Abstract
Background
Surgery remains the mainstay of gastric cancer treatment. It is, however, associated with a relatively high risk of perioperative complications. The use of laparoscopy and the Enhanced Recovery After Surgery (ERAS) protocol allows clinicians to limit surgically induced trauma, thus improving recovery and reducing the number of complications. The aim of the study is to present clinical outcomes of patients with gastric cancer undergoing laparoscopic gastrectomy combined with the ERAS protocol.
Material/Methods
Fifty-three (21 female/32 male) patients who underwent elective laparoscopic total gastrectomy due to cancer were prospectively analyzed. Demographic and surgical parameters were assessed, as well as the compliance with ERAS protocol elements, length of hospital stay, number of complications, and readmissions.
Results
Mean operative time was 296.4±98.9 min, and mean blood loss was 293.3±213.8 mL. In 3 (5.7%) cases, conversion was required. Median length of hospital stay was 5 days. Compliance with ERAS protocol was 79.6±14.5%. Thirty (56.6%) patients tolerated an early oral diet well within 24 h postoperatively; in 48 (90.6%) patients, mobilization in the first 24 hours was successful. In 17 (32.1%) patients, postoperative complications occurred, with 7 of them (13.2%) being serious (Clavien-Dindo 3-5). The 30-day readmission rate was 9.4%.
Conclusions
The combination of laparoscopy and the ERAS protocol in patients with gastric cancer is feasible and allows achieving good clinical outcomes.
MeSH Keywords: Gastrectomy; Laparoscopy; Surgical Procedures, Minimally Invasive
Background
Although surgical resection remains the mainstay of gastric cancer treatment, it is associated with a high risk of complications reaching up to 46%, despite recent advancements in surgical technique and perioperative care [1,2]. Moreover, due to poor general status of patients with gastric neoplasms (up to 40% of them are malnourished, almost all of them have at least one serious comorbidity, many undergo neoadjuvant chemotherapy), perioperative mortality can be as high as 13% [3,4]. Not surprisingly, modern upper gastrointestinal surgical oncology puts an emphasis on surgical stress reduction, which is believed to improve clinical outcomes in patients with gastric cancer, especially in those with limited health capacity [5].
Perioperative care programs based on Enhanced Recovery After Surgery (ERAS) protocols have been shown to significantly attenuate postoperative stress response and positively influence short-term outcomes. Over the last 20 years, they have been extensively studied in colorectal surgery [6]. Thanks to their wide acceptance, ERAS is becoming the gold standard for the treatment of patients with large bowel pathology. Moreover, the combination of ERAS with minimally invasive surgery has been shown to further improve clinical outcomes [7,8]. The situation in gastric surgery is less studied. Laparoscopic surgery, despite having been proven to be feasible and safe, has not been widely adopted in most hospitals [9–13]. Additionally, even though the ERAS Society published consensus guidelines for perioperative care after gastrectomy in 2014, there are still a lot of controversies, misplaced conceptions, or even myths that are deeply embedded in everyday surgical practice. Although we are witnessing the enormous spread of so-called evidence-based surgical practice and most surgeons admit to compliance with current guidelines, it seems that the implementation of new patterns may be difficult or even impossible.
The aim of the study is to present short-term outcomes in patients with gastric cancer undergoing laparoscopic gastrectomy combined with the ERAS protocol.
Material and Methods
The prospective study included consecutive patients with histologically confirmed gastric cancer undergoing elective laparoscopic total gastrectomy (performed by the same leading laparoscopic surgeon with expertise in laparoscopic gastric, colorectal, pancreatic, and hepatic surgery) from 2013 to 2015. We are a tertiary referral university hospital; our annual volume of gastric cancer patients is estimated at 50 cases. Since January 2013, the laparoscopic approach has been the preferred access. Patients undergoing multivisceral resection or bypass gastrojejunal anastomosis (due to inoperable, obstructing tumors) were excluded from the study. Preoperative staging included abdominal and chest CT as well as endoscopic ultrasound. All patients were preoperatively assessed by an oncologist, and neoadjuvant chemotherapy was introduced in selected cases according to the MAGIC trial [14].
In all patients the perioperative ERAS protocol according to ERAS Society guidelines was implemented (Table 1) [15]. The modern perioperative care was introduced in 2012 for colorectal surgery. It was later extended to other disciplines of surgery and is now routine perioperative care in our department. This means that all patients (including colorectal, bariatric, pancreatic, hepatobiliary, and gastric) are treated with ERAS care irrespective of general health condition and stage of the disease.
Table 1.
ERAS protocol used in our department.
| 1. Preoperative counselling and patient’s education |
| 2. Pre-operative carbohydrate loading (400 ml of Nutricia preOp® 2 hours prior surgery) |
| 3. Antithrombotic prophylaxis (Clexane® 40 mg sc. starting in the evening prior surgery) |
| 4. Antibiotic prophylaxis (preoperative Ceftriaxone 2 g iv 30–60 min. prior surgery) |
| 5. Laparoscopic surgery |
| 6. Balanced intravenous fluid therapy (<2500 ml intravenous fluids during the day of surgery, less than 150 mmol sodium) |
| 7. No nasogastric tubes postoperatively |
| 8. No drains left routinely |
| 9. TAP block and standard anesthesia protocol |
| 10. Avoiding opioids, multimodal analgesia (oral when possible – Paracetamol 4×1 g, Ibuprofen 2×200 mg, Metamizole 2×500 mg, or Ketoprofen 2×100 mg) |
| 11. Postoperative oxygenation therapy (4–6 l/min.) |
| 12. Early oral feeding (oral nutritional supplement 4 h postoperatively – Nutrcia Nutridrink® or Nestlé Impact®, light hospital diet and oral nutritional supplements on the first postoperative day, full hospital diet in the second postoperative day) |
| 13. Urinary catheter removal on the first postoperative day |
| 14. Full mobilisation on the first postoperative day (getting out of bed, going to toilette, walking along the corridor, at least 4 hours out of bed) |
Primary endpoints were the length of hospital stay (LOS), the complication rate (graded according to the Clavien-Dindo classification), and the 30-day post-discharge readmission rate. Secondly, we calculated compliance with the ERAS protocol. Compliance was calculated as the number of preoperative and intraoperative ERAS interventions fulfilled out of 13 (the number of protocol elements included), similarly to Gustafsson et al. [16]. Thirdly, postoperative recovery parameters were measured, taking into consideration the following items: early mobilization, oral diet tolerance, and the need for opioids within the first 24 h postoperatively. Early mobilization was defined as sitting up in bed without help and a short walk to the toilet on the day of surgery, extending to at least 6 hours spent out of bed on the next postoperative days. Early oral diet intake included drinking fluids and liquid oral nutritional supplements on the day of surgery, gradually extending the diet on the next postoperative days (all patients were actively encouraged by the medical staff), and the need for opioid analgesics in the first 24 hours after surgery. We use neither parenteral nutrition nor a feeding jejunal tube in the postoperative period. Patients are allowed to drink on the day of surgery. If the tolerance of oral fluids is sufficient, iv fluids are ceased. Discharge criteria are well defined in our department and included in the protocol. They comprise full mobilization, no need for iv fluids, full tolerance of oral diet, good pain tolerance with oral nonopioid analgesia, no fever, no other complications, and support from the relatives or social help within the first postoperative days at home. Patients are discharged home when they fulfill the discharge criteria. We do not cooperate with any facility in the postoperative period. However, in the first and third days postdischarge, an ERAS nurse calls every patient and checks his general status in search of alarming symptoms. If any concern is raised that the patient is developing complications, he is immediately advised to come back for a check-up.
The study was approved by the local Ethics Review Committee and was performed in accordance with the ethical standards laid down in the 1964 Declaration of Helsinki and its later amendments. Informed consent was obtained from all patients before surgery.
Out of sixty patients with gastric cancer, four with inoperable tumors who had gastrojejunal bypass anastomosis were excluded. In three cases multivisceral resection was performed. The entire study group consisted of 53 patients (Figure 1).
Figure 1.
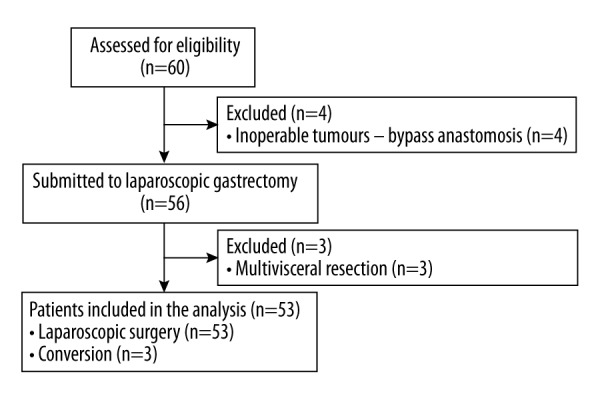
Patients flow through the study.
The studied group included 53 patients who underwent laparoscopic total gastrectomy with lymphadenectomy D2. Thirty-two (60.4%) of them had neoadjuvant chemotherapy. Demographic parameters of the studied group are shown in Table 2.
Table 2.
Demographic parameters of studied group.
| Parameter | Value |
|---|---|
| Number of patients, n | 53 |
| Females, n (%) | 21 (39.6%) |
| Males, n (%) | 32 (60.4%) |
| Mean age, years ±SD | 63.2±10.2 |
| BMI, kg/m2 ±SD | 25.1±4.5 |
| ASA 1, n (%) | 1 (1.9%) |
| ASA 2, n (%) | 36 (67.9%) |
| ASA 3, n (%) | 16 (30.2%) |
| Neoadjuvant chemotherapy, n (%) | 32 (60.4%) |
| AJCC Stage 0, n (%) | 1 (1.9%) |
| AJCC Stage Ia, n (%) | 5 (9.4%) |
| AJCC Stage Ib, n (%) | 8 (15.1%) |
| AJCC Stage IIa, n (%) | 7 (13.2%) |
| AJCC Stage IIb, n (%) | 6 (11.3%) |
| AJCC Stage IIIa, n (%) | 7 (13.2%) |
| AJCC Stage IIIb, n (%) | 11 (20.8%) |
| AJCC Stage IIIc, n (%) | 7 (13.2%) |
| AJCC Stage IV, n (%) | 1 (1.9%) |
Results
The mean operative time was 296.4±98.9 min, and the mean intraoperative blood loss was 294.3±213.8 mL. In 3 cases (5.7%), conversion was needed. In 1 case it was due to technical difficulties during anastomosis creation. In 2 cases the reason for conversion was uncertainty during assessment for potential radical resection. The mean number of harvested lymph nodes was 34.7±17.2 (13–52). In 47 cases R0 resection status was achieved. An analysis of surgical parameters is presented in Table 3.
Table 3.
Surgical parameters in analysed group.
| Parameter | Value |
|---|---|
| Mean operative time, min. ±SD | 296.4±98.9 |
| Median operative time, min. (IQR) | 280 (235–330) |
| Mean intraoperative blood loss, ml ±SD | 294.3±213.8 |
| Median intraoperative blood loss, ml (IQR) | 225 (200–300) |
| Conversion, n (%) | 3 (5.7%) |
Postoperative complications occurred in 17 (32.1%) patients, with 7 (13.2%) of them being severe (Clavien-Dindo 3–5). A detailed analysis of complications is presented in Table 4. There were 5 patients who developed anastomotic leakage postoperatively. In 1 case it was managed with endo-VAC therapy. The remaining cases required reoperation due to conservative treatment failure and symptoms of peritonitis or abscess (lavage, drainage, and additional suturing when possible). Another 2 patients required reoperation due to active bleeding and hematoma (both cases were managed laparoscopically). Two patients with anastomotic leakage died due to subsequent complications. Readmission within 30 days after discharge was necessary in 5 patients (9.4%). Reasons for readmissions were dehydration, surgical site infection, anastomotic leakage, and 2 cases of dysphagia. The mean and median LOS was 5.8±3.6 and 5 days, respectively. Thirty-two patients (60.4%) were discharged before the 7th day after surgery (Figure 2). Moreover, there were 2 patients with LOS of 2 days. They were admitted on the day of surgery (most of our patients are admitted the day before) and discharged in 2 postoperative days with no further readmissions. The overall compliance with ERAS protocol was 79.6±14.5%. Figure 3 details compliance with single protocol elements. Thirty (56.6%) patients tolerated an early oral diet well, and 48 patients (90.6%) were mobilized during the first 24 hours after surgery. Twenty-five (47.2%) patients did not require opioid analgesia.
Table 4.
Types of complications according to Clavien-Dindo classification.
| Clavien-Dindo classification | Complications | ||
|---|---|---|---|
| I | 9.4% | Surgical site infection | 1 |
| Postoperative nausea and vomiting | 2 | ||
| Postoperative paralytic ileus (managed conservatively) | 1 | ||
| Fever of unknown origin | 1 | ||
| II | 9.4% | Urinary tract infection | 1 |
| Infectious diarrhea (C. difficile) | 1 | ||
| Pneumonia | 2 | ||
| Surgical site infection (requiring antibiotics) | 1 | ||
| III A | 7.5% | Anastomotic leakage (managed endoscopically) | 1 |
| III B | Anastomotic leakage (reoperation) | 1 | |
| Intraperitoneal hematoma | 1 | ||
| Postoperative bleeding | 1 | ||
| IV | 1.9% | Anastomotic leakage (ICU stay) | 1 |
| V | 3.8% | Death (anastomotic leakage, peritonitis) | 2 |
Figure 2.
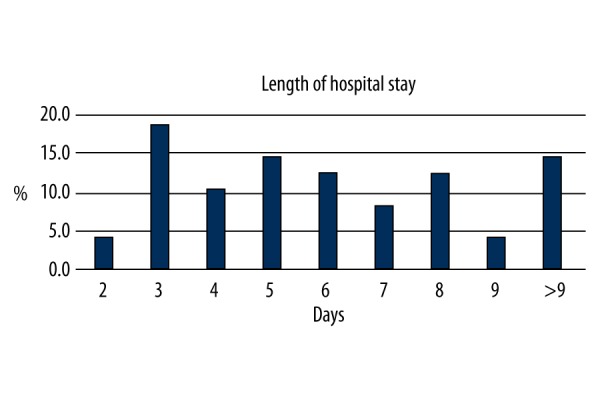
Percentage of patients based on the length of stay in hospital.
Figure 3.
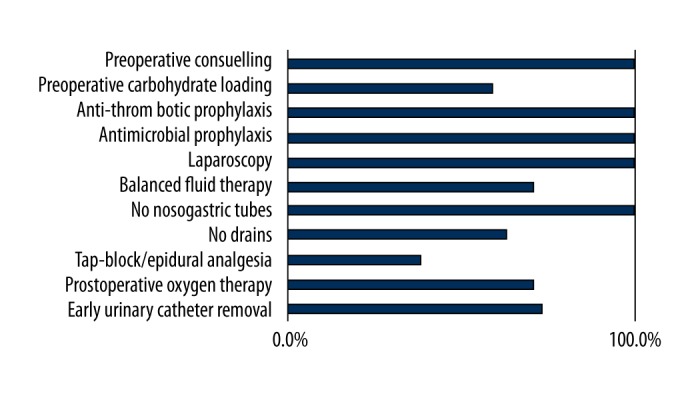
Compliance with pre- and intraoperative ERAS protocol elements in the studied group.
Discussion
The study showed that laparoscopic gastrectomy with D2 lymphadenectomy combined with the ERAS protocol was safe and feasible, and provided satisfactory short-term clinical outcomes.
The first laparoscopic total gastrectomy was successfully performed by Azagra et al. in 1993 [17]. Over the next twenty years it has become evident that the laparoscopic approach, although feasible, is associated with important drawbacks. A longer learning curve and increased operative time are among the main disadvantages of minimally invasive access to gastric cancer surgery. On the other hand, laparoscopy allows for many benefits, such as lower blood loss, reduced postoperative pain, decreased number of complications, faster recovery, and shortened LOS [12,18]. The long-standing discussion regarding the oncological safety of minimally invasive access was addressed in recent meta-analyses that clearly showed that it is non-inferior to open gastrectomy. In centers that routinely perform this procedure laparoscopically, the number of lymph nodes harvested and the R0 resection rate are comparable [10,19,20]. It is rather the experience of the surgeon and the center that influences clinical outcomes. In our unit laparoscopy is the method of choice in different types of oncological surgeries (gastric, colorectal, liver, pancreatic, and adrenal surgery). Therefore, over the last two decades we have gained enough experience to provide versatile and high-quality oncological surgery using the minimally invasive approach. The mean number of harvested lymph nodes was 34.7±17.2; there was only one patient (T2N0) who had fewer than 15 lymph nodes retrieved. R0 resection rate was 89%. These results are in line with other larger trials comprising patients undergoing laparoscopic total gastrectomy [21].
In the 1990s Kehlet brought up a concept of multimodal perioperative care in patients operated on due to colorectal cancer that we now know as the ERAS protocol [22]. He noticed that the combination of some elements of perioperative care leads to faster recovery and a lower complication rate. This resulted in shortening of the LOS to 2–3 days without increasing readmissions [19,23,24]. Short-term benefits of such modern perioperative care were proved by numerous randomized controlled trials on patients undergoing colon or rectal resections [19,23].
As observed in previous studies, the implementation of single ERAS elements influences the perioperative period, but only full compliance results in improved outcomes. The effect is not only shortening of the LOS but also a significant reduction of postoperative complications without an increase in readmissions. Since modern multimodal care involves all medical staff members (surgeons, anesthetists, nurses, dieticians, physiotherapists), the whole team should establish compliance with the protocol. Since 2014, the ERAS protocol has been a mainstay of perioperative care in our center regardless of the type of surgery performed. It allows maintaining a high level of adherence. In the case of gastric surgery, it is almost 80%. In colorectal surgery it was shown that compliance with the ERAS protocol influences outcomes [23].Thus, it can be assumed that high compliance also improves outcomes in gastric surgery, but this, however, needs further detailed analysis.
One of the most rooted dogmas in gastrointestinal surgery is the idea that an oral diet after resection should be introduced gradually, meaning nothing by mouth during the first few days after surgery, liquid meals in subsequent days, and full hospital diet within 4–5 postoperative days. However, there is no evidence for this viewpoint. Lassen et. al. have demonstrated that an early oral diet after major upper gastrointestinal surgery is safe and well tolerated by patients, and reduces the number of complications and even mortality [25]. Moreover, patients prefer an early solid diet rather than a liquid oral diet.
What is important is that in 45.8% our patients iv fluids were stopped within 24 h postoperatively and were replaced with oral intake. It has been shown that balanced perioperative fluid therapy may play a crucial role in postoperative recovery. Therefore, one of the most important ERAS elements is optimal hydration of patients before surgery, avoiding excess sodium and intravenous fluids; early introduction of oral fluids after surgery also seems to be crucial in improvement of clinical outcomes [26,27]. These benefits include faster gastrointestinal recovery, decreased postoperative nausea and vomiting, and improved wound healing. According to recent meta-analyses balanced fluid therapy can reduce the complication rate even up to 50% [27,28].
Dogmas in the use of nasogastric tubes and drains were also revised. It was shown that keeping a nasogastric tube does not help in the reduction of the number of complications, but it slows peristalsis return, increases the number of respiratory complications, and prolongs LOS [29–31]. Routine drainage was also associated with no benefit in the postoperative period. It does not decrease the number of anastomosis dehiscence or intra-abdominal abscesses, and its use also increased LOS [32,33].
In our group of patients, use of the ERAS protocol combined with laparoscopy resulted in 90% of the patients being mobilized early, and in 60% of the patients an oral diet introduced on the day of surgery was tolerated well. Time to first flatus was 1.5 days. Median LOS was 5 days, and it was generally shorter than the results presented by other authors [34–37]. In our opinion it is an effect of laparoscopy in combination with the ERAS protocol. It was shown that these elements shorten LOS, and their simultaneous use has a synergistic effect. In colorectal surgery, ERAS protocol implementation shortens LOS even in patients operated on classically [8].
Looking into our results, we noted that the rate of severe complications was 13.2%. It is comparable to the rates in other reports; however, the leakage rate was relatively high and may be the result of the small number of patients. It should be emphasized that three patients who developed leakage had very high esophago-jejunal anastomosis, which was technically demanding (despite a negative leak test), and this leakage may have been the result of its later insufficiency. Although this requires further studies, we are convinced that ERAS perioperative care guarantees non-inferiority. The rate of complications in gastric surgery can vary significantly. For instance, Cushieri et al. noticed a complication rate of 46% [2]. In the meantime, Kim et al. reported a 10% complication rate in their group [38]. Such a difference can be a result of several factors: the type of surgery (open vs. laparoscopic), demographic parameters, stage of cancer, etc. It is worth mentioning that differences can also result from the manner in which the complications were reported. Only some authors use Clavien-Dindo classification. Others report only severe complications, frequently ignoring those complications that did not require intervention. It is worth pointing out that our study included patients regardless their age, stage of tumor, and history of neoadjuvant chemotherapy.
In 2015, Beamish et al. published the systematic review of fourteen trials (nine randomized and five non-randomized) comparing ERAS and non-ERAS gastric cancer surgery [39]. They noticed reduced LOS in all studies. Although the decrease in the complication rate was not confirmed when all studies were calculated, it became significant when only good-quality trials were included. Moreover, not a single trial showed any difference in the readmission rate. Interestingly, there was a significant trend toward cost reduction in patients with ERAS. The authors concluded that multimodal, standardized perioperative gastrectomy care according to ERAS principles appears feasible, safe, and cost-effective.
Our study has limitations typical of a single-center study. First of all, it included a limited number of patients. Moreover, the ERAS protocol is currently part of our routine perioperative care independently of the type of surgery and operated organ, and it is possible that the results of similar studies in other centers with worse protocol performance could be different. Additionally, it is worth mentioning that we analyzed only short-term outcomes: within 30 days after surgery. Finally, we admit that a comparison with open surgery/traditional care cases would be of great value. However, the simple comparison of an ERAS group with an historical cohort is not possible in our case. Before the study period, we were practically not performing gastric cancer surgery at all. Besides, complications were not reported as carefully as they are now (no prospective database, no classification). For these reasons, including historical open cases would be biased. After changes in the structure of our university hospital (a new laparoscopic oncological surgery unit was created), we started performing gastric cancer surgery laparoscopically. We are strongly convinced of the benefits of laparoscopy in the case of gastric cancer; therefore, it is our method of choice in all cases, so we are not able to provide open surgery cases to compare with our results.
Conclusions
The combination of laparoscopic surgery and ERAS is not inferior to open, traditional surgery. It allows achieving satisfactory short-term outcomes (short LOS, fast postoperative recovery, acceptable complication and readmission rates) in a group of patients operated on for gastric cancer. However, the experience of the surgical team in perioperative care based on ERAS protocol principles is mandatory to provide high compliance with the protocol. Due to the fact that this approach to gastric cancer patients is rather new, more studies are required to further increase the validity of this concept.
Footnotes
Conflict of Interest Statement
Magdalena Pisarska, Michał Pędziwiatr, Piotr Major, Michał Kisielewski, Marcin Migaczewski, Mateusz Rubinkiewicz, Piotr Budzyński, Krzysztof Przęczek, Anna Zub-Pokrowiecka, and Andrzej Budzyński declare no conflict of interest.
Source of support: The publication of this paper was supported by the Faculty of Medicine, Jagiellonian University Medical College, Cracow, Poland, Leading National Research Centre (KNOW) 2012–2017
References
- 1.Bonenkamp JJ1, Songun I, Hermans J, et al. Randomised comparison of morbidity after D1 and D2 dissection for gastric cancer in 996 Dutch patients. Lancet. 1995;345(8952):745–48. doi: 10.1016/s0140-6736(95)90637-1. [DOI] [PubMed] [Google Scholar]
- 2.Cuschieri A, Fayers P, Fielding J, et al. Postoperative morbidity and mortality after D1 and D2 resections for gastric cancer: preliminary results of the MRC randomised controlled surgical trial. The Surgical Cooperative Group. Lancet. 1996;347(9007):995–99. doi: 10.1016/s0140-6736(96)90144-0. [DOI] [PubMed] [Google Scholar]
- 3.Schütz T, Valentini L, Herbst B, et al. [ESPEN guidelines on enteral nutrition – summary]. Z Gastroenterol. 2006;44(8):683–84. doi: 10.1055/s-2006-950850. [in German] [DOI] [PubMed] [Google Scholar]
- 4.Rey-Ferro M, Castaño R, Orozco O, et al. Nutritional and immunologic evaluation of patients with gastric cancer before and after surgery. Nutrition. 1997;13(10):878–81. doi: 10.1016/s0899-9007(97)00269-4. [DOI] [PubMed] [Google Scholar]
- 5.Scott MJ, Baldini G, Fearon KC, et al. Enhanced Recovery After Surgery (ERAS) for gastrointestinal surgery, part 1: Pathophysiological considerations. Acta Anaesthesiol Scand. 2015;59(10):1212–31. doi: 10.1111/aas.12601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Spanjersberg WR, van Sambeeck JD, Bremers A, et al. Systematic review and meta-analysis for laparoscopic versus open colon surgery with or without an ERAS programme. Surg Endosc. 2015;29(12):3443–53. doi: 10.1007/s00464-015-4148-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Vlug MS, Wind J, Hollmann MW, et al. Laparoscopy in combination with fast track multimodal management is the best perioperative strategy in patients undergoing colonic surgery: A randomized clinical trial (LAFA-study) Ann Surg. 2011;254(6):868–75. doi: 10.1097/SLA.0b013e31821fd1ce. [DOI] [PubMed] [Google Scholar]
- 8.Kennedy RH, Francis EA, Wharton R, et al. Multicenter randomized controlled trial of conventional versus laparoscopic surgery for colorectal cancer within an enhanced recovery programme: EnROL. J Clin Oncol. 2014;32(17):1804–11. doi: 10.1200/JCO.2013.54.3694. [DOI] [PubMed] [Google Scholar]
- 9.Wang W, Li Z, Tang J, Wang M, et al. Laparoscopic versus open total gastrectomy with D2 dissection for gastric cancer: A meta-analysis. J Cancer Res Clin Oncol. 2013;139(10):1721–34. doi: 10.1007/s00432-013-1462-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Chen XZ, Wen L, Rui YY, et al. Long-term survival outcomes of laparoscopic versus open gastrectomy for gastric cancer: A systematic review and meta-analysis. Medicine (Baltimore) 2015;94(4):e454. doi: 10.1097/MD.0000000000000454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Chen K, Pan Y, Cai JQ, et al. Totally laparoscopic gastrectomy for gastric cancer: A systematic review and meta-analysis of outcomes compared with open surgery. World J Gastroenterol. 2014;20(42):15867–78. doi: 10.3748/wjg.v20.i42.15867. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Straatman J, van der Wielen N, Cuesta MA, et al. Minimally invasive versus open total gastrectomy for gastric cancer: A systematic review and meta-analysis of short-term outcomes and completeness of resection: Surgical techniques in gastric cancer. World J Surg. 2016;40(1):148–57. doi: 10.1007/s00268-015-3223-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Muneer M, Abdelrahman H, El-Menyar A, et al. Portomesenteric vein thrombosis after laparoscopic sleeve gastrectomy: 3 case reports and a literature review. Am J Case Rep. 2016;17:241–47. doi: 10.12659/AJCR.896892. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Cunningham D, Allum WH, Stenning SP, et al. Perioperative chemotherapy versus surgery alone for resectable gastroesophageal cancer. N Engl J Med. 2006;355(1):11–20. doi: 10.1056/NEJMoa055531. [DOI] [PubMed] [Google Scholar]
- 15.Mortensen K, Nilsson M, Slim K, et al. Consensus guidelines for enhanced recovery after gastrectomy: Enhanced Recovery After Surgery (ERAS®) Society recommendations. Br J Surg. 2014;101(10):1209–29. doi: 10.1002/bjs.9582. [DOI] [PubMed] [Google Scholar]
- 16.Gustafsson UO, Hausel J, Thorell A, et al. Adherence to the enhanced recovery after surgery protocol and outcomes after colorectal cancer surgery. Arch Surg. 2011;146(5):571–77. doi: 10.1001/archsurg.2010.309. [DOI] [PubMed] [Google Scholar]
- 17.Azagra JS, Goergen M, De Simone P, Ibañez-Aguirre J. Minimally invasive surgery for gastric cancer. Surg Endosc. 1999;13(4):351–57. doi: 10.1007/s004649900988. [DOI] [PubMed] [Google Scholar]
- 18.Zou ZH, Zhao LY, Mou TY, et al. Laparoscopic vs. open D2 gastrectomy for locally advanced gastric cancer: A meta-analysis. World J Gastroenterol. 2014;20(44):16750–64. doi: 10.3748/wjg.v20.i44.16750. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Zhuang CL, Huang DD, Chen FF, et al. Laparoscopic versus open colorectal surgery within enhanced recovery after surgery programs: A systematic review and meta-analysis of randomized controlled trials. Surg Endosc. 2015;29(8):2091–100. doi: 10.1007/s00464-014-3922-y. [DOI] [PubMed] [Google Scholar]
- 20.Kim W, Kim HH, Han SU, et al. Decreased morbidity of laparoscopic distal gastrectomy compared with open distal gastrectomy for stage I gastric cancer: Short-term outcomes from a multicenter randomized controlled trial (KLASS-01) Ann Surg. 2016;263(1):28–35. doi: 10.1097/SLA.0000000000001346. [DOI] [PubMed] [Google Scholar]
- 21.Haverkamp L, Weijs TJ, van der Sluis PC, et al. Laparoscopic total gastrectomy versus open total gastrectomy for cancer: A systematic review and meta-analysis. Surg Endosc. 2013;27(5):1509–20. doi: 10.1007/s00464-012-2661-1. [DOI] [PubMed] [Google Scholar]
- 22.Kehlet H. Multimodal approach to control postoperative pathophysiology and rehabilitation. Br J Anaesth. 1997;78(5):606–17. doi: 10.1093/bja/78.5.606. [DOI] [PubMed] [Google Scholar]
- 23.Greco M, Capretti G, Beretta L, et al. Enhanced recovery program in colorectal surgery: A meta-analysis of randomized controlled trials. World J Surg. 2014;38(6):1531–41. doi: 10.1007/s00268-013-2416-8. [DOI] [PubMed] [Google Scholar]
- 24.Nicholson A, Lowe MC, Parker J, et al. Systematic review and meta-analysis of enhanced recovery programmes in surgical patients. Br J Surg. 2014;101(3):172–88. doi: 10.1002/bjs.9394. [DOI] [PubMed] [Google Scholar]
- 25.Lassen K, Kjaeve J, Fetveit T, et al. Allowing normal food at will after major upper gastrointestinal surgery does not increase morbidity: A randomized multicenter trial. Ann Surg. 2008;247(5):721–29. doi: 10.1097/SLA.0b013e31815cca68. [DOI] [PubMed] [Google Scholar]
- 26.Miller TE, Roche AM, Mythen M. Fluid management and goal-directed therapy as an adjunct to Enhanced Recovery After Surgery (ERAS) Can J Anaesth. 2015;62(2):158–68. doi: 10.1007/s12630-014-0266-y. [DOI] [PubMed] [Google Scholar]
- 27.Brandstrup B, Tønnesen H, Beier-Holgersen R, et al. Effects of intravenous fluid restriction on postoperative complications: comparison of two perioperative fluid regimens: A randomized assessor-blinded multicenter trial. Ann Surg. 2003;238(5):641–48. doi: 10.1097/01.sla.0000094387.50865.23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Varadhan KK, Lobo DN. A meta-analysis of randomised controlled trials of intravenous fluid therapy in major elective open abdominal surgery: Getting the balance right. Proc Nutr Soc. 2010;69(4):488–98. doi: 10.1017/S0029665110001734. [DOI] [PubMed] [Google Scholar]
- 29.Nelson R, Tse B, Edwards S. Systematic review of prophylactic nasogastric decompression after abdominal operations. Br J Surg. 2005;92(6):673–80. doi: 10.1002/bjs.5090. [DOI] [PubMed] [Google Scholar]
- 30.Chen K, Mou YP, Xu XW, et al. [Necessity of routine nasogastric decompression after gastrectomy for gastric cancer: A meta-analysis]. Zhonghua Yi Xue Za Zhi. 2012;92(26):1841–44. [in Chinese] [PubMed] [Google Scholar]
- 31.Wang D, Li T, Yu J, et al. Is nasogastric or nasojejunal decompression necessary following gastrectomy for gastric cancer? A systematic review and meta-analysis of randomised controlled trials. J Gastrointest Surg. 2015;19(1):195–204. doi: 10.1007/s11605-014-2648-4. [DOI] [PubMed] [Google Scholar]
- 32.Liu HP, Zhang YC, Zhang YL, et al. Drain versus no-drain after gastrectomy for patients with advanced gastric cancer: Systematic review and meta-analysis. Dig Surg. 2011;28(3):178–89. doi: 10.1159/000323954. [DOI] [PubMed] [Google Scholar]
- 33.Wang Z, Chen J, Su K, Dong Z. Abdominal drainage versus no drainage post-gastrectomy for gastric cancer. Cochrane Database Syst Rev. 2015;5:CD008788. doi: 10.1002/14651858.CD008788.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Zhang Y, Qi F, Jiang Y, et al. Long-term follow-up after laparoscopic versus open distal gastrectomy for advanced gastric cancer. Int J Clin Exp Med. 2015;8(8):13564–70. [PMC free article] [PubMed] [Google Scholar]
- 35.Tuttle R, Hochwald SN, Kukar M, Ben-David K. Total laparoscopic resection for advanced gastric cancer is safe and feasible in the Western population. Surg Endosc. 2016;30(8):3552–58. doi: 10.1007/s00464-015-4652-5. [DOI] [PubMed] [Google Scholar]
- 36.Jung HS, Park YK, Ryu SY, Jeong O, et al. Laparoscopic total gastrectomy in elderly patients (≥70 years) with gastric carcinoma: A retrospective study. J Gastric Cancer. 2015;15(3):176–82. doi: 10.5230/jgc.2015.15.3.176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Lee SH, Kim IH, Kim IH, et al. Comparison of short-term outcomes and acute inflammatory response between laparoscopy-assisted and totally laparoscopic distal gastrectomy for early gastric cancer. Ann Surg Treat Res. 2015;89(4):176–82. doi: 10.4174/astr.2015.89.4.176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Kim HH, Hyung WJ, Cho GS, et al. Morbidity and mortality of laparoscopic gastrectomy versus open gastrectomy for gastric cancer: an interim report – a phase III multicenter, prospective, randomized Trial (KLASS Trial) Ann Surg. 2010;251(3):417–20. doi: 10.1097/SLA.0b013e3181cc8f6b. [DOI] [PubMed] [Google Scholar]
- 39.Beamish AJ, Chan DS, Blake PA, et al. Systematic review and meta-analysis of enhanced recovery programmes in gastric cancer surgery. Int J Surg. 2015;19:46–54. doi: 10.1016/j.ijsu.2015.05.021. [DOI] [PubMed] [Google Scholar]


