Abstract
Ambient fine particle (PM2.5) pollution triggers acute cardiovascular events. Individual-level preventions are proposed to complement regulation in reducing the global burden of PM2.5–induced cardiovascular diseases. We determine whether B vitamin supplementation mitigates PM2.5 effects on cardiac autonomic dysfunction and inflammation in a single-blind placebo-controlled crossover pilot trial. Ten healthy adults received two-hour controlled-exposure-experiment to sham under placebo, PM2.5 (250 μg/m3) under placebo, and PM2.5 (250 μg/m3) under B-vitamin supplementation (2.5 mg/d folic acid, 50 mg/d vitamin B6, and 1 mg/d vitamin B12), respectively. At pre-, post-, 24 h-post-exposure, we measured resting heart rate (HR) and heart rate variability (HRV) with electrocardiogram, and white blood cell (WBC) counts with hematology analyzer. Compared to sham, PM2.5 exposure increased HR (3.8 bpm, 95% CI: 0.3, 7.4; P = 0.04), total WBC count (11.5%, 95% CI: 0.3%, 24.0%; P = 0.04), lymphocyte count (12.9%, 95% CI: 4.4%, 22.1%; P = 0.005), and reduced low-frequency power (57.5%, 95% CI: 2.5%, 81.5%; P = 0.04). B-vitamin supplementation attenuated PM2.5 effect on HR by 150% (P = 0.003), low-frequency power by 90% (P = 0.01), total WBC count by 139% (P = 0.006), and lymphocyte count by 106% (P = 0.02). In healthy adults, two-hour PM2.5 exposure substantially increases HR, reduces HRV, and increases WBC. These effects are reduced by B vitamin supplementation.
Ambient fine particulate matter (PM2.5) pollution contributes to 3.7 million premature deaths per year worldwide, predominantly through acute effects on the cardiovascular system1. Indeed, PM pollution is the most frequent trigger for myocardial infarction at the population level2. Even at levels below the current National Ambient Air Quality Standards (NAAQS), associations of PM2.5 exposure with increased cardiovascular risk have been found in sensitive individuals3,4. Moreover, many urban areas outside of North America continue to have elevated levels of PM2.5 pollution1,5. Reducing the global burden of cardiovascular disease (CVD) due to PM2.5 pollution requires defined options for individual-level prevention that complement regulatory measures4.
Reduced heart rate variability (HRV), reflecting a perturbation in autonomic function6,7, is a sensitive marker that changes rapidly in response to PM2.5 exposure3. It represents a primary pathophysiologic intermediate that may proceed PM-related adverse cardiovascular events4. In the Normative Aging Study, we found associations of reduced HRV with short-term PM2.5 exposure that were limited to subjects with lower intakes of vitamin B6 or B12 and were abrogated in those with higher intakes6. These findings suggest that B vitamins provide protection against the effect of PM2.5 on the autonomic nervous system.
Previous epidemiologic studies have implicated B vitamin levels (folic acid, vitamins B6 and B12) in CVD susceptibility8,9. However, to date, the results from randomized clinical trials do not support the benefit of B vitamin supplementation for CVD prevention10,11,12,13,14,15. Recent studies suggest that B vitamins may minimize health effects of environmental stressors through their anti-inflammatory and antioxidant properties6,16. In animal models, B vitamin supplementation has been successfully used to curb oxidative stress, inflammation, and metabolic phenotype change due to environmental stressors17,18. However, no clinical trial has yet investigated whether B vitamin supplementation alters the biologic response to ambient air pollution exposure.
To the best of our knowledge, we established the first trial to evaluate whether B vitamin supplementation can attenuate the acute autonomic effects of PM2.5 using a single-blind crossover intervention with controlled exposure to fine concentrated ambient particles (fine CAP, i.e., PM2.5) in ten healthy adults. We investigated the PM2.5 effect on HRV and, because of the central role of inflammation in modulating the cardiovascular effects of PM2.5, on total and differential white blood cell (WBC) counts, as well as the potential for B vitamins to counteract these effects.
Results
Study population and exposure levels
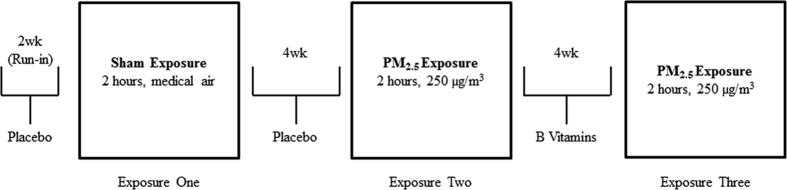
As previously described19, all volunteers (baseline characteristics described in Supplementary Table 1) completed three controlled exposure experiments (July 2013 to February 2014) (Fig. 1). The baseline resting HR ranged from 43.0 to 74.0 bmp (median, 58.9 bpm), and did not vary substantially by age, gender, race, or being overweight.
Figure 1. Study design: A single-blind, cross-over intervention trial with controlled exposure experiments in ten healthy volunteers19.
The target PM2.5 concentrations were controlled by design; however, there was some variations in the actual PM2.5 concentration (Supplementary Table 2). Among all controlled exposures to PM2.5, the concentration varied from 100.6 to 287.5 μg/m3 (median, 234.0 μg/m3). Previous studies using the same exposure facility reported minimal PM2.5 concentration in medical air (median, 0.0 μg/m3; interquartile range, 2.40 μg/m3)20. No significant difference in PM2.5 concentration existed between exposure 2 and 3 (P = 0.38). During the study period, the 7-day moving average of ambient PM2.5 level was 9.30 ± 0.36 μg/m3 in the study area.
Plasma concentrations of B vitamins
Four-week B vitamin supplementation significantly increased plasma concentrations of folic acid, vitamins B6 and B12 (P = 0.02, P = 0.004, P = 0.01; respectively), while placebo had no effect (P = 0.82, P = 0.75, P = 0.42, respectively) (Supplementary Table 3).
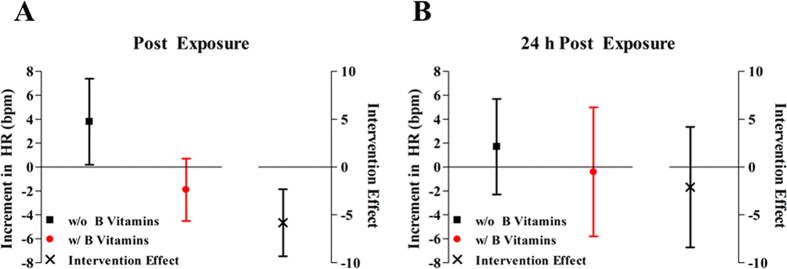
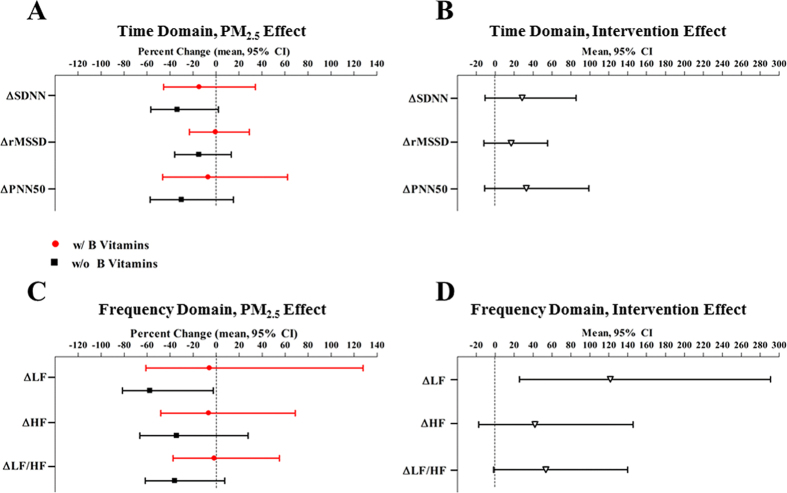
Effect of PM2.5 on heart rate (HR), HRV, and WBC without B vitamin supplement
In the absence of B vitamin supplement, HR increased (Fig. 2) and HRV decreased (Fig. 3) after PM2.5 exposure. Compared to sham, two-hour PM2.5 exposure was associated with 3.8 bpm (95% CI, 0.3 bpm, 7.4 bpm; P = 0.04) higher resting HR. PM2.5 exposure was associated with 33.6% (95% CI, −2.1%, 56.8%; P = 0.06), 57.5% (95% CI, 2.5%, 81.5%; P = 0.04), and 35.9% (95% CI, −7.5%, 61.8%; P = 0.09) lower standard deviation of NN intervals (SDNN), low-frequency (LF) power, and low-frequency/high-frequency (LF/HF) ratio compared to sham, respectively (Supplementary Table 4). At 24 h post-exposure, we did not observe any significant effect of PM2.5 exposure on HR or HRV (Fig. 4 and Supplementary Table 5).
Figure 2. Increment in heart rate (HR) associated with PM2.5, and the intervention effect of B vitamin supplementation.
The intervention effect represents the difference in estimated PM2.5 effects between exposure 2 and exposure 3 (due to B vitamin supplementation). Results were adjusted for chamber humidity, chamber temperature, and season (Spring/Summer/Fall/Winter).
Figure 3. Immediate change of heart rate variability (HRV) associated with PM2.5, and the intervention effect of B vitamin supplementation.
SDNN indicates the standard deviation of normal-to-normal (NN) intervals; rMSSD indicates the root mean square of successive differences; PNN50 indicates percentage of differences between adjacent NN intervals that are greater than 50 milliseconds; LF indicates low-frequency power (0.04–0.15 Hz); HF indicates high-frequency power (0.15–0.4 Hz). Panel A and C represents the % change in post-exposure HRV/pre-exposure HRV ratio associated with PM2.5 exposure, compared to medical air. Results were adjusted for chamber humidity, chamber temperature, and season (Spring/Summer/Fall/Winter).
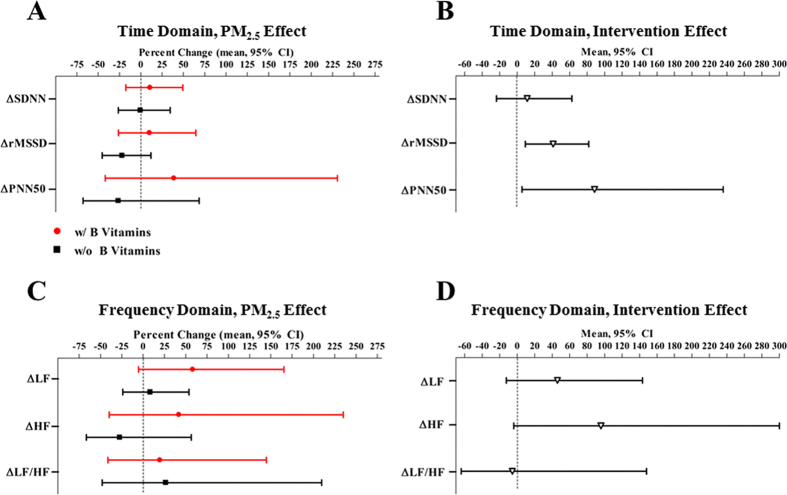
Figure 4. Twenty-four h post-exposure change of heart rate variability (HRV) associated with PM2.5, and the intervention effect of B vitamin supplementation.
SDNN indicates the standard deviation of normal-to-normal (NN) intervals; rMSSD indicates the root mean square of successive differences; PNN50 indicates percentage of differences between adjacent NN intervals that are greater than 50 milliseconds; LF indicates low-frequency power (0.04–0.15 Hz); HF indicates high-frequency power (0.15–0.4 Hz). Panel A and C represents the % change in 24 h post-exposure HRV/pre-exposure HRV ratio associated with PM2.5 exposure, compared to medical air. Results were adjusted for chamber humidity, chamber temperature, and season (Spring/Summer/Fall/Winter).
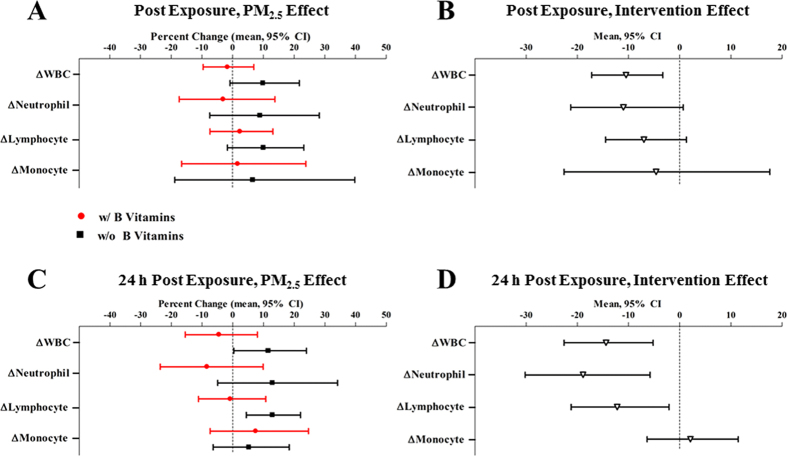
Exposure to PM2.5 increased total and differential WBC counts, compared to sham (Fig. 5). Immediately after exposure, PM2.5 was non-significantly associated with 9.9% (95% CI, −0.8%, 21.8%; P = 0.07) and 10.0% (95% CI, −1.7%, 23.2%; P = 0.09) higher total WBCs and lymphocytes. Twenty-four hours later, PM2.5 exposure was significantly associated with 11.5% (95% CI, 0.3%, 24.0%; P = 0.04) and 12.9% (95% CI, 4.4%, 22.1%; P = 0.005) higher total WBCs, neutrophils, lymphocytes, and monocytes, respectively (Supplementary Table 6).
Figure 5. Change of total and differential white blood cell (WBC) counts associated with PM2.5, and the intervention effect of B vitamin supplementation.
Panel A and C represents the % change in post-exposure cell count/pre-exposure cell count ratio associated with PM2.5 exposure, compared to medical air. Results were adjusted for chamber humidity, chamber temperature, and season (Spring/Summer/Fall/Winter).
B vitamin supplementation attenuated the effects of PM2.5
After four-week B vitamin supplementation, the associations of PM2.5 with outcomes, for example, post-exposure HR (Pintervention = 0.003), HRV (Pintervention = 0.01 for LF), and total WBC count (Pintervention = 0.008), were significantly attenuated. The effect of PM2.5 on HR was no longer significant with B vitamin supplementation (−1.9 bpm, 95% CI, −4.6 bpm, 0.7 bpm; P = 0.14) (Fig. 2). Likewise, B vitamin supplementation reduced the effect size of PM2.5 by 90% for LF and 96% for LF/HF ratio (Fig. 3). Further, exposure to two-hour PM2.5 was associated with 5.8% (95% CI, −127.8%, 61.0%; P = 0.89; Pintervention = 0.01) and 1.6% (95% CI, −55.0%, 37.5%; P = 0.94; Pintervention = 0.06) lower LF and LF/HF ratio, respectively, with B vitamin supplementation (Supplementary Table 4). In addition, although non-significant, B vitamin supplementation attenuated the PM2.5 effect by 57% on SDNN, 97% on square root of the mean squared differences of successive NN intervals (rMSSD), 77% on proportion of successive NN intervals with differences >50 msec (pNN50), and 81% on HF (Fig. 3).
The attenuation of the PM2.5-HR or PM2.5-HRV relationship (Pintervention = 0.003, 0.01, 0.03 for HR, rMSSD, and PNN50, respectively) by B vitamins remained significant at 24 h post-exposure (Fig. 4).
The associations of PM2.5 with post-exposure total and differential WBC counts were also weakened by B vitamin supplementation (Fig. 5). Compared to sham, effects of PM2.5 on WBCs were non-significant in the presence of B vitamin supplementation: two-hour PM2.5 exposure was associated with a −1.7% (95% CI, −9.6%, 6.9%; P = 0.67; Pintervention = 0.008), −3.1% (95% CI, −17.4%, 13.8%; P = 0.68; Pintervention = 0.06), and 2.4% (95% CI, −7.4%, 13.1%; P = 0.62; Pintervention = 0.09) change in total WBCs, neutrophils, and lymphocytes, respectively (Supplementary Table 6). In summary, B vitamin supplementation reduced the PM2.5 effect by 117%, 134%, 76%, and 75% on total WBCs, neutrophils, lymphocytes, and monocytes, respectively (Fig. 5).
Likewise, B vitamin supplementation attenuated the PM2.5 effects on total and differential WBC counts at 24 h post-exposure (Pintervention = 0.006, 0.01, 0.02, 0.61 for total WBC, neutrophil, lymphocyte, and monocyte) (Supplementary Table 6). B-vitamin supplementation significantly reduced the PM2.5 effect by 139% on total WBC, 165% on neutrophil, and 106% on lymphocyte (Fig. 5).
Sensitivity analysis
We dealt with potential influence by season by adjusting for spring/summer/fall/winter in all models. In a sensitivity analysis, we additionally adjusted for seasonality (defined using sine and cosine functions)21 to further address residual confounding, and our conclusions remained the same (data not shown). We observed no significant changes in dietary intake of folic acid, vitamins B6, and B12 during the study period, therefore confounding due to dietary B vitamins was minimized (Supplementary Table 7). To rule out the possibility that the observed change in HRV was partially due to HR fluctuation, we adjusted for HR in PM2.5-HRV analysis and obtained similar results (data not shown). In addition, we conducted sensitivity analysis using HR-normalized HRV measurements and our conclusions were consistent (Supplementary Table 8).
Discussion
This single-blind crossover intervention trial with controlled exposure experiments found that two-hour exposure to concentrated ambient PM2.5 (250 μg/m3) has substantial physiologic impacts on HR, HRV, and WBCs among healthy adults. Further, we demonstrated that these effects are nearly abolished with four-week B-vitamin supplementation.
With ambient PM2.5 levels far exceeding NAAQS in many urban megacities worldwide22, pollution regulation remains the backbone of public health protection against its cardiovascular health effects. Indeed, improved cardiovascular health, reflected in reduced morbidity and mortality, has been documented as pollution levels have decreased in the U.S23. Nevertheless, even in U.S. cities complying with NAAQS, cardiovascular effects of particle pollution have been observed, with no evidence for a threshold for effect in sensitive individuals3,4,6,22. Thus, the medical and public health communities have sought adjunct personal measures that might complement regulation in reducing the cardiovascular risk of pollution in sensitive people24.
Previous studies suggested that dietary supplementations with vitamins C, vitamins E, or polyunsaturated fatty acids might protect against short-term air pollution-induced adverse cardiopulmonary responses25,26,27. In a randomized double-blinded controlled exposure study, Tong and coauthors successfully demonstrated that a four-week fish oil supplementation attenuated CAP-induced HRV reductions26. Our choice to assess the potential protective benefits of B vitamin supplementation against PM-induced cardiac autonomic dysfunction and inflammation was motivated by the anti-inflammatory, antioxidant, and immunoepigenetic effects of B vitamins28,29. Recent epidemiological and in vivo studies suggest that B vitamins might be particularly protective against air pollution-induced cardiovascular effects—as it was demonstrated to modulate the epigenetic and inflammatory signaling pathways linking air pollution, intermediate biomarkers, and cardiovascular outcomes6,17,27,28. For example, folic acid and vitamin B6 lower chemokine release from peripheral blood mononuclear cells and circulating levels of pro-inflammatory molecules28,29, indicating reduced risk for acute cardiovascular events such as stroke. In mice model, folic acid protects against lipopolysaccharide-induced nuclear factor-kβ pathway activation and adverse birth outcomes16. Furthermore, B vitamins are essential nutrients involved in the biochemical process of DNA methylation3. In the presence of air pollution, adequate B vitamin intake ensures proper epigenetic status of leukocytes to warrant proper immuno-regulation, and prevents excessive oxidative damage to the cardiovascular system3. Although the results of randomized controlled trials on supplementation with folic acid, vitamin B6 and B12 do not support benefits of B vitamins for either primary or secondary CVD prevention12,14,15,30, the mentioned interactive biological properties of B vitamins render it a promising preventive strategy to minimize the cardiovascular damage due to ambient PM2.5 pollution. However, no prior clinical investigation has tested whether B vitamin supplementation can be used to guard the cardiovascular system from the adverse health effects of PM2.5.
Our findings of a primary autonomic effect of PM2.5 are consistent with previous human controlled exposures studies31,32,33,34, showing that short-term PM2.5 exposure perturbed cardiorespiratory autonomic function as reflected in increased HR and reduced HRV6. Immediately following two-hour exposure to ambient concentrated PM2.5, we observed a substantial increase in resting HR and a reduction in LF power. These results indicate a consistent reduction in HRV across five measures – which reflects the adverse pathophysiological modulations in cardiac autonomic control by PM2.5 exposure.
PM2.5 is a potent trigger for leukocyte-mediated inflammation, which is proposed as the key mechanism underlying the pathological modulation of the cardiovascular system by PM2.5 exposure4. Our data support this hypothesis by showing that two-hour PM2.5 exposure triggers increased total WBC count and lymphocyte count at 24-hour post exposure. In healthy adults, PM pollution increases the number of neutrophils and lymphocytes in alveolar lavage and peripheral blood35. While the underlying biological mechanism remains unclear, in vivo studies suggest that PM stimulates bone marrow via alveolar macrophages-mediated cytokine signaling, leading to accelerated release of immature leukocytes in to the circulation36,37.
Twenty-four hours after exposure, the effect of PM2.5 on HR and HRV weakened. However, PM2.5 exposure remained significantly associated with higher numbers of total WBCs and lymphocytes. Taken together, although the acute physiological responses due to PM2.5 exposure peak might be reversible, the pro-inflammatory effects of PM2.5 appears to be sustained beyond 24 hours and represent a biomarker that could have clinical relevance to sensitive individuals in a community setting4.
For the first time, our trial provides evidences demonstrating the unique preventive benefits of B vitamin administration in the context of air pollution: B vitamin supplementation can diminish the acute effects of PM2.5 on cardiac autonomic dysfunction and inflammatory markers. These findings are in agreement with our results from the Normative Aging Study6 – a population with average B vitamins intakes well above the standard dietary references – in which short-term PM2.5 exposure was associated with lower HRV (7.1% reduction in SDNN per 10 μg/m3 increase in PM2.5), and the adverse effect of PM2.5 was limited to subjects with lower (<median) intakes of vitamin B6, vitamin B12, or methionine.
This study has several strengths, including its crossover design with controlled exposure experiments – which simulate conditions similar to urban air pollution peaks, while allowing for control of exposure and treatment at the individual level. The Harvard ambient particle concentrators do not affect the concentration of gaseous pollutants, therefore, minimizing the confounding due to gaseous co-pollutants such as ozone and sulfur dioxide. All exposure experiments were conducted at the same time of day to eliminate impacts of diurnal variation. We adjusted for time-varying factors including season, chamber temperature and humidity to minimize their influence on the observed associations, while time invariant factors are controlled by the crossover design.
We acknowledge several limitations, however. We determined the number to recruit in the current study using power estimates that are penalized by conservative Bonferroni’s adjustments for multiple HRV indexes. Although our sample size is comparable to previous controlled CAP exposure studies, which succeeded in demonstrating health effects of CAP exposure32,33,38,39, our study is evidently limited in power to detect small effects with only 10 subjects (30 controlled exposure experiments).
Further, treatment sequence could not be randomized due to the long half-life of B vitamins, therefore might be subject to confounding by period or ordering effects. For example, the first exposure experiment is likely to produce more distress on volunteers because of psychological effect. We intentionally provided medical air as the first exposure experiment; therefore the psychological effect is expected to bias the effect of PM2.5 towards the null. The short study duration with four-week intervals between exposure experiments also reduced the impact of temporal trends. In addition, we contrasted the post- vs pre-exposure status to ascertain all outcome measurements, which is expected to be less prone to confounding due to temporal trend than the absolute values. While residual confounding is possible, considering the magnitude of our effect estimates and the consistency across different HRV index, it is unlikely that the observed association reflected bias from confounding. The crossover design of the present study was not complete, as we had no arm of B vitamin supplementation with sham exposure. Therefore, separating the direct effect of B vitamins on cardiac autonomic dysfunction and inflammation (i.e., in the absence of air pollution) from the combined effect of both B vitamins and air pollution can be statistically challenging and requires strong assumptions. In addition, our study was limited to healthy adults from lightly polluted urban environment, therefore our findings might not be generalizable to populations that are at higher risk for pollution-induced cardiovascular effects (eg, children, older adults, individuals with pre-existing cardiovascular disease, and individuals residing in heavily polluted areas).
Apart from avoiding exercising outdoors at peak pollution times, sensitive individuals have limited options to reduce exposure and associated cardiovascular risk. While regulation is the backbone of prevention, residual risk remains for those who are sensitive, and high exposures are, unfortunately, the rule still in many megacities throughout the world. The present study provides novel experimental evidence showing that an ambient PM2.5 exposure peak has unfavorable effect on cardiac autonomic function and the immune system, which can be counteracted by B vitamin supplementation. Our project inaugurates a line of research for the development of preventive pharmacological interventions using B vitamins to contain the health effects of air pollution. Future studies will identify the precise pathophysiological processes of PM-induced cardiovascular responses and inflammation, as well as the mechanistic pathway underlying the protective effect of B vitamins.
Methods
Study population and sample size
We recruited ten healthy, 18–60-year-old, non-smoking volunteers who were not on any form of B vitamin supplementation or other medication, from the University of Toronto St. George campus and surrounding area (downtown Toronto, Ontario, Canada)19. The number to recruit was determined through power calculation based on a 2-sided alternative at α = 0.05/6 = 0.0833 to reflect a Bonferroni correction for multiple testing (six HRV indexes). We estimate 80% (90%) power to detect correlations with absolute magnitude of 0.40 (0.45) in ten volunteers with two repeated measures, which is less than or equal to the magnitude of the correlations reported in our previous studies33,38,39. The trial and experimental protocols were approved by all participating institutional review board (University of Toronto, St. Michael’s Hospital, and Harvard T.H. Chan School of Public Health) and registered (clinicaltrials.gov NCT01864824, date of registration: May 8, 2013). All methods were performed in accordance with the relevant guidelines and regulations. All volunteers provided written informed consent. The conduct of the trial was monitored by an independent data and safety monitoring committee.
Study design
We conducted a single-blind placebo-controlled crossover pilot trial (Fig. 1)19 with controlled exposure experiments (July 2013 to February 2014). A two-hour sham exposure experiment (exposure one, particle-free medical air) was included to provide baseline data. All volunteers then received placebo for four weeks preceding the two-hour exposure experiment to concentrated ambient PM2.5 (exposure two, 250 μg/m3). After exposure two, we administered B vitamin supplements for four weeks before the next two-hour exposure experiment to PM2.5 (exposure three, 250 μg/m3). The four-week placebo or B vitamin treatment also served as washout periods between exposure experiments to diminish the carryover effect of PM2.5 exposure19,40, while minimizing the impact of seasonality and temporal trend on the source and composition of the concentrated ambient PM2.5. To ensure comparable conditions across all controlled exposure experiments to PM2.5, the present study could not randomize on the treatment (placebo vs B vitamins) sequence because vitamin B12 has a biological half-life longer than four months41. Study volunteers were blinded to exposure and treatment allocation. Based on our symptom survey, none of the volunteers was able to discern the exposure type for any exposure experiment.
Exposure facility
Harvard fine particle concentrators with a dilution control system delivered target-concentration PM2.542, and the sham exposures with medical air were generated as previously described38. The concentrated ambient PM2.5 air stream was delivered directly to the volunteer who was seated inside a 4.9 m3 (1.1 × 1.9 × 2.0 m) Lexan enclosure, at rest and breathing normally via an “oxygen type” facemask covering his/her nose and mouth. During each exposure experiment to PM2.5, particles were collected on Teflon filters for monitoring gravimetric determination of PM2.5 exposure mass concentration (μg/m3).
Folic acid, vitamin B6 and B12 supplement
During three four-week periods, we administered one B vitamin tablet (2.5 mg folic acid, 50 mg vitamin B6, and 1 mg vitamin B12) or placebo daily. The placebo tablets contain identical non-medical ingredients as the B vitamin tablets. Tablet preparation and packaging were done by an external lab (Jamieson Laboratory, Toronto, Canada). The label coding was blinded to the volunteers. We monitored volunteers’ plasma folic acid and vitamin B6 and B12 levels before each exposure experiment. A self-administered validated semi-quantitative Food Frequency Questionnaire was used to assess dietary B vitamin intake at the first and last visits to rule out potential impact from diet.
Heat rate, heart rate variability, and WBC measurement
We measured supine resting HR and HRV as the primary outcome before (pre-exposure) and after (immediately post-exposure and 24 h post-exposure) each exposure experiment, using high-resolution (1 KHz sample rate) digital 12-lead Holter electrocardiogram monitors (H12 + recorder, Mortara Instruments, Milwaukee, WI). We extracted ten-minute HRV readings on time domain outcomes (SDNN, rMSSD, pNN50), and frequency domain outcomes (LF power, HF power, and LF/HF ratio). We discarded the first three minutes and the last two minutes during the ten-minute recording and analyzed the remaining five-minute electrocardiogram data using standardized techniques43. SDNN represents the total variability. PNN50, rMSSD, and HF are sensitive to high-frequency heart rate fluctuations and are considered as measures of cardiac vagal tone modulation, while LF power is linked to the activity of both sympathetic and parasympathetic nervous system.
Blood samples (pre-, post-, and 24 h post-exposure) were obtained in ethylenediaminetetraacetic acid vacutainer tubes, stored at 4 °C, and subsequently processed in a local laboratory within two hours for total and differential WBC counts using the Technicon H-1 automated hematology analyzer (Technicon Instruments Corp, Tarrytown, NY, USA).
Statistical methods
We conducted graphical explorations and log10-transformed the HRV measures and WBC counts to improve normality and stabilize the variance. We examined the linear relationships between HR/HRV/WBC and all independent variables and covariates, and observed no deviation from linearity. For the ease of interpretation, we scaled the effect estimates to the percent changes in HRV and WBC in all models.
We used linear mixed-effects models with a robust/sandwich estimator for the variance (Model 1) to account for within-subject correlation in the outcome measures. Random intercepts were assigned to each subject. In all models, we adjusted for covariates with potential influences on HR, HRV, and WBC – selected based on prior knowledge and the existing literature – season (fall/winter/spring/summer), chamber temperature, and relative humidity.
 |
In the above model, Yij was the change in HR, HRV, or WBC (i.e., ΔHR = post-exposure HR – pre-exposure HR) for participant i at exposure occasion j. β0 was the overall intercept, and bi was the separate random intercept for subject i with, bi ~ N(0, ϴ), εij ~ N(0, σ2). X1ij was a binary variable indicating exposure to PM2.5 or medical air. X2ij was a binary variable indicating placebo or B vitamin supplementation. X3ij–Xpij were the covariates, for participant i at measurement j. The main effect of B vitamin supplementation was not included in the model, given volunteers did not receive any medical air exposure while on B vitamin supplementation. β1 represents the effect of PM2.5 exposure without B vitamin supplementation and β1 +β2 represents the effect of PM2.5 exposure with B vitamin supplementation. β2 thus represents the intervention effect of B vitamin supplementation (i.e, the attenuation of PM2.5 effect due to B vitamin supplementation). A two tailed value of P ≤ 0.05 was considered statistically significant. We represent the P value for the intervention effect, β2,by Pintervention. Analyses were performed using SAS 9.4 (SAS Institute, Cary NC).
Additional Information
How to cite this article: Zhong, J. et al. B-vitamin Supplementation Mitigates Effects of Fine Particles on Cardiac Autonomic Dysfunction and Inflammation: A Pilot Human Intervention Trial. Sci. Rep. 7, 45322; doi: 10.1038/srep45322 (2017).
Publisher's note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Material
Acknowledgments
We thank the Jamison laboratory for providing the B vitamins and placebo tablets for our trial. This study was supported by NIH grants R21ES021895, R01ES021733, R01ES020836, R01ES021357, T32ES007142, and P30ES000002. This publication was made possible by U.S. Environmental Protection Agency grant RD-834798 and RD-832416. Its contents are solely the responsibility of the grantee and do not necessarily represent the official views of the USEPA. Further, USEPA does not endorse the purchase of any commercial products or services mentioned in the publication.
Footnotes
The authors declare no competing financial interests.
Author Contributions J.Z. coordinated the study, analysed the data, and wrote the manuscript. F.S., B.U., and M.S. conducted the exposure experiments and collected data. G.L. and A.T. supervised the volunteer safety and contributed to data collection. P.K. developed the Harvard fine particle concentrators with dilution system. B.C., A.W., P.K., D.R.G., L.T., X.L., and S.W. provided critical revisions. A.A.B. conceived the study, oversaw research, helped to write the manuscript, and provided intellectual input throughout the study. All authors have read and approved the final manuscript.
References
- World Health Organization. Burden of disease from ambient air pollution for 2012. Public Health, Social and Environmental Determinants of Health Department, World Health Organization, Geneva, Switzerland (2014). [Google Scholar]
- Nawrot T. S., Perez L., Kunzli N., Munters E. & Nemery B. Public health importance of triggers of myocardial infarction: a comparative risk assessment. Lancet 377, 732–740, doi: S0140-6736(10)62296-9 (2011). [DOI] [PubMed] [Google Scholar]
- Zhong J. et al. Cardiac Autonomic Dysfunction: Particulate Air Pollution Effects Are Modulated by Epigenetic Immunoregulation of Toll‐like Receptor 2 and Dietary Flavonoid Intake. Journal of the American Heart Association 4, e001423 (2015). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brook R. D. et al. Particulate matter air pollution and cardiovascular disease: An update to the scientific statement from the American Heart Association. Circulation 121, 2331–2378, doi: CIR.0b013e3181dbece1 (2010). [DOI] [PubMed] [Google Scholar]
- Wong E. On Scale of 0 to 500, Beijing’s Air Quality Tops ‘Crazy Bad’ at 755, http://www.nytimes.com/2013/01/13/science/earth/beijing-air-pollution-off-the-charts.html?_r=0 (2013).
- Baccarelli A. et al. Cardiac Autonomic Dysfunction: Effects from Particulate Air Pollution and Protection by Dietary Methyl Nutrients and Metabolic Polymorphisms. Circulation 117 (2008). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gold D. R. et al. Ambient pollution and heart rate variability. Circulation 101, 1267–1273 (2000). [DOI] [PubMed] [Google Scholar]
- Voutilainen S., Rissanen T. H., Virtanen J., Lakka T. A. & Salonen J. T. Low dietary folate intake is associated with an excess incidence of acute coronary events The Kuopio Ischemic Heart Disease Risk Factor Study. Circulation 103, 2674–2680 (2001). [DOI] [PubMed] [Google Scholar]
- Bazzano L. A. et al. Dietary intake of folate and risk of stroke in US men and women: NHANES I Epidemiologic Follow-up Study. National Health and Nutrition Examination Survey. Stroke 33, 1183–1188 (2002). [DOI] [PubMed] [Google Scholar]
- Righetti M., Serbelloni P., Milani S. & Ferrario G. Homocysteine-lowering vitamin B treatment decreases cardiovascular events in hemodialysis patients. Blood Purif 24, 379–386, doi: 10.1159/000093680 (2006). [DOI] [PubMed] [Google Scholar]
- Zoungas S. et al. Cardiovascular morbidity and mortality in the Atherosclerosis and Folic Acid Supplementation Trial (ASFAST) in chronic renal failure: a multicenter, randomized, controlled trial. Journal of the American College of Cardiology 47, 1108–1116 (2006). [DOI] [PubMed] [Google Scholar]
- Liem A., Reynierse-Buitenwerf G., Zwinderman A., Jukema J. & Van Veldhuisen D. Secondary prevention with folic acid: results of the Goes extension study. Heart 91, 1213–1214 (2005). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wrone E. M. et al. Randomized trial of folic acid for prevention of cardiovascular events in end-stage renal disease. Journal of the American Society of Nephrology 15, 420–426 (2004). [DOI] [PubMed] [Google Scholar]
- Toole J. F. et al. Lowering homocysteine in patients with ischemic stroke to prevent recurrent stroke, myocardial infarction, and death: the Vitamin Intervention for Stroke Prevention (VISP) randomized controlled trial. JAMA 291, 565–575 (2004). [DOI] [PubMed] [Google Scholar]
- Wang X. et al. Efficacy of folic acid supplementation in stroke prevention: a meta-analysis. The Lancet 369, 1876–1882 (2007). [DOI] [PubMed] [Google Scholar]
- Zhao M. et al. Folic acid protects against lipopolysaccharide-induced preterm delivery and intrauterine growth restriction through its anti-inflammatory effect in mice (2013). [DOI] [PMC free article] [PubMed]
- Dolinoy D. C., Huang D. & Jirtle R. L. Maternal nutrient supplementation counteracts bisphenol A-induced DNA hypomethylation in early development. Proceedings of the National Academy of Sciences 104, 13056–13061 (2007). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kolling J., Scherer E. B., Da Cunha A. A., Da Cunha M. J. & Wyse A. T. Homocysteine induces oxidative–nitrative stress in heart of rats: prevention by folic acid. Cardiovascular toxicology 11, 67–73 (2011). [DOI] [PubMed] [Google Scholar]
- Zhong et al. B vitamins attenuate the epigenetic effects of ambient fine particles in a pilot human intervention trial,PNAS, doi: 10.1073/pnas.1618545114 (2017). [DOI] [PMC free article] [PubMed]
- Zhong J. et al. Endotoxin and β-1, 3-d-glucan in concentrated ambient particles induce rapid increase in blood pressure in controlled human exposures. Hypertension 66, 509–516 (2015). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stolwijk A., Straatman H. & Zielhuis G. Studying seasonality by using sine and cosine functions in regression analysis. Journal of epidemiology and community health 53, 235–238 (1999). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lelieveld J., Evans J. S., Fnais M., Giannadaki D. & Pozzer A. The contribution of outdoor air pollution sources to premature mortality on a global scale. Nature 525, 367–371, doi: 10.1038/nature15371 (2015). [DOI] [PubMed] [Google Scholar]
- US Environmental Protection Agency. The Benefits and Costs of the Clean Air Act: 1990 to 2010. Washington, DC: US Environmental Protection Agency, Office of Air and Radiation (1997).
- Gold D. R. & Samet J. M. Air pollution, climate, and heart disease. Circulation 128, e411–e414 (2013). [DOI] [PubMed] [Google Scholar]
- Tong H. Dietary and pharmacological intervention to mitigate the cardiopulmonary effects of air pollution toxicity. Biochimica et Biophysica Acta (BBA)-General Subjects 12, 2891–2898 (2016). [DOI] [PubMed] [Google Scholar]
- Tong H. et al. Omega-3 fatty acid supplementation appears to attenuate particulate air pollution-induced cardiac effects and lipid changes in healthy middle-aged adults. Environmental health perspectives 120, 952 (2012). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tong H. et al. Dietary supplementation with olive oil or fish oil and vascular effects of concentrated ambient particulate matter exposure in human volunteers. Environmental health perspectives 123, 1173 (2015). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holven K. B., Aukrust P., Holm T., Ose L. & Nenseter M. S. Folic acid treatment reduces chemokine release from peripheral blood mononuclear cells in hyperhomocysteinemic subjects. Arteriosclerosis, thrombosis, and vascular biology 22, 699–703 (2002). [DOI] [PubMed] [Google Scholar]
- Friso S., Jacques P. F., Wilson P. W., Rosenberg I. H. & Selhub J. Low circulating vitamin B6 is associated with elevation of the inflammation marker C-reactive protein independently of plasma homocysteine levels. Circulation 103, 2788–2791 (2001). [DOI] [PubMed] [Google Scholar]
- Yang H.-T., Lee M., Hong K.-S., Ovbiagele B. & Saver J. L. Efficacy of folic acid supplementation in cardiovascular disease prevention: an updated meta-analysis of randomized controlled trials. European journal of internal medicine 23, 745–754 (2012). [DOI] [PubMed] [Google Scholar]
- Brook R. D. et al. Insights into the mechanisms and mediators of the effects of air pollution exposure on blood pressure and vascular function in healthy humans. Hypertension 54, 659–667, doi: 10.1161/HYPERTENSIONAHA.109.130237 (2009). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Urch B. et al. Relative contributions of PM2.5 chemical constituents to acute arterial vasoconstriction in humans. Inhal Toxicol 16, 345–352, doi: 10.1080/08958370490439489 (2004). [DOI] [PubMed] [Google Scholar]
- Brook R. D. et al. Inhalation of fine particulate air pollution and ozone causes acute arterial vasoconstriction in healthy adults. Circulation 105, 1534–1536 (2002). [DOI] [PubMed] [Google Scholar]
- Devlin R., Ghio A., Kehrl H., Sanders G. & Cascio W. Elderly humans exposed to concentrated air pollution particles have decreased heart rate variability. European Respiratory Journal 21, 76s–80s (2003). [DOI] [PubMed] [Google Scholar]
- Salvi S. et al. Acute inflammatory responses in the airways and peripheral blood after short-term exposure to diesel exhaust in healthy human volunteers. American journal of respiratory and critical care medicine 159, 702–709 (1999). [DOI] [PubMed] [Google Scholar]
- Mukae H. et al. The effect of repeated exposure to particulate air pollution (PM10) on the bone marrow. American Journal of Respiratory and Critical Care Medicine 163, 201–209 (2001). [DOI] [PubMed] [Google Scholar]
- Goto Y. et al. Particulate matter air pollution stimulates monocyte release from the bone marrow. American journal of respiratory and critical care medicine 170, 891–897 (2004). [DOI] [PubMed] [Google Scholar]
- Behbod B. et al. Endotoxin in concentrated coarse and fine ambient particles induces acute systemic inflammation in controlled human exposures. Occupational and environmental medicine, oemed-2013-101498 (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bellavia A. et al. DNA hypomethylation, ambient particulate matter, and increased blood pressure: findings from controlled human exposure experiments. Journal of the American Heart Association 2, e000212 (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Urch B. et al. Acute blood pressure responses in healthy adults during controlled air pollution exposures. Environ Health Perspect 113, 1052–1055 (2005). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Butler C. C. et al. Oral vitamin B12 versus intramuscular vitamin B12 for vitamin B12 deficiency: a systematic review of randomized controlled trials. Family Practice 23, 279–285, doi: 10.1093/fampra/cml008 (2006). [DOI] [PubMed] [Google Scholar]
- Demokritou P., Gupta T., Ferguson S. & Koutrakis P. Development of a high-volume concentrated ambient particles system (CAPS) for human and animal inhalation toxicological studies. Inhalation Toxicology 15, 111–129, doi: 10.1080/08958370304475 (2003). [DOI] [PubMed] [Google Scholar]
- Task Force of the European Society of Cardiology and the North American Society of Pacing and Electrophysiology. Heart rate variability. Standards of measurement, physiological interpretation, and clinical use. European Heart Journal 17, 354–381 (1996). [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.