Abstract
Introduction
Impaction Bone grafting (IBG) in Revision THR is challenging and places demands on allograft stores. Identifying a potential synthetic replacement that works in the longer term was the aim of this study.
Methods
We retrospectively reviewed 21 sequential patients who had undergone revision THR using IBG. They were randomised to receive either combined allograft and synthetic graft or Allograft alone. Among the surviving 15 patients, there were total of 25 procedures were carried out. 15 hips underwent IBG in the acetabulum and 10 hips underwent femoral IBG. Eight patients received a 50/50 mixture of allograft and synthetic Bone graft (Apapore) and seven allograft alone. Bone loss was classified using Paprosky classification. The average follow up was 10 years.
Results
Of the 21 patients, 6 had died of unrelated causes and were excluded. There were 3 re-operations but no revision of the original components. There was no significant implant migration detected. 3 acetabular components had confluent lucent lines in zone-1 which remained stable on long term follow up. 2 patients sustained femoral peri-prosthetic fractures after a simple fall and one patient who developed deep infection treated by DAIR. The modified oxford hip score post-operatively was 18 in allograft group and 22 in Apapore group
Conclusion
Long-term results indicate that the combined use of synthetic graft in Impaction Bone grafting is an effective substitute
Keywords: Impaction bone graft, Apapore, Revision hip arthroplasty
1. Introduction
With an increasing life expectancy in the west from modern healthcare, there will be a greater demand for total hip replacement (THR) surgery. The Recent National Joint Registry reported over 97,000 hip replacements were performed yearly in the United Kingdom.1 This in turn will lead to an increase in the presentation of loosening around these implants or peri-prosthetic fractures. It will create a major challenge for the surgeon when faced with an increasing number of bone deficient acetabulum or femur. A significant amount of bone loss is frequently encountered with revision hip replacement surgery.2 Multiple options are available for impaction bone grafting (IBG) of these defects. Autograft bone harvested from the patient can cause significant morbidity and be of a limited supply. Allograft harvesting of cadaveric femoral head is therefore preferable and commonly performed allowing large volumes of bone graft to be harvested and implanted. This carries the risk of pathogen transmission, increased cost and a time limited shelf life. De Roek et al. have highlighted that a freeze dried allograft has much larger shelf life but requires prolonged rehydration and affects the operation time with different handling properties.3
A Potential solution could be a synthetic bone graft substitute material that would allow a material similar to the bone to be impacted into the defect. IBG of the acetabulum in arthroplasty of the hip was originally described by Hastings and Parker in 1975.4 Subsequently Sloof, Hastings and Parker described the impaction bone grafting using a cemented acetabular component.5, 4 This technique has been replicated in multiple centres.6 Later it also became increasingly popular to use impaction bone grafting with uncemented implants. Pulido et al. highlighted the increasing popularity of using impaction bone grafting with cementless acetabular components.7
With demand out stripping for supply of fresh femoral heads, the search for synthetic alternatives has increased. Since the introduction of calcium sulphate as a bone graft substitute in 1892, there is a continuous drive to improve the material properties of calcium sulphate and development of newer bio-ceramics. Bio-ceramics are neither osteogenic nor osteoinductive, but work by creating an osteoconductive scaffold to promote osteosynthesis.8, 9 Currently, there are four main types of bio-ceramics that are used as bone graft substitutes: calcium phosphate, tricalcium phosphate, calcium sulphate and coralline hydroxyapatite. Composite Bio-ceramics use a combination of these types to provide materials with improved properties. These bone graft substitutes are available in multiple forms ranging from pellets and solid blocks to injectable putty. Apapore is one such synthetic bone graft substitute produced by ApaTech™ and consists of hydroxyapatite. It is shaped similarly to cancellous bone in a trabecular structure providing similar mechanical properties to that of bone.10
2. Materials and methods
We retrospectively reviewed 21 patients who had undergone revision hip arthroplasty using IBG between January 2004 and October 2007. Patients were randomised to receive either plain allograft or a 50:50 mix by volume of Apapore and allograft. Patients over the age of 18 were included in the trial with no upper age limit. Patients that were operated on outside this time period or who had died of unrelated causes during follow up were excluded. The Operation notes and Radiographs were examined to ascertain which methods were used to augment the implants along with the size of bone defect. The demographics and amount of bone loss (classified using the Paprosky classification system) shown in Table 1, Table 2 respectively. The indication for surgery in all cases was aseptic loosening with significant bone loss.
Table 1.
Demographics.
| Groups | Apapore + Allograft | Allograft alone |
|---|---|---|
| No of cases | 8 | 7 |
| No of Procedures. | 14 | 11 |
| Average Age(years) | 72.8 | 71.9 |
| Male | 4 | 3 |
| Female | 4 | 4 |
| Oxford hip score | 22 | 18 |
Table 2.
Paprosky classification of Bone loss.
| Acetabulum Bone loss | Apapore + Allograft | Allograft alone |
|---|---|---|
| 2A | 1 | 4 |
| 3A | 6 | 2 |
| 3B | 1 | 1 |
| Femur Bone loss 3A | 6 | 4 |
There were two trial arms with one population, receiving a 50:50 mixture of allograft and Apapore synthetic bone graft and the other population, receiving only Allograft alone. 15 acetabular revision procedures underwent IBG whilst 10 femoral revisions underwent IBG (Total 25 procedures).
Eight Patients (8 Acetabulum and 6 Femur) received a 50:50 mixture of allograft bone and synthetic bone graft (Apapore) and seven patients (7 acetabulum + 4 femur) allograft alone. Bone loss was classified using the Paprosky classification with the majority being type 3 (Table 2). Among the 15 patients with Acetabular cup fixation, 11 were cemented with mesh containment, one without mesh and three uncemented without mesh. Ten hips had femoral IBG with cemented components and two were bilateral. All bone defects were treated with bone graft impaction using appropriate specially designed tamps (Stryker Exchange system). Two Patients with Paproski type 3 B defects needed mesh and IBG using the Gap II cup cage construct (Styrker).
Fresh Femoral heads from the bone bank were used as the allograft. Apapore 60 (ApaTech Ltd, Elstree, United Kingdom) was the synthetic material which came in a 40 ml pack size with 5–10 mm granule size. It has a 60% porosity and is a phase-pure hydroxyapatite (HA). The combination of the pure-phase HA and porous structure is likely to improve osteoconductivity and encourage the bone ingrowth and remodelling.7, 10., 11 The grafts were mixed with 1 g of vancomycin prior to impaction to reduce the risk of infection. Post-operatively all patients were mobilised with partial weight bearing for 3/12 and progressed to full weight bearing gradually after that. The patients were followed-up both clinically and radiologically at 6 weeks, 6months initially and annually there after. Radiologically assessed for graft incorporation, lucent zones and component migration. More than 2 mm radiological lucency is considered to be significant. Revision of original components for any reason is considered as failure. The outcome measurements included to be an oxford hip score and radiographic analysis.
3. RESULTS (Fig. 1, Fig. 2)
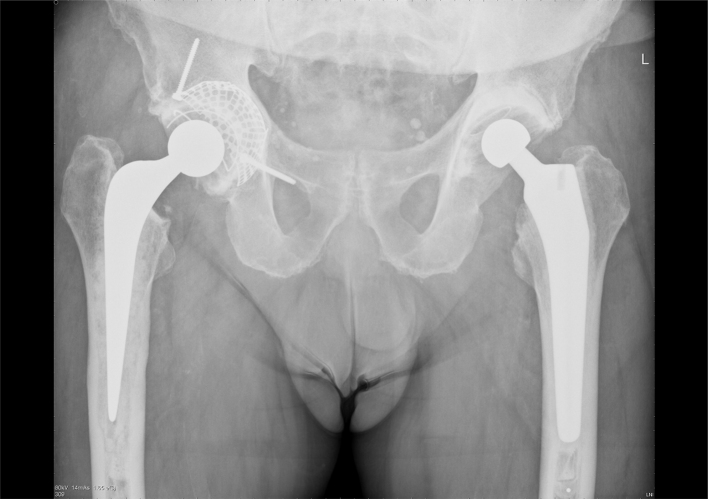
Fig. 1.
AP radiograph showing IBG (Allograft group) of Right femur and Acetabulum –10 year follow up.
Fig. 2.
Radiographs showing AP view of IBG (Apapore group) of left Acetabulum at 9 years follow up.
21 patients were reviewed as part of this study. Six died of unrelated causes during follow up and were excluded from study. Any revision surgery needing replacement of original component is considered to be a failure. Among the surviving 15 patients, there was an even distribution of gender with eight female and seven male patients. The average age at the time of surgery was 72.4 years (60–89). The average follow-up was 10 years (Range 9–11 years).
There were three re-operations and no significant implant migration detected. Three acetabular components had confluent lucent lines which remained stable on long term follow up.
Two patients (13.3%) who had undergone femoral IBG sustained a Vancouver type B1 femoral Peri-prosthetic fracture (PPF) after a simple fall. One patient after 2 years and the other patient, seven years post-operatively. Graft was well incorporated in both of these cases. Both patients were treated with an open reduction and internal fixation (ORIF) along with a strut graft without needing to revise the stem. Fracture union noted in both cases at final follow up both clinically and radiologically.
One patient (6.5%) developed deep infection from haematogenous spread 4yrs after IBG. This infection was identified early and successfully treated with the debridement, antibiotics and implant retention (DAIR). No recurrence of infection at final follow-up.
Three acetabular components (20%) from the Apapore group had confluent lucent lines in zone–1 noted on post-operative radiographs. They remained stable without progression during the follow-up. There were no significant differences noted clinically and radiologically between each group.
The mean modified Oxford hip score post operatively is shown in Table 1 for each group. The mobility at final follow up – seven patients were independent, six patients using a stick and two patients using a frame.
4. Discussion
There is a great deal of literature relating to the clinical outcomes of bone graft substitutes although rather non-specific to the harsh environment of IBG. It is largely comprised of retrospective studies with few randomised controlled trials.
Kurien etal (2013) performed a systematic review on the use of bone graft substitutes in orthopaedic practice. They found that the only bone graft substitutes with Level I evidence were Norian SRS (Synthes), Vitoss (Orthovita), Cortoss (Orthovita), and Alpha-BSM (Etex). They concluded that there is a considerable need for further prospective randomised controlled trials to facilitate an informed decision with regard to the use of current and future bone graft substitutes in clinical practice.12
Slooff et al. (1984) presented a series of 43 hips who underwent the IBG procedure for acetabular protrusion.13 They addressed large defects with a combination of IBG, mesh and protrusion rings. In 1996, he presented the results of 88 hips with acetabular and femoral reconstruction using IBG.5 After a mean follow up of 70 months, four cases of clinical failures (including on infection) and six cases of radiologic failure of the reconstructions were observed, resulting in a failure percentage of 11.4% after 5 years.
Comba et al.,6 presented 142 hips with a follow up between 2 and 13 years with similar results.
Pulido et al. in his review article highlighted that, with improved methods of fixation and revision techniques with availability of trabecular metal cups, there is increasing popularity of using bone graft with cementless acetabular components.7
Various authors have advocated different techniques to improve integration and mechanical stability of the impaction bone graft. Dunlop DG et al. in a laboratory study showed removal of fat and marrow fluid from milled human allograft by washing the graft allows the production of stronger compacted graft that is more resistant to shear, which is the usual mode of failure.14
Whilst Toms et al. demonstrated that bone graft must be contained and sufficiently compacted to provide mechanical stability.15 We used same techniques with special tampons and Exeter exchange system for IBG in our study.
The optimum size of BG chips for impaction is not clear, however, biomechanical studies demonstrate that large bone chips of between 8 mm and 10 mm confer greater stability to an acetabular model with a cemented component than a graft composed of smaller chips IBG.16, 17, 18 In our study we used Apapore 60 with 5–10 mm size. Another biomechanical study19 demonstrated that 50% addition of ApaPore-60 to allograft reduced subsidence and rotation of the stem and will offer better initial stability than allograft alone during femoral impaction grafting.
Schreurs BW et al. in 2004, presented the clinical and radiological results of 62 consecutive acetabular revisions in 58 patients, at a mean of 16.5 years follow-up (15–20 years). They concluded 79% survival at 15 years. In their series, two patients needed revision for sepsis. Seven acetabular reconstructions showed radiolucent lines in one or two zones. They suggested that Acetabular revision using impacted large morsellised bone chips (7 mm to 10 mm) and a cemented cup, is a reliable technique of reconstruction.20
Mc Namara et al., in their retrospective study of 48 patients with 50 consecutive acetabular IBG in primary and revision THA using Apapore 60 as 1:1 mixture, showed clinical survival of 100% at 5 years follow up. However radiologically 10 hips (20%) showed radiolucent lines and two hips showed acetabular migration.21 Our results and complication rates are very similar to the above studies from the literature.
The main strength of our study is the longer term follow-up of randomised patients. It is a comparison study of homogenous patient group between the use of allograft and a mixture of Apapore and allograft. It is a single surgeon series and is the largest comparison case series of patients with allograft versus Apapore mixture in revision arthroplasty. The limitations of this study is the small population size
5. Conclusion
We conclude from our study that, Apapore remains a viable option for the use of impaction bone grafting in revision arthroplasty. It is potentially a safer option due to the reduced requirement for donor allograft bone and produces comparable results to allograft alone. Although it is a small sample, the long term results indicate that it is an effective substitute for allograft graft alone.
References
- 1.2016. National Joint Registry for England and Wales; Annual Report.www.njrcentre.org.uk [(date accessed 15]February 2016) [Google Scholar]
- 2.Pitto R., Muria G., Hohmannet D. Impaction grafting and acetabular reinforcement in revision hip replacement. Int Orthop. 1998;22(3):161–164. doi: 10.1007/s002640050232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.De Roeck N., Drabu K. Impaction bone grafting using freeze- dried allograft in revision hip arthroplasty. J Arthroplasty. 2001;16(2):201–206. doi: 10.1054/arth.2001.20250. [DOI] [PubMed] [Google Scholar]
- 4.Hastings D., Parker S. Protrusio acetabuli in rheumatoid arthritisi. Clin Orthop Relat Res. 1975;108:76–83. doi: 10.1097/00003086-197505000-00012. [DOI] [PubMed] [Google Scholar]
- 5.Slooff T.J., Buma P., Schreurs B.W. Acetabular and femoral reconstruction with impacted graft and cement. Clin Orthop Related Res. 1996;324:108–115. doi: 10.1097/00003086-199603000-00013. [DOI] [PubMed] [Google Scholar]
- 6.Coomba F., Buttaro M., Pusso R., Piccaluga F. Acetabular reconstruction with impacted bone allografts and cemented acetabular components: a 2 to 13 year follow up study of 142 aseptic revisions. J Bone Joint Surg (Br) 2006;88-B:865–869. doi: 10.1302/0301-620X.88B7.17227. [DOI] [PubMed] [Google Scholar]
- 7.Pulido L., Rachala S.R., Cabanela M.E. Cementless acetabular revision:Past, present, future: Revision Total Arthropalsty: the acetabular side using cementless implants. Int Orthop. 2011;35:289–298. doi: 10.1007/s00264-010-1198-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Fillingham Y., Jacobs J. Bone grafts and their substitutes. Bone Joint J. 2016;98-B:6–9. doi: 10.1302/0301-620X.98B.36350. [1 Sul A] [DOI] [PubMed] [Google Scholar]
- 9.Whitehouse M., Dacombe P., Webb J., Blom A. Impaction grafting of the acetabulum with ceramic bone graft substitute mixed with femoral head allograft: survivorship in 43 patients with a median follow up of 7 years. J Acta Orthop. 2013;84(4):365–370. doi: 10.3109/17453674.2013.792031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Properties of Apapore. http://www.bio-medicine.org/medicine-products/ApaPore-Hydroxyapatite-Bone-Graft-Substitute, Accessed 29 December 2015.
- 11.Schreurs B.W., Bolder S., Gardeniers J.N., Verdonschot T.J.J.H., Slooff R.P.H. Vet Acetabular revision with impacted morsellised cancellous bone grafting and a cemented cup A 15- To 20-year follow up. Bone Joint J. 2004;86(4) [PubMed] [Google Scholar]
- 12.Kurien T., Pearson R.G., Scammell B.E. Bone graft substitutes currently available in orthopaedic practice: the evidence for their use. Bone Joint J. 2013;95-B(May (5)):583–597. doi: 10.1302/0301-620X.95B5.30286. [DOI] [PubMed] [Google Scholar]
- 13.Slooff T.J., Huiskes R., van Horn J., Lemmens A.J. Bone grafting in total hip replacement for acetabular protrusion. Acta Orthop Scand. 1984;55(December (6)):593–596. doi: 10.3109/17453678408992402. [DOI] [PubMed] [Google Scholar]
- 14.Dunlop D.G., Brewster N.T., Madabhushi S.P., Usmani A.S., Pankaj P., Howie C.R. Techniques to improve the shear strength of impacted bone graft: the effect of particle size and washing of the graft. J Bone Joint Surg Am. 2003;85-A(April (4)):639–646. doi: 10.2106/00004623-200304000-00009. [DOI] [PubMed] [Google Scholar]
- 15.Toms A., Barker R., Jones R., Kuiper J. Impaction bone grafting in revision joint replacement surgery, The journal of bone and joint surgery. Am Vol. 2004;86(September (9)):2050–2060. doi: 10.2106/00004623-200409000-00028. [DOI] [PubMed] [Google Scholar]
- 16.Bolder S., Schreurs B., Verdonschot N. Particle size of bone graft and method of impaction affect initial stability of cemented cups: human cadaveric and synthetic pelvic specimen studies. Acta Orthop Scand. 2003;74:652–657. doi: 10.1080/00016470310018144. [DOI] [PubMed] [Google Scholar]
- 17.Bolder S., Verdoschot N., Schreurs B. Technical factors affecting cup stability in impaction bone grafting. Proc Inst Mech Eng H. 2007;221:81–86. doi: 10.1243/09544119JEIM245. [DOI] [PubMed] [Google Scholar]
- 18.Ullmark G. Bigger size and defatting of bone chips will increase cup stability. Arch Orthop Trauma Surg. 2000;120:445–447. doi: 10.1007/s004029900122. [DOI] [PubMed] [Google Scholar]
- 19.Phipps K.L., Pegrum J., Smith N., Blunn G. Mechanical testing of apapore-60 as a bone graft extender in a femoral model. 50th Annual Meeting of the Orthopaedic Research Society Poster No: 1049. 2017 [Google Scholar]
- 20.Schreurs B.W., Bolder S., Gardeniers J.N., Verdonschot T.J.J.H., Slooff R.P.H. Vet Acetabular revision with impacted morsellised cancellous bone grafting and a cemented cup A 15- To 20-year follow up. Bone Joint J. 2004;86(4) [PubMed] [Google Scholar]
- 21.McNamara S., Deshpande S., Porteus M. Impaction grafting of the acetabulum with a mixture of frozen, ground irradiated bone graft and porous synthetic bone substitute (Apapore 60) J Bone Joint Surg Br. 2010;92(5):617–623. doi: 10.1302/0301-620X.92B5.23044. [DOI] [PubMed] [Google Scholar]