Abstract
Recent proposals for revisions to the 11th edition of the International Classification of Diseases (ICD-11) posttraumatic stress disorder (PTSD) diagnostic criteria have argued that the current symptom constellation under the Diagnostic and Statistical Manual of Mental Disorders-5 is unwieldy and includes many symptoms that overlap with other disorders. The newly proposed criteria for the ICD-11 include only six symptoms. However, restricting the symptoms to those included in the ICD-11 has implications for PTSD diagnosis prevalence estimates, and it remains unclear whether these six symptoms are most strongly associated with a diagnosis of PTSD. Network analytic methods, which assume that psychiatric disorders are networks of interrelated symptoms, provide information regarding which symptoms are most central to a network. We estimated network models of PTSD in a national sample of veterans of the Iraq and Afghanistan wars. In the full sample, the most central symptoms were persistent negative emotional state, efforts to avoid external reminders, efforts to avoid thoughts or memories, inability to experience positive emotions, distressing dreams, and intrusive distressing thoughts or memories; i.e., three of the six most central items to the network would be eliminated from the diagnosis under the current proposal for ICD-11. An empirically-defined index summarizing the most central symptoms in the network performed comparably to an index reflecting the proposed ICD-11 PTSD criteria at identifying individuals with an independently-assessed DSM-5 defined PTSD diagnosis. Our results highlight the symptoms most central to PTSD in this sample, which may inform future diagnostic systems and treatment.
Keywords: posttraumatic stress disorder, network analysis, ICD-11
General Scientific Summary
This study suggests that persistent negative emotional state, efforts to avoid external reminders, efforts to avoid thoughts or memories, inability to experience positive emotions, distressing dreams, and intrusive distressing thoughts or memories are important to the PTSD network. Findings were similar for men and women.
The Diagnostic and Statistical Manual of Mental Disorders (DSM) criteria for posttraumatic stress disorder (PTSD) have received criticism for including symptoms that overlap with many other mental disorders (e.g., anxiety disorders, mood disorders, dissociative disorders; Brewin, Lanius, Novac, Schnyder, & Galea, 2009; Rosen & Lilienfeld, 2008; Rosen, Spitzer, & McHugh, 2008). For example, PTSD and major depressive disorder (MDD) share several diagnostic criteria: sleep disturbance, difficulty concentrating, and anhedonia (American Psychiatric Association, 2013). Concerns about the extent to which the symptoms of PTSD overlap with symptoms of other mental disorders were renewed following publication of the fifth edition of the DSM (e.g., Brewin, 2013). In the fifth revision of the DSM (DSM-5), the number of PTSD symptoms was expanded from 17 to 20, and those that were added (i.e., distorted blaming of oneself or others, persistent negative emotional state, and self-destructive or reckless behavior) overlap with symptoms of other mental disorders. Critics have suggested that such syndromal indistinctiveness may not only inflate the estimated worldwide prevalence of PTSD but possibly undermine the validity of the PTSD diagnosis (Rosen, Lilienfeld, Frueh, McHugh, & Spitzer, 2010; Spitzer, Rosen, & Lilienfeld, 2008).
To address this persistent concern, some have suggested that these overlapping symptoms be eliminated from the PTSD diagnosis (e.g., Spitzer, First, & Wakefield, 2007). In contrast to the DSM-5’s 20 PTSD symptoms, the newly proposed PTSD criteria for the 11th edition of the International Classification of Diseases (ICD) include only six symptoms. In reducing the number of PTSD symptoms, the stated goals of the ICD-11 PTSD working group are to improve diagnostic utility (i.e., sensitivity and specificity) and decrease psychiatric comorbidity (Maercker et al., 2013). The six symptoms chosen by the ICD-11 working group (distressing dreams, dissociative reactions (flashbacks), efforts to avoid thoughts memories, efforts to avoid external reminders, hypervigilance, and exaggerated startle response) were assumed to be both core to the entity of PTSD and not shared by other psychiatric disorders (Cloitre, Garvert, Brewin, Bryant, & Maercker, 2013; Maercker et al., 2013). At least one re-experiencing symptom (distressing dreams or dissociative flashbacks), one avoidance symptom (efforts to avoid thoughts or memories or efforts to avoid external reminders), and one hyperarousal symptom (hypervigilance or exaggerated startle response), plus distress or impairment, is to be required for an ICD-11 PTSD diagnosis.
Recent empirical studies have found that restricting the symptoms to those included in the ICD-11 has important implications for the estimated prevalence of PTSD. For example, Hansen and colleagues (2015) found that 30.4% of participants with varying trauma exposure histories received DSM-5 PTSD diagnoses, but only 22.6% received ICD-11 diagnoses. Recently, Wisco and colleagues (2016) found past-month prevalence estimates of 3.7% for DSM-5 PTSD and 2.4% for ICD-11 PTSD in a U.S. community-based sample and 38.7% (DSM-5) and 34.4% (ICD-11) in a sample of trauma-exposed veterans. Across these samples and a third sample of US veterans and their intimate partners, 20.8–54.7% of participants meeting DSM-5 criteria for PTSD did not meet ICD-11 criteria; the main reasons for this discrepancy were lack of endorsement of distressing dreams or dissociative flashbacks and lack of endorsement of hypervigilance or exaggerated startle response despite endorsing other intrusion and alterations in arousal and reactivity symptoms that were sufficient for meeting the DSM-5 PTSD criteria (Wisco et al., 2016).
Although many PTSD symptoms overlap with symptoms of other mental disorders, many disorders, particularly mood and anxiety disorders, share symptoms (Byllesby, Charak, Durham, Wang, & Elhai, 2016; Watson, 2005; Zbozinek et al., 2012). Further, there are several important questions that need to be addressed before we can presume that the non-specific symptoms can or should be eliminated. First, we do not know if any non-specific symptoms are essential for a diagnosis of PTSD, i.e., the extent to which they have strong predictive value for diagnostic caseness. Second, we do not know which PTSD-specific symptoms are most central to the PTSD diagnosis, such that, by having strong connections with many other symptoms, the most central variables provide the most information about the other symptoms in the model. It remains unclear if the six symptoms chosen for inclusion in the ICD-11 are the most appropriate to reduce comorbidity with other diagnoses and to retain the most central features of the diagnosis; in other words, these six symptoms may not be the most essential symptoms of PTSD, nor are they necessarily more impairing than other PTSD symptoms that were not selected for inclusion under ICD-11. Although factor analytic studies of the ICD-11 PTSD criteria have generally found that this model fits the data well across samples (Hansen et al., 2015), these studies are unable to tell us if the symptoms chosen for inclusion in ICD-11 are those that best represent the diagnosis as currently defined.
Network analytic methods, previously used to examine connections between individuals and disease symptoms as well as actors associated via “degrees of separation” with Kevin Bacon (Barabasi, 2003; Barabasi & Oltvai, 2004; Brandes & Erlebach, 2005), were recently applied to the study of psychiatric symptoms and may help answer the question of which symptoms are the foundation of the PTSD diagnosis. Network models provide a visual representation of associations among variables and focus on direct associations among symptoms, an approach that aligns well with the theory that PTSD symptoms have direct causal effects on one another. For example, alterations in arousal and reactivity symptoms have been associated with emotional numbing (diminished interest in activities, detachment from others, inability to experience positive emotions; Litz et al., 1997). Also, it has been hypothesized that avoidance symptoms may develop as a consequence of intrusion symptoms (Creamer, Burgess, & Pattison, 1992). Thus, network models are a natural fit for the study of interrelationships among PTSD symptoms.
Network model results also provide information about which variables are most central to a given network. The only published network analysis of DSM-IV PTSD symptoms was conducted using a sample of 362 trauma-exposed Chinese adults, and findings revealed that difficulty concentrating, sleep disturbance, hypervigilance, and distressing dreams were highly central to the network (McNally et al., 2015). Importantly, only two of the proposed ICD-11 PTSD criteria (nightmares and hypervigilance) were identified as being most central to the network in this sample.
Item centrality results could be useful in determining which symptoms are most essential to a diagnosis of PTSD. Individuals with higher scores on the most central items should have higher overall PTSD severity scores and a greater likelihood of receiving a diagnosis of PTSD compared with individuals with lower scores. For example, in a study of complicated grief, change in the activation of highly central symptoms over time, relative to less central symptoms, was more strongly associated with naturalistic change in activation of the overall network (Robinaugh, Millner, & McNally, 2016). Symptoms with high centrality scores may be important targets for treatment, as addressing these symptoms would, in theory, affect the larger network and also inform which symptoms provide the most information about other symptoms in the network (van Borkulo et al., 2015). However, this proposition has not yet been tested.
Network model results may also be useful for examining comorbidity among psychiatric disorders. Symptoms shared by disorders may appear in the graphs as bridge symptoms, linking the two disorders (Borsboom & Cramer, 2013; Cramer, Waldorp, van der Maas, & Borsboom, 2010). Further, evaluating the extent to which the most central PTSD symptoms are also related to comorbid diagnoses (e.g., MDD) would partly address concerns regarding syndromal indistinctiveness. These findings could have important implications for the ICD-11 definition of PTSD, which purports to restrict PTSD symptoms to those not shared by other disorders.
An additional important point to address is the extent to which there are sex differences in models of PTSD or patterns of PTSD symptom endorsement. The lifetime prevalence of PTSD in the general U.S. adult population is more than twice as high among women (11.7%) as men (4.0%; Kessler, Petukhova, Sampson, Zaslavsky, & Wittchen, 2012), as is the 12-month prevalence (5.2% women, 1.8% men; Kessler, Chiu, Demler, Merikangas, & Walters, 2005). It is noteworthy, however, that sex differences in prevalence may depend on trauma type and are less apparent in highly trauma-exposed samples (Street, Vogt, & Dutra, 2009; Wolf et al., 2013). For example, Street and colleagues (Street, Gradus, Giasson, Vogt, & Resick, 2013) found comparable rates of probable past-month PTSD among male (23.4%) and female (21.0%) veterans of the Iraq and Afghanistan wars, indicating that trauma severity may equalize rates of PTSD among men and women. However, a recent prospective study found that the effect of combat experiences on post-deployment PTSD was stronger for women than men (Polusny et al., 2014). In addition, it has been suggested that the factor structure of PTSD may differ for women compared with men. Specifically, a previous study of adolescents found significantly higher error variances among female participants relative to male participants, suggesting that the latent PTSD factors did not account for as much of the item covariance among girls (Armour et al., 2011). These findings offer compelling reasons to assess for sex similarities and differences in PTSD studies, as failing to address potential sex differences in symptoms may have the unintended consequence of biasing the diagnostic criteria toward one sex or the other. In many studies of PTSD among veterans, it is nearly impossible to evaluate sex differences in the phenomenology of the disorder because of the traditionally smaller number of female veterans. This study addresses this limitation.
In this study, we used network models to examine the centrality of each of the PTSD symptoms included in the DSM-5. In doing so, our objectives were: 1a) to evaluate the proposed ICD-11 revisions to the PTSD criteria by examining the centrality of the six symptoms suggested for inclusion; 1b) to the extent that these six symptoms are not the most central, to further examine network model results to determine which PTSD symptoms are the most central; 2) to determine the extent to which the ICD-11 versus the most central symptoms in the network could be used to index independently assessed DSM-5 PTSD diagnoses; 3a) to evaluate a network model of PTSD and MDD symptoms to better understand how symptoms of each disorder are related to one another; 3b) to investigate the extent to which the ICD-11 and most central symptoms were associated with MDD; and 4) to compare results across men and women using a sample in which there were equal numbers of female and male veterans.
Method
Participants
Participants in this study were Operation Enduring Freedom (OEF) and Operation Iraqi Freedom (OIF) veterans enrolled in the Veterans After-discharge Longitudinal Registry (Project VALOR), a longitudinal national registry of Iraq and Afghanistan Army and Marine Corps veterans (Rosen et al., 2012). To be included in Project VALOR, veterans must have undergone a mental health evaluation at a VA facility. Veterans with probable PTSD (i.e., at least two instances of a PTSD diagnosis by a mental health professional associated with two separate visits) according to VA medical records were oversampled to create a 3:1 (PTSD: no PTSD) ratio, and women, underrepresented among veterans, were oversampled to create a 1:1 sex ratio. The VA Environmental Epidemiology Service provided a roster of veterans who met inclusion criteria. Potential participants received opt-out letters; those who did not return the letter, thus providing tacit agreement for future contact, were telephoned by study staff who provided additional information and assessed whether they were also currently participating in a clinical trial (an exclusion criterion). The data from 1,649 male and female veterans who completed both questionnaires and a diagnostic interview were included in Project VALOR. Further details on study design and recruitment are available in previous publications (Rosen et al., 2012).
For the purposes of this study, we employed a subsample of 1,458 Project VALOR veterans who completed the PTSD Checklist for DSM-5 (PCL-5; Weathers et al., 2013). Their average age was 40.69 (SD = 9.79); 51.1% were female. The majority (73.6%) were White, 15.9% were Black, 3.3% were American Indian or Alaska Native, 2.1% were Asian, 0.6% were Pacific Islander, 1.4%, reported other races, and 11.7% were Hispanic. Data for the current study were collected during Phase 2 of Project VALOR, the first time point that included DSM-5 PTSD assessments.
Measures
Demographics
Participants completed a demographic questionnaire online or by mail. They reported their age, race, and sex.
Life Events Checklist for DSM-5 (LEC-5)
The LEC-5 (Gray, Litz, Hsu, & Lombardo, 2004; Weathers et al., 2013), is a two-part self-report questionnaire of trauma exposure. In part one, participants are asked to indicate if they experienced, witnessed, learned about, or were repeatedly exposed to any of 16 potentially traumatic events, or another extraordinarily stressful event not captured by the first 16 items. In part two, participants are asked to identify the worst event of those they endorsed, and provide additional information about the event.
Structured Clinical Interview for DSM-5 (SCID-5)
The SCID-5 (First, Williams, Karg, & Spitzer, 2015) was used to assess current (past month) PTSD diagnostic status. The SCID-5 for PTSD has good reliability (κ = .69; Regier et al., 2013). We also employed the SCID-5 MDD module to assess current MDD diagnostic status. A previous study found that SCID-5 for MDD had poor reliability (κ = .20–.35; Clarke et al., 2013). However, in the present study, inter-rater agreement was excellent for both PTSD (κ = .82) and MDD (κ = .75) among a random subset of interviews (n = 100) that were independently reviewed and rated by an assessor who did not complete the initial interview.
PTSD Checklist for DSM-5 (PCL-5)
The PCL-5 (Weathers et al., 2013) is a 20-item self-report measure that assesses DSM-5 symptoms of PTSD and was the focus of the network model analyses. For each symptom, respondents provide a severity rating ranging from 0 to 4 (0 = not at all to 4 = extremely) indicating the degree of distress associated with each symptom in the past month. The PCL-5 possesses excellent psychometric properties in veteran samples (Bovin et al., 2015; Keane et al., 2014). In this study, reliability was excellent (Cronbach’s α = .96).
Patient Health Questionnaire-9 (PHQ-9)
Depressive symptoms were assessed using the nine-item self-report PRIME-MD Patient Health Questionnaire (PHQ-9; Kroenke, Spitzer, & Williams, 2001; Spitzer, Kroenke, & Williams, 1999). Respondents rate the degree to which they were bothered by symptoms during the past two weeks on a four-point scale ranging from 0 to 3 (0 = not at all to 3 = nearly every day). Items are summed to create a total score, with higher scores indicating greater symptom severity. In this study, the total score demonstrated strong internal consistency (Cronbach’s α = .87).
Procedure
Participants completed self-report questionnaires online or by mail and were then interviewed via telephone by doctoral-level clinicians to determine PTSD and MDD diagnostic status on the SCID-5. All participants had completed Phase 1 of Project VALOR approximately 2.5 years prior to the current assessment. All participants provided informed consent prior to participation, and the study was approved by the local Institutional Review Boards and the Human Research Protection Office (HRPO) of the US Army Medical Research and Materiel Command.
Statistical Analysis
For the primary analyses, we randomly assigned our participants to one of two separate datasets, termed the discovery and validation subsamples, in order to evaluate the relationship between the most central symptoms as determined by network analyses, in their relationship to independent, clinician-rated PTSD and MDD diagnoses. Unless otherwise noted, analyses were performed in the combined sample of men and women. We first estimated network models of PTSD symptoms as reported on the PCL-5 in the discovery subsample using the least absolute shrinkage and selection operator (LASSO). Graphical LASSO networks are based on regularized partial correlations among all variables in which each edge (path) represents the association between two nodes (variables) independent from all other variables in the model (Epskamp & Fried, under review; J. Friedman, Hastie, & Tibshirani, 2008). LASSO networks shrink coefficients while estimating networks, controlling for spurious associations and resulting in more parsimonious networks. The absence of paths in a graphical LASSO network suggests that two variables do not directly interact. We implemented the LASSO in the R package qgraph (Epskamp, Cramer, Waldorp, Schmittman, & Borsboom, 2012), which uses the Extended Bayesian Information Criterion (EBIC) to select the best network by optimizing fit. We set the hyperparameter gamma = 0.5, so that the EBIC would err on the side of parsimony.
Graphical LASSO networks are considered weighted graphs, with the partial correlations as weights signifying the magnitude of associations among variables. qgraph produces several types of useful output, including visual models. We used the Fruchterman-Reingold algorithm, in which the length of paths between nodes corresponds to the absolute edge weight, i.e., the regularized partial correlation coefficient, to specify the layout of the nodes in the graph. Thus, nodes that are strongly associated with one another appear closer together in the graphs, allowing for inspection of the clustering among variables (Epskamp et al., 2012). Nodes with multiple strong associations will be located near the center of the graph, where the distance to other nodes is the shortest.
Qgraph also produces three main types of centrality indices for weighted graphs: betweenness, closeness, and strength. Betweenness is the degree to which a node lies on the shortest paths, based on weights (i.e., partial correlations in this study), between two other nodes and can be thought of as a measure of how much the node exerts control over information flow in the network (Opsahl, Agneessens, & Skvoretz, 2010). These are cross-sectional data, and accordingly, we conceptualize betweenness as reflecting the extent to which a variable connects to other variables. Closeness is the inverse of the mean shortest weighted path length (based on partial correlations) from a node to all other nodes; a high score indicates a short average distance to other nodes. Strength is the sum of weights of the paths connected to a node and reflects the degree of involvement of the node in the network (Opsahl et al., 2010). For all measures, higher scores are indicative of greater centrality.
Centrality indices are calculated based on the absolute values of edge weights. However, negative associations may exist within psychological networks, as increases in some symptoms may lead to decreases in other symptoms. The expected influence (EI) index has been developed to account for negative edge weights and is equal to the sum of weights between a node and all other nodes in the model (Robinaugh et al., 2016). If all edges are positive, the EI is equal to the node’s strength.
Recent research has focused on evaluating the reliability of network model parameters, given that sample size can impact their accuracy and replicability. We used the new R package bootnet (Epskamp, Borsboom, & Fried, under review) to construct confidence intervals (CIs) around edges in our network models as well as to determine the stability of our centrality indices. Non-parametric bootstrapping, with 1000 draws, was used to approximate the CIs in order to assess variability of edge-weights. Overlapping edge-weight CIs indicate that the edge-weights do not differ from one another and that interpreting their order should be done with care.
Centrality stability was determined by subsetting the data and correlating the original centrality indices with those from the subsamples. This correlation is a stability coefficient used to determine the maximum number of cases that can be dropped without compromising the reliability of the centrality index. Epskamp and colleagues (under review) recommended that the order of nodes not be interpreted for centrality indices with stability coefficients < 0.25, i.e., a maximum of 25% of cases can be dropped without impacting the index’s reliability. A stability coefficient of > 0.5 is ideal, although the authors note that evidence for these guidelines is currently limited. For each of the models below, we present stability coefficients for centrality indices (betweenness, closeness, and strength) in order to guide our interpretation of the most central symptoms. In addition, we used the differenceTest function in bootnet to statistically compare centrality for pairs of variables by constructing bootstrapped CIs around the difference in strength scores.
We reasoned that, to the extent that the ICD-11 PTSD symptoms emerged as the most central or most important to the overall PTSD network, this would provide support for the decision to limit the ICD-11 PTSD diagnosis to these symptoms. Further, if these symptoms emerged as the most central, they would be expected to provide the most information about the other PTSD symptoms not included in the ICD-11 proposal, reducing the potential for redundancy both within the PTSD diagnosis and across PTSD and comorbid conditions. This would ensure that even with elimination of other PTSD symptoms, the severity of these symptoms would still be represented by the diagnosis. On the other hand, to the extent that these symptoms were not the most important or central to the overall network, this would suggest that the ICD-11 PTSD definition was missing key features of the disorder that reflect overall severity and casesness. We conducted several follow-up analyses to further evaluate whether the most central items vs. the ICD-11 items were more strongly associated with PTSD diagnoses. For each PCL-5 item, we created weights using strength scores (the most reliable centrality index, as described below) derived from the discovery sample. Next, for each of the six most central variables from the network analysis, we multiplied the item weight (strength score) with the item score and summed the weighted severity score across all six items. We also created an equivalent sum score for ICD-11 symptoms as well as for six randomly selected symptoms. In the validation subsample, we used t-tests to compare these weighted sum scores for participants with and without SCID PTSD diagnoses and calculated Cohen’s d effect sizes to determine if the ICD-11, top six most central symptoms as identified in the discovery sample, or randomly selected symptoms better identified veterans with and without PTSD diagnoses. We also estimated logistic regression models with PTSD diagnoses as the outcome variable and the weighted sum scores as independent variables, respectively, to determine the extent to which these scores contributed to the variance in PTSD diagnoses. Of the 1,458 participants, a total of 1,377 completed the SCID-5 and were included in these analyses.
To explore the extent to which the symptoms in our graphs were potentially more reflective of comorbid MDD, we conducted several additional analyses. In the discovery subsample, we estimated graphical LASSO networks of PTSD (PCL-5) and MDD symptoms (PHQ-9) to visually inspect the closeness of the ICD-11 symptoms to the MDD symptoms. We then selected participants with PTSD with and without SCID-5-based MDD diagnoses from the full sample and estimated the graphical LASSO networks in these two subsamples separately to determine whether symptom centrality differed among individuals in the different diagnostic groups. In the validation subsample, we first used t-tests to compare the aforementioned weighted sum scores for participants with and without MDD diagnoses. We then calculated Cohen’s d effect sizes to determine whether the ICD-11, six most central, or six randomly selected symptoms better discriminated people with and without MDD diagnoses. We also estimated logistic regression models with MDD diagnosis as the outcome variable and the weighted sum scores as independent variables, respectively, to determine the extent to which these scores contributed to the variance in MDD diagnosis.
Results
Trauma Exposure
Participants endorsed a range of trauma exposure types on the LEC-5. The majority (86.7%) reported exposure to combat; 57.9% reported being physically assaulted, and 41.7% reported a history of sexual trauma, including sexual assault or harassment. Other frequently endorsed traumas included transportation accidents (55.4%) and unexpected death of a loved one (45.3%). The majority of participants (87.4%) reported that their worst trauma occurred during their military service. By design, the majority (62.9%) met DSM-5 criteria for PTSD; 24.1% met DSM-5 criteria for MDD.
Graphical LASSO Network: PCL-5 Items
The graphical LASSO network, estimated in the discovery subsample, is presented in Supplemental Figure 1. Nodes that are more highly associated with one another appear physically closer in the graph. Green lines represent positive associations, and red lines represent negative associations; the thickness of the line indicates the magnitude of a given partial correlation. Symptoms and abbreviations, as well as rankings for centrality measures, are presented in Table 1. Generally, there were strong, positive associations among symptoms within each cluster; thus, in the graphs, symptoms tended to cluster closely together with other symptoms in their DSM-5 criterion set, particularly the intrusion and the negative alterations in cognitions and mood symptoms, with the exception of inability to recall features of the trauma (symptom D1). In addition, irritable behavior and self-destructive or reckless behavior were less connected to other arousal and reactivity symptoms. Problems with concentration, self-destructive or reckless behavior, distressing dreams, diminished interest in activities, persistent negative emotional state, and exaggerated startle response were the top six symptoms on betweenness, indicating that they acted as connectors among the variables in the network. Self-destructive or reckless behavior, distressing dreams, problems with concentration, intrusive distressing thoughts or memories, diminished interest in activities, and sleep disturbance had the highest scores on the closeness statistic, indicating they had the shortest average distances to the other variables (based on regularized partial correlations). Persistent negative emotional state, efforts to avoid external reminders, efforts to avoid thoughts or memories, inability to experience positive emotions, distressing dreams, and intrusive distressing thoughts or memories had the highest strength scores; these variables were the most involved in the network.
Table 1.
PTSD symptoms, abbreviations and ranking on measures of strength centrality
| DSM-5 Symptom Cluster and Number |
DSM-5 Symptoms | Abbreviation | Discovery Sample |
PTSD-MDD | PTSD +MDD |
|---|---|---|---|---|---|
| B1 | Intrusive distressing thoughts or memories |
Mem | X | X | X |
| B2 | Distressing dreamsa | Drm | X | ||
| B3 | Dissociative flashbacksa | Fls | X | ||
| B4 | Psychological distress | Ups | X | X | |
| B5 | Physiological reactions | Phy | |||
| C1 | Efforts to avoid thoughts/memoriesa | Avm | X | X | |
| C2 | Efforts to avoid external remindersa | Avx | X | ||
| D1 | Inability to recall features of the trauma | Amn | |||
| D2 | Negative beliefs | Blf | |||
| D3 | Distorted blaming of oneself or others | Blm | |||
| D4 | Persistent negative emotional state | Neg | X | X | X |
| D5 | Diminished interest in activities | Anh | X | ||
| D6 | Detachment from others | Cut | |||
| D7 | Inability to experience positive emotions | Pos | X | X | X |
| E1 | Irritable behavior | Irr | |||
| E2 | Self-destructive or reckless behavior | Rsk | |||
| E3 | Hypervigilancea | Hyp | X | X | |
| E4 | Exaggerated startle responsea | Str | |||
| E5 | Problems with concentration | Cnc | |||
| E6 | Sleep disturbance | Slp |
Note. Results are presented for the full sample. PTSD = posttraumatic stress disorder; DSM = Diagnostic and Statistical Manual of Mental Disorders; MDD = major depressive disorder; PTSD-MDD = subgroup of participants who met criteria for PTSD but not MDD; PTSD+MDD = subgroup of participants who met criteria for PTSD and MDD. X = symptom was in the top 6 items on a given centrality measure.
symptoms proposed for inclusion in the International Classification of Disease (ICD)-11.
The stability coefficients for betweenness (0.206), closeness (0.128), and strength (0.439) indicated that only the strength index could be reliably used to rank symptoms. We also calculated the EI of all symptoms to determine which had the highest expected influence in the network. The six items with the highest EI scores were persistent negative emotional state, efforts to avoid external reminders, efforts to avoid thoughts or memories, inability to experience positive emotions, intrusive distressing thoughts or memories, and psychological distress. Notably, five out of the top six symptoms overlapped for strength and EI. We, therefore, used items with the highest strength scores as our “top six” PTSD symptoms. Of these, efforts to avoid external reminders, efforts to avoid thoughts or memories, and distressing dreams are proposed for inclusion in the ICD-11.
In addition to investigating the stability of our centrality indices, we used non-parametric bootstrapping to calculate CIs around our edge weights. Results revealed overlapping CIs for most edge weights, indicating that their order should be interpreted with care. The edges between efforts to avoid external reminders and efforts to avoid thoughts or memories, hypervigilance and exaggerated startle response, and intrusive distressing thoughts or memories and distressing dreams were the strongest and overlapped with few other edges (see Supplemental Figure 2).
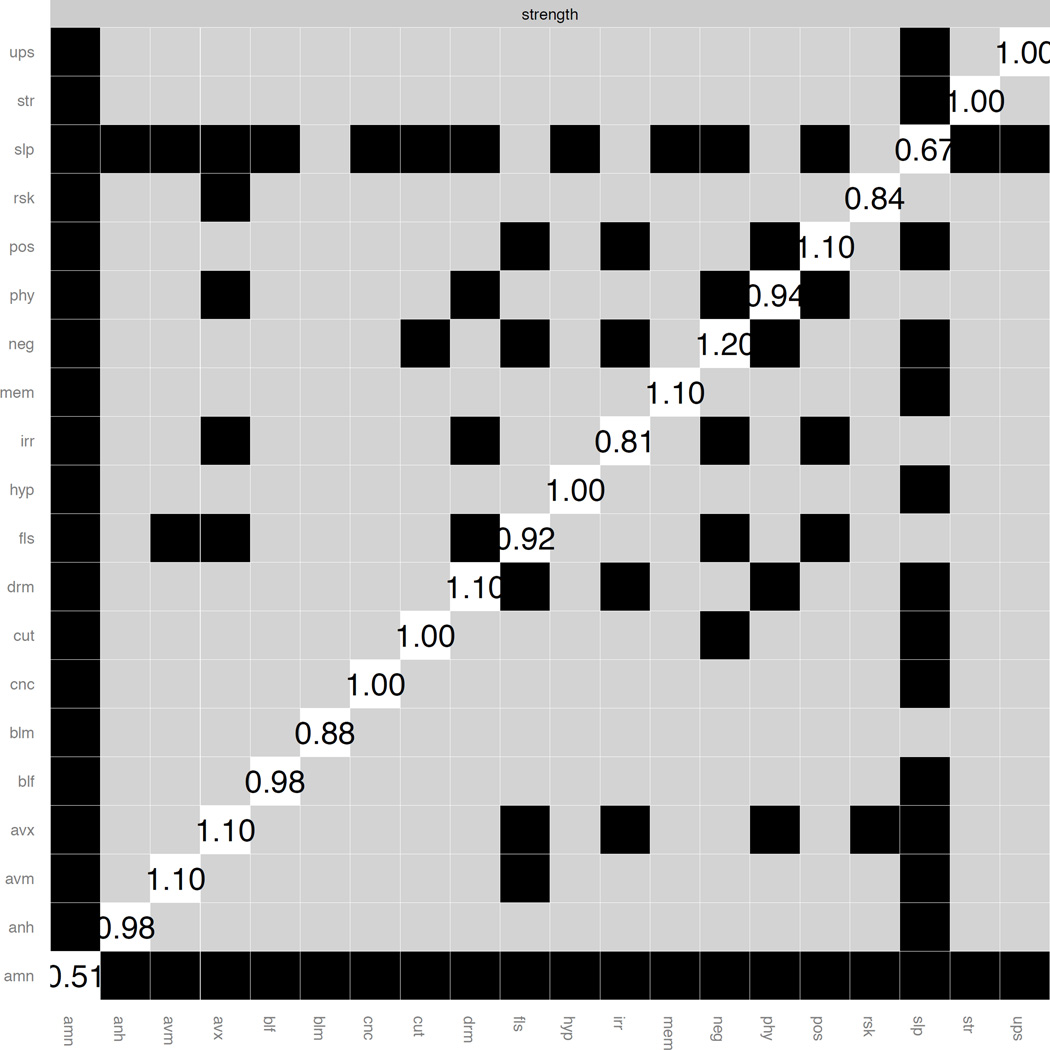
We also constructed a plot to determine whether strength differed significantly among PTSD symptoms. As shown in Figure 1, many variables did not differ in terms of strength. Further, there were few significant differences between our top six and ICD-11 items: inability to experience positive emotions, efforts to avoid external reminders and efforts to avoid thoughts or memories all had significantly higher strength scores than did dissociative flashbacks.
Figure 1.
Differences in strength between PTSD symptoms in the graphical LASSO network.
Note. Bootstrapped difference tests between node strength for all PTSD symptoms in the discovery sample. Values in the white boxes are node strength scores. Gray boxes are nodes that do not differ significantly from one another; black boxes represent nodes that do differ significantly from one another. PTSD = posttraumatic stress disorder; mem = intrusive distressing thoughts or memories; drm = distressing dreams; fls = dissociative flashbacks; ups = psychological distress; phy = physiological reactivity; avm = efforts to avoid thoughts or memories; avx = efforts to avoid external reminders; amn = Inability to recall features of the trauma; blf = negative beliefs; blm = Distorted blaming of oneself or others; neg = persistent negative emotional state; anh = diminished interest in activities; cut = detachment from others; pos = inability to feel positive emotions; irr = irritable behavior; rsk = self-destructive or reckless behavior; hyp = hypervigilance; str = exaggerated startle response; conc = problems with concentration; slp=sleep disturbance.
Graphical LASSO Networks: PCL-5 and PHQ-9 Items
The graphical LASSO network for the PCL-5 and PHQ-9 items, estimated in the discovery subsample, is presented in Supplemental Figure 3. The items from each measure tended to cluster within their respective measures, demonstrating fairly good distinction of the two constructs. Not surprisingly, there were strong, positive associations between bridge symptoms shared by both disorders, i.e., problems concentrating, diminished interest in activities, and sleep disturbance, which accounted for most of the linkage between disorders. The stability coefficients for betweenness (0.284), closeness (0.361), and strength (0.361) indicated that all three indices may be reliably used to rank symptoms. Problems with concentration (PTSD) had high scores on all three indices. Anhedonia (MDD), distressing dreams (PTSD), problems with concentration (MDD), and sleep disturbance (PTSD) had high betweenness and closeness scores. Sleep disturbance (MDD), persistent negative emotional state (PTSD), feeling down or depressed (MDD), intrusive distressing thoughts or memories (PTSD), and efforts to avoid external reminders (PTSD) had the highest strength scores.
In order to numerically evaluate the strength of associations between the top six most central items (from the PCL-5 graph), the ICD-11 items, and the PHQ-9 items, we summed the regularized partial correlations from the graphical LASSO between the top six items and PHQ-9 items and took the average of this value to derive an average association of 0.006. We computed this average association for the ICD-11 symptoms as well; this value was 0.0007. Thus, the difference between the two symptom sets was less than 1% in terms of variance accounted for, suggesting that their associations with MDD did not differ meaningfully.
PTSD ± Depression
In order to further investigate the extent to which comorbid MDD symptoms influenced our network analysis results, we estimated the graphical LASSO models for the PCL-5 among subsamples of participants (from the full sample) with SCID-5 PTSD diagnoses, with (n = 516) and without (n = 299) SCID-5 MDD diagnoses. For both subsamples, the stability coefficients indicated that only the strength index could be reliably used to rank symptoms. Among participants with PTSD only, the six symptoms with the highest strength scores were persistent negative emotional state, intrusive distressing thoughts or memories, hypervigilance, psychological distress, inability to experience positive emotions, and efforts to avoid external reminders (i.e., two ICD-11 criteria made this list). In contrast, among participants with PTSD and MDD, the top six symptoms were psychological distress, persistent negative emotional state, hypervigilance, intrusive distressing thoughts or memories, diminished interest in activities, and dissociative flashbacks (i.e., two ICD-11 criteria made this list). Thus, the most central variables among both groups of participants included a mix of putative PTSD-specific symptoms and symptoms shared between the two disorders.
Comparison of Network Model Results with PTSD Diagnoses
We estimated correlations between the six most central variables from the PCL-5 graph suggested by our analyses in the discovery sample, the six ICD-11 variables, and six randomly selected variables (i.e., detachment from others, distorted blaming of oneself or others, inability to recall features of the trauma, physiological reactions, self-destructive or reckless behavior, and intrusive distressing thoughts or memories) and total PCL scores in the validation subsample. The top six (r = .959, p < 0.001), ICD-11 (r = .930, p < 0.001), and random six (r = .969, p < 0.001) symptoms were highly, significantly associated with PCL scores. We then created weighted1 scores of the six most central variables, the six ICD-11 variables, and six randomly selected variables by multiplying each variable by its strength score, then summing across the six weighted variables. We then compared mean values on these weighted sum scores for participants with and without SCID-5 PTSD diagnoses in the validation subsample to test if these different criteria sets were differentially associated with independently assessed PTSD diagnoses. All t-test results were significant, such that participants with PTSD consistently had higher mean scores than those without PTSD (see Table 2). Further, Cohen’s d effect sizes were quite similar for the top six (d = 1.37), ICD-11 (d = 1.31), and random six (d = 1.30) sum scores.
Table 2.
T-test results comparing weighted sum scores by PTSD and MDD diagnosis
| PTSD + | PTSD − | MDD + | MDD − | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Mean | SD | Mean | SD | T | p | Mean | SD | Mean | SD | T | p | |
| Top six symptoms |
16.572 | 5.924 | 7.990 | 6.589 | −16.695 | <0.001 | 17.054 | 6.489 | 11.872 | 7.349 | −8.535 | <0.001 |
| ICD-11 symptoms |
15.895 | 5.797 | 7.773 | 6.546 | −15.951 | <0.001 | 15.907 | 6.677 | 11.605 | 7.141 | −7.032 | <0.001 |
| Random six symptoms |
12.288 | 4.550 | 6.144 | 4.891 | −16.220 | <0.001 | 13.205 | 4.790 | 8.770 | 5.357 | −9.477 | <0.001 |
Note. PTSD = posttraumatic stress disorder; PTSD + = participants with PTSD diagnoses; PTSD - = participants without PTSD diagnoses; MDD = major depressive disorder; MDD + = participants with MDD diagnoses; MDD - = participants without MDD diagnoses; ICD-11 = International Classification of Disease-11; T = t−test. The top six symptoms were persistent negative emotional state, efforts to avoid external reminders, efforts to avoid thoughts or memories, inability to experience positive emotions, distressing dreams, and intrusive distressing thoughts or memories. The symptoms proposed for inclusion in the ICD-11 are distressing dreams, dissociative reactions, efforts to avoid thoughts/memories, efforts to avoid external reminders, hypervigilance, and exaggerated startle response. The random six symptoms were detachment from others, distorted blaming of oneself or others, inability to recall features of the trauma, physiological reactions, self-destructive or reckless behavior, and intrusive distressing memories. Weighted sum scores for each of the three groups of symptoms were created by multiplying each item score by their strength scores, then summing the six weighted variables.
We also estimated logistic regression models for each of the three weighted sum scores, respectively, with SCID-5-based PTSD diagnoses as the dependent variable, to determine the percent variance in diagnosis accounted for by the sum scores. Nagelkerke’s R2 for each sum score was: 0.404 (top six), 0.379 (ICD-11), and 0.380 (random six). The 95% confidence intervals for each odds ratio (OR) overlapped with one another: top six (OR = 1.223, 95%CI: 1.184, 1,262), ICD-11 (1.213, 95%CI: 1.176, 1.252), random six (OR = 1.300, 95%CI: 1.245, 1.357). These results suggest that associations between each weighted sum score and PTSD diagnosis did not differ significantly from each other.
Comparison of Network Model Results with MDD Diagnoses
We then compared mean values on the three weighted2 sum scores for participants with and without SCID MDD diagnoses. As shown in Table 2, all t-tests were significant, such that participants with MDD consistently had higher mean scores than those without MDD. Cohen’s d effect sizes were similar for the top six (d = 0.747), ICD-11 (d = 0.622), and random six (d = 0.873) sum scores.
Finally, we estimated logistic regression models for each of the three weighted sum scores, with SCID MDD diagnosis as the dependent variable. Nagelkerke’s R2 for each sum score was: 0.137 (top six), 0.101 (ICD-11), and 0.179 (random six). In comparing the odds ratios for the three symptom sets, the 95% confidence intervals differed significantly for the ICD-11 (OR=1.093, 95%CI: 1.063, 1.123) and random six (OR = 1.175, 95%CI: 1.131, 1.220) symptom scores, but were overlapping between the ICD-11 and top six scores (OR = 1.109, 95%CI: 1.079, 1,140), and between the random six and top six symptom scores.
Comparison of Graphs by Sex
There were both similarities and differences in the top six items from the PTSD network (see Supplemental Figure 4) when estimated separately among women (n = 375) and men (n = 354) in the discovery sample. The stability coefficients indicated that only the strength index could be reliably used to rank symptoms in both subsamples. Persistent negative emotional state, inability to experience positive emotions, efforts to avoid external reminders, and intrusive distressing thoughts or memories were in the top six symptoms for both sexes (see Supplemental Table 1). Among women, the additional two items with the highest centrality scores were hypervigilance and diminished interest in activities. Among men, the additional top two items were distressing dreams and problems concentrating.
When examining graphs separately for women (n = 260) and men (n = 256) with PTSD only, persistent negative emotional state, intrusive distressing thoughts or memories, and hypervigilance appeared in the top six symptoms in both subgroups. Inability to experience positive emotions, physiological distress, and efforts to avoid thoughts or memories appeared more central for women, whereas detachment from others, efforts to avoid external reminders, and psychological distress were more salient for men. Similarly, only dissociative flashbacks and psychological distress were in the top six symptoms for both women (n = 253) and men (n = 146) with PTSD and MDD. It should be noted, however, that none of the stability coefficients reached the minimum acceptable level of 0.25 proposed by Epskamp and colleagues (under review) among women with PTSD and MDD or among men with PTSD only, implying that interpretation of these results should be done with caution. The strength index had the highest coefficient among men with PTSD only (0.207), and strength and closeness tied for highest among women with PTSD and MDD (0.131).
Discussion
To our knowledge, this is the first network analysis of DSM-5 PTSD symptoms. The most central PTSD symptoms were persistent negative emotional state, efforts to avoid external reminders, efforts to avoid thoughts or memories, inability to experience positive emotions, distressing dreams, and intrusive distressing thoughts or memories. Inability to experience positive emotions and persistent negative emotional state could be present in many other disorders including MDD. When we estimated our network model of PTSD symptoms in participants with PTSD but not MDD, persistent negative emotional state, intrusive distressing thoughts or memories, inability to experience positive emotions, and efforts to avoid external reminders remained among the most central symptoms, along with psychological distress, and hypervigilance. Taken together, our results suggest that the putatively PTSD-specific symptoms that are most central to this network are efforts to avoid external reminders, efforts to avoid thoughts or memories, distressing dreams, intrusive distressing thoughts or memories, psychological distress (in response to trauma reminders), and hypervigilance. That said, symptoms that are thought to overlap with depression (persistent negative emotional state and inability to experience positive emotions) were also central to those with PTSD without MDD, suggesting that eliminating them from the ICD-11 PTSD diagnosis might have the unintended consequence of failing to identify “pure” cases of PTSD (at least with respect to comorbid MDD).
Symptom non-specificity has long been an issue in defining PTSD, as many PTSD symptoms overlap with other mental health disorders, including mood and anxiety disorders (Spitzer et al., 2007), although this is a problem inherent to many DSM diagnoses, not just PTSD (Byllesby et al., 2016; Watson, 2005; Zbozinek et al., 2012). Our findings indicate that some of these non-specific symptoms are important to the PTSD network. However, it is worth noting that network analyses are only as good as their input data. That is, we defined our network using the 20 DSM-5 symptoms, the diagnostic system currently recognized in the PTSD field. We therefore began with the assumption that all these symptoms have the potential to provide value in defining the PTSD construct, an issue that continues to be under debate since the publication of DSM-5 (Friedman, Kilpatrick, Schnurr, & Weathers, 2016; Hoge et al., 2016). These results cannot determine whether one set of criteria is more correct than another. However, we can test to some extent if, given existing criteria, eliminating some of them might lose valuable information. Phenotype refinement is important because the search for the biomarkers, correlates, and interventions to treat PTSD will be hampered if the phenotype is not psychometrically sophisticated and externally valid. Our results may represent an initial effort to evaluate the proposed PTSD phenotype and shed light on its potential refinement. To meet the goals of improving diagnostic utility and reducing psychiatric comorbidity, the ICD-11 PTSD working group’s intention was to select symptoms that are specific to PTSD and not shared with other disorders. However, of the proposed ICD-11 symptoms, only efforts to avoid external reminders, efforts to avoid thoughts or memories, and distressing dreams were among the top six symptoms in the network. This suggests that the three other proposed ICD-11 symptoms may not be the most central to the DSM-5 PTSD network and that potentially critical information from the most central symptoms not included in the ICD-11 proposal may be lost if that proposal is advanced.
Network model results alone cannot fully address whether the non-specific symptoms should be excluded due to their limited discriminant validity, which is the very argument that the ICD-11 committee made for excluding these symptoms. In an effort to remedy this limitation, we also estimated a model of PTSD and MDD symptoms and found, as predicted, that their shared symptoms acted as bridge symptoms among the two disorders. However, network models of both PTSD and MDD showed relative distinction between the two criterion sets, providing us with additional confidence that the majority of the symptoms that were the most central in our analyses had relatively low overlap across diagnoses.
Two aspects of our results underscore the need to interpret these findings with caution. First, although stability coefficients suggested that our strength indices met the proposed minimally acceptable criteria for interpretation, we found very few significant differences in strength between our top six symptoms and the ICD-11 symptoms. Second, we found negligible differences in effect size when comparing indices (weighted mean sum scores) of the top six items, six ICD-11 items, and a random selection of six symptoms between participants with and without PTSD diagnoses. Importantly, ICD-11 symptoms do not appear to discriminate individuals with and without PTSD better than the top 6 symptoms or the randomly selected symptom set, suggesting that these symptoms may not meet the working group’s stated goal of improving diagnostic utility (Maercker et al., 2013). Ideally, a reduced set of PTSD symptoms would be substantially more predictive of PTSD diagnoses than sets of symptoms not included in the reduced set. In addition, the ICD-11 and top six symptoms appeared similarly associated with MDD diagnoses, even though one would expect that the ICD-11 symptoms, none of which is a criterion for MDD (by design of the ICD-11 workgroup), would be less related to depression. Further, these findings are consistent with those of Wisco and colleagues (2016), who found that the ICD-11 definition of PTSD was no less associated with psychiatric comorbidity than was DSM-IV PTSD.
Our results regarding the most central PTSD symptoms for men and women have implications for ICD-11 as well. Distressing dreams and problems concentrating were particularly central among men in this study, underscoring the potential usefulness of these symptoms as treatment targets. In contrast, hypervigilance and diminished interest in activities were more central for women. The literature is mixed regarding endorsement of specific PTSD symptoms in men vs. women (Carmassi et al., 2014; King, Street, Gradus, Vogt, & Resick, 2013; Maguen, Luxton, Skopp, & Madden, 2012). However, our results are consistent with previous findings that anhedonia in PTSD is more prevalent among women and the suggestion that reward functioning deficits observed in PTSD may differ by sex. Specifically, it has been suggested that women have a stronger bias toward negative stimuli under stress, and thus are more likely to focus on loss avoidance, whereas men have greater reward sensitivity and approach motivation (Carmassi et al., 2014; Nawijn et al., 2015). The DSM-5 includes a broader range of symptoms than does ICD-11, implying that despite sex-related differences in centrality, the symptoms most central to men and women would both be captured by the DSM-5 diagnosis. In contrast, the narrow ICD-11 symptom set could systematically bias the construct and diagnosis so that it was less applicable to one sex, as there are very few symptoms included in the diagnostic criteria to function as a safety net to capture symptom presentations that may differ across sex and other demographic or trauma groups. Greater consideration and research is required to evaluate if the ICD-11 symptom set may be more or less applicable to certain groups of individuals.
In the only other available network analysis of PTSD symptoms, McNally and colleagues (2015) found that difficulty concentrating, hypervigilance, distressing dreams and sleep disturbance were highly central to their network of DSM-IV PTSD symptoms. Of these, only difficulty concentrating and distressing dreams were among our most central symptoms. Although both studies used the PCL, they were based on different versions of the DSM, and the samples were quite different - McNally and colleagues’ sample included Chinese adult survivors of a major earthquake. Therefore, the differences in findings could be due to the network topology of PTSD differing by trauma type, the existence of multiple network structures of PTSD, or subtle differences in analytic approaches due to the advancement of network modeling over time, which are reflected in the differences reported in our respective studies. Regardless of the reason for the discrepancy, these differences underscore the importance of replication across a range of samples. As well, to the extent that there are differences in network structure across populations, this would suggest that it might be best to rely on an overly-inclusive criteria set relative to an overly-restrictive one as the former has a built in safeguard that would identify individuals with PTSD even when the most central symptoms differ across the populations, whereas the latter would risk missing PTSD in some populations or being otherwise biased as a function of population characteristics.
In addition to the need for replication, several limitations should be noted. Data from this study are based on a self-report measure of PTSD, the PCL-5. The PCL-5 does not require responses to be linked to a specific traumatic event; rather, instructions ask participants to indicate how often they have experienced symptoms that people sometimes have in response to a very stressful experience. Although SCID-5 data were available, the use of skip-outs in the SCID-5 makes these data less than ideal for analysis in network models, which is why we used the SCID-5 data only to index PTSD diagnosis. Data from this study were cross-sectional; future studies will need to investigate associations among PTSD symptoms over time. In addition, the use of a sample of male and female veterans who have very high rates of combat trauma may not generalize to other trauma-exposed populations. Nonetheless, this study has several major strengths, including the large subsamples of women and men. Female veterans remain understudied, and many samples are not large enough to evaluate sex differences.
Relative to the DSM-5 PTSD criteria, the ICD-11 definition of PTSD has consistently produced lower PTSD diagnostic rates in prior studies (Hansen et al., 2015; Wisco et al., 2016). Given that the ICD-11 will presumably be used for billing and reimbursement in the US, the lack of interchangeability across the two systems may pose a significant problem in clinical practice. The goals of the ICD-11 are to improve diagnostic utility and reduce psychiatric comorbidity. Our findings, and those from previous studies (e.g., Wisco et al., 2016) raise doubts about the extent to which these aims have been achieved using the proposed limited symptom set. We recommend that future studies explore alternate definitions of PTSD that strike a better balance of identifying a consistent group of individuals with the diagnosis and allowing for greater parsimony, ease of assessment, and diagnostic specificity. As noted above, network model results alone likely cannot tell us how best to diagnose a disorder or what guiding principles should be prioritized as the network is limited by the extant set of criteria for a disorder and is agnostic about the broader aims of the diagnostic taxonomy. Further, it is important to determine whether the most central symptoms provide information about other symptoms in the network or are highly representative of those with a given diagnosis, as these results may be worth considering in determining how to best assess the PTSD construct. Results of network analysis using longitudinal data could be used to identify the symptoms that most strongly influence other symptoms and to assess whether these variables are strong candidates for a reduced set of PTSD criteria that does not lose substantial information or exclude patients who should be classified as having the disorder.
Supplementary Material
Acknowledgments
There are no published or submitted papers from this dataset that address related questions. The manuscript has not been posted on a website, and findings have not yet been presented at a conference. Dr. Mitchell’s contribution to this work was supported by funding from the National Institute of Mental Health (K01MH093750). Dr. Wolf’s contribution to this work was supported by a Career Development Award (no grant #) from the United States (U.S.) Department of Veterans Affairs, Clinical Sciences Research and Development Program and by a Presidential Early Career Award for Scientists and Engineers as administered by U.S. Department of Veterans Affairs Office of Research and Development (PECASE 2013A). Dr. Marx was supported by funding from the Department of Defense (W81XWH-10-2-0181 and W81XWH-12-2-0117), Defense Advanced Research Programs Agency (N66001-11-C-4006) and Department of Veterans Affairs (Cooperative Studies Program # 591). Lewina O. Lee was supported by funding from the National Institute on Aging (K08-AG048221). Dr. Rosen was supported by funding from the Department of Defense, (W81XWH-12-1-0532; W81XWH-14-2-0139; and W81XWH-12-2-0121). Terence M. Keane was supported by funding from Department of Veterans Affairs (Clinical Science Research & Development), Department of Defense (W81XWH-10-2-0181; W81XWH-12-2-0117), and the National Institute of Mental Health (T32MH019836-16A1). The contents of this article do not represent the views of the U.S. Department of Veterans Affairs or the United States Government.
We wish to thank Matthew King, PhD, for sharing his R expertise in coding the relative importance graphs.
Footnotes
The pattern of results for the t-tests, Cohen’s d, and logistic regression models was very similar when using raw sum scores compared to the weighted sum scores.
The pattern of results for the t-tests, Cohen’s d, and logistic regression models was very similar when using raw sum scores compared to the weighted sum scores.
References
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 5th. Washington, DC: Author; 2013. [Google Scholar]
- Armour C, Elhai JD, Layne CM, Shevlin M, Duraković-Belko E, Djapo N, Pynoos RS. Gender differences in the factor structure of posttraumatic stress disorder symptoms in war-exposed adolescents. Journal of Anxiety Disorders. 2011;25:604–611. doi: 10.1016/j.janxdis.2011.01.010. https://doi.org/10.1016/j.janxdis.2011.01.010. [DOI] [PubMed] [Google Scholar]
- Barabasi A-L. Linked. New York: Plume; 2003. [Google Scholar]
- Barabasi A-L, Oltvai ZN. Network biology: Understanding the cell’s functional organization. Nature Reviews Genetics. 2004;5:101–115. doi: 10.1038/nrg1272. [DOI] [PubMed] [Google Scholar]
- Borsboom D, Cramer AOJ. Network analysis: An integrative approach to the structure of psychopathology. Annual Review of Clinical Psychology. 2013;9:91–121. doi: 10.1146/annurev-clinpsy-050212-185608. https://doi.org/10.1146/annurev-clinpsy-050212-185608. [DOI] [PubMed] [Google Scholar]
- Bovin MJ, Marx BP, Weathers FW, Gallagher MW, Rodriguez P, Schnurr PP, Keane TM. Psychometric properties of the PTSD Checklist for Diagnostic and Statistical Manual of Mental Disorders-Fifth Edition (PCL-5) in veterans. Psychological Assessment. 2015 doi: 10.1037/pas0000254. https://doi.org/10.1037/pas0000254. [DOI] [PubMed] [Google Scholar]
- Brandes U, Erlebach T, editors. Network analysis: Methodological foundations. Germany: Springer-Verlag Berlin Heidelberg; 2005. [Google Scholar]
- Brewin CR. “I Wouldn’t Start From Here”—An alternative perspective on PTSD from the ICD-11: Comment on Friedman (2013) Journal of Traumatic Stress. 2013;26:557–559. doi: 10.1002/jts.21843. https://doi.org/10.1002/jts.21843. [DOI] [PubMed] [Google Scholar]
- Brewin CR, Lanius RA, Novac A, Schnyder U, Galea S. Reformulating PTSD for DSM-V: Life after Criterion A. Journal of Traumatic Stress. 2009;22:366–373. doi: 10.1002/jts.20443. https://doi.org/10.1002/jts.20443. [DOI] [PubMed] [Google Scholar]
- Byllesby BM, Charak R, Durham TA, Wang X, Elhai JD. The underlying role of negative affect in the association between PTSD, major depressive disorder, and generalized anxiety disorder. Journal of Psychopathology and Behavioral Assessment. 2016:1–11. https://doi.org/10.1007/s10862-016-9555-9. [Google Scholar]
- Carmassi C, Akiskal HS, Bessonov D, Massimetti G, Calderani E, Stratta P, Dell’Osso L. Gender differences in DSM-5 versus DSM-IV-TR PTSD prevalence and criteria comparison among 512 survivors to the L’Aquila earthquake. Journal of Affective Disorders. 2014;160:55–61. doi: 10.1016/j.jad.2014.02.028. https://doi.org/10.1016/j.jad.2014.02.028. [DOI] [PubMed] [Google Scholar]
- Clarke DE, Narrow WE, Regier DA, Kuramoto SJ, Kupfer DJ, Kuhl EA, Kraemer HC. DSM-5 field trials in the United States and Canada, Part I: Study design, sampling strategy, implementation, and analytic approaches. The American Journal of Psychiatry. 2013;170:43–58. doi: 10.1176/appi.ajp.2012.12070998. https://doi.org/10.1176/appi.ajp.2012.12070998. [DOI] [PubMed] [Google Scholar]
- Cloitre M, Garvert DW, Brewin CR, Bryant RA, Maercker A. Evidence for proposed ICD-11 PTSD and complex PTSD: A latent profile analysis. European Journal of Psychotraumatology. 2013;4:27344–27352. doi: 10.3402/ejpt.v4i0.20706. https://doi.org/10.3402/ejpt.v4i0.20706. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cramer AOJ, Waldorp LJ, van der Maas HLJ, Borsboom D. Comorbidity: A network perspective. Behavioral and Brain Sciences. 2010;33:137–193. doi: 10.1017/S0140525X09991567. [DOI] [PubMed] [Google Scholar]
- Creamer M, Burgess P, Pattison P. Reaction to trauma: A cognitive processing model. Journal of Abnormal Psychology. 1992;101:452–459. doi: 10.1037//0021-843x.101.3.452. [DOI] [PubMed] [Google Scholar]
- Epskamp S, Borsboom D, Fried EI. Estimating psychological networks and their accuracy: A tutorial paper. doi: 10.3758/s13428-017-0862-1. under review. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Epskamp S, Cramer AOJ, Waldorp LJ, Schmittman VD, Borsboom D. qgraph: Network visualizations of relationships in psychometric data. Journal of Statistical Software. 2012;48:1–18. [Google Scholar]
- Epskamp S, Fried EI. A primer on estimating regularized psychological networks. under review. [Google Scholar]
- First MB, Williams JBW, Karg RS, Spitzer RL. Structured Clinical Interview for DSM-5--Research Version (SCID-5 for DSM-5, Research Version; SCID-5-RV) Arlington, VA: American Psychiatric Association; 2015. [Google Scholar]
- Friedman J, Hastie T, Tibshirani R. Sparse inverse covariance estimation with the graphical lasso. Biostatistics. 2008;9:432–441. doi: 10.1093/biostatistics/kxm045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Friedman M, Kilpatrick D, Schnurr P, Weathers F. Correcting misconceptions about the diagnostic criteria for posttraumatic stress disorder in DSM-5. JAMA Psychiatry. 2016;73:753–754. doi: 10.1001/jamapsychiatry.2016.0745. https://doi.org/10.1001/jamapsychiatry.2016.0745. [DOI] [PubMed] [Google Scholar]
- Gray MJ, Litz BT, Hsu JL, Lombardo TW. Psychometric properties of the life events checklist. Assessment. 2004;11:330–341. doi: 10.1177/1073191104269954. https://doi.org/10.1177/1073191104269954. [DOI] [PubMed] [Google Scholar]
- Hansen M, Hyland P, Armour C, Shevlin M, Elklit A. Less is more? Assessing the validity of the ICD-11 model of PTSD across multiple trauma samples. European Journal of Psychotraumatology. 2015;6:28766–28777. doi: 10.3402/ejpt.v6.28766. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hoge C, Yehuda R, Castro C, McFarlane A, Vermetten E, Jetly R, Rothbaum BO. Unintended consequences of changing the definition of posttraumatic stress disorder in DSM-5: Critique and call for action. JAMA Psychiatry. 2016;73:750–752. doi: 10.1001/jamapsychiatry.2016.0647. https://doi.org/10.1001/jamapsychiatry.2016.0647. [DOI] [PubMed] [Google Scholar]
- Keane TM, Rubin A, Lachowicz M, Brief D, Enggasser JL, Roy M, Rosenbloom D. Temporal stability of DSM-5 posttraumatic stress disorder criteria in a problem-drinking sample. Psychological Assessment. 2014;26:1138–1145. doi: 10.1037/a0037133. https://doi.org/10.1037/a0037133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessler RC, Chiu WT, Demler O, Merikangas KR, Walters EE. Prevalence, severity, and comorbidity of 12-month DSM-IV disorders in the National Comorbidity Survey Replication. Archives of General Psychiatry. 2005;62:617–27. doi: 10.1001/archpsyc.62.6.617. https://doi.org/10.1001/archpsyc.62.6.617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessler RC, Petukhova M, Sampson NA, Zaslavsky AM, Wittchen H-U. Twelve-month and lifetime prevalence and lifetime morbid risk of anxiety and mood disorders in the United States. International Journal of Methods in Psychiatric Research. 2012;21:169–184. doi: 10.1002/mpr.1359. https://doi.org/10.1002/mpr.1359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- King MW, Street AE, Gradus JL, Vogt DS, Resick PA. Gender differences in posttraumatic stress symptoms among OEF/OIF veterans: An item response theory analysis. Journal of Traumatic Stress. 2013;26:175–183. doi: 10.1002/jts.21802. https://doi.org/10.1002/jts.21802. [DOI] [PubMed] [Google Scholar]
- Kroenke K, Spitzer RL, Williams JB. The PHQ-9: Validity of a brief depression severity measure. Journal of General Internal Medicine. 2001;16:606–613. doi: 10.1046/j.1525-1497.2001.016009606.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Litz BT, Schlenger WE, Weathers FW, Caddell JM, Fairbank JA, LaVange LM. Predictors of emotional numbing in posttraumatic stress disorder. Journal of Traumatic Stress. 1997;10:607–618. doi: 10.1023/a:1024845819585. https://doi.org/10.1023/A:1024845819585. [DOI] [PubMed] [Google Scholar]
- Maercker A, Brewin CR, Bryant RA, Cloitre M, Reed GM, van Ommeren M, Saxena S. Proposals for mental disorders specifically associated with stress in the International Classification of Diseases-11. Lancet (London, England) 2013;381:1683–1685. doi: 10.1016/S0140-6736(12)62191-6. https://doi.org/10.1016/S0140-6736(12)62191-6. [DOI] [PubMed] [Google Scholar]
- Maguen S, Luxton DD, Skopp NA, Madden E. Gender differences in traumatic experiences and mental health in active duty soldiers redeployed from Iraq and Afghanistan. Journal of Psychiatric Research. 2012;46:311–316. doi: 10.1016/j.jpsychires.2011.11.007. https://doi.org/10.1016/j.jpsychires.2011.11.007. [DOI] [PubMed] [Google Scholar]
- McNally RJ, Robinaugh DJ, Wu GWY, Wang L, Deserno MK, Borsboom D. Mental disorders as causal systems: A network approach to posttraumatic stress disorder. Clinical Psychological Science. 2015;3:836–849. [Google Scholar]
- Nawijn L, van Zuiden M, Frijling JL, Koch SB, Veltman DJ, Olff M. Reward functioning in PTSD: A systematic review exploring the mechanisms underlying anhedonia. Neuroscience & Biobehavioral Reviews. 2015;51:189–204. doi: 10.1016/j.neubiorev.2015.01.019. [DOI] [PubMed] [Google Scholar]
- Opsahl T, Agneessens F, Skvoretz J. Node centrality in weighted networks: Generalizing degree and shortest paths. Social Networks. 2010;32:245–251. https://doi.org/10.1016/j.socnet.2010.03.006. [Google Scholar]
- Polusny MA, Kumpula MJ, Meis LA, Erbes CR, Arbisi PA, Murdoch M, Johnson AK. Gender differences in the effects of deployment-related stressors and pre-deployment risk factors on the development of PTSD symptoms in National Guard Soldiers deployed to Iraq and Afghanistan. Journal of Psychiatric Research. 2014;49:1–9. doi: 10.1016/j.jpsychires.2013.09.016. https://doi.org/10.1016/j.jpsychires.2013.09.016. [DOI] [PubMed] [Google Scholar]
- Regier DA, Narrow WE, Clarke DE, Kraemer HC, Kuramoto SJ, Kuhl EA, Kupfer DJ. DSM-5 field trials in the United States and Canada, Part II: Test-retest reliability of selected categorical diagnoses. The American Journal of Psychiatry. 2013;170:59–70. doi: 10.1176/appi.ajp.2012.12070999. https://doi.org/10.1176/appi.ajp.2012.12070999. [DOI] [PubMed] [Google Scholar]
- Robinaugh DJ, Millner AJ, McNally RJ. Identifying highly influential nodes in the complicated grief network. Journal of Abnormal Psychology. 2016;125:747–757. doi: 10.1037/abn0000181. https://doi.org/10.1037/abn0000181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosen GM, Lilienfeld SO. Posttraumatic stress disorder: An empirical evaluation of core assumptions. Clinical Psychology Review. 2008;28:837–868. doi: 10.1016/j.cpr.2007.12.002. https://doi.org/10.1016/j.cpr.2007.12.002. [DOI] [PubMed] [Google Scholar]
- Rosen GM, Lilienfeld SO, Frueh BC, McHugh PR, Spitzer RL. Reflections on PTSD’s future in DSM-V. The British Journal of Psychiatry. 2010;197:343–344. doi: 10.1192/bjp.bp.110.079699. https://doi.org/10.1192/bjp.bp.110.079699. [DOI] [PubMed] [Google Scholar]
- Rosen GM, Spitzer RL, McHugh PR. Problems with the post-traumatic stress disorder diagnosis and its future in DSM-V. The British Journal of Psychiatry. 2008;192:3–4. doi: 10.1192/bjp.bp.107.043083. https://doi.org/10.1192/bjp.bp.107.043083. [DOI] [PubMed] [Google Scholar]
- Rosen RC, Marx BP, Maserejian NN, Holowka DW, Gates MA, Sleeper LA, Keane TM. Project VALOR: Design and methods of a longitudinal registry of post-traumatic stress disorder (PTSD) in combat-exposed veterans in the Afghanistan and Iraqi military theaters of operations. International Journal of Methods in Psychiatric Research. 2012;21:5–16. doi: 10.1002/mpr.355. https://doi.org/10.1002/mpr.355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spitzer RL, First MB, Wakefield JC. Saving PTSD from itself in DSM-V. Journal of Anxiety Disorders. 2007;21:233–241. doi: 10.1016/j.janxdis.2006.09.006. https://doi.org/10.1016/j.janxdis.2006.09.006. [DOI] [PubMed] [Google Scholar]
- Spitzer RL, Kroenke K, Williams JB. Validation and utility of a self-report version of PRIME-MD: The PHQ primary care study. JAMA. 1999;282:1737–1744. doi: 10.1001/jama.282.18.1737. [DOI] [PubMed] [Google Scholar]
- Spitzer RL, Rosen GM, Lilienfeld SO. Revisiting the Institute of Medicine report on the validity of posttraumatic stress disorder. Comprehensive Psychiatry. 2008;49:319–320. doi: 10.1016/j.comppsych.2008.01.006. https://doi.org/10.1016/j.comppsych.2008.01.006. [DOI] [PubMed] [Google Scholar]
- Street AE, Gradus JL, Giasson HL, Vogt D, Resick PA. Gender differences among veterans deployed in support of the wars in Afghanistan and Iraq. Journal of General Internal Medicine. 2013;28:556–562. doi: 10.1007/s11606-013-2333-4. https://doi.org/10.1007/s11606-013-2333-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Street AE, Vogt D, Dutra L. A new generation of women veterans: Stressors faced by women deployed to Iraq and Afghanistan. Clinical Psychology Review. 2009;29:685–694. doi: 10.1016/j.cpr.2009.08.007. https://doi.org/10.1016/j.cpr.2009.08.007. [DOI] [PubMed] [Google Scholar]
- van Borkulo C, Boschloo L, Borsboom D, Penninx BH, Waldorp LJ, Schoevers RA. Association of symptom network structure with the course of depression. JAMA Psychiatry. 2015;72:1219–1226. doi: 10.1001/jamapsychiatry.2015.2079. https://doi.org/10.1001/jamapsychiatry.2015.2079. [DOI] [PubMed] [Google Scholar]
- Watson D. Rethinking the mood and anxiety disorders: A quantitative hierarchical model for DSM-V. Journal of Abnormal Psychology. 2005;114:522–536. doi: 10.1037/0021-843X.114.4.522. https://doi.org/10.1037/0021-843X.114.4.522. [DOI] [PubMed] [Google Scholar]
- Weathers FW, Litz BT, Keane TM, Palmieri PA, Marx BP, Schnurr PP. The PTSD Checklist for DSM-5 (PCL-5) Scale Available from the National Center for PTSD at Www.ptsd.va.gov. 2013 [Google Scholar]
- Wisco BE, Miller MW, Wolf EJ, Kilpatrick D, Resnick HS, Badour CL, Friedman MJ. The impact of proposed changes to ICD-11 on estimates of PTSD prevalence and comorbidity. Psychiatry Research. 2016;240:226–233. doi: 10.1016/j.psychres.2016.04.043. https://doi.org/10.1016/j.psychres.2016.04.043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wolf EJ, Mitchell KS, Logue MW, Baldwin CT, Reardon AF, Humphries DE, Miller MW. Corticotropin releasing hormone receptor 2 (CRHR-2) gene is associated with decreased risk and severity of posttraumatic stress disorder in women. Depression and Anxiety. 2013;30:1161–1169. doi: 10.1002/da.22176. https://doi.org/10.1002/da.22176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zbozinek TD, Rose RD, Wolitzky-Taylor KB, Sherbourne C, Sullivan G, Stein MB, Craske MG. Diagnostic overlap of generalized anxiety disorder and major depressive disorder in a primary care sample. Depression and Anxiety. 2012;29:1065–1071. doi: 10.1002/da.22026. https://doi.org/10.1002/da.22026. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.