Abstract
Background
Falling duration of psychiatric inpatient stays over the past two decades and recent recommendations to tighten federal regulation of electroconvulsive therapy (ECT) devices have focused attention on trends in ECT use, but current national data have been unavailable.
Methods
We calculated the annual number of inpatient stays involving ECT and proportion of general hospitals conducting the procedure at least once in the calendar year using a national sample of discharges from 1993–2009. We estimated adjusted probabilities that inpatients with severe recurrent major depression (N=465,646) were treated in a hospital which conducts ECT and, if so, received the procedure.
Results
The annual number of stays involving ECT fell from 12.6 to 7.2 per 100,000 adult US residents, driven by dramatic declines among the elderly, while the percentage of hospitals conducting ECT decreased from 14.8% to 10.6%. The percentage of stays for severe recurrent major depression in hospitals which conducted ECT fell from 70.5% to 44.7%, while receipt of ECT where conducted declined from 12.9% to 10.5%. For depressed inpatients, the adjusted probability that the treating hospital conducts ECT fell 34%, while probability of receiving ECT was unchanged for patients treated in facilities which conducted the procedure. Adjusted declines were greatest for the elderly. Throughout the period inpatients from poorer neighborhoods or who were publicly- or un-insured were less likely receive care from hospitals conducting ECT.
Conclusions
ECT use for severely depressed inpatients has fallen markedly, driven exclusively by a decline in the probability that their hospital conducts ECT.
Keywords: recurrent major depression, electroconvulsive therapy (ECT), hospital psychiatry, somatic therapy, general hospitals, mental health services
INTRODUCTION
Professional medical guidelines recommend electroconvulsive therapy (ECT) as the treatment of choice for depression resistant to multiple trials of antidepressant pharmacotherapy and for depressive episodes with psychotic features, catatonia, severe suicidality, or food refusal with nutritional compromise (1). ECT is also widely regarded as the most efficacious treatment for major depressive disorder (2). However, a number of factors may have contributed to the limited and highly uneven use of the procedure in the US (3), including concerns over the adverse effect of memory loss; the popular perception of ECT as antiquated, unsafe, or even inhumane; state regulations restricting ECT use (4); and the specialized equipment and personnel and close clinical supervision required to conduct ECT (1).
Questions about ECT availability have been also been prompted by uncertainty surrounding a pending US Food and Drug Administration (FDA) regulatory decision. Opponents of tighter regulation of ECT devices have argued new restrictions would reduce use of a procedure already unavailable in many geographic areas (3, 5) and obstruct evidence-based care of the most severe and treatment-resistant depression (6). Because the most recent published national trends in ECT utilization date from 1992 (7), there is little information regarding use of ECT to inform US policy discussion.
We examined national patterns and trends in the use of inpatient ECT in a national hospital sample over a 17-year period from 1993 to 2009. We tested whether observed trends can be explained by changing patient, hospital, and inpatient unit characteristics and whether particular characteristics have been associated with more rapid changes.
METHOD
Data Source
We analyzed data for the years 1993 to 2009 from the Nationwide Inpatient Sample (NIS), a nationally representative survey of US community hospitals conducted annually by the Agency for Healthcare Research and Quality (AHRQ). Community hospitals are designated annually as nonfederal, short-term, general, or specialty hospitals, including both public and private facilities and academic medical centers (8). Excluded are freestanding psychiatric and chemical dependency facilities, long-term hospitals, hospital units of institutions, and short-term rehabilitation hospitals. A 20% sample of all community hospitals is surveyed in a stratified process based on five hospital characteristics: census region, control (public, private not-for-profit, or private investor-owned), urbanicity (urban or rural), teaching status, and bed size (small, medium, or large). We refer to participating facilities as general rather than community hospitals elsewhere in the manuscript to avoid creating an erroneous impression that tertiary care hospitals are excluded.
Hospitals provide abstracts of all discharges in the calendar year. Annual NIS databases contain 5–8 million discharge abstracts from approximately 1,000 hospitals, including up to 15 diagnoses and procedures. We use the term inpatient stay interchangeably with hospital discharge throughout the manuscript. Following AHRQ recommendations, we examined years following 1992 employing designated trend variables and weights (9).
Subjects and Outcome
To estimate the annual number of inpatient stays involving ECT, we identified all stays with ECT administration (ICD-9-CM code 94.27). This yielded a 20% sample of 83,485 stays, producing a weighted estimate of 424,235 stays nationally over the period. To examine inpatient ECT use for depression, we analyzed stays of inpatients aged ≥18 years with a principal diagnosis of recurrent major depression, current episode severe with or without psychotic features (ICD-9-CM codes 296.34 or -3). This yielded a 20% sample of 465,646, producing an estimate of 2,322,504 (consisting of 35% with and 65% without psychotic features).
Characteristics of Inpatient Stays for Recurrent Major Depression
Patient characteristics included age, sex, race/ethnicity, the presence of psychotic features, admission source, income in the patient’s ZIP code, and primary payer. From secondary diagnoses we also identified deliberate self-harm events (E950-E959), psychiatric co-morbidities (290–319), co-morbid medical conditions that might increase the risk of ECT (1, 10) (diagnoses available on request), and other general medical co-morbidities. Hospital characteristics included census region and urbanicity, size, teaching status, and whether the hospital conducted ECT in any inpatient stay for any principal diagnosis during the calendar year. Inpatient unit characteristics consisted of whether a specialty psychiatric unit was the likely site of care. Using a method developed and validated by AHRQ with these data, we classified depression stays within hospitals with at least 300 annual mental health stays as occurring on a psychiatric unit or unit scatter bed (11).
Statistical Analyses
Describing trends in ECT use
We described the annual number of hospital stays involving ECT administration per 100,000 US residents using US Census population estimates (12). We also described the annual number and percentage of community hospitals conducting the procedure and, among hospitals with a psychiatric unit, the percentage conducting the procedure. Among hospital conducting ECT, the number of stays involving ECT per hospital were calculated. Among inpatients treated for severe recurrent major depression, we calculated annual percentage treated in hospitals which conducted ECT, and for those treated where ECT was conducted, the percentage who received the procedure.
Testing sources of the observed trend in ECT use
We tested for linear time trends in use of ECT with two sets of logistic models intended to disaggregate two potential sources of change: (1) change in the probability that a depressed inpatient’s treating hospital conducted versus did not conduct ECT and (2) change in the probability that an inpatient treated in a hospital which conducts ECT received the procedure. In the first set of models, the outcome was treatment in a hospital which conducted versus did not conduct ECT and the observations were all stays for severe recurrent major depression. In the second set of models, the outcome was receipt of ECT and the observations were the subsample of depression stays in hospitals where ECT was conducted (a 20% sample of 278,461, yielding an estimated of 1,392,082 stays.) Year was treated as a continuous variable. The approach is illustrated below using the first set of models.
We first fit a bivariate model with year as the independent variable. Next, we estimated a time trend adjusted for the effects of patient and hospital characteristics in a multivariate model including main effects and time interaction effects. Variable selection began by testing each patient characteristic variable in a bivariate model. Variables with coefficients differing from zero at p<.25 were included along with year in a preliminary multivariate model. Backwards stepwise variable removal was conducted until remaining variable coefficients differed from zero at p<.05. Hospital characteristics were then added in a similar backwards stepwise fashion. In order to test for moderators of time trends, interaction terms (year * covariate) were similarly added. Finally, to test whether a shift in treatment away from psychiatric units mediated observed time trends, we examined change in the estimated time effect when the variable for unit type was added to the model.
To estimate time trends, we obtained predicted probabilities of treatment in a hospital conducting ECT from the bivariate and multivariate models (13) and presented risk ratios (RRs) and adjusted risk ratios (ARRs), respectively, for 2009 versus 1993. These were calculated overall and for specific moderator levels. To examine stable differences between groups in the probability of treatment in a hospital conducting ECT, we similarly estimated RRs and ARRs.
Transfers to other short-term hospitals
To examine if declining probability of treatment in a hospital conducting ECT was mitigated by transfers to hospitals potentially conducting the procedure, we calculated for stays where ECT was not conducted the annual percentage transferred to another short-term facility.
Analytic software
Analyses were conducted using SUDAAN 10.1.
Ethical Considerations
Analyses of these publicly available, de-identified data were deemed not to constitute human subjects research by the Nathan Kline Institute Institutional Review Board Director.
RESULTS
Number of US Inpatient Stays involving ECT use
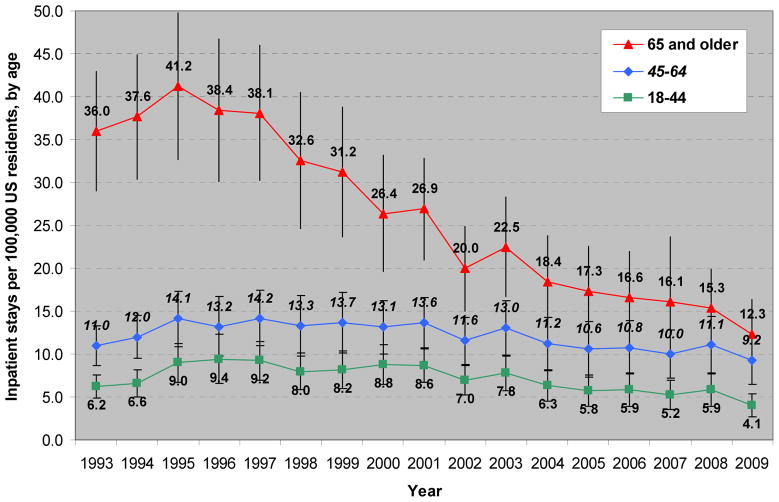
The number of inpatient stays involving ECT use rose from 12.6 per 100,000 residents (95% CI 10.2–14.9) in 1993 to 15.9 (12.5–19.3) in 1995, then fell gradually to 7.2 (5.2–9.3) in 2009. Declining stays with the procedure among the elderly accounted for the overall trend (Figure 1).
Figure 1.
Annual number of inpatient stays in US general hospitals involving ECT administration per 100,000 US residents, by age group, with 95% confidence intervals, 1993–2009
See text for sample description.
Among Americans aged 65 and older, stays involving ECT use fell from a peak of 41.2 (32.7–49.8) in 1995 to 12.3 (8.3–16.3) in 2009, while the number of stays for younger groups were lower but comparatively stable over the period. Declines occurred in each US region (Figure S1), but stays were generally more numerous in the Northeast and Midwest than in the South and West (12.6, 9.1, 5.9, and 2.7, respectively in 2009).
Proportion of US Hospitals Conducting ECT
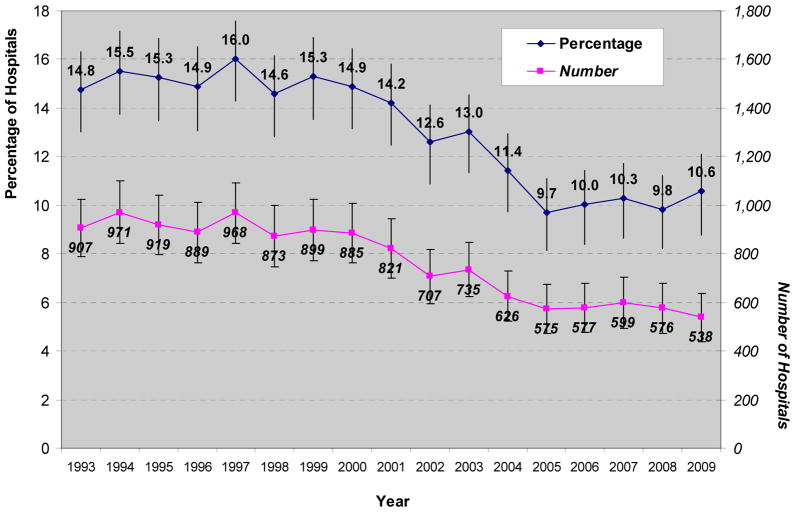
The annual percentage and number of US general hospitals which conducted ECT during any inpatient stay are presented in Figure 2.
Figure 2.
Annual percentage and number of US general hospitals which conducted ECT, with 95% confidence intervals, 1993–2009
See text for sample description.
The number fell from 907 (788–1,026) in 1993 to 538 (438–637) in 2009, while the percentage declined from 14.8% (13.2–16.5) in 1993 to 10.6% (9.0–12.4) in 2009, reflecting a concurrent reduction in the number of community hospitals operating in the US. The percentage declined in each region (Figure S2), with Northeastern hospitals retaining the highest percentage in each year, followed typically by Midwestern, Southern, and Western hospitals (17.0%, 12.3%, 8.2%, and 6.1%, respectively in 2009). Declines were concentrated within hospitals with psychiatric inpatient units; the percentage of these hospitals conducting ECT fell from 55.1% to 34.6% over the period (Figure S3).
Number of Stays Involving ECT per Hospital
Among hospitals which conducted ECT, the median number of annual stays involving ECT over the period was 21, while the 25th and 75th percentiles were 7 and 42 stays, respectively (Figure S4). Approximately 10% of these hospitals conducted ECT in a single patient over a calendar year. Time trends indicated that while the 95th percentile appear to rise substantially, from 82 stays in 1993 to 116 in 2009, lower percentiles appeared largely unchanged over the period (Figure S5).
Use of ECT for Severe Recurrent Major Depression
Descriptive trends in ECT use
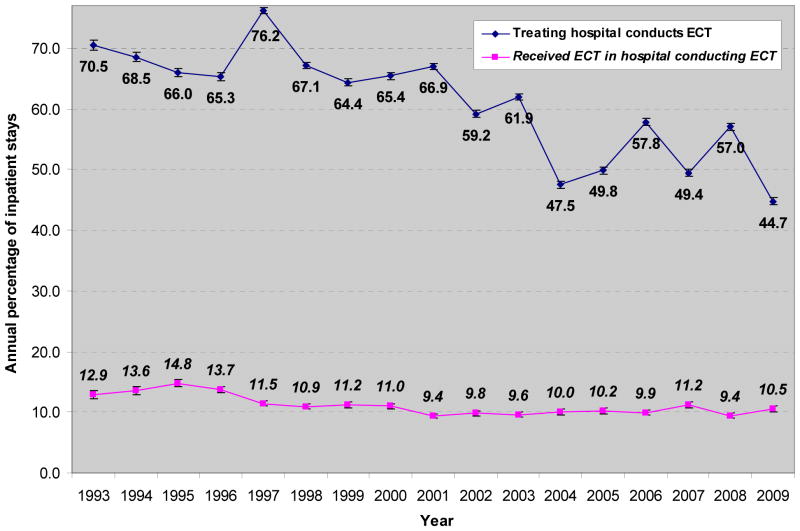
Annual percentages of depression stays in hospitals which conduct ECT and of depressed inpatients who received ECT during stays in hospitals which conduct the procedure are presented in Figure 3.
Figure 3.
The annual percentages of inpatients treated in hospitals which conduct ECT and of inpatients who received ECT where the procedure is conducted, with 95% confidence intervals, among stays for recurrent major depression in US general hospitals, 1993–2009
See text for sample description.
The percentage of stays in hospitals which conduct ECT fell from 70.5% (69.7–71.2) in 1993 to 44.7% (44.1–45.3) in 2009, while receipt of ECT in those facilities declined more modestly from 12.9% (12.3–13.5) to 10.5% (10.0–11.1).
Testing whether declining ECT use is caused by declining probability that treating hospitals conduct ECT
The unadjusted risk ratio (RR) of treatment in a hospital conducting ECT in 2009 versus 1993 was 0.67 (0.57–0.78) for all depression stays (Table 1).
Table 1.
Trends in the percentage of inpatients treated in a hospital which conducts ECT, and risk ratios (RRs) of treatment where ECT is conducted for 2009 vs 1993, among inpatient stays for severe recurrent major depression in US general hospitals (N=465,646), by signficant predictors of treatment in a hospital which conducts ECT
| Characteristic (% of stays in ‘93–’98, ‘99–’03, ‘04–’09) | % of stays in a hospital which conducts ECT
|
Probability that the treating hospital conducts ECT, ‘09 vs ‘93 (95% CI)
|
|||
|---|---|---|---|---|---|
| 93–’98 | ‘99–’03 | ‘04–’09 | Unadjusted RR | Adjusted RR | |
| All stays | 69.0 | 63.6 | 51.0 | 0.67 (0.57 –0.78) | 0.66 (0.55 – 0.77) |
| Patient Characteristics | |||||
| Age, in years | |||||
| 18–34 (26.0, 25.9, 24.9) | 63.3 | 60.7 | 48.3 | 0.71 (0.58 – 0.86) | 0.68 (0.55 – 0.83) |
| 35–44 (27.0, 27.6, 23.1) | 66.5 | 62.4 | 50.1 | 0.69 (0.58 – 0.82) | 0.68 (0.56 – 0.81) |
| 45–54 (15.9, 21.3, 25.1) | 67.6 | 63.6 | 50.6 | 0.67 (0.57 – 0.79) | 0.65 (0.54 – 0.78) |
| 55–64 (8.1, 8.9, 12.7) | 69.9 | 65.1 | 53.0 | 0.68 (0.59 – 0.79) | 0.66 (0.56 – 0.79) |
| 65–74 (10.5, 7.3, 7.0) | 77.0 | 68.3 | 54.1 | 0.62 (0.54 – 0.71) | 0.60 (0.51 – 0.70) |
| ≥75 (12.5, 9.1, 7.2) | 80.4 | 70.0 | 58.5 | 0.64 (0.55 – 0.75) | 0.60 (0.51 – 0.71) |
| Potential medical contraindication | |||||
| No (79.7, 79.1, 75.6) | 67.7 | 63.0 | 50.9 | 0.68 (0.58 – 0.80) | - |
| Yes (20.3, 20.9, 23.7) | 74.1 | 65.7 | 51.5 | 0.61 (0.53 – 0.71) | - |
| Admission source | |||||
| Routine (53.9, 45.1, 42.6) | 72.1 | 65.3 | 52.0 | 0.63 (0.50 – 0.79) | - |
| Emergency Dept (37.5, 44.7, 45.7) | 63.5 | 61.7 | 47.6 | 0.67 (0.53 – 0.84) | - |
| Other hospital (5.5, 6.3, 7.6) | 70.8 | 67.4 | 57.1 | 0.74 (0.57 – 0.95) | - |
| Long term facility (2.5, 2.9, 2.9) | 72.0 | 55.8 | 58.6 | 0.78 (0.57 – 1.07) | - |
| Court/law enforcement (0.7, 1.0, 1.3) | 56.3 | 44.9 | 53.9 | 0.97 (0.32 – 2.91) | - |
| Percentile of median household income in patient ZIP code | |||||
| 0–25th (33.0, 29.1, 31.2) | 62.7 | 53.6 | 43.4 | 0.62 (0.49 – 0.78) | - |
| 26th–50th (22.6, 28.4, 27.8) | 70.3 | 62.5 | 47.5 | 0.58 (0.48 – 0.69) | - |
| 51st–75th (19.0, 23.0, 22.3) | 73.6 | 68.3 | 56.8 | 0.70 (0.59 – 0.84) | - |
| 76th–100th (25.4, 19.5, 18.7) | 73.3 | 74.5 | 63.2 | 0.83 (0.69 – 1.00) | - |
| Primary Payer | |||||
| Private Insurer (30.1, 35.0, 34.1) | 72.4 | 70.4 | 57.4 | 0.73 (0.63 – 0.85) | - |
| Medicare (36.2, 30.6, 29.4) | 74.6 | 65.9 | 52.8 | 0.62 (0.54 – 0.72) | - |
| Medicaid (23.5, 23.2, 22.8) | 61.6 | 55.6 | 43.3 | 0.63 (0.50 – 0.80) | - |
| Self pay (6.2, 7.2, 8.0) | 53.7 | 51.5 | 42.3 | 0.69 (0.53 – 0.91) | - |
| Hospital Characteristics | |||||
| Teaching Status | |||||
| Non-teaching (53.6, 55.3, 56.3) | 48.6 | 50.2 | 37.8 | 0.59 (0.45 – 0.77) | - |
| Teaching (46.5, 44.7, 43.7) | 77.7 | 80.0 | 68.0 | 0.74 (0.62 – 0.87) | - |
| Hospital Bed Size | |||||
| Small (9.4, 8.9, 9.3) | 53.4 | 50.9 | 30.5 | 0.50 (0.25 – 0.98) | - |
| Medium (29.3, 25.5, 23.7) | 67.7 | 55.6 | 41.6 | 0.52 (0.37 – 0.73) | - |
| Large (61.3, 65.7, 67.0) | 72.5 | 68.3 | 57.2 | 0.72 (0.60 – 0.86) | - |
CI denotes confidence interval. ARR varied only by age group; - indicates ARR did not differ from overall ARR of 0.66. Results based on HCUP-NIS weighted sampling of 465,646 inpatients aged ≥18 discharged with a principal ICD-9-CM diagnosis 296.33–34. Hospitals conducting ECT were defined as those in which at least one inpatient received ECT during the calendar year. See text for sample description, variable definitions and modelling procedures.
In stratified bivariate analyses, RRs ranged from 0.50 for stays in small hospitals to 0.97 in the small proportion of patients admitted from a court or law enforcement authority. Notable changes in stay characteristics included a growing proportion of stays by patients who were non-elderly, from less wealthy neighborhoods, admitted through the emergency department or by hospital transfer, and treated in larger hospitals. After multivariate adjustment, the adjusted risk ratio (ARR) of treatment in a hospital conducting ECT in 2009 versus 1993 was 0.66 (0.55–0.77). Among all individual and hospital characteristics, only age significantly moderated the downward trend. ARRs ranged from 0.68 for 18–44 year olds to 0.60 for those aged 65 or older. Patient and hospital characteristics not significantly associated with probability of treatment in hospitals which conduct ECT, either as main or interaction effects in multivariate modeling, were: sex, race/ethnicity, the presence of psychotic features, record of deliberate self-harm, psychiatric co-morbidities, general medical co-morbidities, hospital census region and urbanicity.
Testing whether declining ECT use is caused by declining probability of receiving ECT for inpatients in hospitals which conduct ECT
The unadjusted RR of receiving ECT for 2009 vs. 1993 was 0.69 (0.56–0.85). A time trend was no longer observed (ARR 1.00) after adjusting for changes in the visit characteristics significantly associated with ECT use.
Testing whether the declining probability that treating hospitals conduct ECT is caused by declining presence of a psychiatric inpatient unit
Inclusion of inpatient unit type in modeling probability of treatment in a hospital which conducts ECT did not meaningfully alter adjusted trend estimates (ARR 0.65, 0.55–0.78).
Testing whether transfers from hospitals where ECT was not conducted increased during the period
The annual proportion of stays in hospitals where ECT was not conducted resulting in transfer was stable and low, ranging from 2.0–3.0%.
Testing for stable patterns in the probability that the treating hospital conducts ECT
Characteristics significantly and stably associated with conduct of ECT included older age, greater household income in the patient’s residential ZIP, private insurance coverage, routine admission or hospital transfer rather than emergency department, and record of a potential medical contraindication, and treatment in larger, teaching facilities (Table 2).
Table 2.
Risk ratios (RRs) of treatment in hospital which conducts ECT, compared to reference levels, among inpatient stays for severe recurrent major depression in US general hospitals in 1993–2009 (N=465,646), by characteristics significantly associated with treatment where ECT is conducted
| Characteristic | Probability that the treating hospital conducts ECT vs reference level (95% CI)
|
|
|---|---|---|
| Unadjusted RR | Adjusted RR | |
| Patient Characteristics | ||
| Age, in years | ||
| 18–34 (Reference) | 1.00 | 1.00 |
| 35–44 | 1.03 (1.01 – 1.05) | 1.03 (1.01 – 1.04) |
| 45–54 | 1.03 (1.01 – 1.05) | 0.99 (0.97 – 1.01) |
| 55–64 | 1.06 (1.03 – 1.10) | 1.01 (0.98 – 1.04) |
| 65–74 | 1.18 (1.12 – 1.24) | 1.09 (1.05 – 1.14) |
| 75 and older | 1.24 (1.17 – 1.32) | 1.14 (1.08 1.20) |
| Potential medical contraindication | ||
| No (Reference) | 1.00 | 1.00 |
| Yes | 1.03 (1.01 – 1.06) | 1.01 (0.99 – 1.04) |
| Admission source | ||
| Routine (Reference) | 1.00 | 1.00 |
| Emergency Department | 0.90 (0.84 – 0.95) | 0.90 (0.85 – 0.96) |
| Other hospital | 1.01 (0.94 – 1.08) | 0.97 (0.91 – 1.04) |
| Long term facility | 0.96 (0.86 – 1.07) | 0.92 (0.84 – 1.01) |
| Court/law enforcement | 0.80 (0.58 – 1.11) | 0.93 (0.74 – 1.18) |
| Percentile of median household income in patient ZIP code | ||
| 0–25th (Reference) | 1.00 | 1.00 |
| 26th–50th | 1.11 (1.05 – 1.18) | 1.12 (1.07 – 1.19) |
| 51st–75th | 1.24 (1.16 – 1.33) | 1.19 (1.12 – 1.27) |
| 76th–100th | 1.34 (1.23 – 1.45) | 1.27 (1.18 – 1.38) |
| Primary Payer | ||
| Private Insurer (Reference) | 1.00 | 1.00 |
| Medicare | 0.98 (0.94 – 1.01) | 0.96 (0.94 –0.99) |
| Medicaid | 0.80 (0.75 – 0.86) | 0.86 (0.81 – 0.91) |
| Self pay | 0.73 (0.68 – 0.79) | 0.80 (0.75 – 0.85) |
| Hospital Characteristics | ||
| Teaching Status | ||
| Non-teaching (Reference) | 1.00 | 1.00 |
| Teaching | 1.64 (1.48 – 1.82) | 1.67 (1.51 – 1.85) |
| Hospital Bed Size | ||
| Small (Reference) | 1.00 | 1.00 |
| Medium | 1.25 (1.00 – 1.56) | 1.39 (1.09 – 1.79) |
| Large | 1.49 (1.21 – 1.82) | 1.73 (1.38 – 2.18) |
CI denotes confidence interval. Reference denotes reference level for risk ratio comparisons. Results based on HCUP-NIS weighted sampling of 465,646 inpatients aged ≥18 discharged with a principal ICD-9-CM diagnosis 296.33–4. Hospitals conducting ECT were defined as those in which at least one inpatient received ECT during the calendar year. See text for sample description, variable definitions and modelling procedures.
DISCUSSION
Between 1993 and 2009, the probability that a severely depressed inpatient’s treating hospital conducts ECT fell by one third. Declines were concentrated in the elderly, a group traditionally thought to benefit most from ECT (1) and for whom commonly used antidepressant pharmacotherapies may be only modestly effective (14), and were not ameliorated by the presence of clinical indications like psychotic features. By contrast, receipt of ECT was unchanged for patients treated within hospitals which conduct the procedure. Throughout the period, depressed inpatients from poor neighborhoods, and those who were publicly- or uninsured, remained less likely to be treated in facilities which conduct ECT. Declining conduct of ECT by hospitals treating severely depressed inpatients occurred against a scientific background of evidence for ECT’s superior efficacy in the treatment of depression (2), including a distinctive role in severe illness (10, 15).
Why are fewer hospitals conducting ECT? Our analyses cannot definitively identify the cause, but our findings do weaken some plausible explanations and strengthen others. Older data (7) and anecdote suggest use of outpatient settings to conduct ECT is growing, a phenomenon which could explain our finding that the number of inpatient visits per capita involving ECT has fallen. Nonetheless, the patterns of markedly declining conduct of ECT in US hospitals that we observed argue against the inference that inpatient administration has simply been replaced by outpatient care. Outpatients commonly use the same hospital ECT suites as inpatients, since professional and payer guidelines require anesthesia and nursing care prior to and following ECT administration as well as dedicated treatment and recovery facilities (16–18). Cessation of inpatient ECT at a hospital is therefore likely to eliminate conduct of the procedure for outpatients as well. Further, provider guidelines regarding outpatient ECT recommend at least a brief inpatient stay for treatment-naïve patients (17) and advise against outpatient initiation in patients at high risk for self harm or falls, suffering from catatonia of potentially complicating medical illnesses, or lacking the ability to care for themselves or a reliable caregiver (16, 17). Guidelines from the largest US private insurer additionally specify that outpatient ECT initiation is authorized only when patients show low to no risk for suicide, are not psychotic, and are not cognitively impaired (19). The proportion of psychiatric inpatients with acute safety risks may have risen as inpatient utilization declined over the past two decades (20, 21), and one third of our severely depressed sample was diagnosed with psychotic features, suggesting that falling conduct of inpatient ECT by hospitals caring for these patients could signal growing limitations on the safe initiation of ECT in people with severe depressive illness.
We found no increase in transfers from hospitals which do not conduct ECT, suggesting transfers to facilities which do conduct the procedure are not mitigating the trends we observed. Comprehensive Veteran’s Administration data indicates that ECT initiation is highly sensitive to geographic proximity of facilities offering the procedure and suggests the widespread elimination of hospital-based ECT we observed has likely reduced use of the procedure rather than shifting it to more distant inpatient or outpatient programs (22). Because our sample excluded freestanding psychiatric hospitals, we could not test whether ECT use in patients directly admitted to these facilities rose and offset the reductions we observed. Limited data suggest that while psychiatric facilities are an important source of ECT, treatment in these settings is unlikely to have offset declines of the magnitude we found. Psychiatric hospitals provided a large but declining proportion of inpatient mental health care over the period, accounting for 35.7% of stays in 1992 and 31.9% in 2004, while the proportion treated in general hospital psychiatric units rose from 47.2% to 56.5% (23). Further, data from a 2008 US Substance Abuse and Mental Health Services Administration survey of mental health programs indicate that 150 psychiatric hospitals (18.5% of the national total of 661 hospitals) offered ECT, compared with 501 general hospitals with psychiatric units (28.7% of a total of 811 hospitals) (24). The most recent published data on volume of ECT administration in specialty hospitals (25)—which suggest that use of the procedure is relatively rare in these facilities—date from 1980 and cannot inform interpretation of our findings.
The declines in conduct of ECT we observed were concentrated within hospitals with discharge patterns indicating the presence of active psychiatric units. While prior data support the concern that general hospitals are gradually closing specialty psychiatric units (11), this trend did not explain declining conduct of ECT by these facilities. Despite unit closures, general hospital mental health care has remained overwhelmingly concentrated in facilities with specialty units (11), including 99% of all stays for mood disorders in 2003 (26).
Adjustment for patient and hospital characteristics did not weaken our trend estimates, indicating that a putative decline in the prevalence of the observed clinical indications for ECT or rise in prevalence of contraindications could not meaningfully explain falling probability that treating hospitals conduct ECT. And declines did not vary by observed patient clinical characteristics, such as the presence of psychotic features or of co-morbid medical conditions that might increase the risk of ECT, suggesting that declining hospital conduct of ECT lead to a clinically indiscriminate reduction in use of the treatment. Information on concurrent and prior medication treatments were not available in our data, and therefore we could not evaluate how changing pharmacological practices in the treatment of depression may have influenced the trends we observed. However, international data and age-related US trends in the use of antidepressants suggest rising antidepressant use is an unlikely cause of the marked decline of ECT use in the elderly. Data on the treatment of depression in older Canadians from 1992 to 2004 indicate that while prevalence of antidepressant use rose 90% over the period, use of ECT remained stable (27). In the US use of antidepressants rose for all age groups between 1996 and 2005, but increases were more modest among the elderly than for other groups (28). Further, while treated non-elderly adults received a growing number of prescriptions, suggesting rising antidepressant adherence or polypharmacy, these trends did not extend to the elderly (28). We could not assess whether vagus nerve stimulation or transcranial magnetic stimulation—two somatic therapies for depression—might have delayed or replaced ECT in some patients following FDA approval in 2006 and 2008, respectively.
We could not explore whether changes in provider training and attitudes towards ECT (3)—or in public or patient perception of the treatment—contributed to the observed trends. In one study of depressed inpatients, those viewing ECT favorably were more likely to receive it, indicating that patient preference influences ECT use (29). Limited data indicate that those who receive ECT develop more positive impressions of the procedure (29, 30) and that providers who are taught about ECT similarly become more supportive of its use (31), suggesting that declining use of ECT may contribute to a cycle of unfamiliarity and more negative attitudes. Nonetheless, if declining patient or provider interest were the principal cause of changes in utilization of ECT, we would expect declines in use of ECT where it was available, rather than the stable use we observed.
We found that publicly-insured depressed inpatients were less likely to be treated in hospitals which conduct ECT than their privately-insured counterparts, even after adjusting for other patient and hospital characteristics. Strong pressure from payers to contain the cost of inpatient psychiatric units over the last two decades, and large declines in inpatient length of stay for mental disorders (20, 21), may have contributed to the patterns we observed. While national comparisons among Medicare, Medicaid, and private insurer reimbursement of inpatient ECT are not available, our experience is that private insurer reimbursement of inpatient days and ECT procedure fees substantially exceeds that of public insurers. This pattern of differential reimbursement may impose uncompensated costs on hospitals treating publicly insured inpatients with ECT. Financial pressures may have been particularly pronounced in hospitals treating larger populations of publicly and uninsured patients. Similar processes may constrain ECT availability for patients residing in lower income areas. While primary payer type was identified in our data, we could not identify the presence of managed care, which grew increasingly prevalent in Medicaid programs over the period studied (32), or identify any changes in reimbursement agreements made by private and Medicaid plans and individual hospitals over the period. In 2005 Medicare began a three-year transition from payment based on facility costs to a prospective system for psychiatric inpatient care (33). The new system reimburses each ECT procedure in addition to a daily rate adjusted for patient and hospital factors. Future research should seek to clarify the effect of these changes on hospital incentives to conduct ECT.
We did not find geographic variation in ECT availability, but our geographic measures were limited to four regions and urban or non-urban location. Patients treated in academic facilities and larger hospitals were far more likely than others to have access to ECT in their treating facility, and geographic variation in these hospital characteristics have been found in prior studies of national patterns of ECT use (3). We could not directly evaluate some other important potential causes of geographic variation, such as provider density or restrictiveness of state ECT regulations (3, 4). State variation in regulation of ECT use is considerable, and provider survey data suggest introduction of new restrictions may impede availability of the treatment for candidate patients. A survey of Texas psychiatrists following introduction of restrictions and public reporting requirements for ECT providers found that almost 90% believed restrictions interfered with the care of patients, and concern was most common among those with the greatest experience providing ECT (34).
Our study has additional limitations. First, because the analyses were conducted with cross-sectional data, temporal changes in the conduct of ECT within specific hospitals could not be evaluated. Second, unmeasured changes in sample composition could theoretically have biased trend findings. However, bias arising from random changes in national hospital sampling over the 17-year period is more likely to contribute to a type II error of failing to identify true trends and is unlikely to generate the large and sustained trends we observed.
Our data cannot not inform questions about the benefits or harms of ECT for severe depressive illness, but our findings do address speculation about community patterns of ECT use which have surrounded recent FDA regulatory deliberations. Since implementing the current device regulatory scheme in 1976, the FDA has considered ECT devices as high risk (Class III). While new Class III devices require pre-market approval, marketing of ECT and other “pre-amendment” devices first sold before 1976 has been allowed through an alternate regulatory pathway (35). In 2009, the Government Accounting Office recommended ending differential regulation of pre-amendment devices and reevaluating their classification. After reviewing ECT safety and efficacy (35), a panel recommended in January, 2011, that the FDA retain Class III status for ECT, although psychiatrists on the panel unanimously supported reclassification as intermediate risk (Class II). If the FDA follows the panel recommendation, device manufacturers will have 30 months to apply for pre-market approval using safety and efficacy data from prior or new trials. Denial of the application would end marketing of ECT devices in the US. Our findings provide empirical support for concerns that many severely depressed inpatients, especially those with few resources and those treated outside of large academic medical centers, receive care in settings where ECT is not conducted. As the FDA considers imposing new regulations on the availability of ECT devices, we hope a public health perspective informed by ECT use in the community weighs in their policy deliberations.
Supplementary Material
Acknowledgments
Supported in part by K12 DA000357-11 (trainee Dr. Case) and the Leon Levy Foundation (Dr. Case). The views and information presented do not necessarily state or reflect those of supporting organizations. We gratefully acknowledge the editorial comments of Christopher F. Koller and the clinical guidance of Patrick Ying.
Footnotes
FINANCIAL DISCLOSURES
Dr. Case has received support from the American Academy of Child and Adolescent Psychiatry Eli Lilly Pilot Research Award and the American Psychiatric Association AstraZeneca Young Minds in Psychiatry Award. In the past three years, Dr. Price has served as an investigator on research supported Medtronic, Neuronetics, Cyberonics, and NeoSync, none of which involved electroconvulsive therapy. Only the research supported by NeoSync was active during the time of his involvement with this project, and he has received no direct support or compensation for any of this work. Dr. Price has served on the advisory panels of Abbott and AstraZeneca, and has consulted for Abbott and AstraZeneca. Dr. Olfson has received a research grant to Columbia University from Eli Lilly & Company. Dr. Marcus has received grant support from Ortho-McNeil Janssen and Forest Research Institute and has served as a consultant to AstraZeneca. All other authors report no biomedical financial interests or potential conflicts of interest.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.American Psychiatric Association. The Practice of Electroconvulsive Therapy: Recommendations for Treatment, Training, and Privileging. 2. Washington, D.C: American Psychiatric Publishing, Inc; 2001. [Google Scholar]
- 2.Pagnin D, de Queiroz V, Pini S, Cassano GB. Efficacy of ECT in depression: a meta-analytic review. J Ect. 2004;20(1):13–20. doi: 10.1097/00124509-200403000-00004. [DOI] [PubMed] [Google Scholar]
- 3.Hermann RC, Dorwart RA, Hoover CW, Brody J. Variation in ECT use in the United States. Am J Psychiatry. 1995;152(6):869–75. doi: 10.1176/ajp.152.6.869. [DOI] [PubMed] [Google Scholar]
- 4.Harris V. Electroconvulsive therapy: administrative codes, legislation, and professional recommendations. J Am Acad Psychiatry Law. 2006;34(3):406–11. [PubMed] [Google Scholar]
- 5.Hermann RC, Ettner SL, Dorwart RA, Hoover CW, Yeung E. Characteristics of psychiatrists who perform ECT. Am J Psychiatry. 1998;155(7):889–94. doi: 10.1176/ajp.155.7.889. [DOI] [PubMed] [Google Scholar]
- 6.Kellner CH. The FDA Advisory Panel on the Reclassification of ECT Devices: Unjustified Ambivalence. Psychiatric Times. 2011 [Google Scholar]
- 7.Rosenbach ML, Hermann RC, Dorwart RA. Use of electroconvulsive therapy in the Medicare population between 1987 and 1992. Psychiatr Serv. 1997;48(12):1537–42. doi: 10.1176/ps.48.12.1537. [DOI] [PubMed] [Google Scholar]
- 8.Design of the HCUP Nationwide Inpatient Sample, 2000. Rockville, Maryland: Agency for Healthcare Research and Quality, 2002; May, 2002. Report No. [Google Scholar]
- 9.Whalen D, Houchens R, Elixhauser R. 2005 HCUP Nationwide Inpatient Sample (NIS) Comparison Report, HCUP Methods Series Report # 2008-01. U.S. Agency for Healthcare Research and Quality; 2008. [Google Scholar]
- 10.Practice guideline for the treatment of patients with major depressive disorder (revision) American Psychiatric Association. Am J Psychiatry. 2000;157(4 Suppl):1–45. [PubMed] [Google Scholar]
- 11.Mark TL, Stranges E, Levit KR. Using Healthcare Cost and Utilization Project State Inpatient Database and Medicare Cost Reports Data to Determine the Number of Psychiatric Discharges from Psychiatric Units of Community Hospitals. Agency for Healthcare Research and Quality (AHRQ); 2010. [Google Scholar]
- 12.US Centers for Disease Control and Prevention. Bridged-Race Population Estimates. Vintage: 2009. [Google Scholar]
- 13.Bieler GS, Brown GG, Williams RL, Brogan DJ. Estimating model-adjusted risks, risk differences, and risk ratios from complex survey data. Am J Epidemiol. 2010;171(5):618–23. doi: 10.1093/aje/kwp440. [DOI] [PubMed] [Google Scholar]
- 14.Nelson JC, Delucchi K, Schneider LS. Efficacy of second generation antidepressants in late-life depression: a meta-analysis of the evidence. Am J Geriatr Psychiatry. 2008;16(7):558–67. doi: 10.1097/JGP.0b013e3181693288. [DOI] [PubMed] [Google Scholar]
- 15.Fochtmann lJ, Gelenberg AJ. Guideline Watch: Practice Guideline for the Treatment of Patients With Major Depressive Disorder. 2. Arlington, VA: American Psychiatric Association; 2005. [Google Scholar]
- 16.Fink M, Abrams R, Bailine S, Jaffe R. Ambulatory electroconvulsive therapy: report of a task force of the association for convulsive therapy. Association for Convulsive Therapy. Convuls Ther. 1996;12(1):42–55. [PubMed] [Google Scholar]
- 17.Reti IM, Walker M, Pulia K, Gallegos J, Jayaram G, Vaidya P. Safety considerations for outpatient electroconvulsive therapy. J Psychiatr Pract. 2012;18(2):130–6. doi: 10.1097/01.pra.0000413280.95843.d3. [DOI] [PubMed] [Google Scholar]
- 18.Aetna. Clinical Policy Bulletin: Electroconvulsive Therapy. 2011 [updated 07/29/2011]; Available from: www.aetna.com/cpb/medical/data/400_499/0445.html.
- 19.United Behavioral Health. COVERAGE DETERMINATION GUIDELINE: Electroconvulsive Therapy (ECT) 2010 [updated 09/2010]; Available from: www.ubhonline.com/html/pdf/coverageDetermGuidelines/ECT.pdf.
- 20.Blader JC. Acute inpatient care for psychiatric disorders in the United States, 1996 through 2007. Arch Gen Psychiatry. 2011;68(12):1276–83. doi: 10.1001/archgenpsychiatry.2011.84. [DOI] [PubMed] [Google Scholar]
- 21.Case BG, Olfson M, Marcus SC, Siegel C. Trends in the inpatient mental health treatment of children and adolescents in US community hospitals between 1990 and 2000. Arch Gen Psychiatry. 2007;64(1):89–96. doi: 10.1001/archpsyc.64.1.89. [DOI] [PubMed] [Google Scholar]
- 22.Pfeiffer PN, Valenstein M, Hoggatt KJ, Ganoczy D, Maixner D, Miller EM, et al. Electroconvulsive therapy for major depression within the Veterans Health Administration. J Affect Disord. 2011;130(1–2):21–5. doi: 10.1016/j.jad.2010.09.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Substance Abuse and Mental Health Services Administration. Mental Health, United States, 2008. Rockville, MD: Center for Mental Health Services, Substance Abuse and Mental Health Services Administration; 2010. HHS Publication No. (SMA) 10–4590. [Google Scholar]
- 24.Substance Abuse and Mental Health Services Administration. National Survey of Mental Health Treatment Facilities. Rockville, MD: 2008. [Google Scholar]
- 25.Thompson JW, Blaine JD. Use of ECT in the United States in 1975 and 1980. Am J Psychiatry. 1987;144(5):557–62. doi: 10.1176/ajp.144.5.557. [DOI] [PubMed] [Google Scholar]
- 26.Mark TL, Vandivort-Warren R, Owens PL, Buck JA, Levit KR, Coffey RM, et al. Psychiatric discharges in community hospitals with and without psychiatric units: how many and for whom? Psychiatric services. 2010;61(6):562–8. doi: 10.1176/ps.2010.61.6.562. [DOI] [PubMed] [Google Scholar]
- 27.Rapoport MJ, Mamdani M, Herrmann N. Electroconvulsive therapy in older adults: 13-year trends. Can J Psychiatry. 2006;51(9):616–9. doi: 10.1177/070674370605100910. [DOI] [PubMed] [Google Scholar]
- 28.Olfson M, Marcus SC. National patterns in antidepressant medication treatment. Arch Gen Psychiatry. 2009;66(8):848–56. doi: 10.1001/archgenpsychiatry.2009.81. [DOI] [PubMed] [Google Scholar]
- 29.Pettinati HM, Tamburello TA, Ruetsch CR, Kaplan FN. Patient attitudes toward electroconvulsive therapy. Psychopharmacol Bull. 1994;30(3):471–5. [PubMed] [Google Scholar]
- 30.Kalayam B, Steinhart MJ. A survey of attitudes on the use of electroconvulsive therapy. Hosp Community Psychiatry. 1981;32(3):185–8. doi: 10.1176/ps.32.3.185. [DOI] [PubMed] [Google Scholar]
- 31.Gazdag G, Sebestyen G, Ungvari GS, Tolna J. Impact on psychiatric interns of watching live electroconvulsive treatment. Acad Psychiatry. 2009;33(2):152–6. doi: 10.1176/appi.ap.33.2.152. [DOI] [PubMed] [Google Scholar]
- 32.Data and System Group. 2010 Medicaid Managed Care Enrollment Report. Baltimore, MD: Centers for Medicare & Medicaid Services; 2011. [Google Scholar]
- 33.Office of the Federal Register. Medicare Program: Inpatient Psychiatric Facilities Prospective Payment System-Update for Rate Year Beginning. 2011 Jul 1;2011 (RY 2012) [PubMed] [Google Scholar]
- 34.Finch JM, Sobin PB, Carmody TJ, DeWitt AP, Shiwach RS. A survey of psychiatrists’ attitudes toward electroconvulsive therapy. Psychiatric services. 1999;50(2):264–5. doi: 10.1176/ps.50.2.264. [DOI] [PubMed] [Google Scholar]
- 35.US Food and Drug Administration. FDA Executive Summary Prepared for the January 27–28, 2011 meeting of the Neurological Devices Panel. 2011 [cited 2011 12/20/11]; Available from: http://www.fda.gov/downloads/AdvisoryCommittees/CommitteesMeetingMaterials/MedicalDevices/MedicalDevicesAdvisoryCommittee/NeurologicalDevicesPanel/UCM240933.pdf.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.