Abstract
Introduction Smoking has many adverse effects on the oral and pharyngeal mucosa. Outcomes may be developing tonsillar infections and predisposing for post tonsillectomy bleeding (PTB).
Objective The objective of our study was to determine whether smokers have more chronic/recurrent tonsillitis indicating for tonsillectomy or develop more PTB episodes.
Methods We conducted a retrospective study on two groups of adults (age ≥18 years). Cohort 1: Smoking among patients who underwent tonsillectomy for recurrent/chronic tonsillitis. Cohort 2: Smoking among patients requiring control of PTB that were operated primarily for recurrent/chronic tonsillitis. Cohort 1 served as a population-reference for the second. We retrieved the data from medical records.
Results Cohort 1: 206 adults aged 18–50 years (mean 26 ± 7.6). 28% (57 patients) were smokers, versus 24% and 20% in the general population (in the years 2000 and 2010; p = 0.5, p = 0.18, respectively). Cohort 2: 114 adults aged 18–73 years (mean 26 ± 7.6). 43% were smokers, double the incidence in the general population (p = 0.004, p = 0.0004, in 2000 and 2010, respectively), and 1.5 times cohort 1 (p = 0.02). Smoking rates among bleeders on post-operative days 8–10 and later than day 10 were 53% and 60% (p = 0.0005 and p < 0.0001, respectively). Five of ten patients presenting a second PTB were smokers. Timing of re-bleedings was similar to their first PTB and dated similarly as first PTB of the entire group, mean 5.6 days (SD ± 3.2).
Conclusion Smokers may encounter more chronic/recurrent tonsillitis episodes, indicating tonsillectomy and significantly are more prone for PTB. Smoking cessation may perhaps diminish recurrent/chronic tonsillitis. Whether pre-operative abstinence or its length would reduce PTB incidence is yet to be determined.
Keywords: tonsillitis, tonsillectomy, smoking, postoperative complications, postoperative hemorrhage
Introduction
Smoking has adverse effects on the oral, gingival, and pharyngeal mucosal surfaces, causing structural changes and atrophy.1 2 In addition to the reduction in salivary flow and the decreased mucosal immunity, smoking has been shown to adversely affect the oral microflora.3 4 5 6 These changes may result in developing more tonsillar infections. In fact, smoking has been reported to be associated with having a greater incidence of peritonsillar abscesses.7 8 9
Infections of the tonsillar fossa (peritonsillar abscesses, recurrent and chronic tonsillitis) are considered to be indications for tonsillectomy. Although this is a common surgical procedure, tonsillectomy can be complicated by a major post-operative complication, such as post tonsillectomy bleeding (PTB). The incidence of PTB in adults has been recently reported to be between 2–15%.10 11 12 Therefore, understanding the factors that may cause PTB is of great interest. PTB was previously associated with the following risk factors: an older age, that is, above 35 years, hot dissection vis-à-vis cold dissection techniques, complete tonsillectomy in comparison to tonsillotomy, occurrence of a minor post-operative bleeding episode, surgery performed during the winter months, male sex, and blood group O.13 14 15 16 17 18
To date, smoking has not been clearly considered a significant risk factor for PTB. Yet, smoking was associated with increased rates of post-operative bleeding in several other surgical procedures, such as abdominal, thyroid, and kidney operations.19 20 21 22
The objectives of this study were to study the occurrence of tobacco smoking among adults with recurrent/chronic tonsillitis warranting tonsillectomy, and to assess whether adult smokers who underwent tonsillectomy for such indications are more prone to develop PTB. In addition, a short practical clinical discussion is presented.
Patients and Methods
The Institutional Review Board of the Edith Wolfson Medical Center approved the study (Protocol Number: 123–14-WOMC), which included two different independent cohorts of patients. Each cohort included adults aged 18 or older who received treatment over 11 years (between January 1st, 2000, and December 31st, 2010) in the Otolaryngology-Head and Neck Surgery Department in a secondary medical center providing regional 24/7 medical emergency care.
Our first research question was to study the rate of smokers among adults undergoing tonsillectomy. Therefore, the first cohort included eligible patients who underwent an elective tonsillectomy for recurrent/chronic tonsillitis in our medical center (“Cohort 1”). Our second research question was to study the incidence of smokers among patients presenting with PTB (“Cohort 2”). Therefore, the second cohort included patients who had undergone an elective tonsillectomy in various medical centers, including our own, and were admitted to our service, since they required intervention under anesthesia to control considerable PTB.
All patients included had undergone tonsillectomy for recurrent/chronic tonsillitis, according to the accepted guidelines.23 24 Various surgeons operated on the patients utilizing different operative techniques, that is, cold dissection, electro-dissection, and coblation. A few of the patients who were enrolled in cohort 1 were also enrolled in cohort 2 if they had been operated in our medical center and later presented with PTB. The significance of this fact is low, since we studied the relative share of smokers in each cohort, and reported them in our PTB rates.
For both studies, we retrieved demographic and clinical data from hospital medical records and included age, gender, medical past history, indication for tonsillectomy, medical treatment, blood tests (PTT; partial thromboplastin time, PT; prothrombin time, and platelets count), and smoking habits. “Smoking” status was considered if 1) a patient declared him/herself as a smoker as stated in the medical interview, and 2) had been smoking more than 5 cigarettes per day.
For patients who presented with PTB (cohort 2), we recorded the post-operative date on which the bleeding occurred, re-PTB bleeding date(s) and the surgical technique employed as well. The day on which PTB (or re-PTB) occurred was calculated from the day on which tonsillectomy was performed (day “0”).
Exclusion criteria for both studies included age less than 18 years, patients who had tonsillectomy for indications other than recurrent acute or chronic tonsillitis. We excluded patients who underwent an expanded or additive intervention along with tonsillectomy, such as adenoidectomy or UPPP (uvulo-palato-pharyngoplasty), since they may possibly have a higher probability to bleed and to create a homogenous group. We also excluded patients with abnormal coagulation blood workup, past history of excessive bleeding, on current anti-coagulant/anti-platelet treatment, and with any disease that could potentially lead to bleeding tendency.
Statistical analysis was performed with SPSS (IBM Corp., Armonk, U.S.A.) for Windows version 10.0 software employing χ2 test. p < 0.05 was considered significant. In the discussion section, we used a χ2 test to compare between our results to results previously reported in other studies.
Results
Cohort 1: we identified 206 adults who underwent tonsillectomy for recurrent/chronic tonsillitis in our medical center and met the eligibility criteria. Among them, 126 (53%) were women and 80 (47%) men, aged 18–50 years (mean 26, SD ± 7.2 years). Of them, 57 (28%) patients were smokers, which is a higher rate than the reported smoking incidence in the adult local population, that is, 24% in 2000 and 20% in 2010 (p = 0.5 and 0.18, respectively).25 26
Cohort 2: we identified 114 adults with PTB. Sixty were men (53%), and 54 (47%) women, aged 18–73 years (mean 26, SD ± 7.6 years). 50 (43%) PTB patients were smokers, double the reported incidence in the general adult population (p = 0.004 and p = 0.0004, regarding 2000 and 2010, respectively), and 1.5 times higher than the incidence of the reference population (cohort 1) (p = 0.02).
Most patients (60%) presented with PTB on post-operative days 3 to 4 while mean was 5.6 days (SD ± 3.2) with no significant “timing” difference between smokers and non-smokers. Noteworthy is that the proportion of smokers was higher than the mean (43%) in patients with PTB presenting on post-operative days 8–10, and was even more remarkable in those patients who presented with PTB after more than 10 days post-operatively: 53% (p = 0.0005) and 60% (p < 0.0001), respectively (Table 1, Fig. 1).
Table 1. Post-tonsillectomy bleeding (PTB) in adults: demographics and data.
| PTB datea | Day 1 | Day 2–3 |
Day 4–5 |
Day 6–7 |
Day 8–9 |
Day ≥ 10 |
Total |
|---|---|---|---|---|---|---|---|
| Patients | 9 | 17 | 33 | 36 | 9 | 10 | 114 |
| Men | 7 | 9 | 16 | 21 | 3 | 5 | 60 |
| Women | 2 | 8 | 17 | 15 | 6 | 5 | 54 |
| Age, years ( ± SD) | 30.6 (17) | 25.3 (4.6) | 25.7 (5.6) | 26 (5) | 23.3 (8) | 28.2 (6) | 26.3 (7.5) |
| Smoker | 4 (44%) | 9 (53%) | 12 (36%) | 15 (42%) | 4 (44%) | 6 (60%) | 50 (43%) |
| Non-smoker | 5 (56%) | 8 (47%) | 21 (64%) | 21 (58%) | 5 (56%) | 4 (40%) | 64 (57%) |
PTB date: post-operative day.
Fig. 1.
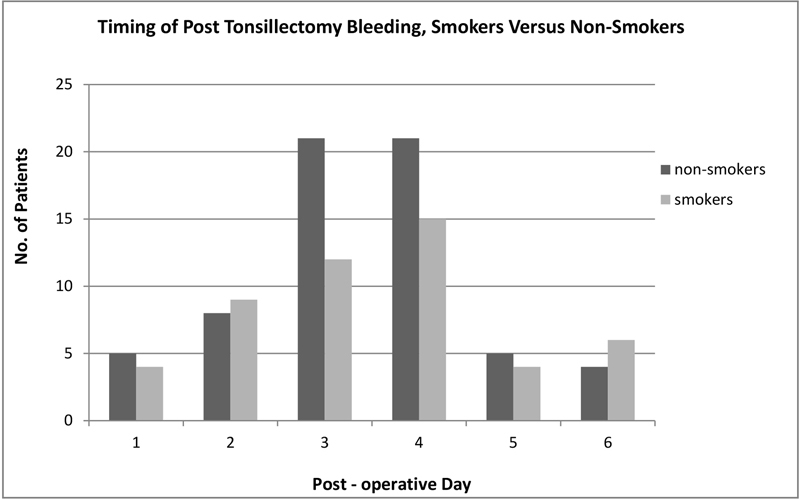
60% bleed between post-operative days 3–4. No significant “timing” difference between smokers and non-smokers. Proportion of smokers among bleeders was 43%, double their share in the general population, 1.5 times cohort 1. Smoking among bleeders presenting on post-operative days 8–10, and after more than 10 days was 53% (p = 0.0005) and 60% (p < 0.0001), respectively.
Ten patients required a second surgical intervention under anesthesia to control re-bleeding, 6 of them men and 4 were women, aged 18–34 years (mean 26, SD ± 5.8 years). Of them, 5 (50%) were smokers. Six (60%) had their first PTB between days 4–5, and a similar “timing” of re-bleeding episodes (mean: 4.5, SD ± 5.2 days), similar to the entire PTB group (Table 2, Fig. 2).
Table 2. Post-tonsillectomy recurrent bleeding: timing of PTB episodes.
| Day 1 |
Day 2–3 |
Day 4–5 |
Day 6–7 |
Day 8–9 |
Day ≥ 10 |
Total | |
|---|---|---|---|---|---|---|---|
| a PTB 1 | 1 | 1 | 6 | 2 | -- | -- | 10 |
| b PTB 2 | 1 | -- | 1 | 4 | 2 | 2 | 10 |
PTB 1: post-operative day on which bleeding occurred, dating from the original tonsillectomy.
PTB 2: post-operative day on which second bleeding occurred, dating from intervention to control first PTB.
Fig. 2.
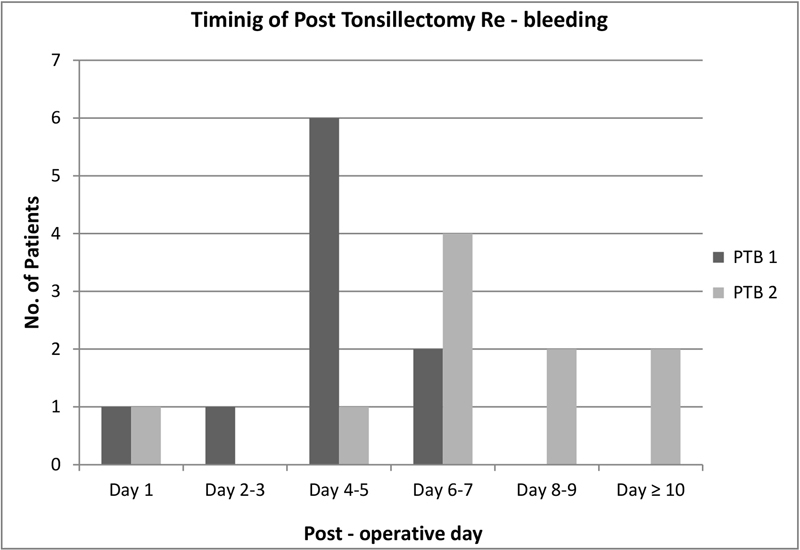
Ten patients required a second intervention to control re-bleeding. Five (50%) were smokers. Timing of their first episode was similar to the entire PTB group. Although it may seem that the “timing” of the re-bleeding episode was longer than the first, difference was insignificant (mean: 5.6 days versus 4.5, respectively).
Discussion
The association between smoking and infectious diseases of the tonsils among adults was our interest. Recent publications pointed out that smoking is associated with the development of more events of peritonsillar abscess episodes in adults.7 8 9 However, the association of smoking and recurrent acute and/or chronic tonsillitis has been neither extensively investigated nor clarified.
Although not statistically significant, cohort 1 had a higher rate of smokers among the adult population who underwent tonsillectomy for recurrent/chronic tonsillitis, in comparison to smokers' presentation in the relevant adult general population. This implies that smoking may affect or predispose adults to develop recurrent and chronic tonsillitis in such gravity that tonsillectomy is indicated.
We found an additional strength to our observation by retrieving and analyzing data from a study conducted by Demars et al in addition to the relevant demographic information obtained from statistics released by the Washington State Department of Health respectively and the Centers for Disease Control and Prevention.27 28 29 30 They reported that among 569 adult patients, aged 29 ± 10 years, who underwent tonsillectomy alone, 164 (28.8%) were smokers. The reported adult smokers' rate in the general population in the state of Washington was 15% in 2008, lower than in our group and lower than the average U.S. rate. We have compared the smokers rate in the operated group reported by Demars et al, to the general population (state of Washington), and found it significantly higher (p = 0.016). Noteworthy is that the medical center in which the study took place served mostly military personnel and their families, a population in which smoking in males is estimated at ∼24% for the same age, as the operated cohort.7 30 Although not all the operated patients were military personnel males, even a comparison to the higher smoking rate of among military male personnel reveals an elevated, yet non-statistically significant, rate of smokers in the operated group (p = 0.4).
The population of our first cohort was a homogenous group (adults that underwent tonsillectomy for recurrent/chronic tonsillitis), which was clearly different from the general population, in terms of the smoking rates. Therefore, it was the most valid reference group to which we could compare the rate of smokers among PTB who underwent the same procedure for the same indication. An additional strength of our first cohort was the patients' age, which compared well with other populations of adults who underwent tonsillectomy for recurrent/chronic tonsillitis in other studies.24 27
Cohort 2 showed a clear association between smoking and PTB in adults: the rate of smokers among bleeders was double the incidence of smokers in the relevant general population, and more importantly, 1.5 times higher than the reference study population. This association was even more remarkable among late bleeders and observed in 5/10 patients with re-PTB. Noteworthy is the observation that the timing of most second PTBs after the first PTB-control intervention dated similar to the first PTB for the entire group.
In his article “Haemorrhage following Tonsillectomy” published in 1938, Ashcroft listed factors that he thought would precipitate PTB: chronic alcoholism, menstruation, patients having “unstable temperaments,” sandy haired children, and heavy smokers. He recommended abstaining from alcohol and smoking three days before tonsillectomy to avoid PTB, however without providing any supporting data.31
Since then, studies have reported numerous risk factors for the development of PTB as previously mentioned. Yet, the relation between smoking and PTB has not been thoroughly investigated. A recent publication reported 68 episodes of PTB in 56 adult patients, of which 28 (41%) were smokers. A significant increased rate of PTB among the operated smokers was found when compared with non-smoker adults (10.2% and 5.4%, respectively, p = 0.01). It is noteworthy that this study included patients who had undergone both tonsillectomy alone and UPPP, an extended procedure that may have a higher chance to bleed.31 Another study reported 17 adults with an average age of 45.5 years who presented with re-PTB bleeding. Within this group, 11 (64%) were smokers.32
The strengths of “cohort 2” results are having a homogenous adult group of patients sharing the same indications for the same intervention. In addition, we compared smoking habits not only to the general population, but to a specifically generated reference-population (“cohort 1”), rendering greater validity to our results. Our results are further supported by being in line with previously reported observations, that is, most PTBs occurred between post-operative days 4–7, as well as the fact that the average age of both bleeders and re-bleeders was 26 years.24 27 32
Explanations for a higher rate of recurrent acute or chronic tonsillitis among smokers as well as PTB may be attributed to systemic and local factors, since smoking decreases tissue oxygenation and aerobe metabolism.33 34 Such alterations induce pharyngeal microflora changes that have an adverse effect of oropharyngeal colonization with potential pathogens.3 4 5 Smokers were reported to have significant Vitamin D deficiency, a modulator of the immune system, which may have a negative impact.35 Coupled with the information that adults with Vitamin D deficiency suffer from more recurrent acute streptococcal tonsillitis, this may offer additional understanding of our observation in cohort 1.36 37
There is a significant body of evidence showing the adverse effect of smoking upon wound healing and post-operative bleeding.19 20 21 22 34 38 39 40 Local factors have an unfavorable impact upon healing response and bleeding. A histological study of tonsils from 22 patients who had tonsillectomy for recurrent tonsillitis compared 10 non-smokers with 12 smokers. The tonsils removed from smokers had severe impairment of their histological architecture: dense collagen matrix, fibrosis, edema, hemorrhage, and crypt epithelium with focal basement membrane disruption, cellular degeneration and superficial erosions.2 Smoking causes reduction of inflammatory cell chemotactic responsiveness, migratory function, and oxidative bactericidal mechanisms. The proliferative response is impaired by a reduced fibroblast migration and proliferation in addition to an impaired collagen synthesis and deposition.36
The presented study has some limitations we acknowledge. This was a retrospective study of not a large-scale population. However, it did hold a fair number of participants and significance has been pointed out regarding several outcomes. The data available did not include, and was therefore not reported, some possibly interesting and relevant information, more precisely, the exact smoking details of the patients who presented with PTB (how many cigarettes after the surgery). Yet, we attribute the propensity to develop PTB to the chronic effects of smoking on the tonsillar mucosa, as previously discussed. Additionally, the method of surgery can also influence the risk for PTB. We minimized this bias by enrolling PTB patients who were operated by various specialist surgeons in several medical facilities employing different surgical methods. We were unable to demonstrate that operative differences predisposed for PTB among patients in cohort 2 (data not shown).
At this time, it seems that PTB may be facilitated by smoking and it is reasonable to advise for smoking cessation before tonsillectomy. However, the period of abstinence providing an evident reduction in PTB needs to be determined.
Based on a broad body of reported data, a preoperative smoking abstinence may generally reduce postoperative complications, especially allowing better wound healing. It may diminish general anesthesia related complications which smokers are prone to encounter, such as barotrauma injuries and infections, having hyperactivity of airways and excessive sputum production.41 42 43 44 45 46 47 48
Conclusions
Despite the heterogeneity of factors associated with developing chronic/recurrent tonsillitis and PTB, in addition with the limited cohort, adult smokers do seem to encounter more chronic/recurrent tonsillitis indicating tonsillectomy and significantly greater PTB. Whether smoking cessation diminishes recurrent/chronic tonsillitis or preoperative abstinence and its length would reduce PTB is yet to be determined.
References
- 1.Taybos G. Oral changes associated with tobacco use. Am J Med Sci. 2003;326(04):179–182. doi: 10.1097/00000441-200310000-00005. [DOI] [PubMed] [Google Scholar]
- 2.Torre V, Bucolo S, Giordano C et al. Palatine tonsils in smoker and non-smoker patients: a pilot clinicopathological and ultrastructural study. J Oral Pathol Med. 2005;34(07):390–396. doi: 10.1111/j.1600-0714.2005.00319.x. [DOI] [PubMed] [Google Scholar]
- 3.Brook I, Gober A E. Recovery of potential pathogens and interfering bacteria in the nasopharynx of smokers and nonsmokers. Chest. 2005;127(06):2072–2075. doi: 10.1378/chest.127.6.2072. [DOI] [PubMed] [Google Scholar]
- 4.Brook I. The impact of smoking on oral and nasopharyngeal bacterial flora. J Dent Res. 2011;90(06):704–710. doi: 10.1177/0022034510391794. [DOI] [PubMed] [Google Scholar]
- 5.Michaud D S, Izard J, Rubin Z et al. Lifestyle, dietary factors, and antibody levels to oral bacteria in cancer-free participants of a European cohort study. Cancer Causes Control. 2013;24(11):1901–1909. doi: 10.1007/s10552-013-0265-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Rad M, Kakoie S, Niliye Brojeni F, Pourdamghan N. Effect of Long-term Smoking on Whole-mouth Salivary Flow Rate and Oral Health. J Dent Res Dent Clin Dent Prospect. 2010;4(04):110–114. doi: 10.5681/joddd.2010.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Marom T, Cinamon U, Itskoviz D, Roth Y. Changing trends of peritonsillar abscess. Am J Otolaryngol. 2010;31(03):162–167. doi: 10.1016/j.amjoto.2008.12.003. [DOI] [PubMed] [Google Scholar]
- 8.Hidaka H, Kuriyama S, Yano H, Tsuji I, Kobayashi T. Precipitating factors in the pathogenesis of peritonsillar abscess and bacteriological significance of the Streptococcus milleri group. Eur J Clin Microbiol Infect Dis. 2011;30(04):527–532. doi: 10.1007/s10096-010-1114-9. [DOI] [PubMed] [Google Scholar]
- 9.Klug T E, Rusan M, Clemmensen K K, Fuursted K, Ovesen T. Smoking promotes peritonsillar abscess. Eur Arch Otorhinolaryngol. 2013;270(12):3163–3167. doi: 10.1007/s00405-013-2474-4. [DOI] [PubMed] [Google Scholar]
- 10.Tolska H K, Takala A, Pitkäniemi J, Jero J. Post-tonsillectomy haemorrhage more common than previously described--an institutional chart review. Acta Otolaryngol. 2013;133(02):181–186. doi: 10.3109/00016489.2012.723825. [DOI] [PubMed] [Google Scholar]
- 11.Bhattacharyya N, Kepnes L J. Revisits and postoperative hemorrhage after adult tonsillectomy. Laryngoscope. 2014;124(07):1554–1556. doi: 10.1002/lary.24541. [DOI] [PubMed] [Google Scholar]
- 12.Lopatin A S, Chuchueva N D. [Hemorrhage following tonsillectomy: analysis of the prevalence and risk factors] Vestn Otorinolaringol. 2013;(03):71–75. [PubMed] [Google Scholar]
- 13.Akin R C, Holst R, Schousboe L P. Risk factors for post-tonsillectomy haemorrhage. Acta Otolaryngol. 2012;132(07):773–777. doi: 10.3109/00016489.2012.660545. [DOI] [PubMed] [Google Scholar]
- 14.Mösges R, Hellmich M, Allekotte S, Albrecht K, Böhm M. Hemorrhage rate after coblation tonsillectomy: a meta-analysis of published trials. Eur Arch Otorhinolaryngol. 2011;268(06):807–816. doi: 10.1007/s00405-011-1535-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Sarny S, Ossimitz G, Habermann W, Stammberger H. Hemorrhage following tonsil surgery: a multicenter prospective study. Laryngoscope. 2011;121(12):2553–2560. doi: 10.1002/lary.22347. [DOI] [PubMed] [Google Scholar]
- 16.Eski E, Dogan I, Yilmaz I. Seasonal variation of secondary post tonsillectomy hemorrhage rates. B-ENT. 2011;7(03):165–168. [PubMed] [Google Scholar]
- 17.Hessén Söderman A C, Ericsson E, Hemlin C et al. Reduced risk of primary postoperative hemorrhage after tonsil surgery in Sweden: results from the National Tonsil Surgery Register in Sweden covering more than 10 years and 54,696 operations. Laryngoscope. 2011;121(11):2322–2326. doi: 10.1002/lary.22179. [DOI] [PubMed] [Google Scholar]
- 18.Leonard D S, Fenton J E, Hone S. ABO blood type as a risk factor for secondary post-tonsillectomy haemorrhage. Int J Pediatr Otorhinolaryngol. 2010;74(07):729–732. doi: 10.1016/j.ijporl.2010.03.003. [DOI] [PubMed] [Google Scholar]
- 19.Tomkinson A, De Martin S, Gilchrist C R, Temple M. Instrumentation and patient characteristics that influence postoperative haemorrhage rates following tonsil and adenoid surgery. Clin Otolaryngol. 2005;30(04):338–346. doi: 10.1111/j.1365-2273.2005.01045.x. [DOI] [PubMed] [Google Scholar]
- 20.Morton R P, Mak V, Moss D, Ahmad Z, Sevao J. Risk of bleeding after thyroid surgery: matched pairs analysis. J Laryngol Otol. 2012;126(03):285–288. doi: 10.1017/S0022215111001460. [DOI] [PubMed] [Google Scholar]
- 21.Richstone L, Montag S, Ost M C et al. Predictors of hemorrhage after laparoscopic partial nephrectomy. Urology. 2011;77(01):88–91. doi: 10.1016/j.urology.2008.05.022. [DOI] [PubMed] [Google Scholar]
- 22.Mjøen G, Øyen O, Holdaas H, Midtvedt K, Line P D. Morbidity and mortality in 1022 consecutive living donor nephrectomies: benefits of a living donor registry. Transplantation. 2009;88(11):1273–1279. doi: 10.1097/TP.0b013e3181bb44fd. [DOI] [PubMed] [Google Scholar]
- 23.de la Fuente S G, Khuri S F, Schifftner T, Henderson W G, Mantyh C R, Pappas T N. Comparative analysis of vagotomy and drainage versus vagotomy and resection procedures for bleeding peptic ulcer disease: results of 907 patients from the Department of Veterans Affairs National Surgical Quality Improvement Program database. J Am Coll Surg. 2006;202(01):78–86. doi: 10.1016/j.jamcollsurg.2005.09.001. [DOI] [PubMed] [Google Scholar]
- 24.Erickson B K, Larson D R, St Sauver J L, Meverden R A, Orvidas L J. Changes in incidence and indications of tonsillectomy and adenotonsillectomy, 1970-2005. Otolaryngol Head Neck Surg. 2009;140(06):894–901. doi: 10.1016/j.otohns.2009.01.044. [DOI] [PubMed] [Google Scholar]
- 25.Hoddeson E K, Gourin C G. Adult tonsillectomy: current indications and outcomes. Otolaryngol Head Neck Surg. 2009;140(01):19–22. doi: 10.1016/j.otohns.2008.09.023. [DOI] [PubMed] [Google Scholar]
- 26.The Israeli Ministry of health. The minister of health report of smoking is Israel, 2003 Available at: http://www.health.gov.il/PublicationsFiles/smoke2003_2002.pdf" [Hebrew]. Accessed Dec 7, 2015.
- 27.The Israeli Ministry of health. The minister of health report of smoking in Israel, 2010 Available at: http://www.old.health.gov.il/download/pages/smoke10_290511.pdf. [Heberew]. Accessed Dec 7, 2015.
- 28.Demars S M, Harsha W J, Crawford J V. The effects of smoking on the rate of postoperative hemorrhage after tonsillectomy and uvulopalatopharyngoplasty. Arch Otolaryngol Head Neck Surg. 2008;134(08):811–814. doi: 10.1001/archotol.134.8.811. [DOI] [PubMed] [Google Scholar]
- 29.Washington Tobacco facts 2013.Tobacco Prevention & Control Program Washington state department of health DOH 340–149. January 2014. Available at: http://www.doh.wa.gov/Portals/1/Documents/Pubs/340-149-washingtontobaccofacts.pdf
- 30.Kramarow E A, Pastor P N. The health of male veterans and nonveterans aged 25-64: United States, 2007-2010. NCHS Data Brief. 2012;(101):1–8. [PubMed] [Google Scholar]
- 31.Nelson J P, Pederson L L. Military tobacco use: a synthesis of the literature on prevalence, factors related to use, and cessation interventions. Nicotine Tob Res. 2008;10(05):775–790. doi: 10.1080/14622200802027123. [DOI] [PubMed] [Google Scholar]
- 32.Ashcroft D W.Haemorrhage following Tonsillectomy BMJ 19382(4064):1079–1082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Kontorinis G, Schwab B. Significance of advanced haemostasis investigation in recurrent, severe post-tonsillectomy bleeding. J Laryngol Otol. 2011;125(09):952–957. doi: 10.1017/S0022215111000879. [DOI] [PubMed] [Google Scholar]
- 34.Schrock A, Send T, Heukamp L, Gerstner A O, Bootz F, Jakob M. The role of histology and other risk factors for post-tonsillectomy haemorrhage. Eur Arch Otorhinolaryngol. 2009;266(12):1983–1987. doi: 10.1007/s00405-009-0958-z. [DOI] [PubMed] [Google Scholar]
- 35.Sørensen L T. Wound healing and infection in surgery: the pathophysiological impact of smoking, smoking cessation, and nicotine replacement therapy: a systematic review. Ann Surg. 2012;255(06):1069–1079. doi: 10.1097/SLA.0b013e31824f632d. [DOI] [PubMed] [Google Scholar]
- 36.Larose T L, Chen Y, Camargo C A, Jr, Langhammer A, Romundstad P, Mai X M. Factors associated with vitamin D deficiency in a Norwegian population: the HUNT Study. J Epidemiol Community Health. 2014;68(02):165–170. doi: 10.1136/jech-2013-202587. [DOI] [PubMed] [Google Scholar]
- 37.Baeke F, Takiishi T, Korf H, Gysemans C, Mathieu C. Vitamin D: modulator of the immune system. Curr Opin Pharmacol. 2010;10(04):482–496. doi: 10.1016/j.coph.2010.04.001. [DOI] [PubMed] [Google Scholar]
- 38.Nseir W, Mograbi J, Abu-Rahmeh Z, Mahamid M, Abu-Elheja O, Shalata A. The association between vitamin D levels and recurrent group A streptococcal tonsillopharyngitis in adults. Int J Infect Dis. 2012;16(10):e735–e738. doi: 10.1016/j.ijid.2012.05.1036. [DOI] [PubMed] [Google Scholar]
- 39.Gill J F, Yu S S, Neuhaus I M. Tobacco smoking and dermatologic surgery. J Am Acad Dermatol. 2013;68(01):167–172. doi: 10.1016/j.jaad.2012.08.039. [DOI] [PubMed] [Google Scholar]
- 40.Deliaert A E, Van den Kerckhove E, Tuinder S, Noordzij S M, Dormaar T S, van der Hulst R R. Smoking and its effect on scar healing. Eur J Plast Surg. 2012;35(06):421–424. doi: 10.1007/s00238-011-0661-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.McRobert J.Smoking and its effects on the healing process of chronic wounds Br J Community Nurs 2013; Suppl: S18, S20–23. [DOI] [PubMed] [Google Scholar]
- 42.Warner M A, Offord K P, Warner M E, Lennon R L, Conover M A, Jansson-Schumacher U. Role of preoperative cessation of smoking and other factors in postoperative pulmonary complications: a blinded prospective study of coronary artery bypass patients. Mayo Clin Proc. 1989;64(06):609–616. doi: 10.1016/s0025-6196(12)65337-3. [DOI] [PubMed] [Google Scholar]
- 43.Cavichio B V, Pompeo D A, Oller G A, Rossi L A. [Duration of smoking cessation for the prevention of surgical wound healing complications] Rev Esc Enferm USP. 2014;48(01):174–180. doi: 10.1590/s0080-623420140000100022. [DOI] [PubMed] [Google Scholar]
- 44.Rinker B. The evils of nicotine: an evidence-based guide to smoking and plastic surgery. Ann Plast Surg. 2013;70(05):599–605. doi: 10.1097/SAP.0b013e3182764fcd. [DOI] [PubMed] [Google Scholar]
- 45.Rodrigo C. The effects of cigarette smoking on anesthesia. Anesth Prog. 2000;47(04):143–150. [PMC free article] [PubMed] [Google Scholar]
- 46.Nicod P, Rehr R, Winniford M D, Campbell W B, Firth B G, Hillis L D. Acute systemic and coronary hemodynamic and serologic responses to cigarette smoking in long-term smokers with atherosclerotic coronary artery disease. J Am Coll Cardiol. 1984;4(05):964–971. doi: 10.1016/s0735-1097(84)80058-3. [DOI] [PubMed] [Google Scholar]
- 47.Lee S M, Landry J, Jones P M, Buhrmann O, Morley-Forster P. The effectiveness of a perioperative smoking cessation program: a randomized clinical trial. Anesth Analg. 2013;117(03):605–613. doi: 10.1213/ANE.0b013e318298a6b0. [DOI] [PubMed] [Google Scholar]
- 48.Wong J, Lam D P, Abrishami A, Chan M T, Chung F. Short-term preoperative smoking cessation and postoperative complications: a systematic review and meta-analysis. Can J Anaesth. 2012;59(03):268–279. doi: 10.1007/s12630-011-9652-x. [DOI] [PubMed] [Google Scholar]


