Abstract
Previous studies have demonstrated the potential for using smartwatches with a built-in accelerometer as feedback devices for high-quality chest compression during cardiopulmonary resuscitation. However, to the best of our knowledge, no previous study has reported the effects of this feedback on chest compressions in action. A randomized, parallel controlled study of 40 senior medical students was conducted to examine the effect of chest compression feedback via a smartwatch during cardiopulmonary resuscitation of manikins. A feedback application was developed for the smartwatch, in which visual feedback was provided for chest compression depth and rate. Vibrations from smartwatch were used to indicate the chest compression rate. The participants were randomly allocated to the intervention and control groups, and they performed chest compressions on manikins for 2 min continuously with or without feedback, respectively. The proportion of accurate chest compression depth (≥5 cm and ≤6 cm) was assessed as the primary outcome, and the chest compression depth, chest compression rate, and the proportion of complete chest decompression (≤1 cm of residual leaning) were recorded as secondary outcomes. The proportion of accurate chest compression depth in the intervention group was significantly higher than that in the control group (64.6±7.8% versus 43.1±28.3%; p = 0.02). The mean compression depth and rate and the proportion of complete chest decompressions did not differ significantly between the two groups (all p>0.05). Cardiopulmonary resuscitation-related feedback via a smartwatch could provide assistance with respect to the ideal range of chest compression depth, and this can easily be applied to patients with out-of-hospital arrest by rescuers who wear smartwatches.
Introduction
The new 2015 American Heart Association (AHA) guidelines recommend rescuers to perform compressions to a depth of 5–6 cm and at a rate of 100–120 counts/min; this is in contrast to the previous guidelines, which recommended a depth of at least 5 cm and a rate of 100 counts/min [1, 2]. This range of chest compression (CC) depth is sufficient to achieve an effective outcome without the development of complications, including fracture of the ribs, pneumothorax, and hemothorax, which are associated with a compression depth of >6 cm [3–5]. In addition, compressions at a rate of >120 compressions/min might have result in poor coronary perfusion and low cardiac output by reducing the diastolic filling time [6]. It is often challenging for rescuers to reach the recommended range of CC depth during cardiopulmonary resuscitation (CPR). CPR skills can be improved by regular training [7]; however, rescuers cannot be expected to retain CPR skills after a certain period of time owing to a decline in learning effects [8–10]. A CPR feedback system that provides accurate information in real-time could overcome this problem in real-life situations involving cardiac arrest.
In previous studies, various feedback devices with a built-in accelerometer and pressure sensor could provide data regarding the CC depth, rate, and intensity [11–19]. Rescuers who performed CC with auditory-visual feedback devices were found to have improved individual CPR performances [11–13, 17, 19]. Recently, feedback systems involving a smartphone with a built-in accelerometer have been developed [20, 21]. Such devices provide auditory-visual information to the rescuer via a speaker and screen on the device. Smartwatches as the newest wearable smart device also have a built-in accelerometer and could be useful as a CPR feedback device. In our previous study, we verified and reported an algorithm of compression depth estimation using a smartwatch, and developed a smartwatch application that was able to provide visual information on CC depth and rate in real-time [22].
Although a previous study reported on the potential use of smartwatches with built-in accelerometers as feedback devices for high-quality CC [22], no study has reported the effect of this feedback on CC during CPR. We hypothesized that the CPR feedback system of a smartwatch might improve the parameters of CC performed by rescuers who have received CPR training.
Materials and methods
Design
We designed a prospective, randomized controlled parallel study to evaluate the ability of a feedback application on a smartwatch to improve the quality of CC administered during simulated cardiac arrest. The study was performed at Hanyang University’s Simulation Center (Seoul, Republic of Korea) in April 2016. The study was approved by the Institutional Review Board of the Hanyang University Hospital (HYUH201512024001-HE002), and the study protocol was registered in the Clinical Research Information Service (cris.nih.go.kr: KCT0001799).
Participants
Forty medical students from Hanyang University participated voluntarily in this study. The inclusion criteria were healthy individuals aged >18 years. Volunteers were excluded if they had wrist, spine, or pulmonary/heart diseases. Two certified Basic Life Support instructors taught all participants the high-quality curriculum of Basic Life Support, for a total of 4 hours in 2 weeks. The participants received information related to this study before the experiments. All participants provided their written informed consent.
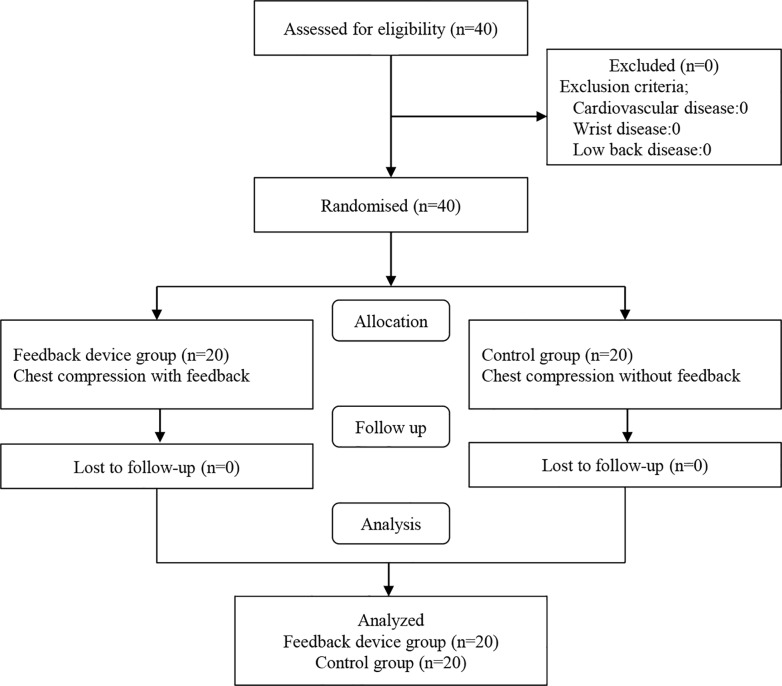
A pilot study was conducted to detect a difference in the proportion of CC depth (≥5 cm and ≤6 cm) between the smartwatch feedback group and the control group. The proportion (mean±SD) of accurate CC depth was 96.8±3.2% and 69.8±30.2%, respectively. G-power 3.1.2® (Heine Heinrich University, Düsseldorf, German) was used to calculate a required sample size of 18 participants per group with an effect size of 1.25, α-error of 0.05, and power of 0.95. We aimed to recruit 40 participants to account for a possible drop-out rate of 10% (Fig 1).
Fig 1. A flowchart showing participant enrolment.
Equipment and materials
The present study used a CPR training manikin (SkillReporter™; Laerdal, Stavanger, Norway) and the manikin’s recording programme via a laptop for simulation. The manikin could estimate several parameters, including CC depth, rate, and relaxation depth via a sensor when participants compressed the middle part of the manikin’s chest. As a feedback device, a smartwatch (Galaxy Gear Live; Samsung Electronics, Seoul, Republic of Korea) was used to implement the application [22]. The experiment was performed on a flat and firm surface to avoid the mattress effect, which absorbs some of the force of the CC.
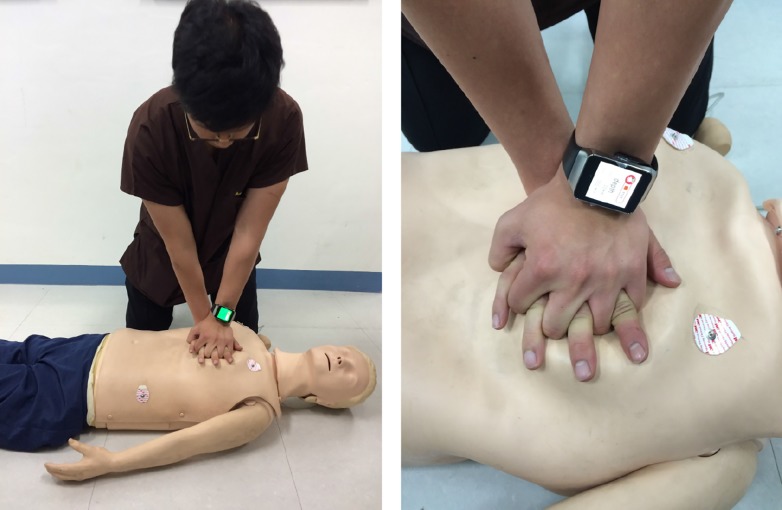
The participants performed CC on a manikin while wearing a smartwatch, during which the display of the device showed three different colors as visual feedback (Fig 2). A blue color was shown on the display when the CC depth was >6 cm, whereas a red color was shown when the CC depth was <5 cm. A green color was shown when the range of the CC depth was between 5 and 6 cm (Fig 3). In addition, regular vibrations generated by the smartwatch at a rate of 110/min were used to guide the CC rate.
Fig 2. Chest compressions using a smartwatch-based feedback system.
Participants, in a kneeling position adjacent to a manikin, compressed the chest of the manikin placed on a flat and firm surface. The smartwatch provided visual feedback and vibratory guidance regarding the chest compression depth and rate, respectively.
Fig 3. Visual feedback was given in the form of different colors according to the chest compression depth.
(A) The color shown on the display of the smartwatch was red when the depth was <5 cm, (B) green, when the depth was between 5 and 6 cm, and (C) blue, when the depth was >6 cm.
Intervention
All participants were allocated in a 1:1 ratio randomly into two groups: intervention (n = 20) and control (n = 20) groups. Randomization was performed using a sequence generator (http://www.random.org/). All participants in the two groups performed CC continuously without artificial breathing in the kneeling position beside the manikin for 2 min (Fig 2). In the intervention group, participants initiated CC wearing the smartwatch, which was running the feedback program. Conversely, the participants of the control group performed CC without the aid of a feedback device. A partition was placed on the floor between investigators and a participant so that the investigators could not recognize the participants’ group during the experiment. Participant characteristics, such as age, weight, CPR education frequency, and experience of a real-life CPR situation, were evaluated. Data were downloaded and collected directly from the manikin’s recording system by one author who was blinded to the participants’ group allocation.
Primary and secondary outcomes
In this study, the primary outcome was the proportion of accurate CC depth that was defined as the ratio of the number of CC whose depth was between 5 and 6 cm to the total number of CC in 2 min. In addition, CC depth and rate, and the proportion of complete chest decompression were investigated as secondary outcomes. The proportion of complete chest decompression was defined as the ratio of the number of decompressions whose recoil depth was <1 cm to the total number of decompressions in 2 min.
Statistical analyses
The data were compiled using a standard spreadsheet application (Excel 2016; Microsoft, Redmond, WA, USA) and were analyzed using the Statistical Package for the Social Sciences (SPSS), version 21.0 KO for Windows (SPSS Inc., Chicago, IL, USA). The Kolmogorov-Smirnov tests were performed for normality of all dataset. Descriptive statistics were used to describe the baseline characteristics of the study participants and to present categorical variables as frequencies and percentages. Normally distributed data are presented as the mean±SD with 95% confidence intervals (CI), whereas non-normally distributed data are presented as medians with interquartile ranges (IQR) with 95% CI. Student’s t-tests and Mann-Whitney U-tests were used for comparisons of continuous variables, and Chi-square or Fisher’s exact test, for categorical variables. Analysis of covariance (ANCOVA) was performed to adjust for influencing factors [23]. A p-value of <0.05 was considered statistically significant.
Results
A total of 40 participants were recruited in this study; there were no exclusions (Fig 1). The baseline characteristics of the participants are summarized in Table 1. The proportion of accurate CC depth (mean±SD) for the intervention and control groups was 64.6±7.8% and 43.1±28.3%, respectively (p = 0.02). There were no significant differences in the CC depth, CC rate, and proportion of complete chest decompression (Table 2).
Table 1. Characteristics of the intervention and control participants.
| Intervention group (n = 20) | Control group (n = 20) | P-valuea | |
|---|---|---|---|
| Age; years | 19 [18–24] | 19 [18–19] | 0.398 |
| Male | 19 (95%) | 15 (75%) | 0.182 |
| Height; cm | 174.1±6.8 | 171.3±5.5 | 0.168 |
| Weight; kg | 69.2±9.6 | 64.1±9.0 | 0.090 |
| Body mass index | 22.9±3.2 | 21.8±2.6 | 0.250 |
| Number of CPR training | 2 [1–3] | 2 [1–4] | 0.221 |
| Performance CPR in real world | 0 [0–0] | 0 [0–0] | - |
Values are mean (SD), median [IQR] or number (proportion).
ap-value <0.05 is significant.
Table 2. Quality of CC performed by the intervention and control group participants.
| Intervention group (n = 20) | Control group (n = 20) | P-valuea | P-valuea ANCOVA | |
|---|---|---|---|---|
| Proportion of accurate CC depth; % | 64.6±7.8 | 43.1±28.3 | 0.020 | 0.049 |
| CC rate; counts/min | 115.5±8.2 | 115.2±12.1 | 0.915 | 0.555 |
| CC depth; mm | 53.1±4.1 | 51.1±7.7 | 0.310 | 0.927 |
| Proportion of complete chest decompression; % | 100.0 (99.3–100.0) | 100.0 (99.5–100.0) | 0.366 | N/A |
Values are mean (SD), median [IQR], or number (proportion), and tested by the independent t-test or Mann-Whitney test. ANCOVA included age, sex, and body mass index as covariates. Proportion of accurate CC depth was defined as the ratio of the number of CC whose depth was between 5 and 6 cm to the total compression number for 2 min. Proportion of complete chest decompression was defined as the ratio of the number of CC whose recoil depth was <1 cm to the total decompression number for 2 min.
CC, chest compression; ANCOVA, analysis of covariance, N/A, not applicable
ap-value <0.05 is significant.
We performed ANCOVA to adjust for factors such as sex, age, and, body mass index in order to investigate the main factors influencing the outcomes (Table 2). The only independent factor affecting the proportion of accurate CC depth was feedback (p = 0.05). There were no significant differences in CC depth and rate between the intervention and control groups.
Additionally, CC depth was affected by sex (p = 0.02), regardless of the intervention. There was no significant influencing factor for the CC rate.
Discussion
High-quality CPR, including the maintenance of accurate depth and rate, is major requisite for improving the survival rates of cardiac arrest patients [1, 19, 24–26]. Various studies on CPR feedback devices have shown that feedback improves the CC depth and/or rate in both novice and/or trained participants [11–13, 16–18, 27]. In this simulation study with trained participants, we have shown that the use of a feedback system using a smartwatch does not improve the mean CC depth and decompression, but it improves the proportion of accurate CC depth. Thus, a smartwatch may be a good device for providing feedback while performing CC and ensuring an accurate range of depth without any complications during CPR.
There was no significant difference in the mean CC rate between the two groups. The participants received feedback regarding the CC rate by the vibration from the smartwatch instead of an auditory signal. It might have been difficult for them to perceive the vibration because of the CC motion. Hence, it is unlikely that feedback regarding the CC rate in the form of vibrations would be as effective as auditory feedback. In further studies, we will investigate whether vibration intensity affects the ability to recognize a vibration.
Several studies have reported that female rescuers with a low body weight might find CC challenging and that physical differences between male and female rescuers might affect the CC depth [28–31]. In this study, there was a significant difference between the sexes in the mean CC depth while the existence of feedback regarding the proportion of accurate CC depth, after adjusting for influencing factors. We believe that the ability to compress the chest deeper depends on physical strength. And, feedback could be important to achieve the proper CC depth without developing complications according to the guidelines.
Recently, the use of smart devices has spread exponentially, and a feedback system based on the use of smart devices to improve the quality of CC has emerged. The effectiveness of a feedback system based on a smartphone has previously been reported in manikin studies [20, 21]. This system involves the rescuer grasping the smartphone in the palm of one hand or placing the smartphone in a pouch or pocket when performing CC. However, this could lead to errors in the acceleration measurement depending on the mounting method [21, 32]. Smartwatches might overcome the limitations of smartphones because they can be worn and they are lightweight devices that are strapped to the wrist. Thus, smartwatches could be useful feedback devices for individuals who use a smartwatch for performing CPR in real-life situations.
This study has several limitations. First, this was a simulation study using a manikin; thus, the various features in clinical environment were not considered. To address this, clinical studies on the effects of CC-related feedback are required. Second, this feedback system with an accelerometer could not compensate for the mattress compression and may be inappropriate for in-hospital cardiac arrest patients placed on a bed. Third, participants consisted of young attendees of a medical school. A previous study reported that CPR is often performed by elderly rescuers [33], which may be because the majority of cardiac arrests occur in the elderly, and it is often the responsibility of their cohabitee to perform CPR. Therefore, the age of our study population is a limitation of this study. Fourth, a cardiac arrest in real life is often urgent and a rescuer is typically in a panicked state; hence, it is important that feedback devices are operated and applied quickly. However, this study did not assess the time it took participants to operate the smartwatch feedback program.
Conclusions
In conclusion, a smartwatch CPR feedback system could assist rescuers by providing feedback regarding the ideal range for CC depth in concordance with CPR guidelines from the AHA. A smartwatch is a good and wearable feedback device for CC during CPR, and this system could easily be applied to CPR performed for out-of-hospital cardiac arrest patients by rescuers who wear smartwatches.
Supporting information
(XLSX)
Acknowledgments
This paper was supported by the Bumsuk Academic Research Fund in 2015.
Data Availability
All relevant data are within the paper and its Supporting Information files.
Funding Statement
This paper was supported by Bumsuk Academic Research Fund in 2015, http://www.bumsuk.or.kr/. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1.Kleinman ME, Brennan EE, Goldberger ZD, Swor RA, Terry M, Bobrow BJ, et al. Part 5: Adult Basic Life Support and Cardiopulmonary Resuscitation Quality 2015 American Heart Association guidelines update for cardiopulmonary resuscitation and emergency cardiovascular care. Circulation. 2015;132 Suppl:414–35. [DOI] [PubMed] [Google Scholar]
- 2.Berg RA, Hemphill R, Abella BS, Aufderheide TP, Cave DM, Hazinski MF, et al. Part 5: Adult basic life support 2010 American Heart Association guidelines for cardiopulmonary resuscitation and emergency cardiovascular care. Circulation. 2010;122 Suppl:685–705. [DOI] [PubMed] [Google Scholar]
- 3.Kim MJ, Park YS, Kim SW, Yoon YS, Lee KR, Lim TH, et al. Chest injury following cardiopulmonary resuscitation: a prospective computed tomography evaluation. Resuscitation. 2013;84(3):361–4. 10.1016/j.resuscitation.2012.07.011 [DOI] [PubMed] [Google Scholar]
- 4.Hellevuo H, Sainio M, Nevalainen R, Huhtala H, Olkkola KT, Tenhunen J, et al. Deeper chest compression–More complications for cardiac arrest patients? Resuscitation. 2013;84(6):760–5. 10.1016/j.resuscitation.2013.02.015 [DOI] [PubMed] [Google Scholar]
- 5.Hoke RS, Chamberlain D. Skeletal chest injuries secondary to cardiopulmonary resuscitation. Resuscitation. 2004;63(3):327–38. 10.1016/j.resuscitation.2004.05.019 [DOI] [PubMed] [Google Scholar]
- 6.Swenson RD, Weaver WD, Niskanen RA, Martin J, Dahlberg S. Hemodynamics in humans during conventional and experimentl methods of cardiopulmonary resuscitation. Circulation. 1988;78(3):630–9. [DOI] [PubMed] [Google Scholar]
- 7.van Tulder R, Laggner R, Kienbacher C, Schmid B, Zajicek A, Haidvogel J, et al. The capability of professional- and lay-rescuers to estimate the chest compression-depth target: a short, randomized experiment. Resuscitation 2015;89:137–41. 10.1016/j.resuscitation.2015.01.031 [DOI] [PubMed] [Google Scholar]
- 8.Yang C-W, Yen Z-S, McGowan JE, Chen HC, Chiang W-C, Mancini ME, et al. A systematic review of retention of adult advanced life support knowledge and skills in healthcare providers. Resuscitation. 2012;83(9):1055–60. 10.1016/j.resuscitation.2012.02.027 [DOI] [PubMed] [Google Scholar]
- 9.Jensen ML, Lippert F, Hesselfeldt R, Rasmussen MB, Mogensen SS, Jensen MK, et al. The significance of clinical experience on learning outcome from resuscitation training—a randomised controlled study. Resuscitation. 2009;80(2):238–43. 10.1016/j.resuscitation.2008.10.026 [DOI] [PubMed] [Google Scholar]
- 10.Birnbaum ML, Robinson NE, Kuska BM, Stone HL, Fryback DG, Rose JH. Effect of advanced cardiac life-support training in rural, community hospitals. Crit Care Med. 1994;22(5):741–9. [DOI] [PubMed] [Google Scholar]
- 11.Kirkbright S, Finn J, Tohira H, Bremner A, Jacobs I, Celenza A. Audiovisual feedback device use by health care professionals during CPR: a systematic review and meta-analysis of randomised and non-randomised trials. Resuscitation. 2014;85(4):460–71. 10.1016/j.resuscitation.2013.12.012 [DOI] [PubMed] [Google Scholar]
- 12.Yeung J, Meeks R, Edelson D, Gao F, Soar J, Perkins GD. The use of CPR feedback/prompt devices during training and CPR performance: a systematic review. Resuscitation. 2009;80(7):743–51. 10.1016/j.resuscitation.2009.04.012 [DOI] [PubMed] [Google Scholar]
- 13.Abella BS, Edelson DP, Kim S, Retzer E, Myklebust H, Barry AM, et al. CPR quality improvement during in-hospital cardiac arrest using a real-time audiovisual feedback system. Resuscitation. 2007;73(1):54–61. 10.1016/j.resuscitation.2006.10.027 [DOI] [PubMed] [Google Scholar]
- 14.Hostler D, Everson-Stewart S, Rea TD, Stiell IG, Callaway CW, Kudenchuk PJ, et al. Effect of real-time feedback during cardiopulmonary resuscitation outside hospital: prospective, cluster-randomised trial. BMJ. 2011;342:d512 10.1136/bmj.d512 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kramer-Johansen J, Myklebust H, Wik L, Fellows B, Svensson L, Sørebø H, et al. Quality of out-of-hospital cardiopulmonary resuscitation with real time automated feedback: A prospective interventional study. Resuscitation. 2006;71(3):283–92. 10.1016/j.resuscitation.2006.05.011 [DOI] [PubMed] [Google Scholar]
- 16.Buléon C, Parienti J-J, Halbout L, Arrot X, Régent HDF, Chelarescur D, et al. Improvement in chest compression quality using a feedback device (CPRmeter): a simulation randomized crossover study. Am J Emerg Med. 2013;31(10):1457–61. 10.1016/j.ajem.2013.07.029 [DOI] [PubMed] [Google Scholar]
- 17.Krasteva V, Jekova I, Didon J-P. An audiovisual feedback device for compression depth, rate and complete chest recoil can improve the CPR performance of lay persons during self-training on a manikin. Physiol Meas. 2011;32(6):687 10.1088/0967-3334/32/6/006 [DOI] [PubMed] [Google Scholar]
- 18.Skorning M, Beckers SK, Brokmann JC, Rörtgen D, Bergrath S, Veiser T, et al. New visual feedback device improves performance of chest compressions by professionals in simulated cardiac arrest. Resuscitation. 2010;81(1):53–8. 10.1016/j.resuscitation.2009.10.005 [DOI] [PubMed] [Google Scholar]
- 19.Bohn A, Weber TP, Wecker S, Harding U, Osada N, VanAken H, et al. The addition of voice prompts to audiovisual feedback and debriefing does not modify CPR quality or outcomes in out of hospital cardiac arrest–A prospective, randomized trial. Resuscitation. 2011;82(3):257–62. 10.1016/j.resuscitation.2010.11.006 [DOI] [PubMed] [Google Scholar]
- 20.Gruber J, Stumpf D, Zapletal B, Neuhold S, Fischer H. Real-time feedback systems in CPR. Curr Anaesth Crit Care. 2012;2(6):287–94. [Google Scholar]
- 21.Song Y, Oh J, Chee Y. A new chest compression depth feedback algorithm for high-quality CPR based on smartphone. Telemed E Health. 2015;21(1):36–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Song Y, Chee Y, Oh J, Ahn C, Lim TH. Smartwatches as chest compression feedback devices: A feasibility study. Resuscitation. 2016;103:20–3. 10.1016/j.resuscitation.2016.03.014 [DOI] [PubMed] [Google Scholar]
- 23.Bland JM, Altman DG. Best (but oft forgotten) practices: testing for treatment effects in randomized trials by separate analyses of changes from baseline in each group is a misleading approach. Am J Clin Nutr. 2015;102:991–4 10.3945/ajcn.115.119768 [DOI] [PubMed] [Google Scholar]
- 24.Meaney PA, Bobrow BJ, Mancini ME, Chiristenson J, DeCaen AR, Bhanji F, et al. Cardiopulmonary resuscitation quality: improving cardiac resuscitation outcomes both inside and outside the hospital a consensus statement from the American Heart Association. Circulation. 2013;128(4):417–35. 10.1161/CIR.0b013e31829d8654 [DOI] [PubMed] [Google Scholar]
- 25.Nolan JP. High-quality cardiopulmonary resuscitation. Curr Opin Crit Care 2014;20(3):227–33. 10.1097/MCC.0000000000000083 [DOI] [PubMed] [Google Scholar]
- 26.Stiell IG, Brown SP, Christenson J, Cheskes S, Nichol G Powell J, et al. What is the role of chest compression depth during out-of-hospital cardiac arrest resuscitation? Crit Care Med. 2012;40(4):1192 10.1097/CCM.0b013e31823bc8bb [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Li Q, Ma E-L, Liu J, Fang L-Q, Xia T. Pre-training evaluation and feedback improve medical students’ skills in basic life support. Med Teach. 2011;33(10):e549–e55. 10.3109/0142159X.2011.600360 [DOI] [PubMed] [Google Scholar]
- 28.Peberdy MA, Silver A, Ornato JP. Effect of caregiver gender, age, and feedback prompts on chest compression rate and depth. Resuscitation. 2009;80(10):1169–74. 10.1016/j.resuscitation.2009.07.003 [DOI] [PubMed] [Google Scholar]
- 29.Riegel B, Birnbaum A, Aufderheide TP, Thode HC, Henry MC, VanOttinghan L, et al. Predictors of cardiopulmonary resuscitation and automated external defibrillator skill retention. Am Heart J. 2005;150(5):927–32. 10.1016/j.ahj.2005.01.042 [DOI] [PubMed] [Google Scholar]
- 30.Verplancke T, De Paepe P, Calle P, De Regge M, Van Maele G, Monsieurs K. Determinants of the quality of basic life support by hospital nurses. Resuscitation. 2008;77(1):75–80. 10.1016/j.resuscitation.2007.10.006 [DOI] [PubMed] [Google Scholar]
- 31.Ashton A, McCluskey A, Gwinnutt C, Keenan A. Effect of rescuer fatigue on performance of continuous external chest compressions over 3 min. Resuscitation. 2002;55(2):151–5. [DOI] [PubMed] [Google Scholar]
- 32.Lee S, Oh J, Kang H, Lim T, Kim W, Chee Y, et al. Proper target depth of an accelerometer-based feedback device during CPR performed on a hospital bed: a randomized simulation study. Am J Emerg Med. 2015;33(10):1425–9. 10.1016/j.ajem.2015.07.010 [DOI] [PubMed] [Google Scholar]
- 33.Neset A, Birkenes TS, Myklebust H, Mykletun RJ, Odegaard S, Kramer-Johansen J. A randomized trial of the capability of elderly lay persons to perform chest compression only CPR versus standard 30: 2 CPR. Resuscitation. 2010;81(7):887–92. 10.1016/j.resuscitation.2010.03.028 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(XLSX)
Data Availability Statement
All relevant data are within the paper and its Supporting Information files.