Abstract
Background
Multi-dimensional self-report measures of sexual function for women do not include assessment of vulvar discomfort, limiting our understanding of its prevalence. In an effort to improve the measurement of patient-reported health, the National Institutes of Health funded creation of the Patient Reported Outcomes Measurement Information System® (PROMIS®). This included development of the PROMIS® Sexual Function and Satisfaction (SexFS) measure, and version 2.0 of the SexFS included two scales to measure vulvar discomfort with sexual activity.
Objectives
To describe the development of two self-reported measures of vulvar discomfort with sexual activity, describe the relationships between these scales and scales for lubrication and vaginal discomfort, and report the prevalence of vulvar discomfort with sexual activity in a large, nationally-representative sample of US women.
Study Design
We followed PROMIS measure development standards, including qualitative development work with patients and clinicians and psychometric evaluation of candidate items based on item response theory in a probability sample of 1686 English-speaking US adult women. We tested 16 candidate items on vulvar discomfort. We present descriptive statistics for these items, correlation coefficients among the vulvar and vaginal scales, and mean PROMIS scores with 95% confidence intervals separately by menopausal status for the 1046 women who reported sexual activity in the past 30 days.
Results
Based on the psychometric evaluation of the candidate items, we created two 4-item scales, one to measure labial discomfort and pain and one to measure clitoral discomfort and pain. Additional items not included in the scales assess pain quality, numbness, and bleeding. The correlations between the lubrication, vaginal discomfort, and the two vulvar discomfort measures ranged from 0.46 to 0.77, suggesting that these measures represent related yet distinct concepts. In our nationally representative sample, 1 in 5 US women endorsed some degree of vulvar discomfort with sexual activity in the past 30 days. Menopausal status was associated with lower lubrication and higher vaginal discomfort but not with vulvar discomfort.
Conclusion
The PROMIS Vulvar Discomfort with Sexual Activity–Labial and Vulvar Discomfort with Sexual Activity–Clitoral scales are publically available for use in research and clinical settings. There is limited overlap between vulvar discomfort and lubrication or vaginal discomfort. The importance of measuring vulvar discomfort as part of a comprehensive assessment of sexual function is underscored by its prevalence.
INTRODUCTION
Diagnosis and treatment of dyspareunia require the gynecologist or other health care provider to localize the patient’s discomfort and to determine its etiology. Whereas dyspareunia typically involves introital and deeper vaginal pain, clinical insight suggests that some women also complain of vulvar pain or discomfort. Vulvar pain terminology has evolved over time, and an updated expert consensus on classification of persistent pain (vulvodynia) was recently published.1 Research has explored correlates and causes of vulvar pain,2, 3 for example, dermatoses,4-6 and, in women with cancer, iatrogenic conditions including radiation changes, lymphedema, and estrogen suppression.7 Regardless of the cause, it is important to consider the role that vulvar discomfort plays in women’s experiences of sexual activity.
The most commonly used multi-dimensional patient-reported outcome measures of sexual function for women do not include specific references to the vulva. This gap in assessment limits the ability to understand women’s experiences with vulvar discomfort or pain during sexual activity. Likewise, the prevalence of vulvar discomfort with sexual activity in the US general population is unknown. In this manuscript, first we provide details about two new measures of vulvar discomfort and pain that are part of the Patient-Reported Outcomes Measurement Information System® Sexual Function and Satisfaction measure version 2.0 (PROMIS® SexFS v2). Second, we describe the relationships between these vulvar discomfort scales and the PROMIS scales for lubrication and vaginal discomfort. Finally, we report the prevalence of vulvar discomfort or pain with sexual activity in a large, nationally-representative sample of US women.
MATERIALS AND METHODS
This study was approved by the Institutional Review Board of the Duke University School of Medicine. All patient participants provided informed consent.
PROMIS SexFS v2 Vulvar Discomfort Scales
In an effort to improve the measurement of patient-reported health, the National Institutes of Health funded creation of the PROMIS, which included development of the SexFS measures v18 and v2.9 In the next two subsections we summarize the qualitative and psychometric development of the new measures of Vulvar Discomfort with Sexual Activity – Labial and Vulvar Discomfort with Sexual Activity – Clitoral.
Qualitative Development
After a literature review to examine extant patient-reported outcome measures, we conducted 27 patient10 and 10 physician focus groups.9 Initial patient focus groups focused on experiences of sexual function broadly, and general comments about pain and discomfort with sexual activity were common. However, we did not include a specific question about vulvar discomfort in these groups, and few patients spontaneously distinguished vulvar discomfort from vaginal discomfort in their comments. Subsequent focus group discussions with clinicians (especially those specializing in sexual medicine) revealed a need to emphasize distinctions between vaginal and vulvar discomfort as well as the distinctions between labial and clitoral discomfort. These clinical experts noted that the different functions and sensitivities of these tissues and anatomic locations were important and advised that these distinctions were essential for the appropriate identification of symptoms, formulation of treatment needs, and assessment of clinical outcomes.
Accordingly, we generated 16 candidate questionnaire items about vulvar discomfort distinguishing between the labia and clitoris, with item form modeled on existing items about vaginal discomfort. We tested these items in cognitive interviews with patients to evaluate comprehension of the question stems and response options. From these patient interviews, it was clear that modifications to define labia and clitoris within each item were necessary.11 Based on patient feedback, our approach was to add “(lips around the opening of your vagina)” whenever we used the word labia, to add “(clit)” after using the word clitoris, and to further distinguish these items from vaginal discomfort when possible by specifying “inside your vagina” for questions related to vaginal discomfort. After making these changes, we tested the revised items with new patients to reevaluate comprehension and found that patients generally understood the revised items. The 16 revised items on vulvar discomfort were then included in item testing for the PROMIS SexFS v2.
Psychometric Evaluation of Items
We wanted to collect a representative sample on which to base our psychometric evaluation of the PROMIS SexFS items. In June 2013, English-speaking US adult women were recruited through GfK’s KnowledgePanel®, an online panel that uses a probability sample of US mailing addresses to select its participants. For those individuals who are selected to the panel who do not already have internet access, a laptop and internet access are provided by GfK.12 For those individuals who are selected to the panel and already have internet access, GfK provides a small incentive for survey completion (~$6). After a pilot test of the survey, 5039 female GfK panel members were invited to participate. Of those, 2219 viewed the informed consent form and 1498 completed the survey. The full sample available for psychometric evaluation included this general U.S. sample of 1498 women plus an oversample of 188 women recruited after the general sample who reported recent oral, vaginal, or vulvar discomfort with sexual activity, based on responses to screener questions. There was no explicit refusal conversion process; instead, enrollment ended when the targeted sample size was met, based on pre-planned psychometric analyses for measure development.
To keep the overall SexFS v2 measure as streamlined as possible, our measurement goal was to develop a single measure (scale) of vulvar discomfort that covered both labial and clitoral discomfort. However, we recognized from our initial qualitative work that this might not be a unidimensional construct; thus, we pre-specified analyses to compare confirmatory models with labial and clitoral items on separate factors versus all items loading on a single factor. Following methods outlined by Reeve et al., we used a variety of approaches to assess unidimensionality and model fit.13 The detailed psychometric results have been published elsewhere.9
Scoring the PROMIS SexFS
The PROMIS SexFS v2 measures use the T-score metric, where a score of 50 on each scale corresponds to the average for sexually active adults in the U.S. general population with a standard deviation of 10. For each domain, higher scores represent more of that domain, so a higher score on the vulvar or vaginal discomfort scales indicates more discomfort while a higher score on the lubrication scale indicates more lubrication.
Statistical Analysis
For analyses used in measure development and in reporting the prevalence of responses to individual items, the full, unweighted sample was used (n=1686). Where the sample is noted as representative, it refers to the weighted sample (n=1757, of whom 1046 were sexually active and provided data on the vulvar discomfort items). This included weighting (by gender) to the October 2012 Current Population Survey based on age, race/ethnicity, education, income, Census region, metropolitan status, and Internet access. Statistical analyses of this group adjusted for the sample design. We present mean PROMIS scores with 95% confidence intervals based on the mean estimate and standard error of the mean for each of the four domains, separately by self-reported menopausal status and compared using a Wald F-test in survey regression analysis. To examine overlap among the vulvar and vaginal measures we calculated Pearson product moment correlations among the 4 scale scores. We used SAS version 9.4 (SAS Institute, Cary, NC) and a 2-tailed significance level of 0.05 for all assessments.
RESULTS
Sample
Sociodemographic and health characteristics were generally similar between the full unweighted sample and the representative weighted samples (Table 1). However, notable differences included age and menopausal status. The mean age was 49 years in the unweighted sample compared to 47 years in the weighted total sample and 43 years in the weighted sexually active sample. Sixty-two percent of women were menopausal or perimenopausal in the unweighted sample compared to 56% in the weighted total sample and 50% in the weighted sexually active sample.
Table 1.
Characteristics of study sample*
| Characteristic | Full sample†
(Unweighted) No. (%) |
Representative Sample‡ (Weighted) No. (%) |
Representative Sample‡ (Weighted), Sexually Active Only No. (%) |
|---|---|---|---|
| Total | 1686 | 1757 | 1046 |
| Age | |||
| 18-29 years | 284 (17%) | 352 (20%) | 244 (23%) |
| 30-44 years | 368 (22%) | 434 (25%) | 325 (31%) |
| 45-59 years | 534 (32%) | 495 (28%) | 319 (31%) |
| 60+ years | 500 (30%) | 477 (27%) | 158 (15%) |
| Race | |||
| White | 1324 (83%) | 1371 (78%) | 804 (77%) |
| Black/African-American | 169 (11%) | 234 (13%) | 148 (14%) |
| Asian | 27 (2%) | 58 (3%) | 41 (4%) |
| Multiple races or other | 80 (5%) | 95 (5%) | 42 (4%) |
| Hispanic or Latino ethnicity | 141 (8%) | 207 (12%) | 139 (13%) |
| Sexual identity | |||
| Heterosexual or straight | 1596 (95%) | 1652 (94%) | 972 (94%) |
| Gay/Lesbian | 23 (1%) | 29 (1%) | 20 (2%) |
| Bisexual | 49 (3%) | 55 (3%) | 43 (4%) |
| Other | 9 (1%) | 7 (0%) | 4 (0%) |
| Educational attainment | |||
| Less than high school | 110 (7%) | 186 (11%) | 105 (10%) |
| High school graduate/GED | 525 (31%) | 529 (30%) | 274 (26%) |
| Some college | 534 (32%) | 527 (30%) | 329 (32%) |
| Bachelor’s degree or higher | 517 (31%) | 516 (29%) | 339 (32%) |
| Relationship status | |||
| Married or in a civil union or domestic partnership | 954 (57%) | 871 (50%) | 617 (59%) |
| Living with a partner | 146 (9%) | 182 (10%) | 149 (14%) |
| In a relationship but not living together | 129 (8%) | 144 (8%) | 110 (11%) |
| Dating | 68 (4%) | 89 (5%) | 73 (7%) |
| Single | 309 (18%) | 380 (22%) | 79 (8%) |
| Other | 73 (4%) | 81 (5%) | 11 (1%) |
| Employment status | |||
| Working (employee or self-employed) | 836 (50%) | 857 (49%) | 564 (54%) |
| On temporary layoff or looking for work | 166 (10%) | 215 (12%) | 153 (15%) |
| Retired | 359 (21%) | 342 (19%) | 119 (11%) |
| Disabled | 119 (7%) | 122 (7%) | 58 (6%) |
| Other | 207 (12%) | 221 (13%) | 152 (15%) |
| Household income | |||
| < $25,000 | 298 (18%) | 364 (21%) | 180 (17%) |
| $25,001 - $50,000 | 420 (25%) | 426 (24%) | 228 (22%) |
| $50,001 - $75,000 | 330 (20%) | 319 (18%) | 186 (18%) |
| $75,001 - $100,000 | 265 (16%) | 283 (16%) | 198 (19%) |
| > $100,000 | 373 (22%) | 364 (21%) | 254 (24%) |
| Health conditions | |||
| Arthritis or rheumatism | 470 (28%) | 429 (24%) | 203 (20%) |
| Hypertension | 448 (27%) | 442 (25%) | 191 (18%) |
| Depression | 390 (23%) | 375 (21%) | 206 (20%) |
| Anxiety | 335 (20%) | 300 (17%) | 161 (15%) |
| Migraines or severe headaches | 331 (20%) | 301 (17%) | 196 (19%) |
| Diabetes (type I or type II) | 153 (9%) | 149 (8%) | 69 (7%) |
| Heart disease | 143 (9%) | 124 (7%) | 56 (5%) |
| Cancer (other than non-melanoma skin cancer) | 116 (7%) | 113 (6%) | 46 (4%) |
| Self-rated health | |||
| Excellent | 239 (14%) | 285 (16%) | 206 (20%) |
| Very good | 605 (36%) | 622 (35%) | 408 (39%) |
| Good | 531 (32%) | 531 (30%) | 283 (27%) |
| Fair | 239 (14%) | 234 (13%) | 109 (11%) |
| Poor | 49 (3%) | 54 (3%) | 30 (3%) |
Not all fields add to 100 due to rounding and weighting.
Full sample available for psychometric evaluation that includes the general population sample and an oversample from the general population of women with oral, vaginal, or vulvar discomfort with sexual activity based on responses to screener questions
General population sample weighted to the October 2012 Current Population Survey
PROMIS SexFS Vulvar Discomfort Scales
Psychometric evaluation of the new measures indicated acceptable reliability and model fit (Table 2). We found that separate dimensions (scales) for clitoral and labial discomfort were more appropriate than a unidimensional model that combined them into one scale. Best model fit for each of the scales was achieved by including the items on frequency and intensity of pain and discomfort with sexual activity, which is conceptually similar to many other measures of bodily pain. Items on pain quality, numbness, and bleeding can be used as individual items to provide additional context and/or detail but were not included in the final PROMIS scale scores.
Table 2.
Reliability and fit indices for confirmatory factor analysis of vulvar discomfort domains
| Instrument Name | Vulvar Discomfort – Clitoral | Vulvar Discomfort – Labial |
|---|---|---|
| Number of items | 4 | 4 |
| Cronbach’s α* | 0.96 | 0.97 |
| Comparative fit index† | 1.00 | 1.00 |
| Tucker-Lewis index‡ | 0.99 | 1.00 |
| Root-mean-square error of approximation§ |
0.04 | 0.06 |
Numbers originally presented in Weinfurt et al. (2015)9
Measure of reliability; values greater than 0.70 considered acceptable
Measure of model fit; values above 0.95 considered acceptable
Measure of model fit; values above 0.95 considered acceptable
Measure of model fit; values below 0.06 considered acceptable
Correlations Among Vulvar and Vaginal Scales
The magnitudes of the correlations between the PROMIS lubrication, vaginal discomfort, and the two vulvar discomfort measures suggest that these measures represent related yet distinct concepts (Table 3). The correlation among women who had any non-zero response (that is, anything greater than “none” or “never”) within any of the 4 measures was highest between scores on the clitoral and labial discomfort domains (r = 0.77), indicating 59% shared variance (r2) between the two, which means 41% of the differences among women in clitoral discomfort are not accounted for by differences in labial discomfort and vice versa. The correlation between labial and vaginal discomfort was higher than the correlation between clitoral and vaginal discomfort, and the correlations between either vulvar discomfort scale and lubrication were notably lower than the correlation between vaginal discomfort and lubrication.
Table 3.
Correlations between PROMIS SexFS vaginal lubrication, vaginal discomfort, and two vulvar discomfort measures*
| Correlation, r† (95% Confidence Interval) | |||
|---|---|---|---|
| Domains | Vulvar Discomfort – Labial |
Vaginal Lubrication |
Vaginal Discomfort |
| Vulvar Discomfort – Clitoral | 0.77 (0.74, 0.79) | 0.46 (0.41, 0.50) | 0.61 (0.57, 0.64) |
| Vulvar Discomfort – Labial | 1.00 | 0.51 (0.47, 0.56) | 0.69 (0.65, 0.72) |
| Vaginal Lubrication | 1.00 | 0.67 (0.64, 0.70) | |
From the 1294 women from the full sample available for psychometric evaluation who had any non-zero response within any of the 4 measures
From Pearson product moment correlation
Prevalence of Vulvar Discomfort with Sexual Activity
In the full, unweighted sample, the prevalence of each of the candidate items on vulvar discomfort varied by concept (Table 4). In general, numbness and bleeding were less common than discomfort and pain, and clitoral discomfort or pain was somewhat less common than labial discomfort or pain.
Table 4.
Vulvar discomfort with sexual activity*
| Item Content | Item Responses in Full sample† (Unweighted) No. (%) |
||||
|---|---|---|---|---|---|
| Never or None |
Rarely or A little bit |
Sometimes or Some |
Often or Quite a bit |
Always or A lot |
|
| Vulvar Discomfort with Sexual Activity – Labial | |||||
| Frequency of labial discomfort | 767 (73%) | 119 (11%) | 93 (9%) | 44 (4%) | 26 (2%) |
| Intensity of labial discomfort | 781 (74%) | 136 (13%) | 74 (7%) | 34 (3%) | 25 (2%) |
| Frequency of labial pain | 789 (75%) | 113 (11%) | 90 (9%) | 36 (3%) | 24 (2%) |
| Intensity of labial pain | 812 (77%) | 120 (11%) | 69 (7%) | 35 (3%) | 19 (2%) |
| Additional items on labial discomfort | |||||
| Frequency of labial numbness or lack of feeling | 847 (81%) | 82 (8%) | 81 (8%) | 26 (2%) | 14 (1%) |
| Intensity of labial numbness or lack of feeling | 876 (83%) | 81 (8%) | 59 (6%) | 17 (2%) | 17 (2%) |
| Frequency of labial itching, burning, or swelling | 775 (74%) | 119 (11%) | 91 (9%) | 41 (4%) | 25 (2%) |
| Intensity of labial itching, burning, or swelling | 779 (74%) | 135 (13%) | 75 (7%) | 42 (4%) | 24 (2%) |
| Frequency of blood during or after sexual activity | 954 (90%) | 46 (4%) | 41 (4%) | 11 (1%) | 8 (1%) |
| Amount of blood during or after sexual activity | 963 (91%) | 54 (5%) | 28 (3%) | 4 (0%) | 5 (0%) |
| Vulvar Discomfort with Sexual Activity – Clitoral | |||||
| Frequency of clitoral discomfort | 807 (77%) | 116 (11%) | 86 (8%) | 25 (2%) | 20 (2%) |
| Intensity of clitoral discomfort | 844 (80%) | 106 (10%) | 63 (6%) | 35 (3%) | 9 (1%) |
| Frequency of clitoral pain | 836 (79%) | 96 (9%) | 76 (7%) | 34 (3%) | 16 (2%) |
| Intensity of clitoral pain | 875 (83%) | 95 (9%) | 55 (5%) | 22 (2%) | 12 (1%) |
| Additional items on clitoral discomfort | |||||
| Frequency of clitoral numbness or lack of feeling | 838 (79%) | 96 (9%) | 85 (8%) | 24 (2%) | 20 (2%) |
| Intensity of clitoral numbness or lack of feeling | 849 (80%) | 100 (9%) | 66 (6%) | 19 (2%) | 21 (2%) |
Not all fields add to 100 due to rounding.
From the full sample available for psychometric evaluation, n=1686. Not shown is the frequency of responses to the option of “no sexual activity in the past 30 days”, which comprises the remainder of the full sample.
In the representative sample, combining responses to the 8 items included in the 2 vulvar discomfort scales, 21% of sexually active U.S. adult women endorsed recent vulvar discomfort or pain with sexual activity in the past 30 days. Specifically, 11% of women had experienced both labial and clitoral discomfort with sexual activity, an additional 7% had experienced labial discomfort but not clitoral discomfort, and 3% had experienced clitoral discomfort but not labial discomfort.
Menopause and Discomfort with Sexual Activity
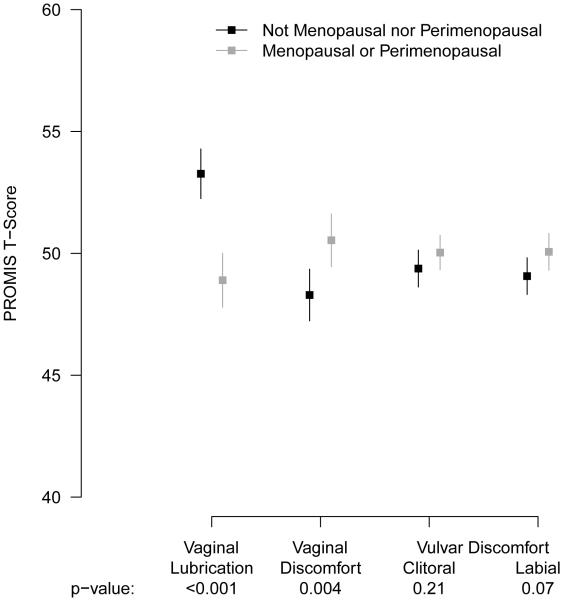
Sexually active women who were menopausal or perimenopausal reported significantly lower vaginal lubrication (by 4.4 points, p < 0.001) and significantly higher vaginal discomfort (by 2.2 points, p = 0.004) with sexual activity than non-menopausal women (Figure). The differences in the vulvar discomfort scale scores by menopausal status were smaller and did not reach statistical significance – 1 point for labial discomfort (p = 0.07) and 0.7 points for clitoral discomfort (p = 0.21).
Figure.
Mean PROMIS Vaginal Lubrication, Vaginal Discomfort, and Vulvar Discomfort scores and 95% confidence intervals among US women by menopausal status, 2013
COMMENT
Vulvar discomfort with sexual activity has been understudied, in part due to the lack of validated measures to assess it in extant multi-dimensional measures of pain or sexual function. We have summarized the development process that resulted in two new PROMIS scales measuring vulvar discomfort and described their relationships with the related domains of vaginal lubrication and vaginal discomfort with sexual activity. We found limited overlap among these domains, which suggests the new PROMIS measures of vulvar discomfort with sexual activity offer unique information about sexual function.
We also reported the prevalence of vulvar discomfort with sexual activity in a large, nationally-representative sample of US women. The importance of including measurement of these concepts as part of a comprehensive assessment of sexual health is underscored by their prevalence: 1 in 5 sexually-active US women endorsed some degree of vulvar discomfort with sexual activity in the past 30 days. Few women reported severe vulvar pain or discomfort.
We found no direct comparisons between the presented data and other studies. Estimates of related concepts vary: the prevalence of dyspareunia (i.e., pain with intercourse) in general population studies in the US has been estimated at 7-19%,14, 15 while vulvodynia (i.e., persistent vulvar pain without identifiable etiology) has been estimated at 8%.16 Having a history of vulvar pain is more common, with as many as 38% of women reporting it in one study.17 Genitourinary syndrome of menopause, for which vulvovaginal atrophy is an important component, occurs naturally during the menopausal transition and can also contribute to pain,18, 19 through vulvovaginal symptoms including dryness, tightness, and susceptibility to abrasion and fissuring with intercourse. In this study, we observed significant differences by menopausal status in PROMIS scores on vaginal lubrication for sexual activity and vaginal pain with sexual activity. However, the differences in scores on vulvar discomfort with sexual activity were smaller and did not reach the pre-specified significance threshold of p<0.05, suggesting that factors other than menopausal status may contribute more significantly to the etiology of vulvar discomfort compared to vaginal discomfort. We found no national estimates of clitoral pain to which we could compare our findings.
The Vulvovaginal Symptom Questionnaire (VSQ) also measures vulvar symptoms, though somewhat differently than PROMIS, as the VSQ aims to measure the impact of vulvovaginal symptoms on quality of life among postmenopausal women.20 Accordingly, the VSQ is not specific to symptoms associated with sexual activity and it includes emotions and life impact of symptoms within its 21-item scale. The VSQ does not distinguish between the labia and clitoris. Development of the VSQ included cognitive interviews with 5 women and psychometric evaluation in 120 women. The PROMIS SexFS vulvar discomfort scales measure both labial and clitoral discomfort associated with sexual activity. We also presented data from over 1000 US women on additional self-report items that provide details about pain quality, numbness, and bleeding that may be of interest for particular studies or settings, such as to aid clinical decisions in the treatment of female pelvic pain or sexual function. These self-report items underwent the same qualitative validation as the items that comprise the PROMIS scales, a development process that incorporated feedback from people with lower literacy and a range of ages, health conditions, and sexual orientations.
Our original focus group guides did not include specific probes about vulvar symptoms, and very few patients spontaneously addressed vulvar pain as distinct from vaginal pain. We suspect this is due to imprecise language (e.g., common usage of the word vagina to mean both internal and external anatomy) rather than a lack of experience with these symptoms, especially given the high prevalence of vulvar discomfort/pain later observed in our national sample. Second, even with simply worded items that underwent multiple rounds of cognitive interviews, not all women may be able to understand or accurately distinguish between labial, clitoral, and vaginal discomfort. Third, our qualitative work to develop and initially test these items was limited to one geographic location. Fourth, while our comprehensive item testing was conducted in a large, national sample, it was limited to English-speaking women. Finally, as with all sample surveys, there is the possibility for errors of non-observation.
The PROMIS SexFS v2.0 scales for Vulvar Discomfort with Sexual Activity – Labial and Vulvar Discomfort with Sexual Activity – Clitoral may help meet both clinical and research needs. While they were developed primarily as a research tool, development included specific input from clinicians to improve their clinical utility. Effective treatment of women with dyspareunia should begin with a comprehensive assessment that includes evaluation of clitoral and labial pain.21 If administered clinically, inclusion of the vulvar discomfort items alongside measures of lubrication and vaginal discomfort could assist clinicians in quantifying discomfort as well as clarifying the nature and anatomic location of genital discomfort experienced by women during sexual activity. Vulvar and vaginal tissue quality often changes simultaneously, and clinicians might consider treating both simultaneously as well, that is, by pairing vaginal estrogen with non-hormonal vulvar moisturizing creams that are applied to the vaginal opening and all of the vulvar tissues. With regard to research implications, the open-access availability of the PROMIS scales and the additional items presented here should make it possible for new research on the effects of diseases and their treatments on vulvar discomfort with sexual activity, as well as for evaluating interventions to mitigate vulvar discomfort. The PROMIS SexFS instruments underwent an extensive development process and are available in English and Spanish. PROMIS SexFS scores are centered on the US general population mean, and our presentation of average scores by age and menopausal status allows for built-in comparisons for study samples in a research setting or individual patients in a clinical setting. Future work should explore the utility of these new measures in clinical care for triage and symptom monitoring.
ACKNOWLEDGMENTS
We wish to acknowledge the contributions of the members of the PROMIS Sexual Function domain group and the Scientific Network on Female Sexual Health and Cancer.
Acknowledgment of Financial Support: The study was supported by funding from the National Institute of Arthritis and Musculoskeletal and Skin Diseases (U01AR052186, PI Kevin Weinfurt). Dr. Flynn was funded in part by the Research and Education Program Fund, a component of the Advancing a Healthier Wisconsin endowment at the Medical College of Wisconsin.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Disclosure Statement: The authors report no conflicts of interest.
Disclaimer: The contents of this manuscript are solely the responsibility of the authors and do not necessarily represent the official views of the National Institutes of Health, the National Institute on Aging or the National Institute of Arthritis and Musculoskeletal Skin Diseases.
An earlier version of this work was presented at the World Meeting on Sexual Medicine; Sao Paolo, Brazil; October 10, 2014, where it won the prize for “Best Abstract – Female.”
CONDENSATION AND SHORT VERSION OF TITLE
The PROMIS Vulvar Discomfort with Sexual Activity scales (Labial and Clitoral) offer robust self-reported measurement of a common but often overlooked aspect of sexual health.
References
- [1].Bornstein J, Goldstein AT, Stockdale CK, et al. 2015 ISSVD, ISSWSH and IPPS Consensus Terminology and Classification of Persistent Vulvar Pain and Vulvodynia. Obstet Gynecol. 2016;127:745–51. doi: 10.1097/AOG.0000000000001359. [DOI] [PubMed] [Google Scholar]
- [2].Ben-Aroya Z, Edwards L. Vulvodynia. Semin Cutan Med Surg. 2015;34:192–8. doi: 10.12788/j.sder.2015.0181. [DOI] [PubMed] [Google Scholar]
- [3].Leusink P, Kaptheijns A, Laan E, van Boven K, Lagro-Janssen A. Comorbidities Among Women With Vulvovaginal Complaints in Family Practice. J Sex Med. 2016;13:220–5. doi: 10.1016/j.jsxm.2015.12.010. [DOI] [PubMed] [Google Scholar]
- [4].Burger MP, Obdeijn MC. Complications after surgery for the relief of dyspareunia in women with lichen sclerosus: a case series. Acta Obstet Gynecol Scand. 2016;95:467–72. doi: 10.1111/aogs.12852. [DOI] [PubMed] [Google Scholar]
- [5].Thorstensen KA, Birenbaum DL. Recognition and management of vulvar dermatologic conditions: lichen sclerosus, lichen planus, and lichen simplex chronicus. J Midwifery Womens Health. 2012;57:260–75. doi: 10.1111/j.1542-2011.2012.00175.x. [DOI] [PubMed] [Google Scholar]
- [6].Simonetta C, Burns EK, Guo MA. Vulvar Dermatoses: A Review and Update. Mo Med. 2015;112:301–7. [PMC free article] [PubMed] [Google Scholar]
- [7].Goetsch MF, Lim JY, Caughey AB. Locating pain in breast cancer survivors experiencing dyspareunia: a randomized controlled trial. Obstet Gynecol. 2014;123:1231–6. doi: 10.1097/AOG.0000000000000283. [DOI] [PubMed] [Google Scholar]
- [8].Flynn KE, Lin L, Cyranowski JM, et al. Development of the NIH PROMIS® Sexual Function and Satisfaction Measures in patients with cancer. Journal of Sexual Medicine. 2013;10(Suppl 1):43–52. doi: 10.1111/j.1743-6109.2012.02995.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9].Weinfurt KP, Lin L, Bruner DW, et al. Development and Initial Validation of the PROMIS((R)) Sexual Function and Satisfaction Measures Version 2.0. J Sex Med. 2015;12:1961–74. doi: 10.1111/jsm.12966. [DOI] [PubMed] [Google Scholar]
- [10].Flynn KE, Jeffery DD, Keefe FJ, et al. Sexual functioning along the cancer continuum: focus group results from the Patient-Reported Outcomes Measurement Information System (PROMIS(R)) Psychooncology. 2011;20:378–86. doi: 10.1002/pon.1738. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].Alexander AM, Flynn KE, Hahn EA, et al. Improving patients' understanding of terms and phrases commonly used in self-reported measures of sexual function. J Sex Med. 2014;11:1991–8. doi: 10.1111/jsm.12599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12].Knowledge Networks. KnowledgePanel Design Summary. 2014 [Google Scholar]
- [13].Reeve BB, Hays RD, Bjorner JB, et al. Psychometric evaluation and calibration of health-related quality of life item banks: plans for the Patient-Reported Outcomes Measurement Information System (PROMIS) Med Care. 2007;45:S22–S31. doi: 10.1097/01.mlr.0000250483.85507.04. [DOI] [PubMed] [Google Scholar]
- [14].Laumann EO, Paik A, Rosen RC. Sexual dysfunction in the United States: prevalence and predictors. JAMA. 1999;281:537–44. doi: 10.1001/jama.281.6.537. [DOI] [PubMed] [Google Scholar]
- [15].Lindau ST, Schumm LP, Laumann EO, Levinson W, O'Muircheartaigh CA, Waite LJ. A study of sexuality and health among older adults in the United States. New England Journal of Medicine. 2007;357:762–74. doi: 10.1056/NEJMoa067423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [16].Reed BD, Harlow SD, Sen A, et al. Prevalence and demographic characteristics of vulvodynia in a population-based sample. Am J Obstet Gynecol. 2012;206:170. doi: 10.1016/j.ajog.2011.08.012. e1-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [17].Reed BD, Haefner HK, Harlow SD, Gorenflo DW, Sen A. Reliability and validity of self-reported symptoms for predicting vulvodynia. Obstet Gynecol. 2006;108:906–13. doi: 10.1097/01.AOG.0000237102.70485.5d. [DOI] [PubMed] [Google Scholar]
- [18].Nappi RE, Palacios S, Panay N, Particco M, Krychman ML. Vulvar and vaginal atrophy in four European countries: evidence from the European REVIVE Survey. Climacteric. 2016;19:188–97. doi: 10.3109/13697137.2015.1107039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [19].Parish SJ, Nappi RE, Krychman ML, et al. Impact of vulvovaginal health on postmenopausal women: a review of surveys on symptoms of vulvovaginal atrophy. Int J Womens Health. 2013;5:437–47. doi: 10.2147/IJWH.S44579. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [20].Erekson EA, Yip SO, Wedderburn TS, et al. The Vulvovaginal Symptoms Questionnaire: a questionnaire for measuring vulvovaginal symptoms in postmenopausal women. Menopause. 2013;20:973–9. doi: 10.1097/GME.0b013e318282600b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [21].Parada M, D'Amours T, Amsel R, Pink L, Gordon A, Binik YM. Clitorodynia: A Descriptive Study of Clitoral Pain. J Sex Med. 2015;12:1772–80. doi: 10.1111/jsm.12934. [DOI] [PubMed] [Google Scholar]