Abstract
Implant-Insertion-Torque-Value (ITV) proved to be a significant clinical parameter to predict long term implant success-rates and to decide upon immediate loading. The study evaluated ITVs, when four different and commonly used biomaterials were used in sinuslift-procedures compared to natural subantral bone in two-stage-implant-procedures. The tHUCSL-INTRALIFT-method was chosen for sinuslifting in 155 sinuslift-sites for its minimal invasive transcrestal approach and scalable augmentation volume. Four different biomaterials were inserted randomly (easy-graft CRYSTAL n = 38, easy-graft CLASSIC n = 41, NanoBone n = 42, BioOss n = 34), 2 ccm in each case. After a mean healing period of 8,92 months uniform tapered screw Q2-implants were inserted and Drill-Torque-Values (DTV) and ITV were recorded and compared to a group of 36 subantral sites without need of sinuslifting. DTV/ITV were processed for statistics by ANOVA-tests. Mean DTV/ITV obtained in Ncm were: Control Group 10,2/22,2, Bio-Oss 12,7/26,2, NanoBone 17,5/33,3, easy-graft CLASSIC 20,3/45,9, easy-graft CRYSTAL 23,8/56,6 Ncm, significance-level of differences throughout p < 0,05. Within the limits of this study the results suggest self-hardening solid-block-like bone-graft-materials to achieve significantly better DTV/ITV than loose granulate biomaterials for its suspected improvement of vascularization and mineralization of the subantral scaffold by full immobilization of the augmentation site towards pressure changes in the human sinus at normal breathing.
1995 Friberg B. et al.1 proved a statistically significant correlation between the cutting resistance of implant drills and the bone quality of the mandible and maxilla in a human cadaver study.
Furthermore, implant-drill torque and implant-insertion torque seem to be a core-indicator for primary implant stability and superior long-term implant survival rates as suggested 2007 by Alsaadi G. et al.2 and Turkyilmaz I. et al.3,4,5,6 as results of clinical studies. In 2009 Turkyilmaz I. et al.7 proved a significant correlation between radiographic bone densities, implant insertion torque and implant stability quotient (ISQ) -values for maxillary bone in a human cadaver study.
Trisi P. et al.8 investigated micromovements of endosseus dental implants inserted into bovine cadaver bone of different densities at different insertion torque rates and was able to prove “a high dependence between the micromotion and the peak insertion torque indicating that micromotion decreases with increasing peak insertion torque”. Since micromotion of freshly inserted dental implants - especially in the early healing phase of osseointegration - is considered as main cause for dental implant failure on immediate loading especially in the maxilla (Szmukler-Moncler S. et al.9), Cannizzaro G. et al.10 suggested an insertion torque of 45 Ncm or more for immediate loading of dental implants inserted into maxillary bone. Esposito M. et al.11 backed these experimental and clinical results in a Cochrane systematic review as well as later Chung S. et al.12 in a literature review referring to immediate loading in the maxilla.
Rabel A. et al.13 stated resonance frequency values not to appear suitable for the evaluation of implant stability as a single method but higher insertion torque to confirm higher primary stability.
Walker L. R. et al.14 recently suggested the insertions torque values achieved at dental implant insertion to be significant for the prediction of implant success for the clinician in the everyday implantology routine. Pommer B. et al.15 revealed a highly significant correlation between insertion-torque-values (ITV), periotest-values (PTV), resonance frequency analysis (RFA) and radiographic bone density (RBD) in maxillary sinus augmentation with simultaneous implant insertion in a human cadaver study.
Degidi M. et al.16 proved in a clinical study with 4.135 inserted implants the ITV (insertion-torque-value) to be a reliable intrasurgical clinical indicator directly influenced by bone density.
Only few articles were published regarding investigations on resonance frequency analysis of implants inserted into sinus-augmentation sites (Degidi M. et al.17,18, Di Lallo S. et al.19, Jensen S.S. et al.20), none were found investigating comparative ITVs in sinus augmentation sites with different biomaterials when implants were inserted at a second stage surgery after completed bone reformation in the augmented site.
Iezzi G. et al.21 2013 introduced a computerized implant motor recording ITVs at implant insertion and experimentally found a close correlation between the ITVs recorded by this device and the later histomorphometric analysis pf bone density.
Aim of the present controlled randomized clinical study was the evaluation of the drill-torque-values (DTV) and implant-insertion-torque-values (ITV) in augmented sinus sites in two-stage dental-implant-insertion-procedures with four different bone graft materials compared to non-augmented natural subantral alveolar crest sites to determine the physical properties of sinus-augmentation-sites for its possible clinical value as intrasurgical “decision-making-tool” intrasurgically.
Methods
Between January 2011 and December 2012 a number of 109 regular patients aged between 43 yrs and 64 yrs – applying for the tHUCSL-procedure, presenting 157 potential sinus-lift sites and being generally eligible for sinuslift surgery - were chosen. The only restriction for possible election for the study was a remnant subantral crest height of only 1–4 mm and a crest width of minimum 5 mm measured in CT-scans which – for overall treatment safety – suggests an implant insertion in a second surgery favourable.
Reporting the planned study to the Ethical Committee of the Medical University of Vienna the authors were informed by the Chairman, that – according to the EMEA-guidelines – no approval was necessary, since both the sinuslift-method and biomaterials are CE-certified, long established and in common use, and randomization of applied biomaterial in every case would not cause any disadvantage to the patients, who – as a general legal rule in Austria and Germany – have to sign their legal informed consent for both the surgical method and biomaterial used, and measurement of torque-values at implant-insertion are generally considered “good practice” in surgical documentation in dental implantology. Surgical protocols and surgery-documentation were not specially altered for the presented study compared to routine patient treatment in the authors' clinics.
All sinuslifts were performed with the transcrestal hydrodynamic ultrasonic cavitational sinuslift22 (tHUCSL-INTRALIFT)-method. All patients provided an approval by an ENT-specialist for sinuslift-surgery. The tHUCSL-INTRALIFT was chosen to provide the least invasive sinuslift-procedure with a possible augmentation volume comparable to lateral approach sinus-lift techniques and the least risk of sinus-membrane perforation23. Using tHUCSL-INTRALIFT, unbiased results and almost negligible iatrogenic failure-interference with natural subantral bone regeneration24 can be achieved by reproducible clean and undissected separation of the osteogenic layer of the sinus-membrane from the antrum-floor25.
155 sinus sites were augmented in these patients. All patients were antimicrobial shielded with either Amoxicillin/Clavulan Acid 1 g 2x/day or Clindamycin 300 mg 3x/day for 5 days, starting one day before surgery.
Four chemically and physically different CE-marked and widely used biomaterials were chosen for sinusfloor-augmentation:
easy-graft CRYSTAL, granule size 0,45–1 mm (SUNSTAR Degradable Solutions AG/Zurich/CH): microporous compound particles of 40% beta-tricalciumphosphate (beta-TCP) and 60% hydroxyapatite (HA), each particle covered by a 10 micrometer layer of polylactic-co-glycolic acid (PLGA). The primary loose particles are mixed with Biolinker (N-methyl-2-pyrrolidone solution) and once the Biolinker is washed out by the natural blood flow the biomaterial hardens to a solid bone-substitute block.
easy-graft CLASSIC, granule size 0,5–1 mm (SUNSTAR Degradable Solutions AG/Zurich/CH): equal to easy-graft CRYSTAL, only difference: particles are chemically pure beta-TCP.
NanoBone granule size 0,6–2 mm (ArtOss GmbH/Rostock/GER): nanocrystal HA embedded in a SiO2-matrix
Bio-Oss granule size 0,25–1 mm (Geistlich Pharma AG/Wolhusen/CH): bovine xenograft
For each tHUCSL-INTRALIFT-site, one of the four biomaterials were assigned randomly in the Excel-Data-sheet (Excel Random Generator formula “ = RUNDEN(ZUFALLSZAHL()*3;0)+1”) resulting in four test-groups: Bio-Oss (n = 34), NanoBone (n = 42), easy-graft CLASSIC (n = 41), easy-graft CRYSTAL (n = 38). All patients had to sign their consent for the use of the specific CE-marked biomaterial after random allocation by the IT-based random-allocator.
Each tHUCSL-INTRALIFT-surgery was strictly accessed via a 6 × 6 to 8 × 8 mm topcrestal full-thickness mucoperiostal flap at the very bottom of the antrum (mostly in the first molar region, Fig. 1A). The bony sinus-floor then was opened with the diamond-coated ultrasonic tip “TKW 2” Ø 2,2 mm (Fig. 1B) and a receptacle prepared with the diamond coated tip “TKW 4” Ø 2,8 mm (Fig. 1C). The Schneiderian membrane was detached with the ultrasonic tip “TKW 5” Ø 3,0 mm (Fig. 1D), strictly following the surgical protocol at a saline flow-rate of 30 ml/min for 5 seconds, and each site was augmented with 2 ccm of the randomly assigned biomaterial (Fig. 1E). The subantral trepanation then was marked with medical ink (Codman-pen) for later exact localization (Fig. 1E, Fig. 2A), the crestal flap repositioned and sutured (Fig. 2B).
Figure 1.
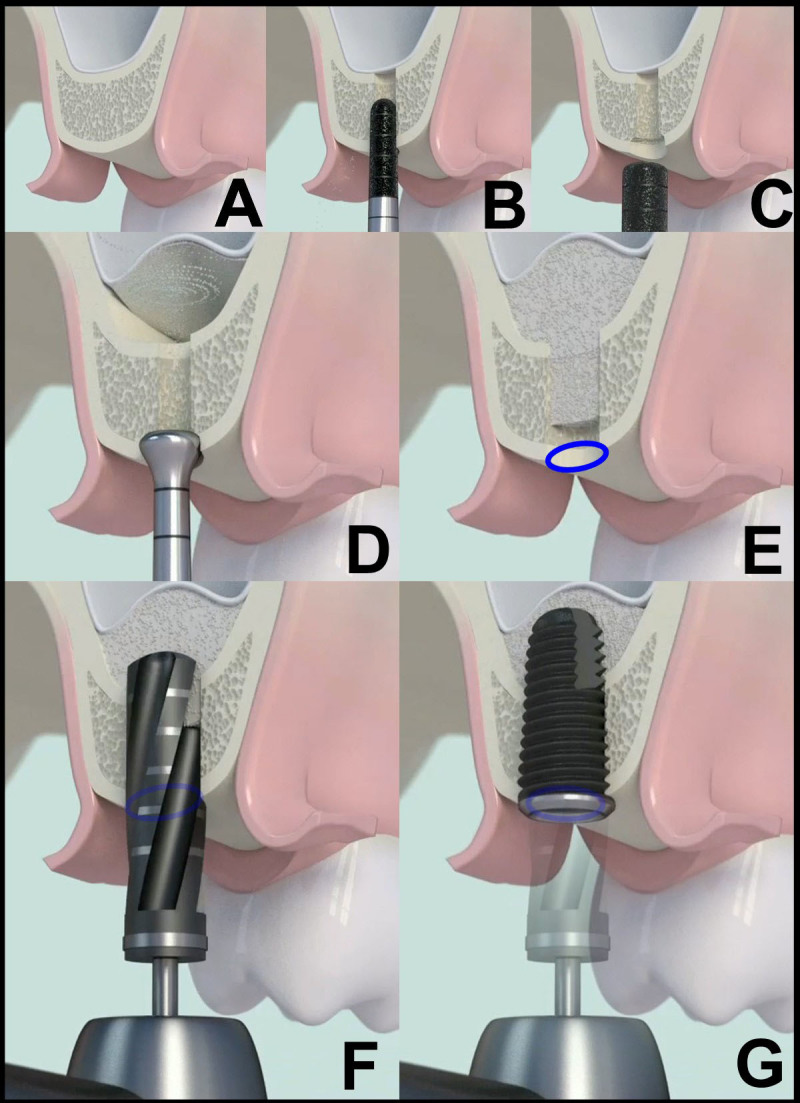
tHUCSL-INTRALIFT surgical protocol for Piezotome II/SOLO/Implant Center II: minimal invasive crestal flap (A), opening of the bony antral floor with the diamond coated ultrasonic tip “TKW 2” (B), preparation of the receptacle with the diamond coated ultrasonic tip “TKW 4” (C), tight-fit insertion of the ultrasonic detachment tip “TKW 5” and hydrodynamic ultrasonic detachment of the sinus-membrane utilizing the ultrasonic cavitation effect (D), subantral application of 2 ccm biomaterial and marking the osteotomy-site with medical ink (E), Drill-Torque-measurement after mean healing period of 8,92 months at original osteotomy-site marked with medical ink (F), Implant-Insertion-Torque-measurement (G).
Figure 2. Clinical depiction of a typical transcrestal osteotomy.
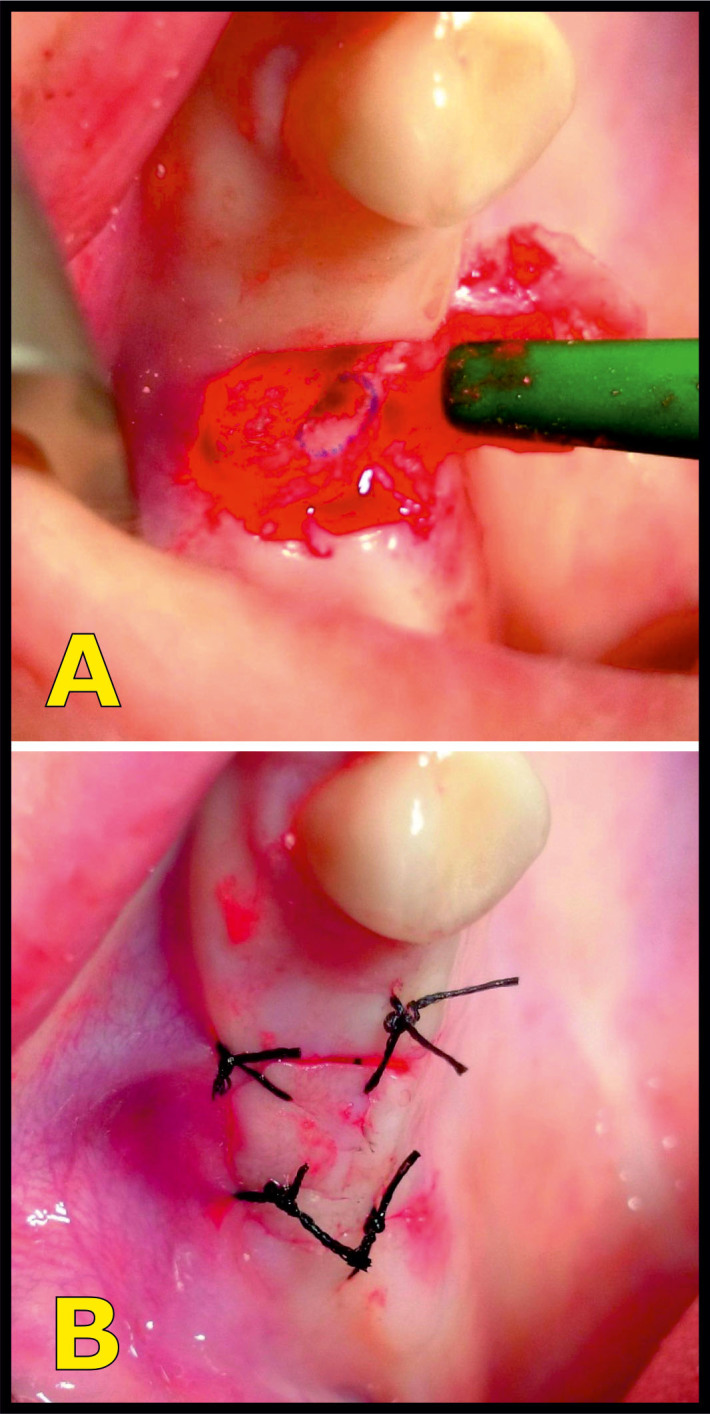
Site is marked with a medical marker after subantral augmentation with biomaterial for precise location of later ITV/DTV-measurements (A) and after wound-closure (B).
Implant insertion was performed after a healing period of mean 8,92 months (min: 8,7, max: 9,5) after tHUCSL-INTRALIFT-surgery according to the results presented by the authors24, suggesting the subantral bone regeneration can be considered as to be fully completed at that time.
Torque-measurements of DTV and ITV were taken with Implant Center II (Satelec-ACTEON/FR), allowing a torque-increase in steps of 1 Ncm up to 100 Ncm.
As reference-implant the Q2-implant (self-taper, root analogue screw-design; TRINON-Karlsruhe GmbH/GER) was chosen exclusively with a diameter of 4 mm and of 12 mm length only. The implants were inserted by a different surgeon than the surgeon performing the tHUCSL-INTRALIFT and augmentation procedure, therefore the surgeon was unaware of the biomaterial applied to the sinuslift-site and unbiased results were achieved.
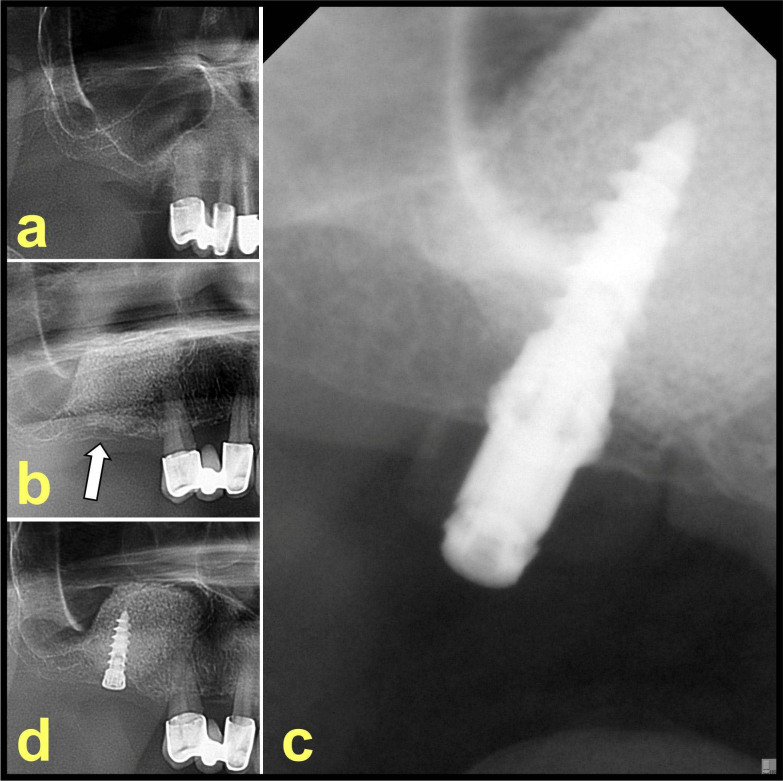
Final form-drilling was performed according to the Q2-systems precise drilling protocol at 50 rpm (Fig. 1F) with an unused form drill for each treated site and implants were inserted exactly into the former tHUCSL-trepanation marked with medical ink at 2 rpm (Fig. 1G) to obtain unbiased results for each biomaterial and least influence by the remaining subantral natural bone. Drilling and implant insertion were started with a basic torque-setting of 5 Ncm increased in 1 Ncm-steps by an assistant until the form-drill reached the 12 mm-mark and the 12 mm-length Q2-implant was inserted at bone-level. Fig. 3 shows a typical case in radiographic follow-up with their state before tHUCSL-INTRALIFT (Fig. 3a), post-surgical state (Fig. 3b) and after implant insertion after the mean healing period of 8,92 months (Fig. 3c and d).
Figure 3. Typical clinical case.
a) presurgical x-ray, b) post-surgical x-ray after tHUCSL-INTRALIFT, the transcrestal osteotomy site is marked with a white arrow, c) intrasurgical x-ray with implant in site after ITV/DTV determination, d) post-surgical x-ray after implant insertion.
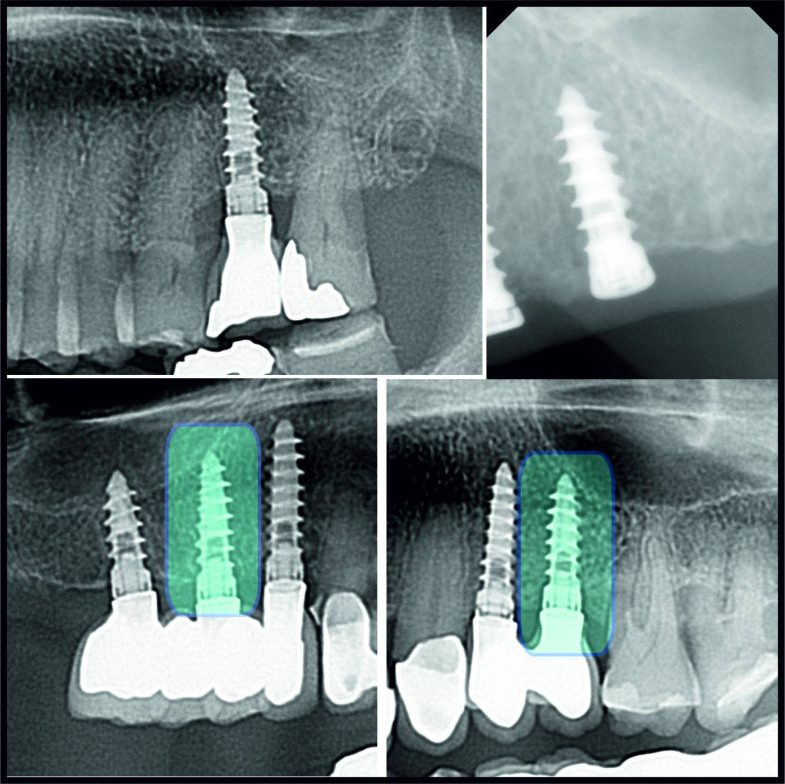
As a control group 36 consecutive patients - eligible for implant insertion within the study period - were selected, presenting a subantral alveolar crest height of minimum 12 mm and maxillary premolar and/or molar tooth loss of more than 2 years prior to implant insertion to guarantee unbiased results in native subantral bone (Fig 4).
Figure 4. Various cases of the control group with implants inserted in natural subantral bone.
Implants used for determination of DTV/ITV are marked with bluish rectangles.
Statistical analysis was performed with a one-way ANOVA and post-hoc multiple comparisons by Fisher's Least Significant Difference (LSD) to test mean DT- and IT-values and variance in each group, and mean difference significance between all groups. Additionally, the data were depicted in notched box plots to show the data distribution and interquartile ranges (IQR) between the 25th and 75th percentile of the specific biomaterial tested.
Results
From 109 patients two patients with two possible subantral augmentation sites had to be excluded from subantral augmentation due to visible perforations of the sinus-membrane after preparation of the transcrestal approach. 107 patients were included in the study with 155 subantral augmentation sites, showing no visible or clinical signs of sinus-membrane-perforations after transcrestal osteotomy and tHUCSL-INTRALIFT.
All 155 sinus-sites treated with the tHUCSL-INTRALIFT progressed clinically and radiologically uneventful. No puncture or rupture of the sinus-membrane could be observed intrasurgically or post-surgically as report of nose bleeding or loss of biomaterial by the 107 patients, leading to no exclusion of sinuslift-sites from later determination of DTV and ITV at implant insertion.
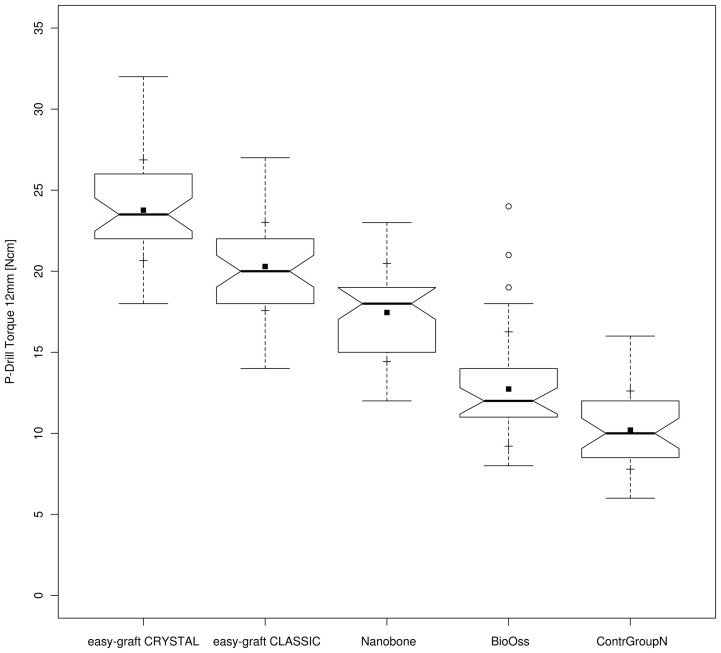
Drill-torque measurements at implant insertion surgery revealed a mean DTV (Drill Torque Value) of 10,2 Ncm [standard deviation (SD) 2,4] in the control group of patients when implants were inserted into natural subantral bone, constantly increasing in the group treated with Bio-Oss (mean value: 12,7 Ncm [SD 3,5]), NanoBone (mean value: 17,5 Ncm [SD 3,0]), easy-graft CLASSIC (mean value: 20,3 Ncm [SD 2,7]) and easy-graft CRYSTAL (mean value: 23,8 Ncm [SD 3,1]). (Fig. 5)
Figure 5. Drill-Torque notched box plot: depicts the interquartile range (IQR) between the 25th and 75th percentile of the specific biomaterial tested where 50% of the data points were located.
Additionally, the upper whiskers represent data within the 75th percentile +1.5 times the IQR. The lower whisker delimits data of the 25th percentile – 1.5 times the IQR. Circles [ ] represent the outliers. Within the boxes the notches mark the confidence interval based on the median +/− 1.58 (IQR/sqrt of n) [n = number of measurements]. Additionally, the mean value is indicated by a black square [
] represent the outliers. Within the boxes the notches mark the confidence interval based on the median +/− 1.58 (IQR/sqrt of n) [n = number of measurements]. Additionally, the mean value is indicated by a black square [ ] and the cross symbol [+] displays the standard deviation. Bio-Oss (n = 34), NanoBone (n = 42), easy-graft CLASSIC (n = 41), easy-graft CRYSTAL (n = 38), Control Group (n = 36).
] and the cross symbol [+] displays the standard deviation. Bio-Oss (n = 34), NanoBone (n = 42), easy-graft CLASSIC (n = 41), easy-graft CRYSTAL (n = 38), Control Group (n = 36).
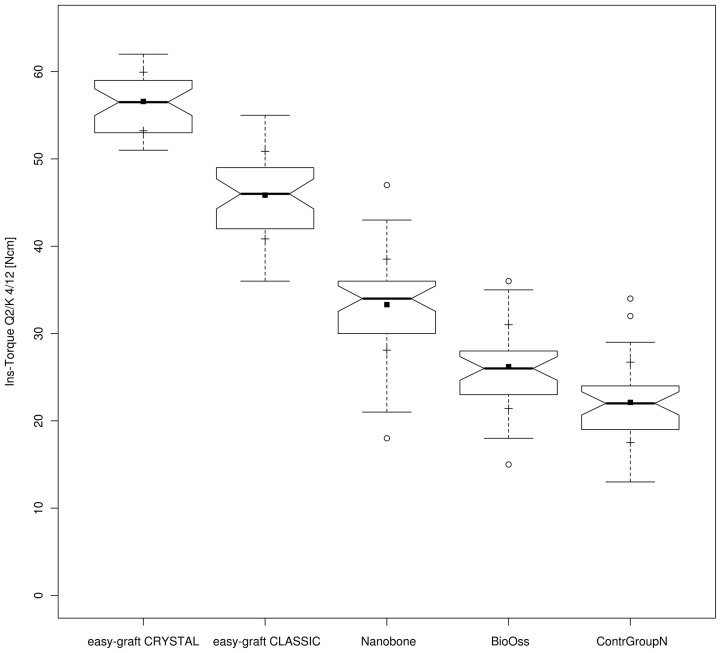
Implant-insertion torque values (ITV) showed a similar behaviour with a mean ITV of 22,2 Ncm (SD 4,6) in the control group of patients when implants were inserted into natural subantral bone, constantly increasing in the group treated with Bio-Oss (mean value: 26,2 Ncm [SD 4,8]), NanoBone (mean value: 33,3 Ncm [SD 5,2]), easy-graft CLASSIC (mean value: 45,9 Ncm [SD 5,0]) and easy-graft CRYSTAL (mean value: 56,6 Ncm [SD 3.4]). (Fig. 6)
Figure 6. Implant-Insertion-Torque notched box plot: depicts the interquartile range (IQR) between the 25th and 75th percentile of the specific biomaterial tested where 50% of the data points were located.
Additionally, the upper whiskers represent data within the 75th percentile +1.5 times the IQR. The lower whisker delimits data of the 25th percentile – 1.5 times the IQR. Circles [ ] represent the outliers. Within the boxes the notches mark the confidence interval based on the median +/− 1.58 (IQR/sqrt of n) [n = number of measurements]. Additionally, the mean value is indicated by a black square [
] represent the outliers. Within the boxes the notches mark the confidence interval based on the median +/− 1.58 (IQR/sqrt of n) [n = number of measurements]. Additionally, the mean value is indicated by a black square [ ] and the cross symbol [+] displays the standard deviation. Bio-Oss (n = 34), NanoBone (n = 42), easy-graft CLASSIC (n = 41), easy-graft CRYSTAL (n = 38), Control Group (n = 36).
] and the cross symbol [+] displays the standard deviation. Bio-Oss (n = 34), NanoBone (n = 42), easy-graft CLASSIC (n = 41), easy-graft CRYSTAL (n = 38), Control Group (n = 36).
One-way ANOVA- and Post Hoc Tests returned sig. values of 0,000 (p < 0,05), indicating a significant difference at 95% level between all tested groups within the data set for both, DTVs (Table 1 & 2) and ITVs (Table 3 & 4) with easy-graft CRYSTAL achieving a significant higher DTV/ITV than easy-graft CLASSIC, followed by Nanobone and Bio-Oss with natural subantral bone providing the least DTV/ITV with rare outliers in the Bio-Oss-group for DTVs and more outliers in the Control-, Bio-Oss- and Nanobone-group for ITVs depicted in the box plots (Fig. 5 and 6).
Table 1. Drill-Torque-Value (DTV) Comparison ANOVA-Test: Statistical analysis of Drill-Torque-Values (DTV) by one-way ANOVA at 95% level of significance for the parameters evaluated.
| DRILL Torque Values (DTV) | Sum of Squares | df | Mean Square | F | Sig. |
|---|---|---|---|---|---|
| Between Groups | 4423,895 | 4 | 1105,974 | 124,913 | ,000 |
| Within Groups | 1637,979 | 185 | 8,854 | ||
| Total | 6061,874 | 189 |
Table 2. DTV-Post Hoc Test (Multiple comparisons with dependent variable: DRILL Torque Values (DTV) calculating Least Signficance Difference (LSD)): Post-hoc multiple comparisons by Fisher’s Least Significant Difference test to discern whether the differences between the means of the different biomaterials were statistically significant. Values with p <0.05 were considered statistically significant.
| Biomaterial compared to | Biomaterial | Mean Difference | Std. Error | Sig. |
|---|---|---|---|---|
| easy-graft CRYSTAL | easy-graft CLASSIC | 3,470* | ,670 | ,000 |
| NanoBone | 6,311* | ,666 | ,000 | |
| Bio-Oss | 11,028* | ,702 | ,000 | |
| ContrGroupNormBone | 13,563* | ,697 | ,000 | |
| easy-graft CLASSIC | easy-graft CRYSTAL | −3,470* | ,670 | ,000 |
| NanoBone | 2,840* | ,653 | ,000 | |
| Bio-Oss | 7,557* | ,690 | ,000 | |
| ContrGroupNormBone | 10,093* | ,685 | ,000 | |
| NanoBone | easy-graft CRYSTAL | −6,311* | ,666 | ,000 |
| easy-graft CLASSIC | −2,840* | ,653 | ,000 | |
| Bio-Oss | 4,717* | ,686 | ,000 | |
| ContrGroupNormBone | 7,252* | ,681 | ,000 | |
| Bio-Oss | easy-graft CRYSTAL | −11,028* | ,702 | ,000 |
| easy-graft CLASSIC | −7,557* | ,690 | ,000 | |
| NanoBone | −4,717* | ,686 | ,000 | |
| ContrGroupNormBone | 2,535* | ,717 | ,001 | |
| ContrGroupNormBone | easy-graft CRYSTAL | −13,563* | ,697 | ,000 |
| easy-graft CLASSIC | −10,093* | ,685 | ,000 | |
| NanoBone | −7,252* | ,681 | ,000 | |
| Bio-Oss | −2,535* | ,717 | ,001 |
*. The mean difference is significant at the 0.05 level
Table 3. Insertion-Torque-Value (ITV) Comparison ANOVA-Test: Statistical analysis of Insertion-Torque-Values (ITV) by one-way ANOVA at 95% level of significance for the parameters evaluated.
| INSERTION Torque Values (ITV) | Sum of Squares | df | Mean Square | F | Sig. |
|---|---|---|---|---|---|
| Between Groups | 30047,979 | 4 | 7511,995 | 345,661 | ,000 |
| Within Groups | 4020,463 | 185 | 21,732 | ||
| Total | 34068,442 | 189 |
Table 4. ITV-Post Hoc Test (Multiple comparisons with dependent variable: INSERTION Torque Values (ITV) calculating Least Signficance Difference (LSD)): Post-hoc multiple comparisons by Fisher’s Least Significant Difference test to discern whether the differences between the means of the different biomaterials were statistically significant. Values with p <0.05 were considered statistically significant.
| Biomaterial compared to | Biomaterial | Mean Difference | Std. Error | Sig. |
|---|---|---|---|---|
| easy-graft CRYSTAL | easy-graft CLASSIC | 10,725* | 1,050 | ,000 |
| NanoBone | 23,269* | 1,044 | ,000 | |
| Bio-Oss | 30,373* | 1,100 | ,000 | |
| ContrGroupNormBone | 34,465* | 1,092 | ,000 | |
| easy-graft CLASSIC | easy-graft CRYSTAL | −10,725* | 1,050 | ,000 |
| NanoBone | 12,544* | 1,023 | ,000 | |
| Bio-Oss | 19,648* | 1,081 | ,000 | |
| ContrGroupNormBone | 23,739* | 1,073 | ,000 | |
| NanoBone | easy-graft CRYSTAL | −23,269* | 1,044 | ,000 |
| easy-graft CLASSIC | −12,544* | 1,023 | ,000 | |
| Bio-Oss | 7,104* | 1,075 | ,000 | |
| ContrGroupNormBone | 11,195* | 1,067 | ,000 | |
| Bio-Oss | easy-graft CRYSTAL | −30,373* | 1,100 | ,000 |
| easy-graft CLASSIC | −19,648* | 1,081 | ,000 | |
| NanoBone | −7,104* | 1,075 | ,000 | |
| ContrGroupNormBone | 4,092* | 1,123 | ,000 | |
| ContrGroupNormBone | easy-graft CRYSTAL | −34,465* | 1,092 | ,000 |
| easy-graft CLASSIC | −23,739* | 1,073 | ,000 | |
| NanoBone | −11,195* | 1,067 | ,000 | |
| Bio-Oss | −4,092* | 1,123 | ,000 |
*. The mean difference is significant at the 0.05 level.
Discussion
Although Drill-Torque-Values (DTV) already show significant differences starting with natural subantral bone, constantly increasing in the Bio-Oss-, NanoBone- and easy-graft CLASSIC – group, hitting the highest value in the easy-graft CRYSTAL – group, the value as diagnostic and/or predictive tool in practical surgery is questionable, taking into consideration that most implant-motors provide torque adjustments only in 3–5 Ncm-steps. This might be reconsidered once implant-motors as described by Iezzi G. et al.21 are generally available.
Mean differences in intrasurgical drill-torque-measurements of 2–5 Ncm between natural subantral bone (DTV: 10,2 Ncm) and the four tested biomaterials are far too small to judge the bone stability correctly as a reliable sign of bone quality when overlapping variances between the groups are taken into consideration. Therefore our results concerning DTV suggest – although proposed by Friberg et al. 19951 - the DTV currently not to be suitable as reliable clinical diagnostic tool for an intrasurgical decision wether single-piece implants for immediate loading or two-stage-implants should be preferred for a comparable suitable long-term prognosis of the inserted implant.
This is different when Implant-Insertion-Torque-Values (ITV) are registered intrasurgically. Even when implant motors are used that allow torque-adjustments only in 3 or 5 Ncm-steps, highly significant differences of a mean minimum of 4 Ncm can be detected between natural subantral bone and Bio-Oss-augmented sinuses and 34 Ncm with easy-graft CRYSTAL-augmented sinuslift-sites, providing the surgeon a proper tool to decide wether immediate implant-loading could be possible or an unloaded healing time has to be kept, provided a consensus can be found to establish absolute margin values for immediate loading in the maxilla as proposed by Cannizzaro G. et al.10.
While only small differences of DTV and ITV between natural subantral bone and xenograft-augmented sites seem clear from the biological standpoint, one of the results of the present study needs closer attention: the significant DTV- and ITV-difference between the Biomaterial NanoBone and easy-graft CLASSIC in favour of easy-graft CLASSIC with both significant higher DTV and ITV.
NanoBone – by its chemical components – consists of very slow resorbing nanocrystal Hydroxyapatite embedded in a microporous Silicadioxide (SiO2)-matrix and by this is – from the chemical and biological standpoint - closer related to easy-graft CRYSTAL with its chemical components of Hydroxyapatite (60%) and beta-TCP (40%) than to easy-graft CLASSIC (fast resorbing pure microporous beta-TCP). While NanoBone as particulate granules - when soaked with blood by the physical capillary effect and then clots - build an elastic and mobile subantral scaffold for bone regeneration, easy-graft CLASSIC – also soaked with a blood clot – hardens to a solid bone-block graft under the detached and initially highly mobile Schneiderian membrane.
The human sinus undergoes a constant pressure-change in routine breathing activities at a frequency of 12–18 times/minute in grown-ups when breathing through the nose, which represents the natural breathing behavior, resulting in a constant pressure change in the maxillary sinus of 5–10 mbar26,27 that might add to even significant higher pressure forces at sneezing28.
Premise for sufficient subantral bone regeneration at the intial stage is the sufficient ingrowth of blood vessels into the surgically created vast subantral scaffold which was proven by Mammoto, A. et al.29 to be highly mechanosensitive: the more tissues are immobilized in their regenerative period the more blood-vessel ingrowth can be observed. This might lead to the conclusion, that immobile block-like subantral bone-grafts like easy-graft CLASSIC and easy-graft CRYSTAL offer significant higher requirements for a richer vascularization of the surgically created subantral scaffold as prerequisite for later sufficient and denser calcification than mobile granules, when mobility by pressure changes in the human maxillary sinus are taken into consideration. Nevertheless, this assumption is a plausible theory - although backed by clinical observations referring complications in fracture healing processes resulting in pseudarthrosis30 and by theoretical studies (Geris L et al. 2008)31 – and still has to be proven in experimental studies.
Another additive and/or cumulative effect beside the immobilization of the subantral biomaterial could be the angiogenesis-enhancing and osteoblast-stimulating effect of the ultrasonic surgical procedure itself. As already proven for the therapeutic application of ultrasound32,33,34 (Reher P et al., 1999, 2002; Suchkova VN, 2002) the application of ultrasound at frequencies of 30–40 kHz results to a significantly enhanced bone repair in the maxillofacial region35,36 improving the entire cascade of bone healing starting with an enhanced vascularization – if properly immobilized29 – and enhanced activity of osteoblasts.
These mechanisms of bone regeneration described above could – within the limits of this study - possibly also explain the highly significant difference of DTV and ITV when the two chemically similar biomaterials “NanoBone” and “easy-graft CRYSTAL” (60% HA/40% beta-TCP) are compared while the steadiness of the results could be attributed to the surgical procedure performed minimally invasive with an ultrasonic surgical device.
By again referring to the suggestions of Cannizzaro G. et al.10 to accept an ITV of 45 Ncm as “margin line” for the clinician's decision on immediate loading of freshly inserted subantral implants, this “margin line” is safely complied with the use of the biomaterial easy-graft CRYSTAL and sharply met with the use of easy-graft CLASSIC. Nevertheless it still has to be proven in clinical studies that comparable DTVs and ITVs can be achieved with these biomaterials also, when sinuslift-techniques other than the tHUCSL-INTRALIFT are used. Even more, clinical studies have to be performed in the same experimental setup to determine the achievable DTVs and ITVs with different dental implant systems. By this, the absolute numbers of DTV and ITV determined in the present study can be considered only valid for the Q2-implant or similar systems with a self-taper, root analogue screw-design, the significant relative differences in DTV and ITV might be applicable generally.
Conclusions
The tHUCSL-INTRALIFT by its well documented innate atraumaticity25 seems not only to provide steady clinical results in praxem37 but might be suitable as standard-procedure in clinical research to obtain unbiased results when subantral grafting materials are investigated for their bone regeneration behaviour and final physical bone-density quality.
Drill-Torque-Values are useful in experimental research but still are questionable as reliable clinical parameter for the surgeon to decide upon immediate or delayed implant loading, mostly also due to the fact that implant motors rarely provide torque-adjustments in 1 Ncm-steps. Furthermore, the different mechanical properties of implant-drills - specific for each implant system - are not comparable and have to be determined in experimental and/or clinical studies for each implant drill system.
Self-hardening bone graft materials such as easy-graft CLASSIC and easy-graft CRYSTAL - resulting in a bone-block-like subantral scaffold after insertion similar to autologous bone-block-grafts - seem to enable a physical denser and mechanical more stable bone regeneration than loose particulate bone graft-materials with significant better ITV-results in favour of HA-components-containing materials such as easy-graft CRYSTAL. To better understand the biomechanical properties of bone/betaTCP/HA-compounds and strain-distribution of implants inserted into such compounds, finite-elemente simulations will have to be undertaken once 3D-micro-CT-results are published by other research-groups currently investigating this issue.
Further studies have to be undertaken also to determine DTVs and ITVs for implant systems other than the Q2-implant-system used in this study for a direct comparison, as well as experimental, histological and micromolecular studies to reveal and verify the biological mechanisms described by Mammoto, A. et al.29, to be valid also for subantral bone regeneration in regard to the continuous pressure changes in the human sinus at breathing.
Footnotes
The presented study was conducted without any exterior funding as part of routine patient treatment by all authors. Surgery-documentation were not specially altered for the presented study compared to routine patient treatment in the authors' clinics.DrDr Troedhan A, Dr Schlichting I, Dr Kurrek A and Dr Wainwright M declare no conflicts of interests by monetary funding or compensation of their research by Satelec-ACTEON (Piezo-devices), TRINON-Karlsruhe-GmbH (Implant-system), Geistlich (BioOss), ArtOss (NanoBone), SUNSTAR-Degradable (easy-graft), personal funding or dependencies by and from the above mentioned companies or any kind of benefitial remuneration in cash, stocks or stock options or equities.All devices used in this study were regularly purchased from national dental suppliers and are owned by the authors, as well as the used dental-implants and biomaterials as the same implants and biomaterials among other brands are used in the clinical routine of the authors' clinics in all indications for bone-augmentation and implant insertion since 2001 (DrDr Troedhan A, Dr Kurrek A) and 2004 for Dr Schlichting I and Dr Wainwright M.DrDr Troedhan A, Dr Kurrek A and Dr Wainwright M - forming the independent “TKW-Research-Group” - hold a non-remunerated co-inventorship on the patent filed for the ultrasonic surgical tool-tips for the Intralift-sinuslift and are supported by Satelec-ACTEON in prototyping and manufacturing new Piezotome-applicator-tips designed by these three authors since Satelec-ACTEON discloses revelation of exact specifications on metal/resin-alloys and oscillation-induction for their ultrasonic surgical devices. In case of invitations of DrDr Troedhan A, Dr Schlichting I, Dr Kurrek A and Dr Wainwright M by Universities, educational institutions or organizers of hands-on workshops for qualified dentists' training in cooperation with one of the above mentioned companies, travel-expenses, accommodation and daily diets, regulated by Austrian and German law, are remunerated.Dr Kurrek A was a non-remunerated chief-medical advisor in the development of the Q-implant-system from 1997–1999 and Dr Kurrek A and Dr Troedhan A lead international implantology-courses as visiting Professors at the Health Science University Vientiane/Laos, Faculty of Dentistry in cooperation with TRINON GmbH.
Author Contributions T.A., S.I., K.A. and W.M. equally performed tHUCSL-Intralift-surgeries and implant-insertions and data-acquisition for this study. T.A. and S.I. wrote the manuscript text which was revised then by K.A. and W.M. Fig. 1,2,5,6 and Table 1,2 were prepared by T.A. and S.I., Fig. 3 and 4 by K.A. and W.M. All authors reviewed the final manuscript.
References
- Friberg B., Sennerby L., Roos J. & Lekholm U. Identification of bone quality in conjunction with insertion of titanium implants. A pilot study in jaw autopsy specimens. Clin Oral Impl Res. 6, 213–219 (1995). [DOI] [PubMed] [Google Scholar]
- Alsaadi G., Quirynen M., Michiels K., Jacobs R. & Van Steenberghe D. A biomechanical assessment of the relation between the oral implant stability at insertion and subjective bone quality assessment. J. Clin Periodontol. 34, 359–366 (2007). [DOI] [PubMed] [Google Scholar]
- Turkyilmaz I., Tözüm T. F., Tumer C. & Ozbek E. N. Assessment of correlation between computerized tomography values of the bone, and maximum torque and resonance frequency values at dental implant placement. J. Oral Rehab. 33, 881–888 (2006). [DOI] [PubMed] [Google Scholar]
- Turkyilmaz I., Tumer C., Ozbek E. N. & Tözüm T. F. Relations between the bone density values from computerized tomography, and implant stability parameters: a clinical study of 230 regular platform implants. J. Clin Periodontol. 34, 716–722 (2007). [DOI] [PubMed] [Google Scholar]
- Turkyilmaz I., Aksoy U. & McGlumphy E. A. Two alternative surgical techniques for enhancing primary implant stability in the posterior maxilla: a clinical study including bone density, insertion torque, and resonance frequency analysis data. Clin Impl Dent Rel Res. 10, 231–237 (2008). [DOI] [PubMed] [Google Scholar]
- Turkyilmaz I. & McGlumphy E. A. Influence of bone density on implant stability parameters and implant success: a retrospective clinical study. BMC Oral Health 8, 32 (2008). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Turkyilmaz I., Sennerby L., McGlumphy E. A. & Tözüm T. F. Biomechanical aspects of primary implant stability: a human cadaver study. Clin Impl Dent Rel Res. 11, 113–119 (2009). [DOI] [PubMed] [Google Scholar]
- Trisi P. et al. Implant micromotion is related to peak insertion torque and bone density. Clin Oral Impl Res. 20, 467–471 (2009). [DOI] [PubMed] [Google Scholar]
- Szmukler-Moncler S., Salama H., Reingewirtz Y. & Dubruille J. H. Timing of loading and effect of micromotion on bone–dental implant interface: review of experimental literature. J Biomed Mat Res. 43, 192–203 (1998). [DOI] [PubMed] [Google Scholar]
- Cannizzaro G., Leone M. & Esposito M. Immediate functional loading of implants placed with flapless surgery in the edentulous maxilla: 1-year follow-up of a single cohort study. Int J. Oral Maxillofac Impl. 22, 87–95 (2007). [PubMed] [Google Scholar]
- Esposito M., Grusovin M. G., Willings M., Coulthard P. & Worthington H. V. The effectiveness of immediate, early, and conventional loading of dental implants: a Cochrane systematic review of randomized controlled clinical trials. Int J. Oral Maxillofac Impl. 22, 893–904 (2007). [PubMed] [Google Scholar]
- Chung S., McCullagh A. & Irinakis T. Immediate loading in the maxillary arch: evidence-based guidelines to improve success rates: a review. J. Oral Implant. 37, 610–621 (2011). [DOI] [PubMed] [Google Scholar]
- Rabel A., Köhler S. G. & Schmidt-Westhausen A. M. Clinical study on the primary stability of two dental implant systems with resonance frequency analysis. Clin Oral Invest. 11, 257–265 (2007). [DOI] [PubMed] [Google Scholar]
- Walker L. R., Morris G. A. & Novotny P. J. Implant insertional torque values predict outcomes. J Oral Maxillofac Surg. 69, 1344–1349 (2011). [DOI] [PubMed] [Google Scholar]
- Pommer B. et al. Primary implant stability in the atrophic sinus floor of human cadaver maxillae: impact of residual ridge height, bone density, and implant diameter. Clin Oral Impl Res. 25, e109–e113 (2012). [DOI] [PubMed] [Google Scholar]
- Degidi M., Daprile G. & Piattelli A. Primary stability determination by means of insertion torque and RFA in a sample of 4,135 implants. Clin Impl Dent Rel Res. 14, 501–507 (2012). [DOI] [PubMed] [Google Scholar]
- Degidi M., Daprile G., Piattelli A. & Carinci F.. Evaluation of factors influencing Resonance Frequency Analysis Values, at insertion surgery, of implants placed in sinus-augmented and nongrafted sites. Clin Impl Dent Rel Res. 9, 144–149 (2007). [DOI] [PubMed] [Google Scholar]
- Degidi M., Daprile G. & Piattelli A.. RFA values of implants placed in sinus grafted and nongrafted sites after 6 and 12 months. Clin Impl Dent Rel Res. 11, 178–182 (2009). [DOI] [PubMed] [Google Scholar]
- Di Lallo S. et al. Resonance frequency analysis assessment of implants placed with a simultaneous or a delayed approach in grafted and nongrafted sinus sites: A 12-month clinical study. Clin Impl Dent Rel Res. published online ahead of print 10.1111/cid.12002 (2012). [DOI] [PubMed] [Google Scholar]
- Jensen S. S. et al. Influence of particle size of deproteinized bovine bone mineral on new bone formation and implant stability after simultaneous sinus floor elevation: a histomorphometric study in minipigs. Clin Impl Dent Rel Res. Epub ahead of print 10.1111/cid.12101 (2013). [DOI] [PubMed] [Google Scholar]
- Iezzi G. et al. Correlation between the bone density recorded by a computerized implant motor and by a histomorphometric analysis: a preliminary in vitro study on bovine ribs. Clin Impl Dent Rel Res. Epub ahead of print 10.1111/cid.12121 (2013). [DOI] [PubMed] [Google Scholar]
- Troedhan A. C., Kurrek A., Wainwright M. & Jank S. Hydrodynamic ultrasonic sinus floor elevation — an experimental study in sheep. J. Oral Maxillofac Surg. 68, 1125–1130 (2010). [DOI] [PubMed] [Google Scholar]
- Jank S., Kurrek A., Wainwright M., Bek V. E. & Troedhan A. Rupture length of the sinus membrane after 1.2 mm puncture and surgical sinus elevation: an experimental animal cadaver study. Oral Surg Oral Med Oral Pathol Oral Radiol Endodont. 112, 568–572 (2011). [DOI] [PubMed] [Google Scholar]
- Troedhan A., Kurrek A. & Wainwright M. Biological principles and physiology of bone regeneration under the Schneiderian Membrane after sinus lift surgery: a radiological study in 14 patients treated with the transcrestal Hydrodynamic Ultrasonic Cavitational Sinus Lift (Intralift). Int J. Dent. Article ID 576238, 12 pp, 10.1155/2012/576238 (2012). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Troedhan A., Kurrek A., Wainwright M. & Jank S. Schneiderian membrane detachment using transcrestal hydrodynamic ultrasonic cavitational sinuslift: a human cadaver head study and histology analysis. J. Oral Maxillofac Surg. 10.1016/j.joms.2014.02.021, e1–e10 (2014). [DOI] [PubMed] [Google Scholar]
- Aust R. & Drettner B. Experimental studies of the gas exchange through the ostium of the maxillary sinus. Upsala J. Med Sciences 79, 177–186 (1974). [DOI] [PubMed] [Google Scholar]
- Kutluhan A. et al. The effects of uncinectomy and natural ostial dilatation on maxillary sinus ventilation: a clinical experimental study. Europ Arch Oto Rhin Laryng. 268, 569–573 (2011). [DOI] [PubMed] [Google Scholar]
- Gonzalez F., Cal V. & Elhendi W.. Orbital emphysema after sneezing. Ophthal Plastic Reconstr Surg. 21, 309–311 (2005). [DOI] [PubMed] [Google Scholar]
- Mammoto A. et al. A mechanosensitive transcriptional mechanism that controls angiogenesis. Nature 457, 1103–1108 (2009). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Frost H. M. The biology of fracture healing: An overview for clinicians. Part II. Clin Orthopaed Rel Res. 248, 294–309 (1989). [PubMed] [Google Scholar]
- Geris L., Gerisch A., Sloten J. V., Weiner R. & Oosterwyck H. V. Angiogenesis in bone fracture healing: a bioregulatory model. J. Theor Biol. 251, 137–158 (2008). [DOI] [PubMed] [Google Scholar]
- Reher P., Doan N., Bradnock B., Meghji S. & Harris M. Effect of ultrasound on the production of IL-8, basic FGF and VEGF. Cytokine 11, 416–423 (1999). [DOI] [PubMed] [Google Scholar]
- Reher P., Harris M., Whiteman M., Hai H. K. & Meghji S. Ultrasound stimulates nitric oxide and prostaglandin e2 production by human osteoblasts. Bone 31, 236–241 (2002). [DOI] [PubMed] [Google Scholar]
- Suchkova V. N., Baggs R. B., Sahni S. K. & Francis C. W. Ultrasound improves tissue perfusion in ischemic tissue through a nitric oxide dependent mechanism. Thromb Haemost. 88, 865–870 (2002). [PubMed] [Google Scholar]
- Schortinghuis J., Stegenga B., Raghoebar G. M., & de Bont L. G. M. Ultrasound stimulation of maxillofacial bone healing. Crit Rev Oral Biol Med. 14, 63–74 (2003). [DOI] [PubMed] [Google Scholar]
- Mouraret S. et al. Cell viability after osteotomy and bone harvesting: comparison of piezoelectric surgery and conventional bur. Int J. Oral Maxillofac Surg 2014; Epub ahead of print: 10.1016/j.ijom.2013.11.018 (2014). [DOI] [PubMed] [Google Scholar]
- Troedhan A. et al. The transcrestal hydrodynamic ultrasonic cavitational sinuslift: results of a 2 year prospective multicenter study on 404 patients, 446 sinuslift sites and 637 inserted implants. Open J. Stomatol. 3, 471–485 (2013). [Google Scholar]