Abstract
Background
The variability in outcomes after anterior cruciate ligament reconstruction (ACLR) might be related to the criteria that are used to determine athletes’ readiness to return to their preinjury activity level. A battery of return-to-activity criteria (RTAC) that emphasize normal knee function and movement symmetry has been instituted to quantitatively determine athletes’ readiness to return to preinjury activities.
Purpose
To investigate performance-based and patient-reported measures at 12 and 24 months after ACLR between patients who passed or failed RTAC at 6 months after ACLR.
Study Design
Cohort study; Level of evidence, 2.
Methods
A total of 108 patients who had participated in International Knee Documentation Committee level 1 or 2 sports activities completed RTAC testing at 6, 12, and 24 months after surgery. The RTAC included the isometric quadriceps strength index (QI), 4 single-legged hop tests, the Knee Outcome Survey–activities of daily living subscale (KOS-ADLS), and the global rating scale of perceived function (GRS). Patients who scored ≥90% on all RTAC were classified as the pass group, and those who scored <90% on any RTAC were classified as the fail group. At 12- and 24-month follow-ups, patients were asked if they had returned to the same preinjury activity level.
Results
At the 6-month follow-up, there were 48 patients in the pass group and 47 in the fail group. At the 12-month follow-up, 31 patients (73.8%) from the pass group and 15 patients (39.5%) from the fail group passed RTAC, and at the 24-month follow-up, 25 patients (75.8%) from the pass group and 14 patients (51.9%) from the fail group passed RTAC. The rate of return to activities in the pass group was 81% and 84% at 12 and 24 months after ACLR, respectively, compared with only 44% and 46% in the fail group (P ≤ .012), respectively; however, some patients in the fail group participated in preinjury activities without being cleared by their therapists. At 12 and 24 months, 60.5% and 48.1% of patients continued to fail again on the criteria, respectively. A statistically significant group × time interaction was found for the single hop and 6-m timed hop limb symmetry indices (LSIs) (P ≤ .037), with only the fail group demonstrating a significant improvement over time. A main effect of group was detected for the QI and the crossover hop and triple hop LSIs (P <.01), with patients in the pass group demonstrating higher performance. A main effect of time was detected for the crossover hop and triple hop LSIs and the GRS, with improvements seen in both groups (P <.05).
Conclusion
Patients who passed the RTAC early after ACLR were more likely to demonstrate normal knee function and movement symmetry at 12 and 24 months postoperatively, while patients who failed the RTAC early were more likely to demonstrate impaired knee function and movement asymmetry at 12- and 24-month follow-ups. Patients in the pass group had a higher rate of return to their preinjury activity level compared with those in the fail group. A group of patients chose to return to their preinjury activities, even though they were functionally not ready.
Keywords: anterior cruciate ligament reconstruction, limb-to-limb symmetry, patient-reported measures, return-to-activity criteria, knee function
An injury to the anterior cruciate ligament (ACL) is frequently seen during sports activities25 and can result in a variety of structural and functional impairments that challenge patients’ ability to perform both daily living and sports tasks.14 Currently, ACL reconstruction (ACLR) has been advocated as the standard of care for active patients desiring to return to high-level activities.36 The common goal of ACLR is to restore mechanical knee stability, normal knee function, and limb-to-limb movement symmetry so that athletes can return to their preinjury level of activity and prevent further damage to the knee structures.11,12 Although ACLR can restore mechanical stability to the knee,45,46 quadriceps strength deficits and functional limitations often continue to persist long after surgery.15,27,31,34 Additionally, the rate of return to the pre-injury activity level is lower than anticipated, and the incidence of secondary ACL injuries is high after ACLR.5
A successful return to the preinjury activity level and a low incidence of secondary knee injuries after ACLR are desired outcomes; however, such outcomes are currently less than optimal.16,27 Ardern and colleagues5,8 reported that 55% of athletes returned to competitive-level sports after surgery, with only one-third of athletes returning to full sports competition at 1 year postoperatively. Athletes are 15 times more likely to experience secondary ACL injuries after ACLR compared with healthy persons.39 Furthermore, up to 21% of athletes who returned to sports had major functional limitations that could lead to a reduced level of performance.43 The poor postoperative outcomes highlight concerns over the criteria used to define readiness to return to the preinjury activity level and further point to the absence of a consensual, comprehensive set of return-to-activity criteria (RTAC).
Criteria related to the achievement of mechanical knee stability, minimum quadriceps strength deficits, and time from surgery are frequently used as guidelines to clear patients to return to activities.6,20 Barber-Westin and Noyes9 reported that only 15% of studies use time from surgery along with subjective factors to determine the return to unrestricted sports activities after ACLR. Only 13% of studies reported using objective criteria such as lower extremity muscle strength, limb movement symmetry, knee range of motion, and joint effusion.9 Recently, a comprehensive battery of RTAC that include both performance-based and patient-reported measures has been instituted to determine a patient’s readiness to return to multidirectional activities.1,16,21 The measures include quadriceps strength testing, 4 single-legged hop tests, and 2 patient-reported outcome questionnaires (Knee Outcome Survey–activities of daily living subscale [KOS-ADLS] and global rating scale of perceived function [GRS]). These RTAC measures emphasize good knee function and normal limb-to-limb movement symmetry. Additionally, the majority of these RTAC measures are sensitive to knee functional changes over time and have the potential to provide therapists with clinically relevant information, including patients’ functional deficits and responses to different therapeutic interventions,16,34 so as to provide appropriate rehabilitation training.
However, it is currently unknown whether patients demonstrating poor knee functional performance and limb movement asymmetry on RTAC early after surgery will continue to fail RTAC after an extended period of time. Therefore, the purpose of our study was to investigate functional performance and patient-reported outcome measures at 12 and 24 months after ACLR between those patients who passed (score ≥90%) and those who failed (score <90%) RTAC at 6 months after surgery and to further examine how these measures changed over time.
METHODS
A total of 108 patients who underwent ACLR from an ongoing prospective cohort study were included in this study. All patients were regular participants in International Knee Documentation Committee (IKDC) level 1 or 2 sports activities,13,28 which included jumping, cutting, pivoting, and lateral movements for more than 50 hours in the year before their ACL injury.30 Excluded from the study were patients having a concomitant ligamentous injury, a repairable meniscal injury, full-thickness articular cartilage damage, or a history of serious ipsilateral or contralateral lower extremity injuries (ie, fractures). All study patients underwent the same preoperative rehabilitation program, which included 5 weeks’ training of progressive quadriceps strengthening and specific perturbation training as described by Fitzgerald et al.22 ACLR was performed (mean [±SD] time from injury to surgery, 27.22 ± 3.48 weeks) using a soft tissue allograft (n = 69), semitendinosusgracilis autograft (n = 37), or bone–patellar tendon–bone autograft (n = 2). After surgery, all patients underwent a supervised, progressive postoperative rehabilitation protocol that targeted the early resolution of joint effusion, range of motion deficits, quadriceps strength impairments, and functional limitations.1 Performance-based and patient-reported data were collected from patients at 6-, 12-, and 24-month follow-ups. This study was approved by the University of Delaware’s Institutional Human Subjects Review Board. All patients provided written informed consent for participation in this study.
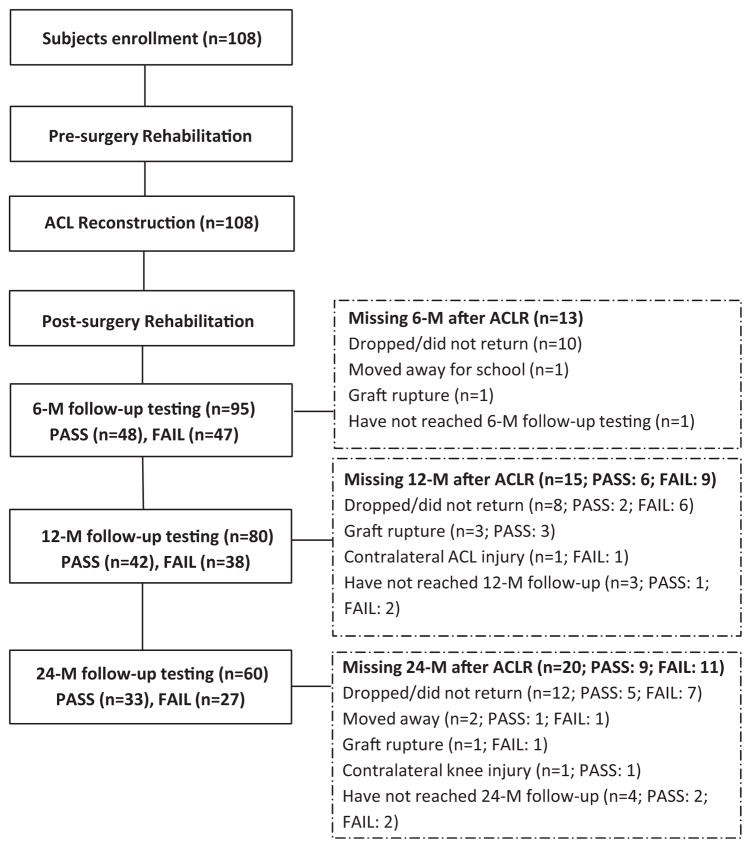
Although 108 patients were enrolled in the study, complete functional and patient-reported data were only available for 95 patients (63 men, 32 women; mean age, 27.14 ± 10.59 years) at 6 months (mean, 6.26 ± 0.81 months), 80 patients (51 men, 29 women) at 12 months (mean, 12.44 ± 1.13 months), and 60 patients (38 men, 22 women) at 24 months (mean, 25.1 ± 4.16 months) postoperatively. Data were unavailable for 13 patients at 6-month, 15 patients at 12-month, and 20 patients at 24-month follow-ups for a variety of reasons (Figure 1).
Figure 1.
Flow diagram for patient participation at 6-, 12-, and 24-month follow-ups after anterior cruciate ligament reconstruction (ACLR).
Testing
Performance-Based Measures
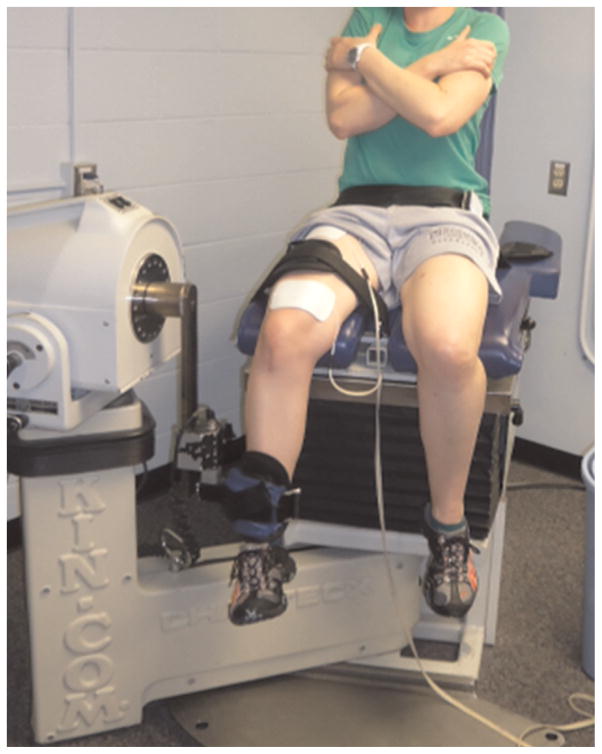
Quadriceps strength was measured using a maximal voluntary isometric contraction of the quadriceps muscle with an electromechanical dynamometer (Kin-Com; Chattanooga Group).44 Patients were seated with the hip and knee flexed to 90° with stabilization at the hip, knee, and ankle (Figure 2). Patients performed 3 practice trials before testing (2 submaximal and 1 maximal effort). During testing, patients were verbally encouraged, and real-time visual feedback from the force dynamometer was used to facilitate a maximal quadriceps muscle contraction. Testing was first completed on the uninvolved limb, followed by the involved limb, with no more than 3 tests being performed on any limb to avoid muscle fatigue. The isometric quadriceps strength index (QI) was calculated by dividing the involved quadriceps muscle force by the uninvolved quadriceps muscle force, multiplied by 100. One patient at 6 months and another patient at 24 months after ACLR did not complete quadriceps strength testing because of patellofemoral pain and a recent ankle fracture, respectively.
Figure 2.
Maximal voluntary isometric contraction with an electromechanical dynamometer.
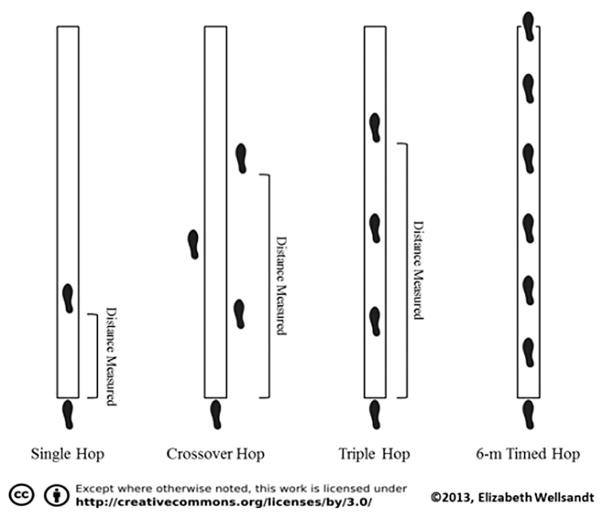
Hop performance testing was measured using a series of single-legged hop tests in the following order: single hop, crossover hop, triple hop, and 6-m timed hop (Figure 3).38 Patients were required to have full knee range of motion, have minimal knee joint effusion,21 have a QI of ≥80%, and be pain free while hopping up and down on the involved limb before performing the single-legged hop tests. All hop test data at 6 and 12 months were collected from patients wearing a functional knee brace, while 24-month hop data were collected without a brace. All patients performed 2 practice trials, followed by 2 measurement trials, of each hop test on each lower limb. Hop tests were first completed on the uninvolved limb, followed by the involved limb. Measurement trial results were included if patients maintained balance during landing without touching the ground with the uninvolved foot. Hop performance limb symmetry indices (LSIs) were calculated as the percentage of the average hop distance of the involved limb divided by the average hop distance of the uninvolved limb for each hop test, multiplied by 100. The LSI for the 6-m timed hop was calculated as the percentage of the average time of the involved limb divided by the average time of the uninvolved limb, multiplied by 100. Five patients at the 6-month, 4 patients at the 12-month, and 7 patients at the 24-month follow-ups did not complete the hop tests because of quadriceps weakness (QI <80%) or a recent lower limb injury.
Figure 3.
The 4 single-legged hop tests used in the testing sessions.
Patient-Reported Measures
After all performance-based testing, patients completed the KOS-ADLS and the GRS. The KOS-ADLS, a 14-item questionnaire, measures patients’ perceptions of knee symptoms and functional limitations related to ACLR and how these limitations affect their ability to perform activities of daily living such as walking, ascending and descending stairs, kneeling, sitting, and squatting.30 The KOS-ADLS has been shown to be a reliable, valid, and responsive measure for assessing knee functional limitations, with a high intraclass coefficient of 0.97 and with test-retest reliability.30 The KOS-ADLS scores were reported as a percentage of the patient’s score divided by the total possible score, multiplied by 100. The GRS, used to assess patients’ current knee functional performance, asks patients to rate their current knee function on a scale from 0% (inability to perform any activities) to 100% (level of knee function before injury, including sports activities). It has been reported that the analog GRS has a high test-retest intraclass coefficient of 0.96.35
Return-to-Activity Criteria
Patients were tested on RTAC at least 3 months after ACLR and when their impairments were resolved. All patients were cleared to begin gradual reintegration into their preinjury activities once they achieved at least 90% on all performance-based and patient-reported measures. Patients who achieved scores of ≥90% on all RTAC at 6-month follow-up were categorized as the pass group, and those who had scores of<90% on any RTAC were categorized as the fail group. These criteria were used to classify patients as passing or failing RTAC at 6-, 12-, and 24-month follow-up testing. In addition to completing the RTAC testing, patients were asked a yes/ no question about whether they had returned to the same preinjury activity level at the 12- and 24-month follow-ups.
Statistical Analysis
An independent t test was used to determine differences between groups for patient demographics and to compare mean differences of RTAC measures between the pass and fail groups at 6 months after ACLR. A chi-square test was used to determine significant differences between groups in terms of the female/male ratio. If the chi-square test showed a statistically significant difference in the female/ male ratio, an independent t test was used to evaluate whether the difference existed within each group or overall. Likelihood ratios (LHRs) were used to determine the relationship between patients in the pass group at 6-month follow-up and those who continued to pass at 12- and 24-month follow-ups; likewise, LHRs were used to determine the relationship between patients in the fail group at 6 months and those who continued to fail at 12 and 24 months. A 2 × 3 repeated-measures analysis of variance (ANOVA) was used to determine the relationship between groups (pass or fail) and over time (6, 12, and 24 months) for each RTAC measure. Bonferroni correction was used to adjust for multiple comparisons. Univariate ANOVA was used to determine whether the pass and fail groups demonstrated significant improvement between various follow-up time points. All data were analyzed with SPSS 20.0 (IBM Corp), with a significance level of .05 set a priori.
RESULTS
Ninety-five patients completed the 6-month, 80 patients completed the 12-month, and 60 patients completed the 24-month follow-up testing protocols (Figure 1). Six months after ACLR, there were 48 patients (50.5%) in the pass group (mean time to pass, 6.41 ± 2.69 months) and 47 patients (49.5%) in the fail group. There was no difference in age or body mass index (BMI) between patients in the pass and fail groups at 6-month follow-up (P > .05). However, the percentage of women to men was significantly different between the groups, with more men in the pass group than women (chi-square test, P = .03). Post hoc testing showed that the number of women was significantly lower in the pass group (P < .001), and the number of men was significantly higher than the number of women in the study overall (P <.001) (Table 1).
TABLE 1.
Patient Demographics and RTAC Measures for the Pass and Fail Groups at 6 Months After ACLRa
| Measure | Pass Group (n = 48) | Fail Group (n = 47) | P Value |
|---|---|---|---|
| Patients, women/men, n | 11/37 | 21/26 | .03 |
| Age, y | 26.33 ± 9.39 | 28.02 ± 11.81 | .45 |
| Body mass index, kg/m2 | 24.71 ± 3.17 | 25.32 ± 4.62 | .49 |
| Graft type, autograft/allograft, n | 19/29 | 17/30 | .431 |
| QIb | 103.02 ± 9.91 | 91.07 ± 12.09 | <.001 |
| Single-legged hop test LSIb | |||
| Single hop | 97.74 ± 4.57 | 88.10 ± 11.34 | <.001 |
| Crossover hop | 97.92 ± 4.57 | 93.71 ± 9.81 | .01 |
| Triple hop | 97.30 ± 4.53 | 92.78 ± 7.54 | .001 |
| 6-m timed hop | 99.57 ± 5.22 | 92.45 ± 8.73 | <.001 |
| KOS-ADLSb | 96.86 ± 2.81 | 97.70 ± 4.38 | .37 |
| GRSb | 94.50 ± 4.85 | 87.63 ± 12.00 | <.001 |
Data are reported as mean ± SD unless otherwise indicated. Bolded P values indicate a statistically significant difference between groups (P <.05). ACLR, anterior cruciate ligament reconstruction; GRS, global rating scale of perceived function; KOS-ADLS, Knee Outcome Survey–activities of daily living subscale; LSI, limb symmetry index; QI, isometric quadriceps strength index; RTAC, return-to-activity criteria.
Data are expressed as percentages.
At 12 months after ACLR, the rate of return to the pre-injury activity level in the pass group (81.1%; 30 patients) was significantly higher than that in the fail group (44.2%; 19 patients) (P = .002). At 24 months after ACLR, the rate of return to the preinjury activity level in the pass group (84.4%; 27 patients) was also significantly higher than that in the fail group (46.4%; 13 patients) (P = .012).
Patients in the pass group performed significantly better than those in the fail group on all measures except the KOS-ADLS (P = .37) at 6-month follow-up (Table 1). There were 15 patients who completed the 6-month but did not complete the 12-month testing protocol. When their data were compared with those who completed the 12-month testing session, there were no significant differences for sex, graft type, pass/fail ratio, age, or BMI (P > .16). However, there were significant differences in the LSIs for the crossover hop (P = .01), triple hop (P = .049), and 6-m timed hop (P = .03), with patients who did not complete the 12-month testing session demonstrating higher performance.
Likelihood Ratios
At 12-month follow-up, 80 patients completed the testing session; of these, 31 patients in the pass group at 6 months passed the RTAC again at 12 months after ACLR (Table 2). In addition, 15 patients in the fail group at 6 months passed the RTAC at 12 months after ACLR. Table 3 summarizes the reasons that these 15 patients failed at 6-month follow-up. In comparison, 23 patients in the fail group at the 6-month time point failed again at 12 months, and 11 patients who passed at 6 months failed at 12 months (Table 2). The reasons for failure in these 11 patients at 12 months after ACLR are indicated in Table 4.
TABLE 2.
Number of Patients Who Passed and Failed RTAC at 6 and 12 Months After ACLRa
| Passed at 12 mo | Failed at 12 mo | Total | |
|---|---|---|---|
| Passed at 6 mo | 31 | 11 | 42 |
| Failed at 6 mo | 15 | 23 | 38 |
| Total | 46 | 34 | 80 |
ACLR, anterior cruciate ligament reconstruction; RTAC, return-to-activity criteria.
TABLE 3.
Reasons for Failing RTAC in Patients Who Failed at 6 Months and Then Passed at 12 Monthsa
| Reason for Failing RTAC at 6 mo | No. of Patients |
|---|---|
| Scored <90% on QI | 6 |
| Scored <90% on QI and all hop LSIs | 2 |
| Scored <90% on all hop LSIs | 1 |
| Scored <90% on single hop, triple hop, and 6-m timed hop LSIs | 1 |
| Scored <90% on single hop and crossover hop LSIs | 2 |
| Scored <90% on single hop LSI and QI | 1 |
| Scored <90% on single hop LSI | 1 |
| Scored <90% on GRS | 1 |
| Total | 15 |
GRS, global rating scale of perceived function; LSI, limb symmetry index; QI, isometric quadriceps strength index; RTAC, return-to-activity criteria.
TABLE 4.
Reasons for Failing RTAC in Patients Who Passed at 6 Months and Then Failed at 12 Monthsa
| Reason for Failing RTAC at 12 mo | No. of Patients |
|---|---|
| Scored <90% on QI | 5 |
| Scored <90% on single hop, crossover hop, and triple hop LSIs | 2 |
| Scored <90% on single hop and crossover hop LSIs | 1 |
| Scored <90% on triple hop LSI and KOS-ADLS | 1 |
| Scored <90% on single hop LSI | 1 |
| Scored <90% on GRS | 1 |
| Total | 11 |
GRS, global rating scale of perceived function; KOS-ADLS, Knee Outcome Survey–activities of daily living subscale; LSI, limb symmetry index; QI, isometric quadriceps strength index; RTAC, return-to-activity criteria.
Sixty patients completed follow-up testing at the 24-month follow-up. Of these, 25 patients in the pass group at 6 months passed again at 24 months, and 14 patients in the fail group at 6 months passed at 24 months (Table 5). The reasons for failure in these 14 patients are indicated in Table 6. In comparison, 13 patients who failed at 6 months failed again at 24 months, and 8 patients who passed at 6 months failed at 24 months (Table 5). Table 7 shows the reasons that these 8 patients failed at 24-month follow-up.
TABLE 5.
Number of Patients Who Passed and Failed RTAC at 6 and 24 Months After ACLRa
| Passed at 24 mo | Failed at 24 mo | Total | |
|---|---|---|---|
| Passed at 6 mo | 25 | 8 | 33 |
| Failed at 6 mo | 14 | 13 | 27 |
| Total | 39 | 21 | 60 |
ACLR, anterior cruciate ligament reconstruction; RTAC, return-to-activity criteria.
TABLE 6.
Reasons for Failing RTAC in Patients Who Failed at 6 Months and Then Passed at 24 Monthsa
| Reason for Failing RTAC at 6 mo | No. of Patients |
|---|---|
| Scored <90% on QI | 5 |
| Scored <90% on QI and all hop LSIs | 1 |
| Scored <90% on all hop LSIs | 1 |
| Scored <90% on QI and 6-m timed hop LSI | 1 |
| Scored <90% on QI and crossover hop LSI | 1 |
| Scored <90% on single hop and crossover hop LSIs | 1 |
| Scored <90% on single hop LSI | 2 |
| Scored <90% on GRS | 2 |
| Total | 14 |
GRS, global rating scale of perceived function; LSI, limb symmetry index; QI, isometric quadriceps strength index; RTAC, return-to-activity criteria.
TABLE 7.
Reasons for Failing RTAC in Patients Who Passed at 6 Months and Then Failed at 24 Monthsa
| Reason for Failing RTAC at 24 mo | No. of Patients |
|---|---|
| Scored <90% on QI | 3 |
| Scored <90% on QI and crossover hop LSI | 1 |
| Ankle fracture | 1 |
| ACL retear | 1 |
| Medial knee pain | 1 |
| Knee instability and joint effusion | 1 |
| Total | 8 |
ACL, anterior cruciate ligament; LSI, limb symmetry index; QI, isometric quadriceps strength index; RTAC, return-to-activity criteria.
The positive LHRs for patients who passed RTAC at 6 months after ACLR to pass again at 12 and 24 months were 2.08 and 1.68, respectively, and the negative LHRs for those who failed RTAC at 6 months to fail again at 12 and 24 months were 2.07 and 1.72, respectively (P < .05) (Tables 2 and 5). The positive LHRs for patients who failed at 6 months to pass at 12 and 24 months were 0.48 and 0.59, respectively (P < .05), and the negative LHRs for those who passed at 6 months to fail at 12 and 24 months were 0.48 and 0.57, respectively (P <.05).
Functional Performance Changes Over Time
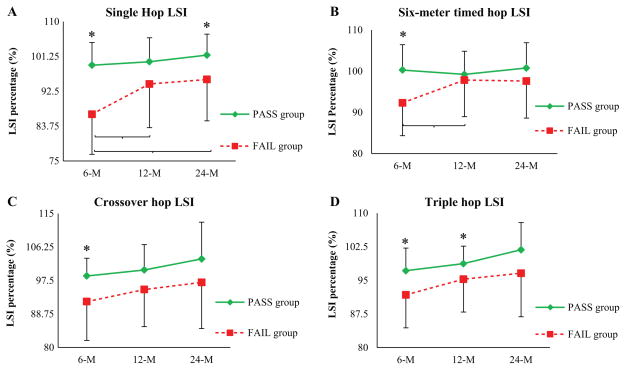
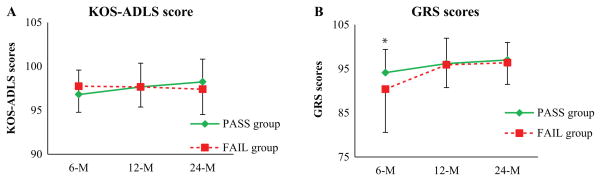
The pass group scored higher than the fail group on all outcome measures at all follow-up testing sessions after ACLR, with the exception of the KOS-ADLS in which both groups had similar scores at all follow-up testing sessions. A significant group × time interaction was found for the single hop (P = .006) and 6-m timed hop (P = .037) LSIs, with the fail group demonstrating a larger improvement specifically between the 6- and 12-month follow-ups compared with the pass group. A significant main effect of group was detected for the QI and the crossover hop and triple hop LSIs (P < .01). A main effect of time was detected for the crossover hop LSI, triple hop LSI, and GRS (P <.05).
Performance-Based Measures
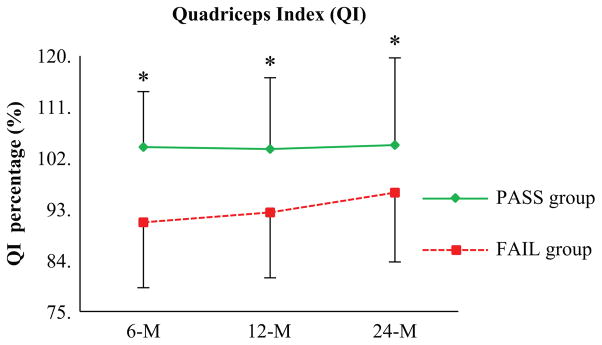
Isometric Quadriceps Strength Index
A significant main effect of group was found for the QI (P<.01). The QI was significantly different between the groups at 6 (P < .001), 12 (P <.001), and 24 months (P = .04) after ACLR (Figure 4).
Figure 4.
Mean isometric quadriceps strength index (QI) of the pass and fail groups at 6, 12, and 24 months postoperatively. Error bars indicate SD. *Significant difference between groups (P <.05).
Hop Performance LSI
A significant group × time interaction was found for the single hop (P = .006) and 6-m timed hop (P = .037) LSIs (Figure 5, A and B). In addition, a significant main effect of group and main effect of time were found for the crossover hop LSI (P <.05). The crossover hop LSI was significantly different between the pass and fail groups only at 6-month follow-up (P = .01). Both the pass and fail groups significantly improved their crossover hop LSI over time (P <.05) (Figure 5C). A significant main effect of group and main effect of time were found for the triple hop LSI (P <.05). The triple hop LSI was significantly different between the groups at 6 months (P = .001) and 12 months (P = .02) after ACLR. Both groups significantly improved in the triple hop LSI over time (P < .05) (Figure 5D).
Figure 5.
Mean single-legged hop limb symmetry indices (LSIs) of the pass and fail groups at 6, 12, and 24 months postoperatively. Error bars indicate SD. *Significant difference between groups (P <.05).
Patient-Reported Measures
Both the pass and fail groups had similar scores on the KOS-ADLS at all follow-up testing times (P > .05). Neither group improved their KOS-ADLS scores significantly between the follow-up times (P > .05) (Figure 6A).
Figure 6.
Mean patient-reported outcome scores for the pass and fail groups at 6, 12, and 24 months postoperatively. Error bars indicate SD. *Significant difference between groups (P <.05). GRS, global rating scale of perceived function; KOS-ADLS, Knee Outcome Survey–activities of daily living subscale.
A main effect of time was detected for the GRS (P <.05). The GRS was significantly different between the pass and fail groups only at 6-month follow-up (P < .001). The GRS score improved significantly in the fail group between 6 and 12 months (P = .04) and between 6 and 24 months (P = .01), while in the pass group, it improved significantly between 6 and 24 months after ACLR (P = .03) (Figure 6B). The greatest improvement in the GRS score in the fail group was achieved between the 6- and 12-month follow-ups.
DISCUSSION
The purpose of this study was to investigate performance-based and patient-reported measures at 12 and 24 months after ACLR between patients who passed or failed the RTAC at 6 months and to further investigate how their functional performance and patient-reported measures changed over time. The rate of returning to the preinjury activity level at 12 and 24 months after surgery was higher in the pass group. More than half of the patients in the fail group did not return to their preinjury activity level because of residual functional deficits. However, almost one-half of the patients in the fail group participated in preinjury activities at 12 and 24 months after ACLR by their own choice, without being cleared by their therapists. This may have, in part, influenced the results of this study and affected the effectiveness of the RTAC to identify those who can return to their preinjury activity level after ACLR based on their functional performance. The results of this study show that the pass group achieved higher knee performance-based and patient-reported scores early after ACLR compared with the fail group and continued to maintain higher knee function up to 24-month follow-up. Patients in the fail group improved their outcomes between the 6- and 12-month follow-up testing sessions and continued to improve at the 24-month follow-up session.
The results of this study indicate that about 81% and 84% of patients who passed the RTAC at 6 months after ACLR returned to their preinjury activity level at 12 and 24 months after ACLR. These rates are higher than what has been reported by other studies,5,8 and they most likely result from using robust RTAC to determine patients’ readiness to return to preinjury activity levels. Our RTAC were able to identify about 55% of those patients with poor functional performance who failed the testing sessions and did not return to their preinjury activity level. About 45% of the fail group reported that they had returned to the same preinjury activity level at both 12 and 24 months after surgery; however, these patients were not cleared to return by their rehabilitation team. Additionally, these patients were instructed to participate in a training program for 4 to 5 weeks to address their functional deficits and to be scheduled for another RTAC testing session. However, they chose to return to activities on their own volition. This development may highlight how important returning to preinjury activities is for patients after ACLR. Those patients who failed the RTAC and returned to participate at the same preinjury activity level may have a higher risk for secondary injuries. A recent study reported that athletes who returned to professional sports without meeting a set of clinical discharge criteria possess a 4-times greater risk of ACL graft ruptures compared with those who met all the criteria.26,32
Our strict RTAC of passing all 7 performance-based and patient-reported measures were used to evaluate patients’ self-reported knee function and limb-to-limb movement symmetry. At 6-month follow-up, only half of the patients demonstrated normal quadriceps strength and hop performance LSIs and scored ≥90% on patient-reported measures. The total percentage of patients who passed RTAC at 6 months increased at both 12 and 24 months, and patients in the pass group at 6 months were 2 times more likely to pass again at 12 and 24 months compared with those in the fail group. In comparison, the total percentage of patients who failed RTAC at 6 months after surgery continued to be within the same range at 12 and 24 months. Patients in the fail group at 6 months were 2.07 and 1.72 times more likely to fail again at 12 and 24 months, respectively, compared with those in the pass group. The results of this study reveal that patients demonstrating normal quadriceps strength and hop limb-to-limb symmetry as well as good self-reported knee function at 6 months after ACLR are more likely to exhibit normal functional performance-based and patient-reported knee function at 12 and 24 months. By comparison, patients demonstrating quadriceps strength deficits, hop limb-to-limb asymmetry, and poor self-reported knee function at 6 months after surgery are more likely to demonstrate similar performance-based and self-reported knee function at 12 and 24 months. Previous studies by Di Stasi and colleagues16 and Hartigan and colleagues27 reported similar results to our study, with nearly half of the patients passing RTAC at 6 months postoperatively. A study by Logerstedt and colleagues34 indicated that patients improved between baseline and 6-month follow-up after ACLR and continued to improve from 6 to 12 months after surgery; however, the authors only reported the percentage of patients who achieved ≥90% on individual outcome measures and not as collective criteria.
Patients who still demonstrate limb-to-limb asymmetry after ACLR are a main concern to clinicians, as they may have a lower likelihood to return to their preinjury activity level and may be at a higher risk for secondary ACL injuries.40 This study’s results highlight the usefulness of the RTAC in identifying patients who are more susceptible to persistent, poor knee function and limb-to-limb asymmetry postoperatively and compel clinicians to consider individualized, extended treatment programs.
The results of this study showed that the fail group improved their functional performance on several outcome measures. This improvement, however, did not result in all patients passing RTAC measures, as 60.5% (23/38) and 48.1% (13/27) of patients continued to fail again on the criteria at 12 and 24 months, respectively. In contrast, a select number of patients who failed the RTAC at 6 months were able to pass at 12 and 24 months after surgery. Patients who failed RTAC at 6 months after surgery were 0.48 and 0.59 times more likely to pass at 12 and 24 months, respectively, compared with those who passed at 6 months after surgery. These results suggest that patients who failed the RTAC at 6 months after ACLR are 50% more likely to pass the RTAC by restoring normal knee functional performance and limb-to-limb movement symmetry at 12 and 24 months after ACLR compared with those who passed at 6 months after surgery. Many of the patients who failed at the 6-month time point scored <90% on 1 or 2 RTAC measures. In fact, the majority of patients passed the RTAC at 12 and 24 months postoperatively because of improvement in quadriceps strength. Therefore, these patients had a high potential to pass the RTAC, especially if they continued to participate in an extended training program.
Disappointingly, the study also showed that patients who passed the RTAC at 6 months were 0.48 and 0.57 times more likely to fail at 12 or 24 months, respectively. Those who failed the RTAC demonstrated a quadriceps strength deficit in the involved limb of >10% compared with the uninvolved limb. Underlying quadriceps strength deficits in the reconstructed limb may contribute to poor hop performance, as patients with quadriceps weakness hop more slowly and for shorter distances on hop tests. Additionally, patients may have failed the RTAC at the 12- and 24-month time points because of poor functional performance on hop tests, recent lower extremity injuries, or low scores on patient-reported measures (mainly the GRS). These patients may have failed the RTAC at the 12- and 24-month sessions because they chose to stop participation in functional or sports activities. The results of this study showed that about 20% and 15% of the patients who passed RTAC did not return to the same preinjury activity level at 12 and 24 months after ACLR, respectively. Patients may have also failed the RTAC because of changes in lifestyle, less opportunity to participate in activities, or fear of sustaining further injuries.17,29
Additionally, the study population included mainly students who may have graduated or moved to another school or for work. These factors may have affected the reported rates of return to the preinjury activity level among groups and the ability to evaluate the effectiveness of the RTAC in identifying those patients who can return to their preinjury activity level after ACLR. A lack of confidence in the knee joint, being psychologically unready, and a fear of reinjuries have been reported as factors for not returning to the preinjury activity level.3,4 These factors may also account for the poor functional performance during functional testing. Our RTAC, however, do not account for psychological readiness and fear of reinjuries during the decision-making process to determine patients’ readiness to return to their preinjury activity level. Future studies may account for the psychological aspects of injuries and reconstruction surgery as part of the RTAC.
The data in this study were reported for both the pass and fail groups using the group means but not the individual score of each patient on each RTAC measure. Therefore, while the reported group means are ≥90% on ≥1 RTAC measure, this does not necessarily indicate that the patients in the fail group passed RTAC. In this study, patients were classified in the fail group if they scored <90% on any one of the RTAC measures. Quadriceps strength deficits and single-legged hop performance limb-to-limb asymmetries are prevalent after an ACL injury and can persist after ACLR.7,40
The presence of limb-to-limb asymmetry after ACLR can affect lower extremity performance, especially during participation in vigorous activities such as competitive interactions with opponents and being in less controlled environments.7,19,40 Consequently, limb-to-limb asymmetry may predispose patients to reinjuries and lead to the initiation and progression of osteoarthritis in the knee joint.37,40 Kinematic and kinetic asymmetries are linked to the development of knee osteoarthritis and predisposed factors for a second ACL injury.2,40 Patients with limb-to-limb asymmetry may overuse the uninjured limb, resulting in overuse injuries to that limb, or may underuse the injured limb because of a lack of confidence.2 Further work is needed to evaluate whether patients who fail RTAC and who demonstrate poor knee function and limb movement asymmetry will have a higher incidence of second ACL injuries in the short and long term after reconstruction surgery compared with those with normal knee function and limb movement symmetry. Additional studies are needed to determine whether patients who fail RTAC will develop radiological signs of knee osteoarthritis after ACLR compared with patients with normal knee function and movement symmetry.
A significant group × time interaction was only found for the single hop and 6-m timed hop LSIs; however, patients in both the pass and fail groups improved in quadriceps strength, crossover hop and triple hop LSIs, and the GRS score over time. The improvements between 6-, 12-, and 24-month follow-ups most likely resulted from patient participation in both functional and athletic activities that included repetitive running, jumping, landing, and turning movements. By contrast, results of the KOS-ADLS show that patients in both groups did not change over time; this is not surprising in light of the KOS-ADLS asking about basic daily living activities performed by most patients without difficulty at the time of follow-up testing.
A pattern of improvement on some outcome measures was seen for the fail group after ACLR; the majority of those patients achieved the greatest improvement between the 6- and 12-month follow-ups. This improvement can be explained by the fact that patients in the fail group initially scored lower on performance-based tests and patient-reported knee function measures at 6 months postoperatively. Therefore, they had more potential for improvement compared with patients in the pass group, who did not show nearly the degree of improvement as a result of less room for improvement on outcome measures of interest. A study using the same RTAC after ACLR reported that 50% of athletes demonstrated normal knee function and limb movement symmetry on RTAC at 6 months and more than 75% at 1 year after ACLR.27
Returning to the preinjury activity level is multifactorial.8 Therefore, the decision to determine patients’ readiness to return to preinjury activities was based on their performance on a comprehensive set of RTAC that required a modest time commitment from the therapists and patients. The RTAC included multiple measures that are able to assess different aspects of knee function and physical performance. Logerstedt and colleagues33 used the IKDC 2000 as a simple and quick tool to discriminate between those who passed and failed the same RTAC after ACLR. The findings of the Logerstedt et al33 study revealed that scoring low on the IKDC 2000 is an indication of failing the RTAC. However, scoring high on the IKDC 2000 does not indicate passing the RTAC.29 Patients who score high on the IKDC can be tested with the RTAC to determine their functional deficits. Furthermore, this can help modify the rehabilitation program to provide an appropriate intervention to address functional deficits. This may highlight the importance of using comprehensive criteria to determine patients’ readiness to return to preinjury activities. The comprehensiveness of the RTAC provides clinicians with crucial information about patients’ impairments and functional deficits. The results of the current study show that most of the patients from the fail group failed the RTAC because they demonstrated quadriceps strength weakness and poor performance on the single hop test. Quadriceps weakness is a major impairment after ACLR, affecting patient performance during functional activities.27,31 Failing the single hop might be related to the order of the single-legged hop tests instead of only the challenge of the test itself. In the current study, we started testing the patients’ hop performance with the single hop. Therefore, administering the single hop as the first hop test might have affected the performance of the patients. Patients may have performed poorly on the single hop because they felt anxiety or lacked confidence with hopping on the reconstructed limb. The single-legged hop tests have been used as screening tests to discriminate patients with dynamic knee stability from those with dynamic knee instability early after an ACL injury for non-surgical management.18,23 Eastlack and colleagues18 reported that the crossover hop was the only predictive measure of the single-legged hop tests that discriminated patients with dynamic knee stability from those with dynamic knee instability after an acute ACL injury. Despite this finding, these authors suggested that all 4 hop tests be performed as part of the screening, as the order of performing the hop tests may have an effect on which of the tests might be the predictive measure.18
The results of the current study identify those measures that patients continue to fail after ACLR. This, in turn, helps clinicians to address these patients’ functional limitations by providing an appropriate intervention. In light of our study results, those patients planning to return to their preinjury activities but who fail to restore limb-to-limb symmetry might need to participate in an extended rehabilitation program. Clinicians might consider the administration of an extended training program that includes intensive quadriceps strengthening, agility drills, and plyometric training to ensure the restoration of limb-to-limb symmetry before reintegration into vigorous activities. If, however, patients still exhibit limb-to-limb asymmetry after participating in an extended rehabilitation program, they might need to be advised to change from or modify their activities to less high-risk activities.
Our RTAC were developed to assess patients’ dynamic knee stability, as knee instability is a major issue after an ACL injury and ACLR. The RTAC also were developed to assess the presence of impairments and functional deficits that are commonly reported after ACLR such as quadriceps weakness, functional performance deficits, aberrant biomechanics, and neuromuscular dysfunction.15,27,31,34,41 Our RTAC encompass both performance-based and patient-reported measures that provide testing conditions that replicate the demand of sports activities. Therefore, the criteria permit us to assess limb-to-limb movement symmetry and capture any functional deficits that need to be addressed by providing an appropriate intervention. Some of these criteria were used as part of the decision-making process to select potential candidates for nonsurgical management after ACL ruptures.23 Additionally, these same RTAC were effective measures to identify those athletes who successfully returned to high-level activities after ACL injuries without undergoing reconstruction surgery.21 The proposed cutoff values to determine normal functional performance and limb-to-limb symmetry range from 70% to 90%.10,24,42 A 90% cutoff value was used for our criteria to ensure that the patients achieved normal functional performance and limb-to-limb symmetry and that they were not favoring one limb over the other. Based on the work of Fitzgerald and colleagues,21 all successful patients who returned to high-level activities with no reconstruction surgery scored, on average, ≥90% on the RTAC measures.
Although we used the time basis approach in the study design for follow-up testing, which is a limitation of the study, the group factor used in the analysis was based on classifying the patients on a criterion basis (ie, pass and fail). Therefore, the results of this study suggest testing patients on an individual basis using performance-based and patient-reported measures rather than using only time-based criteria as a guideline to determine patients’ readiness to return to preinjury activities. In addition, testing patients on a regular basis using a battery of tests after rehabilitation is seen to be a preferred method to assess knee functional performance and limb-to-limb movement symmetry and to identify patients with a high risk for further knee injuries.
Limitations
The study population was limited to patients who had participated in IKDC level 1 or 2 sports activities and underwent ACLR. Therefore, these findings cannot be generalized to patients participating in less demanding activities or to those with an ACL rupture who chose to be managed nonoperatively. In this study, we used the 6-month time point after ACLR as baseline testing instead of using time to pass the RTAC, with the reason being that passing RTAC varied among patients. In addition, there were patients who dropped out from the study and did not return to the follow-up testing sessions. Some of the patients dropped out from the study because of scholastic transition, as a majority of the study’s population were college students who moved away after finishing college or for work. College students represented a large percentage of the eligible patients in this study, and this may have caused transfer bias. Therefore, we cannot determine, based on the data of this study, whether those patients who were followed up are representative of those who were not. Additional reasons were related to changes in lifestyle, lower opportunity to participate in activities, fear of sustaining another knee injury, or socioeconomic status.7 In this study, few patients sustained either graft tears or other lower extremity injuries. Additionally, while patients who failed the RTAC were advised not to return to their preinjury activity level until they resolved their functional deficits, a large number of patients in the fail group did return to participate in the same preinjury activity level at 12 and 24 months after ACLR by their own choice. This in turn may have, at least in part, affected the rates of return to the same preinjury activity level between the groups.
CONCLUSION
The findings of this study revealed that patients who passed the RTAC early after ACLR were more likely to demonstrate normal knee function and movement symmetry at 12 and 24 months after ACLR. In comparison, patients who failed the RTAC at 6 months after ACLR were more likely to demonstrate impaired knee function and limb-to-limb movement asymmetry at 12 and 24 months after ACLR. Additionally, up to 81% and 84% of patients who passed the RTAC returned to the same preinjury activity level at 12- and 24-month follow-ups, respectively. More than half of the patients who failed the RTAC did not return to the same preinjury activity level at 12 and 24 months after ACLR. A group of patients who failed the RTAC chose to return to their preinjury activities, even though they were functionally not ready. The majority of the patients in the fail group did improve knee performance, limb-to-limb symmetry, and patient-reported measures during the first year after ACLR. Although a subgroup of the fail group passed RTAC testing, this improvement did not allow some to pass. Using a battery of RTAC that include performance-based and patient-reported measures can help to identify patients with limb-to-limb asymmetry and therefore could be utilized in a rehabilitation setting to identify these persistent dysfunctions.
Acknowledgments
The authors thank the University of Delaware Physical Therapy Clinic for assistance in this study’s patient management and data collection. They also thank Martha Callahan for research coordination.
Footnotes
One or more of the authors has declared the following potential conflict of interest or source of funding: This ongoing prospective cohort study was funded by the National Institutes of Health (NIH R37HD37985, P30 GM103333) and a Promotion of Doctoral Studies (PODS) I Scholarship.
References
- 1.Adams D, Logerstedt DS, Hunter-Giordano A, Axe MJ, Snyder-Mackler L. Current concepts for anterior cruciate ligament reconstruction: a criterion-based rehabilitation progression. J Orthop Sports Phys Ther. 2012;42(7):601–614. doi: 10.2519/jospt.2012.3871. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Andriacchi TP, Mündermann A, Smith RL, Alexander EJ, Dyrby CO, Koo S. A framework for the in vivo pathomechanics of osteoarthritis at the knee. Ann Biomed Eng. 2004;32(3):447–457. doi: 10.1023/b:abme.0000017541.82498.37. [DOI] [PubMed] [Google Scholar]
- 3.Ardern CL. Anterior cruciate ligament reconstruction: not exactly a one-way ticket back to the preinjury level. A review of contextual factors affecting return to sport after surgery. Sports Health. 2015;7(3):224–230. doi: 10.1177/1941738115578131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ardern CL, Osterberg A, Tagesson S, et al. The impact of psychological readiness to return to sport and recreational activities after anterior cruciate ligament reconstruction. Br J Sports Med. 2014;48(22):1613–1619. doi: 10.1136/bjsports-2014-093842. [DOI] [PubMed] [Google Scholar]
- 5.Ardern CL, Taylor NF, Feller JA, Webster KE. Fifty-five per cent return to competitive sport following anterior cruciate ligament reconstruction surgery: an updated systematic review and meta-analysis including aspects of physical functioning and contextual factors. Br J Sports Med. 2014;48(21):1543–1552. doi: 10.1136/bjsports-2013-093398. [DOI] [PubMed] [Google Scholar]
- 6.Ardern CL, Taylor NF, Feller JA, Webster KE. Return-to-sport outcomes at 2 to 7 years after anterior cruciate ligament reconstruction surgery. Am J Sports Med. 2012;40(1):41–48. doi: 10.1177/0363546511422999. [DOI] [PubMed] [Google Scholar]
- 7.Ardern CL, Taylor NF, Feller JA, Webster KE. A systematic review of the psychological factors associated with returning to sport following injury. Br J Sports Med. 2013;47(17):1120–1126. doi: 10.1136/bjsports-2012-091203. [DOI] [PubMed] [Google Scholar]
- 8.Ardern CL, Webster KE, Taylor NF, Feller JA. Return to the preinjury level of competitive sport after anterior cruciate ligament reconstruction surgery: two-thirds of patients have not returned by 12 months after surgery. Am J Sports Med. 2011;39(3):538–543. doi: 10.1177/0363546510384798. [DOI] [PubMed] [Google Scholar]
- 9.Barber-Westin SD, Noyes FR. Factors used to determine return to unrestricted sports activities after anterior cruciate ligament reconstruction. Arthroscopy. 2011;27(12):1697–1705. doi: 10.1016/j.arthro.2011.09.009. [DOI] [PubMed] [Google Scholar]
- 10.Barton CJ, Webster KE, Menz HB. Evaluation of the scope and quality of systematic reviews on nonpharmacological conservative treatment for patellofemoral pain syndrome. J Orthop Sports Phys Ther. 2008;38(9):529–541. doi: 10.2519/jospt.2008.2861. [DOI] [PubMed] [Google Scholar]
- 11.Beynnon BD, Johnson RJ, Abate JA, et al. Treatment of anterior cruciate ligament injuries, part 2. Am J Sports Med. 2005;33(11):1579–1602. doi: 10.1177/0363546505279913. [DOI] [PubMed] [Google Scholar]
- 12.Biau DJ, Tournoux C, Katsahian S, Schranz P, Nizard R. ACL reconstruction: a meta-analysis of functional scores. Clin Orthop Relat Res. 2007;458:180–187. doi: 10.1097/BLO.0b013e31803dcd6b. [DOI] [PubMed] [Google Scholar]
- 13.Daniel DM, Stone ML, Dobson BE, Fithian DC, Rossman DJ, Kaufman KR. Fate of the ACL-injured patient: a prospective outcome study. Am J Sports Med. 1993;22(5):632–644. doi: 10.1177/036354659402200511. [DOI] [PubMed] [Google Scholar]
- 14.Daniel DM, Stone ML, Sachs R, Malcom L. Instrumented measurement of anterior knee laxity in patients with acute anterior cruciate ligament disruption. Am J Sports Med. 1985;13(6):401–407. doi: 10.1177/036354658501300607. [DOI] [PubMed] [Google Scholar]
- 15.de Jong SN, van Caspel DR, van Haeff MJ, Saris DBF. Functional assessment and muscle strength before and after reconstruction of chronic anterior cruciate ligament lesions. Arthroscopy. 2007;23(1):21–28. 28.e1–e3. doi: 10.1016/j.arthro.2006.08.024. [DOI] [PubMed] [Google Scholar]
- 16.Di Stasi SL, Logerstedt D, Gardinier ES, Snyder-Mackler L. Gait patterns differ between ACL-reconstructed athletes who pass return-to-sport criteria and those who fail. Am J Sports Med. 2013;41(6):1310–1318. doi: 10.1177/0363546513482718. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Dunn WR, Spindler KP. Predictors of activity level 2 years after anterior cruciate ligament reconstruction (ACLR): a Multicenter Orthopaedic Outcomes Network (MOON) ACLR cohort study. Am J Sports Med. 2010;38(10):2040–2050. doi: 10.1177/0363546510370280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Eastlack ME, Axe MJ, Snyder-Mackler L. Laxity, instability, and functional outcome after ACL injury: copers versus noncopers. Med Sci Sports Exerc. 1999;31:210–215. doi: 10.1097/00005768-199902000-00002. [DOI] [PubMed] [Google Scholar]
- 19.Eitzen I, Moksnes PH, Moksnes HH, et al. A progressive 5-week exercise therapy program leads to significant improvement in knee function early after anterior cruciate ligament injury. J Orthop Sports Phys Ther. 2010;40(2):705–721. doi: 10.2519/jospt.2010.3345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Feller JA, Webster KE. A randomized comparison of patellar tendon and hamstring tendon anterior cruciate ligament reconstruction. Am J Sports Med. 2003;31(4):564–573. doi: 10.1177/03635465030310041501. [DOI] [PubMed] [Google Scholar]
- 21.Fitzgerald GK, Axe MJ, Snyder-Mackler L. A decision-making scheme for returning patients to high-level activity with nonoperative treatment after anterior cruciate ligament rupture. Knee Surg Sports Traumatol Arthrosc. 2000;8(2):76–82. doi: 10.1007/s001670050190. [DOI] [PubMed] [Google Scholar]
- 22.Fitzgerald GK, Axe MJ, Snyder-Mackler L. The efficacy of perturbation training in nonoperative anterior cruciate ligament rehabilitation programs for physical active individuals. Phys Ther. 2000;80(2):128–140. [PubMed] [Google Scholar]
- 23.Fitzgerald GK, Axe MJ, Snyder-Mackler L. Proposed practice guidelines for non operative anterior cruciate ligament rehabilitation of physically active individuals. J Orthop Sports Phys Ther. 2000;30:194–203. doi: 10.2519/jospt.2000.30.4.194. [DOI] [PubMed] [Google Scholar]
- 24.Gobbi A, Diara A, Mahajan S, Zanazzo M, Tuy B. Patellar tendon anterior cruciate ligament reconstruction with conical press-fit femoral fixation: 5-year results in athletes population. Knee Surg Sports Traumatol Arthrosc. 2002;10(2):73–79. doi: 10.1007/s00167-001-0265-8. [DOI] [PubMed] [Google Scholar]
- 25.Griffin LY, Agel J, Albohm MJ, et al. Noncontact anterior cruciate ligament injuries: risk factors and prevention strategies. J Am Acad Orthop Surg. 2000;8:141–150. doi: 10.5435/00124635-200005000-00001. [DOI] [PubMed] [Google Scholar]
- 26.Grindem H, Snyder-Mackler L, Moksnes H, Engebretsen L, Risberg MA. Simple decision rules can reduce reinjury risk by 84% after ACL reconstruction: the Delaware-Oslo ACL cohort study. Br J Sports Med. 2016;50(13):804–808. doi: 10.1136/bjsports-2016-096031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Hartigan EH, Axe MJ, Snyder-Mackler L. Time line for noncopers to pass return-to-sports criteria after anterior cruciate ligament reconstruction. J Orthop Sports Phys Ther. 2010;40(3):141–154. doi: 10.2519/jospt.2010.3168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Hefti E, Müller W, Jakob RP, Stäubli HU. Evaluation of knee ligament injuries with the IKDC form. Knee Surg Sports Traumatol Arthrosc. 1993;1(3–4):226–234. doi: 10.1007/BF01560215. [DOI] [PubMed] [Google Scholar]
- 29.Hopper DM, Strauss GR, Boyle JJ, et al. Functional recovery after anterior cruciate ligament reconstruction: a longitudinal perspective. Arch Phys Med Rehabil. 2008;89(8):1535–1541. doi: 10.1016/j.apmr.2007.11.057. [DOI] [PubMed] [Google Scholar]
- 30.Irrgang JJ, Snyder-Mackler L, Wainner RS, Fu FH, Harner CD. Development of a patient-reported measure of function of the knee. J Bone Joint Surg Am. 1998;80(8):1132–1145. doi: 10.2106/00004623-199808000-00006. [DOI] [PubMed] [Google Scholar]
- 31.Keays SL, Bullock-Saxton J, Keays AC, Newcombe P. Muscle strength and function before and after anterior cruciate ligament reconstruction using semitendonosus and gracilis. Knee. 2001;8(3):229–234. doi: 10.1016/s0968-0160(01)00099-0. [DOI] [PubMed] [Google Scholar]
- 32.Kyritsis P, Bahr R, Landreau P, Miladi R, Witvrouw E. Likelihood of ACL graft rupture: not meeting six clinical discharge criteria before return to sport is associated with a four times greater risk of rupture. Br J Sports Med. 2016;50(15):946–951. doi: 10.1136/bjsports-2015-095908. [DOI] [PubMed] [Google Scholar]
- 33.Logerstedt D, Di Stasi S, Grindem H, et al. Self-reported knee function can identify athletes who fail return-to-activity criteria up to 1 year after anterior cruciate ligament reconstruction: a Delaware-Oslo ACL Cohort Study. J Orthop Sports Phys Ther. 2014;44(12):914–923. doi: 10.2519/jospt.2014.4852. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Logerstedt D, Lynch A, Axe MJ, Snyder-Mackler L. Symmetry restoration and functional recovery before and after anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc. 2013;21(4):859–868. doi: 10.1007/s00167-012-1929-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Marx RG, Jones EC, Allen AA, et al. Reliability, validity, and responsiveness of four knee outcome scales for athletic patients. J Bone Joint Surg Am. 2001;83(10):1459–1469. doi: 10.2106/00004623-200110000-00001. [DOI] [PubMed] [Google Scholar]
- 36.Marx RG, Jones EC, Angel M, Wickiewicz TL, Warren RF. Beliefs and attitudes of members of the American Academy of Orthopaedic Surgeons regarding the treatment of anterior cruciate ligament injury. Arthroscopy. 2003;19(7):762–770. doi: 10.1016/s0749-8063(03)00398-0. [DOI] [PubMed] [Google Scholar]
- 37.Myer GD, Paterno MV, Ford KR, Quatman CE, Hewett TE. Rehabilitation after anterior cruciate ligament reconstruction: criteria-based progression through the return-to-sport phase. J Orthop Sports Phys Ther. 2006;36(6):385–402. doi: 10.2519/jospt.2006.2222. [DOI] [PubMed] [Google Scholar]
- 38.Noyes FR, Barber SD, Mangine RE. Abnormal lower limb symmetry determined by function hop tests after anterior cruciate ligament rupture. Am J Sports Med. 1991;19(5):513–518. doi: 10.1177/036354659101900518. [DOI] [PubMed] [Google Scholar]
- 39.Paterno MV, Rauh MJ, Schmitt LC, Ford KR, Hewett TE. Incidence of second ACL injuries 2 years after primary ACL reconstruction and return to sport. Am J Sports Med. 2014;42(7):1567–1573. doi: 10.1177/0363546514530088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Paterno MV, Schmitt LC, Ford KR, et al. Biomechanical measures during landing and postural stability predict second anterior cruciate ligament injury after anterior cruciate ligament reconstruction and return to sport. Am J Sports Med. 2010;38(10):1968–1978. doi: 10.1177/0363546510376053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Rudolph KS, Eastlack ME, Axe MJ, Snyder-Mackler L. 1998 Basmajian Student Award Paper. Movement patterns after anterior cruciate ligament injury: a comparison of patients who compensate well for the injury and those who require operative stabilization. J Electromyogr Kinesiol. 1998;8(6):349–362. doi: 10.1016/s1050-6411(97)00042-4. [DOI] [PubMed] [Google Scholar]
- 42.Shelbourne KD, Klotz C. What I have learned about the ACL: utilizing a progressive rehabilitation scheme to achieve total knee symmetry after anterior cruciate ligament reconstruction. J Orthop Sci. 2006;11(3):318–325. doi: 10.1007/s00776-006-1007-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Smith FW, Rosenlund EA, Aune AK, MacLean JA, Hillis SW. Subjective functional assessments and the return to competitive sport after anterior cruciate ligament reconstruction. Br J Sports Med. 2004;38(3):279–284. doi: 10.1136/bjsm.2002.001982. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Snyder-Mackler L, De Luca PF, Williams PR, et al. Reflex inhibition of the quadriceps femoris muscle after injury or reconstruction of the anterior cruciate ligament. J Bone Joint Surg Am. 1994;76(4):555–560. doi: 10.2106/00004623-199404000-00010. [DOI] [PubMed] [Google Scholar]
- 45.Spindler KP, Kuhn JE, Freedman KB, Matthews CE, Dittus RS, Harrell FE., Jr Anterior cruciate ligament reconstruction autograft choice: bone-tendon-bone versus hamstring. Does it really matter? A systematic review. Am J Sports Med. 2004;32(8):1986–1995. doi: 10.1177/0363546504271211. [DOI] [PubMed] [Google Scholar]
- 46.Yagi M, Kuroda R, Nagamune K, Yoshiya S, Kurosaka M. Double-bundle ACL reconstruction can improve rotational stability. Clin Orthop Relat Res. 2007;454:100–107. doi: 10.1097/BLO.0b013e31802ba45c. [DOI] [PubMed] [Google Scholar]