Abstract
Introduction
Compared to the general population, veterans of the wars in Afghanistan and Iraq (OEF/OIF) are more likely to engage in hazardous alcohol use and meet criteria for mental health disorders including Posttraumatic Stress Disorder (PTSD) and Major Depressive Disorder. Less is known how distinct profiles of alcohol use behavior relate to mental health symptoms.
Method
The current study examined the extent that indicators of alcohol use (i.e., drinks per week, peak blood alcohol concentration, and alcohol-related problems) are categorized into different alcohol risk profiles utilizing a person-centered approach. We also examined how mental health symptoms (i.e., PTSD, depression, and anxiety-related symptoms) were associated with the alcohol risk profiles. Participants were 252 Veterans who reported consuming alcohol within the past month.
Results
Latent profile analysis indicated a four-class solution yielded the best-fitting model, and profiles were named based on their respective levels and patterns of alcohol use. Mental health symptoms were significantly different among the four profiles. Profiles of veterans who endorsed more alcohol-related problems (i.e., the “Severe alcohol behavior” and “Steady drinkers with functional impairment”) also reported comorbid clinical symptoms of PTSD, depression, and anxiety. The “Binge drinkers with no functional impairment” and “Mild alcohol behavior” profiles reported the lowest levels of mental health symptoms.
Discussion
Findings highlight the unique relationship between distinct alcohol risk profiles and mental health outcomes. Targeted interventions and treatment options based on unique alcohol risk profiles may be helpful in tailoring prevention and intervention efforts in detecting co-occurring mental health symptoms among OEF/OIF veterans.
Keywords: Veterans, Alcohol, Comorbid, PTSD, Depression
1. Introduction
1.1 Veteran Alcohol Use
Research has indicated that up to 13% of veterans of the wars in Iraq (Operation Iraqi Freedom [OIF]) and Afghanistan (Operation Enduring Freedom [OEF]) meet criteria for an Alcohol Use Disorder (Kehle et al., 2012), compared to 8% of the general US population (Grant et al., 2004). Rates of hazardous drinking among OEF/OIF veterans [defined as binge drinking (using the 4/5+ cut off) and/or scores 8 or higher on the Alcohol Use Disorders Identification Test (AUDIT; Babor, Higgins-Biddle, Saunders, & Monteiro, 2001)], have ranged from 18% to 40% (Calhoun, Elter, Jones, Kudler, & Straits-Troster, 2008; Eisen et al., 2012; Hoge et al., 2004), and are higher than non-OEF/OIF veterans (Hawkins, Lapham, Kivlahan, & Bradley, 2010) and non-veterans (Wagner et al., 2007). Research examining hazardous alcohol use in OEF/OIF samples typically use brief screeners, such as the AUDIT, which combine questions regarding quantity/frequency of alcohol use, alcohol-related problems, and diagnostic symptoms, into one composite variable (e.g., Burnett-Zeigler et al., 2011; Calhoun et al., 2008; Eisen et al., 2012; Hoge et al., 2004; Jakupcak et al., 2010; McDevitt-Murphy et al., 2010; McDevitt-Murphy, Fields, Monahan, & Bracken, 2015; Smith et al., 2014; Wilk et al., 2010). By examining variable-level outcomes that combine multiple alcohol-related indices (e.g., quantity/frequency/problems), these approaches may be limited as they do not identify groups of people who share similarities on specific indices. The dimension of drinking quantity/frequency could be examined separately from alcohol-related problems to further clarify alcohol outcomes.
1.2. Mental Health and Alcohol Use
Previous studies among veterans have addressed the co-occurrence of hazardous alcohol consumption and PTSD (McDevitt-Murphy et al., 2015; Wilk et al., 2010). Other studies have indicated OEF/OIF veterans experience more mental health symptomology compared to the general population (Eisen et al., 2012); 36.9% of OEF/OIF veterans (n=289,328) entering VA healthcare met criteria for a mental health disorder. Of those, 29% experienced two disorders and 33% met criteria for three or more disorders (Seal et al., 2009). Studies have indicated that 37.3% of OEF/OIF veterans screening positive for mental health disorders also engaged in hazardous drinking (Heltemes, Clouser, MacGregor, Norman, & Galarneau, 2014). In turn, 26.9% of hazardous drinkers screened positive for significant mental health symptoms (Smith et al., 2014). Mental health disorders most commonly associated with hazardous alcohol use include symptoms of posttraumatic stress disorder (PTSD), depression, and other anxiety-related disorders (Burnett-Zeigler et al., 2011; Stecker, Fortney, Owen, McGovern, & Williams, 2010).
Of all medical and psychiatric diagnoses, depression and PTSD were the second and third most common, occurring in nearly 13% and 12% of a national OEF/OIF sample, respectively; PTSD was the most common mental health diagnosis (Seal et al., 2009; Stecker, Fortney, Owen, McGovern, & Williams, 2010). For comparison, 7% of the general US population meets criteria for Major Depressive Disorder and 11% meets criteria for any anxiety disorder (Grant et al., 2004). OEF/OIF veterans endorsing PTSD or depression symptoms are two times more likely to engage in hazardous alcohol use relative to veterans not endorsing symptoms (Jakupcak et al., 2010). Additionally, PTSD symptoms, depression symptoms, and hazardous drinking are highly predictive of one another (Mustillo et al., 2015). Studied less often in OEF/OIF samples is the presence of anxiety symptoms (distinct from PTSD-related symptomology), despite 5% of veterans being diagnosed with a current anxiety-related disorder (Stecker et al., 2010), 16% to 8% reporting anxiety-related symptoms (Hoge et al., 2004), and links between anxiety symptoms and hazardous drinking in OEF/OIF samples (Barry, Whiteman, MacDermid Wadsworth, & Hitt, 2012).
Most studies have focused on PTSD when attempting to explain the link between alcohol use and mental health symptoms in OEF/OIF veterans. Findings have indicated that combat experiences and PTSD onset prior to alcohol use disorders (Kline et al., 2014), and symptom clusters related to avoidance and numbing (Jakupcak et al., 2010; Kehle et al., 2012) predict alcohol use behaviors. Moreover, PTSD symptom severity in OEF/OIF veterans was positively associated with increased coping-related drinking motives (McDevitt-Murphy et al., 2015). Such findings suggest that alcohol consumption may serve as a method of managing mental health symptoms, consistent with theories of self-medication where hazardous drinking is negatively reinforced via reduction in symptom-related experiences (Khantzian, 2003; Stewart, 1996). Although a substantial amount of research has reported on the association between hazardous drinking and mental health symptoms, much less research has examined how mental health symptoms relate to distinct profiles of alcohol risk indices.
1.3. Person-Centered Analyses
Latent Profile Analysis (LPA)/Latent Class Analysis (LCA) are person-centered analyses where individuals are categorized into different groups (known as “profiles”) based on shared characteristics. Profiles can then be examined to understand how groups differ on external criteria (Muthén & Muthén, 2002). LPA approaches are helpful in identifying groups who may be at increased risk and therefore candidates for targeted interventions. To date, there has been little research explicitly examining alcohol use profiles. Previous research that has focused on patterns of alcohol use and mental health symptoms has typically created variable level categories of drinking status (i.e., using cut points for moderate and heavy drinking) based on individuals’ quantity/frequency estimates (e.g., Alati et al., 2005; Caldwell et al., 2002; O’Donnell, Wardle, Dantzer, & Steptoe, 2006).
1.4. The Current Study
Taken together, OEF/OIF veterans engage in elevated rates of hazardous drinking. Most findings, however, rely on brief screeners where alcohol-related behaviors such as quantity/frequency estimates and problems are combined in variable-level analyses as a composite alcohol risk variable. To build on the existing literature, the first aim of the current study was to determine the extent to which OEF/OIF alcohol use indices (i.e., drinks per week, peak blood alcohol concentration (BAC), and alcohol-related problems) may be categorized into different alcohol risk profiles utilizing a person-centered approach. Although we made no hypothesizes on the exact number of profiles, we did predict that individuals with greater alcohol use and problems would form a distinct profiles from those with less use and consequently less problems. While the co-occurrence of mental health symptoms and hazardous drinking has been well-documented in OEF/OIF samples, to our knowledge no studies have examined how mental health symptoms may relate to alcohol use profiles. Accordingly, the second aim of the study was to examine how different mental health symptoms (i.e., PTSD, depression, and anxiety-related symptoms) are associated with alcohol risk profiles. We hypothesized that profiles with greater alcohol use indices would be associated with increased mental health symptoms, and profiles with less alcohol use indices would be associated with less mental health symptoms.
2. Method
2.1. Participants and Procedure
The current project analyzed baseline data from 252 veterans (95% male; 83% white, M age = 31.77 years) who participated in a brief alcohol intervention and reported consuming alcohol within the past 30 days. Martens, Cadigan, Rogers, and Osborn (2015) provide a detailed description of the study procedures and the main outcomes of the study. Veterans presenting to the Operation Enduring Freedom/Operation Iraqi Freedom/Operation New Dawn (OEF/OIF/OND) Seamless Transition Clinic at the Harry S. Truman Memorial Veterans’ Hospital were eligible to participate. The Seamless Transition Clinic is a one-time clinic for returning combat veterans to assess post deployment needs. The day of the clinic appointment, veterans interested in participating in the study met with project staff to complete informed consent and the baseline battery of questions. Participants were randomized into one of two intervention conditions: a personalized drinking feedback intervention where they received personalized information on their alcohol use or an educational information control condition describing the effects of alcohol on the body. Participants were compensated with a $30 check after completing their baseline assessment. This study was approved by the University of Missouri Institutional Review Board and the Veterans Administration Subcommittee for Research Safety.
2.2. Measures
2.2.1. Alcohol use and problems
Daily Drinking Questionnaire (DDQ)
The DDQ (Collins, Parks, & Marlatt, 1985) asks participants to indicate the number of drinks typically consumed on each day of the week over the past 30 days, the most number of drinks consumed, and hours spent drinking. Standard definitions of an alcoholic drink were provided: a 12oz beer (i.e., most bottled or canned beer), a 5oz glass of wine (i.e., a regular-sized glass of wine), or a 1.25oz (one shot) drink of hard alcohol. Average number of drinks per week consumed and peak estimated BAC were calculated from the DDQ.
Short Inventory of Problems (SIP)
The SIP (Miller et al., 1995) is a 15-item measure used to assess alcohol-related problems in the past 6 months on a range of 0 (no problems) to 15 (endorsed each of the 15 problems). For each item, participants indicated “yes” (coded as “1”) or “no” (coded as “0”) if they had experienced the alcohol-related problem. Items include “My drinking has damaged my social life, popularity, or reputation”; “I have had money problems because of my drinking”; “I have failed to do what is expected of me because of my drinking.” The internal consistency estimate for the measure was .87 in the present study.
2.2.2. Mental health symptoms
Posttraumatic Stress Disorder Checklist-Military version (PCLM)
Based on the DSM-IV, the PCLM (Weathers, Litz, Herman, Huska, & Keane, 1993) is a 17-item measure with a 5-point Likert scale used to assess the presence and severity of PTSD symptoms in the past month. Responses range from 1 (not at all) to 5 (extremely), with scores ranging from 17 to 85, with higher scores indicating greater symptoms. A clinical cutoff score of 50 or greater is used to detect PTSD symptoms in military samples, with sensitivity of .69 and specificity of .83 (Karstoft, Andersen, Bertelsen, & Madsen, 2014). Internal consistency was .96 in the present study.
Center for Epidemiologic Studies Depression Scale (CES-D)
The CES-D (Radloff, 1977) is a widely-used 20 item measure with a 4-point Likert scale used to assess depression symptoms in non-clinical populations (Radloff, 1991). Participants were asked to indicate the number of times they have experienced each symptom in the past week, ranging from 0 (< 1 day) to 3 (5–7 days), with scores ranging from 0 to 60, with higher scores indicating more depression symptoms. The sensitivity of the CES-D in identifying those with a diagnosis of major depressive disorder has ranged from .83 to .94 (Rost, Burnam, & Smith, 1993), with a clinical cutoff score of 16 or greater used to detect depressive symptoms (Radloff, 1977). The internal consistency estimate for the measure was .79 in the present study.
Anxiety
A modified version of the GAD-2, (Kroenke, Spitzer, Williams, Monahan, & Lowe, 2007) was used to assess anxiety symptoms in the past month. Items asked are “Have you been feeling nervous, anxious, or on edge” and “Have you not been able to control or stop worrying”. These items assess core diagnostic criteria of Generalized Anxiety Disorder (GAD) and are the first two items of the GAD-7 (Sptizer, Kroenke, Williams, & Lowe, 2006), a widely used anxiety screening measure. The GAD-2 has a sensitivity of .65 and specificity of .88 for identifying any anxiety disorder (Kroenke, Spitzer, Williams, Monahan, & Lowe, 2007). A modified version of the GAD-2 was used as each item was dichotomous scored (no =0, yes =1). Scores of the two items were then summed and ranged from 0 to 2, with higher scores indicative of greater levels of anxiety.
2.3. Analytic Procedure
Latent Profile Analysis (LPA) is a person-centered analysis that enables researchers to categorize individuals into different groups based on similar characteristics and then examine the degree to which groups differ on external criterion (Muthén & Muthén, 2002). LPA was used to classify veterans’ alcohol use into optimal profiles using three indicators of alcohol risk over the past 30 days: peak BAC, drinks per week, and alcohol-related problems.
Analyses were conducted using MPlus version 7.0 (Muthén & Muthén, 2004). The fit of five models (one-class through a five-class solution) were assessed. Selection of class solution (also known as “profiles”) was based in part on Bayesian Information Criterion (BIC; Schwartz, 1978), entropy (Ramaswamy et al., 1993), and the Vuong-Lo-Mendell-Rubin (VLMR) likelihood difference test. BIC is a goodness of fit index where lower values indicate better fit. Entropy values range from 0 – 1 and measure how accurately individuals are classified, with high values indicating better fit (Muthén et al., 2002). VLMR is used to assess the fit between two solutions that differ by one class and a significant p value suggests a better fitting model. The Parametric Bootstrap Likelihood Validation Test (MPlus 7.0) was then used to confirm the final class solution, testing if the selected solution provides a better fit than the solution with one less class. Maximum likelihood estimation was used to account for missing data, which assumes data are missing at random (Arbuckle, 1996; Little, 1995), and is a common method for addressing missing data (Muthén & Shedden, 1999).
After determining the optimal class solution, we used analysis of variance (ANOVA) to examine the relationship between the profiles and mental health outcomes (i.e., depression symptoms, anxiety symptoms, PTSD symptoms). Post-hoc pairwise comparisons were used to examine differences among profiles with regards to each outcome.
3. Results
For the entire sample of 252 veterans, the average number of drinks per week consumed was 13.76 (SD = 12.27), average peak BAC was 0.07 (SD = 0.09), and average number of alcohol-related problems was 2.07 (SD = 2.71). Correlations, means, and standard deviations of all measured variables for each profile are shown in Table 1. All alcohol variables were positively correlated with each other (p’s < .01). Drinks per week and peak BAC were not significantly correlated with any mental health outcome (p’s > .05) and alcohol-related problems were positively correlated with each mental outcome (p’s < .01). All mental health outcomes were positively correlated with each other (p’s < .01).
Table 1.
Means, standard deviations, and correlations among all measured variables in the entire sample of Veterans (N = 252).
| 1 | 2 | 3 | 4 | 5 | 6 | M | SD | |
|---|---|---|---|---|---|---|---|---|
| 1 Drinks per Week | - | 13.76 | 12.27 | |||||
| 2 Peak BAC | .52* | - | 0.07 | 0.09 | ||||
| 3 Alcohol-Related Problems | .50* | .30* | - | 2.07 | 2.71 | |||
| 4 PTSD | .09 | .10 | .39* | - | 42.39 | 18.56 | ||
| 5 Depression | .07 | .08 | .41* | .77* | - | 15.70 | 12.91 | |
| 6 Anxiety | .09 | .12 | .35* | .69* | .64* | - | 1.03 | 0.85 |
Note.
p < .01;
peak BAC = peak blood alcohol concentration, alcohol-related problems were measured by the SIP, PTSD was measured by the PCLM, depression was measured by the CESD, anxiety was measured by the GAD-2.
3.1. Identification of Latent Profiles
Model fit indices are reported in Table 2. A four-class solution was determined to be the best-fitting model due to lowest BIC, significant VLMR p value (meaning the four-class solution was a better fit to the data than the five-class solution by this criteria), and entropy value (.94) indicating good classification of individuals.
Table 2.
Model fit indices for 1–5 class solutions of peak BAC, drinks per week, and alcohol-related problems.
| Model | AIC | BIC | Adj BIC | VLMRp | Entropy |
|---|---|---|---|---|---|
| 1 class solution | 2787.77 | 2808.95 | 2789.93 | - | - |
| 2 class solution | 2579.12 | 2614.41 | 2582.71 | 0.04 | 0.92 |
| 3 class solution | 2498.21 | 2547.63 | 2503.24 | 0.11 | 0.93 |
| 4 class solution | 2405.46 | 2468.99 | 2411.92 | 0.02 | 0.94 |
| 5 class solution | 2392.82 | 2470.47 | 2400.73 | 0.53 | 0.97 |
Note. Bold indicates best fit. AIC = Akaike information criterio; BIC = Bayesian information criterion; VLMR = Vuong-Lo-Mendell-Rubin likelihood difference test.
3.2. Descriptive Analysis of Latent Profiles
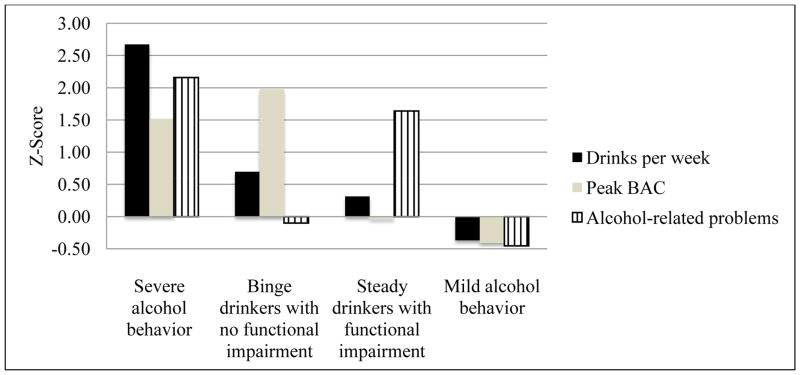
Z-scores of the indicators of the alcohol risk profiles are shown in Figure 1. Profiles were named relative to the alcohol risk indicators of the other profiles. The “Severe alcohol behavior” profile (N = 14; 5.6%; 100% male; 71% White; M age = 26.79) consumed the most drinks per week of all groups (51.91), had a high peak BAC (0.21), and reported the most alcohol-related problems of all groups (7.92). The “Binge drinkers with no functional impairment” profile (N = 28; 11.1%; 96.4% male; 86% White; M age = 27.68) consumed an elevated number of drinks per week (23.74), had the highest peak BAC of all groups (0.25), but reported few alcohol-related problems (1.80). The “Steady drinkers with functional impairment” profile (N = 32; 12.7%; 90.6% male; 84% White; M age = 31.59) reported an elevated number of drinks per week (18.27), a low peak BAC (0.06), and a high number of alcohol-related problems (6.51). Last, the “Mild alcohol behavior” profile (N = 178; 70.6%; 94.4% male; 82% White; M age = 32.78) reported consuming the least amount of drinks per week (8.50), the lowest peak BAC (0.03), and the lowest number of alcohol-related problems (0.84).
Figure 1.
Z scores of alcohol risk indicators of the four-class solution
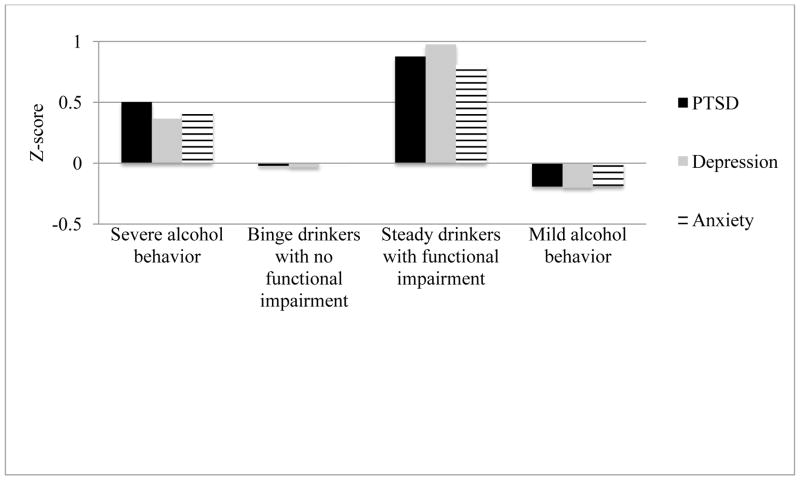
3.3. Relationship Between Latent Profiles and Mental Health Outcomes
After the latent profiles of alcohol risk were identified, ANOVA models were used to assess the relationship between profiles and mental health outcomes. Means, standard deviations, and post-hoc significant class comparisons for each latent profile are shown in Table 3. Z-scores of the alcohol risk profiles and mental health outcomes (PTSD, depression, and anxiety symptoms) are shown in Figure 2.
Table 3.
Means, standard deviations, and significant class comparisons of the 4 alcohol classes.
| Severe alcohol behavior | Binge drinkers with no functional impairment | Steady drinkers with functional impairment | Mild alcohol behavior | Significant class comparisons and effect size | |
|---|---|---|---|---|---|
|
| |||||
| M (SD) | M (SD) | M (SD) | M (SD) | ||
| Peak BAC | 0.21 (0.08) | 0.25 (0.09) | 0.06 (0.06) | 0.03 (0.03) | Severe vs. Binge: p < .05, d = .47 |
| Severe vs. Steady: p < .01, d = 2.12 | |||||
| Severe vs. Mild: p < .01, d = 2.98 | |||||
| Binge vs. Steady: p < .01, d = 3.17 | |||||
| Binge vs. Mild: p < .01, d = 4.64 | |||||
| Steady vs. Mild: p < .01, d = .63 | |||||
| Drinks per Week | 51.91 (15.12) | 23.74 (13.32) | 18.27 (10.92) | 8.50 (7.71) | Severe vs. Binge: p < .01, d = 1.97 |
| Severe vs. Steady: p < .01, d = 2.55 | |||||
| Severe vs. Mild: p < .01, d = 3.62 | |||||
| Binge vs. Steady: p < .01, d = .45 | |||||
| Binge vs. Mild: p < .01, d = 1.40 | |||||
| Steady vs. Mild: p < .01, d = 1.03 | |||||
| Alcohol-Related Problems | 7.92 (1.96) | 1.80 (1.36) | 6.51 (1.79) | 0.84 (1.16) | Severe vs. Binge: p < .01, d = 3.63 |
| Severe vs. Steady: p < .01, d = .75 | |||||
| Severe vs. Mild: p < .01, d = 4.40 | |||||
| Binge vs. Steady: p < .01, d = 2.96 | |||||
| Binge vs. Mild: p < .01, d = .76 | |||||
| Steady vs. Mild: p < .01, d = 3.76 | |||||
| PTSD | 51.71 (18.39) | 41.96 (17.29) | 58.66 (18.04) | 38.82 (17.07) | Severe vs. Binge: ns |
| Severe vs. Steady: ns | |||||
| Severe vs. Mild: p < .01, d = .73 | |||||
| Binge vs. Steady: p < .01, d = .95 | |||||
| Binge vs. Mild: ns | |||||
| Steady vs. Mild: P < .01, D = 1.13 | |||||
| Depression | 20.43 (14.34) | 15.29 (11.71) | 28.31 (13.63) | 13.09 (11.39) | Severe vs. Binge: ns |
| Severe vs. Steady: p < .01, d = .56 | |||||
| Severe vs. Mild: p < .05, d = .57 | |||||
| Binge vs. Steady: p < .01, d = 1.02 | |||||
| Binge vs. Mild: ns | |||||
| Steady vs. Mild: p < .01, d = 1.21 | |||||
| Anxiety | 1.40 (0.85) | 1.03 (0.84) | 1.72 (0.52) | 0.87 (0.83) | Severe vs. Binge: ns |
| Severe vs. Steady: ns | |||||
| Severe vs. Mild: p < .05, d = .63 | |||||
| Binge vs. Steady: p < .01, d = .99 | |||||
| Binge vs. Mild: ns | |||||
| Steady vs. Mild: p < .01, d = 1.23 | |||||
Note. Ns = non significant; peak BAC = peak blood alcohol concentration, alcohol-related problems were measured by the SIP, PTSD was measured by the PCLM, depression was measured by the CESD, anxiety was measured by a modified GAD-2.
Figure 2.
Z scores of mental health outcomes associated with each alcohol risk profile
3.4 Association Between Alcohol Risk Profiles and Depression Symptoms
Depression symptoms among the four alcohol risk profiles were significantly different, F(3, 248) = 15.59, p < .001, ηp2 = .16. The “Steady drinkers with functional impairment” profile reported an average score of 28, the highest number of depression symptoms among the profiles, and the “Severe alcohol behavior” profile reported an average score of 20. Findings suggested, on average, that both profiles exceed the clinical cut-off for a probable diagnosis of Major Depressive Disorder. The “Binge drinkers with no functional impairment” profile reported an average score of 15 and the “Mild alcohol behavior” profile reported an average score of 13, both below the clinical cut-off. Post-hoc pairwise comparisons revealed significant differences in depression symptoms between the Steady vs. Severe classes (p < .01), the Steady vs. Binge classes (p < .01), the Steady vs. Mild classes (p < .05), and the Severe vs. Mild classes (p < .05).
3.5 Association Between Alcohol Risk Profiles and Anxiety Symptoms
Results indicated anxiety symptoms among the four profiles were significantly different, F(3, 248) = 11.15, p < .001, ηp2 = .12. The highest rates of anxiety symptoms were found in the “Steady drinkers with functional impairment” and “Severe alcohol behavior” profiles, with each profile reporting an average anxiety score of 1.72 and 1.40, respectively. The “Binge drinkers with no functional impairment” and “Mild alcohol behavior” profiles had the lowest levels of anxiety symptoms with average anxiety scores of 1.03 and 0.87, respectively. Post-hoc pairwise comparisons revealed significant differences in anxiety symptoms between the Steady vs. Binge classes (p < .01), the Steady vs. Mild classes (p < .01), and the Severe vs. Mild classes (p < .05).
3.6 Association Between Alcohol Risk Profiles and PTSD Symptoms
There were significant differences in PTSD symptoms among the profiles, F(3, 248) = 13.33, p < .001, ηp2 = .14. The “Steady drinkers with functional impairment” and “Severe alcohol behavior” profiles reported the highest PTSD scores, 58 and 51, respectively. Results indicated that, on average, both profiles exceed the clinical cut-off for a probable diagnosis of PTSD. The “Binge drinkers with no functional impairment” and “Mild alcohol behavior” profiles had the lowest levels of PTSD symptoms with average scores of 41 and 38, respectively. Post-hoc pairwise comparisons revealed significant differences in PTSD symptoms between the Steady vs. Binge classes (p < .01), the Steady vs. Mild classes (p < .01), and the Severe vs. Mild classes (p < .01).
4. Discussion
The present study examined the extent to which three indicators of OEF/OIF alcohol behavior could be categorized into different alcohol risk profiles utilizing a person-centered approach. A four-class solution best fit the data and profiles were named on their level of alcohol risk relative to the other profiles: “Severe alcohol behavior” profile (with elevated levels of all indicators of alcohol risk), “Binge drinkers with no functional impairment” profile (with elevated levels of BAC, high drinks, and low problems), “Steady drinkers with functional impairment” profile (with low levels of BAC, moderate drinks, and elevated problems), and “Mild alcohol behavior” profile (with low levels of all indicators). Results indicated alcohol risk profiles were uniquely associated with varying severity of mental health symptoms. The “Steady drinkers with functional impairment” profile reported the highest levels of PTSD, depression, and anxiety symptoms, the “Severe alcohol behavior” profile reported the second highest levels of mental health symptoms, and the “Binge drinkers with no functional impairment” and “Mild alcohol behavior” profiles reported the lowest levels of mental health symptoms. These profiles provide a more nuanced understanding of the relationship between alcohol outcomes and co-occurring mental health symptomology.
Although prior research has found OEF/OIF veterans with mental health symptoms are more likely to report hazardous alcohol use (Heltemes, Clouser, MacGregor, Norman, & Galarneau, 2014; Jakupcak et al., 2010), the current study suggests this relationship may be dependent on alcohol-related problems. Our findings indicate profiles of veterans who endorse higher levels of alcohol-related problems (and therefore impaired overall functioning), regardless of levels of alcohol use, also report comorbid clinical symptoms of PTSD, depression, and anxiety that, on average, exceed the respective clinical cut-offs. It has been documented that increased alcohol-related problems are associated with greater mental health symptoms. For example, the alcohol profiles found in the current study are consistent with previous research in which greater depression symptoms were associated with alcohol-related consequences, regardless of level of alcohol use (e.g. Cadigan, Martens, & Herman, 2015; Camatta & Nagoshi, 1995; Martens et al., 2008), and PTSD symptoms were associated with increased alcohol-related consequences (Breslau, Davis, Peterson, Schultz, 1997; Miller, Vogt, Mozley, Kaloupek, & Keane, 2006; Ouimette, Brown, & Najavits, 1998; Read, Colder, Merrill, Ouimette, White, & Swartout, 2012). A similar pattern of results was found by Ginzburg and colleagues (2010), who assessed over 600 Israeli male veterans and found those with a triple comorbidity of PTSD, depression, and anxiety, reported the greatest impairment in overall psychosocial functioning (i.e., decreased occupational performance and decreased functioning in domains related to family, social, interpersonal, and social independence). Although Ginzburg and colleagues (2010) did not assess alcohol use, it is possible that Israeli veterans’ alcohol use and related problems contributed to their psychosocial impairment.
Building on the existing literature reporting the co-occurrence of hazardous alcohol consumption and mental health difficulties (e.g., McDevitt-Murphy et al., 2015; Jakupcak et al., 2010), the current findings provide a more detailed understanding of this comorbid relationship. While we found evidence for profiles of veterans with hazardous alcohol use and co-morbid mental health symptoms (i.e., “Severe alcohol behavior” and “Steady drinkers with functional impairment” profiles), it is notable that, relative to the other profiles in this sample, the “Binge drinkers with no functional impairment” reported fewer mental health symptoms despite heavy alcohol use. Clinically, it is important to note that all mental health symptoms of the “Severe alcohol behavior” and “Steady drinkers with functional impairment” profiles exceeded their respective clinical cut-off levels on average. In contrast, symptoms of the “Binge drinkers with no functional impairment” did not reach a level of clinical significance.
Despite profound differences in quantity of alcohol use, the “Binge drinkers” and “Mild alcohol” profiles did not differ on any mental health symptomology. This suggests that for some Veterans, heavy drinking patterns (in terms of quantity/frequency) may not be comorbid with mental health difficulties or alcohol related problems. Although previous research with OEF/OIF Veterans has found a relationship between hazardous alcohol use and increased mental health symptoms (Barry, Whiteman, MacDermid Wadsworth, & Hitt, 2012; Mustillo et al., 2015), our findings show quantity/frequency of alcohol use alone is not related to mental health outcomes.
There are several implications for prevention and treatment based on the findings from the current study. Targeted interventions based on unique alcohol risk profiles may be helpful in tailoring prevention and intervention efforts in detecting co-occurring mental health symptoms among OEF/OIF veterans. Although a structured clinical interview was not used to assess criteria for diagnoses, from a treatment perspective it appears the “Severe alcohol behavior” profile is the most easily identifiable for intervention due to their heightened level of all alcohol risk indicators and subsequent heightened levels of mental health symptoms. This profile of veterans may benefit from treatment for comorbid alcohol use and PTSD (Carter, Capone, & Short, 2010) which has been shown to also reduce depression symptoms (Kaysen et al., 2014).
Although the “Steady drinkers with functional impairment” profile reported a low peak BAC and a relatively moderate number of drinks per week, they are the most impaired by alcohol-related problems. This suggests that although they are not reaching hazardous levels of alcohol use through patterns of binge drinking, and consequently may not be identified by brief alcohol screening measures (as opposed to both the “Severe alcohol behavior” and “Binge drinkers with no functional impairment” profiles), they do report significant impairment related to their alcohol consumption. These veterans may benefit from treatment options and areas of focus including harm reduction strategies to limit negative alcohol-related consequences, treatments for PTSD and depression, and improved general coping strategies.
It is possible the “Binge drinkers with no functional impairment” profile may not seek treatment as they report minimal life problems due to the effects of alcohol and subclinical symptoms of mental health problems. However, although they deny functional impairment, this group of veterans reaches significantly elevated BAC levels that place them at risk for alcohol-related blackouts. Early intervention efforts, such as brief alcohol interventions frequently used for college student binge drinkers (e.g., Carey, Scott-Sheldon, Elliott, Garey, & Carey, 2012), could assist this group in preventing future risk of alcohol-related consequences including development of alcohol use disorders.
There were several limitations to the current study. First, the study consisted of a relatively homogenous sample of White male veterans. Additionally, all mental health outcomes were highly correlated, with r’s ranging from .64 to .77. Instead of creating a composite mental health variable, we chose to include each individual external criterion (i.e., PTSD, depression, and anxiety) as they represent distinct mental health diagnoses. Additionally, previous studies have found evidence for a temporal sequencing of PTSD predicting an alcohol use disorder (Kehle et al., 2012; Kline et al., 2014; Jakupcak et al., 2010), which is consistent with a self-medication theory where alcohol is used to manage or reduce mental health symptoms. As results from the current study were cross-sectional, causal claims about the relationship between mental health symptoms and alcohol use cannot be made. Although we found the total score of PTSD symptoms to vary as a function of alcohol risk profile, we did not examine specific PTSD symptoms clusters (i.e., emotional numbing and hyperarousal symptoms) which have been shown to be uniquely associated with increased hazardous alcohol use (Jakupcak et al., 2010). We also relied on self-report measures of mental health and alcohol outcomes, although these diagnostic tools have shown strong psychometric properties (Babor, Steinberg, Anton, & Del Boca, 2000; Blanchard, Jones-Alexander, Buckley, & Forneris, 1996; Miller et al., 2002; Radloff, 1977).
Despite these limitations, the current study provides a unique understanding of veterans’ alcohol risk profiles and concurrent mental health symptoms. Our findings show veterans have distinct alcohol profiles and such profiles are associated with varying levels of comorbid mental health symptoms. This approach could be used to identify profiles of veterans who are particularly at-risk for both negative alcohol-related outcomes and mental health symptoms, and therefore candidates for targeted intervention efforts.
Highlights.
We examined alcohol risk profiles of OEF/OIF veterans
Profiles were associated with different severity of mental health symptoms
Interventions could target co-occurring alcohol risk and mental health symptoms
Acknowledgments
This project was supported by NIAAA grants R21AA020180 to Matthew P. Martens and F32AA025263 Jennifer M. Cadigan. This research is the result of work supported with resources and the use of facilities at the Harry S. Truman Memorial Veterans’ Hospital.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Alati R, Lawlor DA, Najman JM, Williams GM, Bor W, O’Callaghan M. Is there really a ‘j-shaped’ curve in the association between alcohol consumption and symptoms of depression and anxiety? Findings from the Mater-University Study of Pregnancy and its outcomes. Addiction. 2005;100:643–651. doi: 10.1111/j.1360-0443.2005.01063.x. [DOI] [PubMed] [Google Scholar]
- Arbuckle JL. Full information estimation in the presence of incomplete data. In: Marcoulides GA, Schumacker RE, editors. Advanced structural equation modeling: Issues and techniques. Mahwah, NJ: Erlbaum; 1996. pp. 243–277. [Google Scholar]
- Babor TF, Higgins-Biddle JC, Saunders JB, Monteiro MG. The Alcohol Use Disorders Identification Test: Guidelines for use in primary care. World Health Organization; Geneva: 2001. [Google Scholar]
- Babor TF, Steinberg K, Anton R, Del Boca F. Talk is cheap: Measuring drinking outcomes in clinical trials. Journal of Studies on Alcohol. 2000;61:55–63. doi: 10.15288/jsa.2000.61.55. [DOI] [PubMed] [Google Scholar]
- Barry AE, Whiteman S, MacDermid Wadsworth S, Hitt S. The alcohol use and associated mental health problems of student service members/veterans in higher education. Drugs: Education, Prevention and Policy. 2012;19:415–425. doi: 10.3109/09687637.2011.647123. [DOI] [Google Scholar]
- Blanchard EB, Jones-Alexander J, Buckley TC, Forneris CA. Psychometric properties of the PTSD Checklist (PCL) Behaviour research and therapy. 1996;34:669–673. doi: 10.1016/0005-7967(96)00033-2. [DOI] [PubMed] [Google Scholar]
- Breslau N, Davis GC, Peterson EL, Schultz L. Psychiatric sequelae of posttraumatic stress disorder in women. Archives of General Psychiatry. 1997;54:81–87. doi: 10.1001/archpsyc.1997.01830130087016. [DOI] [PubMed] [Google Scholar]
- Burnett-Zeigler I, Ilgen M, Valenstein M, Zivin K, Gorman L, Blow A. Prevalence and correlates of alcohol misuse among returning Afghanistan and Iraq veterans. Addictive Behaviors. 2011;36:801–806. doi: 10.1016/j.addbeh.2010.12.032. doi:10.1016.j.addbeh.2010.12.032. [DOI] [PubMed] [Google Scholar]
- Cadigan JM, Martens MP, Herman KC. A latent profile analysis of drinking motives among heavy drinking college students. Addictive Behaviors. 2015;51:100–105. doi: 10.1016/j.addbeh.2015.07.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Caldwell TM, Rodgers B, Jorm AF, Christensen H, Jacomb PA, Korten AE, Lynskey MT. Patterns of association between alcohol consumption and symptoms of depression and anxiety in young adults. Addiction. 2002;97:583–594. doi: 10.1046/j.1360-0443.2002.00092.x. [DOI] [PubMed] [Google Scholar]
- Calhoun PS, Elter JR, Jones ER, Kudler H, Straits-Troster K. Hazardous alcohol use and receipt of risk-reduction counseling among U.S. veterans of the wars in Iraq and Afghanistan. Journal of Clinical Psychiatry. 2008;69:1686–1693. doi: 10.4088/jcp.v69n1103. [DOI] [PubMed] [Google Scholar]
- Carey KB, Scott-Sheldon LA, Elliott JC, Garey L, Carey MP. Face-to-face versus computer-delivered alcohol interventions for college drinkers: a meta-analytic review, 1998 to 2010. Clinical Psychology Review. 2012;32:690–703. doi: 10.1016/j.cpr.2012.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carter AC, Capone C, Eaton Short E. Co-occurring posttraumatic stress disorder and alcohol use disorders in veteran populations. Journal of Dual Diagnosis. 2011;7:285–299. doi: 10.1080/15504263.2011.620453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Camatta CD, Nagoshi CT. Stress, depression, irrational beliefs, and alcohol use and problems in a college student sample. Alcoholism: Clinical and Experimental Research. 1995;19:142–146. doi: 10.1111/j.1530-0277.1995.tb01482. [DOI] [PubMed] [Google Scholar]
- Collins RL, Parks GA, Marlatt GA. Social determinants of alcohol consumption: The effects of social interaction and model status on the self-administration of alcohol. Journal of Consulting and Clinical Psychology. 1985;53:189–200. doi: 10.1037//0022-006x.53.2.189. [DOI] [PubMed] [Google Scholar]
- Eisen SV, Schultz MR, Vogt D, Glickman ME, Elwy AR, Drainoni M, … Martin J. Mental and physical health status and alcohol and drug use following return from deployment to Iraq or Afghanistan. American Journal of Public Health. 2012;102:S66–S73. doi: 10.2105/AJPH.2011.300609. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ginzburg K, Ein-Dor T, Solomon Z. Comorbidity of posttraumatic stress disorder, anxiety and depression: a 20-year longitudinal study of war veterans. Journal of Affective Disorders. 2010;123:249–257. doi: 10.1016/j.jad.2009.08.006. [DOI] [PubMed] [Google Scholar]
- Grant BF, Stinson FS, Dawson DA, Chou SP, Dufour MC, Compton W, … Kaplan K. Prevalence and co-occurrence of substance use disorders and independent mood and anxiety disorders: Results from the national epidemiologic survey on alcohol and related conditions. Archives of general psychiatry. 2004;61(8):807–816. doi: 10.1001/archpsyc.61.8.807. [DOI] [PubMed] [Google Scholar]
- Hawkins EJ, Lapham GT, Kivlahan DR, Bradley KA. Recognition and management of alcohol misuse in OEF/OIF and other veterans in the VA: A cross-sectional study. Drug and Alcohol Dependence. 2010;109:147–153. doi: 10.1016/j.drugalcdep.2009.12.025. [DOI] [PubMed] [Google Scholar]
- Heltemes KJ, Clouser MC, MacGregor AJ, Norman SB, Galarneau MR. Co-occurring mental health and alcohol misuse: Dual disorder symptoms in combat injured veterans. Addictive Behaviors. 2014;39:392–398. doi: 10.1016/j.addbeh.2013.06.001. [DOI] [PubMed] [Google Scholar]
- Hoge CW, Castro CA, Messer SC, McGurk D, Cotting DI, Koffman RL. Combat duty in Iraq and Afghanistan, mental health problems, and barriers to care. The New England Journal of Medicine. 2004;351:13–22. doi: 10.1056/NEJMoa040603. [DOI] [PubMed] [Google Scholar]
- Jakupcak M, Tull MT, McDermott MJ, Kaysen D, Hunt S, Simpson T. PTSD symptom clusters in relationship to alcohol misuse among Iraq and Afghanistan war veterans seeking post-deployment VA health care. Addictive Behaviors. 2010;35:840–843. doi: 10.1016/j.addbeh.2010.03.023. [DOI] [PubMed] [Google Scholar]
- Karstoft KI, Andersen SB, Bertelsen M, Madsen T. Diagnostic accuracy of the Posttraumatic Stress Disorder Checklist Civilian Version in a representative military sample. Psychological Assessment. 2014;26:321–325. doi: 10.1037/a0034889. [DOI] [PubMed] [Google Scholar]
- Kaysen D, Schumm J, Pedersen ER, Seim RW, Bedard-Gilligan M, Chard K. Cognitive Processing Therapy for Veterans with Comorbid PTSD and Alcohol Use Disorders. Addictive Behaviors. 2014;39:420–427. doi: 10.1016/j.addbeh.2013.08.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kehle SM, Ferrier-Auerbach AG, Meis LA, Arbisi PA, Erbes CR, Polusny MA. Predictors of postdeployment alcohol use disorders in National Guard soldiers deployed to Operation Iraqi Freedom. Psychology of Addictive Behaviors. 2012;26:42–50. doi: 10.1037/a0024663. [DOI] [PubMed] [Google Scholar]
- Khantzian EJ. The self-medication hypothesis revisited: The dually diagnosed patient. Primary Psychiatry. 2003;10:47–54. [Google Scholar]
- Kline A, Weiner MD, Ciccone DS, Interian A, St Hill L, Losonczy M. Increased risk of alcohol dependency in a cohort of National Guard troops with PTSD: A longitudinal study. Journal of Psychiatric Research. 2014;50:18–25. doi: 10.1016/j.jpsychires.2013.11.007. [DOI] [PubMed] [Google Scholar]
- Kroenke K, Spitzer RL, Williams JBW, Monahan PO, Lowe B. Anxiety disorders in primary care: Prevalence, impairment, comorbidity, and detection. Annals of Internal Medicine. 2007;146:317–325. doi: 10.7326/0003-4819-146-5-200703060-00004. [DOI] [PubMed] [Google Scholar]
- Little RJ. Modeling the dropout mechanism in repeated-measures studies. Journal of the American Statistical Association. 1995;90:1112–1121. [Google Scholar]
- Martens MP, Cadigan JM, Rogers RE, Osborn ZH. Personalized drinking feedback intervention for veterans of the wars in Iraq and Afghanistan: a randomized controlled trial. Journal of Studies on Alcohol and Drugs. 2015;76:355–359. doi: 10.15288/jsad.2015.76.355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martens MP, Martin JL, Hatchett ES, Fowler RM, Fleming KM, Karakashian MA, Cimini MD. Protective behavioral strategies and the relationship between depressive symptoms and alcohol-related negative consequences among college students. Journal of Counseling Psychology. 2008;55:535–541. doi: 10.1037/a0013588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McDevitt-Murphy ME, Fields JA, Monahan CJ, Bracken KL. Drinking motives among heavy-drinking veterans with and without posttraumatic stress disorder. Addiction Research & Theory. 2015;23:148–155. doi: 10.3109/16066359.2014.949696. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McDevitt-Murphy ME, Williams JL, Bracken KL, Fields JA, Monahan CJ, Murphy JG. PTSD symptoms, hazardous drinking, and health functioning among U.S. OEF and OIF veterans presenting to primary care. Journal of Traumatic Stress. 2010;23:108–111. doi: 10.1002/jts.20482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller ET, Neal DJ, Roberts LJ, Baer JS, Cressler SO, Metrik J, Marlatt GA. Test-retest reliability of alcohol measures: Is there a difference between internet-based assessment and traditional methods? Psychology of Addictive Behaviors. 2002;16:56–63. [PubMed] [Google Scholar]
- Miller WR, Tonigan JS, Longabaugh R. NIAAA Project MATCH Monograph Series. Vol. 4. Bethesda, MD: National Institute on Alcohol Abuse and Alcoholism; 1995. NIH Publication No. 95–3911. The Drinker Inventory of Consequences (DrInC): An Instrument for Assessing Adverse Consequences of Alcohol Abuse (Test Manual) [Google Scholar]
- Miller MW, Vogt DS, Mozley SL, Kaloupek DG, Keane TM. PTSD and substance-related problems: the mediating roles of disconstraint and negative emotionality. Journal of Abnormal Psychology. 2006;115:369–379. doi: 10.1037/0021-843X.115.2.369. [DOI] [PubMed] [Google Scholar]
- Mustillo SA, Kysar-Moon A, Douglas SR, Hargraves R, MacDermid Wadsworth S, Fraine M, Frazer NL. Overview of depression, post-traumatic stress disorder, and alcohol misuse among active duty service members returning from Iraq and Afghanistan, self-report and diagnosis. Military Medicine. 2015;180:419–427. doi: 10.7205/MILMED-D-14-00335. [DOI] [PubMed] [Google Scholar]
- Muthén LK, Muthén BO. Mplus User’s Guide. 7. Los Angeles, CA: Muthén & Muthén; 1998–2010. [Google Scholar]
- Muthén BO, Shedden K. Finite mixture modeling with mixture outcomes using the EM algorithm. Biometrics. 1999;6:463–469. doi: 10.1111/j.0006-341x.1999.00463.x. [DOI] [PubMed] [Google Scholar]
- O’Donnell K, Wardle J, Dantzer C, Steptoe A. Alcohol consumption and symptoms of depression in young adults from 20 countries. Journal of Studies on Alcohol. 2006;67:837–840. doi: 10.15288/jsa.2006.67.837. [DOI] [PubMed] [Google Scholar]
- Ouimette PC, Brown PJ, Najavits LM. Course and treatment of patients with both substance use and posttraumatic stress disorders. Addictive Behaviors. 1998;23:785–795. doi: 10.1016/S0306-4603(98)00064-1. [DOI] [PubMed] [Google Scholar]
- Radloff LS. The CES-D scale a self-report depression scale for research in the general population. Applied Psychological Measurement. 1977;1:385–401. doi: 10.1177/014662167700100306. [DOI] [Google Scholar]
- Radloff LS. The use of the Center for Epidemiologic Studies Depression Scale in adolescents and young adults. Journal of Uouth and Adolescence. 1991;20:149–166. doi: 10.1007/BF01537606. [DOI] [PubMed] [Google Scholar]
- Ramaswamy V, DeSarbo W, Reibstein D, Robinson W. An empirical pooling approach for estimating marketing mix elasticities with PIMS data. Marketing Science. 1993;12:103–124. [Google Scholar]
- Read JP, Colder CR, Merrill JE, Ouimette P, White J, Swartout A. Trauma and posttraumatic stress symptoms predict alcohol and other drug consequence trajectories in the first year of college. Journal of Consulting and Clinical Psychology. 2012;80:426–439. doi: 10.1037/a0028210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rodgers B, Korten AE, Jorm AF, Jacomb PA, Christensen H, Henderson AS. Non-linear relationships in associations of depression and anxiety with alcohol use. Psychological Medicine. 2000;30:421–432. doi: 10.1017/s0033291799001865. [DOI] [PubMed] [Google Scholar]
- Schwartz G. Estimating the dimensions of a model. The Annals of Statistics. 1978;6:461–464. [Google Scholar]
- Seal KH, Bertenthal D, Miner CR, Sen S, Marmar C. Bringing the war back home: Mental health disorders among 103-788 US veterans returning from Iraq and Afghanistan seen at Department of Veterans Affairs Facilities. Archives of Internal Medicine. 2007;167:476–482. doi: 10.1001/archinte.167.5.476. [DOI] [PubMed] [Google Scholar]
- Seal KH, Metzler TJ, Gima KS, Bertenthal D, Maguen S, Marmar CR. Trends and risk factors for mental health diagnoses among Iraq and Afghanistan veterans using Department of Veterans Affairs health care 2002–2008. American Journal of Public Health. 2009;99:1651–1658. doi: 10.2105/AJPH.2008.150284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith TC, LeardMann CA, Smith B, Jacobson IG, Miller SC, Wells TS, … Ryan M. Longitudinal assessment of mental disorders, smoking, and hazardous drinking among a population-based cohort of US service members. Journal of Addiction Medicine. 2014;8(4):271–281. doi: 10.1097/ADM.0000000000000050. [DOI] [PubMed] [Google Scholar]
- Spitzer RL, Kroenke K, Williams JB, Löwe B. A brief measure for assessing generalized anxiety disorder: the GAD-7. Archives of Internal Medicine. 2006;166(10):1092–1097. doi: 10.1001/archinte.166.10.1092. [DOI] [PubMed] [Google Scholar]
- Stecker T, Fortney J, Owen R, McGovern MP, Williams S. Co-occurring medical, psychiatric, and alcohol-related disorders among veterans returning from Iraq and Afghanistan. Psychosomatics. 2010;51:503–507. doi: 10.1176/appi.psy.51.6.503. [DOI] [PubMed] [Google Scholar]
- Stewart SH. Alcohol abuse in individuals exposed to trauma: A critical review. Psychological Bulletin. 1996;120:83–112. doi: 10.1037/0033-2909.120.1.83. [DOI] [PubMed] [Google Scholar]
- Wagner TH, Harris KM, Federman B, Dai L, Luna Y, Humphreys K. Prevalence of substance use disorders among veterans and comparable nonveterans from the National Health Survey on Drug Use and Health. Psychological Services. 2007;4:149–157. [Google Scholar]
- Weathers FW, Litz BT, Herman DS, Huska JA, Keane TM. The PTSD Checklist (PCL): Reliability, validity and diagnostic utility. Paper presented at the annual meeting of the International Society for Traumatic Stress Studies; San Antonio, TX. 1993. [Google Scholar]
- Wilk JE, Bliese PD, Kim PY, Thomas JL, McGurk D, Hoge CW. Relationship of combat experiences to alcohol misuse among U.S. soldiers returning from the Iraq war. Drug and Alcohol Dependence. 2010;108:115–121. doi: 10.1016/j.drugalcdep.2009.12.003. [DOI] [PubMed] [Google Scholar]