Abstract
Background
As the largest integrated US health system, the Veterans Health Administration (VHA) provides unique national data to expand knowledge about the association between neighborhood socioeconomic status (NSES) and health. Although living in areas of lower NSES has been associated with higher mortality, previous studies have been limited to higher-income, less diverse populations than those who receive VHA care.
Objective
To describe the association between NSES and all-cause mortality in a national sample of veterans enrolled in VHA primary care.
Design
One-year observational cohort of veterans who were alive on December 31, 2011. Data on individual veterans (vital status, and clinical and demographic characteristics) were abstracted from the VHA Corporate Data Warehouse. Census tract information was obtained from the US Census Bureau American Community Survey. Logistic regression was used to model the association between NSES deciles and all-cause mortality during 2012, adjusting for individual-level income and demographics, and accounting for spatial autocorrelation.
Participants
Veterans who had vital status, demographic, and NSES data, and who were both assigned a primary care physician and alive on December 31, 2011 (n = 4,814,631).
Main Measures
Census tracts were used as proxies for neighborhoods. A summary score based on census tract data characterized NSES. Veteran addresses were geocoded and linked to census tract NSES scores. Census tracts were divided into NSES deciles.
Key Results
In adjusted analysis, veterans living in the lowest-decile NSES tract were 10 % (OR 1.10, 95 % CI 1.07, 1.14) more likely to die than those living in the highest-decile NSES tract.
Conclusions
Lower neighborhood SES is associated with all-cause mortality among veterans after adjusting for individual-level socioeconomic characteristics. NSES should be considered in risk adjustment models for veteran mortality, and may need to be incorporated into strategies aimed at improving veteran health.
Electronic supplementary material
The online version of this article (doi:10.1007/s11606-016-3905-x) contains supplementary material, which is available to authorized users.
KEY WORDS: risk adjustment, veteran, socioeconomic factors, public health, clinical epidemiology
INTRODUCTION
Social and environmental factors such as neighborhood characteristics are increasingly recognized as potentially better determinants of health than direct health care services.1 Lower neighborhood socioeconomic status (NSES) has been associated with higher mortality, lower physical functioning, and worse health status.2 – 5 The mechanisms by which NSES affects health may include increased physiologic stress, lack of resources necessary for a healthy lifestyle, lower levels of social cohesion and social support,6 – 8 and less availability of public services and access to quality medical care.9
Increasingly, health care organizations are being asked to assume financial risk for enrolled patients. However, current risk adjustment measures may not adequately capture all dimensions of patient risk.10 There are ongoing efforts by the Veterans Health Administration (VHA) and other integrated health systems to develop population health indicators and risk adjustment methods to account for differences in population health.11 As one of the largest US integrated health systems, the VHA is increasingly interested in social determinants of veterans’ health,12 in part because the Department of Veterans Affairs (VA) is charged by statute with addressing both the medical and non-medical needs of the veteran population. The VHA prioritizes the provision of health care services based on military service-related disability and income. Veterans who use VHA services generally have worse health status and increased disability days, and are from more socially disadvantaged groups, than the general population.13 , 14 Despite the large body of literature examining the impact of neighborhood on health, previous studies in the US have been limited by (1) examination of higher-income populations with limited racial/ethnic diversity15 or (2) national studies with limited information on individual health status and comorbidity.16 , 17 The goal of this study is to describe the association between NSES and all-cause mortality in a national sample of veterans enrolled in VHA primary care, using national data from a diverse multi-racial sample.
METHODS
Study Design
We performed an observational cohort study of veterans who received health services from the VHA, had a VHA primary care provider in 2011, and were alive on December 31, 2011. Our outcome of interest was death in the following year, with ascertainment of vital status through December 31, 2012. We included all veterans enrolled in VHA primary care, regardless of VHA utilization, given the VHA mission to care for this population of patients. We used data from the VHA Corporate Data Warehouse (CDW) to obtain clinical and administrative data and vital status.18 We used census tract data from the American Communities Survey (ACS) to determine neighborhood SES, which was linked to geocoded individual veteran data.
Data Sources
VHA Corporate Data Warehouse (CDW)
Information about individual demographic and health characteristics were obtained from the VHA CDW. The Primary Care Management Module (PCMM), contained within the CDW, is used to manage patient panels in primary care, and allows facilities to track patients and their assigned primary care provider (PCP). Because we wanted to include only veterans engaged in care at the VHA, we included veterans who were enrolled and assigned to a PCP.
Sociodemographic and health information included age, sex, race/ethnicity, and household income. In addition, the CDW has information on individual disease comorbidities, which we used to generate Gagne comorbidity scores based on diagnoses occurring in 2011.19 The Gagne score combines previously validated Charlson Index and Elixhauser comorbidity classification systems and performs numerically better in predicting both short- and long-term mortality.19 Eligibility for VHA services is determined by enrollment in priority groups based on service-connected medical conditions, length of military service, disability, and income.20 We categorized individuals based on their copayment requirement according to VHA definitions (copayment-exempt vs. not copayment-exempt). Low-income patients or those with a 50 % or higher service-connected disability receive care without copayments, while others have copayments for medications and office visits.20
The Planning Systems Support Group (PSSG) enrollment file contains the geographic coordinates geocoded from veteran addresses.21 We spatially joined the x/y coordinates of the most recently known residential addresses of our patients to the 2010 census tract boundary file to obtain the census tract Federal Information Processing Series (FIPS) code for each patient. The majority of the geocoded data (87.6 %) were based on actual addresses. The remainder were based on ZIP Codes, ZIP+4, or street midpoints (2.8 %, 8.9 %, and 0.8 %, respectively), and the majority of the less precise coordinates came from rural regions (63.0 %). There was also a systematic increase in the proportion of these coordinates in the SES deciles moving from the tenth to the first deciles (Online Appendix Table A5). Because the missing pattern was non-random, veterans with non-address-based coordinates were included in the analysis to prevent bias, at the expense of possibly associating patients with incorrect census tracts. The enrollment file includes information on urban or rural location indicators for each veteran based on US Census Bureau delineations.
American Communities Survey (ACS)
The ACS is a survey of approximately 3.5 million households, collected annually by the US Census Bureau throughout the year using mailed questionnaires, telephone interviews, and visits from Census Bureau field representatives. The ACS accumulates samples over 5-year intervals to produce estimates for smaller geographic areas, including census tracts.22 We used the 5-year rolling average from 2008 to 2012. Census tracts are designed to be relatively homogeneous with respect to population characteristics, economic circumstances, and living conditions, and contain a consistent number of residents (3000–8000 individuals).23 We used census tracts (n = 72,722) as proxies for neighborhoods.
Neighborhood SES Measure
Neighborhood SES was measured using a previously developed 100-point NSES index.6 , 8 , 24 Because there is no uniformly accepted criterion in the US for measuring neighborhood socioeconomic status and area deprivation, we chose the NSES index based on previous studies in the veteran population14 and in the national US population.6 , 8 , 24 Components of the NSES index were identified in previous national US studies using factor analysis to understand the influence of neighborhood on health.6 , 8 , 24 The NSES index consists of six components: 1) percentage of adults age 25 years or older with less than a high school education; 2) percentage of men who are unemployed; 3) percentage of households with income below the poverty level; 4) percentage of households receiving public assistance; 5) percentage of households with children in which the head of household is female; and 6) median household income. A Z-score was computed for each variable by subtracting the population mean and then dividing by the population standard deviation. The NSES index was calculated by subtracting the Z-scores for the first five components from that of the median household income, and then scaling the result to range from 0 to 100, with higher values corresponding to higher NSES. Veterans were classified by the decile of NSES index, with deciles derived from the calculated distribution of veteran NSES scores.
Statistical Analysis
Logistic regression was used to estimate the odds of mortality in 2012 as a function of NSES index. In order to understand the influence of neighborhood SES as compared to individual factors and medical comorbidity, three models were considered. The first model tests the association of NSES decile of residence and mortality, adjusting for age, gender, race/ethnicity, and census tract rurality. We included individual-level income and copayment status in the second model, because it has been shown previously that studies that did not adjust for individual-level SES measures were more likely to observe an area-level SES effect, while studies that included individual SES indicators generally found lower neighborhood effects.4 As a sensitivity analysis, we ran models 1 and 2 among the veterans who had address-based geocodes. Because of the potential for reverse causality (e.g. health status determining neighborhood choice), comorbidity was considered separately. The results of these two models, with the Gagne scores, are included in the appendix (models 1b and 2b, respectively).
Given the spatial nature of the data, a spatially correlated random effect was entered into each model to account for spatial autocorrelation at the county or county-equivalent level. The random effect was modeled with the intrinsic conditional autoregressive model (ICAR).25 , 26 This model fits a county-level random effect with each county effect s i distributed normally with a mean of its neighboring county effects and variance equal to the overall random effect variance scaled by the number of its neighbors: , where is the neighborhood of county i, and n i is the number of counties in θ i. The county level was chosen as the unit of correlation instead of the census tract, as the number of census tracts (over 72,000) made the estimation prohibitively difficult. Spatial models are often built using Bayesian methods.25 However, this was not practical here due to the size of the models considered. All models were therefore fit using the GLIMMIX procedure in SAS 9.4 (SAS Institute Inc., Cary, NC), with the ICAR covariance random effects matrix developed using R (R Core Team). Neighborhood adjacency was based on the queen continuity which defines two polygons as being adjacent if they share one or more common points. Our analysis is hierarchical, using the census tract-level SES index and county-level correlation structure. We also calculated the C-statistic for each model, which defines how well the model discriminates subjects who have an event (death) from those who do not.
For each model, we also estimated the average marginal effect (AME)27 of the NSES index on the probability of death using the tenth NSES decile (highest SES) as a baseline. The AME can be interpreted here as the excess probability associated with being in a lower NSES compared to the tenth (highest) decile. The AME on excess lives lost was then determined by taking the product of the number of veterans at risk within each NSES decile and the marginal effect of that risk category.
RESULTS
Our study population consisted of all veterans having vital status, demographic, and NSES data, and who were both assigned a primary care physician and alive on December 31, 2011 (n = 4,814,631), representing 96 % of veterans enrolled in VHA primary care. The sample was mostly men, almost half of the sample was over the age of 65, and two-thirds of the population lived in urban areas (Table 1). Seventy-five percent were white and 15 % African American. The overall unadjusted mortality for the population during the study period was 2.7 % (n = 127,693 deaths for those with complete vital status, demographic, and NSES data).
Table 1.
Population Characteristics, National Sample of Veterans in VHA Primary Care
| Total population (n = 5,018,726) | Alive through 12/31/2011 (n = 4,887,836) | Died on or before 12/31/2012 (n = 130,890) | ||||
|---|---|---|---|---|---|---|
| n | % | n | Column % | n | Column % | |
| Age categories (years) | ||||||
| Missing | 280 | 0.01 | 274 | 0.01 | 6 | 0.005 |
| 18–44 | 687,060 | 13.69 | 685,802 | 14.03 | 1258 | 0.96 |
| 45–64 | 1,966,944 | 39.19 | 1,941,361 | 39.72 | 25,583 | 19.55 |
| 65–74 | 1,115,337 | 22.22 | 1,090,122 | 22.30 | 25,215 | 19.26 |
| 75 or greater | 1,249,105 | 24.89 | 1,170,277 | 23.94 | 78,828 | 60.22 |
| Race/ethnicity | ||||||
| Missing | 142,109 | 2.83 | 141,040 | 2.89 | 1069 | 0.82 |
| White | 3,679,766 | 73.32 | 3,571,524 | 73.07 | 108,242 | 82.70 |
| Black | 744,914 | 14.84 | 731,561 | 14.97 | 13,353 | 10.20 |
| Hispanic | 281,672 | 5.61 | 276,758 | 5.66 | 4914 | 3.75 |
| Asian, non-Hispanic | 35,263 | 0.7 | 34,823 | 0.71 | 440 | 0.34 |
| Pacific Islander | 23,192 | 0.46 | 22,697 | 0.46 | 495 | 0.38 |
| American Indian/Alaskan Native (non-Hispanic) | 29,558 | 0.59 | 28,886 | 0.59 | 672 | 0.51 |
| Other non-Hispanic | 5216 | 0.1 | 5098 | 0.10 | 118 | 0.09 |
| Multi-race non-Hispanic | 75,065 | 1.5 | 73,499 | 1.50 | 1566 | 1.20 |
| Asian non-Hispanic Pacific Islander | 1971 | 0.04 | 1950 | 0.04 | 21 | 0.02 |
| Sex | ||||||
| Missing | 44,135 | 0.88 | 42,697 | 0.87 | 1438 | 1.10 |
| Male | 4,669,989 | 93.05 | 4,542,946 | 92.94 | 127,043 | 97.06 |
| Female | 304,602 | 6.07 | 302,193 | 6.18 | 2409 | 1.84 |
| Residence | ||||||
| Missing | 42 | 0 | 41 | 0.00 | 1 | 0.00 |
| Urban | 3,111,186 | 61.99 | 3,032,657 | 62.05 | 78,529 | 60.00 |
| Rural | 1,907,498 | 38.01 | 1,855,138 | 37.95 | 52,360 | 40.00 |
| Income | ||||||
| Missing | 1,146,131 | 22.84 % | 1,118,548 | 22.29 % | 27,583 | 22.07 % |
| Mean individual (SD) | $27,924 ($20,361) | $28,029 ($20,444) | $24,091 ($16,648) | |||
Veterans resided in 98 % of all US and Puerto Rican census tracts (n = 72,722 of 74,001 total tracts). The majority of veterans (97 %) lived in census tracts that contained more than 20 veterans. There was significant variation in neighborhood characteristics between tracts that were in the lowest decile of NSES compared with those in the highest NSES decile (Table 2). In areas with the lowest NSES index, for example, 30 % of residents had less than a high school education, compared with only 3 % in the highest-decile areas.
Table 2.
Variation in Neighborhood SES (NSES) Characteristics
| Census tract variables | Lowest decile | Highest decile |
|---|---|---|
| Less than high school education, % | 33 % | 3 % |
| Unemployed males, % | 23 % | 5 % |
| Below poverty, % | 38 % | 2 % |
| Receiving public assistance, % | 39 % | 2 % |
| Household headed by female, % | 57 % | 8 % |
| Median household income | $24,113 | $114,015 |
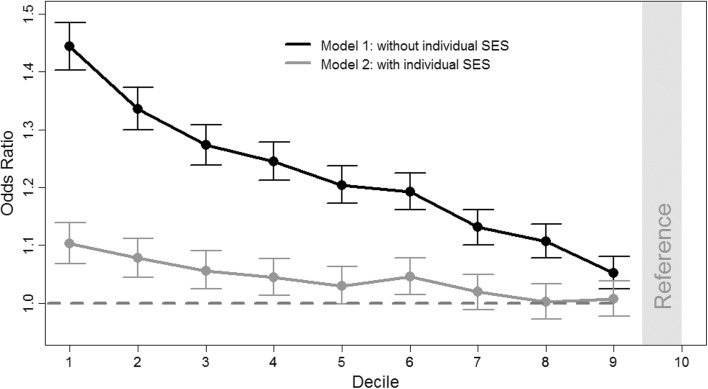
We observed a risk gradient of mortality from the lowest decile of the NSES index to the highest after adjusting for age, gender, comorbidity, race/ethnicity, urban/rural status, and copayment status, as seen in the black curve in Fig. 1 (model 1). The odds of mortality were 44 % (95 % CI 1.40, 1.49) greater for the first (lowest) decile compared to the tenth (highest). The odds then steadily decreased to the ninth decile, where individual mortality was 5 % (95 % CI 1.025, 1.08) more likely to be observed compared to the tenth decile. This association was attenuated after further adjustment for individual-level income and requirement for copayment exemption (displayed by lighter gray curve in Fig. 1). However, veterans living in the four lowest NSES still had significantly higher odds of death than those in the highest NSES decile, with 10 % greater odds of mortality for veterans living in the first decile (OR 1.10, 95 % CI 1.07, 1.14). In a model that included comorbidity status and income, the effect was reduced to 5 % (OR 1.05, 95 % CI 1.02, 1.08). These results were not significantly different for the subset of veterans with address-based geocodes (results not shown). A complete list of odds ratios for all models can be found in the supplementary appendix (Online appendix Tables A1–A4).
Figure 1.
Odds of mortality by neighborhood SES index decile. Model 1, adjusting for age, gender, race/ethnicity, urban/rural (n = 4,813,729). Model 2, adjusting for individual SES (copayment status and household income) and age, gender, race/ethnicity, urban/rural (n = 3,728,655).
The average marginal effects of probability and their associated effects on mortality are presented in Table 3. In the first model, the average marginal effect of being in the first (lowest) decile of NSES was an additional probability of death of 0.006 relative to the tenth (highest) decile. With 479,972 patients at risk in the first decile, this translates into 2961 deaths (95 % CI 2701, 3221) attributed to being in the first decile instead of the tenth. Like the modeled odds ratios, the number of deaths decreased with increasing NSES, and the effect was again attenuated in model 2, where the AME of probability in the first decile was 0.002. For model 1, the cumulative AME on mortality from the first nine NSES deciles was 13,334 (95 % CI 12698, 13964). The cumulative AME for model 2 was 2311 (95 % CI [1759, 2866]) deaths.
Table 3.
Marginal Effect of Neighborhood SES on Probability and Mortality
| Model 1 (n = 4,813,729) | Model 2 (n = 3,728,655) | |||||||
|---|---|---|---|---|---|---|---|---|
| NSES Decile | Population at risk | Probability | Deaths, n (95 % CI) | Deaths, % of total | Population at risk | Probability | Deaths, n (95 % CI) | Deaths, % of total |
| Lowest | 479,972 | 0.0062 | 2961 (2701, 3221) | 2.32 % | 415,618 | 0.00157 | 652 (434, 869) | 0.65 % |
| 2 | 481,302 | 0.0047 | 2256 (2027, 2484) | 1.77 % | 399,537 | 0.00119 | 475 (278, 673) | 0.47 % |
| 3 | 481,642 | 0.0038 | 1837 (1620, 2054) | 1.44 % | 391,838 | 0.00086 | 338 (147, 529) | 0.33 % |
| 4 | 481,482 | 0.0034 | 1648 (1436, 1861) | 1.29 % | 384,010 | 0.00068 | 262 (75, 448) | 0.26 % |
| 5 | 482,174 | 0.0029 | 1375 (1170, 1581) | 1.08 % | 379,118 | 0.00046 | 175 (−7, 358) | 0.17 % |
| 6 | 482,394 | 0.0027 | 1297 (1095, 1499) | 1.02 % | 370,354 | 0.00070 | 259 (81, 437) | 0.26 % |
| 7 | 482,081 | 0.0018 | 886 (693, 1080) | 0.69 % | 363,418 | 0.00029 | 104 (−68, 277) | 0.10 % |
| 8 | 481,305 | 0.0015 | 719 (530, 909) | 0.56 % | 353,836 | 0.00003 | 11 (−156, 177) | 0.01 % |
| 9 | 480,734 | 0.0007 | 354 (172, 536) | 0.28 % | 342,737 | 0.00010 | 35 (−125, 195) | 0.03 % |
| Highest | 480,643 | Reference | 328,189 | Reference | ||||
Model 1, adjusting for age, gender, race/ethnicity, urban/rural; without individual income
Model 2, adjusting for individual SES (income and copayment status), missing income data for n = 1,146,131
From a predictive perspective, C-statistics were 0.740 and 0.748 in models 1 and 2, respectively, and 0.812 and 0.813 in the respective models adjusting for patient comorbidities, suggesting that they have similar power in discriminating between patients who had an event and those who did not (Tables A1–A4 in the online appendix). This suggests that NSES may be a useful parameter for mortality risk adjustment when individual income information is not available—an important result, as individual income data was missing for over one million patients (Table 1).
DISCUSSION
Based on a national population of veterans enrolled in VHA primary care, we found that veterans living in areas of lower NSES had higher mortality than those living in areas of higher NSES, independent of their individual-level demographic and health characteristics. Ours is the largest such study conducted in a US population, and differs from previous studies in our use of a large national multi-racial sample from an enrolled primary care population with extensive sociodemographic and clinical data. These results are consistent with a previous work in a non-national veteran cohort28 and a recent meta-analysis of multi-level studies that found higher mortality for individuals living in areas with low NSES.4 To determine whether area conditions have an effect on mortality distinct from health determinants linked to individual SES, this meta-analysis included only studies that had both individual- and area-level measures of income and SES.4 We observed an attenuating effect on NSES when individual-level income was included in the models, which is consistent with previous literature regarding the detrimental effects of poverty.29
There is a growing awareness among policymakers and health system leaders that improving health outcomes will require not only providing high-quality medical care, but also addressing the social determinants of health. Our work suggests that accounting for contextual and individual-level SES may be needed for appropriate risk adjustment of health outcomes. Without such adjustments, hospitals and health systems with more disadvantaged populations are in danger of being inadequately compensated and inequitably compared with peers. For example, recent studies suggest that safety-net hospitals are being penalized by new Medicare readmission rules that do not include patient-level risk adjustment.30 , 31 These policies are in direct contrast to those of European countries, where area-level deprivation indices are used for resource planning, health care resource allocation, monitoring population health, and health policy development.32 – 34 The VA currently uses risk adjustment in assessing hospital performance and a tiered capitation system, Veterans Equitable Resource Allocation (VERA), for financing. Neither system includes adjustment for the neighborhood of residence of veteran enrollees. However, our results suggest that NSES may be a useful parameter estimate for mortality risk-adjustment scores, especially in cases where individual-level income information is missing.
There are several limitations to our study, including the cross-sectional nature of the analysis and the use of self-reported individual income. We were not able to examine the potential mediators of the relationship between NSES and mortality. We also relied on a single point-in-time estimate for addresses, which might introduce misclassification if veterans moved between census tracts. However, previous studies have shown low rates of residential mobility among older individuals and, for those who do move, high correlations of neighborhood characteristics over time.35 Although the vast majority (86 %) of veterans have house-level geocodes, some veterans were assigned lower-resolution geocodes based on ZIP Codes, mostly among those who live in rural areas. This may have increased variability within our estimates. We included only veterans who received care at the VHA, and our results cannot be generalized to other veterans. The proper identification of neighborhood effects on health is currently a matter of debate, given the self-selection of residents in their neighborhood and unobserved determinants of health that may be correlated with neighborhood choice. However, several studies of the determinants of neighborhood choice suggest that income and education are the most important factors.36 Despite these limitations, the main strengths of our results are the study population, comprising a large, geographically dispersed, diverse national cohort of veterans, and the availability of extensive clinical, demographic, and other data that are often not available in other standard US sources.37
The VA is charged by statute with addressing both medical and non-medical determinants of veterans’ health, and is uniquely positioned to do so, as it provides social services such as housing support, financial support, and education assistance directly to veterans.38 The largest study to date on the directionality of the association between place of residence and health status is the Moving to Opportunity (MTO) program. The goal of MTO was to determine whether families who moved from inner-city, high-poverty areas to low-poverty areas could attain better outcomes, including health-related ones.39 All of the studies based on this experiment have found significant health benefits for moving to less disadvantaged areas.39 – 42 Exploratory analyses of a joint program between the VA and the US Department of Housing and Urban Development (HUD) to house homeless veterans suggest that those who receive services are more likely to be placed in less disadvantaged neighborhoods.43 Further realigning the VA’s considerable resources to address social determinants of health may produce greater gains in health for the veteran population.
Electronic supplementary material
Below is the link to the electronic supplementary material.
(DOCX 19 kb)
(DOCX 20 kb)
(DOCX 19 kb)
(DOCX 20 kb)
(DOCX 17 kb)
ACKNOWLEDGMENTS
This material is based upon work supported by the US Department of Veterans Affairs, VHA Office of Analytics and Business Intelligence. This work was presented at the Society for General Internal Medicine National Meeting (May, 2015) and at Academy Health (June, 2015). The views expressed in this article are those of the authors and do not necessarily represent the views of the Department of Veterans Affairs.
Compliance with Ethical Standards
Conflict of Interest
The authors declare that they do not have a conflict of interest.
Footnotes
Electronic supplementary material
The online version of this article (doi:10.1007/s11606-016-3905-x) contains supplementary material, which is available to authorized users.
REFERENCES
- 1.Koh HK. A 2020 vision for healthy people. N Engl J Med. 2010;362(18):1653–1656. doi: 10.1056/NEJMp1001601. [DOI] [PubMed] [Google Scholar]
- 2.Balfour JL, Kaplan GA. Neighborhood environment and loss of physical function in older adults: evidence from the Alameda County Study. Am J Epidemiol. 2002;155(6):507–515. doi: 10.1093/aje/155.6.507. [DOI] [PubMed] [Google Scholar]
- 3.Do DP, Wang L, Elliott MR. Investigating the relationship between neighborhood poverty and mortality risk: a marginal structural modeling approach. Soc Sci Med. 2013;91:58–66. doi: 10.1016/j.socscimed.2013.03.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Meijer M, Rohl J, Bloomfield K, Grittner U. Do neighborhoods affect individual mortality? A systematic review and meta-analysis of multilevel studies. Soc Sci Med. 2012;74(8):1204–1212. doi: 10.1016/j.socscimed.2011.11.034. [DOI] [PubMed] [Google Scholar]
- 5.Yen IH, Michael YL, Perdue L. Neighborhood environment in studies of health of older adults: a systematic review. Am J Prev Med. 2009;37(5):455–463. doi: 10.1016/j.amepre.2009.06.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bird CE, Seeman T, Escarce JJ, et al. Neighbourhood socioeconomic status and biological ‘wear and tear’ in a nationally representative sample of US adults. J Epidemiol Community Health. 2010;64(10):860–865. doi: 10.1136/jech.2008.084814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Feldman PJ, Steptoe A. How neighborhoods and physical functioning are related: the roles of neighborhood socioeconomic status, perceived neighborhood strain, and individual health risk factors. Ann Behav Med: Publ Soc Behav Med. 2004;27(2):91–99. doi: 10.1207/s15324796abm2702_3. [DOI] [PubMed] [Google Scholar]
- 8.Merkin SS, Basurto-Davila R, Karlamangla A, et al. Neighborhoods and cumulative biological risk profiles by race/ethnicity in a national sample of US adults: NHANES III. Ann Epidemiol. 2009;19(3):194–201. doi: 10.1016/j.annepidem.2008.12.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Brown AF, Ettner SL, Piette J, et al. Socioeconomic position and health among persons with diabetes mellitus: a conceptual framework and review of the literature. Epidemiol Rev. 2004;26:63–77. doi: 10.1093/epirev/mxh002. [DOI] [PubMed] [Google Scholar]
- 10.Rosen AK, Reid R, Broemeling AM, Rakovski CC. Applying a risk-adjustment framework to primary care: can we improve on existing measures? Ann Fam Med. 2003;1(1):44–51. doi: 10.1370/afm.6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Wennberg DE, Sharp SM, Bevan G, Skinner JS, Gottlieb DJ, Wennberg JE. A population health approach to reducing observational intensity bias in health risk adjustment: cross sectional analysis of insurance claims. BMJ. 2014;348:g2392. doi: 10.1136/bmj.g2392. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lushniak BD, Alley DE, Ulin B, Graffunder C. The National Prevention Strategy: leveraging multiple sectors to improve population health. Am J Public Health. 2015;105(2):229–231. doi: 10.2105/AJPH.2014.302257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hoerster KD, Lehavot K, Simpson T, McFall M, Reiber G, Nelson KM. Health and health behavior differences: US Military, veteran, and civilian men. Am J Prev Med. 2012;43(5):483–489. doi: 10.1016/j.amepre.2012.07.029. [DOI] [PubMed] [Google Scholar]
- 14.Nelson KM, Starkebaum GA, Reiber GE. Veterans using and uninsured veterans not using Veterans Affairs (VA) health care. Public Health Rep. 2007;122(1):93–100. doi: 10.1177/003335490712200113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Doubeni CA, Schootman M, Major JM, et al. Health status, neighborhood socioeconomic context, and premature mortality in the United States: The National Institutes of Health-AARP Diet and Health Study. Am J Public Health. 2012;102(4):680–688. doi: 10.2105/AJPH.2011.300158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Anderson RT, Sorlie P, Backlund E, Johnson N, Kaplan GA. Mortality effects of community socioeconomic status. Epidemiology. 1997;8(1):42–47. doi: 10.1097/00001648-199701000-00007. [DOI] [PubMed] [Google Scholar]
- 17.Backlund E, Rowe G, Lynch J, Wolfson MC, Kaplan GA, Sorlie PD. Income inequality and mortality: a multilevel prospective study of 521 248 individuals in 50 US states. Int J Epidemiol. 2007;36(3):590–596. doi: 10.1093/ije/dym012. [DOI] [PubMed] [Google Scholar]
- 18.Sohn MW, Zhang H, Arnold N, et al. Transition to the new race/ethnicity data collection standards in the Department of Veterans Affairs. Popul Health Metrics. 2006;4:7. doi: 10.1186/1478-7954-4-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Gagne JJ, Glynn RJ, Avorn J, Levin R, Schneeweiss S. A combined comorbidity score predicted mortality in elderly patients better than existing scores. J Clin Epidemiol. 2011;64(7):749–759. doi: 10.1016/j.jclinepi.2010.10.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Department of Veterans Affairs, Oct 4, 2016]. Available at: (http://www.va.gov/healthbenefits/resources/priority_groups.asp).
- 21.Phibbs CSCE, Fan AY. Guide to the PSSG Enrollee File. Guidebook. Menlo Park, CA: VA Palo Alto: Health Economics Resource Center; 2015. [Google Scholar]
- 22.US Census Bureau 2015. [accessed Oct 4, 2016]. Available at: https://www.census.gov/programs-surveys/acs/. American Communities Survey.
- 23.O’Campo P. Invited commentary: advancing theory and methods for multilevel models of residential neighborhoods and health. Am J Epidemiol. 2003;157(1):9–13. doi: 10.1093/aje/kwf171. [DOI] [PubMed] [Google Scholar]
- 24.Dubowitz T, Heron M, Bird CE, et al. Neighborhood socioeconomic status and fruit and vegetable intake among whites, blacks, and Mexican Americans in the United States. Am J Clin Nutr. 2008;87(6):1883–1891. doi: 10.1093/ajcn/87.6.1883. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Besag J, York J, Mollié A. Bayesian image restoration, with two applications in spatial statistics. Ann Inst Stat Math. 1991;43:1–20. doi: 10.1007/BF00116466. [DOI] [Google Scholar]
- 26.Rasmussen S. Modelling of discrete spatial variation in epidemiology with SAS using GLIMMIX. Comput Methods Prog Biomed. 2004;76:83–89. doi: 10.1016/j.cmpb.2004.03.003. [DOI] [PubMed] [Google Scholar]
- 27.Karaca-Mandic P, Norton EC, Dowd B. Interaction terms in nonlinear models. Health Serv Res. 2012;47(1 Pt 1):255–274. doi: 10.1111/j.1475-6773.2011.01314.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Nelson K, Taylor L, Lurie N, Escarce J, McFarland L, Fihn SD. Neighborhood environment and health status and mortality among veterans. J Gen Intern Med. 2011;26(8):862–867. doi: 10.1007/s11606-011-1710-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Signorello LB, Cohen SS, Williams DR, Munro HM, Hargreaves MK, Blot WJ. Socioeconomic status, race, and mortality: a prospective cohort study. Am J Public Health. 2014;104(12):e98–e107. doi: 10.2105/AJPH.2014.302156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Barnett ML, Hsu J, McWilliams JM. Patient characteristics and differences in hospital readmission rates. JAMA Intern Med. 2015;175(11):1803–1812. [DOI] [PMC free article] [PubMed]
- 31.Boozary AS, Manchin J, 3rd, Wicker RF. The Medicare Hospital Readmissions Reduction Program: time for reform. JAMA: J Am Med Assoc. 2015;314(4):347–348. doi: 10.1001/jama.2015.6507. [DOI] [PubMed] [Google Scholar]
- 32.Banks J, Marmot M, Oldfield Z, Smith JP. Disease and disadvantage in the United States and in England. JAMA: J Am Med Assoc. 2006;295(17):2037–2045. doi: 10.1001/jama.295.17.2037. [DOI] [PubMed] [Google Scholar]
- 33.Jarman B, Townsend P, Carstairs V. Deprivation indices. BMJ. 1991;303(6801):523. doi: 10.1136/bmj.303.6801.523-a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Sundquist K, Malmstrom M, Johansson SE, Sundquist J. Care need index, a useful tool for the distribution of primary health care resources. J Epidemiol Community Health. 2003;57(5):347–352. doi: 10.1136/jech.57.5.347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Whitsel EA, Rose KM, Wood JL, Henley AC, Liao D, Heiss G. Accuracy and repeatability of commercial geocoding. Am J Epidemiol. 2004;160(10):1023–1029. doi: 10.1093/aje/kwh310. [DOI] [PubMed] [Google Scholar]
- 36.Bayoh I, Irwin EG, Haab T. Determinants of residential location choice: how important are local public goods in attracting homeowners to Central City locations? J Reg Sci. 2006;46(1):97–120. doi: 10.1111/j.0022-4146.2006.00434.x. [DOI] [Google Scholar]
- 37.Krieger N, Chen JT, Waterman PD, Rehkopf DH, Subramanian SV. Painting a truer picture of US socioeconomic and racial/ethnic health inequalities: the Public Health Disparities Geocoding Project. Am J Public Health. 2005;95(2):312–323. doi: 10.2105/AJPH.2003.032482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Garg A, Jack B, Zuckerman B. Addressing the social determinants of health within the patient-centered medical home: lessons from pediatrics. JAMA: J Am Med Assoc. 2013;309(19):2001–2002. doi: 10.1001/jama.2013.1471. [DOI] [PubMed] [Google Scholar]
- 39.Katz LF, Kling JR, Liebman JB. Moving to opportunity in Boston: early results of a randomized mobility experiment. Q J Econ. 2001;116(2):607–654. doi: 10.1162/00335530151144113. [DOI] [Google Scholar]
- 40.Kling JR, Liebman JB, Katz LF. Experimental analysis of neighborhood effects. Econometrica. 2007;75(1):83–119. doi: 10.1111/j.1468-0262.2007.00733.x. [DOI] [Google Scholar]
- 41.Ludwig J, Sanbonmatsu L, Gennetian L, et al. Neighborhoods, obesity, and diabetes--a randomized social experiment. N Engl J Med. 2011;365(16):1509–1519. doi: 10.1056/NEJMsa1103216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Rosenbaum E, Harris LE. Low-income families in their new neighborhoods: the short-term effects of moving from Chicago’s public housing. J Fam Issues. 2001;22(2):183–210. doi: 10.1177/019251301022002004. [DOI] [Google Scholar]
- 43.Patterson KL, Nochajski T, Wu L. Neighborhood outcomes of formally homeless Veterans participating in the HUD-VASH program. J Community Pract. 2014;22(3):324–341. doi: 10.1080/10705422.2014.929605. [DOI] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(DOCX 19 kb)
(DOCX 20 kb)
(DOCX 19 kb)
(DOCX 20 kb)
(DOCX 17 kb)