Abstract
Schizophrenia is characterised by the psychotic symptoms of hallucinations and delusions, accompanied by variable degrees of loss of insight. Whilst there is heterogeneity in the clinical profile, and presumably in the pathogenesis of what is currently called 'schizophrenia', it has become absolutely clear over the past decade that schizophrenic symptoms are consequent upon serious brain dysfunction. This new perspective has laid to rest a variety of 'crazy' theories, including the notion that mental illness was a myth, or that schizophrenia could be caused by faulty child rearing.
The use of dopamine-blocking drugs has led to an improvement in symptom control, and diminished the need for prolonged hospital stays. It was hoped that the clear relationship between antipsychotic activity and dopamine blockade would help to elucidate the pathophysiology of schizophrenia, but to date no consistent abnormalities of the dopamine system have been found. Nevertheless, we have learned much about both the aetiology of schizophrenia and the origin of particular symptoms. Much of this has stemmed from increased understanding of the brain abnormalities underlying the disorder.
Full text
PDF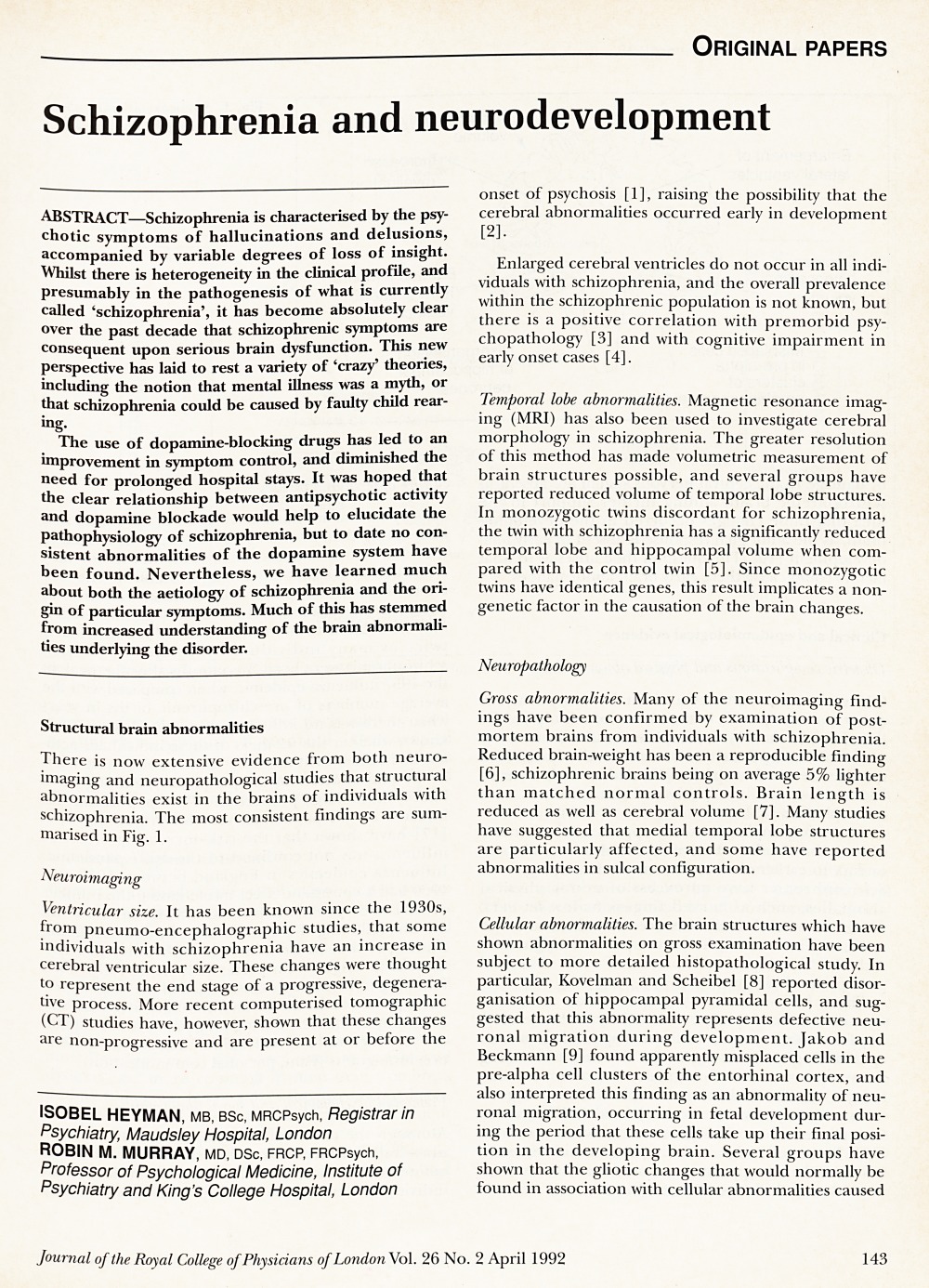
Contributor Information
Isobel Heyman, Registrar in Psychiatry, Maudsley Hospital, London.
Robin M. Murray, Professor of Psychological Medicine, Institute of Psychiatry and King's College Hospital, London