Abstract
Background:
The RxEACH trial was a randomized trial to evaluate the efficacy of community pharmacy-based case finding and intervention in patients at high risk for cardiovascular (CV) events. Community-dwelling patients with poorly controlled risk factors were identified and their CV risk reduced through patient education, prescribing and follow-up by their pharmacist. Perspectives of patients, family physicians and community pharmacists were obtained regarding pharmacists' identification and management of patients at high risk for CV events, to identify strategies to facilitate implementation of the pharmacist's expanded role in routine patient care.
Methods:
We used a qualitative methodology (individual semistructured interviews) with conventional qualitative content analysis to describe perceptions about community pharmacists' care of patients at high risk for CV events. Perceptions were categorized into macro (structure), meso (institution) and micro (practice) health system levels, based on a conceptual framework of care for optimizing scopes of practice.
Results:
We interviewed 48 participants (14 patients, 13 family physicians and 21 community pharmacists). Patients were supportive of the expanded scope of practice of pharmacists. All participant groups emphasized the importance of communication, ability to share patient information, trust and better understanding of the roles, responsibilities, accountabilities and liabilities of the pharmacist within their expanded role.
Interpretation:
Despite support from patients and changes to delivery of care in primary care settings, ongoing efforts are needed to understand how to best harmonize family physician and community pharmacist roles across the health system. This will require collaboration and input from professional associations, regulatory bodies, pharmacists, family physicians and patients.
Community pharmacists are well positioned to contribute to identification and management of chronic medical conditions such as hypertension, diabetes and cardiovascular disease (CVD).1 In Canada, legislative and regulatory changes have supported an expansion of a pharmacist's scope of practice.2 Depending on the province, because each province has its own body for registering and regulating pharmacy practice,2 pharmacists can renew, adjust, initiate or substitute prescriptions, as well as order and interpret laboratory tests.
The current pharmacy legislation has provided pharmacists an opportunity to overcome the classic barriers (time constraints, limited remuneration models and low public expectations) to implementing the expanded scope of practice.3 Indeed, pharmacists across many provinces provide medication management and vaccination services, as well as change drug dosage, formulation and renewing or extending prescriptions for continuity of care since the launch of this legislation (https://www.pharmacists.ca/pharmacy-in-canada/scope-of-practice-canada/). Recent studies have reported effective pharmacist interventions on individual risk factors such as hypertension, diabetes and dyslipidemia.4-6 The Alberta Vascular Risk Reduction Community Pharmacy Project: RxEACH trial7 was recently conducted to evaluate the efficacy of a community pharmacy-based case-finding and intervention program in patients at high risk for CVD. Findings of the trial indicated that compared with usual care, the pharmacist-based intervention significantly reduced the risk of cardiovascular (CV) events. In this intervention, pharmacists used a proactive case-finding strategy to identify patients based on their medications and risk factors. As a secondary objective of the RxEACH trial, we sought to identify perspectives of patients, family physicians and community pharmacists regarding pharmacists' identification and management of complex patients (namely adults at high risk for CVD) to identify strategies to facilitate implementation of the pharmacist's expanded role in routine patient care.
Methods
Study design and participants
We used a qualitative descriptive design, a methodological approach that presents the facts in everyday terms as reported by participants, with no deeper interpretation of their experiences.8 Using purposive sampling, patients, physicians and pharmacists who participated in the RxEACH trial7 were eligible to participate in an individual semistructured telephone interview. A letter was sent to community pharmacists inviting them to participate and to identify patients and family physicians who were also involved in the study (to achieve a triad of patient, physician and pharmacist perspectives). After being approached by the pharmacists, interested patients and physicians were sent a letter of invitation describing the study and interview process. A snowball sampling strategy was also used to identify other family physicians outside the RxEACH trial, to obtain adequate representation of family physicians. Participants provided verbal informed consent.
Data collection
The interview guide for each participant group was developed based on a review of the literature2,9 and in consultation with the research team (pharmacists, nurses, family physicians and researchers) (Appendix 1, available at www.cmajopen.ca/content/5/1/E205/suppl/DC1), and was piloted with 4 community pharmacists. Questions generally focused on: skills and knowledge to manage patients at high risk for CVD (patients, physicians, pharmacists); changes in practice behaviour (physicians, pharmacists); communication/interaction (patients, physicians, pharmacists); and suggestions for sustainability (patients, physicians, pharmacists). Experienced qualitative interviewers (M.D., J.P. and P.L.: see acknowledgements) conducted the 20- to 30-minute interviews from September 2015 to May 2016. All interviews were audio-recorded and transcribed verbatim. Field notes were recorded at the time of the interview and used to inform data analysis. Recruitment and interviews were continued until the research team was satisfied that the data indicated saturation (i.e., similar emerging themes).
Data analysis
Conventional qualitative content analysis10 was used. The 3 interviewers (M.D., J.P. and P.L.) independently categorized data based on a conceptual framework of care for optimizing scopes of practice. The framework identifies factors at 3 health system levels: macro (legal and regulatory, education and training, economic and political); meso (institutional, technological and community); and micro (team composition and professional cultures).11 Transcripts were initially read to acquire an overall sense of the phenomenon of interest. Words and phrases that captured key concepts were highlighted to create codes, which identified evolving themes and subthemes. Data analysis and collection were done iteratively so that interview questions could be altered to enhance clarity of emerging themes. Final themes were determined through a series of discussions with the research team members; consensus on final themes was achieved.
Ethics approval
The Conjoint Health Research Ethics Board, University of Calgary, approved this study.
Results
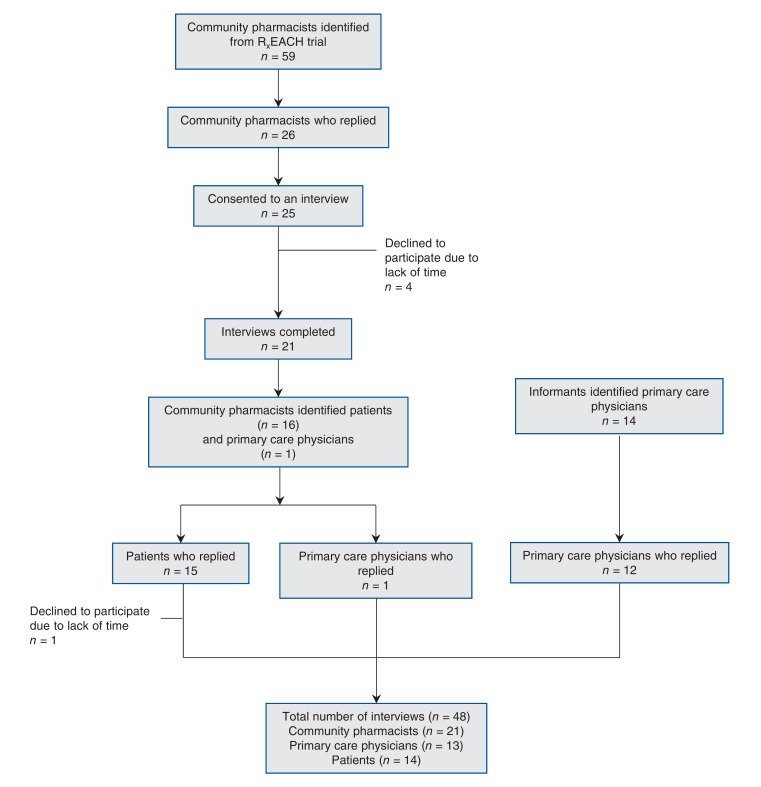
A total of 48 participants (14 patients, 13 family physicians and 21 community pharmacists) were interviewed (Figure 1). One physician was identified by a pharmacist, while the other 12 physicians (who care for patients at high risk for CVD but were not involved in the RxEACH trial) were identified by key informants (members of the research team, and then subsequent physician participants). Demographics for each of the participant groups are presented in Table 1 and Table 2. One triad of participants (patient, physician and pharmacist), 8 dyads (patient and pharmacist) and the remaining pharmacists and patients (who were not part of a family physician or community pharmacist unit from the RxEACH trial) were interviewed. An overview of barriers, enablers and selected quotations are provided (Box 1, Box 2, Box 3, Box 4 and Box 5).
Figure 1.
Participant recruitment.
Table 1: Characteristics of community pharmacists (n = 21) and family physicians (n = 13).
| Characteristic | No. (%) |
|---|---|
| Community pharmacists | |
| Sex | |
| Male | 9 (42.8) |
| Age group, yr | |
| ≤ 35 | 7 (33,3) |
| 36-45 | 9 (42.8) |
| 46-64 | 5 (23.8) |
| ≥ 65 | 0 (0.0) |
| Years in practice | |
| ≤ 10 | 9 (42.8) |
| 11-20 | 7 (33.3) |
| 21-30 | 4 (19.0) |
| ≥ 31 | 1 (4.8) |
| Practice location | |
| Urban | 12 (57.1) |
| Rural | 9 (42.8) |
| Practice type | |
| Independent (not affiliated with any corporately run banner) | 9 (42.8) |
| Banner (independent pharmacy affiliated with a central office) | 2 (9.5) |
| Chain (head office directs pharmacy practice) | 10 (47.6) |
| Employment status | |
| Full-time | 17 (80.9) |
| Part-time | 4 (19.0) |
| Pharmacist status | |
| Owner | 7 (33.3) |
| Employee | 14 (66.7) |
| Family physicians | |
| Sex | |
| Male | 7 (53.8) |
| Years in practice | |
| ≤ 10 | 0 (0.0) |
| 11-20 | 3 (23.1) |
| 21-30 | 7 (53.8) |
| ≥ 31 | 3 (23.1) |
| Practice location | |
| Urban | 10 (76.9) |
| Rural | 3 (23.1) |
Table 2: Characteristics of patients (n = 14).
| Characteristic | No. (%) |
|---|---|
| Sex | |
| Male | 7 (50.0) |
| Female | 7 (50.0) |
| Age group (yr) | |
| ≤ 50 | 2 (14.3) |
| 51-60 | 4 (28.6) |
| 61-70 | 6 (42.8) |
| 71-80 | 1 (7.1) |
| ≥ 81 | 1 (7.1) |
| Residence location | |
| Urban | 8 (57.1) |
| Rural | 6 (42.8) |
| Comorbidities | |
| Diabetes | 12 (85.7) |
| Chronic kidney disease | 8 (57.1) |
| Previous cardiovascular disease | 5 (35.7) |
| Hypertension | 14 (100.0) |
| Smoking | 2 (14.3D) |
Box 1: Macro (structure) level issues reported by patients, family physicians and community pharmacists.
• Health care professional accountability and liability: "You recognize things that you wanted to change and it was hard to sometimes get the doctors on board to make the change, to let either myself be in control of it or they want to be in control of it" (Pharmacist)
"Unclear and simply don't know what guidelines pharmacists adhere to" (Physician)
• Health care compensation and funding models: "Duplication of comprehensive care plans are seen as particularly wasteful, as is the involvement of a diabetic educator at the pharmacy when diabetic education has already been provided" (Physician)
"Expanded scope, the added services, they (pharmacists) were doing it because they wanted to, because it is the right thing to do, felt patients would benefit from it, and now there is a big push basically do it so that you can bill" (Pharmacist)
• Professional education needs and requirements: "They don't feel adequately trained, I don't think they feel competent to be doing this and my worry is that it'll be the people (pharmacists) who don't know what they don't know" (Physician)
"Wonderful thing to have the pharmacist do it as long as they know what they're doing and that they're educated" (Patient)
• Community pharmacy business models: "It's very difficult to do this (clinical) work because you still have to dispense medication, income comes from dispensing" (Pharmacist)
• Professional and regulatory bodies: "It's going to take undeniably, leadership from both the College of Physicians and Surgeons and the College of Pharmacists" (Pharmacist)
Box 2: Macro (structure) level enablers reported by patients, family physicians and community pharmacists.
• Educate professionals and public on changes to pharmacists' expanded scope of practice; provide guidance regarding quality assurance framework for all professionals; ensure professional accountability: "We have to communicate that we're not trying to take their (physician) jobs, we're just trying to do a better job for the patients" (Pharmacist)
"Prove to the public what their pharmacists are making a difference, especially in cardiovascular" (Pharmacist)
"Have the pharmacists do it as long as they know what they're doing, he has gone through what they need to do" (Patient)
• Standardize funded services across all jurisdictions; implement audit process: "I think right from the get go there should be some Blue Cross audits, professional services billing, which initially when they came out there wasn't - the government was paying for all this stuff" (Pharmacist)
"Being a pharmacy owner, call backs and audits and the challenge I have is making sure that the work I'm doing pleases everybody involved" (Pharmacist)
• Provide continuing professional development for pharmacists; implement interprofessional education: "More confidence and respect for recommendations that I would be making, whereas maybe a year ago they (physicians) would be like, well I'm not sure if I believe that, whereas now I have a physician standing beside me" (Pharmacist)
"More pharmacist directed - maybe some sort of basic diagnostic type courses or ongoing that would help focus or specialize in other areas" (Pharmacist)
"Learning it in school, but in real life you have to just get out and do it, and even just a couple of programs that would be available - get a useful skill" (Pharmacist)
• Support pharmacists to provide higher quality clinical services: "We had to convince head office … prove that this time and med review services actually benefits them" (Pharmacist)
"The patient is the most important person, the patient is the driver - marrying clinical services with production" (Pharmacist)
• Representation of the interests of the professionals to support interprofessional practice: "We need somebody to advocate, we need avocation, we need someone to say you're not there yet" (Pharmacist)
"I think in the future definitely recommend shared learning and brainstorming about strategies and things, on a quarterly or twice yearly basis just to keep everybody engaged" (Pharmacist)
Box 3: Meso (institutional) level issues and enablers reported by family physicians.
• Information management across multiple care settings: "Find that errors get propagated in the electronic medical records (EMRs) so I've changed writing records, I've had a lot more queries and feedback just because of EMR problems" (Physician)
• Implement and upkeep of shared EMRs: "Always a bit of a search when it comes to clinical data, moving forward it would be nice if we had EMRs built into pharmacy software" (Physician)
Box 4: Micro (practice) level issues reported by patients, family physicians and community pharmacists.
• Communication between pharmacists and family physicians: "In the absence of effective communication we (physicians) can feel overwhelmed by the large volumes of faxes, notes" (Physician)
• Role clarity: "I had great concerns when it (expanded scope of practice) came on the radar, sounded as though they would be presuming to diagnose and initiate therapy and medication which I wasn't sure that was appropriate" (Physician)
"This is a little beyond what I thought they do, but I know they are well educated and stuff" (Patient)
• Trusting relationships: "We had that relationship going into it (expanded scope of practice) and we continue that relationship, there's mutual respect for what we can do" (Pharmacist)
" … I have a number of people that are looking after me which gives a lot of confidence and relaxation when you know your being taken care of" (Patient)
• Access: "The closer they (pharmacist) are the more regular the interaction is - hallway consultations, the more relationship you have built, the more trust each other and the less friction there is around decision making" (Physician)
" … A lot more closer contact with your pharmacist than you do with your doctor…can get in to see your pharmacist without an appointment … " (Patient)
• Workplace environment and workforce: "I couldn't imagine being in a pharmacy with 10 people with only 1 person doing this (expanded scope of practice), I think it would be very difficult" (Pharmacist)
Box 5: Micro (practice) level enablers reported by patients, family physicians and community pharmacists.
• Ensure adequate, timely and reciprocal communication: "You need to work on your relationships, communicate with them (family physicians) in a way that they like, send them follow-ups when you promise" (Pharmacist)
"They (physician, pharmacist) connect back and forth by whatever it is, by email or faxes, so they're both aware of what is going on" (Patient)
• Acknowledge that pharmacists have expertise and provide valuable services; function as team to co-manage patient: "They are consulted often, appreciated for their expertise, and provide numerous educational services since their credentials, training and scope of practice are well known and well defined" (Physician)
"Doctors can't be experts on everything, refer to somebody that is more knowledgeable" (Patient)
" … He (pharmacist) didn't just prescribe drugs for us, he explained them and explained things that we could do the help ourselves … he keeps us very involved and knowledgeable." (Patient)
• Recognize pharmacist's qualifications and training; invest time and effort in getting to know each other: "We have more and more trust with each other and communication and from patient's feedback, they get more information about the problem and self-management, also about testing" (Physician)
"Doctors should diagnose and pharmacists should prescribe - they (pharmacists) know their drugs, know interactions, so I want their opinion, knowledge" (Patient)
• Colocate or identify pharmacy/pharmacist in close physical proximity; easy and open access to pharmacist: "A lot more closer contact with your pharmacist than you do with your doctor … can get in to see your pharmacist without an appointment" (Patient)
• Support for pharmacist autonomy for expanded scope of practice; provide appropriate space and equipment to do clinical assessments: "I am the owner/manager, so I redesigned my workflow so the technical work is being handled by technicians, I'm just getting involved in the clinical part of interacting with the patient" (Pharmacist)
"Going forward having a bit more prepopulation of information, some better tools that work on computers" (Pharmacist)
Macro (structure) level
Health care professional accountability and liability
All 3-participant groups identified concerns about liability and "lack of clarity" regarding who was responsible and ultimately accountable for adverse patient outcomes, should they occur. Physicians expressed concern that they may be left "holding the bag" if a patient problem arose. Physicians and pharmacists were concerned about possible differences between standards of practice based on their regulatory bodies and jurisdictions. Participants identified strategies to overcome this including education of health care professionals and the public regarding the pharmacists' expanded scope of practice and providing a quality assurance framework for health care professionals.
Health care compensation and funding models
Some physicians and pharmacists felt that the current model did not support comanagement, with potential duplication of services and "potential waste of health care dollars." They thought both parties should not be compensated for the same service to a patient (e.g., comprehensive annual care plan for chronic disease management). To address this barrier, participants recommended that funding for services should be monitored and standardized across jurisdictions, with an audit process to reduce potential duplication.
Professional education needs and requirements
Both physicians and pharmacists identified that not all pharmacists "embrace the expanded scope of practice." However, those who did showed higher clinical confidence and have typically established a "network of support." Pharmacists also identified the need for continuing education, particularly in management of patients with multiple comorbidities. Both physicians and pharmacists supported interprofessional education.
Community pharmacy business model
Pharmacists reported difficulties balancing their requirements to "perform as an employee" within an often corporate business model with the capacity to deliver high-quality expanded services. Physicians questioned whether there may be conflict of interest for pharmacists who prescribe and dispense medications, "pushing products due to business agenda." Pharmacists reflected on the importance of having the support of the larger pharmacy chains as a mechanism to enable pharmacists to function in their expanded role.
Professional and regulatory bodies
Both physicians and pharmacists identified lack of engagement, guidance and support from their representative professional colleges and associations. They expressed the need for all parties to promote a team-based approach for patient care. Similarly, a key enabler identified was having support of their professional organizations and regulatory bodies for interprofessional practice.
Meso (institutional) level
Patient information management across multiple care settings
All 3-participant groups identified the need for sharing patient information across care settings, ideally through an electronic health record. Patients reported that access to their health information would allow them to take more responsibility for their health. Physicians expressed concern that patients may be at risk when pharmacists made medication changes without a complete patient history. All groups identified that "mixed messaging" may occur and result in patient confusion and "eroding" of the care plan. Patients, physicians and pharmacists uniformly agreed that implementation of shared electronic medical records would facilitate an integrated model of care.
Micro (practice) level
Patient satisfaction
Patients reported appreciation for care from a team, highlighting the pharmacist's pivotal role. They indicated that pharmacists allowed them to take more responsibility in their care and spent time explaining their treatment plan and answering questions. Patients appreciated the compassion that pharmacists showed.
Communication between physicians and pharmacists
All 3-participant groups identified absence of effective communication between physicians and pharmacists. Physician and pharmacist groups reported the importance of a "consistent and effective" means of communication, whether face to face, or through fax, phone or electronic means. Some patients also perceived that physicians and pharmacists did not communicate well based on "mixed messages" about recommended medications. Potential enablers included the importance of physician-pharmacist collaboration through timely and effective communication.
Role clarity
Patients and physicians reported lack of clearly defined roles and understanding of the expanded scope of practice for pharmacists Patient and physician participants who had a better understanding reported a "greater appreciation" of the potential benefits. Recognizing that pharmacists can contribute to the interdisciplinary care of patients in the community setting was identified as an enabler.
Trusting relationships
Patients' trust in their pharmacists stemmed from their "existing, long-term relationship" with the pharmacist. Patients and physicians identified the need to be aware of pharmacists who were able to provide expanded role services. This information could be made public by "creating a registry of certified pharmacists." The importance of "investing time and effort in forming relationships" with each other was also highlighted. Physicians considered personal contact with pharmacists as a starting point for a collaborative relationship.
Access
Both patients and physicians commented on the importance of close proximity and timely access to pharmacists. Physicians reported that when the pharmacist was located nearby it lent itself to convenient, brief and frequent consults about patients - "the pharmacy next door" or "in-house" pharmacist (in-team setting). Patients appreciated not having to make an appointment with the pharmacist to get medication adjustments or laboratory results, and the time pharmacists spent with them.
Workplace environment and workforce
Pharmacists reported the importance of having "up-to-date medical equipment, computers with adequate software, as well as support staff and counseling rooms" to assist them in their expanded scope.
Interpretation
Changes to the scope of practice of pharmacists are changing the way primary care is delivered in Canada. Using qualitative methodology, we identified key issues to optimizing the pharmacist's expanded scope of practice for patients at high risk for CVD. To facilitate the delivery of patient-centreed care, it is important to understand perceptions of patients, family physicians and community pharmacists. Patient participants were very supportive of the expanded scope of practice model, and reported that they received timely access to a qualified professional who they trusted. At all levels of the health care system (macro, meso and micro), the importance of communication, ability to share patient information, trust and better understanding of the roles, responsibilities, accountabilities and liabilities of pharmacists within their expanded role of practice was emphasized. Physicians and pharmacists recognized that shared care should be patient-centred, and that to implement this model of care effectively, all parties will need to embrace the notion of a collaborative care model.
As previously reported,9 a core concept that evolved was the need for better communication, with enhanced 2-way electronic communications through electronic health records to facilitate real-time and reciprocal relay of information about patient care. Effective and shared communication would enable physicians to be notified about modifications or initiation of therapy, and similarly for pharmacists to be aware of changes to patients' health status and therapy as provided by the family physician. The potential for communication to be facilitated through colocation has also been recognized.12,13
At the micro level, the importance of role clarity and trusting relationships was highlighted. Hatah and colleagues also reported lack of understanding by general practitioners regarding pharmacists' roles.14 We found that some of the RxEACH patients were cautious about the pharmacist's role initially, but with ongoing interaction they were receptive to this model of care. Although community pharmacists hold liability insurance,2 the lack of a clear understanding of accountability and liability was identified as a potential barrier by patients and physicians in our study. The Canadian Medical Protective Association has outlined liability issues, and indicate that each member of the health care team in an interprofessional model of care is potentially liable for his or her actions.15 The importance of trust and mutual respect between physicians and pharmacists was emphasized by participants, with similar findings from Saskatchewan16 and Australia.14,17 Gregory and Austin identified that pharmacists and family physicians have different concepts of trust and that they are inherently different.18 Strategies to achieve trust and mutual respect may include the use of interprofessional education between family physicians and community pharmacists.19 Indeed, universities across Canada are beginning to offer opportunities where students from across health care faculties train together to prepare for collaborative and interprofessional roles in the clinical setting.2
Limitations
We identified participants from Alberta using purposive and snowball sampling strategies, thus their experiences are reflective of health care delivery in Alberta, which may limit generalizability. However, considering the universal nature of health care in Canada, there is no reason to believe these results are not relevant to other provinces, particularly those with similar expanded pharmacist roles. Although attempts were made to include family physicians who were involved in the care of patients in the RxEACH trial,7 consent was obtained from only 1 physician who fulfilled this criterion. The remainder of the physicians were identified through a purposive, snowball sampling technique. However, all interviewed physicians were practising in a setting that included patients at high risk of CVD, and thus their perspectives would be relevant and representative of family physicians, although they would not have the benefit of seeing firsthand the experience of patients managed through the RxEACH trial. Patient participants were identified by the pharmacists, as requested by our ethics board. Although pharmacists may have selected patients who were more satisfied with the expanded scope of practice, the wide range of patient responses suggests this is unlikely. As is common in all studies of this nature, the results are representative of those who responded and completed the interviews. The family physicians who participated had all been in practice for at least 10 years. The extent to which this study incorporates the perceptions of family physicians who have just completed their training and are starting their practice cannot be determined.
Conclusion
Optimizing the scope of practice of health care professionals is key to transforming our health care system and delivering high-quality, patient-centred care. The expanded scope of pharmacists' practice is one such example where we can support patients in the community setting. Despite the support from the patients and the current regulations to enable the integration of pharmacists into routine clinical care, ongoing efforts are needed to understand how to best harmonize family physician and community pharmacist roles across the health system. This will require collaboration and input from professional associations, regulatory bodies, practising pharmacists, family physicians and patients.2
Supplemental information
For reviewer comments and the original submission of this manuscript, please see www.cmajopen.ca/content/5/1/E205/suppl/DC1
Supplementary Material
Acknowledgements
We thank all participants for sharing their thoughtful perspectives in this study. We thank Sarah Gil for her role in the recruitment process; Jo Anne Plested and Pam Leblanc for their assistance with data collection and analysis; and Connie Jolicoeur for her transcription services.
Footnotes
Disclaimer: The results presented in this paper have not been published previously in whole or part, except in abstract format. This research was supported by a team grant funded by Alberta Innovates-Health Solutions. The sponsors of the study had no role in study design, data collection, data analysis, data interpretation or writing of the report.
Funding: This study was funded by a team grant from Alberta Innovates-Health Solutions.
References
- 1.Shiu J, Simpson SH, Johnson JA, et al. Quantifying opportunities to affect diabetes management in the community. Can Pharm J. 2006;139:37–8. [Google Scholar]
- 2.Tannenbaum C, Tsuyuki RT. The expanding scope of pharmacists' practice: implications for physicians. CMAJ. 2013;185:1228–32. doi: 10.1503/cmaj.121990. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Rosenthal M, Austin Z, Tsuyuki R. Are pharmacists the ultimate barrier to pharmacy practice change? Can Pharm J. 2010;143:37–42. [Google Scholar]
- 4.Tsuyuki RT, Houle SK, Charrois TL, et al. RxACTION Investigators. A randomized trial of the effect of pharmacist prescribing on improving blood pressure in the community: the Alberta clinical trial in optimizing hypertension (RxACTION). Circulation. 2015;132:93–100. doi: 10.1161/CIRCULATIONAHA.115.015464. [DOI] [PubMed] [Google Scholar]
- 5.Tsuyuki RT, Rosenthal M, Pearson GJ. A randomized trial of a community-based approach to dyslipidemia management: pharmacist prescribing to achieve cholesterol targets (RxACT Study). Can Pharm J (Ott) 2016;149:283–92. doi: 10.1177/1715163516662291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Al Hamarneh YN, Charrois T, Lewanczuk R, et al. Pharmacist intervention for gylcaemic control in the community (the RxING study). BMJ Open. 2013;3:e003154. doi: 10.1136/bmjopen-2013-003154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Tsuyuki RT, Al Hamarneh YN, Jones CA, et al. The effectiveness of pharmacist interventions on cardiovascular risk: the multicenter randomized controlled RxEACH trial. J Am Coll Cardiol. 2016;67:2846–54. doi: 10.1016/j.jacc.2016.03.528. [DOI] [PubMed] [Google Scholar]
- 8.Sandelowski M. Whatever happened to qualitative description? Res Nurs Health. 2000;23:334–40. doi: 10.1002/1098-240x(200008)23:4<334::aid-nur9>3.0.co;2-g. [DOI] [PubMed] [Google Scholar]
- 9.Morrison J. Expanded pharmacy practice: Where are we, and where do we need to go? Can Pharm J (Ott) 2013;146:365–7. doi: 10.1177/1715163513508914. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hsieh HF, Shannon SE. Three approaches to qualitative content analysis. Qual Health Res. 2005;15:1277–88. doi: 10.1177/1049732305276687. [DOI] [PubMed] [Google Scholar]
- 11.Nelson S, Turnbull J, Bainbridge L, et al. Optimizing scopes of practice: new models for a new health care system. Ottawa: Canadian Academy of Health Sciences. 2014. [Google Scholar]
- 12.Bardet JD, Vo TH, Bedouch P, et al. Physicians and community pharmacists collaboration in primary care: a review of specific models. Res Social Adm Pharm. 2015;11:602–22. doi: 10.1016/j.sapharm.2014.12.003. [DOI] [PubMed] [Google Scholar]
- 13.McGrath SH, Snyder ME, Dueñas GG, et al. Physician perceptions of pharmacist-provided medication therapy management: qualitative analysis. J Am Pharm Assoc (2003) 2010;50:67–71. doi: 10.1331/JAPhA.2010.08186. [DOI] [PubMed] [Google Scholar]
- 14.Hatah E, Braund R, Duffull S, et al. General practitioners' perceptions of pharmacists' new services in New Zealand. Int J Clin Pharm. 2012;34:364–73. doi: 10.1007/s11096-012-9617-3. [DOI] [PubMed] [Google Scholar]
- 15.Maxwell-Alleyne A, Farber A. Pharmacists' expanded scope of practice: professional obligations for physicians and pharmacists working collaboratively. Toronto; Ontario Medical Review. 2013. pp. 17–9.
- 16.Laubscher T, Evans C, Blackburn D, et al. Collaboration between family physicians and community pharmacists to enhance adherence to chronic medications: opinions of Saskatchewan family physicians. Can Fam Physician. 2009;55:e69–75. [PMC free article] [PubMed] [Google Scholar]
- 17.Van C, Costa D, Abbott P, et al. Community pharmacist attitudes towards collaboration with general practitioners: development and validation of a measure and a model. BMC Health Serv Res. 2012;12:320. doi: 10.1186/1472-6963-12-320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Gregory PA, Austin Z. Trust in interprofessional collaboration: perspectives of pharmacists and physicians. Can Pharm J (Ott) 2016;149:236–45. doi: 10.1177/1715163516647749. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Gallagher RM, Gallagher HC. Improving the working relationship between doctors and pharmacists: Is inter-professional education the answer? Adv Health Sci Educ Theory Pract. 2012;17:247–57. doi: 10.1007/s10459-010-9260-5. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.