Abstract
Objectives
1) Describe national patterns of chronic rhinosinusitis (CRS) care across academic and community practices. 2) Determine the prevalence of comorbid disorders in CRS patients, including nasal polyposis, allergic rhinitis, asthma and cystic fibrosis. 3) Identify demographic, clinical and practice type factors associated with endoscopic sinus surgery (ESS).
Study Design
Multisite cross-sectional study.
Setting
Otolaryngology’s CHEER national research network.
Subjects and Methods
A total of 17,828 adult patients with CRS were identified of which 10,434 were seen at community (59%, n=8 sites), and 7,394 at academic practices (41%, n=10 sites). Multivariate logistic regression was used to evaluate the association between demographic, practice type and clinical factors and the odds of patient undergoing ESS.
Results
Average age was 50.4 years, 59.5% of patients were female and 88.3% Caucasian. The prevalence of comorbid diseases was: allergic rhinitis (35.1%), nasal polyposis (13.3%), asthma (4.4%), and cystic fibrosis (0.2%). 24.8% of patients at academic centers underwent ESS compared to 12.3% at community sites. In multivariate analyses, nasal polyposis (OR 4.28), cystic fibrosis (OR 2.42) and academic site type (OR 1.86) were associated with ESS (p<0.001) while adjusting for other factors.
Conclusions
We describe practice patterns of CRS care, as well clinical as demographic, clinical factors associated with ESS. This is the first study of practice patterns in CRS utilizing the CHEER network and may be used to guide future research.
Keywords: CHEER, national research network, clinical practice guidelines, academic, community, chronic rhinosinusitis, sinus surgery, ESS, FESS, CRS, disease comorbidities
Introduction
Chronic rhinosinusitis (CRS) is one of the most common chronic diseases, with a reported prevalence of 2–16%.1 Its impact on patient quality of life and productivity are substantial,2,3 and carry an economic cost to the United States healthcare system of over $22 billion per year.4 Despite this burden, compared to other chronic diseases with similar prevalence like asthma and diabetes, CRS remains a relatively under-researched disease entity.5,6 Furthermore, a recent review of the evidence has revealed that the majority of research looking into CRS and sinus surgery mostly utilizes low-quality evidence, such as from retrospective studies that lack controls.7
As the number of sinus surgeries has grown to 250,000/year,8 a better understanding of the driving factors for surgery and variations in practice patterns is becoming more important. The balance of surgical vs. medical treatment of disease still being investigated, and we are just beginning to understand the relationship of CRS with its other frequent comorbid conditions, such allergic rhinitis and asthma, and how they impact the CRS disease management.9,10 In addition, there are recent suggestions that variations in sinus surgery and its extent may also be driven by some non-clinical factors, such as patient age, gender and surgeon experience.11,12 Meanwhile an important limitation has remained to the existing research findings – while most of the CRS patients are likely being cared for in the community practices, the majority of CRS research so far has been based on patients and outcomes from academic centers. In this work we aim to describe some of the clinical and surgical patterns of chronic rhinosinusitis (CRS) care. We explore the differences between academic and community practices and hypothesize that patient demographic and clinical factors vary by practice setting.
The recently updated 2015 Clinical Practice Guidelines (CPGs) on adult sinusitis released by the American Academy of Otolaryngology present a number of recommendations with the goal of improving quality of care.13 Pertinent recommendations (Statements 7B, 8 and 10) suggest assessing CRS patients for disease modifying comorbid conditions, as well as using nasal endoscopy for objective confirmation of the disease. We explore the prevalence of these co-morbid conditions, and frequency of sinus endoscopy use within our study population. Similarly, we utilize our study population to examine which demographic, clinical, and practice type variables are associated with increased odds of undergoing endoscopic sinus surgery (ESS). This may help to develop a patient profile with demographic and clinical factors, which may be associated with increased odds of undergoing ESS.
National practice-based research networks incorporate a variety of practice settings and as such enable research questions to be explored across a diverse array of patients, providers, and practices, thus culminating in research findings that are more generalizable. They also serve as a tool for assessing quality of care, and are crucial to coordinating multi-institutional studies.14–16 The CHEER (Creating Healthcare Excellence through Education and Research) network is the only national research network in otolaryngology, and has grown to encompass over 30 academic and community sites in 19 states.17,18 It has been tested and validated in multiple disorders cared for by otolaryngologists.19–25 Thus the CHEER network may be perfectly suited to conduct future prospective and retrospective multi-center trials in CRS and yield new discoveries. This is the first study of CRS within the national research network.
Methods
Dataset and Patient Selection
This is a multisite cross-sectional study within the CHEER research network. The study was granted approval as exempt research by the Duke University Medical Center Institutional Review Board. The Retrospective Data Collection (RDC) component of CHEER was developed as a site capacity descriptor database for CHEER to facilitate feasibility analyses of proposed projects for the network. Participating sites have contributed one-year of patient data (either 2011–2012 or 2012–2013) encompassing all patient encounters. This includes patient demographic, diagnostic and procedure data. An interim summary of the RDC project and details about the network are posted at www.cheerapplied.org. At time of this analysis, the RDC project was complete in 22 sites and contained 277,519 unique patients.
Variable Definitions
The cohort included all adult patients (>=18 years of age) with an ICD-9 diagnosis code for CRS (473.X). We used CPT codes to define outcomes of interest including nasal endoscopy (CPT 31231) and ESS (CPT 31237, 31254, 31255, 31256, 31267, 31276, 31287, 31288). As expected, a single episode of sinus surgery often included having more than one procedure. We also captured relevant comorbid diseases of CRS that are important to consider in this population. These included nasal polyposis (ICD-9 471.0, 471.1, 471.8, 471.9); allergic rhinitis (ICD-9 477.0, 477.1, 477.2, 477.8, 477.9); asthma (ICD-9493.00, 493.01, 493.02, 493.10, 493.11, 493.12, 493.20, 493.21, 493.22, 493.81, 493.82, 493.90, 493.91, 493.92) and cystic fibrosis (ICD-9 277.00, 277.01, 277.02, 277.03, 277.09). We attempted to capture all codes that could represent a comorbid disorder to increase our sensitivity.
Statistical Analysis
Sites without demographic information (n=1) and sites that did not provide procedure codes (n=1) were excluded from the analysis. We built a multivariate logistic regression model to examine odds of patient undergoing ESS; with the dependent binary outcome variable being whether a patient underwent ESS. We explored predictor variables including: patient age (5-year intervals), gender, practice site type (academic vs. community), as well as presence of comorbid nasal polyposis, allergic rhinitis, asthma, or cystic fibrosis in our study cohort. Odds ratios and 95% confidence intervals (CI) were calculated and are reported with our results. Odds ratios for continuous variable age can be interpreted as the likelihood of ESS for every unit increase in age. The RDC data was analyzed using SAS v9.4 and JMP Pro 12.1 software.
Results
A total of 17,828 adult patients with CRS were identified of which 10,434 were seen at community (59%, n=8 sites), and 7,394 at academic practices (41%, n=10 sites). Average age for all patients was 50.4 years (SD 15.9). Overall, 59.5% of patients were female and 88.3% were Caucasian. There were a higher proportion of females (62% vs. 56%) and Caucasians (92% vs. 82%) seen at community practices (Table 1). A total of 1,831 patients (24.8%) underwent ESS at academic practices compared to 1,282 (12.3%) in community practices. We noted the breakdown by each endoscopic procedure type (Table 2). Patients at academic practices had more frontal (39%) and sphenoid sinus (22%) procedures during ESS, than patients seen at community practices – frontal (29%) and sphenoid (15%).
Table 1.
Patients with Chronic Rhinosinusitis within CHEER: Demographics and Clinical Characteristics
| All Sites (n=18) | Academic Sites (n=10) | Community Sites (n=8) | |
|---|---|---|---|
| Demographics | |||
| Patients | 17,828 | 7,394 | 10,434 |
| Visits | 47,111 | 20,262 | 26,849 |
| Visits per Patient – Mean (SD) | 2.6 (2.9) | 2.7 (2.9) | 2.6 (3.0) |
| Age – Mean (SD) | 50.4 (15.9) | 49.9 (15.9) | 50.7 (15.9) |
| Female % | 59.5% | 56.0% | 61.9% |
| Caucasian %1 | 88.3% | 81.7% | 91.7% |
| Disease Comorbidities | |||
| Allergic Rhinitis %(n) | 35.1% (6,265) | 8.8% (647) | 53.8% (5,618) |
| Nasal Polyposis % (n) | 13.3% (2,363) | 14.7% (1,088) | 12.2% (1,275) |
| Asthma % (n) | 4.4% (791) | 2.0% (146) | 6.2% (645) |
| Cystic Fibrosis%(n) | 0.2% (29) | 0.3% (23) | 0.1% (6) |
Race data was not available from all sites
Table 2.
Endoscopic Sinus Surgery Procedures in CRS Patients in CHEER Network, n=17,828
| Procedure Type | All Sites Patients (%) | Academic Sites Patients (%) | Community Sites Patients (%) |
|---|---|---|---|
| Endoscopic Sinus Procedure: | |||
| Polypectomy | 2,310 (71%) | 1,407 (76%) | 903 (63%) |
| Ethmoidectomy | 2,148 (66%) | 1,291 (70%) | 857 (60%) |
| Maxillary antrostomy | 2,088 (65%) | 1,107 (60%) | 981 (69%) |
| Frontal sinusotosmy | 1,126 (34%) | 711 (39%) | 415 (29%) |
| Sphenoidotoomy | 624 (19%) | 406 (22%) | 218 (15%) |
| Total | 3,270 | 1,846 | 1,424 |
Total patient count represents the number of unique patients. (%) Indicates percent of patients of total in each practice type category, which underwent a particular procedure.
Predictors of Endoscopic Sinus Surgery
A multivariate logistic regression model was built to examine the odds of a patient undergoing ESS, accounting for demographic, clinical and practice type covariates (Table 3). Figure 1 demonstrates the same findings using a forest plot. We observed that ESS was 0.82 times as likely to occur in women than men (OR 0.82; 95% CI: 0.76, 0.90, p<0.001). It is unclear why gender was associated with odds of ESS controlling for other covariates. It may be possible that CRS disease development may be influenced by gender, or likely there are other medical comorbidities that are influenced by gender that were not captured in our model. There was a decreasing trend for sinus surgery with age (OR 0.94; 95% CI: 0.92, 0.95, p<0.001), which represents the likelihood of ESS decreasing by 6.0% for every 5-year increase in age. However, plotting OR’s by age shows that only 40–44 group which is associated with decreased odds of ESS, and there are no clinically significant trends by age controlling for over covariates (Figure 2). Looking at site type as an independent variable, our results demonstrate that patients at an academic site were 1.86 times more likely to undergo ESS (95% CI: 1.70, 2.04, p<0.001). CRS patients with concurrent nasal polyposis had the highest odds ratio (OR 4.28, p<0.001) followed by cystic fibrosis (2.42, p=0.0237). Asthma was not a statistically significant factor (OR 1.08, p=0.470). Interestingly, allergic rhinitis was associated with the decreased odds of undergoing sinus surgery (OR 0.60; 95%CI: 0.54, 0.66, p<0.001).
Table 3.
Factors Associated with Patient Undergoing Endoscopic Sinus Surgery (ESS)
| Patient Variable [Reference] | Odds Ratio [95% CI] | P-Value |
|---|---|---|
| Age [based on a 5-year increase] | 0.94 [0.93, 0.95] | <0.001 |
| Sex [male] | 0.82 [0.76, 0.90] | <0.001 |
| Site Type [community] | 1.86 [1.70, 2.04] | <0.001 |
| Nasal Polyposis [no] | 4.28 [3.88, 4.72] | <0.001 |
| Allergic Rhinitis [no] | 0.60 [0.54, 0.66] | <0.001 |
| Asthma [no] | 1.08 [0.88, 1.34] | 0.47 |
| Cystic fibrosis [no] | 2.42 [1.13, 5.21] | 0.024 |
For continuous variable age odds ratios are interpreted as the likelihood of ESS for every unit increase (5-year interval).
Figure 1.
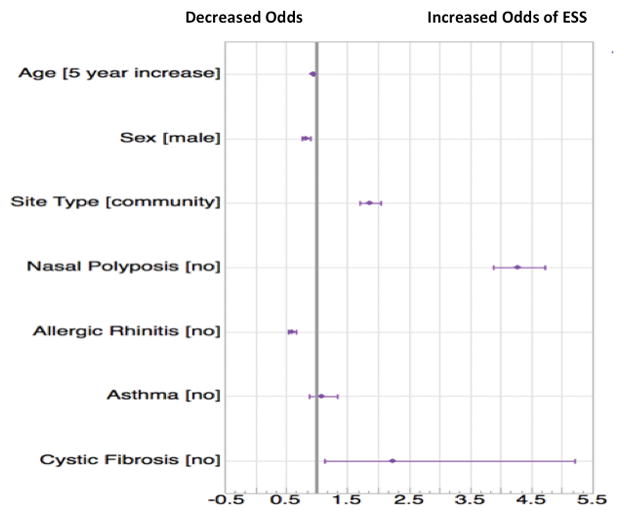
Forest plot with the odds ratios and 95% confidence intervals for each of the variables included in the model
Figure 2.
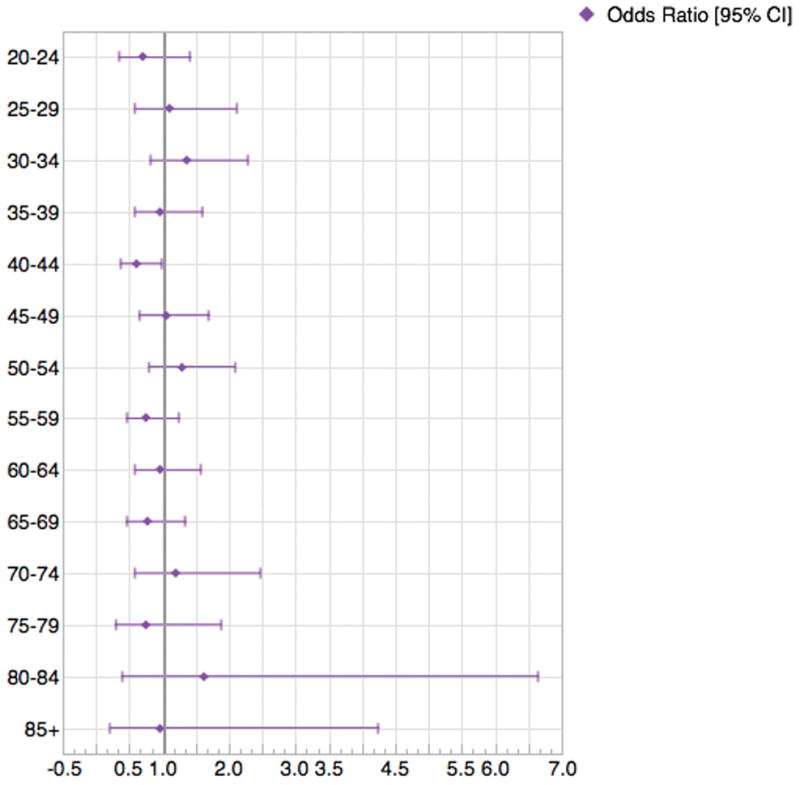
OR’s for a patient undergoing ESS by each age group and after adjusting for other covariates
CPGs recommend objective confirmation of disease with either endoscopy or CT for all patients with suspected CRS, and testing for disease modifying factors (Statements 7B, 8 and 10). 60.8% of patients with CRS had documentation of undergoing nasal endoscopy by associated CPT code. A number of CRS comorbid conditions were assessed in this study cohort and included nasal polyposis, asthma, allergic rhinitis, and cystic fibrosis with results presented in Table 1. Interestingly, the proportion of patients with comorbid diagnoses was similar between academic and community practices for all diagnoses except for allergic rhinitis. Allergic rhinitis was the most prevalent concurrent diagnosis, affecting 35.1% of all patients with chronic rhinosinusitis. We found that 54.8% of CRS patient in community sites had concurrent diagnosis of allergic rhinitis, compared to only 8.8% at academic practices. Nasal polyposis was present in 13.3% of all patients. Asthma was relatively uncommon (4.4%), and only 0.2% (29) patients had a concurrent diagnosis of cystic fibrosis.
Discussion
A unique feature of the CHEER research network is that it brings together academic and community otolaryngologists on a national scale and their associated patient populations to generate new discoveries. Our findings also suggest that patient demographics vary by practice type, namely there was a higher proportion of females and Caucasians seen at community practices (Table 1). As expected, the majority of CRS patients were treated at community practices. But despite treating fewer CRS patients, academic practices had a higher proportion of patients who underwent ESS (24.8% vs. 12.3%). Controlling for other clinical and demographic factors, our multivariate model demonstrated that academic site type was associated with increased odds of undergoing sinus surgery (Table 3; OR 1.86). One interpretation of this finding is that patients at academic centers are presenting with more extensive or medically refractive CRS disease. This may reflect referral practice patterns wherein most patients with CRS are initially seen at the community practices, and patients with more comorbid disease are referred by physicians or self-referred to academic centers. Alternatively, this may indicate that other socioeconomic factors not captured in our model may be associated with a patient undergoing ESS.
The balance of medical vs. ESS in CRS is an ongoing discussion among the otolaryngology research community. Usually, failure of maximal medical therapy prompts surgical management with ESS. Maximal medical therapy may be defined by weeks of broad-spectrum antibiotic therapy, nasal irrigations, allergy management and a short course of oral steroids.26 However, patient demographic and clinical factors as well as practice settings that may influence whether a patient undergoes sinus surgery are still uncertain. Controlling for other factors, our findings suggest that ESS is 17% less likely to occur in women than men p<0.001). The likelihood of surgery is also predicted to decrease by 6.0% for every 5-year increase in age. However, plotting OR’s by age and controlling for other covariates shows that only 40–44 group which is associated with decreased odds of ESS, and there are no clinically significant trends by age controlling for over covariates (Figure 2). A previous large study within the Medicare population showed a decreasing frequency of surgery in the 65- to 69-year-old patients compared to older age groups,11 but that study did not control for patient demographics and presence of disease comorbidities. Patients with CRS and comorbid nasal polyposis had the highest odds of undergoing ESS (OR 4.28, p<0.001) followed by patients with cystic fibrosis (OR 2.42, p=0.024). These findings are not surprising since nasal polyps may interfere with medical therapy and obstruct airflow, and often require surgical intervention.9 On the contrary, the diagnosis of allergic rhinitis was associated with decreased odds of needing sinus surgery, possibly due to the ability to successfully manage allergic sinus disease medically. CRS and allergic rhinitis have overlapping symptoms, and it is possible that some of the patients with CRS and allergic rhinitis may have clinical just had allergic rhinitis. This could contribute to the decreased odds of ESS for the allergic rhinitis covariate.
In 2015, the American Academy of Otolaryngology—Head and Neck Surgery Foundation released the updated Clinical Practice Guidelines (CPGs) on Adult Sinusitis, which included recommendations on CRS.13 In an effort to create actionable recommendations and improve quality the of CRS care, there was an emphasis on increasing the CRS diagnostic accuracy and assessing for chronic comorbid conditions that modify its management.13 It includes a strong recommendation for an objective documentation of sinonasal inflammation through imaging. Nasal endoscopy continues to serve as the gold standard for CRS diagnosis,27 and our study demonstrated that 60.8% of all patients underwent nasal endoscopy within 1 year of data. CT imaging was also likely used by the practices for disease confirmation. Unfortunately, since most of the CT imaging and billing were done in outside radiology departments we could not reliably use this as a variable.
With the pathophysiology of CRS still not entirely understood, there are suggestions in literature that contribution of frequent comorbid conditions may lead to disease that is refractory to the standard treatment.10 CPGs recommend that clinicians assess for multiple comorbid disorders that may modify the management of CRS, such as nasal polyposis, cystic fibrosis, asthma and allergic rhinitis.13 Our findings suggest that 13.3% of all patients with CRS had a comorbid diagnosis of nasal polyposis, asthma was seen in 4.4%, and cystic fibrosis was present in 0.2%. There were more CRS patients with comorbid allergic rhinitis in community practices (53.8%) compared to academic practices (8.8%). This is of interest, especially since there is an ongoing debate on possible role of allergy in development of CRS.28,29 This may represent a real difference in populations, or possibly indicate that academic practices may not commonly assess for allergic rhinitis and document it.
This study has several limitations. This work uses diagnostic and procedural codes, which lack specificity and depend on coding practices, and therefore should be used cautiously in drawing conclusions. There is variability in coding practices and some conditions like nasal polyposis and others may not be used by some physicians or practices. In interpreting the results, it is important to note that this data is limited to 1-year interval and our analysis is cross-sectional in design, although there are plans to soon expand the RDC database to include multiple years. Furthermore, our multivariate model was built to test associations and not to serve as a predictive model. Similarly, not all clinical and socioeconomic factors that likely influence management of CRS, such as income and insurance status were included in the analysis.
In conclusion, we describe clinical and surgical patterns of chronic rhinosinusitis across academic and community sites, and report the prevalence of common comorbid disorders in these patient populations. Furthermore, we assess for clinical and demographic patient variables that may be associated with increased odds of a patient undergoing endoscopic sinus surgery, which may help us understand the patient profile, specifically which demographic and clinical factors are associated with increased odds of undergoing ESS. Being aware of disease modifying conditions and their prevalence across different populations and practice setting may improve their recognition in clinical practice. This is also the first national study of CRS utilizing the CHEER network and proof of principle in utilizing the network for studying rhinologic disorders. These findings may be used to guide future research and clinical practice guideline assessment.
Acknowledgments
We thank all of the CHEER network sites that contribute data to the RDC. This study was supported by the NIDCD-funded CHEER infrastructure grant (1U24DC012206-01A1). Research reported in this publication was also supported by the National Center For Advancing Translational Sciences of the National Institutes of Health under Award Number TL1TR001116. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Footnotes
Sponsorships or competing interests that may be relevant to content are disclosed at the end of this article.
This article was presented at the 2016 AAO-HNSF Annual Meeting and OTO EXPOSM, San Diego, CA, September 18-21, 2016.
References
- 1.Halawi AM, Smith SS, Chandra RK. Chronic rhinosinusitis: epidemiology and cost. Allergy Asthma Proc. 2013;34:328–34. doi: 10.2500/aap.2013.34.3675. [DOI] [PubMed] [Google Scholar]
- 2.Soler ZM, Wittenberg E, Schlosser RJ, et al. Health state utility values in patients undergoing endoscopic sinus surgery. Laryngoscope. 2011;121:2672–78. doi: 10.1002/lary.21847. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Rudmik L, Smith TL, Schlosser RJ, Hwang PH, Mace JC, Soler ZM. Productivity costs in patients with refractory chronic rhinosinusitis. Laryngoscope. 2014;124:2007–12. doi: 10.1002/lary.24630. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Smith KA, Orlandi RR, Rudmik L. Cost of adult chronic rhinosinusitis: A systematic review. Laryngoscope. 2015;125:1547–56. doi: 10.1002/lary.25180. [DOI] [PubMed] [Google Scholar]
- 5.Rudmik L. Chronic rhinosinusitis: an under-researched epidemic. J Otolaryngol Head Neck Surg. 2015;44:11. doi: 10.1186/s40463-015-0064-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hopkins C, Rudmik L. Disparities in grant funding for Chronic rhinosinusitis. Laryngoscope. 2016;126:E136–40. doi: 10.1002/lary.25685. [DOI] [PubMed] [Google Scholar]
- 7.Smith TL, Batra PS, Seiden AM, Hannley M. Evidence supporting endoscopic sinus surgery in the management of adult chronic rhinosinusitis: a systematic review. Am J Rhinol. 2005;19:537–43. [PubMed] [Google Scholar]
- 8.Bhattacharyya N. Ambulatory sinus and nasal surgery in the United States: demographics and perioperative outcomes. Laryngoscope. 2010;120:635–638. doi: 10.1002/lary.20777. [DOI] [PubMed] [Google Scholar]
- 9.Luong A, Marple BF. Sinus surgery: indications and techniques. Clin Rev Allergy Immunol. 2006;30:217–22. doi: 10.1385/CRIAI:30:3:217. [DOI] [PubMed] [Google Scholar]
- 10.Rosati MG, Peters AT. Relationships among allergic rhinitis, asthma, and chronic rhinosinusitis. Am J Rhinol Allergy. 2016;30:44–7. doi: 10.2500/ajra.2016.30.4252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Venkatraman G, Likosky DS, Zhou W, Finlayson SR, Goodman DC. Trends in endoscopic sinus surgery rates in the Medicare population. Arch Otolaryngol Head Neck Surg. 2010;136:426–30. doi: 10.1001/archoto.2010.58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Pynnonen MA, Davis MM. Extent of sinus surgery, 2000 to 2009: a population-based study. Laryngoscope. 2014;124:820–5. doi: 10.1002/lary.24335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Rosenfeld RM, Piccirillo JF, Chandrasekhar SS, et al. Clinical Practice Guideline (Update): Adult Sinusitis. Otolaryngol Head Neck Surg. 2015;152(2 Suppl):S1–S39. doi: 10.1177/0194599815572097. [DOI] [PubMed] [Google Scholar]
- 14.Heintzman J, Gold R, Krist A, et al. Practice-based research networks (PBRNs) are promising laboratories for conducting dissemination and implementation research. J Am Board Fam Med. 2014;27:759–62. doi: 10.3122/jabfm.2014.06.140092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Westfall JM, Mold J, Fagnan L. Practice-Based Research--“Blue Highways” on the NIH Roadmap. JAMA. 2007;297:403–406. doi: 10.1001/jama.297.4.403. [DOI] [PubMed] [Google Scholar]
- 16.Bullmunt AM, Roberts R, Lee WT, et al. Does an Otolaryngology-Specific Database Have Added Value? A Comparative Feasibility Analysis. Otolaryngol Head Neck Surg. 2016;155:56–64. doi: 10.1177/0194599816651036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Tucci DL, Schulz K, Witsell DL. Building a national research network for clinical investigations in otology and neurotology. Otol Neurotol. 2010;31:190–5. doi: 10.1097/MAO.0b013e3181c9940c. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Witsell DL, Schulz KA, Moore K, Tucci DL CHEER Investigators. Implementation and testing of research infrastructure for practice-based research in hearing and communication disorders. Otolaryngol Head Neck Surg. 2011;145:565–71. doi: 10.1177/0194599811406369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Shin JJ. The Potential of Life within CHEER. Otolaryngol Head Neck Surg. 2016;155:3–4. doi: 10.1177/0194599816651073. [DOI] [PubMed] [Google Scholar]
- 20.Parham K, Chapurin N, Schulz K, et al. Thyroid Disease and Surgery in CHEER: The Nation’s Otolaryngology–Head and Neck Surgery Practice-Based Network. Otolaryngol Head Neck Surg. 2016;155:28–32. doi: 10.1177/0194599815627641. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Lee WT, Witsell DL, Parham K, et al. Tonsillectomy bleed rates across the CHEER practice research network: Pursuing guideline adherence and quality improvement. Otolaryngol Head Neck Surg. 2016;155:22–7. doi: 10.1177/0194599816630523. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Crowson MG, Schulz K, Parham K, et al. Meniere’s Disease: A CHEER Database Study of Local and Regional Patient Encounter and Procedure Patterns. Otolaryngol Head Neck Surg. 2016;155:15–21. doi: 10.1177/0194599815617752. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Misono S, Marmor S, Roy N, Mau T, Cohen SM. Multi-institutional Study of Voice Disorders and Voice Therapy Referral: Report from the CHEER Network. Otolaryngol Head Neck Surg. 2016;155:33–41. doi: 10.1177/0194599816639244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Piker EG, Schulz K, Parham K, et al. Variation in the Use of Vestibular Diagnostic Testing for Patients Presenting to Otolaryngology Clinics with Dizziness. Otolaryngol Head Neck Surg. 2016;155:42–47. doi: 10.1177/0194599816650173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Witsell DL, Khoury T, Schulz K, Stachler R, Tucci DL, Wojdyla D. Evaluation of Compliance for Treatment of Sudden Hearing Loss: A CHEER Network Study. Otolaryngol Head Neck Surg. 2016;155:48–55. doi: 10.1177/0194599816650175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Dautremont JF, Rudmik L. When are we operating for chronic rhinosinusitis? A systematic review of maximal medical therapy protocols prior to endoscopic sinus surgery. Int Forum Allergy Rhinol. 2015;5:1095–103. doi: 10.1002/alr.21601. [DOI] [PubMed] [Google Scholar]
- 27.Macdonald KI, Kilty SJ, van Walraven C. Chronic rhinosinusitis identification in administrative databases and health surveys: A systematic review. Laryngoscope. 2016;126:1303–10. doi: 10.1002/lary.25804. [DOI] [PubMed] [Google Scholar]
- 28.Krouse JH. Allergy and chronic rhinosinusitis. Otolaryngol Clin North Am. 2005;38:1257–66. doi: 10.1016/j.otc.2005.07.002. [DOI] [PubMed] [Google Scholar]
- 29.Georgalas C, Vlastos I, Picavet V, et al. Is chronic rhinosinusitis related to allergic rhinitis in adults and children? Applying epidemiological guidelines for causation. Allergy. 2014;69:828–33. doi: 10.1111/all.12413. [DOI] [PubMed] [Google Scholar]


