Abstract
Introduction
Clinical symptoms and sociodemographic variables predict level of functioning and quality of life in patients with schizophrenia. However, few studies have examined the effect of personality traits on quality of life and overall functioning in schizophrenia. Personality traits are premorbid to illness and may predict the way patients experience schizophrenia. The aim of this study was to examine the individual and additive effects of two core personality traits—neuroticism and extraversion—on quality of life and functioning.
Methods
Patients with schizophrenia-spectrum disorders (n = 153) and healthy controls (n = 125) completed personality and quality of life questionnaires. Global functioning was assessed during a clinician-administered structured interview. Neuroticism and extraversion scores were analyzed both as continuous variables and as categorical extremes (High versus Normal Neuroticism, Low versus Normal Extraversion).
Results
Quality of life was significantly associated with neuroticism, extraversion, and the neuroticism × diagnosis and extraversion × diagnosis interactions. For patients, a lower neuroticism score (in the normal range) was associated with quality of life scores comparable to controls; whereas high neuroticism scores in patients were associated with the lowest quality of life. For overall functioning, only diagnosis had a significant effect.
Conclusion
Neuroticism modulates quality of life and may provide an important key to improving the life of patients with schizophrenia.
Keywords: Neuroticism, Extraversion, Schizophrenia, Quality of Life
1. Introduction
Quality of life and overall functioning are important clinical outcomes in psychiatry. They represent crucial benchmarks for a more personalized approach to patient care. While people with psychiatric disorders are generally at risk of poor functioning and poor quality of life, those with schizophrenia are especially affected (Bobes et al., 2007). Quality of life is lower in schizophrenia patients who are younger, have more psychotic symptoms, have less contact with family, are in worse financial situations, and have achieved lower levels of education (Bobes et al., 2007; Gardsjord et al., 2016). Overall functioning is lower in schizophrenia patients with more negative symptoms or are unemployed (Chabungbam et al., 2007; Herbener and Harrow, 2004; Rabinowitz et al., 2012). However, much remains unknown about these diagnosis-specific impairments in quality of life and functioning.
Quality of life and overall functioning in schizophrenia can be predicted by antecedent risk factors of the illness, such as temperament and personality (Barrantes-Vidal et al., 2009; Boyette et al., 2014b; Compton et al., 2015; Herrán et al., 2006; Kentros et al., 1997; Lahey, 2009; Lysaker et al., 1998). For example, neuroticism and extraversion are associated with quality of life and overall functioning in schizophrenia (Boyette et al., 2014b; Lahey, 2009; Lysaker et al., 1998), and the effect on quality of life persists when controlling for symptoms and sociodemographic factors (Boyette et al., 2014b, 2014a; Kentros et al., 1997). Moreover, higher neuroticism and lower extraversion are linked to factors that contribute to quality of life, such as passive, avoidant coping, deficits in intrinsic motivation, and greater emotional discomfort (Lysaker et al., 2004; Lysaker and Taylor, 2007; Vohs et al., 2013). Similarly, neuroticism is negatively associated with overall functioning, while extraversion, agreeableness, and conscientiousness are positively associated with overall functioning (Compton et al., 2015). In addition, higher neuroticism and agreeableness scores predict relapse after first-episode psychosis (Gleeson et al., 2005).
While previous studies have demonstrated the predictive value of personality factors for quality of life and overall functioning in schizophrenia, the potential additive effects of personality factors have yet to be explored. For example, a patient with schizophrenia who has both high neuroticism and low extraversion may be more socially isolated, have more trouble holding a job, and have trouble responding to stressful situations—compared to a patient with only high neuroticism or low extraversion--, leading to poor quality of life and overall functioning. Thus, the combined effect of neuroticism and extraversion may represent a more significant risk profile for patients. Furthermore, previous studies examined personality factors in psychotic patients only, though quality of life and overall functioning can be measured in healthy controls as well. Finally, research to date has examined personality factors as continuous variables, although using categorical measures may be more likely to influence clinical treatment (Kagan and Snidman, 2004).
The present study tested the hypothesis that the personality factors neuroticism and extraversion are associated with overall functioning and quality of life in patients with schizophrenia. We hypothesized that the combination of neuroticism and extraversion would predict quality of life and overall functioning, such that patients with higher neuroticism and lower extraversion would have the poorest quality of life and functioning. We also hypothesized that categorical methods for defining personality would be better at predicting quality of life and overall functioning, such that those with “high” neuroticism and “low” extraversion would have the poorest overall functioning and quality of life. Ultimately, we hope that these extreme categories could make it easier for clinicians to identify patients with schizophrenia who are at risk of poor subjective quality of life and overall functioning.
2. Methods
2.1 Setting and Sample
Participants were recruited as part of an ongoing research study and included 153 patients with schizophrenia-spectrum disorders (38 schizoaffective, 77 schizophrenia, 38 schizophreniform) and 125 healthy control subjects. Psychosis patients were recruited from the Vanderbilt Psychiatric Hospital; healthy controls were recruited via community advertisements. The Vanderbilt University Institutional Review Board (Nashville, Tennessee) approved the study protocol and all subjects completed informed consent. Subjects were considered for the study if they were between the ages of 14 and 65, had pre-morbid IQ scores greater than 70, were not pregnant or lactating, did not suffer from a chronic medical illness (such as diabetes or heart disease) or a central nervous system disorder (such as multiple sclerosis or epilepsy) that might affect the study results, and did not have a history of traumatic brain injury. Control subjects were included if they did not have a history of a psychiatric disorder and patients were included if they had no substance abuse within the last three months. Participants completed self-report measures of personality and quality of life. Trained research staff performed a Structured Clinical Interview of the DSM-IV-TR (SCID) (First et al., 2001). The SCID was used to confirm diagnoses and symptom experiences in patients and to rule out past or present psychiatric illness in psychiatrically-healthy controls. A Global Assessment of Functioning (GAF) score was assigned to each subject as a measure of current level of overall functioning (see Table 1 for subject characteristics).
Table 1.
Subject demographic characteristics.
| Schizophrenia Patients (N = 153) | Healthy Controls (N = 125) | p-Value | |
|---|---|---|---|
| Mean Age | 32.35 ± 1.00 | 30.83 ± 1.03 | 0.29 |
| Sex | 0.16 | ||
| Male | 103 | 74 | |
| Female | 50 | 51 | |
| Race | 0.28 | ||
| White | 93 | 86 | |
| Black/African American | 52 | 34 | |
| Other | 8 | 5 | |
| Mean Parental Education | 13.88 ± 0.28 | 14.53 ± 0.19 | 0.05 |
| Mean Age at Onset of Illness | 21.08 ± 0.47 | -- | -- |
| Mean Duration of Illness | 10.34 ± 1.19 | -- | -- |
| Mean Chlorpromazine Equivalent | 468.46 ± 26.48 | -- | -- |
| Mean PANSS Score | |||
| Positive Subscale | 18.35 ± 0.54 | -- | -- |
| Negative Subscale | 16.15 ± 0.61 | -- | -- |
| General Subscale | 32.15 ± 0.67 | -- | -- |
* significant at α=0.05 level
2.2 Measures and Rating Scales
2.2.1 Personality: Neuroticism and Extraversion
All participants completed the NEO Five-Factor Inventory (NEO-FFI), a well-validated personality self-report questionnaire commonly used in mental health research (Costa and McCrae, 1992). For this study, we focused on the personality traits of Neuroticism and Extraversion based on past research findings (Camisa et al., 2005; Compton et al., 2015; Dinzeo and Docherty, 2007). Neuroticism and Extraversion scores are continuous, ranging from 0 to 48. In a normative sample, the mean Neuroticism subscale score was 15.77 ± 7.47 and the mean Extraversion subscale score was 28.50 ± 6.26 (McCrae and Costa, 2004). Therefore, in addition to the continuous measure, we created categorical variables for High/Normal Neuroticism and Low/Normal Extraversion using the top/bottom 25% of neuroticism and extraversion scores based on the normative distributions (neuroticism scores greater than 20.8 and extraversion scores less than 24.3). This cut-off was chosen to balance standard cut-offs in extreme groups research (typically ± 1 standard deviation or 15%) and practical constraints of having sufficient sample size in the extreme groups (Blackford et al., 2011; Kagan et al., 1988).
2.2.2 Quality of Life
All participants completed the Quality of Life Enjoyment and Satisfaction Questionnaire, Short Form (Q-LES-Q-SF), which is a self-report measure of perceived quality of life during the past week (Endicott et al., 1993). The reliability and validity of the Q-LES-QSF have been verified in independent studies using both healthy controls and patients with schizophrenia and we found similarly high reliability in both groups in the present study (Rapaport et al., 2005; Ritsner et al., 2005; Stevanovic, 2011). The questionnaire is regularly used to measure quality of life in mental health research and in clinical settings. QLES-Q-SF scores are typically expressed as a percent of the maximum score of 70 and in a normative sample, the mean percent maximum score is 0.83 (Rapaport et al., 2005).
2.2.4 Global Functioning
Participants were evaluated using the Global Assessment of Functioning (GAF), which is the final component of the multiaxial diagnostic categorization scheme used in Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition, Text Revision (American Psychiatric Association, 2000). The GAF is rated on a 0 – 100 scale; higher scores represent better overall functioning. The reliability and validity of the GAF scale have been verified previously (Startup et al., 2002). Furthermore, GAF scores are frequently used to measure overall functioning in both clinic and research settings.
2.3 Data Analyses
To determine whether the personality traits of neuroticism and extraversion differed as a function of diagnosis (patients/controls), a binomial logistic regression was performed with neuroticism, extraversion, and the neuroticism × extraversion interaction as predictor variables and diagnosis as the outcome variable. For the categorical personality variables, a Cochran-Mantel-Haenszel test was used to examine the association between diagnosis, high neuroticism, and low extraversion.
To assess the effects of diagnosis, neuroticism, and extraversion on quality of life and functioning, analyses of variance (ANOVA) were performed. Diagnosis (dummy coded), neuroticism, extraversion, and their two- and three-way interactions were included as predictors. Neuroticism and extraversion were centered to remove the inherent collinearity with interaction terms. Separate ANOVAs were performed for quality of life and for global functioning. For the categorical analyses, the categorical variables were dummy coded and analyses were performed with diagnosis, neuroticismcat, extraversioncat, and the two- and three-way interactions as predictor variables and quality of life or overall functioning as the outcome.
All analyses were conducted using Stata 13 (StataCorp, 2013).
3. Results
3.1 Patient Characteristics
Patients and controls did not differ with regard to sex, mean age, race, and mean parental education (Table 1). Psychotic patients had significantly higher neuroticism scores relative to controls (β = .25 [95% CI: .03, .47], p = .02) but showed no significant difference on extraversion scores. With the categorical approach, patients were significantly more likely to be in the high neuroticism group (Q(1) = 68.92, p < .001) and in the low extraversion group (Q(1) = 7.44, p = .01) (Table 1 in Supplement).
3.2 Effects of Diagnosis and Personality on Quality of Life and Functioning
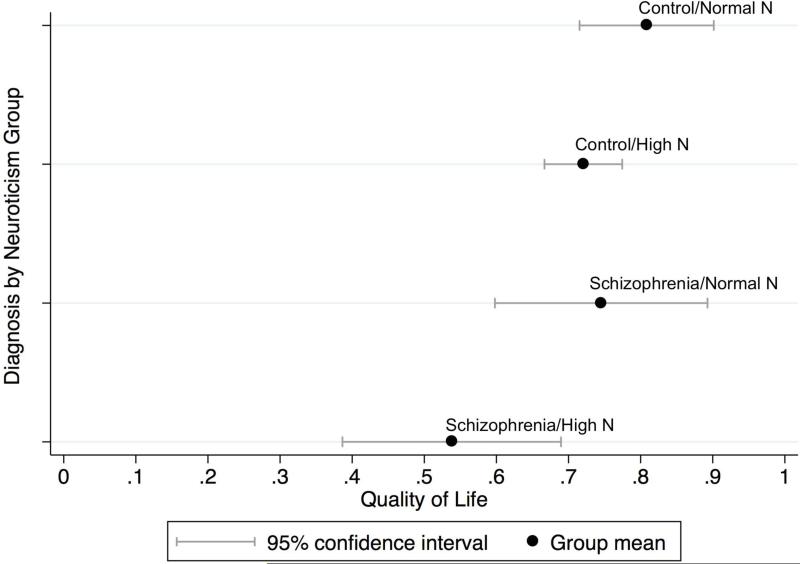
When examining the effect of personality traits on quality of life, we found significant effects of diagnosis (F7,270 = 18.23, p < .001, η2 = .06), neuroticism (F7,270 = 53.16, p < .001, η2 = .16), extraversion (F7,270 = 13.30, p = .001, η2 = .05), and the interaction between diagnosis and extraversion (F7,270 = 5.36, p = .02, η2 = .02) (Table 2). Lower quality of life was associated with a diagnosis of schizophrenia (r2 = .31), higher neuroticism scores (r2 = .41), and lower extraversion scores (r2 = .18). With the categorical approach, the findings were very similar with diagnosis, neuroticismcat, and extraversioncat all having a significant effect on quality of life. The diagnosis by neuroticismcat interaction was also significant (F7,270 = 6.66, p = .01, η2 = .02), but the diagnosis by extraversioncat interaction was only significant at trend level (p = .08) (Table 3). A post-hoc regression analysis of neuroticismcat on quality of life by diagnosis showed a stronger effect of neuroticismcat on quality of life in the patients (r2 = .29) than in the controls (r2 = .10). A comparison of the quality of life means by diagnosis revealed that healthy controls in the normal neuroticismcat group had the highest quality of life, followed by patients with schizophrenia in the normal neuroticismcat group, healthy controls in the high neuroticismcat group and finally patients in the high neuroticismcat group (Figure 1).
Table 2.
Association between dimensional personality traits, quality of life, and overall functioning.
| Quality of Life | Partial Sum of Squares | F | p-Value | Partial η2 |
|---|---|---|---|---|
| Diagnosis | 0.24 | 18.23 | <0.001* | 0.06 |
| Neuroticism | 0.70 | 53.16 | <0.001* | 0.16 |
| Extraversion | 0.18 | 13.30 | <0.001* | 0.05 |
| Diagnosis * Neuroticism | 0.02 | 1.84 | 0.18 | 0.01 |
| Diagnosis * Extraversion | 0.07 | 5.36 | 0.02* | 0.02 |
| Neuroticism * Extraversion | 0.03 | 2.57 | 0.11 | 0.01 |
| Diagnosis * Neuroticism * Extraversion | 0.01 | 0.59 | 0.44 | 0.002 |
| Overall Functioning | Partial Sum of Squares | F | p-Value | Partial η2 |
|---|---|---|---|---|
| Diagnosis | 84164.18 | 711.57 | <0.001* | 0.72 |
| Neuroticism | 0.51 | 0.00 | 0.95 | 0.000 |
| Extraversion | 78.82 | 0.67 | 0.42 | 0.003 |
| Diagnosis * Neuroticism | 403.01 | 3.41 | 0.07 | 0.01 |
| Diagnosis * Extraversion | 53.09 | 0.45 | 0.50 | 0.002 |
| Neuroticism * Extraversion | 91.37 | 0.77 | 0.38 | 0.003 |
| Diagnosis * Neuroticism * Extraversion | 9.56 | 0.08 | 0.78 | 0.000 |
significant at α=0.05 level
Table 3.
Association between categorical personality traits, quality of life, and overall functioning.
| Quality of Life | Partial Sum of Squares | F | p-Value | Partial η2 |
|---|---|---|---|---|
| Diagnosis | 0.51 | 33.63 | <0.001* | 0.11 |
| Neuroticism | 0.66 | 43.06 | <0.001* | 0.14 |
| Extraversion | 0.07 | 4.33 | 0.04* | 0.02 |
| Diagnosis * Neuroticism | 0.10 | 6.66 | 0.01* | 0.02 |
| Diagnosis * Extraversion | 0.05 | 3.08 | 0.08 | 0.01 |
| Neuroticism * Extraversion | 0.02 | 1.16 | 0.28 | 0.004 |
| Diagnosis * Neuroticism * Extraversion | 0.000 | 0.01 | 0.92 | 0.000 |
| Overall Functioning | Partial Sum of Squares | F | p-Value | Partial η2 |
|---|---|---|---|---|
| Diagnosis | 79588.23 | 660.83 | <0.001* | 0.72 |
| Neuroticism | 1.38 | 0.01 | 0.91 | 0.000 |
| Extraversion | 12.99 | 0.11 | 0.74 | 0.000 |
| Diagnosis * Neuroticism | 64.41 | 0.53 | 0.47 | 0.002 |
| Diagnosis * Extraversion | 0.36 | 0.00 | 0.96 | 0.000 |
| Neuroticism * Extraversion | 30.00 | 0.25 | 0.62 | 0.001 |
| Diagnosis * Neuroticism * Extraversion | 221.13 | 1.84 | 0.18 | 0.007 |
significant at α=0.05 level
Figure 1.
Mean quality of life for each personality group and diagnosis.
For the outcome measure of overall functioning, the only significant effect was for diagnosis (continuous approach: F7,260 = 711.57, p < .001, η2 = .73; categorical approach: F7,260 = 660.83, p < .001, η2 = .72). Patients had lower overall functioning than controls with diagnosis accounting for more than two thirds of the variance in functioning. Neither personality trait significantly increased the prediction of overall functioning beyond the information provided by diagnosis.
4. Discussion
We studied the effects of neuroticism and extraversion on quality of life and functioning in schizophrenia using two different approaches—a continuous approach using dimensional personality measures and a categorical approach using groups that were high on neuroticism or low on extraversion. We found three strong and independent predictors of quality of life: diagnosis, neuroticism and extraversion. In addition, the effects of extraversion and neuroticismcat on quality of life were moderated by diagnosis. This result can be conceptualized as three separate “hits” on quality of life: a diagnosis of schizophrenia, high neuroticism, and low extraversion. In general, neuroticism and extraversion impacted quality of life for both patients and healthy controls. The results of the continuous and categorical approaches were largely similar, with two exceptions: the interaction between diagnosis and extraversion was only revealed with the continuous approach, whereas the interaction between diagnosis and neuroticism on quality of life was only revealed with the categorical approach. Lower extraversion subjects demonstrated lower perceived quality of life than those with average or higher extraversion. In contrast, designating high versus average neuroticism using normative data, revealed that the patients in the average neuroticism group had higher perceived quality of life than the healthy controls in the high neuroticism group. The significant effect of neuroticism and extraversion on quality of life is consistent with previous studies of patients with schizophrenia (Boyette et al., 2014b; Kentros et al., 1997). By including a large healthy control group, we were able to test the interaction effect of diagnosis and personality traits. The effects of neuroticism and extraversion differed by group and were stronger in the patient groups.
Patients with schizophrenia and high neuroticism had by far the lowest quality of life. Intriguingly, patients with schizophrenia and average neuroticism had better quality of life than the healthy controls with high neuroticism. These results indicate that personality traits impact quality of life, and should be considered in clinical settings after replication of these results. Patients with schizophrenia and high neuroticism should be observed for signs of dissatisfaction with quality of life, such as suicidal ideation (Kao et al., 2012; Kasckow et al., 2007; Yan et al., 2013). Moreover, patients with high neuroticism may benefit from therapies which have been shown to reduce neuroticism and increase extraversion. This has been demonstrated in patients with depression using cognitive-behavioral therapy, treatment with selective serotonin-reuptake inhibitors (SSRIs), and repetitive transcranial magnetic stimulation (rTMS) (Berlim et al., 2013; Ilieva, 2015; Tang et al., 2009). Similarly, the negative affect and maladaptive response to stress experienced by patients with schizophrenia and high neuroticism may be good targets for treatment with metacognitive and insight therapies (REFs) (Dimaggio and Lysaker, 2015; Hillis et al., 2015). Personality scales such as the NEO-FFI are reliable, valid and feasible in clinical practice. Adding them to the standard clinical assessment of patients with schizophrenia may allow for better treatment planning and prediction of outcome.
In contrast to the quality of life results in this analysis, personality traits did not impact overall functioning; only diagnosis had an effect. Results from previous studies examining personality and functioning have been mixed (Barrantes-Vidal et al., 2009; Compton et al., 2015; Herrán et al., 2006; Jones et al., 2009; Lysaker et al., 1998). One possibility is that the failure to detect effects of personality on functioning resulted from a Type II error. However, we believe this is unlikely given the relatively large sample size of both patients and controls. Another possible explanation is that the effect of diagnosis on overall functioning is so large that it hides any smaller effects that personality traits may have.
Finally, we compared dimensional and categorical approaches with the hypothesis that examining the extreme personality groups of high neuroticism and low extraversion would be more predictive of quality of life and overall functioning. However, the results from the two approaches were largely similar, with the exception of the diagnosis × extraversion interaction (significant in the dimensional analysis) and diagnosis × neuroticism interaction (significant in the categorical analysis). While the statistical significance differed by approach, the effect sizes for the interactions were very similar for the two analyses (ranging from η2 of .01 - .02), suggesting that the small effects were slightly more detectable with one approach or another, depending on small differences in how variance was accounted for. Given the similar findings of the two approaches, we recommend the categorical cut-offs for high neuroticism and low extraversion as a simple and practical screen in clinical settings.
4.1 Limitations
There are several potential limitations to this study. First, the quality of life measure was self-report, which may introduce self-report bias or may be reported differently in patients with schizophrenia. However, a previous study demonstrated excellent validity and reliability with the quality of life measure in patients with schizophrenia and our study replicated these results (Ritsner et al., 2005). Yet, it will be important for future studies to also examine objective measures of quality of life. Second, the quality of life measure is time-dependent, measuring the subject's perceived quality of life only at the time of questionnaire administration; therefore, it is possible that the relationships between personality traits and quality of life may change over the course of illness. Studies that assess quality of life during the prodrome, first episode, and course of illness will be crucial for further characterizing the impact of personality traits on quality of life.
4.2 Conclusions
Diagnosis, neuroticism, and extraversion exert independent and interactive effects on quality of life in patients with schizophrenia. We propose that assessing neuroticism in patients with schizophrenia can provide valuable information that is relatively inexpensive and easy to collect. Patients with average neuroticism scores have better quality of life and patients with high neuroticism scores might benefit from treatment targeting negative affect and high reactivity, core features of neuroticism.
Supplementary Material
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- American Psychiatric Association . Diagnostic and statistical manual of mental disorders. 4th, text rev. ed. Author; Washington, DC: 2000. [Google Scholar]
- Barrantes-Vidal N, Ros-Morente A, Kwapil TR. An examination of neuroticism as a moderating factor in the association of positive and negative schizotypy with psychopathology in a nonclinical sample. Schizophr. Res. 2009;115:303–309. doi: 10.1016/j.schres.2009.09.021. doi:10.1016/j.schres.2009.09.021. [DOI] [PubMed] [Google Scholar]
- Berlim MT, McGirr A, Beaulieu M-M, Van den Eynde F, Tureki G. Are neuroticism and extraversion associated with the antidepressant effects of repetitive transcranial magnetic stimulation (rTMS)? An exploratory 4-week trial. Neurosci. Lett. 2013;534:306–310. doi: 10.1016/j.neulet.2012.12.029. doi:10.1016/j.neulet.2012.12.029. [DOI] [PubMed] [Google Scholar]
- Blackford JU, Avery SN, Cowan RL, Shelton RC, Zald DH. Sustained amygdala response to both novel and newly familiar faces characterizes inhibited temperament. Soc. Cogn. Affect. Neurosci. 2011;6:621–629. doi: 10.1093/scan/nsq073. doi:10.1093/scan/nsq073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bobes J, Garcia-Portilla MP, Bascaran MT, Saiz PA, Bousoño M. Quality of life in schizophrenic patients. Dialogues Clin. Neurosci. 2007;9:215–226. doi: 10.31887/DCNS.2007.9.2/jbobes. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boyette LL, Korver-Nieberg N, Meijer C, de Haan L, Kahn R, van Os J, Wiersma D, Bruggeman R, Cahn W, Myin-Germeys I. Quality of life in patients with psychotic disorders: Impact of symptoms, personality, and attachment. J. Nerv. Ment. Dis. 2014b;202:64–69. doi: 10.1097/NMD.0000000000000071. doi:10.1097/NMD.0000000000000071. [DOI] [PubMed] [Google Scholar]
- Boyette LL, van Dam D, Meijer C, Velthorst E, Cahn W, de Haan L, Kahn R, van Os J, Wiersma D, Bruggeman R, Myin-Germeys I. Personality compensates for impaired quality of life and social functioning in patients with psychotic disorders who experienced traumatic events. Schizophr. Bull. 2014a;40:1356–1365. doi: 10.1093/schbul/sbu057. doi:10.1093/schbul/sbu057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Camisa KM, Bockbrader MA, Lysaker P, Rae LL, Brenner CA, O'Donnell BF. Personality traits in schizophrenia and related personality disorders. Psychiatry Res. 2005;133:23–33. doi: 10.1016/j.psychres.2004.09.002. doi:10.1016/j.psychres.2004.09.002. [DOI] [PubMed] [Google Scholar]
- Chabungbam G, Avasthi A, Sharan P. Sociodemographic and clinical factors associated with relapse in schizophrenia. Psychiatry Clin. Neurosci. 2007;61:587–593. doi: 10.1111/j.1440-1819.2007.01722.x. doi:10.1111/j.1440-1819.2007.01722.x. [DOI] [PubMed] [Google Scholar]
- Compton MT, Bakeman R, Alolayan Y, Balducci PM, Bernardini F, Broussard B, Crisafio A, Cristofaro S, Amar P, Johnson S, Ramsay Wan C. Personality domains, duration of untreated psychosis, functioning, and symptom severity in first-episode psychosis. Schizophr. Res. 2015;168:113–119. doi: 10.1016/j.schres.2015.06.028. doi:10.1016/jschres.2015.06.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Costa PTJ, McCrae RR. Revised NEO Personality Inventory (NEO-PI-R) and the NEO Five-Factor Inventory (NEO-FFI) professional manual. 1992 [Google Scholar]
- Dimaggio G, Lysaker PH. Metacognition and mentalizing in the psychotherapy of patients with psychosis and personality disorders. J. Clin. Psychol. Sess. 2015;71:117–124. doi: 10.1002/jclp.22147. doi:10.1002/jclp.22147. [DOI] [PubMed] [Google Scholar]
- Dinzeo TJ, Docherty NM. Normal personality characteristics in schizophrenia: A review of the literature involving the FFM. J. Nerv. Ment. Dis. 2007;195:421–429. doi: 10.1097/01.nmd.0000253795.69089.ec. doi:10.1097/01.nmd.0000253795.69089.ec. [DOI] [PubMed] [Google Scholar]
- Endicott J, Nee J, Harrison W, Blumenthal R. Quality of life enjoyment and satisfaction questionnaire: A new measure. Psychopharmacol. Bull. 1993;29:321–326. [PubMed] [Google Scholar]
- First MB, Spitzer RL, Gibbon M, Williams JBW. Structured Clinical Interview for DSM-IV-TR Axis I Disorders, Research Version, Patient Edition with Psychotic Screen (SCID-I/P W/ PSY SCREEN) 2001 [Google Scholar]
- Gardsjord ES, Romm KL, Friis S, Barder HE, Evensen J, Haahr U, Hegelsad W. t. V., Joa I, Johannessen JO, Langeveld J, Larsen TK, Opjordsmoen S, Rund BR, Simonsen E, Valgum P, McGlashan T, Melle I, Røssberg JI. Subjective quality of life in first-episode psychosis: A ten year follow-up study. Schizophr. Res. 2016;172:23–28. doi: 10.1016/j.schres.2016.02.034. doi:10.1016/j.schres.2016.02.034. [DOI] [PubMed] [Google Scholar]
- Gleeson JF, Rawlings D, Jackson HJ, McGorry PD. Agreeableness and neuroticism as predictors of relapse after first-episode psychosis. J. Nerv. Ment. Dis. 2005;193:160–169. doi: 10.1097/01.nmd.0000154841.99550.d3. doi:10.1097/01.nmd.0000154841.99550.d3. [DOI] [PubMed] [Google Scholar]
- Herbener ES, Harrow M. Are negative symptoms associated with functioning deficits in both schizophrenia and nonschizophrenia patients? A 10-year longitudinal analysis. Schizophr. Bull. 2004;30:813–826. doi: 10.1093/oxfordjournals.schbul.a007134. doi:10.1093/oxfordjournals.schbul.a007134. [DOI] [PubMed] [Google Scholar]
- Herrán A, Sierra-Biddle D, Cuesta MJ, Sandoya M, Vásquez-Barquero JL. Can personality traits help us explain disability in schizophrenia? Psychiatry Clin. Neurosci. 2006;60:538–545. doi: 10.1111/j.1440-1819.2006.01577.x. doi:10.1111/j.1440-1819.2006.01577.x. [DOI] [PubMed] [Google Scholar]
- Hillis JD, Leonhardt BL, Vohs JL, Buck KD, Salvatore G, Popolo R, Dimaggio G, Lysaker PH. Metacognitive relfective and insight therapy for people in early phase of a schizophrenia spectrum disorder. J. Clin. Psychol. Sess. 2015;71:125–135. doi: 10.1002/jclp.22148. doi:10.1002/jclp.22148. [DOI] [PubMed] [Google Scholar]
- Ilieva I. Enhancement of healthy personality through psychiatric medication: The influence of SSRIs on neuroticism and extraversion. Neuroethics. 2015;8:127–137. doi:10.1007/s12152-014-9226-z. [Google Scholar]
- Jones S, Twiss J, Anderson IM. Do negative cognitive style and personality predict depression symptoms and functional outcomes in severe bipolar and unipolar disorders? Int. J. Cogn. Ther. 2009;2:343–353. doi:10.1521/ijct.2009.2.4.343. [Google Scholar]
- Kagan J, Reznick JS, Snidman N. Biological bases of childhood shyness. Science. 1988;240:167–171. doi: 10.1126/science.3353713. doi:10.1126/science.3353713. [DOI] [PubMed] [Google Scholar]
- Kagan J, Snidman N. The Long Shadow of Temperament. The Belknap Press of Harvard University Press; Cambridge, MA: 2004. The tapestries of temperament: Continua or categories; pp. 51–56. [Google Scholar]
- Kao YC, Liu YP, Cheng TH, Chou MK. Subjective quality of life and suicidal behavior among Taiwanese schizophrenia patients. Soc. Psychiatry Psychiatr. Epidemiol. 2012;47:523–532. doi: 10.1007/s00127-011-0361-0. doi:10.1007/s00127-011-0361-0. [DOI] [PubMed] [Google Scholar]
- Kasckow J, Montross L, Golshan S, Mohamed S, Patterson T, Sollanzano E, Zisook S. Suicidality in middle aged and older patients with schizophrenia and depressive symptoms: Relationship to functioning and quality of life. Int. J. Geriatr. Psychiatry. 2007;22:1223–1228. doi: 10.1002/gps.1817. doi:10.1002/gps.1817. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kentros MK, Terkelsen K, Smith TE, Goodman M. The relationship between personality and quality of life in persons with schizoaffective disorder and schizophrenia. Qual. Life Res. 1997;6:118–122. doi: 10.1023/a:1026433932142. [DOI] [PubMed] [Google Scholar]
- Lahey BB. Public health significance of neuroticism. Am. Psychol. 2009:241–256. doi: 10.1037/a0015309. doi:10.1037/a0015309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lysaker PH, Bell MD, Kaplan E, Bryson GJ. Personality and psychosocial dysfunction in schizophrenia: The association of extraversion and neuroticism to deficits in work performance. Psychiatry Res. 1998;80:61–68. doi: 10.1016/s0165-1781(98)00049-3. doi:10.1016/s0165-1781(98)00049-3. [DOI] [PubMed] [Google Scholar]
- Lysaker PH, Bryson GJ, Marks K, Grieg TC, Bell MD. Coping style in schizophrenia: Associations with neurocognitive deficits and personality. Schizophr. Bull. 2004;30:113–121. doi: 10.1093/oxfordjournals.schbul.a007056. doi:10.1093/oxfordjournals.schbul.a007056. [DOI] [PubMed] [Google Scholar]
- Lysaker PH, Taylor AC. Personality dimensions in schizophrenia: Associations with symptoms and coping concurrently and 12 months later. Psychopathology. 2007;40:338–344. doi: 10.1159/000105532. doi:10.1159/000105532. [DOI] [PubMed] [Google Scholar]
- McCrae RR, Costa PTJ. A contemplated revision of the NEO Five-Factor Inventory. Personal. Individ. Differ. 2004;36:587–596. doi:10.1016/S0191-8869(03)00118-1. [Google Scholar]
- Rabinowitz J, Levine SZ, Garibaldi G, Bugarski-Kirola D, Berardo CG, Kapur S. Negative symptoms have greater impact on functioning than positive symptoms in schizophrenia: Analysis of CATIE data. Schizophr. Res. 2012;137:147–150. doi: 10.1016/j.schres.2012.01.015. doi:10.1016/j.schres.2012.01.015. [DOI] [PubMed] [Google Scholar]
- Rapaport MH, Clary C, Fayyad R, Endicott J. Quality-of-life impairment in depressive and anxiety disorders. Am. J. Psychiatry. 2005;162:1171–1178. doi: 10.1176/appi.ajp.162.6.1171. doi:10.1176/appi.ajp.162.6.1171. [DOI] [PubMed] [Google Scholar]
- Ritsner M, Kurs R, Gibel A, Ratner Y, Endicott J. Validity of an abbreviated Quality of Life Enjoyment and Satisfaction Questionnaire (Q-LES-Q-18) for schizophrenia, schizoaffective, and mood disorder patients. Qual. Life Res. 2005;14:1693–1703. doi: 10.1007/s11136-005-2816-9. doi:10.1007/s11136-005-2816-9. [DOI] [PubMed] [Google Scholar]
- Startup M, Jackson MC, Bendix S. The concurrent validity of the Global Assessment of Functioning (GAF). Br. J. Clin. Psychol. 2002;41:417–422. doi: 10.1348/014466502760387533. doi:10.1348/014466502760387533. [DOI] [PubMed] [Google Scholar]
- StataCorp . Stata statistical software: Release 13. StataCorp LP; College Station, TX: 2013. [Google Scholar]
- Stevanovic D. Quality of Life Enjoyment and Satisfaction Questionnaire - short form for quality of life assessments in clinical practice: A psychometric study. J. Psychiatr. Ment. Health Nurs. 2011;18:744–750. doi: 10.1111/j.1365-2850.2011.01735.x. doi:10.1111/j.1365-2850.2011.01735.x. [DOI] [PubMed] [Google Scholar]
- Tang TZ, DeRubeis RJ, Hollon SD, Amsterdam J, Shelton R, Schalet B. A placebo-controlled test of the effects of paroxetine and cognitive therapy on personality risk factors in depression. Arch. Gen. Psychiatry. 2009;66:1322–1330. doi: 10.1001/archgenpsychiatry.2009.166. doi:10.1001/archgenpsychiatry.2009.166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vohs JL, Lysaker PH, Nabors L. Associations of personality with intrinsic motivation in schizophrenia. Psychiatry Res. 2013;208:78–80. doi: 10.1016/j.psychres.2013.03.008. doi:10.1016/j.psychres.2013.03.008. [DOI] [PubMed] [Google Scholar]
- Yan F, Xiang YT, Hou YZ, Ungvari GS, Dixon LB, Chan SS, Lee EH, Li WY, Li WX, Zhu YL, Chiu HF. Suicide attempt and suicidal ideation and their associations with demographic and clinical correlates and quality of life in Chinese schizophrenia patients. Soc. Psychiatry Psychiatr. Epidemiol. 2013;48:447–454. doi: 10.1007/s00127-012-0555-0. doi:10.1007/s00127-012-0555-0. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.