Abstract
Objectives:
This study was designed to assess the changes of the mandible of patients who underwent orthodontic treatment with or without extraction of four premolars.
Materials and Methods:
Eighteen Class I bimaxillary protrusion patients treated with extraction of four first premolars and retraction of anterior teeth and 18 Class I non-extraction patients with a mean age of 16.38±0.4 years were selected. Cephalometric analysis was performed before and after treatment. Twenty-four variables for analyzing the hard and soft tissues of the mandible were compared between the two groups. Repeated measures ANOVA was used for the comparison of the two groups fallowed by paired t-test. The relationship between the soft and hard tissue variables was studied using the Pearson’s correlation coefficient.
Results:
In both groups, the mean value of angular measurements related to B point and Pogonion (Pog) decreased with treatment (P<0.05). Similarly, the symphysis depth of soft tissue decreased (P=0.008). The mean angular value of Y-axis increased in both groups after treatment (P=0.007). The mean changes in hard tissue symphysis depth after treatment were different in the two groups (P=0.021). Vertical, horizontal and rotational changes in soft tissue B point (B’) and Pogonion (pog’) followed their underlying hard tissue changes (P<0.05).
Conclusions:
Points B and Pog showed backward movement after orthodontic treatments in both extraction and non-extraction patients. Changes in B’ and Pog’ were directly influenced by the changes in the corresponding points of the underlying hard tissue. Orthodontic treatments with and without extraction of premolars produced insignificant changes in vertical facial dimension.
Keywords: Chin, Tooth Extraction, Mandible
INTRODUCTION
Human beings have always been in search of beauty. Mandible plays an important role in facial esthetics. A harmony between the soft and hard tissues of the chin is necessary for an attracttive lower one-third and overall facial beauty.
Contemporary orthodontics aims to restore facial esthetics; which is influenced by the facial hard and soft tissues. It has been reported that soft tissue profile is related to the underlying skeletal and dental structures [1,2]. However other studies believed that hard tissue profile may be affected by dental changes [3,4]. Soft tissue changes have also been attributed to dental changes [5,6]. On the other hand, it has been stated that the underlying hard tissue does not necessarily influence the entire facial soft tissue [7].
Orthodontic treatment may be performed in the form of extraction or non-extraction treatment. Patients with dental crowding or bimaxillary dentoalveolar protrusion usually undergo extraction of the first or second premolars for retraction and alignment of teeth [8,9]. In patients with mild problems or those requiring correction of the angulation of teeth, non-extraction orthodontic treatment is carried out. In both cases, the treatment aims to correct the dentoalveolar problems and subsequently the soft tissue profile to create a more desirable appearance.
Numerous studies have compared the effects of extraction and non-extraction orthodontic treatments. Bishara et al, [10] and Young and Smith [11] stated that extraction of premolars had no deleterious effects on the facial profile. Verma et al, [12] stated that in patients with class II division I malocclusion, the soft-tissue facial profiles of the non-extraction and extraction cases were the same except for a more retruded lower lip and a more pronounced lower labial sulcus in the latter [12]. There are few studies on the effects of extraction and non-extraction orthodontic treatments on the soft tissue of the mandible and chin. Bowman and Johnston [13] and Paquette et al, [14] compared extraction and non-extraction patients and reported that after treatment, extraction patients had a straighter profile than non-extraction patients. Numerous studies have evaluated upper lip and lower lip changes after extraction of premolar teeth and retraction of incisors but limited studies have evaluated hard and soft tissue changes of the mandible and chin in patients after different orthodontic treatments. The aim of this study was to assess the changes in hard and soft tissue of the mandible after treatment with extraction or non-extraction orthodontic protocols.
MATERIALS AND METHODS
This inception cohort study with two arms was conducted on 36 Class I adult patients out of which, 18 were diagnosed with Class I bimaxillary protrusion based on clinical examination and cephalometric analyses; their treatment plan consisted of extraction of all four first premolars and retraction of incisors. The remaining 18 patients comprised the non-extraction group and their treatment plan included correction of the position of incisor teeth without extraction of premolars.
The patients were selected among those presenting to a private office and Orthodontic Department of Tehran University of Medical Sciences. The mean age at the onset of treatment was 16.38±0.4 years and the mean duration of treatment was 24±6 months.
The inclusion criteria were as follows:
- Female patients with Class I malocclusion based on clinical and paraclinical examinations
- Complete health in terms of absence of craniofacial disorders
- No history of trauma to the jaws
- Patient cooperation throughout the treatment course
- Patients treated with fixed straight wire appliances (0.022-inch; MBT prescription, 3M Unitek, Monrovia, CA, USA)
The before and after treatment cephalograms of patients with acceptable quality were manually traced. For the assessment of intra-observer reliability, all cephalograms were traced twice in the morning and in the evening with an intraclass correlation coefficient (ICC) of 0.97.
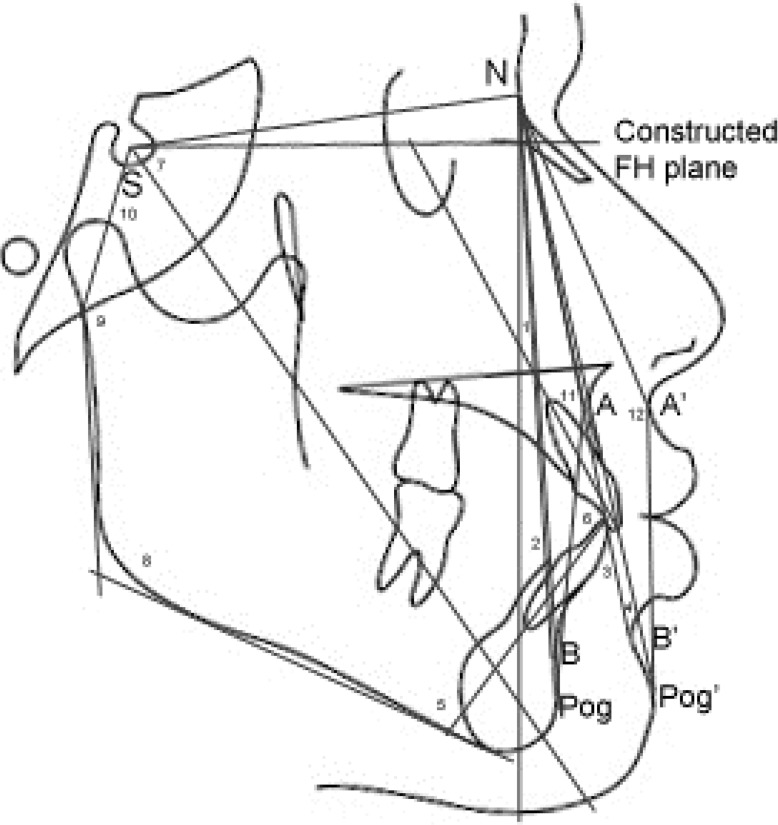
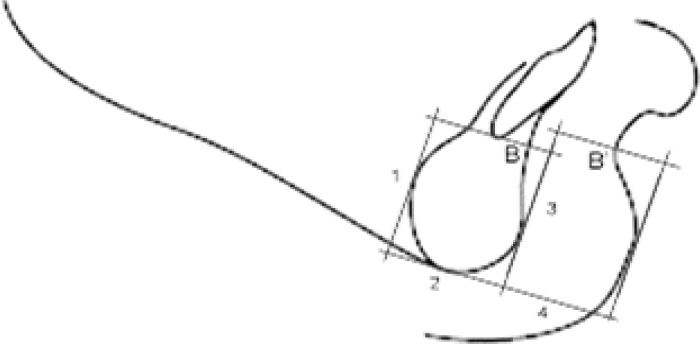
The inter-observer reliability was calculated and confirmed by an expert orthodontist with an ICC of 0.96. The lateral cephalograms were taken in standard centers, and their magnification was taken into account. The measured cephalometric parameters are summarized in Table 1, including angular measurements, the reference planes (Fig. 1) and symphysis measurements (Fig. 2).
Table 1:
Some cephalometric landmarks and parameters used in the present study
| Landmark | Definition |
|---|---|
| SN7° line (constructed FH plane) | Line constructed 7° with the SN plane |
| Angle of convexity | The angle of convexity is formed between the N-A line and A-Pog line |
| B-NP | The perpendicular distance from point B to NP line (in millimeters) |
| Pog-NP | The perpendicular distance from point Pog to NP line (in millimeters) |
| B-SN7° | The distance from point B to SN7° line (constructed FH plane) |
| Pog-SN7° | The distance from point Pog to SN7° line |
| SNB’ | SNB’ angle is formed by the intersection of S-N line and N-B’ line |
| SNPog’ | SNPog’ angle is formed by the intersection of S-N line and N-Pog’ line |
| Angle of convexity of soft tissue | This angle is formed between the N-A’ line and A’-Pog’ line |
| B’-NP | The perpendicular distance from point B’ to NP line (in millimeters) |
| Pog’-NP | The perpendicular distance from point Pog’ to NP line (in millimeters) |
| B’-SN7° | The distance from point B’ to SN7° line |
| Pog’-SN7° | The distance from point Pog’ to SN7° line |
| Y-axis angle | The angle between the Y-axis (S-Gn) and Frankfurt plane |
| Sum of Bjork | The sum of saddle angle, articular angle and gonial angle |
| Symphysis depth in hard tissue | Distance between the two parallel lines of the main symphyseal axis tangent to the most anterior and most posterior points of the symphysis contour (in millimeters) |
| Symphysis height in hard tissue | Distance from point B to the line from the most inferior point in the symphysis in hard tissue perpendicular to the main symphyseal axis (in millimeters) |
| Symphysis depth in soft tissue | Distance between the two parallel lines of the main symphyseal axis tangent to the most anterior point on the hard tissue contour of symphysis and the most anterior point on the soft tissue contour (in millimeters) |
| Symphysis height in soft tissue | Distance from point B’ to the line from the most inferior point in the symphysis in soft tissue perpendicular to the main symphyseal axis (in millimeters) |
Fig. 1:
Cephalometric angular measurements and reference planes (1) SNA (2) SNPog (3) SNB’ (4) SNPog’ (5) IMPA (6) Interincisal angle (7) Y-axis (8) Gonial angle (9) Articular angle (10) Saddle angle (11) Angle of convexity (12) Soft tissue angle of convexity
Fig. 2:
Symphysis measurements (1) Hard tissue height of symphysis (2) Hard tissue depth of symphysis (3) Soft tissue height of symphysis (4) Soft tissue depth of symphysis
Repeated measures ANOVA was used for the comparison of the two groups of extraction and non-extraction patients. Paired t-test was then applied for statistical analysis of significant differences. The relationship between soft and hard tissue variables was studied using the Pearson’s correlation coefficient.
RESULTS
The comparisons of pretreatment and post-treatment cephalometric observations of extraction and non-extraction cases are demonstrated in Tables 2 and 3, respectively. The mean angular changes in B point indicated by the SNB angle were relatively the same (P=0.693) in both groups of extraction (−0.76±1.33) and non-extraction (−1.01±2.31), and the difference between pre and post-treatment results was statistically significant (P=0.008).
Table 2:
Comparison of the pre-treatment and post-treatment values of patients with extraction treatment
| Measurements | Pretreatment (Mean ± SD) | Post-treatment (Mean ± SD) | Change (Mean ± SD) | P-value |
|---|---|---|---|---|
| B-NP | −14.33 ± 7.69 | −15.26 ± 7.29 | −0.93 ± 3.89 | 0.055 |
| B-SN7° | 104.71 ± 8.86 | 106.74 ± 11.00 | 2.03 ± 8.28 | 0.336 |
| SNB | 75.65 ± 3.93 | 74.89 ± 3.34 | −0.76 ± 1.33 | 0.008* |
| Pog-NP | −15.42 ± 9.39 | −15.36 ± 8.71 | 0.06 ± 4.83 | 0.266 |
| Pog-SN7° | 121.31 ± 10.64 | 120.91 ± 10.29 | −0.41 ± 9.80 | 0.832 |
| SNPog | 76.29 ± 4.09 | 75.88 ± 3.60 | −0.42 ± 1.34 | 0.028* |
| B′-NP | −1.93 ± 8.75 | −2.63 ± 8.03 | −0.70 ± 5.53 | 0.278 |
| B′-SN7° | 106.79 ± 9.80 | 107.43 ± 10.37 | 0.63 ± 9.11 | 0.551 |
| SNB′ | 82.10 ± 4.35 | 81.14 ± 3.62 | −0.96 ± 1.81 | 0.465 |
| Pog′-NP | −1.84 ± 10.22 | −1.77 ± 8.16 | 0.08 ± 6.46 | 0.231 |
| Pog′-SN7° | 119.40 ± 10.24 | 120.07 ± 10.72 | 0.67 ± 9.05 | 0.273 |
| SNPog′ | 82.18 ± 4.51 | 81.81 ± 3.74 | −0.38 ± 1.75 | 0.822 |
| NAPog | 2.96 ± 2.88 | 2.76 ± 2.73 | −0.19 ± 1.06 | 0.559 |
| NAPog′ | 9.18 ± 2.82 | 8.06 ± 2.59 | −1.13 ± 1.40 | 0.002* |
| Symphysis depth | 17.02 ± 1.57 | 16.48 ± 1.30 | −0.53 ± 1.10 | 0.021* |
| Symphysis depth soft tissue | 11.62 ± 1.87 | 11.19 ± 2.11 | −0.43 ± 1.22 | 0.008* |
| Symphysis height | 26.35 ± 2.76 | 25.93 ± 3.17 | −0.42 ± 2.18 | 0.449 |
| Symphysis height soft tissue | 30.68 ± 4.31 | 30.92 ± 3.67 | 0.24 ± 3.85 | 0.483 |
| Y axis | 70.50 ± 3.81 | 71.28 ± 3.67 | 0.78 ± 1.31 | 0.007* |
| Sum of Bjork | 396.38 ± 5.42 | 396.90 ± 4.68 | 0.52 ± 2.64 | 0.803 |
=Significant differences (P<0.05)
Table 3:
Comparisons of the pre-treatment and post-treatment values of non-extraction patients
| Measurements | Pretreatment (Mean ± SD) | Post-treatment (Mean ± SD) | Change (Mean ± SD) | P-value |
|---|---|---|---|---|
| B-NP | −9.84 ± 9.36 | −11.77 ± 8.59 | −1.93 ± 4.72 | 0.055 |
| B-SN7° | 107.95 ± 7.43 | 107.55 ± 8.80 | −0.40 ± 6.52 | 0.336 |
| SNB | 78.54 ± 4.08 | 77.53 ± 3.78 | −1.01 ± 2.31 | 0.008* |
| Pog-NP | −8.36 ± 10.88 | −10.22 ± 9.81 | −1.86 ± 5.34 | 0.266 |
| Pog-SN7° | 119.80 ± 6.80 | 118.79 ± 8.34 | −1.01 ± 6.92 | 0.832 |
| SNPog | 79.88 ± 4.69 | 78.71 ± 4.46 | −1.17 ± 2.61 | 0.028* |
| B′-NP | 4.26 ± 8.55 | 1.73 ± 8.64 | −2.54 ± 4.40 | 0.278 |
| B′-SN7° | 106.29 ± 8.51 | 105.33 ± 9.45 | −0.97 ± 6.62 | 0.551 |
| SNB′ | 84.63 ± 4.42 | 84.25 ± 4.03 | −0.38 ± 2.82 | 0.465 |
| Pog′-NP | 6.66 ± 10.19 | 4.27 ± 8.98 | −2.39 ± 5.66 | 0.231 |
| Pog′-SN7° | 119.73 ± 7.38 | 117.45 ± 8.28 | −2.28 ± 6.64 | 0.273 |
| SNPog′ | 85.78 ± 4.31 | 85.24 ± 3.80 | −0.54 ± 2.59 | 0.822 |
| NAPog | −0.17 ± 3.43 | 0.03 ± 3.68 | 0.19 ± 2.59 | 0.559 |
| NAPog′ | 7.31 ± 2.14 | 6.54 ± 2.69 | −0.76 ± 1.95 | 0.002* |
| Symphysis depth | 15.27 ± 1.87 | 15.55 ± 1.91 | 0.28 ± 0.90 | 0.021* |
| Symphysis depth soft tissue | 13.77 ± 2.60 | 13.06 ± 2.77 | −0.71 ± 1.23 | 0.008* |
| Symphysis height | 20.91 ± 2.76 | 21.10 ± 1.74 | 0.19 ± 2.60 | 0.449 |
| Symphysis height soft tissue | 28.30 ± 2.93 | 29.37 ± 3.63 | 1.07 ± 3.19 | 0.483 |
| Y axis | 66.55 ± 3.92 | 67.57 ± 3.75 | 1.02 ± 2.29 | 0.007* |
| Sum of Bjork | 392.26 ± 6.60 | 392.58 ± 5.91 | 0.32 ± 2.18 | 0.803 |
=Significant differences (P<0.05)
The mean changes in the Pogonion (Pog) indicated by SN-Pog were approximately similar (P=0.285) in the two groups of extraction (−0.42±1.34) and non-extraction (−1.17±2.61), and the difference between pre and post-treatment results was statistically significant (P=0.028).The mean changes in angle of convexity of soft tissue (NA’Pog’) were not significantly different between extraction (−1.13±1.40) and non-extraction (−0.76±1.95) groups (P=0.528), and the difference after treatment was statistically significant (P=0.002).
The mean symphysis depth of the soft tissue changed significantly after treatment (P=0.008) but the mean changes were not different in the extraction (−0.43±1.22) and non-extraction (−0.71±1.23) groups (P=0.496). The same was observed for Y-axis angle. The mean changes in symphysis depth in the hard tissue were statistically significant and different in the two groups (P=0.021).
The mean symphysis depth in the hard tissue did not significantly change in the non-extraction group based on paired t-test (P=0.056) but slightly decreased in the extraction group (P=0.204). Other measurements were the same in the two groups and based on repeated measures ANOVA, the changes in the two groups were not significant.
The correlations between soft and hard tissues are presented in Table 4. A significant degree of correlation existed between horizontal linear movements of B point (B-NP) and B’ point (B’-NP) (P<0.001, r=0.779). Similarly, horizontal linear movements of Pog point (Pog-NP) and Pog’ point (Pog’-NP) correlated significantly (P<0.001, r=0.937).
Table 4:
Correlation between soft and hard tissue
| Correlation Coefficient | P-value* | |
|---|---|---|
| B-NP vs. B’-NP | 0.779 | <0.001 |
| Pog-NP vs. Pog’-NP | 0.937 | <0.001 |
| B-SN7° vs. B’-SN7° | 0.842 | <0.001 |
| Pog-SN7° vs. Pog’-SN7 | 0.804 | <0.001 |
| SNB vs. SNB’ | 0.514 | 0.001 |
| SNPog vs. SNPog’ | 0.543 | 0.001 |
All were significant
Vertical linear movements of B point indicated by distance from B to constructed Frankfurt horizontal plane or FH (SN 7°) correlated significantly with B’ point indicated by B’-SN (P<0.001, r=0.842). The same was true for vertical linear movements of Pog by Pog-SN7° and Pog’ by Pog’-SN7° (P<0.001, r=0.806).
There was a significant degree of correlation between rotational movements of B point with SNB and B’ point with SNB’ (P=0.001) and also between rotational movements of Pog (SNPog) and pog’ (SNPog’) (P=0.001).
DISCUSSION
This study evaluated the hard and soft tissue profiles of patients before and after orthodontic treatment. Standard cephalometry was performed for assessment of facial hard and soft tissue changes in the mandible and chin area between the two groups of patients treated with and without tooth extraction. The results showed no significant differences in horizontal or vertical changes in B point and Pog in hard tissue or their corresponding points of B’ and Pog’ in the soft tissue between the two treatment groups. Angular changes in B point and Pog in the hard tissue were the same in the two groups (as reduction in SNB and SN Pog angles). The corresponding angular changes in the soft tissue were not significant. Similar increasing changes in Y-axis angle in both extraction and non-extraction patients and reduction of SNB and SNPog in the two groups indicate that the rotational changes of the chin are directly related to orthodontic treatment and not to extraction of premolar teeth. In terms of alterations in the chin area, changes in depth before and after treatment were observed in both groups. Considering the similar soft tissue changes of the symphysis depth in the two groups and increased symphysis depth in the hard tissue of patients in the non-extraction group, we may conclude that soft tissue retraction in this area causes a slight increase in thickness of the underlying hard tissue during treatment; whereas, in extraction patients, the muscles of this area are relaxed and may remove the pressure from the area leading to no increase in the symphysis depth. In a study by Sharma [2] on changes of A and B points in the hard tissue and A’ and B’ points in the soft tissue following extraction of the four first premolars and retraction of incisors, it was found that pre- and post-treatment changes in these patients were significant in both B and B’ points. Point B and point B’ were retracted by 2.1mm and 1.2mm, respectively. In the current study, the trend of changes in B and B’ was the same in the two groups and these points were retracted. However, these changes in our study were not statistically significant (Tables 2 and 3).
In another study by Al-Abdwani et al, [3] on changes in A and B points in the hard tissue of patients treated with retraction of incisors, changes in B point (before and after treatment) were significant. In response to 10° retraction of mandibular incisors, backward changes in the horizontal dimension were seen, but no significant change was noted in the vertical dimension [3]. In our study, B point in the two groups had a backward movement in the horizontal dimension; while, in terms of vertical dimension, extraction patients showed a downward and non-extraction patients demonstrated an upward movement. However, this difference between the two groups was not statistically significant.
Kachiwala et al, [15] evaluated the facial soft tissue changes in female patients undergoing extraction and correction of the protrusion of anterior teeth in both jaws and reported that B’ point had no significant changes after treatment compared to baseline. Their study only evaluated extraction patients [15]. In our study no significant change was noted in B’ in the two treatment groups. In the current study, we found no significant differences in symphysis height in the two groups but symphysis depth slightly increased.
In a study by Singh [16], changes in the soft tissue contour of the chin area before and after treatment and also five years after completion of treatment were evaluated in extraction orthodontic patients. He reported that the overall soft tissue thickness from B point to Menton increased [16]. In our study, changes in the soft tissue thickness (measured from the most anterior point of the soft tissue symphysis to the most anterior point of the hard tissue symphysis) were similar in the two groups and showed a significant reduction in the soft tissue thickness. Several studies have investigated the changes in upper and lower lips following the retraction of anterior teeth, and a consensus has reached: By the retraction of anterior teeth, the lips are retracted as well. However, fewer studies addressed symphyseal changes after such treatments. Based on our results, changes in B point and Pog in both extraction and non-extraction groups were similar and they were both retracted. Considering the correlation of the above points with their overlying soft tissue, a significant correlation was observed between the hard tissue and soft tissue changes in both study groups.
Evaluating the vertical skeletal growth changes in our patients by the sum of Bjork parameter indicated no significant changes in extraction and non-extraction groups. In addition, a significant increase in Y-axis angle in both groups revealed that contrary to the opinion of some clinicians that extraction of first premolars decreases the vertical facial parameters [17,18], such vertical changes could not be attributed to extraction in our study. Controversy between different studies may be attributed to various systems and methods applied for orthodontic treatment. In the current study, pre-adjusted 0.022-inch slot brackets with MBT technique was applied, which has been advocated by several authors [19,20].
CONCLUSION
In both groups, treated with extraction of the four first premolar teeth and non-extraction, B point and Pog had backward movement after orthodontic treatment. Changes in B’ and Pog’ were also directly influenced by the changes in the corresponding points in the underlying hard tissue in moving backward. The mean soft tissue thickness of the chin (measured from the most anterior point of the soft tissue symphysis to the most anterior point of the hard tissue symphysis) was similar in the two groups. Orthodontic treatments with and without extraction of premolars caused no reduction in vertical facial dimension.
ACKNOWLEDGMENT
This work was based on the thesis submitted to School of Dentistry, Tehran University of Medical Sciences, International campus in partial fulfillment of the doctorate degree in dentistry.
REFERENCES
- 1-. Rathod AB, Araujo E, Vaden JL, Behrents RG, Oliver DR. Extraction vs no treatment: Long-term facial profile changes. Am J Orthod Dentofacial Orthop. 2015. May; 147 (5): 596– 603. [DOI] [PubMed] [Google Scholar]
- 2-. Sharma JN. Skeletal and soft tissue point A and B changes following orthodontic treatment of Nepalese Class I bimaxillary protrusive patients. Angle Orthod. 2010. January; 80 (1): 91– 6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3-. Al-Abdwani R, Moles DR, Noar JH. Change of incisor inclination effects on points A and B. Angle Orthod. 2009. May; 79 (3): 462– 7. [DOI] [PubMed] [Google Scholar]
- 4-. Hosseinzadeh Nik T, Nourozi S, Hosseinizade SM. Hard tissue response to anterior tooth retraction. IJO 2006; 1: 48– 52. [Google Scholar]
- 5-. Konstantonis D. The impact of extraction vs nonextraction treatment on soft tissue changes in Class I borderline malocclusions. Angle Orthod. 2012. March; 82 (2): 209– 17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6-. Hershey HG. Incisor tooth retraction and subsequent profile change in postadolescent female patients. Am J Orthod. 1972. January; 61 (1): 45– 54. [DOI] [PubMed] [Google Scholar]
- 7-. Basciftci FA, Usumez S. Effects of extraction and nonextraction treatment on class I and class II subjects. Angle Orthod. 2003. February; 73 (1): 36– 42. [DOI] [PubMed] [Google Scholar]
- 8-. Tan TJ. Profile changes following orthodontic correction of bimaxillary protrusion with a pre-adjusted edgewise appliance. Int J Adult Orthodon Orthognath Surg. 1996; 11 (3): 239– 51. [PubMed] [Google Scholar]
- 9-. Keating PJ. The treatment of bimaxillary protrusion: a cephalometric consideration of changes in the inter-incisal angle and soft tissue profile. Br J Orthod. 1986. October; 13 (4): 209– 20. [PubMed] [Google Scholar]
- 10-. Bishara SE, Cummins DM, Jakobsen JR, Zaher AR. Dentofacial and soft tissue changes in Class II, division 1 cases treated with and without extractions. Am J Orthod Dentofacial Orthop. 1995; 107 (1): 28– 37. [DOI] [PubMed] [Google Scholar]
- 11-. Young TM, Smith RJ. Effects of orthodontics on the facial profile: A comparison of changes during nonextraction and four premolar extraction treatment. Am J Orthod Dentofacial Orthop. 1993. May; 103 (5): 452– 8. [DOI] [PubMed] [Google Scholar]
- 12-. Verma SL, Sharma VP, Tandon P, Singh GP, Sachan K. Comparison of esthetic outcome after extraction or non-extraction orthodontic treatment in class II division 1 malocclusion patients. Contemp Clin Dent. 2013. April; 4 (2): 206– 12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13-. Bowman SJ, Johnston LE., Jr. The esthetic impact of extraction and nonextraction treatments on Caucasian patients. Angle Orthod. 2000. February; 70 (1): 3– 10. [DOI] [PubMed] [Google Scholar]
- 14-. Paquette DE, Beattie JR, Johnston LE., Jr. A long-term comparison of nonextraction and premolar extraction edgewise therapy in “borderline” Class II patients. Am J Orthod Dentofacial Orthop. 1992. July; 102 (1): 1– 14. [DOI] [PubMed] [Google Scholar]
- 15-. Kachiwala VA, Kalha AS, Machado G. Soft tissue changes associated with first premolar extraction in adult females. Aust Orthod J. 2009. May; 25 (1): 24– 9. [PubMed] [Google Scholar]
- 16-. Singh RN. Changes in the soft tissue chin after orthodontic treatment. Am J Orthod Dentofacial Orthop. 1990. July; 98 (1): 41– 6. [DOI] [PubMed] [Google Scholar]
- 17-. Kumari M, Fida M. Vertical facial and dental arch dimensional changes in extraction vs. non-extraction orthodontic treatment. J Coll Physicians Surg Pak. 2010. January; 20 (1): 17– 21. [PubMed] [Google Scholar]
- 18-. Kocadereli I. The effect of first premolar extraction on vertical dimension. Am J Orthod Dentofacial Orthop. 1999. July; 116 (1): 41– 5. [DOI] [PubMed] [Google Scholar]
- 19-. Jain M, Varghese J, Mascarenhas R, Mogra S, Shetty S, Dhakar N. Assessment of clinical outcomes of Roth and MBT bracket prescription using the American Board of Orthodontics Objective Grading System. Contemp Clin Dent. 2013. July; 4 (3): 307– 12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20-. Hosseinzadeh-Nik T, Farrokhzadeh AM, Golestan B. Horizontal Dental Changes during First Stage of Treatment Using the MBT Technique. J Dent (Tehran) 2007; 4 (1): 9– 14. [Google Scholar]