Abstract
The effects of circuit-like functional high-intensity training (CircuitHIIT) alone or in combination with high-volume low-intensity exercise (Circuitcombined) on selected cardio-respiratory and metabolic parameters, body composition, functional strength and the quality of life of overweight women were compared. In this single-center, two-armed randomized, controlled study, overweight women performed 9-weeks (3 sessions·wk−1) of either CircuitHIIT (n = 11), or Circuitcombined (n = 8). Peak oxygen uptake and perception of physical pain were increased to a greater extent (p < 0.05) by CircuitHIIT, whereas Circuitcombined improved perception of general health more (p < 0.05). Both interventions lowered body mass, body-mass-index, waist-to-hip ratio, fat mass, and enhanced fat-free mass; decreased ratings of perceived exertion during submaximal treadmill running; improved the numbers of push-ups, burpees, one-legged squats, and 30-s skipping performed, as well as the height of counter-movement jumps; and improved physical and social functioning, role of physical limitations, vitality, role of emotional limitations, and mental health to a similar extent (all p < 0.05). Either forms of these multi-stimulating, circuit-like, multiple-joint training can be employed to improve body composition, selected variables of functional strength, and certain dimensions of quality of life in overweight women. However, CircuitHIIT improves peak oxygen uptake to a greater extent, but with more perception of pain, whereas Circuitcombined results in better perception of general health.
Keywords: aerobic fitness, body composition, female, functional training, interval training, power training
Introduction
Programs designed to improve cardiovascular, metabolic, and psychological health have begun to replace low-intensity exercise by repeated short-to-long bouts of high-intensity exercise with intervals of recovery [referred to as high-intensity interval training (HIIT)] (Kessler et al., 2012; Little and Francois, 2014; Elliott et al., 2015; Gielen et al., 2015; Schmitt et al., 2016). In addition to allowing an unlimited number of protocols with different work-to-rest ratios, order of loading and distribution of training intensity, HIIT requires less time than low-intensity-high-volume training, which is attractive, since lack of time appears to be one of the major reasons for not exercising (Godin et al., 1994).
In contrast to the traditional endurance-based HIIT, a relatively novel variation also called functional training/fitness incorporates multi-stimulating, circuit-like, multiple-joint, high-intensity training (CircuitHIIT), and becoming of increasing interest to fitness enthusiasts (Buckley et al., 2015). Such exercise more related to strength can improve body composition (Sillanpää et al., 2009; Neves et al., 2017), as well as cardiovascular (Shaw and Shaw, 2009; Ho et al., 2012a,b), metabolic (Schumann et al., 2014; Neves et al., 2017) and functional fitness (Neves et al., 2017) in physically inactive individuals and, in addition, at least in older individuals, certain aspects of quality of life (Sillanpää et al., 2012). However, with increasing exercise intensity, enjoyment declines, and the excessive demands made by HIIT have been proposed to diminish intrinsic motivation and discourage adherence to further exercise (Hardcastle et al., 2014).
Strength exercise such as CircuitHIIT, is well known to elevate muscle mass and thereby potentially reduce numerous risk factors for cardiovascular disease (Hurley et al., 1988; Poehlman et al., 2000). In contrast, low-intensity endurance exercise is known to augment plasma volume (Green et al., 1987, 1990), muscular blood flow (Coyle, 1999), and capillary and mitochondrial densities (Hoppeler and Weibel, 2000) thereby improving peak oxygen uptake (Hickson et al., 1981). Improved cardiorespiratory fitness (e.g., maximum oxygen uptake) has been associated with improved health and less premature death (Bouchard et al., 2015). Due to the different responses evoked, functional strength training in the form of CircuitHIIT combined with low-intensity endurance exercise (Circuitcombined) may lead to synergistic improvements in cardio-respiratory and metabolic parameters, body composition, functional strength and quality of life, which, to the best of our knowledge, has not yet been investigated in detail with respect to overweight women.
Accordingly, we compare here the psycho-physiological responses of physically inactive women performing a multi-stimulating, circuit-like, multiple-joint conditioning program (CircuitHIIT), or the same program in combination with low-intensity high-volume exercise (Circuitcombined). On the basis of the responses discussed above, our hypothesis was that CircuitHIIT improves functional strength and metabolic parameters as well as body composition, but may at the same time impair quality of life, whereas Circuitcombined improves cardio-respiratory and metabolic parameters and quality of life.
Methods
Participants
In this single-center, two-arm randomized, controlled study, 22 women (age: 23 ± 2 years) recruited via social media platforms and bulletins were initially assigned randomly to perform either CircuitHIIT (n = 11) or Circuitcombined; (n = 8), but three women in the latter group had to withdraw due to time constraints. All were informed in detail about the design of the study, the potential risks and benefits, before providing their written consent to participate. The inclusion criteria were an age of 18–35 years and BMI >25 kg·m−2; not having engaged in routine exercise programs for at least 6 months prior to the study; no daily intake of medication; and completion of more than 80% of the training sessions.
Each woman visited the laboratory once before the actual study to become comfortable performing all exercises. All procedures were conducted in accordance with the Declaration of Helsinki and the protocol was pre-approved by the ethical review board of the Sport Science Institute of the University of Würzburg.
Overall study design
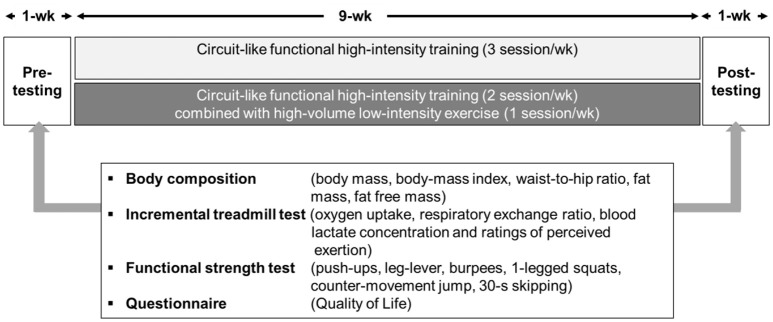
All of the women completed a 9-week intervention involving 3 sessions of either CircuitHIIT or Circuitcombined each week. The overall timeline of this intervention is illustrated in Figure 1.
Figure 1.
The timeline and main outcome variables of this study.
Pre- and post-training testing included assessment of body composition, a treadmill ramp test to assess cardio-respiratory, and metabolic parameters, numerous tests of functional movement, and a questionnaire concerning quality of life. Baseline testing was completed during two visits at least 48 h apart and before assigning the women to one of the interventions. Post-intervention testing, also in two sessions at least 48 h apart, commenced 72 h after the final training session.
The interventions
The 3 weekly sessions of CircuitHIIT were performed either indoors or outdoors, while Circuitcombined involved two sessions of the same nature and a third of low-intensity endurance exercise targeting 65% of peak heart rate (see Table 1 for additional details). Heart rate, especially during the third session during weeks 1, 4, and 7, second session during weeks 2, 5, and 8 and weeks 3, 6 and 9 were monitored continuously (Polar M32, Polar, Oy, Finland).
Table 1.
Details of the 9-week CircuitHIIT and Circuitcombined training interventions.
| Week | Session | CircuitHIIT | Circuitcombined |
|---|---|---|---|
| 1, 4, 7 | 1 | 6 series of - 30-s burpees + 30-s recovery - 30-s skipping + 30-s recovery - 30-s pull-ups + 30-s recovery - 30-s 1-legged squats + 30-s recovery - 30-s leg levers + 30-s recovery - 30-s push-ups + 30-s recovery 7-min Shuttle run |
6 series of - 30-s burpees + 30-s recovery - 30-s skipping + 30-s recovery - 30-s pull-ups + 30-s recovery - 30-s 1-legged squats + 30-s recovery - 30-s leg levers + 30-s recovery - 30-s push-ups + 30-s recovery 7-min Shuttle run |
| 2 | 3 series of - 30-s run/burpees +30-s recovery - 30-s burpees + 30-s leg levers - 60-s lunges + 1-min isometric squat - 45-s rows + 1-min recovery - 8x20-s burpees/plank + 10-s recovery |
3 series of - 30-s run/burpees +30-s recovery - 30-s burpees + 30-s leg levers - 60-s lunges + 1-min isometric squat - 45-s rows + 1-min recovery - 8x20-s burpees/plank + 10-s recovery |
|
| 3 | 5 series of - 30-s burpees + 30-s recovery - 30-s 1-legged squats + 30-s recovery - 30-s push-ups + 30-s recovery - 30-s crunches + 30-s recovery |
4 series of - 10-min jogging + 5-min walking |
|
| 2, 5, 8 | 1 | 3 series of - 45-s lunges/sprints + 30-s recovery - 45-s isometric squat + 30-s recovery - 60-s 1-legged squats + 30-s recovery - 45-s side lunges/sprints + 30-s recovery - 45-s isometric sumo squat + 30-s recovery - 45-s pushups + 30-s rows + 30-s recovery - 30-s plank+30-s skipping + 30-s recovery |
3 series of - 45-s lunges/sprints + 30-s recovery - 45-s isometric squat + 30-s recovery - 60-s 1-legged squats + 30-s recovery - 45-s side lunges/sprints + 30-s recovery - 45-s isometric sumo squat + 30-s recovery - 45-s pushups + 30-s rows + 30-s recovery 30-s plank+30-s skipping + 30-s recovery |
| 2 | 10 series of - 20-s isometric pull-up/push-up + 40-s run + 30-s recovery - 30-s squats/squat jumps + 30-s run + 30-s recovery 3 series of - 45-s rows + 45-s burpees + 3x 30-s lunges + 30-s run + 30-s recovery - 60-s leg levers + 30-s recovery |
4 series of - 10-min jogging + 5-min walking |
|
| 3 | 3 series of - 60-s burpees/run + 30-s recovery - 30-s inchworms/lunges 5 series of - 60-s run + 30-s recovery |
10 series of - 20-s isometric pull-up/push-up + 40-s run + 30-s recovery 30-s squats/squat jumps + 30-s run + 30-s recovery 3 series of - 45-s rows + 45-s burpees 3x 30-s lunges + 30-s run + 30-s recovery 60-s leg levers + 30-s recovery |
|
| 3, 6, 9 | 1 | 2 series of - 60-s jump squats + 30-s recovery - 60-s isometric squat + 30-s recovery - 60-s burpees + 30-s recovery - 60-s 1-legged squats + 30-s recovery - 60-s iron mikes + 30-s recovery - 60-s skipping run + 30-s recovery 10-min Shuttle run |
2 series of - 60-s jump squats + 30-s recovery - 60-s isometric squat + 30-s recovery - 60-s burpees + 30-s recovery - 60-s 1-legged squats + 30-s recovery - 60-s iron mikes + 30-s recovery - 60-s skipping run + 30-s recovery 10-min Shuttle run |
| 2 | 3 series of - 60-s pull-ups + 30-s recovery - 60-s jump rope + 30-s recovery - 60-s push-ups + 30-s recovery - 60-s leg levers + 30-s recovery - 60-s rows + 30-s recovery - 60-s burpees + 30-s recovery 800-m run |
3 series of - 20-min jogging + 10-min walking |
|
| 3 | 3 series - 30-s jumping jacks + 30-s recovery - Skipping + 30-s recovery - Squats + 30-s recovery - 3-min burpees + 30-s recovery - 30-s plank + 30-s lunges + 30-s recovery 15-min run |
3 series of - 60-s pull-ups + 30-s recovery - 60-s jump rope + 30-s recovery - 60-s push-ups + 30-s recovery - 60-s leg levers + 30-s recovery - 60-s rows + 30-s recovery - 60-s burpees + 30-s recovery 800-m run |
Anthropometric data and body composition
Height was measured with a folding yardstick with the subjects standing barefoot. Body fat and fat-free mass were assessed to the nearest 0.1 kg with a four-electrode bio-impedance scale (Model 1609N; Tanita Corp, Tokyo, Japan) and body-mass-index (BMI; in kg·m−2) then calculated. Since dehydration may affect bio-impedance analysis, we instructed all women to consume 500 mL of water 1 h before measurement. The minimal circumference between the iliac crest and rib cage was designated as the waist circumference, the maximal protuberance of the buttocks as the hip circumference, and the waist-to-hip ratio calculated. In our laboratory setting and with repeated measurements, the error of measurement for the waist and hip circumferences is 1.6 and 1.4 cm, respectively, in line with previous findings (Dhaliwal and Welborn, 2009).
The treadmill test
After running for 5 min at 6 km·h−1 on a treadmill (Mercury, h/p/Cosmos Sports & Medical GmbH, Nussdorf-Traunstein, Germany), the submaximal heart rate, oxygen uptake, respiratory exchange ratio, blood lactate concentration, and perceived exertion were all assessed. Thereafter, the speed was increased by 1 km·h−1 each minute until exhaustion for determination of the peak values of these same parameters (Kuipers et al., 2003). Throughout the testing, oxygen uptake, respiratory exchange ratio and heart rate were monitored with an open circuit breath-by-breath gas and volume analyzer (Metamax 3B, Cortex, Leipzig, Germany), employing standard algorithms to compensate for the delay between oxygen consumption and generation of the signal.
All respiratory data and heart rates were averaged over 30-s intervals. The oxygen uptake at 6 km·h−1 was considered to be an indicator of running economy, as described elsewhere (Barnes and Kilding, 2015). The oxygen uptake during the last 30 s of the test was considered to be maximal if (a) this uptake increased <1.0 mL min−1 kg−1 with elevated power output, (b) the respiratory exchange ratio was >1.10, and/or (c) the heart rate was within 5% of the age-predicted maximum. In all cases, at least two of these three criteria were met.
Both after running for 5 min at 6 km·h−1 and at the point of exertion, blood was collected from the right earlobe for analysis of lactate (Lactate Pro 2, Arkray KDK, Kyoto, Japan). With this device and in our laboratory setting, the routinely measured coefficient of variation in repeated measures for blood lactate at rest is 0.07 and 0.04, 0.11, 0.07, 0.06 when running at 70, 80, 90, and 95% of peak heart rate, respectively. At the same time as blood sampling, the rating of perceived exertion (RPE) was assessed employing the 6–20-point Borg scale (Borg, 1970).
Testing functional strength
During all tests of functional strength (separated by 3-min intervals of recovery) the women were asked to perform as many push-ups, leg-levers, burpees, and one-legged squats as they could.
Counter-movement jump and 30-s skipping
The explosive strength of the leg muscles was examined utilizing three counter-movement jumps (OptoJump, MicroGate, Bolzano, Italy) separated by a 1-min rest period, with the best of the three being subjected to further analysis. In the same testing device, the number of times each woman could skip rope within a 30-s period was recorded.
Assessment of quality of life
Prior to baseline testing and again before post-testing, all of the women completed the German version of the health-related quality of life questionnaire (SF-36), which has been shown to be valid and reliable (Bullinger et al., 1995). This questionnaire assesses general health, physical functioning, mental health, social functioning, vitality, bodily pain, and the roles of physical and emotional limitations, with higher scores (0–100) reflecting better quality of life.
Statistical analyses
All data were confirmed to be normally distributed by the Kolmogorov-Smirnov test, so that no transformation was required. Repeated-measures ANOVA [time-point (pre- or post-exercise) × group (CircuitHIIT or Circuitcombined)] was performed for each outcome variable, with an alpha of p < 0.05 being considered statistically significant and indicated by *. In addition, the values obtained were evaluated by calculating the effect size partial eta-square (). The means and standard deviations (SD) for all data sets were calculated and all statistical tests carried out in the SPSS 22.0 software package for Microsoft. The smallest worthwhile effect was defined as the smallest Cohen change in the mean, i.e., 0.2 times the SD of the between-subject baseline values for all participants (Batterham and Hopkins, 2006). Chances of benefit and harm were assessed qualitatively as follows: <1% almost certainly none, 1–5% very unlikely, 5–25% unlikely, 25–75% possibly, 75–95% likely, 95–99% very likely, >99% almost certainly (Hopkins, 2002).
Results
The women in the CircuitHIIT and Circuitcombined groups completed 89 ± 5 and 90 ± 6% of the planned training sessions, respectively. Their pre- and post-values with statistical analysis are documented in Tables 2–5.
Table 2.
Anthropometric values (means ± SD) for the women in the CircuitHIIT and Circuitcombined groups before and after the intervention.
| Parameter | Intervention | Before | After | p(T)/p(T × G) | (T)/(T × G) | F | Mean effecta± 90% CIb | Qualitative inference |
|---|---|---|---|---|---|---|---|---|
| Body mass [kg] | CircuitHIIT | 79.7 ± 7.5 | 77.7 ± 8.2 | 0.02* | 0.243 | 6.41 | −2.0 ± 2.1 | Likely positive |
| Circuitcombined | 83.0 ± 10.5 | 82.5 ± 11.0 | 0.121 | 0.116 | 2.62 | |||
| Body mass index [kg·m−2] | CircuitHIIT | 28.1 ± 2.7 | 27.3 ± 2.8 | 0.015* | 0.263 | 7.12 | −2.0 ± 2.1 | Likely positive |
| Circuitcombined | 28.3 ± 3.3 | 28.1 ± 3.2 | 0.124 | 0.114 | 2.58 | |||
| Waist-to-hip ratio | CircuitHIIT | 0.80 ± 0.06 | 0.75 ± 0.05 | 0.003** | 0.359 | 11.2 | −5.1 ± 4.6 | Unclear |
| Circuitcombined | 0.79 ± 0.03 | 0.78 ± 0.04 | 0.340 | 0.046 | 0.956 | |||
| Fat mass [kg] | CircuitHIIT | 40.0 ± 4.9 | 38.1 ± 5.6 | 0.002** | 0.401 | 13.4 | −2.5 ± 3.9 | Likely positive |
| Circuitcombined | 40.2 ± 4.8 | 39.2 ± 5.6 | 0.240 | 0.068 | 1.47 | |||
| Fat free mass [%] | CircuitHIIT | 26.5 ± 2.4 | 27.4 ± 2.6 | 0.003** | 0.359 | 11.2 | 1.6 ± 2.9 | Likely positive |
| Circuitcombined | 26.4 ± 2.0 | 26.9 ± 2.5 | 0.340 | 0.046 | 0.956 |
HIIT, high-intensity interval training; p, probability; , effect size partial eta-square; T, global effect of time; G, global effect of group; T × G, global effect of Time × Group; F, degrees of freedom.
P < 0.05,
P < 0.01 for the differences between groups.
Refers to CircuitHIIT minus Circuitcombined.
± 90% CI: add or subtract this number from the mean effect to obtain the 90% confidence intervals for the true difference.
Body mass, body-mass index, waist-to-hip ratio and fat mass declined and fat-free mass increased to the same extent in both groups (Table 2).
Ratings of perceived exertion following either intervention were lower than at baseline. Peak oxygen uptake improved to a greater extent following CircuitHIIT than Circuitcombined (Table 3).
Table 3.
Cardio-respiratory and metabolic values and perceived exertion (means ± SD) of the women in the CircuitHIIT and Circuitcombined groups before and after the intervention.
| Intervention | Before | After | p(T)/p(T × G) | (T)/(T × G) | F | Mean effecta± 90% CIb | Qualitative inference | |
|---|---|---|---|---|---|---|---|---|
| VALUES AT A SUBMAXIMAL RUNNING SPEED OF 6 KM·H−1 | ||||||||
| Heart rate [bpm] | CircuitHIIT | 166 ± 18 | 160 ± 18 | 0.087 | 0.140 | 3.250 | −2.3 ± 4.4 | Likely positive |
| Circuitcombined | 167 ± 14 | 165 ± 12 | 0.424 | 0.032 | 0.665 | |||
| Oxygen uptake [ml·min−1] | CircuitHIIT | 2,070 ± 206 | 2,110 ± 141 | 0.742 | 0.006 | 0.112 | 3.4 ± 6.8 | Likely positive |
| Circuitcombined | 2,130 ± 311 | 2,110 ± 304 | 0.391 | 0.039 | 0.770 | |||
| Respiratory exchange ratio | CircuitHIIT | 0.93 ± 0.09 | 0.91 ± 0.10 | 0.136 | 0.113 | 2.430 | 2.5 ± 8.3 | Unclear |
| Circuitcombined | 0.94 ± 0.10 | 0.89 ± 0.07 | 0.556 | 0.019 | 0.359 | |||
| Blood lactate concentration [mmol·L−1] | CircuitHIIT | 4.4 ± 2.0 | 3.1 ± 1.2 | 0.017 | 0.265 | 6.850 | −25.3 ± 17.7 | Very likely positive |
| Circuitcombined | 4.0 ± 2.3 | 3.7 ± 1.7 | 0.088 | 0.146 | 3.25 | |||
| Ratings of perceived exertion [a.u.] | CircuitHIIT | 12.0 ± 1.6 | 9.5 ± 2.0 | <0.001*** | 0.683 | 36.6 | −7.6 ± 11.5 | Likely positive |
| Circuitcombined | 13.1 ± 2.0 | 11.1 ± 1.9 | 0.510 | 0.026 | 0.452 | |||
| PEAK VALUES AT THE POINT OF EXERTION | ||||||||
| Maximal oxygen uptake [ml·min−1] | CircuitHIIT | 2,630 ± 297 | 2,900 ± 298 | <0.001*** | 0.612 | 30.0 | 5.8 ± 4.9 | Very likely positive |
| Circuitcombined | 2,560 ± 348 | 2,670 ± 398 | 0.038* | 0.207 | 4.95 | |||
| Respiratory exchange ratio | CircuitHIIT | 1.23 ± 0.08 | 1.17 ± 0.08 | 0.102 | 0.134 | 2.95 | −2.4 ± 7.6 | Unclear |
| Circuitcombined | 1.18 ± 0.09 | 1.15 ± 0.07 | 0.591 | 0.016 | 0.299 | |||
| Blood lactate concentration [mmol·L−1] | CircuitHIIT | 7.0 ± 2.1 | 8.0 ± 2.8 | 0.645 | 0.011 | 0.220 | 26.5 ± 37.4 | Likely positive |
| Circuitcombined | 7.0 ± 2.2 | 6.5 ± 2.5 | 0.128 | 0.118 | 2.54 | |||
| Ratings of perceived exertion [a.u.] | CircuitHIIT | 18.2 ± 1.5 | 17.9 ± 2.2 | 0.396 | 0.038 | 0.755 | 0.9 ± 9.2 | Unclear |
| Circuitcombined | 17.8 ± 1.8 | 17.3 ± 1.6 | 0.801 | 0.003 | 0.065 | |||
HIIT, high-intensity interval training; p, probability; , effect size partial eta-square; T, global effect of time; G, global effect of group; T × G, global effect of Time × Group; F, degrees of freedom; a.u, arbitrary units.
P < 0.05,
P < 0.001 for the differences between groups.
Refers to CircuitHIIT minus Circuitcombined.
± 90% CI: add or subtract this number from the mean effect to obtain the 90% confidence intervals for the true difference.
The number of push-ups, burpees, one-legged squats and 30-s skipping, as well as the counter-movement jumping height improved after both CircuitHIIT and Circuitcombined, with no differences between these groups (Table 3). The number of leg-levers was improved to a greater extent by CircuitHIIT than Circuitcombined (Table 4).
Table 4.
Funtional performance (means ± SD) of the women in the CircuitHIIT and Circuitcombined groups before and after the intervention.
| Parameter | Intervention | Before | After | p(T)/p(T × G) | (T)/(T × G) | F | Mean effecta ± 90% CIb | Qualitative inference |
|---|---|---|---|---|---|---|---|---|
| Push-ups [n] | CircuitHIIT | 7.5 ± 3.6 | 19.6 ± 4.2 | <0.001*** | 0.869 | 119 | −23.2 ± 47.8 | Unclear |
| Circuitcombined | 4.3 ± 4.0 | 17.4 ± 6.1 | 0.663 | 0.011 | 0.196 | |||
| Leg-levers [n] | CircuitHIIT | 15.7 ± 11.0 | 58.5 ± 22.3 | <0.001*** | 0.754 | 55.0 | 120.4 ±84.5 | Likely positive |
| Circuitcombined | 15.9 ± 8.0 | 28.3 ± 6.5 | 0.001*** | 0.480 | 16.6 | |||
| Burpees [n] | CircuitHIIT | 9.2 ± 3.7 | 24.9 ± 9.9 | <0.001*** | 0.753 | 57.8 | −28.0 ± 33.6 | Likely negative |
| Circuitcombined | 7.0 ± 2.7 | 27.6 ± 10.8 | 0.321 | 0.052 | 1.04 | |||
| 1-Legged squats [n] | CircuitHIIT | 18.0 ± 8.2 | 36.9 ± 10.1 | <0.001*** | 0.868 | 125 | −32.7 ± 24.6 | Very likely negative |
| Circuitcombined | 13.7 ± 5.9 | 39.9 ± 9.4 | 0.086 | 0.147 | 3.28 | |||
| Counter-movement jump [cm] | CircuitHIIT | 23.8 ± 7.0 | 28.3 ± 7.2 | 0.017* | 0.253 | 6.79 | 16.4 ±16.8 | Likely positive |
| Circuitcombined | 24.8 ± 5.1 | 25.3 ± 3.2 | 0.050 | 0.178 | 4.33 | |||
| 30-s Skipping [n] | CircuitHIIT | 84.0 ± 32.2 | 116 ± 8.3 | <0.001*** | 0.679 | 38.0 | −19.0 ± 25.1 | Likely negative |
| Circuitcombined | 76.6 ± 21.9 | 136 ± 37.0 | 0.074 | 0.167 | 3.60 |
HIIT, high-intensity interval training; p, probability; , effect size partial eta-square; T, global effect of time; G, global effect of group; T × G, global effect of Time × Group; F, degrees of freedom.
P < 0.05,
P < 0.001 for the differences between groups.
Refers to the CircuitHIIT minus Circuitcombined.
± 90% CI: add or subtract this number from the mean effect to obtain the 90% confidence intervals for the true difference.
Physical and social functioning, vitality, role of emotional limitations and mental health improved following both CircuitHIIT and Circuitcombined (Table 5). However, perception of physical pain was higher only after CircuitHIIT and perception of general health was enhanced only by Circuitcombined.
Table 5.
Quality of Life (arbitrary units, means ± SD) for the women in the CircuitHIIT and Circuitcombined groups before and after the intervention.
| Dimension | Intervention | Before | After | p(T)/p(T × G) | (T)/(T × G) | F | Mean effecta ± 90% CIb | Qualitative inference |
|---|---|---|---|---|---|---|---|---|
| Physical functioning | CircuitHIIT | 94 ± 5.5 | 98 ± 3 | 0.008** | 0.317 | 8.82 | −7.6 ± 10.4 | Likely negative |
| Circuitcombined | 87 ± 14 | 97 ± 4 | 0.228 | 0.075 | 1.55 | |||
| Role of physical limitations | CircuitHIIT | 100 ± 0 | 98 ± 8 | 0.439 | 0.032 | 0.624 | 0.3 ± 16.1 | Unclear |
| Circuitcombined | 95 ± 16 | 93 ± 17 | 0.970 | 0.000 | 0.001 | |||
| Pain | CircuitHIIT | 96 ± 9 | 74 ± 19 | 0.008** | 0.320 | 8.93 | −24.5 ± 14.3 | Very likely negative |
| Circuitcombined | 91 ± 19 | 90 ± 17 | 0.016* | 0.270 | 7.04 | |||
| Perception of general health | CircuitHIIT | 74 ± 15 | 74 ± 18 | 0.039* | 0.206 | 4.94 | −23.1 ± 16.3 | Very likely negative |
| Circuitcombined | 66 ± 18 | 83 ± 17 | 0.037* | 0.210 | 5.05 | |||
| Vitality | CircuitHIIT | 58 ± 13 | 66 ± 10 | 0.001** | 0.427 | 14.2 | −11.7 ± 17.4 | Likely negative |
| Circuitcombined | 49 ± 14 | 63 ± 13 | 0.336 | 0.049 | 0.975 | |||
| Social functioning | CircuitHIIT | 77 ± 18 | 94 ± 10 | 0.009** | 0.306 | 8.38 | 18.0 ± 19.8 | Likely positive |
| Circuitcombined | 91 ± 10 | 96 ± 8 | 0.130 | 0.116 | 2.50 | |||
| Role of emotional limitations | CircuitHIIT | 73 ± 29 | 91 ± 22 | 0.015* | 0.273 | 7.14 | 3.0 ± 42.0 | Unclear |
| Circuitcombined | 77 ± 39 | 93 ± 21 | 0.909 | 0.001 | 0.014 | |||
| Mental health | CircuitHIIT | 72 ± 14 | 76 ± 11 | 0.013* | 0.285 | 7.57 | −8.0 ± 12.4 | Likely negative |
| Circuitcombined | 68 ± 11 | 79 ± 12 | 0.222 | 0.078 | 1.60 |
HIIT, high-intensity interval training; p, probability; , effect size partial eta-square; T, global effect of time; G, global effect of group; T × G, global effect of Time × Group; F, degrees of freedom.
P < 0.05,
P < 0.01 for the difference between groups.
Refers to CircuitHIIT minus Circuitcombined.
± 90% CI: add or subtract this number from the mean effect to obtain the 90% confidence intervals for the true difference.
Discussion
The major findings of this comparison of several psycho-physiological responses of overweight women to 9 weeks of either CircuitHIIT or Circuitcombined were as follows:
With CircuitHIIT, perception of physical pain and peak oxygen uptake both rose to a greater extent.
Perception of general health was improved more by Circuitcombined.
- Both interventions caused the following changes to a similar degree:
- - lowering of body mass, body-mass index, waist-to-hip ratio, and fat mass and increase in fat-free mass;
- - decreased ratings of perceived exertion during submaximal treadmill running;
- - improvements in the number of push-ups, burpees, one-legged squats, and 30-s skipping, as well as counter-movement jump height;
- - improvements in physical and social functioning, role of physical limitations, vitality, role of emotional limitations and mental health.
Numerous investigations have focused on the effect of HIIT on parameters of cardio-respiratory fitness including VO2peak (Stoggl and Sperlich, 2014; Schmitt et al., 2016; Zinner et al., 2016). Since this value limits ATP production via oxidative phosphorylation and is thus strongly associated with cardiorespiratory fitness, as well as general health and premature death, it is frequently utilized as an integrative indicator of cardiopulmonary fitness (Bassett and Howley, 2000; Bouchard et al., 2015). Here, peak oxygen uptake was improved after 9 weeks with 3 weekly sessions of either CircuitHIIT (10.1%) or Circuitcombined (4.4%). The overall greater response of VO2peak to high-intensity exercise can be explained by better central adaptation, including augmented plasma and blood volumes (Convertino et al., 1980; Green et al., 1987; Graham et al., 2016) with elevated stroke volume (Green et al., 1990; Goodman et al., 2005).
From this point of view, we may conclude that three sessions of CircuitHIIT enhance VO2peak more effectively than two sessions of CircuitHIIT and one session of low-intensity exercise (Circuitcombined).
The CircuitHIIT participants performed primarily resistance training (i.e., squats, lunges, push-ups, etc.) in combination with repeated sprints, with very little rest between these exercises. Although this regimen was more related to strength, the women enhanced their cardiorespiratory fitness (i.e., oxygen uptake) to an extent similar to that observed with earlier circuit-based exercise (Gettman et al., 1982; Beckham and Earnest, 2000). A 7–12% increase in peak oxygen uptake following 4–12 weeks of body weight circuit training is consistent with previous reports (Gettman et al., 1982; McRae et al., 2012). However, our present observations reveal that 3 weekly sessions of CircuitHIIT improve peak oxygen uptake in a time-effective manner.
Circuitcombined consisted of two of the weekly CircuitHIIT sessions and an additional weekly session of high-volume exercise (60–105 min at approximately 65% of peak oxygen uptake). In the case of well-trained endurance athletes a combination of HIIT and high-volume low-intensity exercise might be more beneficial than either alone, since a) low-intensity endurance exercise (<2 mM blood lactate or ~55–85% peak heart rate) allows the body to recover sufficiently and b) excess HIIT may exert a negative impact on the autonomic nervous system (Chwalbinska-Moneta et al., 1998; Esteve-Lanao et al., 2007). Although the combination of low-volume, high-intensity exercise and high-volume, low-intensity exercise (so-called polarized intensity distribution) led to greater improvements in selected endurance values for elite endurance athletes (Stöggl and Sperlich, 2015), our present findings indicate that this is not the case for overweight women performing multi-stimulating, circuit-like, multiple-joint training together with high-volume low-intensity exercise (Circuitcombined).
In the current investigation, the women in the CircuitHIIT group perceived more pain, with no change in perception of general health. High-intensity strength training with eccentric components such as those involved in multi-stimulating, circuit-like, multiple-joint training induces muscle soreness. Although in general in adults, perception of muscle pain is attenuated as training proceeds, (Levinger et al., 2007), the women in the CircuitHIIT group perceived more pain after the 9-week intervention. The injury rate associated with multi-stimulating, circuit-like, multiple-joint training is approximately 20% (Weisenthal et al., 2014), but none of the women in either of our groups mentioned any injury. However, elevated pain in connection with HIIT may discourage untrained individuals from performing regular physical activity (Hardcastle et al., 2014; Del Vecchio et al., 2015), although previous studies showed no effect of high-intensity exercise on perceived pain in female patients (Schmitt et al., 2016). Further studies are needed to clarify the effect of high-intensity training, especially short- and long-term, on perceived pain. However, CircuitHIIT and Circuitcombined induced improvements in several dimensions of quality of life, which are perhaps the most important reasons to continue training. To summarize, in the present investigation Circuitcombined appears to have augmented certain aspects of quality of life somewhat more, because there was no enhanced perception of pain.
Limitations
This study was not designed specifically to assess improvements in body composition, but rather to compare the responses of cardio-respiratory and metabolic parameters, body composition, functional strength and quality of life to CircuitHIIT and CircuitCombined. Although we instructed our participants not to alter their eating habits, we cannot exclude the possibility that some nonetheless altered their nutritional intake. Since the study was relatively time-consuming, we did not ask the women to maintain nutritional diaries as well.
Since CircuitHIIT and CircuitCombined can be designed in very many different ways, we cannot be certain that the exercise described here is superior to other protocols. Nor can we generalize the responses observed to other populations, such as men, younger, and older individuals, or those with greater fitness.
Practical implications
Depending on the training goal, both CircuitHIIT and Circuitcombined achieve potent improvements in body composition, selected parameters of functional strength, and certain dimensions of quality of life in overweight women. Moreover, CircuitHIIT improves peak oxygen uptake, which is associated with improved health and less risk for premature death (Bouchard et al., 2015), in less training time, but with more perception of pain. More pain could, in turn, diminish pleasure and, thereby, the motivation to continue a program of exercise (Hardcastle et al., 2014).
Circuitcombined appears to improve perception of general health to a greater extent than CircuitHIIT and, if this is the goal, Circuitcombined seems to be the method of choice.
Conclusion
Nine weeks of multi-stimulating, circuit-like, multiple-joint training involving either CircuitHIIT or Circuitcombined improved the body composition, selected variables of functional strength and certain dimensions of quality of life in overweight women. CircuitHIIT also improved peak oxygen uptake, but with more perception of pain. Circuitcombined appears to improve perception of general health to a greater extent than CircuitHIIT.
Author contributions
BS, BWS, CZ, VVS, HL, HCH designed and approved the methods, analyzed data, and assisted in manuscript writting. BS, VVS, HL, CZ performed data collection.
Conflict of interest statement
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
References
- Barnes K. R., Kilding A. E. (2015). Strategies to improve running economy. Sports Med. 45, 37–56. 10.1007/s40279-014-0246-y [DOI] [PubMed] [Google Scholar]
- Bassett D. R., Jr., Howley E. T. (2000). Limiting factors for maximum oxygen uptake and determinants of endurance performance. Med. Sci. Sports Exerc. 32, 70–84. 10.1097/00005768-200001000-00012 [DOI] [PubMed] [Google Scholar]
- Batterham A. M., Hopkins W. G. (2006). Making meaningful inferences about magnitudes. Int. J. Sports Physiol. Perform. 1, 50–57. 10.1123/ijspp.1.1.50 [DOI] [PubMed] [Google Scholar]
- Beckham S. G., Earnest C. P. (2000). Metabolic cost of free weight circuit weight training. J. Sports Med. Phys. Fitness 40, 118–125. Available online at: http://www.minervamedica.it/en/journals/sports-med-physical-fitness/article.php?cod=R40Y2000N02A0118 [PubMed] [Google Scholar]
- Borg G. (1970). Perceived exertion as an indicator of somatic stress. Scand. J. Rehabil. Med. 2, 92–98. [PubMed] [Google Scholar]
- Bouchard C., Blair S. N., Katzmarzyk P. T. (2015). Less sitting, more physical activity, or higher fitness? Mayo Clin. Proc. 90, 1533–1540. 10.1016/j.mayocp.2015.08.005 [DOI] [PubMed] [Google Scholar]
- Buckley S., Knapp K., Lackie A., Lewry C., Horvey K., Benko C., et al. (2015). Multimodal high-intensity interval training increases muscle function and metabolic performance in females. Appl. Physiol. Nutr. Metab. 40, 1157–1162. 10.1139/apnm-2015-0238 [DOI] [PubMed] [Google Scholar]
- Bullinger M., Kirchberger I., Ware J. (1995). Der deutsche SF-36 Health Survey Übersetzung und psychometrische Testung eines krankheitsübergreifenden Instruments zur Erfassung der gesundheitsbezogenen Lebensqualität. Zeitschrift für Gesundheitswissenschaften. J. Public Health 3, 21–36. 10.1007/BF02959944 [DOI] [Google Scholar]
- Chwalbinska-Moneta J., Kaciuba-Uscilko H., Krysztofiak H., Ziemba A., Krzeminski K., Kruk B., et al. (1998). Relationship between EMG blood lactate, and plasma catecholamine thresholds during graded exercise in men. J. Physiol. Pharmacol. 49, 433–441. [PubMed] [Google Scholar]
- Convertino V. A., Brock P. J., Keil L. C., Bernauer E. M., Greenleaf J. E. (1980). Exercise training-induced hypervolemia: role of plasma albumin, renin, and vasopressin. J. Appl. Physiol. Respir. Environ. Exerc. Physiol. 48, 665–669. [DOI] [PubMed] [Google Scholar]
- Coyle E. F. (1999). Physiological determinants of endurance exercise performance. J. Sci. Med. Sport 2, 181–189. 10.1016/S1440-2440(99)80172-8 [DOI] [PubMed] [Google Scholar]
- Del Vecchio F. B., Gentil P., Coswig V. S., Fukuda D. H. (2015). Commentary: why sprint interval training is inappropriate for a largely sedentary population. Front. Psychol. 6:1359. 10.3389/fpsyg.2015.01359 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dhaliwal S. S., Welborn T. A. (2009). Measurement error and ethnic comparisons of measures of abdominal obesity. Prev. Med. 49, 148–152. 10.1016/j.ypmed.2009.06.023 [DOI] [PubMed] [Google Scholar]
- Elliott A. D., Rajopadhyaya K., Bentley D. J., Beltrame J. F., Aromataris E. C. (2015). Interval training versus continuous exercise in patients with coronary artery disease: a meta-analysis. Heart Lung Circ. 24, 149–157. 10.1016/j.hlc.2014.09.001 [DOI] [PubMed] [Google Scholar]
- Esteve-Lanao J., Foster C., Seiler S., Lucia A. (2007). Impact of training intensity distribution on performance in endurance athletes. J. Strength Cond. Res. 21, 943–949. 10.1519/00124278-200708000-00048 [DOI] [PubMed] [Google Scholar]
- Gettman L. R., Ward P., Hagan R. D. (1982). A comparison of combined running and weight training with circuit weight training. Med. Sci. Sports Exerc. 14, 229–234. 10.1249/00005768-198203000-00014 [DOI] [PubMed] [Google Scholar]
- Gielen S., Laughlin M. H., O'conner C., Duncker D. J. (2015). Exercise training in patients with heart disease: review of beneficial effects and clinical recommendations. Prog. Cardiovasc. Dis. 57, 347–355. 10.1016/j.pcad.2014.10.001 [DOI] [PubMed] [Google Scholar]
- Godin G., Desharnais R., Valois P., Lepage L., Jobin J., Bradet R. (1994). Differences in perceived barriers to exercise between high and low intenders: observations among different populations. Am. J. Health Promot. 8, 279–385. 10.4278/0890-1171-8.4.279 [DOI] [Google Scholar]
- Goodman J. M., Liu P. P., Green H. J. (2005). Left ventricular adaptations following short-term endurance training. J. Appl. Physiol. 98, 454–460. 10.1152/japplphysiol.00258.2004 [DOI] [PubMed] [Google Scholar]
- Graham M. J., Lucas S. J., Francois M. E., Stavrianeas S., Parr E. B., Thomas K. N., et al. (2016). Low-volume intense exercise elicits post-exercise hypotension and subsequent hypervolemia, irrespective of which limbs are exercised. Front. Physiol. 7:199. 10.3389/fphys.2016.00199 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Green H. J., Jones L. L., Hughson R. L., Painter D. C., Farrance B. W. (1987). Training-induced hypervolemia: lack of an effect on oxygen utilization during exercise. Med. Sci. Sports Exerc. 19, 202–206. 10.1249/00005768-198706000-00003 [DOI] [PubMed] [Google Scholar]
- Green H. J., Jones L. L., Painter D. C. (1990). Effects of short-term training on cardiac function during prolonged exercise. Med. Sci. Sports Exerc. 22, 488–493. 10.1249/00005768-199008000-00012 [DOI] [PubMed] [Google Scholar]
- Hardcastle S. J., Ray H., Beale L., Hagger M. S. (2014). Why sprint interval training is inappropriate for a largely sedentary population. Front. Psychol. 5:1505. 10.3389/fpsyg.2014.01505 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hickson R. C., Hagberg J. M., Ehsani A. A., Holloszy J. O. (1981). Time course of the adaptive responses of aerobic power and heart rate to training. Med. Sci. Sports Exerc. 13, 17–20. 10.1249/00005768-198101000-00012 [DOI] [PubMed] [Google Scholar]
- Ho S. S., Dhaliwal S. S., Hills A. P., Pal S. (2012a). The effect of 12 weeks of aerobic, resistance or combination exercise training on cardiovascular risk factors in the overweight and obese in a randomized trial. BMC Public Health 12:704. 10.1186/1471-2458-12-704 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ho S. S., Radavelli-Bagatini S., Dhaliwal S. S., Hills A. P., Pal S. (2012b). Resistance, aerobic, and combination training on vascular function in overweight and obese adults. J. Clin. Hypertens. 14, 848–854. 10.1111/j.1751-7176.2012.00700.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hopkins W. G. (2002). Probabilitites of clinical or practical significance. Sportscience 6 Available online at: http://www.sportsci.org/jour/0201/wghprob.htm
- Hoppeler H., Weibel E. R. (2000). Structural and functional limits for oxygen supply to muscle. Acta Physiol. Scand. 168, 445–456. 10.1046/j.1365-201x.2000.00696.x [DOI] [PubMed] [Google Scholar]
- Hurley B. F., Hagberg J. M., Goldberg A. P., Seals D. R., Ehsani A. A., Brennan R. E., et al. (1988). Resistive training can reduce coronary risk factors without altering VO2max or percent body fat. Med. Sci. Sports Exerc. 20, 150–154. 10.1249/00005768-198820020-00008 [DOI] [PubMed] [Google Scholar]
- Kessler H. S., Sisson S. B., Short K. R. (2012). The potential for high-intensity interval training to reduce cardiometabolic disease risk. Sports Med. 42, 489–509. 10.2165/11630910-000000000-00000 [DOI] [PubMed] [Google Scholar]
- Kuipers H., Rietjens G., Verstappen F., Schoenmakers H., Hofman G. (2003). Effects of stage duration in incremental running tests on physiological variables. Int. J. Sports Med. 24, 486–491. 10.1055/s-2003-42020 [DOI] [PubMed] [Google Scholar]
- Levinger I., Goodman C., Hare D. L., Jerums G., Selig S. (2007). The effect of resistance training on functional capacity and quality of life in individuals with high and low numbers of metabolic risk factors. Diabetes Care 30, 2205–2210. 10.2337/dc07-0841 [DOI] [PubMed] [Google Scholar]
- Little J. P., Francois M. E. (2014). High-intensity interval training for improving postprandial hyperglycemia. Res. Q. Exerc. Sport 85, 451–456. 10.1080/02701367.2014.963474 [DOI] [PubMed] [Google Scholar]
- McRae G., Payne A., Zelt J. G., Scribbans T. D., Jung M. E., Little J. P., et al. (2012). Extremely low volume, whole-body aerobic-resistance training improves aerobic fitness and muscular endurance in females. Appl. Physiol. Nutr. Metab. 37, 1124–1131. 10.1139/h2012-093 [DOI] [PubMed] [Google Scholar]
- Neves L. M., Fortaleza A. C., Rossi F. E., Diniz T. A., Codogno J. S., Gobbo L. A., et al. (2017). Functional training reduces body fat and improves functional fitness and cholesterol levels in postmenopausal women: a randomized clinical trial. J. Sports Med. Phys. Fitness 57, 448–456. 10.23736/S0022-4707.17.06062-5 [DOI] [PubMed] [Google Scholar]
- Poehlman E. T., Dvorak R. V., Denino W. F., Brochu M., Ades P. A. (2000). Effects of resistance training and endurance training on insulin sensitivity in nonobese, young women: a controlled randomized trial. J. Clin. Endocrinol. Metab. 85, 2463–2468. 10.1210/jc.85.7.2463 [DOI] [PubMed] [Google Scholar]
- Schmitt J., Lindner N., Reuss-Borst M., Holmberg H.-C., Sperlich B. (2016). A 3-week multimodal intervention involving high-intensity interval training in female cancer survivors: a randomized controlled trial. Physiol. Rep. 4:e12693. 10.14814/phy2.12693 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schumann M., Küüsmaa M., Newton R. U., Sirparanta A. I., Syväoja H., Hääkkinen A., et al. (2014). Fitness and lean mass increases during combined training independent of loading order. Med. Sci. Sports Exerc. 46, 1758–1768. 10.1249/MSS.0000000000000303 [DOI] [PubMed] [Google Scholar]
- Shaw B. S., Shaw I. (2009). Compatibility of concurrent aerobic and resistance training on maximal aerobic capacity in sedentary males. Cardiovasc. J. Afr. 20, 104–106. Available online at: http://blues.sabinet.co.za/WebZ/Authorize?sessionid=0:autho=pubmed:password=pubmed2004&/AdvancedQuery?&format=F&next=images/ejour/cardio1/cardio1_v20_n2_a3.pdf [PMC free article] [PubMed] [Google Scholar]
- Sillanpää E., Häkkinen K., Holviala J., Häkkinen A. (2012). Combined strength and endurance training improves health-related quality of life in healthy middle-aged and older adults. Int. J. Sports Med. 33, 981–986. 10.1055/s-0032-1311589 [DOI] [PubMed] [Google Scholar]
- Sillanpää E., Laaksonen D. E., Häkkinen A., Karavirta L., Jensen B., Kraemer W. J., et al. (2009). Body composition, fitness, and metabolic health during strength and endurance training and their combination in middle-aged and older women. Eur. J. Appl. Physiol. 106, 285–296. 10.1007/s00421-009-1013-x [DOI] [PubMed] [Google Scholar]
- Stöggl T. L., Sperlich B. (2015). The training intensity distribution among well-trained and elite endurance athletes. Front. Physiol. 6:295. 10.3389/fphys.2015.00295 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stoggl T., Sperlich B. (2014). Polarized training has greater impact on key endurance variables than threshold, high intensity, or high volume training. Front. Physiol. 5:33 10.3389/fphys.2014.00033 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weisenthal B. M., Beck C. A., Maloney M. D., Dehaven K. E., Giordano B. D. (2014). Injury rate and patterns among crossfit athletes. Orthop. J. Sports Med. 2:2325967114531177. 10.1177/2325967114531177 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zinner C., Sperlich B., Born D. P., Michels G. (2016). Effects of combined high intensity arm and leg training on performance and cardio-respiratory measures. J. Sports Med. Phys. Fitness [Epub ahead of print]. [DOI] [PubMed] [Google Scholar]