Abstract
Background:
The insulin therapy in type 1 diabetes involves a wide array of restrictions in patients and their families. One of those is a difficulty in estimation of the insulin dose programmed for each meal. The purpose of the study is an assessment of functionalities related to the expert system VoiceDiab—a calculator of meal boluses.
Methods:
The sample group composed of 54 patients, aged 3-52, all suffering from type 1 diabetes, treated with the insulin pump, taking part in the clinics RCT (for adults and a pediatrician), with a randomized allocation to a surveyed group and cross-over. The research methodology was based upon questionnaires and open-ended questions.
Results:
40% of respondents recognized the application’s usefulness as high (18 of 47), giving it 10 points, and easy to use (70%). Disadvantages of this app comprised lack of some products in the application database (n = 23), troubles with the mobile range ( n = 4), and no option of a manual data input for processing purposes (n = 23). Advantages, that have been mentioned the most frequently included facilitation of measurements (n = 7), enhanced life quality of the patient (n = 8), and a guarantee of prompt and thorough calculations (n = 22). Of the surveyed individuals, 50% reached their diet, while 100% gave a top grade to the application, claiming it had contributed to a more efficient metabolic control.
Conclusion:
The pilot scheme of the expert system VoiceDiab has potential to become an application, facilitating dosing of the meal insulin and improving the comfort and safety of insulin administering. However, it needs to be modified, as mentioned by the users who have tested the system.
Keywords: type 1 diabetes, bolus calculator, diet, meal insulin dosing
One of the assumptions of the functional intensive insulin therapy is to offer more freedom in terms of a diet to patients with type 1 diabetes.1 Although a certain progress has been made in this area, in many cases an approach to the diabetes treatment, based on a fear of metabolic destabilization, introduces a vast number of food limitations, often remaining in contrary to the needs and existing eating habits of the patients.2 Moreover, thanks to the surveys, we have become aware that insulin dosing, carried out barely on a basis of carbohydrate amount, does not bring an expected metabolic effect, and eating meals in line with an nutritional schedule, imposing a certain amount of carbohydrate substitutes per meal, is often connected with a consumption of calories that is inadequate to actual needs.3 It refers both to the situation, when the patient does not eat enough as well as when he or she, disturbing his or her natural hunger and satiety mechanism, has his or her meal only to maintain a fixed set of carbohydrate substitutes.
Use of the App for Individualization of the Diabetes Treatment
Individualization of the type 1 diabetes treatment process, conducted on a basis of an intense insulin therapy, compared to conventional methods, releases patients from the inconveniences caused by the so-called diabetes diet. Such an approach imposes the meal plan, that is adjusted to individual needs of a particular body, so to match the age, energy consumed due to physical effort and taste preferences of the patient, and not rigid restrictions and guidelines, taking into consideration instructions on healthy eating addressed to a particular population.4 This model is widely approved by the patients, due to the fact that it frees them, to a large extent, from commitments and limitations involved by the illness. Furthermore, the life they live, though still hard, becomes bearable, turning the daily routine of the sick person into the one he or she used to have before the illness started. Individualization of the type 1 diabetes treatment process also assumes an option of dynamic adjusting to diabetic education, depending on his or her variable needs.5 One of those could be a necessity of introducing elimination diets, often related to celiac disease occurring along with type 1 diabetes, or other diets, responding to specific demands of the patient (low-cholesterol diet, reduced diet, etc).6 It forces the patient to deal with further challenges, as he or she needs to modify his or her eating habits and often completely rearrange his or her daily diet, and therefore learn anew how to measure insulin doses, so to correspond to the meal. In addition, another essential component contributes to nutritional needs, that results from the development stage of patients, covering in particular dietary patterns and selection of toddlers and adolescents, that are often in contrary to traditional recommendations on diabetes treatment.7
As we know from our experience and analyses, a wide range of activities performed by the patients allow for reaching a stable glycemia and a proper metabolic long-term control, while on the other hand, the number of measurements and activities related with bolus programming often appear to be difficult and discouraging for the patients, and the decision-making process referring to relevant insulin dosing is, in many cases, just too complicated.8 The study using the VoiceDiab application was of a pilot type and one of the goals standing behind the analysis of the patient evaluation questionnaires was to acquire an opinion on functionality of the tested application in terms of a daily routine.
The VoiceDiab application ultimately facilitates the dosing process of the meal insulin, enhancing the patient’s security at programming of the meal insulin as well as contributes to the control over the metabolic results of the programmed bolus.
In spite of numerous expert systems provided for meal bolus programming available on the market, they are not widely used by patients on an everyday basis. This issue has not been thoroughly examined yet, and there are no studies that may take into account opinions of patients on the range of functionalities of bolus calculators. This article analyzes the data obtained from the questionnaire, filled in by the patients, after the trial on the tested application.
The purpose of the study was to assess functionalities related to the expert system VoiceDiab applied by patients suffering from type 1 diabetes treated with a personal insulin pump.
Methods
The evaluation questionnaire (EQ) was utilized over two studies, one on adults and another at the pediatrician’s office, delivered within the Voice Expert System for Patients Treated with Insulin project. It was approved by the Bioethical Commission (IMiD 06/13/2014) and is part of a clinical trial (clinical trial number 03/26/2015) crossover study with randomization among two groups. Group A used the mobile phone VoiceDiab application, and a control group (B) applied traditional manual calculations.
The study lasted 4 days for each subgroup (experimental and control). Patients used blinded continuous glucose monitoring. This was a crossover study with a two-week washout period in every group. At the end every patient (or, in the event of the youngest age group, his or her parents) filled an anonymous questionnaire to evaluate the tested system. The questionnaire contained 15 questions, split into three categories (1) usefulness, (2) esthetic and technical criteria, and (3) personal comment of the user. Each question was graded on a 0-10 scale, where 10 means maximum positive usefulness. The grades were rated high (7-10 points), average (4-6 points), and low (0-3 points).
Study Group
The sample group comprised 54 patients suffering from type 1 diabetes, treated with insulin pumps. The questionnaire was filled in by 47 persons. The age of patients within the sample group varied from 3 to 52 years and included 15 males, 32 females. The age groups were divided into the following categories: 3-10, 11-14, 15-18, and >18. For the 3-10 group the EQ was filled by their caregivers.
Results
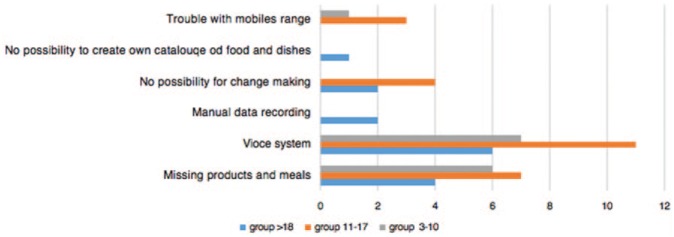
An analysis of 47 filled questionnaires (EQ) has proved that 40% of respondents assessed usefulness of the application as high; 18 out of 47 gave as many as 10 points. Only some individuals considered it low (n = 1). Other patients awarded fewer points, but still above average (see Figure 1). When it comes to difficulty in application management, 70% of users determined it as extremely easy, while the remaining part of the surveyed group, evaluating the application usage, never picked the value less than 5 on a 1-10 grading scale.
Figure 1.
Evaluation of the usefulness of the application.
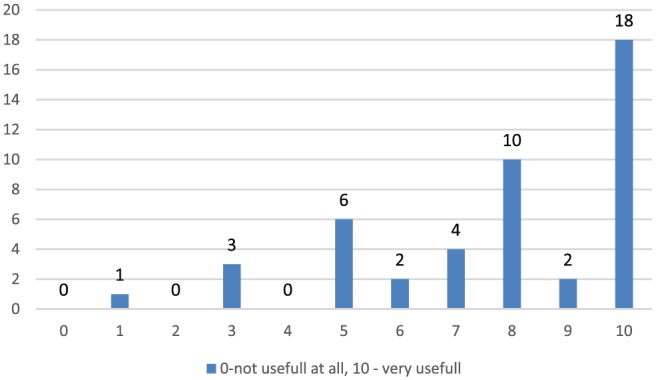
When it comes to the question on disadvantages of the tested application, 40 persons from the sample group pointed out some defects. Answers to another open-ended question on the type of these faults are given in Figure 2.
Figure 2.
Disadvantages of examined system.
The drawbacks indicated by the patients included mostly information on lack of some products in the application database (n = 23), trouble with recognition by the speech analyzer ( n-23), as well as no option of manual data input of data for processing (n = 23).
In the question, where the answerers were supposed to decide whether the application has any advantages, 94% of patients gave a positive answer, and in responses to an open-ended question on that issue, the majority of patients pointed out elements that constituted the base of research assumptions in this project—an application facilitates measurements (n = 7), an application enhances the life quality of the individual with diabetes (n = 8), an application is easy to use (n = 5), an application provides quick and precise measurements (n = 22). An outcome is presented in Figure 3. A vast majority of respondents (87%) declared they would be willing to use the application if it is available—a clear majority within this group (90%) gave their top votes in favor of the application use. Of patients, 81% stated in the questionnaire that the insulin doses indicated in application measurements varied from those they did themselves.
Figure 3.
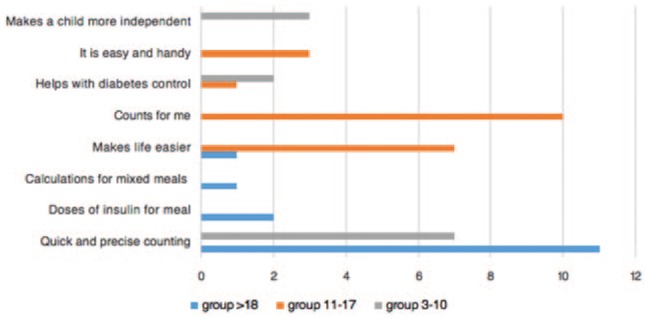
Advantages of examined system.
Comments added to the questionnaire show that more than half of respondents pointed out that the product range included in the application database is insufficient and they advised to supplement it while using the app. In most cases, notes on the lack of data in the product portfolio referred to the variety of particular ingredients, including diversified kinds of meat, cheese, and yogurt as well as dishes coming from different types of cuisines, and those that constitute a component of special diets, such as gluten-free products, vegetarian goods, and vegan items. Of respondents, 34% highlighted an improvement in comfort they felt while using the App, and the reason for a better mood they declared was enhancement of the metabolic balance. Of patients, 40% did not recognize any influence upon their comfort when testing the app. Nonetheless, all the surveyed individuals agreed that this was the system that contributed to a better balancing of their glycemia level. When it comes to this variable, no low grades have been awarded. Nearly 50% of patients also assessed that the application increased the diversification of their diet, since they were able to obtain prompt information, allowing for a quick compensation of a selected meal with a properly adjusted insulin dose, measured through the app. The largest number of difficulties with the regular use of the application occurred within the teenage group, aged 11-14.
As for questions covering technical and IT issues, the majority of answers proved the patients’ satisfaction on the tested solution. Negative assessments of the application given in the responses pointed out mainly two aspects—interdependence of the application usage and access to Internet networks, and difficulties in speech analyzing. In terms of esthetics of the tested app, the overwhelming majority of patients (93%) raised no objections.
Discussion
The expert voice system enclosed in the tested VoiceDiab application is an innovative solution in the bolus measurement area. The EQ filled by the patients using the application as well as an analysis of open-ended questions (with multiple-choice answers) from the questionnaire proved that all the investigated groups were willing to use the app.
Parents of the youngest patients underlined advantages of the application, listing quickness and preciseness of measurements in the light of quite large volatility of nutritional needs among young individuals and necessity of a prompt response with an insulin dose. Adults mostly highlighted benefits of accessibility to meal-related data and they also awarded high grades to the voice system, enabling them to record certain dishes. The largest number of difficulties with the regular use of the application occurred within the teenage group, aged 11-14. For this target, all behaviors revealing their specific situation, involving the social exposure, were considered inconvenient, and the requirement of making recordings in the school environment was often embarrassing to them. In general, this issue has been recognized as a drawback of the application to all the groups involved in the system survey. This article refers to a subjective follow-up evaluation of the application on a basis of a final questionnaire. Overall results show a high interest in a proposed solution and remarks to the tested system may be the inspiration for further modifications and upgrades.
However, taking into account theoretical assumptions referring to the sample model, it is necessary to focus on the fact that nearly half of the respondents were not in favor of using meal recordings, provided by the application. EQ with patients as well as an observation of the way the recordings were made, indicated that they were highly reluctant to reveal activities connected with o recording of meals in the environment involving the social exposure. These were just teenagers, who seemed not to be ready to use the VoiceDiab application at school. It is worth emphasizing the need of setting up a customized dish catalogue, adding and saving those dishes the patient has picked in most cases and putting in new meals and products. The similar opinion of patients was described in the study examining the evaluation of usefulness of Personalize Glucose Advisor in treatment using insulin pumps.9 The questionnaire-based studies prove how important is to focus on individual profile and needs of the patient and his or her family, so to take full advantage of the potential of solutions occurring on the market. One of the issues respondents participating in this survey focused on was a suggestion to provide information on the content of protein and fat in the meal, a functionality the VoiceDiab system actually has.
The staff that educates the patient should each time make an evaluation of the application it offers, not only in terms of health benefits, yet also in terms of other aspects, such as knowledge and expertise on ability to use this particular application of the patient himself or herself, and the goals, the patient has set while choosing it.10 Basing on a personalized approach to the treatment of type 1 diabetes patients, it is advisable that each application offered to the patient should be accompanied by the SWOT (strengths, weaknesses, opportunities, and threats) analysis, that may help determining, whether it will be supportive and helpful, or, perhaps, will be another burden the illness imposes on a sick person.
The SWOT analysis drawn up by the team carrying out the VoiceDiab application project looks as follows. Strengths of the voice system include: promptness and preciseness of measurements, recognition of the bolus type and adjustment of its time to particular needs of the patient, personalization of the treatment process, possibility to carry out measurements in various locations, an easy-to-use device, transparency of data, improvement of life quality, measurement of complex dishes, an option of voice recording of the meal.
When it comes to weaknesses, the following items have to be listed: no measurement history, limited number of products in the database, with no possibility of supplementing them, lack of manual data input, data input solely through a voice option, troubles with speech analyzing, dependence on mobile networks, recording available in the silent environment.
Threats related to using the system comprise misrecognition of the recorded product, which may cause faulty insulin dosing, if the patient remains careless, and the fact that a patient’s education is limited to the user’s manual, with no support from the therapeutic team, which may bring no desired outcome.
Opportunities for the analyzed system are tied to a possibility to use it for education of patients, including particularly the group of patients who seem to be ready to commence a conscious treatment process referring to the illness self-control. In order to achieve more efficient glycemic control, which can be gained through the system, ill persons may obtain quick and easy measurements as well as reduce their reluctance toward the measurement process.
Conclusions
The majority of patients gave positive grades to usefulness and functionality of the expert system VoiceDiab, highlighting a subjective improvement of metabolic control and precise dosing of the meal insulin which was described in a second manuscript. However, there are some areas of the expert system, that need to be rearranged and personalized, as it was shown in the analyzed questionnaires (EQ) completed by the patients. In most cases, it referred to an option enabling to establish one’s own personal dish catalogue and technical background of an application, that would allow for shifting from the speech into the touch mode, and therefore provide some discretion to the users.
Both VD clinical trials have been the first studies worldwide using the speech-based system and therefore the above-mentioned analysis must not be compared to other research output obtained in the area of the expert systems. Undoubtedly, speech-based systems will be practically applied in various fields, including medical devices and mobile applications, and contribute to enhancement of the patients’ decision-making processes.
Certainly, mobile applications are one of the elements delivering support to the patients in the course of type 1 diabetes treatment. A large number of apps that are currently available on the market, misused and deprived of relevant, patient-oriented personalized education, may not provide an expected treatment outcome. Both designing dedicated technological solutions and matching them to patients should be based on an in-depth analysis of the patient’s needs and his or her physical and mental state, which may indicate his or her readiness to use of this very device.
In addition, an increasing number of technological solutions cannot replace the stage of the individual education, conducted by the team of professionals, who work with the patient, and the selection of those has to be each time evaluated by the staff in charge of treatment, not only in terms of advantages of use, but also in terms of the patient’s commitment to apply the support in the treatment control process he or she has been provided with.
Footnotes
Abbreviations: EQ, evaluation questionnaire; SWOT, strengths, weaknesses, opportunities, and threats.
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This study was supported by the Polish National Center for Research and Development grant PBS1/B9/13/2012.
References
- 1. DAFNE Study Group. Training in flexible, intensive insulin management to enable dietary freedom in people with type 1 diabetes: Dose Adjustment for Normal Eating (DAFNE) randomised controlled trial. BMJ. 2002;325(7367):746. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Young V, Eiser C, Johnson B. Eating problems in adolescents with type 1 diabetes: a systematic review with meta-analysis. Diabe Medicine. 2013;189-198. [DOI] [PubMed] [Google Scholar]
- 3. Ayano-Takahara Shiho, Ikeda Kaori, Fujimoto Shimpei, et al. Carbohydrate intake is associated with time spent in the euglycemic range in patients with type 1 diabetes. J Diabetes Investigation. 2015;678-686. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Smart CE, Annan F, Bruno LP, et al. ISPAD clinical practice consensus guidelines 2014. Nutritional management in children and adolescents with diabetes. Pediatr Diabetes. 2014;15(suppl 20):135-153. [DOI] [PubMed] [Google Scholar]
- 5. Smart C, Aslander-van Vliet E, Waldron S. Nutritional management in children and adolescents with diabetes. Pediatr Diabetes. 2009;10(suppl 12):100-117. [DOI] [PubMed] [Google Scholar]
- 6. Kordonouri O, Klingensmith Georgeanna, Knip Mikael, et al. ISPAD clinical practice consensus guidelines 2014. Other complications and diabetes-associated conditions in children and adolescents. Pediatr Diabetes. 2014;15(suppl 20):270-278. [DOI] [PubMed] [Google Scholar]
- 7. Wheeler BJ, Lawrence J, Chae M, et al. Intuitive eating is associated with glycaemic control in adolescents with type I diabetes mellitus. Elsevier. 2015;160-165. [DOI] [PubMed] [Google Scholar]
- 8. Schmidt S, Norgaard K. Bolus calculators. J Diabetes Sci Technol. 2014;8(5):1035-1041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Shepard JA, Gonder-Frederic L, Vajda K, et al. Patient perspectives on personalized glucose advisory systems for type 1 diabetes management. Diabetes Technol Ther. 2012;14(10): 858-861. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Ristau Ryan A., Yang Jessica, White John R., et al. Evaluation and evolution of diabetes mobile applications: key factors for health care professionals seeking to guide patients. Diabetes Spectrum. 2013;26(4):211-215. [Google Scholar]