractures. Osteoporos. Int. 21(7), 1247–1255 (2010). [DOI] [PubMed] [Google Scholar]
- 19.Leslie WD, Lix LM. Comparison between various fracture risk assessment tools. Osteoporos. Int. 25(1), 1–21 (2013). [DOI] [PubMed] [Google Scholar]
- 20.FRAX® WHO Fracture Risk Assessment Tool. www.shef.ac.uk/FRAX
- 21.Silverman SL, Calderon AD. The utility and limitations of FRAX: a US perspective. Curr. Osteoporosis Rep. 8(4), 192–197 (2010). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Ensrud KE, Lui LY, Taylor BC, et al. A comparison of prediction models for fractures in older women: is more better? Arch. Intern. Med. 169(22), 2087–2094 (2009). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Rubin KH, Friis-Holmberg T, Hermann AP, Abrahamsen B, Brixen K. Risk assessment tools to identify women with increased risk of osteoporotic fracture: complexity or simplicity? A systematic review. J. Bone Miner. Res. 28(8), 1701–1717 (2013). [DOI] [PubMed] [Google Scholar]
- •.A review on several tools and clinical risk factors for prediction of fracture.
- 24.De Waard EA, Van Geel TA, Savelberg HH, Koster A, Geusens PP, Van Den Bergh JP. Increased fracture risk in patients with Type 2 diabetes mellitus: an overview of the underlying mechanisms and the usefulness of imaging modalities and fracture risk assessment tools. Maturitas 79(3), 265–274 (2014). [DOI] [PubMed] [Google Scholar]
- 25.Black DM, Thompson DE, Bauer DC, et al. Fracture risk reduction with alendronate in women with osteoporosis: the Fracture Intervention Trial. FIT Research Group. J. Clin. Endocrinol. Metab. 85(11), 4118–4124 (2000). [DOI] [PubMed] [Google Scholar]
- 26.Black DM, Delmas PD, Eastell R, et al. Once-yearly zoledronic acid for treatment of postmenopausal osteoporosis. N. Engl. J. Med. 356(18), 1809–1822 (2007). [DOI] [PubMed] [Google Scholar]
- 27.Cummings SR, Martin J San, McClung MR, et al. Denosumab for prevention of fractures in postmenopausal women with osteoporosis. N. Engl. J. Med. 361(8), 756–765 (2009). [DOI] [PubMed] [Google Scholar]
- 28.Roux C, Cooper C, Diez-Perez A, et al. Prevalence of osteoporosis and fractures among women prescribed osteoporosis medication in five European countries: the POSSIBLE EU study. Osteoporos. Int. 22(4), 1227–1236 (2011). [DOI] [PubMed] [Google Scholar]
- 29.Wade SW, Strader C, Fitzpatrick LA, Anthony MS, O'Malley CD. Estimating prevalence of osteoporosis: examples from industrialized countries. Arch. Osteoporos. 9, 182 (2014). [DOI] [PubMed] [Google Scholar]
- 30.Kanis JA, Oden A, Johansson H, Borgstrom F, Strom O, McCloskey E. FRAX and its applications to clinical practice. Bone 44(5), 734–743 (2009). [DOI] [PubMed] [Google Scholar]
- 31.Compston J, Bowring C, Cooper A, et al. Diagnosis and management of osteoporosis in postmenopausal women and older men in the UK: National Osteoporosis Guideline Group (NOGG) update 2013. Maturitas 75(4), 392–396 (2013). [DOI] [PubMed] [Google Scholar]
- 32.Brismar TB, Janszky I, Toft LI. Calcaneal BMD obtained by dual x-ray and laser predicts future hip fractures – a prospective study on 4 398 Swedish women. J. Osteoporos. 2010, 875647 (2010). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Donnelly E. Methods for assessing bone quality: a review. Clin. Orthop. Relat. Res. 469 (8), 2128–2138 (2011). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Engelke K. Assessment of bone quality and strength with new technologies. Curr. Opin. Endocrinol. Diabetes Obes. 19 (6), 474–482 (2012). [DOI] [PubMed] [Google Scholar]
- 35.Bonnick SL. Bone Densitometry in Clinical Practice (3rd Edition). Humana Press, New York, USA: (2010). [Google Scholar]
- 36.Bousson V, Bergot C, Sutter B, Levitz P, Cortet B. Trabecular bone score (TBS): available knowledge, clinical relevance, and future prospects. Osteoporos. Int. 23(5), 1489–1501 (2012). [DOI] [PubMed] [Google Scholar]
- 37.Omsland TK, Ahmed LA, Gronskag A, et al. More forearm fractures among urban than rural women: the NOREPOS study based on the Tromso study and the HUNT study. J. Bone Miner. Res. 26(4), 850–856 (2011). [DOI] [PubMed] [Google Scholar]
- 38.Rianon NJ, Lang TF, Siggeirsdottir K, et al. Fracture risk assessment in older adults using a combination of selected quantitative computed tomography bone measures: a subanalysis of the age, gene/environment susceptibility – Reykjavik Study. J. Clin. Densitom. 17(1), 25–31 (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Black DM, Bouxsein ML, Marshall LM, et al. Proximal femoral structure and the prediction of hip fracture in men: a large prospective study using QCT. J. Bone Miner. Res. 23(8), 1326–1333 (2008). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Krieg MA, Barkmann R, Gonnelli S, et al. Quantitative ultrasound in the management of osteoporosis: the 2007 ISCD Official Positions. J. Clin. Densitom. 11(1), 163–187 (2008). [DOI] [PubMed] [Google Scholar]
- 41.Moayyeri A, Kaptoge S, Dalzell N, et al. Is QUS or DXA better for predicting the 10 year absolute risk of fracture? J. Bone Miner. Res. 24(7), 1319–1325 (2009). [DOI] [PubMed] [Google Scholar]
- 42.Chan MY, Nguyen ND, Center JR, Eisman JA, Nguyen TV. Quantitative ultrasound and fracture risk prediction in non-osteoporotic men and women as defined by WHO criteria. Osteoporos. Int. 24 (3), 1015–1022 (2013). [DOI] [PubMed] [Google Scholar]
- 43.Garra BS, Locher M, Felker S, Wear KA. Measurements of ultrasonic backscattered spectral centroid shift from spine in vivo: methodology and preliminary results. Ultrasound Med. Biol. 35(1), 165–168 (2009). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Grimal Q, Grondin J, Guerard S, et al. Quantitative ultrasound of cortical bone in the femoral neck predicts femur strength: results of a pilot study. J. Bone Miner. Res. 28(2), 302–312 (2013). [DOI] [PubMed] [Google Scholar]
- 45.Friis-Holmberg T, Brixen K, Rubin KH, Gronbaek M, Bech M. Phalangeal bone mineral density predicts incident fractures: a prospective cohort study on men and women– results from the Danish Health Examination Survey 2007–2008 (DANHES 2007–2008). Arch. Osteoporos. 7(1–2), 291–299 (2012). [DOI] [PubMed] [Google Scholar]
- 46.Dhainaut A, Rohde G, Hoff M, Syversen U, Haugeberg G. Phalangeal densitometry compared with dual energy x-ray absorptiometry for assessment of bone mineral density in elderly women. J. Womens Health (Larchmt). 20(12), 1789–1795 (2011). [DOI] [PubMed] [Google Scholar]
- 47.Dendere R, Whiley SP, Douglas TS. Computed digital absorptiometry for measurement of phalangeal bone mineral mass on a slot-scanning digital radiography system. Osteoporos. Int. 25(11), 2625–2630 (2014). [DOI] [PubMed] [Google Scholar]
- 48.Thevenot J, Hirvasniemi J, Finnila M, et al. Trabecular homogeneity index derived from plain radiograph to evaluate bone quality. J. Bone Miner. Res. 28(12), 2584–2591 (2013). [DOI] [PubMed] [Google Scholar]
- 49.Pulkkinen P, Saarakkala S, Nieminen MT, Jamsa T. Standard radiography: untapped potential in the assessment of osteoporotic fracture risk. Eur. Radiol. 23(5), 1375–1382 (2013). [DOI] [PubMed] [Google Scholar]
- 50.Barnett E, Nordin BE. The radiological diagnosis of osteoporosis: a new approach. Clin. Radiol. 11, 166–174 (1960). [DOI] [PubMed] [Google Scholar]
- 51.Rosholm A, Hyldstrup L, Backsgaard L, Grunkin M, Thodberg HH. Estimation of bone mineral density by digital x-ray radiogrammetry: theoretical background and clinical testing. Osteoporos. Int. 12(11), 961–969 (2001). [DOI] [PubMed] [Google Scholar]
- 52.Ward KA, Cotton J, Adams JE. A technical and clinical evaluation of digital x-ray radiogrammetry. Osteoporos. Int. 14(5), 389–395 (2003). [DOI] [PubMed] [Google Scholar]
- 53.Wilczek ML, Kalvesten J, Algulin J, Beiki O, Brismar TB. Digital x-ray radiogrammetry of hand or wrist radiographs can predict hip fracture risk – a study in 5420 women and 2837 men. Eur. Radiol. 23(5), 1383–1391 (2012). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Dhainaut A, Hoff M, Syversen U, Haugeberg G. Cortical hand bone porosity and its association with distal radius fracture in middle aged and elderly women. PLoS ONE 8(7), e68405 (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Jonasson G, Billhult A. Mandibular bone structure, bone mineral density, and clinical variables as fracture predictors: a 15 year follow-up of female patients in a dental clinic. Oral Surg. 116(3), 362–368 (2013). [DOI] [PubMed] [Google Scholar]
- 56.Ho KY, Hu HH, Keyak JH, Colletti PM, Powers CM. Measuring bone mineral density with fat-water MRI: comparison with computed tomography. J. Magn. Reson. Imaging 37(1), 237–242 (2013). [DOI] [PubMed] [Google Scholar]
- 57.Adams JE. Advances in bone imaging for osteoporosis. Nat. Rev. Endocrinol. 9(1), 28–42 (2012). [DOI] [PubMed] [Google Scholar]
- 58.Christen D, Melton LJ, 3rd, Zwahlen A, Amin S, Khosla S, Muller R. Improved fracture risk assessment based on nonlinear micro-finite element simulations from HRpQCT images at the distal radius. J. Bone Miner. Res. 28(12), 2601–2608 (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Cheung AM, Adachi JD, Hanley DA, et al. High-resolution peripheral quantitative computed tomography for the assessment of bone strength and structure: a review by the Canadian Bone Strength Working Group. Curr. Osteoporos. Rep. 11(2), 136–146 (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Chang G, Rajapakse CS, Babb JS, Honig SP, Recht MP, Regatte RR. In vivo estimation of bone stiffness at the distal femur and proximal tibia using ultra-high-field 7-Tesla magnetic resonance imaging and micro-finite element analysis. J. Bone Miner. Metab. 30(2), 243–251 (2012). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Link TM. Osteoporosis imaging: state of the art and advanced imaging. Radiology 263(1), 3–17 (2012). [DOI] [PMC free article] [PubMed] [Google Scholar]
- •.Comprehensive and more detailed on different technologies dual x-ray absorptiometry, quantitative computed tomography and quantitative ultrasound.
- 62.Augat P, Schorlemmer S. The role of cortical bone and its microstructure in bone strength. Age Ageing. 35 (Suppl. 2), ii27–ii31 (2006). [DOI] [PubMed] [Google Scholar]
- 63.Ural A, Vashishth D. Effects of intracortical porosity on fracture toughness in aging human bone: a microCT-based cohesive finite element study. J. Biomech. Eng 129(5), 625–631 (2007). [DOI] [PubMed] [Google Scholar]
- 64.Granke M, Grimal Q, Saied A, Nauleau P, Peyrin F, Laugier P. Change in porosity is the major determinant of the variation of cortical bone elasticity at the millimeter scale in aged women. Bone 49(5), 1020–1026 (2011). [DOI] [PubMed] [Google Scholar]
- 65.Zebaze RM, Ghasem-Zadeh A, Bohte A, et al. Intracortical remodelling and porosity in the distal radius and postmortem femurs of women: a cross-sectional study. Lancet 375(9727), 1729–1736 (2010). [DOI] [PubMed] [Google Scholar]
- 66.Nishiyama KK, Macdonald HM, Buie HR, Hanley DA, Boyd SK. Postmenopausal women with osteopenia have higher cortical porosity and thinner cortices at the distal radius and tibia than women with normal aBMD: an in vivo HR-pQCT study. J. Bone Miner. Res. 25(4), 882–890 (2010). [DOI] [PubMed] [Google Scholar]
- 67.Burghardt AJ, Kazakia GJ, Ramachandran S, Link TM, Majumdar S. Age- and gender-related differences in the geometric properties and biomechanical significance of intracortical porosity in the distal radius and tibia. J. Bone Miner. Res. 25(5), 983–993 (2010). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Bala Y, Zebaze R, Ghasem-Zadeh A, et al. Cortical porosity identifies women with osteopenia at increased risk for forearm fractures. J. Bone Miner. Res. 29(6), 1356–1362 (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Makowski AJ, Patil CA, Mahadevan-Jansen A, Nyman JS. Polarization control of Raman spectroscopy optimizes the assessment of bone tissue. J. Biomed. Opt. 18(5), 55005 (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Gamsjaeger S, Mendelsohn R, Boskey AL, Gourion-Arsiquaud S, Klaushofer K, Paschalis EP. Vibrational spectroscopic imaging for the evaluation of matrix and mineral chemistry. Curr. Osteoporos. Rep. 12(4), 454–464 (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Szulc P. The role of bone turnover markers in monitoring treatment in postmenopausal osteoporosis. Clin. Biochem. 45(12), 907–919 (2012). [DOI] [PubMed] [Google Scholar]
- 72.Blake GM, Siddique M, Frost ML, Moore AE, Fogelman I. Imaging of site specific bone turnover in osteoporosis using positron emission tomography. Curr. Osteoporos. Rep. 12(4), 475–485 (2014). [DOI] [PubMed] [Google Scholar]
- 73.Diez-Perez A, Guerri R, Nogues X, et al. Microindentation for in vivo measurement of bone tissue mechanical properties in humans. J. Bone Miner. Res. 25 (8), 1877–1885 (2010). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Kazakia GJ, Hyun B, Burghardt AJ, et al. In vivo determination of bone structure in postmenopausal women: a comparison of HR-pQCT and high-field MR imaging. J. Bone Miner. Res. 23(4), 463–474 (2008). [DOI] [PubMed] [Google Scholar]
- 75.Granke M, Coulmier A, Uppuganti S, Gaddy JA, Does MD, Nyman JS. Insights into reference point indentation involving human cortical bone: sensitivity to tissue anisotropy and mechanical behavior. J. Mech. Behav. Biomed. Mater. 37, 174–185 (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Popp AW, Schwyn R, Schiuma D, Keel MJ, Lippuner K, Benneker LM. DensiProbe Spine: an intraoperative measurement of bone quality in spinal instrumentation. A clinical feasibility study. Spine J. 13(10), 1223–1229 (2013). [DOI] [PubMed] [Google Scholar]
- 77.Raum K, Grimal Q, Varga P, Barkmann R, Gluer CC, Laugier P. Ultrasound to assess bone quality. Curr. Osteoporos. Rep. 12(2), 154–162 (2014). [DOI] [PubMed] [Google Scholar]
- 78.Briot K. DXA parameters: beyond bone mineral density. Joint Bone Spine 80(3), 265–269 (2013). [DOI] [PubMed] [Google Scholar]
- 79.Silva BC, Leslie WD, Resch H, et al. Trabecular bone score: a noninvasive analytical method based upon the DXA image. J. Bone Miner. Res. 29(3), 518–530 (2014). [DOI] [PubMed] [Google Scholar]
- 80.Kanterewicz E, Puigoriol E, Garcia-Barrionuevo J, Del Rio L, Casellas M, Peris P. Prevalence of vertebral fractures and minor vertebral deformities evaluated by DXA-assisted vertebral fracture assessment (VFA) in a population-based study of postmenopausal women: the FRODOS study. Osteoporos. Int. 25(5), 1455–1464 (2014). [DOI] [PubMed] [Google Scholar]
- 81.Ferrar L, Roux C, Felsenberg D, Gluer CC, Eastell R. Association between incident and baseline vertebral fractures in European women: vertebral fracture assessment in the Osteoporosis and Ultrasound Study (OPUS). Osteoporos. Int. 23(1), 59–65 (2012). [DOI] [PubMed] [Google Scholar]
- 82.Hawkinson J, Timins J, Angelo D, Shaw M, Takata R, Harshaw F. Technical white paper: bone densitometry. J. Am. Coll. Radiol. 4(5), 320–327 (2007). [DOI] [PubMed] [Google Scholar]
- 83.Khoo BC, Beck TJ, Qiao QH, et al. In vivo short-term precision of hip structure analysis variables in comparison with bone mineral density using paired dual-energy x-ray absorptiometry scans from multi-center clinical trials. Bone 37(1), 112–121 (2005). [DOI] [PubMed] [Google Scholar]
- 84.Guglielmi G, Diacinti D, Van Kuijk C, et al. Vertebral morphometry: current methods and recent advances. Eur. Radiol. 18(7), 1484–1496 (2008). [DOI] [PubMed] [Google Scholar]
- 85.Hoff M, Dhainaut A, Kvien TK, Forslind K, Kalvesten J, Haugeberg G. Short-time in vitro and in vivo precision of direct digital x-ray radiogrammetry. J. Clin. Densitom. 12(1), 17–21 (2009). [DOI] [PubMed] [Google Scholar]
- 86.Al-Beyatti Y, Siddique M, Frost ML, Fogelman I, Blake GM. Precision of 18F-fluoride PET skeletal kinetic studies in the assessment of bone metabolism. Osteoporos. Int. 23(10), 2535–2541 (2012). [DOI] [PubMed] [Google Scholar]