Abstract
Introduction:
Peptic ulcer perforation (PPU) is a common surgical emergency and the mortality rate ranges 10% to 40%, especially in elderly patients. Laparoscopic repair achieved encouraging results.
Materials and Methods:
We enrolled patients performing surgical repair for PPU from January 2007 to December 2015 in our surgical unit. The aim of this retrospective observational study was to compare the results of PPU laparoscopic repair with open technique. The following characteristics of patients were evaluated: age, sex and American Society of Anesthesiologists classification. The site and the diameter of perforation were recorded: gastric, pyloric, duodenal, and the location on the anterior or posterior wall.
Results:
In total, 59 patients (39 males and 20 females) with a mean age of 58.85 years (±SD) were treated surgically. Laparoscopic repair was accomplished in 21 patients. The mean operative time for laparoscopic repair was 72 minutes (±SD), significantly shorter than open repair time (180 min ±SD). The results demonstrated that laparoscopic repair is associated with a shorter operative time, reduced postoperative pain (4.75 vs. 6.42) and analgesic requirements, a shorter hospital stay (7.5 vs. 13.1), and earlier return to normal daily activities.
Discussion:
Laparoscopic surgery minimizes postoperative wound pain and encourages early mobilization and return to normal daily activities. The benefit of early discharge and return to work may outweigh the consumable cost incurred in the execution of laparoscopic procedures.
Conclusions:
Complications in both procedures are similar but laparoscopic procedure shows economic advantages for reducing postoperative hospital stay, postoperative pain, and for a good integrity of abdominal wall.
Key Words: peptic ulcer perforation, laparoscopic repair, omental patch
Peptic ulcer (PU) is a quite common disease and has a multifactorial etiology.1 Complications such as acute hemorrhage or perforation happen in a significant portion of patients. Peptic ulcer perforation (PPU) is a common surgical emergency and the mortality rate ranges 10% to 40%, especially in elderly patients.2,3
The management of PPU is immediate surgery and the development of laparoscopy has improved its treatment.2
Laparoscopic surgery in abdominal emergencies has shown good results in terms of feasibility for cholecystectomy and appendectomy and achieved encouraging results also in PPU repair. In fact, laparoscopic repair ensures the identification of the site and the pathology of the perforation and allows closure of the perforation and peritoneal lavage, just like the open repair does but without a large abdominal incision.3,4
MATERIALS AND METHODS
In this retrospective observational study we reviewed all patients who underwent surgical repair for perforated peptic ulcer from January 2007 to December 2015 in our surgical unit.
The aim of the study was to compare the results of PPU laparoscopic repair with open technique.
The following characteristics of patients were evaluated: age, sex, and American Society of Anesthesiologists (ASA) classification. The site and the diameter of perforation were recorded: gastric, pyloric, duodenal, and the location on the anterior or posterior wall.
The primary endpoints were operative morbidity and mortality at 30 days. The secondary endpoints were the operative time, the analgesic requirement, length of postoperative hospital stay, return to normal daily activities. The interval between hospital admission and surgery has been also taken into account. All patients started a postoperative follow-up.
All patients were diagnosed with perforated ulcer clinically and using x-ray and computed tomographic scan. No patient was excluded even when there were signs of peritonitis or sepsis. The site of perforation was evaluated: anterior gastric or pyloric or duodenal peptic ulcer. All patients received intravenous fluids, nasogastric catheter decompression, and parenteral analgesics before surgery.
Intravenous cefazolin and metronidazole was administered before surgery, and thereafter every 12 hours; surgery was performed as soon as the operating room was ready. Each surgical treatment was performed only after the patient’s consent.
All open repairs were performed according to standard techniques,5,6 by using an upper midline incision. After identification of the site of the perforation, a piece of omentum was encircled on a full-thickness polygalactin (Vicryl) suture placed on both sides of perforation and sutures were tied. This procedure was followed by peritoneal toilet.
Also laparoscopic approaches were performed according to standard techniques.7 Laparoscopic repair was performed by a 3 surgeons team (1 consultant, 1 senior registrar, and 1 registrar), well experienced in laparoscopy. Reverse Trendelenburg position was used. The operating surgeon stood between the patient’s thighs. Open laparoscopy was used for insertion of the 10-mm umbilical port and a 30-degree laparoscope was introduced. Two more ports were inserted plane at the midclavicular line on both sides. At first, there was the exploration of the peritoneal cavity and then the search for the pyloroduodenal region. If the omentum was attached to the suspected perforation site, it was pulled away to evaluate the underlying pathology. The compression of the antrum and of the first duodenum was helpful to find out the PPU because of fluid and bubbles coming from the perforations and also the inflation of the stomach with air or saline solution to facilitate the identification of the perforation. The size of the perforation was measured using the jaws of the grasper.
A 10-mm perforation was defined as the cutoff point for a larger perforation, for which laparoscopic patch repair may not be the right surgical procedure.
Two 3-0 Vicryl sutures on curved needle were used to repair the perforation site using the omentum. The first suture was passed through the full duodenal wall and the omentum and knotted with 4 ties. The second one was passed through the seromuscular part of the duodenal wall and a piece of omentum.
A single 3-0 Vicryl stitch was longitudinally applied with a good bite of healthy tissue in the middle of the perforations. The ulcer edges were knotted, with 3 knots: 2 half knots forming a square and a third and reverse half one. The same stitch was then anchored to the omental patch over the repaired site. At the end of the procedure a hydropneumatic test was made to assess the effectiveness of the repair. Before closure, peritoneal lavage was performed with aspiration of fluids and a drain eventually inserted.
All patients started postoperative follow-up and were controlled at 5 and 7 years after the surgery and until 2012 any laparoscopic patient showed any adhesion, whereas 5 patients with open repair had abdominal pain because of constipation treated pharmacologically.
RESULTS
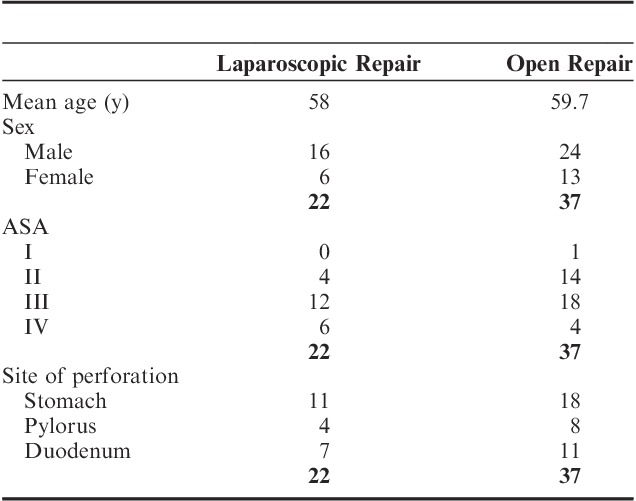
From January 2007 to December 2015, 59 patients (39 males and 20 females) with a mean age of 58.85 years (±SD) with a preoperative diagnosis of perforated peptic ulcer were identified and treated surgically. Written informed consent was obtained from all patients. Ethical standards were followed, in fact Institutional Research Board approval was obtained. Only 1 patient (1.7%) was classified as ASA I, whereas 18 were ASA II (30.5%), 30 ASA III (50.85%), and 10 ASA IV (17%). In total, 22 procedures were performed laparoscopically (37.29%) and 37 with traditional laparotomy (62.71%). Patients demographics are shown in Table 1: age range, sex distribution, and ASA status were similar in both groups. The sites and sizes of ulcer perforations were comparable in both groups.
TABLE 1.
Patients Demographics 2007-2015
Laparoscopic repair was accomplished in 22 patients; there was 1 conversion in the laparoscopic group due to unidentifiable perforation with an overall success rate of 95.5%.
The mean operative time for laparoscopic repair was 72 minutes (±SD), significantly shorter than open repair time (180 min ±SD). The mean postoperative stay was shorter for laparoscopic group (mean, 7.5 d) than the open one (mean, 13.1 d) as well as the average of drainage stay, that was 6.4 days versus 9.33 days. Only 2 patients form the laparoscopic group had postoperative vomiting. The average of nasogastric tube duration was the same in both groups (6.25 vs. 6.44 d), whereas Foley catheter had been maintained for longer time in the open group (8.09 vs. 5.45 d). The mean time to canalization for the open group is 3.54 days, compared with 2.8 days for the laparoscopic one.
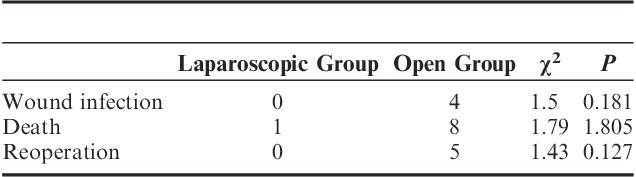
Patients who underwent laparoscopic repair required significantly less parenteral analgesics than the open group. Paracetamol dosage in postoperative laparoscopic group was 1000 mg twice a day, whereas in the open group it was associated to opioids as tramadol or morphine. Analgesic postoperative time was longer for the open group (6.42 d) than for the laparoscopic one (4.75 d). Mortality was definitely higher in the open group (8 patients) then in laparoscopic one (1 patient). Nine patients died with an overall mortality of 15.2%; only 1 death occurred in laparoscopic group (4.5%) compared with 8 deaths observed in the open group (21.6%): the difference does not reach statistical significance (P=0.18055; χ2 test=1.79). Causes of death were led to 1 case of chest infection for laparoscopic group and 2 chest infections, 4 multiorgan failures, and 2 acute respiratory distress syndromes for open group.
Only 4 patients of open group had wound infections. A second surgical treatment was required in 13 patients: 4 in laparoscopic group (18.18%) and 9 in open group (24.32%). Reoperations were necessary because of 3 cases of leakages and 1 case of bleeding for what concerns laparoscopic group; while for what concerns the open one, 2 cases of wound dehiscence, 3 bleedings and 4 leakages: this difference does not reach statistical significance (P=0.127; χ2 test=1.43).
A comparison of various results for the 2 groups is shown in Tables 2, 3.
TABLE 2.
Results
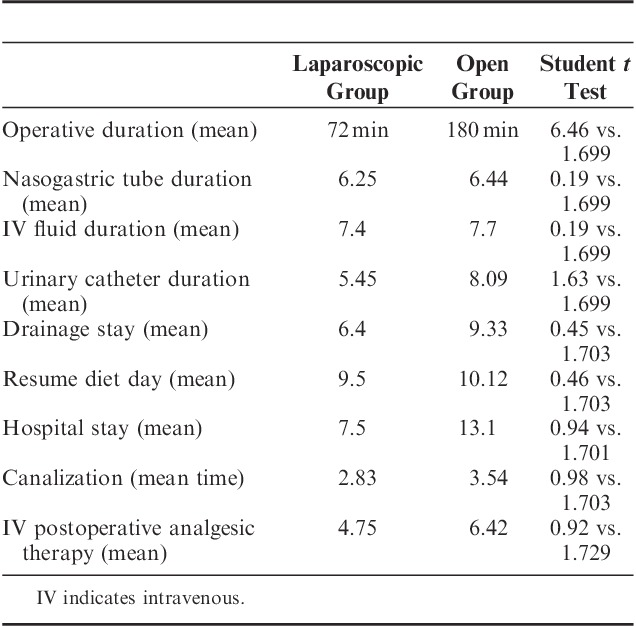
TABLE 3.
Death and Complications
DISCUSSION
Advances in the medical treatment of peptic ulcer disease have led to a dramatic decrease in the number of elective ulcer surgeries performed. Nonetheless, the number of patients requiring surgical intervention for complications such as perforations remains relatively unchanged.8–10 Minimal-access surgery has assumed an ever-expanding role in gastrointestinal surgery since the introduction of laparoscopic cholecystectomy.
When the access trauma of a midline laparotomy is relatively large compared with the procedural trauma of patch repair for perforated peptic ulcer, the benefit of minimal-access laparoscopic surgery increases.
Laparoscopic approach is beneficial for low-risk patients in particular. A recent Cochrane report concludes that data from laparoscopic surgery are not clinically different from those of open surgery.11
We had only 1 patient who needed to be converted to open technique because of technical difficulties in approaching the perforation site laparoscopically. Usually the most common reason for conversion was size of perforation, but by using an omental patch this might not necessarily be a reason to convert anymore. The best parameters to compare 2 different surgical techniques are morbidity and mortality. PPU is still associated with high morbidity and mortality, main problems being wound infection, sepsis, leakage at the repair site, and pulmonary problems.
Many studies showed significant reduction in pain, mortality, morbidity, wound infection, resuming normal diet, and hospital stay with the laparoscopic approach.
This led to the assumption that laparoscopic surgery might be dangerous in patients with prolonged peritonitis.
The results of our retrospective study showed that, comparing with open repair, laparoscopic repair is associated with a shorter operative time (videolaparoscopy group, 72 min; open group, 180 min), reduced postoperative pain (4.74 vs. 6.16) and analgesic requirements, a shorter hospital stay (7.5 vs. 13.1), and earlier return to normal daily activities. According to our statistical analysis (Student t test) it has been demonstrated that laparoscopy provides a shorter surgical time with statistical significance (6.46 vs. 1.699).
The complication rate for laparoscopic repair was low; laparoscopic procedure was associated with fewer chest infections and potentially less wound infection compared with open repair. For what concerns mortality, wound infection, and reoperations, our experience did not show statistical difference between both groups.
Laparoscopic surgery minimizes postoperative wound pain and encourages early mobilization and return to normal daily activities. The benefit of early discharge and early return to work may outweigh the consumable cost incurred in laparoscopic procedures.
CONCLUSIONS
According to our experience, complications in both procedures are similar but laparoscopic procedure shows economic advantages for reducing postoperative hospital stay, postoperative pain, and for a good integrity of abdominal wall.
Footnotes
The authors declare no conflicts of interest.
REFERENCES
- 1.Yeomans ND. Overview of 50 years’ progress in upper gastrointestinal diseases. J Gastroenterol Hepatol. 2009;24(suppl 3):S2–S4. [DOI] [PubMed] [Google Scholar]
- 2.Malfertheiner P, Chan FK, McColl KE. Peptic ulcer disease. Lancet. 2009;374:1449–1461. [DOI] [PubMed] [Google Scholar]
- 3.Bertleff MJ, Lange JF. Perforated peptic ulcer disease: a review of history and treatment. Dig Surg. 2010;27:161–169. [DOI] [PubMed] [Google Scholar]
- 4.Svanes C. Trends in perforated peptic ulcer: incidence, etiology, treatment, and prognosis. World J Surg. 2000;24:277–283. [DOI] [PubMed] [Google Scholar]
- 5.Møller MH, Adamsen S, Wojdemann M, et al. Perforated peptic ulcer: how to improve outcome? Scand J Gastroenterol. 2009;44:15–22. [DOI] [PubMed] [Google Scholar]
- 6.Kirk RM. Stomach and Duodenum, 3rd ed London: Churchill Livingstone; 1994:190–192. [Google Scholar]
- 7.Siu WT, Leong HT, Law BKB, et al. Laparoscopic repair for perforated peptic ulcer: a randomized trial. Ann Surg. 2002;235:313–319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Koo J, Ngan YK, Lam SK. Trends in hospital admissions, perforation and mortality of peptic ulcer in Hong Kong from 1970 to 1980. Gastroenterology. 1983;84:1558–1562. [PubMed] [Google Scholar]
- 9.Gunshefski L, Flancbaum L, Brolin RE, et al. Changing patterns in perforated peptic ulcer disease. Am Surg. 1990;56:270–274. [PubMed] [Google Scholar]
- 10.Kulber DA, Hartunian S, Schiller D, et al. The current spectrum of peptic ulcer disease in the older age groups. Am Surg. 1990;56:737–741. [PubMed] [Google Scholar]
- 11.Sanabria AE, Morales CH, Villegas MI. Laparoscopic repair for perforated peptic ulcer disease. Cochrane Database Syst Rev. 2005;4:CD004778. [DOI] [PubMed] [Google Scholar]


