Abstract
Background:
The aim was to analyze the impact of disease management programs on HbA1c values in type 2 diabetes mellitus (T2DM) patients in Germany.
Methods:
This study included 9017 patients followed in disease management programs (DMPs) who started an antihyperglycemic treatment upon inclusion in a DMP. Standard care (SC) patients were included after individual matching (1:1) to DMP cases based on age, gender, physician (diabetologist versus nondiabetologist care), HbA1c values at baseline, and index year. The main outcome was the share of patients with HbA1c <7.5% or 6.5% after at least 6 months and less than 12 months of therapy in DMP and SC groups. Multivariate logistic regression models were fitted with HbA1c level as a dependent variable and the potential predictor (DMP versus SC).
Results:
The mean age was 64.3 years and 54.7% of the patients were men. The mean HbA1c level at baseline was equal to 8.7%. In diabetologist practices, 64.7% of DMP patients and 55.1% of SC patients had HbA1c levels <7.5%, while 23.4% of DMP patients and 16.9% of SC patients had HbA1c levels <6.5% (P values < .001). By comparison, in general practices, 72.4% of DMP patients and 65.7% of SC patients had HbA1c levels <7.5%, while 29.0% of DMP patients and 25.4% of SC patients had HbA1c levels <6.5% (P values < .001). DMPs increased the likelihood of HbA1c levels lower than 7.5% or 6.5% after 6 months of therapy in both diabetologist and general care practices.
Conclusion:
The present study indicates that the enrollment of T2DM patients in DMPs has a positive impact on HbA1c values in Germany.
Keywords: type 2 diabetes, HbA1c, disease management program, DMP
Approximately 9% of adults 18 years and older were affected by diabetes worldwide in 2014, 90% of which had type 2 diabetes mellitus (T2DM).1 Around 1.5 million deaths each year are directly attributable to this chronic disorder.1 In Germany, it is estimated that 1 in every 13 persons suffers from diabetes.2 Thus, the related health and economic burdens are considerable for this country.3
T2DM is considered a major chronic condition, and as such is covered by disease management programs (DMPs) in Germany. DMPs were initially created in the United States and subsequently introduced in Europe in the early 2000s.4,5 The main goal of German DMPs was to improve the quality of health care and the management of patients with chronic disorders.6 Although around 3.9 million people with T2DM were enrolled in 1820 German DMPs in 2013,6 the real impact of such programs is not sufficiently known.7,8
Hemoglobin A1c (HbA1c) values are commonly used to estimate the average concentration of glucose in the plasma over a period of several weeks/months. Several studies have found that HbA1c levels are positively associated with the risk of developing diabetes complications (eg, retinopathy, nephropathy or cardiovascular diseases).9,10 Therefore, the measurement of HbA1c values is a major tool for ensuring proper management and follow-up of patients with T2DM. It has been shown that HbA1c values should be lower than 6.5% in patients with diabetes to prevent the development of such disorders.11,12
The goal of the present study was to analyze the impact of DMPs on HbA1c values in T2DM patients in Germany.
Methods
Database
The Disease Analyzer database (IMS HEALTH) compiles drug prescriptions, diagnoses, basic medical and demographic data obtained directly and in anonymous format from computer systems used in the practices of general practitioners. Diagnoses (ICD-10), prescriptions (Anatomical Therapeutic Chemical [ATC] Classification System), and the quality of reported data have been monitored by IMS based on a number of criteria (eg, completeness of documentation, linkage between diagnoses and prescriptions).
The sampling method for the Disease Analyzer database is based on summary statistics from all doctors through-out Germany published yearly by the German Medical Association (Bundesärztekammer). The statistical unit of IMS uses these statistics to determine the panel design according to the following strata: specialist group, German federal state, community size category, and age of physician.13
In Germany, the sampling methods used for the selection of physicians’ practices were appropriate to obtain a representative database of primary care practices.14 Prescription statistics for several drugs were very similar to data available from pharmaceutical prescription reports.14 The age groups for given diagnoses in the Disease Analyzer database corresponded well with those in relevant disease registries.14
Finally, this database has been already used in several studies focusing on diabetes15-19 and DMPs.20
Study Population
This study included 9017 patients followed in DMPs who started antihyperglycemic treatment (ATC: A10) between 2004 and 2014 after being included in a DMP. Patients were included in the standard care (SC) group when no DMP registration was evident prior to the index date or during follow-up. SC patients were included after individual matching (1:1) to DMP cases based on age, gender, physician (diabetologist versus nondiabetologist care), HbA1c values at baseline, and index year. People younger than 40 years or with HBA1c values lower than 7.5% at baseline were excluded. Patient follow-up lasted 365 days.
Study Outcome and Covariables
The main outcome of the study was the proportion of patients with HbA1c levels <7.5% or <6.5% after at least 6 months and less than 12 months of therapy in the DMP and SC groups. Baseline HbA1c values were defined as the last values within 183 days prior to the index date. Covariables included the number of medical consultations per year, the number of HbA1c level measurements per year, the type of therapy in the first year after treatment initiation (metformin, sulfonylurea, insulin, dipeptidyl peptidase-4 inhibitors [DPP4i], and other drugs, including alpha-glucosidase-inhibitors, glinids, GLP-1, and SGLT-2), and co-occurring diseases (myocardial infarction [ICD 10: I21-23], stroke [I63, I64, G45], coronary heart disease [I24, I25], peripheral arterial disease [I73.9, E11.3], hyperlipidemia [E78], polyneuropathy [E11.4], and renal complications [N18, N19, E11.2]).
Statistical Analyses
Descriptive analyses were obtained for all demographic variables and mean ± SDs were calculated for normally distributed variables. Multivariate logistic regression models were fitted with HbA1c level as a dependent variable and the potential predictor (DMP versus SC). P values < .05 were considered statistically significant. The analyses were carried out using SAS version 9.3.
Results
Patient Characteristics
Socio-demographic data pertaining to the subjects are shown in Table 1. The mean age was 64.3 years (SD 13.2 years) and 54.7% of patients were men. 21.8% of both DMP and SC individuals were treated by a diabetologist, and 75.3% resided in West Germany. The mean of HbA1c levels at baseline was equal to 8.7% (SD 1.7%) in the 2 different groups. The number of medical consultations was slightly higher in DMP patients compared to SC patients (15.8 versus 15.3). The number of HbA1c level measurements was also slightly higher in people followed in DMPs compared to those followed in SCs (3.5 versus 3.2). Metformin was the most frequently prescribed drug during the first year (71.5% and 63.9% in DMPs and SCs, respectively). Last, hyperlipidemia was the most frequent co-occurring disorder (50.3% in DMPs and 47.5% in SCs).
Table 1.
Characteristics of Type 2 Diabetes Patients in DMP and SC Treated in German Primary Care Practices.
| Variable | DMPa | Standard carea | P-valueb |
|---|---|---|---|
| N | 9017 | 9017 | |
| Age (years) | 64.3 (13.2) | 64.3 (13.2) | 1.000 |
| Men (%) | 54.7 | 54.7 | 1.000 |
| Diabetologist care | 21.8 | 21.8 | 1.000 |
| West Germany | 75.3 | 75.3 | 1.000 |
| Index year | |||
| 2004 | 0.1 | 0.1 | 1.000 |
| 2005 | 0.2 | 0.2 | 1.000 |
| 2006 | 4.6 | 4.6 | 1.000 |
| 2007 | 7.2 | 7.2 | 1.000 |
| 2008 | 8.4 | 8.4 | 1.000 |
| 2009 | 9.0 | 9.0 | 1.000 |
| 2010 | 10.1 | 10.1 | 1.000 |
| 2011 | 15.0 | 15.0 | 1.000 |
| 2012 | 15.7 | 15.7 | 1.000 |
| 2013 | 15.8 | 15.8 | 1.000 |
| 2014 | 13.8 | 13.8 | 1.000 |
| HbA1c at baseline (mean, SD) | 8.7 (1.7) | 8.7 (1.7) | 1.000 |
| Number of physician consultations per year (mean, SD) | 15.8 (9.0) | 15.3 (9.7) | <.001 |
| Number of HbA1c measurements per year (mean, SD) | 3.5 (1.1) | 3.2 (1.3) | <.001 |
| Therapy in the first year | |||
| Metformin (%) | 71.5 | 63.9 | <.001 |
| Sulfonylurea (%) | 15.3 | 17.0 | .002 |
| Insulin (%) | 23.3 | 30.6 | <.001 |
| DPP-4 (%) | 15.4 | 17.5 | <.001 |
| Other therapy3 (%) | 4.3 | 4.7 | .161 |
| Number of different therapy classes in the first year | 1.3 (0.5) | 1.3 (0.6) | .806 |
| Codiagnoses | |||
| Myocardial infarction (%) | 6.5 | 7.2 | .063 |
| Stroke (%) | 3.6 | 3.2 | .189 |
| Coronary heart disease (%) | 22.3 | 23.1 | .201 |
| Peripheral arterial disease (%) | 10.3 | 9.5 | .095 |
| Hyperlipidemy (%) | 50.3 | 47.5 | <.001 |
| Polyneuropathy (%) | 13.1 | 12.0 | .040 |
| Renal complications (%) | 13.8 | 11.6 | <.001 |
| Glomerular filtration rate (mean, SD) | 82.9 (25.2) | 80.1 (26.2) | .006 |
Matching based on age, gender, HbA1c value at baseline, physician, and index year. bP value (DMP vs SC): paired t-tests, Wilcoxon tests for paired samples, or McNemar’s tests. c“Other therapy” includes GLP-1, SGLT-2, alpha-glucosidase inhibitors, glitazones, and glinides.
Impact of DMPs on HbA1c Levels in T2DM Patients
Figure 1 shows the proportion of patients with HbA1c values lower than 7.5% or 6.5% in DMPs and SCs after 6 months of therapy in German diabetologist practices. 64.7% of DMP patients and 55.1% of SC patients had HbA1c levels <7.5%, while 23.4% of DMP patients and 16.9% of SC patients had HbA1c levels <6.5% (both P values < .001). Figure 2 shows the proportion of individuals with HbA1c values lower than 7.5% or 6.5% in DMPs and SCs after 6 months of therapy in German general practices. In all, 72.4% of DMP patients and 65.7% of SC patients had HbA1c levels <7.5%, while 29.0% of DMP patients and 25.4% of SC patients had HbA1c levels <6.5% (both P values < .001). The results of the multivariate logistic regression models are shown in Table 2. Enrollment in a DMP was associated with a higher likelihood of exhibiting HbA1c levels lower than 7.5% or 6.5% after 6 months of therapy in both diabetol-ogist and general cares (HbA1c < 7.5%: diabetologist care: OR = 1.40, general practice: OR = 1.21; HbA1c < 6.5%: diabetologist care: OR = 1.42, general practice: OR = 1.14; all P values < .001).
Figure 1.
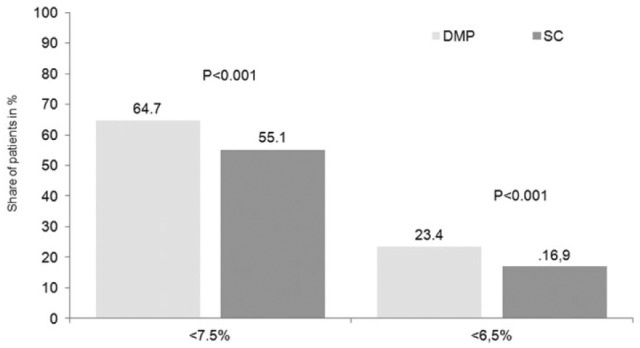
Proportion of patients with HbA1c values lower than 7.5% or 6.5% after 6 months of therapy in German diabetologist practices. DMP, disease management program; SC, standard care.
Figure 2.
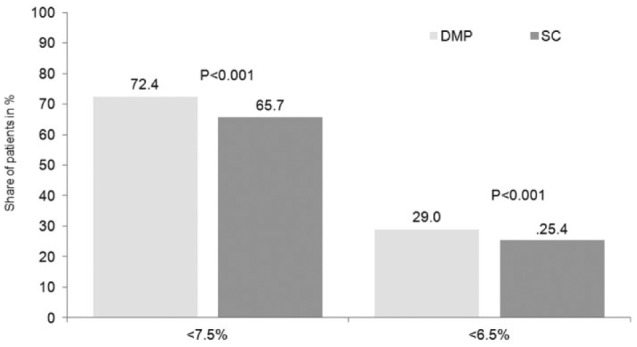
Share of patients with HbA1c values lower than 7.5% or 6.5% after 6 months of therapy in German GP practices. DMP, disease management program; SC, standard care.
Table 2.
Multivariate Logistic Regression Models for the Achievement of HbA1c Goals in Type 2 Diabetes Patients in DMP Versus SC.
| HbA1c goal | Odds ratio (95% CI) for DMP versus SCa | P-value |
|---|---|---|
| HbA1c < 7.5% | ||
| Patients treated by diabetologists | 1.40 (1.22-1.59) | <.001 |
| Patients treated by GPs | 1.21 (1.15-1.34) | <.001 |
| HbA1c < 6.5% | ||
| Patients treated by diabetologists | 1.42 (1.21-1.67) | <.001 |
| Patients treated by GPs | 1.14 (1.06-1.23) | <.001 |
Adjusted by antihyperglycemic therapy (metformin, sulfonylurea, insulin, DPP-4, others) and codiagnoses (myocardial infarction, stroke, coronary heart disease, peripheral arterial disease, hyperlipidemia, polyneuropathy, renal complications).
Discussion
This retrospective study found that DMPs had a positive impact on the reduction of HbA1c levels in German T2DM patients. Interestingly, the effect of DMPs was stronger in people treated in diabetologist practices compared to those treated in general practices.
The impact of DMPs on T2DM in Germany has been the center of a great deal of literature in recent years. In 2014, a systematic literature review comprising 9 studies found that DMPs can improve the care of patients with diabetes.6 As a matter of fact, although these studies differed regarding their characteristics and the parameters analyzed, 3 of them demonstrated that DMP patients had a lower mortality than controls21-24 and 2 of them discovered that DMP participation was associated with an increase in the mean survival time.23,25 Although this review has shed light on the link between DMPs and T2DM in Germany, there are 2 important limitations which must be brought to the fore. First, none of the studies included contained data beyond the year 2008. Thus, since the number of patients enrolled in DMPs has rapidly increased in Europe in recent years, these data are potentially obsolete. Furthermore, one must consider that most of the included works focused on process and economic parameters, as opposed to outcome parameters.6 Therefore, contrary to other countries where the clinical association between DMPs and diabetes has been analyzed by several authors,26-28 the true impact of these management programs on T2DM remains poorly understood in Germany.
The main result of the present work indicates that enrollment in a German DMP improved the reduction of HbA1c levels after 6 months of therapy. These findings corroborate previous data obtained in other regions of the world. In a 2012 meta-analysis of 52 studies, Egginton and colleagues showed that care management for T2DM in the United States is associated with a reduction in HbA1c values.28 It is interesting to note that the same authors also discovered that such measures were particularly effective in patients with high glycated hemoglobin levels. By contrast, results were not significant in a few of the works including small numbers of patients or including individuals with diabetes who exhibited low HbA1c levels at baseline. Although most of these data illustrate that there is a positive correlation between DMPs and the regulation of HbA1c values in diabetes patients, the effect of such programs on this intermediate parameter is still under debate in Europe. In 2011, Berthold et al did not find a significant relation between DMPs and glycated hemoglobin in German outpatients with T2DM.29 Nonetheless, there is one major difference between their work and the current study. Although HbA1c thresholds were not identical (7% versus 6.5% and 7.5%, respectively), it is unlikely that this explains why the 2 studies led to opposite findings. On the other hand, the fact that the cohort used by Berthold and colleagues in their work was created between 2006 and 2007, shortly after the introduction of DMPs in Germany, may explain why they did not find an improvement in the reduction of HbA1c values associated with the enrollment of T2DM patients in such programs. Indeed, one can easily understand that DMPs are complex programs which require several years to show their full efficacy.
Since the impact of DMPs on diabetes remained controversial in Europe—and particularly in Germany—it was suggested that additional measures may assist in the improvement of the treatment and management of patients affected by this chronic condition. Nevertheless, in 2015 Johansson and colleagues found in a study including Austrian T2DM patients that, after 2 years of follow-up, the differences in HbA1c levels did not significantly differ between DMP patients who benefited from additional peer support and patients who were only enrolled in DMPs.30 Such results underline the idea that German DMPs have continued to improve in recent years and that their impact on HbA1c levels is already satisfactory. Finally, our study also showed that the effect of DMPs was stronger in diabetologist practices than in general practices, suggesting that the treatment and management of T2DM patients are more efficient in the former.
In general, retrospective primary care database analyses are limited by the validity and completeness of the data on which they are based. The present study is subject to several limitations, which merit mention at this juncture. First, no valid information was provided on diabetes duration. In addition, the assessment of complications and codiagnoses relied solely on ICD codes provided by primary care physicians. Data in terms of socioeconomic status (eg, education and income) and lifestyle-related risk factors (eg, smoking, alcohol consumption, and physical activity) were also lacking. The strengths of this study are the number of patients included and the duration of the inclusion.
Overall, the present study indicates that the enrollment of T2DM patients in DMPs has a positive impact on HbA1c values in Germany. However, the reason DMP patients exhibit more favorable HbA1c values remains unclear. Further studies including qualitative research, are required to explain this difference.
Footnotes
Abbreviations: ATC, Anatomical Therapeutic Chemical (ATC) Classification System; DMP, disease management program; DPP4i, dipeptidyl peptidase-4 inhibitors; GLP-1, glucagon-like peptid 1; HbA1c, hemoglobin A1c; ICD, International Classification of Diseases; SC, standard care; SD, standard deviation; SGLT-2, sodium dependent glucose transporter; T2DM, type 2 diabetes mellitus.
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
References
- 1. World Health Organization. Diabetes. 2015. Available at: http://www.who.int/mediacentre/factsheets/fs312/en/. Accessed April 1, 2016.
- 2. Statistics—Deutsches Zentrum für Diabetesforschung (DZD). 2015. Available at: https://www.dzd-ev.de/en/diabetes-the-disease/statistics/index.html. Accessed April 1, 2016.
- 3. Köster I, Huppertz E, Hauner H, Schubert I. Costs of diabetes mellitus (CoDiM) in Germany, direct per-capita costs of managing hyperglycaemia and diabetes complications in 2010 compared to 2001. Exp Clin Endocrinol Diabetes. 2014;122:510-516. [DOI] [PubMed] [Google Scholar]
- 4. Ellrodt G, Cook DJ, Lee J, Cho M, Hunt D, Weingarten S. Evidence-based disease management. JAMA. 1997;278:1687-1692. [PubMed] [Google Scholar]
- 5. Busse R. Disease management programs in Germany’s statutory health insurance system. Health Aff Proj Hope. 2004;23:56-67. [DOI] [PubMed] [Google Scholar]
- 6. Fuchs S, Henschke C, Blümel M, Busse R. Disease management programs for type 2 diabetes in Germany. Dtsch Ärztebl Int. 2014;111:453-463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Gerlach FM, Beyer M, Szecsenyi J, Raspe H: [Evaluation of disease management programs–current deficits, demands and methods]. Z Für Ärztl Fortbild Qual. 2003;97:495-501. [PubMed] [Google Scholar]
- 8. Hagen B, Groos S, Kretschmann J, Weber A, Altenhofen L. Qualitätssicherungsbericht 2014. Disease-Management-Programme in Nordrhein. Verlagsservice Baier, Auerstedt. 2015:19-65. [Google Scholar]
- 9. Group TDC and CTR. The relationship of glycemic exposure (HbA1c) to the risk of development and progression of retinopathy in the Diabetes Control and Complications Trial. Diabetes. 1995;44:968-983. [PubMed] [Google Scholar]
- 10. Nathan DM, McGee P, Steffes MW, Lachin JM, Group the DR. Relationship of glycated albumin to blood glucose and glycated hemoglobin (HbA1C) values and to retinopathy, nephropathy and cardiovascular outcomes in the DCCT/EDIC Study. Diabetes. 2014;63:282-90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Del Prato S, Felton AM, Munro N, et al. Improving glucose management: ten steps to get more patients with type 2 diabetes to glycaemic goal. Int J Clin Pract. 2005;59:1345-1355. [DOI] [PubMed] [Google Scholar]
- 12. German Diabetes Association, Matthaei S, Bierwirth R, et al. Medical antihyperglycaemic treatment of type 2 diabetes mellitus: update of the evidence-based guideline of the German Diabetes Association. Exp Clin Endocrinol Diabetes. 2009;117:522-557. [DOI] [PubMed] [Google Scholar]
- 13. Kostev K, Haas G, eds. Medical Care in Germany. Göttingen, Germany: Optimus; 2011. [Google Scholar]
- 14. Becher H, Kostev K, Schröder-Bernhardi D. Validity and representativeness of the “Disease Analyzer” patient database for use in pharmacoepidemiological and pharmacoeconomic studies. Int J Clin Pharmacol Ther. 2009;47:617-626. [DOI] [PubMed] [Google Scholar]
- 15. Rathmann W, Kostev K, Gruenberger JB, Dworak M, Bader G, Giani G. Treatment persistence, hypoglycaemia and clinical outcomes in type 2 diabetes patients with dipeptidyl peptidase-4 inhibitors and sulphonylureas: a primary care database analysis. Diabetes Obes Metab. 2013;15:55-61. [DOI] [PubMed] [Google Scholar]
- 16. Kowall B, Rathmann W, Kostev K. Are sulfonylurea and insulin therapies associated with a larger risk of cancer than metformin therapy? A retrospective database analysis. Diabetes Care. 2015;38:59-65. [DOI] [PubMed] [Google Scholar]
- 17. Jacob L, Kostev K. Prevalence of depression in type 2 diabetes patients in German primary care practices. J Diabetes Complications. 2016;30:432-437. [DOI] [PubMed] [Google Scholar]
- 18. Jacob L, Waehlert L, Kostev K. Changes in type 2 diabetes mellitus patients in German primary care prior to (2006) and after (2010, 2014) launch of new drugs. J Diabetes Sci Technol. 2016;10:414-420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Jacob L, Breuer J, Kostev K. Prevalence of chronic diseases among older patients in German general practices. Ger Med Sci GMS E-J. 2016;14:doc03. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Jacob L, Hadji P, Albert US, Kalder M, Kostev K. Impact of disease management programs on women with breast cancer in Germany. Breast Cancer Res Treat. 2015;153:391-395. [DOI] [PubMed] [Google Scholar]
- 21. Miksch A, Laux G, Ose D, et al. Is there a survival benefit within a German primary care-based disease management program? Am J Manag Care. 2010;16:49-54. [PubMed] [Google Scholar]
- 22. Stock S, Drabik A, Büscher G, et al. German diabetes management programs improve quality of care and curb costs. Health Aff Proj Hope. 2010;29:2197-2205. [DOI] [PubMed] [Google Scholar]
- 23. Drabik A, Büscher G, Thomas K, Graf C, Müller D, Stock S. Patients with type 2 diabetes benefit from primary care-based disease management: a propensity score matched survival time analysis. Popul Health Manag. 2012;15:241-247. [DOI] [PubMed] [Google Scholar]
- 24. Drabik A, Graf C, Büscher G, Stock S. [Evaluating the effectiveness of a disease management program diabetes in the German Statutory Health Insurance: first results and methodological considerations]. Z Für Evidenz Fortbild Qual Im Gesundheitswesen. 2012;106:649-655. [DOI] [PubMed] [Google Scholar]
- 25. Drabik A, Büscher G, Sawicki PT, et al. Life prolonging of disease management programs in patients with type 2 diabetes is cost-effective. Diabetes Res Clin Pract. 2012;95:194-200. [DOI] [PubMed] [Google Scholar]
- 26. Mattke S, Seid M, Ma S. Evidence for the effect of disease management: is $1 billion a year a good investment? Am J Manag Care 2007;13:670-676. [PubMed] [Google Scholar]
- 27. Pimouguet C, Le Goff M, Thiébaut R, Dartigues JF, Helmer C. Effectiveness of disease-management programs for improving diabetes care: a meta-analysis. Can Med Assoc J. 2011;183:E115-127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Egginton JS, Ridgeway JL, Shah ND, et al. Care management for type 2 diabetes in the United States: a systematic review and meta-analysis. BMC Health Serv Res. 2012;12:72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Berthold HK, Bestehorn KP, Jannowitz C, Krone W, Gouni-Berthold I. Disease management programs in type 2 diabetes: quality of care. Am J Manag Care. 2011;17:393-403. [PubMed] [Google Scholar]
- 30. Johansson T, Keller S, Winkler H, et al. Effectiveness of a peer support programme versus usual care in disease management of diabetes mellitus type 2 regarding improvement of metabolic control: a cluster-randomised controlled trial. J. Diabetes Res. 2016:e3248547. [DOI] [PMC free article] [PubMed] [Google Scholar]


