Abstract
Objectives
The aim of this study was to investigate the effect of granulocyte-colony stimulating factor (G-CSF) on mesenchymal stem cell (MSC) proliferation in vitro and to determine whether pre-microfracture systemic administration of G-CSF (a bone marrow stimulant) could improve the quality of repaired tissue of a full-thickness cartilage defect in a rabbit model.
Methods
MSCs from rabbits were cultured in a control medium and medium with G-CSF (low-dose: 4 μg, high-dose: 40 μg). At one, three, and five days after culturing, cells were counted. Differential potential of cultured cells were examined by stimulating them with a osteogenic, adipogenic and chondrogenic medium.
A total of 30 rabbits were divided into three groups. The low-dose group (n = 10) received 10 μg/kg of G-CSF daily, the high-dose group (n = 10) received 50 μg/kg daily by subcutaneous injection for three days prior to creating cartilage defects. The control group (n = 10) was administered saline for three days. At 48 hours after the first injection, a 5.2 mm diameter cylindrical osteochondral defect was created in the femoral trochlea. At four and 12 weeks post-operatively, repaired tissue was evaluated macroscopically and microscopically.
Results
The cell count in the low-dose G-CSF medium was significantly higher than that in the control medium. The differentiation potential of MSCs was preserved after culturing them with G-CSF.
Macroscopically, defects were filled and surfaces were smoother in the G-CSF groups than in the control group at four weeks. At 12 weeks, the quality of repaired cartilage improved further, and defects were almost completely filled in all groups. Microscopically, at four weeks, defects were partially filled with hyaline-like cartilage in the G-CSF groups. At 12 weeks, defects were repaired with hyaline-like cartilage in all groups.
Conclusions
G-CSF promoted proliferation of MSCs in vitro. The systemic administration of G-CSF promoted the repair of damaged cartilage possibly through increasing the number of MSCs in a rabbit model.
Cite this article: T. Sasaki, R. Akagi, Y. Akatsu, T. Fukawa, H. Hoshi, Y. Yamamoto, T. Enomoto, Y. Sato, R. Nakagawa, K. Takahashi, S. Yamaguchi, T. Sasho. The effect of systemic administration of G-CSF on a full-thickness cartilage defect in a rabbit model MSC proliferation as presumed mechanism: G-CSF for cartilage repair. Bone Joint Res 2017;6:123–131. DOI: 10.1302/2046-3758.63.BJR-2016-0083.
Keywords: G-CSF, Cartilage defects, Microfracture
Article focus
We hypothesised that pre-microfracture systemic administration of granulocyte-colony stimulating factor (G-CSF) will improve the quality of repaired tissue in full-thickness articular cartilage defects in a rabbit model.
Key messages
The in vitro administration of G-CSF resulted in proliferation of MSCs.
The systemic administration of G-CSF promoted the repair of damaged areas with hyaline-like cartilage at four weeks in a rabbit model.
Strengths and limitations
Pre-operative systemic G-CSF administration is a minimally invasive, technically simple and inexpensive technique that has important clinical potential.
The detailed mechanism of the cartilage repair from G-CSF administration is unclear, so further study is required.
Introduction
Spontaneous healing of articular cartilage defects rarely occurs because of its avascularity and low cellularity.1,2 Several methods of treating cartilage damage in clinical practice have been reported, including microfracture,3 mosaicplasty,4 autologous chondrocyte implantation (ACI),5 and mesenchymal stem cell (MSC) implantation.6 Each has its merits and demerits, and a definitive therapeutic method is yet to be established.
Microfracture is widely used because of its simplicity and low invasiveness, although it has drawbacks in only being indicated for small defects, in the time required for tissue repair, and because the repair is mainly with fibrous cartilage.7
To compensate for these drawbacks, we devised a method of chemically stimulating the bone marrow with systemic drug administration of bone marrow stimulants. Although several studies have been conducted on the role of drugs in cartilage repair, we focused on the myelostimulant granulocyte-colony stimulating factor (G-CSF). The repair that occurs with microfractures is thought to be due to the action of the myelocytes; our idea was to promote the healing mechanism by stimulating the myelocytes before the microfracture occured.
G-CSF is a cytokine that serves as a growth factor for the haematopoietic stem cells. It acts on the bone marrow by increasing granulocyte production and promoting the functions of the neutrophils. However, several recent reports have indicated that G-CSF also has non-haematopoietic functions and promotes mobilisation of mesenchymal stem cells (MSCs) to both bone marrow and peripheral blood.8
We hypothesised that pre-operative systemic G-CSF administration would lead to the proliferation of MSCs in the bone marrow of a rabbit model, which would create a synergistic effect with the bone marrow stimulation resulting from microfracture. This method could be applicable to larger areas of cartilage damage, could shorten the time required for tissue repair, and create a repair with hyaline cartilage.
The aim of this study was to investigate the effect of G-CSF on MSCs proliferation in vitro, and to determine whether systemic administration of G-CSF, a stimulant of the bone marrow, prior to microfracture, could improve the quality of repaired tissue using a full-thickness articular cartilage defect model in a rabbit.
Materials and Methods
Animals
A total of 35 male 12-week-old New Zealand rabbits were purchased from Japan SLC (Hamamatsu, Japan). Animal experiments were performed following ethical and statutory approval in accordance with local policy. Rabbits were kept in an approved animal-care facility, with strict compliance to care and usage protocols.
Effect of G-CSF on proliferation of MSCs in vitro
Bone marrow cells were harvested from five rabbits. The femurs were dissected and cleaned of the adherent soft tissues. The bone marrow was flushed using a 14-gauge needle with a 10 mL syringe loaded with complete medium (α-minimal essential medium; MEM; Nacalai Tesque, Inc., Kyoto, Japan), supplemented with 10% fetal bovine serum (FBS; HyClone Laboratories, Inc., Logan, Utah).8 The nucleated cells were separated with lymphocyte separation solution (1.077 g/mL; Nacalai Tesque Inc.), resuspended in complete medium, seeded in culture dishes, and incubated in air containing 5% CO2 at 37°C. The non-adherent cells were removed by washing with phosphate-buffered saline (PBS) and the medium was changed after 72 hours. The medium was changed every three to four days thereafter. Upon reaching 80% to 90% confluence, the primary cells were trypsinised with 0.25% trypsin–ethylenediaminetetraacetic acid (EDTA; Nacalai Tesque Inc.), resuspended in the culture medium, and seeded. Cells in passage 3 (P3) were used for in vitro experiments.8,9
Cultured cells (2 × 105) were seeded into dishes with three types of media: control (n = 5), complete medium 10 mL; low-dose (n = 5), complete medium 10 mL with 4 μg G-CSF (GRAN; Kyowa Hakko Kirin, Tokyo, Japan); and high-dose (n = 5), complete medium 10 mL with 40 μg G-CSF. Cells were counted after one, three, and five days, by using hematocytometer.
Assessment of multi-lineage differentiation potential
P3 cells that proliferated in the normal medium and P4 cells that proliferated in the medium with G-CSF were seeded into three types of differentiation media.
Osteogenic differentiation was examined according to the protocol provided by the manufacturer (Osteoblast-Inducer Reagent, Takara, Japan). Briefly the cells were seeded into a dish with Roswell Park Memorial Institute (RPMI) medium (Nacalai Tesque Inc., Kyoto, Japan) supplemented with ascorbic acid (1%), hydrocortisone (0.2%), and β-glycerophosphate (2%) (Osteoblast-Inducer Reagent, Takara, Japan) for three weeks. Alizarin red staining was subsequently performed to observe matrix mineralisation, and microscopically observed at a magnification of 200.
Adipocyte differentiation was examined according to the protocol provided by the manufacturer (AdipoInducer Reagent, Takara, Japan). The cells were seeded into a dish with Dulbecco's modified Eagle's (DMEM) medium (Nacalai Tesque Inc., Kyoto, Japan) and supplemented with insulin (1%), dexamethasone (2.5 μM), and 3-isobutyl-1-methylxanthine (0.5 mM) (AdipoInducer Reagent, Takara, Japan) for 48 hours. Maintenance medium (DMEM supplemented with insulin 1%) was then substituted. Three weeks later, the cells were stained with oil red O for fat droplets, and microscopically observed at a magnification of 200.
For chondrogenic differentiation, by referencing to the previous study,9 2 × 105 cells were pelleted in a 15 mL polypropylene conical tube at 500 g for ten minutes, and placed in DMEM medium supplemented with insulin-transferrin-selenium (ITS) (50 mg, Nacalai Tesque Inc., Kyoto, Japan), dexamethasone (10−7 M, Sigma-Aldrich, corp., St. Louis, Missouri), and transforming growth factor-β3 (TGF-β3) (10 ng/ml, PeproTech, Inc., Rocky Hill, New Jersey). Thereafter, the medium was changed every three to four days. Three weeks later, the pellet was examined immunohistochemically for collagen type II staining. The sections were incubated with a mouse monoclonal antibody against human type II collagen (dilution of 1:250, #F-57, Kyowa Pharma Chemical, Tokyo, Japan) for 50 minutes at room temperature. Antibody binding was visualised by using diaminobenzidine. The sections were counterstained with haematoxylin. They were microscopically observed at a magnification of 400.
Effect of systemic administration of G-CSF on a full-thickness cartilage defect in a rabbit
All procedures were performed under anesthesia induced by intramuscular infection of 25 mg/kg ketamine hydrochloride.6 Animal care was observed in accordance with the guidance of our institute’s animal committee.
A total of 30 12-week-old male New Zealand White rabbits were divided into three groups (control, low dose and high dose).
For the low-dose group (n = 10), 10 μg/kg of G-CSF was administered by subcutaneous injection three times, every 24 hours. Likewise, for the high-dose group (n = 10), 50 μg/kg of G-CSF was administered three times, every 24 hours.10-13 For the control group (n = 10), saline was administered three times, every 24 hours.
Immediately after the final injection, one knee joint, in alternate shifts, was opened through a medial parapatellar approach under sterile conditions and the patella was dislocated laterally to expose the articular surface of the femoral trochlea. A 5.2 mm diameter cylindrical osteochondral defect with 4 mm depth was created in the centre of the femoral trochlear groove using an electric drill.14-16 Post-operatively, the rabbits were allowed to walk freely in the cage.
Five rabbits from each group were killed at four weeks and 12 weeks, respectively, after the operation. Then we evaluated the status of repaired tissue macroscopically and microscopically. Macroscopically, cartilage defects were observed for apparent filling volume and surface smoothness. Microscopically, the dissected distal femurs were then fixed in 4% paraformaldehyde solution at room temperature for two days, decalcified with 10% ethylenediamine tetraacetic acid (EDTA) for three weeks and then embedded in paraffin blocks. Axial sections 5 µm thick were obtained from the centre of each defect and stained histologically with haematoxylin-eosin and safranin-O, and immunohistochemically. For immunohistochemical stain, a mouse monoclonal antibody against human type II collagen (#F-57, Kyowa Pharma Chemical, Tokyo, Japan) was used. The sections were incubated with the antibody against typeII collagen (dilution 1:500) overnight at 4°C. Antibody binding was visualized by using diaminobenzidine. The sections were counterstained with hematoxylin. We observed at a magnification × 100 and evaluated repaired tissue using the Wakitani score.
Statistical analysis
For cell counting, the mixed-effect model for repeated measurements was used. For histological assessment, the Kruskal-Wallis test was used. A p-value < 0.05 was considered to be significant.
Results
MSCs proliferation
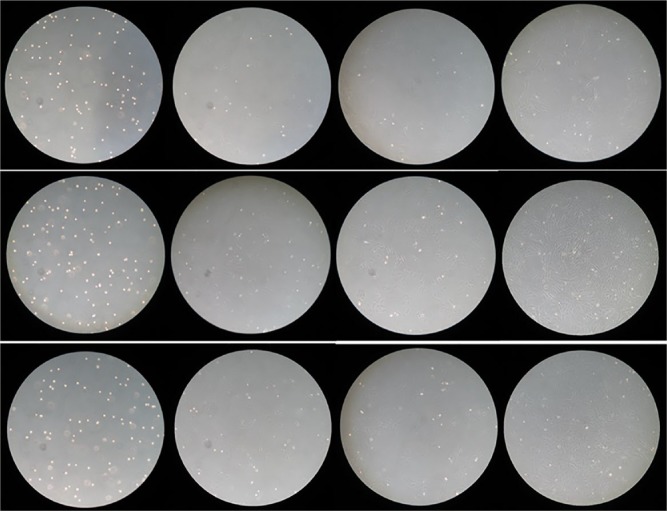
In the low-dose G-CSF medium, proliferation was vigorous, and reached 100% confluence after five days, while the control medium reached 70% to 80% confluence after five days (Fig. 1). The cell count in the low-dose G-CSF medium was significantly higher than that in the control medium. The cell counts of the control medium and the low-dose G-CSF medium were: 2.94 × 105 and 5.95 × 105 (p < 0.0001), respectively, after one day; 6.31 × 105 and 14.82 × 105 (p = 0.0001), respectively, after three days; and 9.90 × 105 and 21.49 × 105 (p = 0.001), respectively, after five days (Table I). The proliferation speed in the high-dose G-CSF medium also tended to be faster than that in the control medium (Fig. 2).
Fig 1.
Microscopic findings (×100). Top row: control group; middle row: low-dose group; bottom row: high-dose group. From left to right are microscopic findings from the start of the culture and after 1, 3, and 5 days.
Table I.
Proliferation of MSCs with G-CSF
| Day 1 | Day 2 | Day 3 | |
|---|---|---|---|
| Control (n = 5) | 2.94 (0.35) × 105 | 6.31 (0.79) × 105 | 9.90 (2.63) × 105 |
| Low dose (n = 5) | 5.95 (0.91) × 105* | 14.82 (3.67) × 105* | 21.49 (5.53) × 105* |
| High dose (n = 5) | 4.21 (0.86) × 105† | 11.26 (2.96) × 105 | 17.04 (5.53) × 105 |
significant difference comparing with control group
significant difference comparing with low dose group (p < 0.005)
Cell count was expressed as mean and standard deviation (in brackets)
Fig 2.
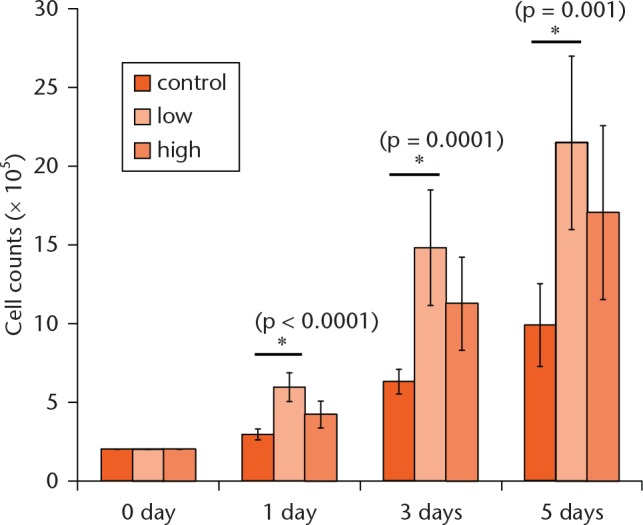
Graph showing cell count. The mixed-effect model for repeated measurements was used for statistical analyses. p< 0.005 was considered significant.
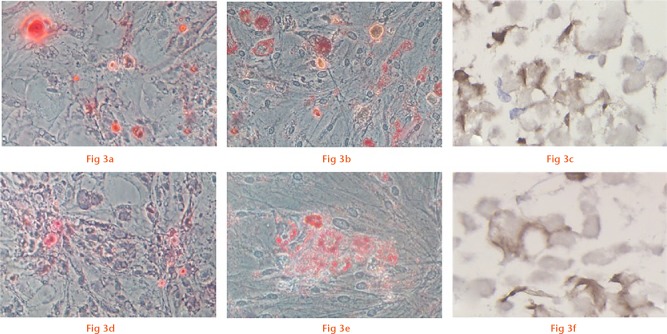
Multi-lineage differentiation potential
P3 cells that proliferated in the normal medium were confirmed to have differentiated into the skeletal tissue (alizarin red: positive), adipose tissue (oil red O: positive), and cartilage (collagen type II: positive) (Figs 3a to 3c).
Multilineage differentiation potential of P3 cells that proliferated in normal medium (a to c) and P4 cells that proliferated in medium with low-dose G-CSF (d to f). Osteogenesis is detected by the deposition of calcium mineralisation using alizarin red staining (a, d, ×200). Adipogenesis is indicated by the accumulation of lipid vacuoles using oil red O staining (b, e, ×200). Chondrogenesis is indicated by the cartilage-specific matrix using collagen type II staining (c, f, ×400).
The P4 cells which proliferated in the G-CSF medium also showed the potential to differentiate into the three tissue types (Figs 3d to 3f).
Macroscopic findings of cartilage repair
At four weeks, only the bottom of the defect was filled in the control group, whereas newly formed tissue filled the defect almost entirely in the high-dose group. The low-dose group exhibited an intermediate level of filling. In the control group, the boundary between the defect and the surrounding normal cartilage was well defined, and the surface was rough. In contrast, the boundary was partially ill-defined and the surface was partially smooth in the G-CSF groups (Fig. 4).
Fig 4.
Macroscopic findings. Top row: at 4 weeks; bottom row: at 12 weeks. From left to right are macroscopic findings from the control group, the low-dose group, and the high-dose group.
At 12 weeks, the quality of repaired cartilage improved further and the defects were almost completely filled with hyaline-like cartilage in all groups (Fig. 4).
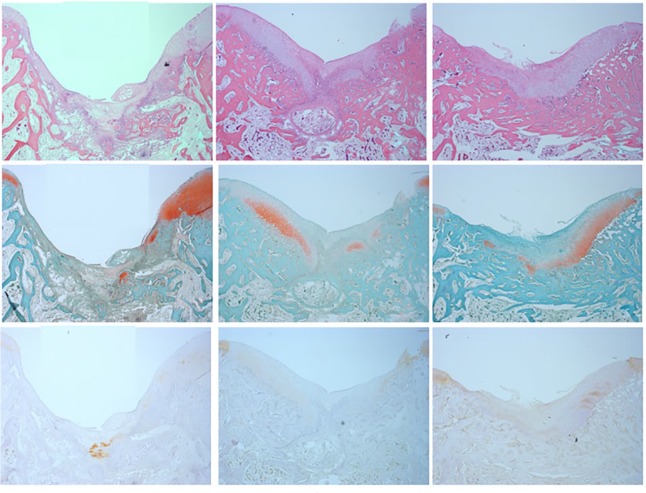
Microscopic findings of cartilage repair
At four weeks, the regenerated tissue was thinner in the control group than in the G-CSF groups: the repaired tissues were partially positive for safranin O and collagen type II staining, and the repair of the subchondral bone was also observed (Fig. 5). Wakitani scores (Fig. 6) were higher in the G-CSF groups, and the high-dose group score (11.8, sd 2.04) was significantly higher than the control group score (7.2, sd 0.75) (one-way analysis of variance Tukey test, p = 0.009).
Fig 5.
Microscopic findings at 4 weeks (×100). Top row: haematoxin and eosin staining; middle row: safranin O staining; bottom row: collagen type II staining. From left to right are microscopic findings from the control group, the low-dose group, and the high-dose group.
Fig 6.
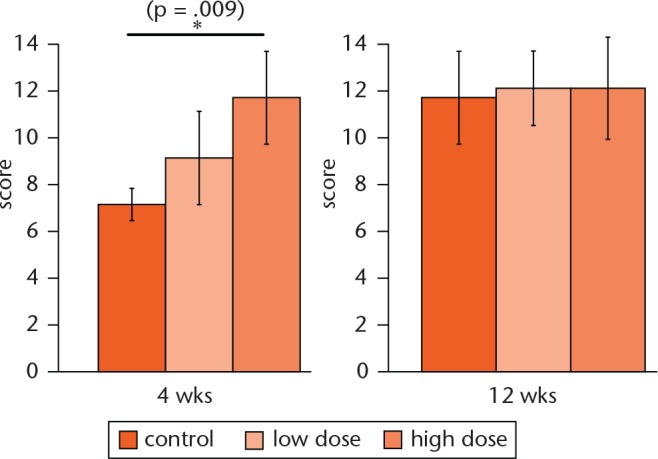
Histological evaluation using the Wakitani score. One-way analysis of variance Tukey test was used for statistical analyses. p < 0.05 was considered significant.
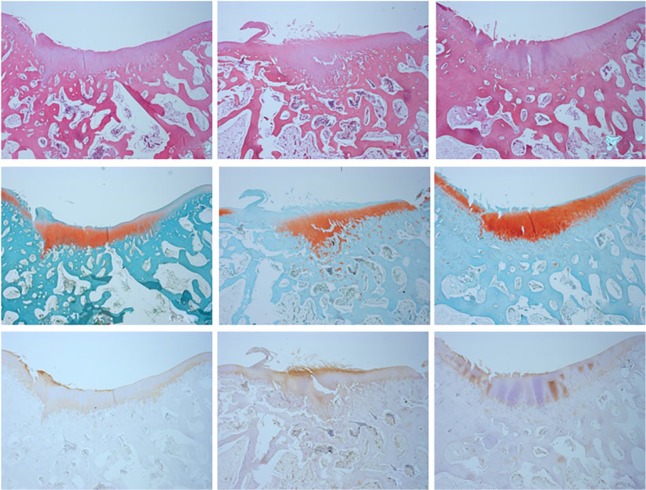
At 12 weeks, the defects were repaired with hyaline-like cartilage, which was positive for safranin O and collagen type II staining, and the repair of the subchondral bone was observed in all groups (Fig. 7). Wakitani scores (Fig. 6) improved further in all groups, and differences between groups were not detected (Kruskal-Wallis test, p = 0.93).
Fig 7.
Microscopic findings at 12 weeks (×100). Top row: H&E staining; middle row: safranin O staining; bottom row: collagen type II staining. From left are microscopic findings from the control group, the low-dose group, and the high-dose group.
Discussion
We evaluated the effect of combining chemical bone marrow stimulation via systemic administration of G-CSF with physical bone marrow stimulation to treat the cartilage damage in a full-thickness cartilage defect in a rabbit model. Prior to our study, a single paper reported the effect of systemic administration of G-CSF on cartilage damage using Lewis rats.17 The authors reported that G-CSF could act as a promoting agent in the repair of osteochondral defects, presumably by increasing the number of peripheral blood nucleated cells, but that underlying mechanisms were unclear. In the present study we confirmed the proliferation of MSCs in response to G-CSF administration in vitro and maintenance of pluripotent phenotype. Although we could only exhibit indirect evidence, we speculated that an increase in MSCs at the damaged site accelerated the repair of osteochondral defects.
Among several options for cartilage repair, microfracture is widely used due to its simplicity.3,18-22 Although many good clinical results were reported, histology revealed that the repaired cartilage was fibrous to hyaline-like.1,18 And the mechanism of cartilage repair has been well demonstrated. Stimulation from microfracture causes a haematoma to be released from the bone marrow, covering the area of cartilage defect. This haematoma is rich in myeloid tissue that contains the MSCs, which have the potential to differentiate into the cartilage, thus forming the basis for cartilage regeneration and repair.23,24
We sought to promote the proliferation of MSCs by stimulating the bone marrow via a different mechanism – systemic drug administration – to expect a synergistic effect with the mechanism of microfracture. We anticipated that this would compensate for the drawbacks of microfracture.
Previous studies have combined microfracture with the administration of various cells and drugs in situ.2,15,16,25-31 Dorotka et al25 reported that the combination of microfracture and collagen matrices seeded with the MSCs or chondrocytes facilitated the regeneration of hyaline-like cartilage. Both Kuo et al2 and Yang et al26 reported that the combination of microfracture and bone morphogenetic protein-7 (BMP-7) in a collagen sponge increased the quality and quantity of repair tissue. Fontana and de Girolamo27 reported that combination of microfracture and a resorbable collagen I/III matrix improved mid-term outcomes which were maintained at a mean of five years post-operatively. While these studies achieved better results via a synergistic effect than microfracture alone, no procedure accomplished regeneration of hyaline cartilage. Thus, considering clinical application, a simple method such as systemic administration of G-CSF would be preferable.
Among other drugs, the usefulness of fibroblast growth factor-2 (FGF-2) has been reported. FGF-2 promotes the mobilisation of the MSCs from the bone marrow into chondral defects, and induces regenerative repair of the articular cartilage in full-thickness defects. Local administration of FGF-2 using a fibrin sealant16 and FGF-2 reflux administration by placing a tube in the joint15,31 achieved good results equivalent to ours, with successful chondrogenic repair, but neither method can be considered superior in terms of technical factors or level of invasiveness.
Recently, Koga et al6 reported that placing the synovial-derived MSCs in suspension on the cartilage defect for ten minutes promoted cartilage regeneration. This method was groundbreaking because it did not require a substrate, unlike the previous methods. This method is being applied in the clinic, but as a surgical approach is needed to collect and culture the MSCs and then administer them locally, it is rather more complicated than simple microfracture plus systemic administration of G-CSF.
In the process of studying new interventions, we realised that the major premise shared by these therapies2,15,16,25-31 was that the MSCs contributed greatly to cartilage repair. Therefore, instead of implanting the MSCs, or using drugs to promote their differentiation into cartilage, we thought that administering G-CSF could be a means of increasing the proliferation of the MSCs. Unlike previous methods requiring implanting autologous cells or some substrates,2,15,16,25-31 the major advantage of this technique is easy and minimally invasive systemic administration via via subcutaneous injections.
G-CSF has been classically applied to mobilise the haematopoietic stem cells (HSCs). The administration of G-CSF is known to mobilise the HSCs from the bone marrow into the peripheral blood.32 Deng et al8 have indicated that G-CSF also has non-haematopoietic functions. They reported that G-CSF promotes mobilisation of the MSCs to both bone marrow and peripheral blood. The authors performed a colony-forming unit-fibroblast assay with the MSCs from rats that received an injection of G-CSF (40 μg/kg once a day for five consecutive days) via the vena caudalis and found a significant increase in the mobilisation of MSCs into the peripheral blood and bone marrow.
In the present study, we added G-CSF to the MSC culture media to evaluate the effect on MSCs. The cell count in these media was significantly higher than that in the control group. This absolute rise in the number of MSCs could be one contributing factor in the promotion of MSC mobilisation that has been reported previously.8 Moreover, the MSCs that proliferated due to G-CSF had the potential to differentiate into three tissue types, suggesting that the cells stimulated by G-CSF could contribute to the repair of damaged cartilage.
At four weeks after damage in the present study, the control group showed insufficient repair, or repair by fibrous cartilage, while relatively good repair had progressed in the systemic G-CSF administration group, with some repair from hyaline-like cartilage. We surmise that stimulation of the bone marrow by systemic administration of G-CSF encouraged the proliferation of the MSCs. Performing concurrent microfracture increased the MSC mobilisation into the site of the cartilage defect, which increased the extent of cartilage differentiation. The results obtained were sufficiently satisfactory, even when compared with those obtained with ACI or administration of various drugs. Compared with the previously examined techniques, this intervention was simpler and less invasive, with results obtainable after a few days of subcutaneous administration, making it an attractive option.
While the present study suggests that systemic G-CSF administration may speed up repair, natural repair had occurred in the control group at 12 weeks. Thus, we were unable to determine if this method can encourage repair in the defects for which natural repair is difficult. In past studies on full-thickness cartilage defects in rabbits, it was reported that chondrogenesis did not occur and defects were filled with fibrous tissue in larger defects (>5.0 mm in diameter).15,16,31 Therefore, we created 5.2 mm diameter defects. However, in contrast to the previous reports,15,16,31 natural repair with hyaline-like cartilage also occurred in the control group after 12 weeks. This may have been due to the difference in age, i.e., the previous studies used adolescent rabbits aged 15 to 16 weeks, or weighing 3.0 kg to 3.4 kg. Meanwhile, in our study, we used 12 week-old rabbits weighing 2.1 kg to 2.7 kg. Therefore, they were younger and still may have had enough natural reparative ability. In the present study, we observed differences in the optimal dose for systemic administration, and for use in a culture medium. However, simple comparisons are not possible between the dose for rabbits and the dose for the cells, nor for the indirect route of systemic administration and the direct route of adding to a culture medium.
Future studies should investigate whether repair occurs in aged rabbits, in which the capability for self-repair is decreased, serving as a model in which the natural repair is less likely to occur.
It is possible that post-operative G-CSF administration can prolong the period of chemical bone marrow stimulation, and the optimal dose should be investigated. When clinically applied, we believe neither method will increase the burden on patients or on the level of invasiveness. Moreover, while aftercare can be difficult to control in rabbits, better results may be obtained by controlling the environment inside a joint, such as lessening loads and increasing range of movement exercises.
There are some limitations to this study. Animals were not allocated randomly. The macroscopic assessment of repair tissues was not blinded. The proliferation of the MSCs was only confirmed in vitro, therefore, the dynamics in vivo are unclear. It is unknown whether G-CSF affected the MSCs directly, affected their precursor cells, or if there was a secondary effect from some other kind of cell. At the very least, the results suggest that G-CSF may affect the MSCs themselves.
The greatest limitation is that we did not evaluate whether the MSCs actually proliferated at the site of the cartilage defect. Accurate quantification of the MSCs that mobilise at a defect site is technically difficult.
Pre-operative systemic G-CSF administration does not require pre-operative cell collection or culture, or invasion of the joint, and is not technically difficult. It is minimally invasive, technically simple and inexpensive, making it a potentially ground-breaking therapy.
In the future, we would like to study the timing of drug administration, appropriate dosage, and the level of administration, with the goal of applying it in clinical practice.
In conclusion, we evaluated the effects of G-CSF on MSC proliferation in vitro as well as on a full-thickness cartilage defect in a rabbit model in vivo. G-CSF promoted proliferation of MSCs in vitro. The systemic administration of G-CSF promoted the repair of damaged cartilage, possibly through increasing the number of MSCs at the damaged site in a rabbit model. In order to clarify the mechanism underlying cartilage repair and MSC proliferation, further study is required.
Footnotes
Author Contributions: T. Sasaki: Performed experiment and drafted the manuscript
R. Akagi: Discussed the results and implications and commented on the manuscript
Y. Akatsu: Technical support and conceptual advice
T. Fukawa: Technical support and conceptual advice
H. Hoshi: Helped to collect the data and perform the analysis
Y. Yamamoto: Helped to collect the data and perform the analysis
T. Enomoto: Sacrifice of animals and macroscopic evaluation
Y. Sato: Helped to collect the data and perform the analysis
R. Nakagawa: Helped to collect the data and perform the analysis
K. Takahashi: Supervised the project
S. Yamaguchi: Discussed the results and implications and commented on the manuscript
T. Sasho: Designed the project and drafted the manuscript
ICMJE Conflicts of Interest: None declared
Funding Statement
This work was supported in part by grants-in-aids from the Japan Society for the Promotion of the Science (C), Grant number 16K10885. The founders had no role in the design collection of the data, analysis, and interpretation of the study or writing of the manuscript.
References
- 1. Frisbie DD, Oxford JT, Southwood L, et al. Early events in cartilage repair after subchondral bone microfracture. Clin Orthop Relat Res 2003;407:215-227. [DOI] [PubMed] [Google Scholar]
- 2. Kuo AC, Rodrigo JJ, Reddi AH, et al. Microfracture and bone morphogenetic protein 7 (BMP-7) synergistically stimulate articular cartilage repair. Osteoarthritis Cartilage 2006;14:1126-1135. [DOI] [PubMed] [Google Scholar]
- 3. Steadman JR, Rodkey WG, Rodrigo JJ. Microfracture: surgical technique and rehabilitation to treat chondral defects. Clin Orthop Relat Res 2001;391(Suppl):S362-S369. [DOI] [PubMed] [Google Scholar]
- 4. Matsusue Y, Yamamuro T, Hama H. Arthroscopic multiple osteochondral transplantation to the chondral defect in the knee associated with anterior cruciate ligament disruption. Arthroscopy 1993;9:318-321. [DOI] [PubMed] [Google Scholar]
- 5. Brittberg M, Lindahl A, Nilsson A, et al. Treatment of deep cartilage defects in the knee with autologous chondrocyte transplantation. N Engl J Med 1994;331:889-895. [DOI] [PubMed] [Google Scholar]
- 6. Koga H, Shimaya M, Muneta T, et al. Local adherent technique for transplanting mesenchymal stem cells as a potential treatment of cartilage defect. Arthritis Res Ther 2008;10:R84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Breinan HA, Martin SD, Hsu HP, Spector M. Healing of canine articular cartilage defects treated with microfracture, a type-II collagen matrix, or cultured autologous chondrocytes. J Orthop Res 2000;18:781-789. [DOI] [PubMed] [Google Scholar]
- 8. Deng J, Zou ZM, Zhou TL, et al. Bone marrow mesenchymal stem cells can be mobilized into peripheral blood by G-CSF in vivo and integrate into traumatically injured cerebral tissue. Neurol Sci 2011;32:641-651. [DOI] [PubMed] [Google Scholar]
- 9. Fu WL, Zhou CY, Yu JK. A new source of mesenchymal stem cells for articular cartilage repair: MSCs derived from mobilized peripheral blood share similar biological characteristics in vitro and chondrogenesis in vivo as MSCs from bone marrow in a rabbit model. Am J Sports Med 2014;42:592-601. [DOI] [PubMed] [Google Scholar]
- 10. Ishida N, Iwata H, Shimabukuro K, et al. Effects of omentopexy combined with granulocyte colony-stimulating factor in a rabbit heart model. Eur J Cardiothorac Surg 2011;39:375-380. [DOI] [PubMed] [Google Scholar]
- 11. Meng J, Yao X, Kang S, et al. Treatment of ischemic limbs by transplantation of G-CSF stimulated bone marrow cells in diabetic rabbits. Clin Invest Med 2010;33:E174-E180. [DOI] [PubMed] [Google Scholar]
- 12. Zhao Q, Sun C, Xu X, et al. Early use of granulocyte colony stimulating factor improves survival in a rabbit model of chronic myocardial ischemia. J Cardiol 2013;61:87-94. [DOI] [PubMed] [Google Scholar]
- 13. Deng MW, Wei SJ, Yew TL, et al. Cell therapy with G-CSF-mobilized stem cells in a rat osteoarthritis model. Cell Transplant 2015;24:1085-1096. [DOI] [PubMed] [Google Scholar]
- 14. Otsuka Y, Mizuta H, Takagi K, et al. Requirement of fibroblast growth factor signaling for regeneration of epiphyseal morphology in rabbit full-thickness defects of articular cartilage. Dev Growth Differ 1997;39:143-156. [DOI] [PubMed] [Google Scholar]
- 15. Mizuta H, Kudo S, Nakamura E, et al. Active proliferation of mesenchymal cells prior to the chondrogenic repair response in rabbit full-thickness defects of articular cartilage. Osteoarthritis Cartilage 2004;12:586-596. [DOI] [PubMed] [Google Scholar]
- 16. Ishii I, Mizuta H, Sei A, et al. Healing of full-thickness defects of the articular cartilage in rabbits using fibroblast growth factor-2 and a fibrin sealant. J Bone Joint Surg [Br] 2007;89-B:693-700. [DOI] [PubMed] [Google Scholar]
- 17. Okano T, Mera H, Itokazu M, et al. Systemic administration of granulocyte colony-stimulating factor for osteochondral defect repair in a rat experimental model. Cartilage 2014;5:107-113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Bae DK, Yoon KH, Song SJ. Cartilage healing after microfracture in osteoarthritic knees. Arthroscopy 2006;22:367-374. [DOI] [PubMed] [Google Scholar]
- 19. Steinwachs MR, Guggi T, Kreuz PC. Marrow stimulation techniques. Injury 2008;39:S26-S31. [DOI] [PubMed] [Google Scholar]
- 20. Asik M, Ciftci F, Sen C, et al. The microfracture technique for the treatment of full-thickness articular cartilage lesions of the knee: midterm results. Arthroscopy 2008;24:1214-1220. [DOI] [PubMed] [Google Scholar]
- 21. Riyami M, Rolf C. Evaluation of microfracture of traumatic chondral injuries to the knee in professional football and rugby players. J Orthop Surg Res 2009;4:13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Mithoefer K, McAdams T, Williams RJ, et al. Clinical efficacy of the microfracture technique for articular cartilage repair in the knee: an evidence-based systematic analysis. Am J Sports Med 2009;37:2053-2063. [DOI] [PubMed] [Google Scholar]
- 23. Ashton BA, Allen TD, Howlett CR, et al. Formation of bone and cartilage by marrow stromal cells in diffusion chambers in vivo. Clin Orthop Relat Res 1980;151:294-307. [PubMed] [Google Scholar]
- 24. Shapiro F, Koide S, Glimcher MJ. Cell origin and differentiation in the repair of full-thickness defects of articular cartilage. J Bone Joint Surg [Am] 1993;75-A:532-553. [DOI] [PubMed] [Google Scholar]
- 25. Dorotka R, Windberger U, Macfelda K, et al. Repair of articular cartilage defects treated by microfracture and a three-dimensional collagen matrix. Biomaterials 2005;26:3617-3629. [DOI] [PubMed] [Google Scholar]
- 26. Yang HS, La WG, Bhang SH, et al. Hyaline cartilage regeneration by combined therapy of microfracture and long-term bone morphogenetic protein-2 delivery. Tissue Eng Part A 2011;17:1809-1818. [DOI] [PubMed] [Google Scholar]
- 27. Fontana A, de Girolamo L. Sustained five-year benefit of autologous matrix-induced chondrogenesis for femoral acetabular impingement-induced chondral lesions compared with microfracture treatment. Bone Joint J 2015;97-B:628-635. [DOI] [PubMed] [Google Scholar]
- 28. Solchaga LA, Dennis JE, Goldberg VM, Caplan AI. Hyaluronic acid-based polymers as cell carriers for tissue-engineered repair of bone and cartilage. J Orthop Res 1999;17:205-213. [DOI] [PubMed] [Google Scholar]
- 29. Løken S, Jakobsen RB, Arøen A, et al. Bone marrow mesenchymal stem cells in a hyaluronan scaffold for treatment of an osteochondral defect in a rabbit model. Knee Surg Sports Traumatol Arthrosc 2008;16:896-903. [DOI] [PubMed] [Google Scholar]
- 30. Bartlett W, Skinner JA, Gooding CR, et al. Autologous chondrocyte implantation versus matrix-induced autologous chondrocyte implantation for osteochondral defects of the knee: a prospective, randomised study. J Bone Joint Surg [Br] 2005;87-B:640-645. [DOI] [PubMed] [Google Scholar]
- 31. Chuma H, Mizuta H, Kudo S, et al. One day exposure to FGF-2 was sufficient for the regenerative repair of full-thickness defects of articular cartilage in rabbits. Osteoarthritis Cartilage 2004;12:834-842. [DOI] [PubMed] [Google Scholar]
- 32. Demetri GD, Griffin JD. Granulocyte colony-stimulating factor and its receptor. Blood 1991;78:2791-2808. [PubMed] [Google Scholar]