Abstract
Background
African Americans experience more problematic and disordered sleep than White Americans. Racial discrimination has been implicated in this disparity. However, the mechanisms by which discrimination disrupts sleep are unclear. It has been theorized that Perseverative Cognition (PC), characterized by recurrent patterns of reflective (i.e., rumination) and anticipatory (i.e., worry) negative thinking about personally relevant stressors, may reflect the functional mechanism linking discrimination to sleep. The present study is the first to empirically examine the dual components of PC as a candidate functional mechanism in the association between racial discrimination and subjective sleep quality.
Participants
Sixty-eight self-identified African American college students (55.9% female; Mage = 20.18, SD = 2.93) were recruited at a large predominantly white public university in the Midwest.
Methods
The participants completed the Perceived Ethnic Discrimination Questionnaire (PEDQ), Pittsburgh Sleep Quality Index (PSQI), Penn State Worry Questionnaire (PSWQ), and Ruminative Responses Scale (RRS).
Results
After adjusting for age, gender, and social class, results revealed a significant indirect effect of racial discrimination (RD) on subjective sleep quality through rumination, 95% CI [.008, .125], but not worry. RD was positively associated with rumination, b =.50, SE =.16, p = .003, and rumination, in turn, was positively associated with poorer sleep quality, b = .09, SE = .04, p = .012.
Conclusions
As both RD and poor sleep quality have been directly linked to heart disease, diabetes, depression, and a number of other maladies, our findings suggest that RD, sleep, and coping strategies (e.g., rumination) employed to manage RD experiences may be important targets for addressing racial disparities in health.
Sleep has garnered significant empirical attention in the last decade, as sleep problems and disorders contribute to a litany of negative health outcomes (e.g., Kim & Dimsdale, 2007). Problematic and disordered sleep (e.g., sleep disturbances, sleepiness, short sleep duration) is linked to all-cause mortality, cardiovascular disease, diabetes, obesity, immune functioning, cancer, and mood disorders (e.g., depression; Gallicchio & Kalesan, 2009; Gottlieb et al., 2006; Grandner, Patel, Gehrman, Perlis, & Pack, 2010; Slopen, Lewis, & Williams, 2016). Poor sleep is clearly a major public health concern; a key goal of the U.S. Department of Health and Human Services’ Healthy People 2020 is to improve Americans’ sleep health (U.S. Department of Health and Human Services, 2016).
Nationally representative and community-based data document poorer sleep quality and greater prevalence of sleep disorders among African Americans than among White Americans (Hall et al., 2009; Knutson, Van Cauter, Rathouz, DeLeire, & Lauderdale, 2010; Slopen et al., 2016). African Americans experience shorter sleep durations, less continuous sleep, and less slow-wave sleep (i.e., deep sleep). In addition to these more quantitative aspects of overall sleep (Buysse, Reynolds, Monk, Berman, & Kupfer, 1989), African Americans also report less restfulness and greater sleepiness (Beatty et al., 2011; Durrence & Lichstein, 2006; Friedman et al., 2006; Mezick et al., 2008; Redline et al., 2004; Slopen & Williams, 2014). Notably, sleep problems and disorders among African Americans are further coincident with various diseases that also disproportionately affect this population, including cardiovascular disease and diabetes (Kochanek, Arias, & Anderson, 2013; Miniño, 2013).
While the pathways linking poor sleep to disease are multifactorial, there has been considerable interest in understanding the contribution of psychosocial factors to sleep problems and disorders among African Americans. Racism and perceived discrimination have come to the forefront as chronic psychosocial stressors contributing to racial and ethnic disparities in sleep (for review, see Slopen et al., 2016). According to the Biopsychosocial Model of Racism, racism is a unique and pervasive, chronic psychosocial stressor that triggers physiological and psychological stress responses (i.e., fight or flight) for African Americans (Clark, Anderson, Clark, & Williams, 1999). Importantly, maladaptive forms of coping (e.g., rumination) are argued to exacerbate the stress process by prolonging physiological and psychological responses to racism-related stressors. Ultimately, this chronic cycle of exposure and response is thought to contribute to global dysregulation of somatic and psychological health among African Americans (Clark et al., 1999).
Contemporary research supports Clark and colleagues’ conceptualization, as findings from several studies document that greater exposure to racism and perceived discrimination adversely impacts sleep among African Americans (Beatty et al., 2011; Grandner, Patel, Gehrman, Xie, et al., 2010; Hicken, Lee, Ailshire, Burgard, & Williams, 2013; Steffen & Bowden, 2006; Yang & Park, 2015). For example, perceived discrimination attributed to race or ethnicity and various other factors (e.g., gender, social class) has been associated with poorer sleep quality, including poorer self-reported 30-day sleep quality (Steffen & Bowden, 2006); less slow-wave sleep (Thomas, Bardwell, Ancoli-Israel, & Dimsdale, 2006); greater self-reported daytime fatigue and sleep disturbances (Grandner et al., 2012); more frequent wake after sleep onset (WASO; Lewis et al., 2013); and shorter overall sleep duration (Slopen et al., 2016). Collectively, these findings suggest that greater self-reported exposure to racism and discrimination is related to greater sleep impairment. While the congruence of these findings with the Biopsychosocial Model of Racism is promising, it is important to further elucidate the potential mechanisms underlying the association between racism and the myriad indicators of poorer sleep among African Americans.
Perseverative Cognition (PC), characterized by recurrent patterns of negative, reflective (i.e., rumination) and anticipatory (i.e., worry) thinking (Brosschot, Gerin, & Thayer, 2006; Brosschot, Pieper, & Thayer, 2005), has been identified as a central mechanism potentially linking racism and racial discrimination (RD) to poorer sleep (e.g., Hicken et al., 2013; Steffen & Bowden, 2006). According to this hypothesis, worry (negative affect-laden and uncontrollable thoughts and images; Borkovec, Ray, & Stober, 1998), rumination (passive and self-reflective perseveration on one’s negative emotions and problems; Nolen-Hoeksema, 1991, 2000), and related cognitive processes (i.e., anticipatory stress) all share a common feature: repetitive or recurring negative thoughts. This framework also delineates that such repetitive or recurring thoughts may largely occur outside of conscious awareness (Brosschot, 2010; Brosschot et al., 2010). Research has long indicated that stress-related intrusive thoughts affect multiple domains of sleep, including shorter sleep duration, greater complaints, lower delta sleep ratio, and longer sleep onset latency (Hall et al., 1997; 2000; Kelly, 2002). Moreover, trait worry and rumination have been associated with indicators of poor sleep—including longer sleep onset latency (Pillai, Steenburg, Ciesla, Roth, & Drake, 2014; Takano, Sakamoto, & Tanno, 2014; Zoccola, Dickerson, & Lam, 2009), shorter sleep duration (Nota & Coles, 2014; Takano et al., 2014), and poorer subjective sleep quality (Ottaviani, Medea, Lonigro, Tarvainen, & Couyoumdjian, 2015; Radstaak, Geurts, Beckers, Brosschot, & Kompier, 2014)—as well as with indicators of cardiovascular hyperarousal during sleep (i.e., higher heart rate, lower heart rate variability; Brosschot, Van Dijk, & Thayer, 2007).
Few studies have empirically examined PC as a functional mechanism or process linking RD to sleep among African Americans. In a notable exception, Beatty and colleagues (2011) found that unfair treatment was associated with increased nightly worry, which in turn, was associated with poorer self-reported sleep quality, greater daytime sleepiness, poorer sleep efficiency, and less REM sleep. In an investigation of the anticipatory features of RD experiences, Hicken et al. (2013) found that African American adults reported greater sleep difficulty than White Americans; however, this disparity was completely attenuated after adjusting for racism-related vigilance. To our knowledge, these investigations represent the current empirical literature regarding the potential mechanistic functioning of PC in the association between racism or discrimination and sleep in African Americans. Neither of these studies directly tested whether the relationship between RD, in particular, and sleep was influenced by both components of PC. In the present study, we examined whether the dual components of PC (i.e., worry and rumination) might serve as the process(es) linking RD and subjective sleep quality among African Americans. In particular, we predicted that more frequent RD experiences would be associated with poorer subjective sleep quality. We also predicted that PC would mediate the association between RD experiences and poorer subjective sleep quality, such that greater RD exposure would be associated with greater PC, which in turn, would be associated with poorer subjective sleep quality.
METHOD
Participants
Sixty-eight self-identified African American college students aged 18 to 37 (55.9% female, Mage = 20.18; SD = 2.93) were recruited at a large predominantly White public university in the Midwest through the Research Experience Program (REP) pool, which allows students to participate in research for partial class credit in an introductory psychology course. Participants were also recruited via flyers, campus newspaper ads, and e-mail listservs; these participants received a small monetary compensation (i.e., $15.00) for their participation.
Procedure
The present questionnaire data were collected during baseline screenings as part of a larger study on PC and health (see Hill et al., in press). All participants provided their written informed consent. Thereafter, participants completed a packet of study questionnaires, including the RD, subjective sleep quality, worry, rumination, and demographics measures. All measures and study procedures were approved by the university Institutional Review Board.
Measures
Racial discrimination
RD was assessed using the brief Perceived Ethnic Discrimination Questionnaire–Community Version (PEDQ-CV; Brondolo et al., 2005). The brief PEDQ-CV is a 17-item questionnaire designed to assess lifetime experiences of RD, particularly in interpersonal and social contexts (α = .87). The experiences include different forms of RD that occur in various domains: social exclusion, stigmatization, discrimination at work or school, and threats or actual acts of harassment or harm. Each item is preceded by the stem phrase: “Because of your Ethnicity/Race, How often”; a sample item is “have others ignored or not paid attention to you?” Participants rated the frequency with which they have experienced RD on a 1 (never) to 7 (very often) scale. All 17 items were summed to create a Lifetime Discrimination scale wherein a higher score indicates more frequent experiences with RD.
Worry
Worry was assessed using the Penn State Worry Questionnaire (PSWQ; Meyer, Miller, Metzger, & Borkovec , 1990), a 16-item Likert-scale type instrument used primarily to assess trait-like as well as pathological worry (α = .90). A sample item is, “I worry all the time.” Participants reported the frequency with which they worry on a scale ranging from 1 (not at all typical of me) to 5 (very typical of me). A higher score indicates a greater tendency to worry. The PSWQ has shown strong internal consistency and overall validity (Meyer et al., 1990).
Rumination
Rumination was assessed using the Ruminative Responses Scale (RRS; Nolen-Hoeksema & Morrow, 1991). The RRS is a 22-item scale designed to assess ruminative tendencies (α = .87). A sample item is, “How often do you think: Why do I always react this way?” Participants reported the frequency with which they ruminate on a 1 (almost never) to 4 (almost always) scale. All 22 items were summed to create a total RRS score wherein a higher score indicates greater ruminative tendencies.
Subjective sleep quality
Self-reported sleep quality was assessed using the Pittsburgh Sleep Quality Index (PSQI; Buysse et al., 1989), a well-validated measure of subjective sleep quality, over the previous month. The 19 primary items were grouped to create seven component scores of overall sleep quality (e.g., duration, sleep efficiency, disturbance, restfulness, daytime dysfunction). These component scores were summed to generate a global or total score ranging from 0 to 21, with higher scores indicating poorer overall sleep quality, and scores greater than 5 indicating clinically significant poor sleep quality.
Covariates
As the extant literature documents gender differences in RD prevalence and vulnerability (Banks, Kohn-Wood, & Spencer, 2006; Sellers & Shelton, 2003) as well as in sleep complaints (Grandner, Patel, Gehrman, Xie, et al., 2010), we adjusted for gender (0 = female, 1 = male). Age was also included as a covariate, as age-related differences in RD experiences, PC, and sleep quality are likely. Finally, we included social class as a covariate, given the evidence linking social class (e.g., SES) to sleep (e.g., Mezick et al., 2008) and to racism exposure and vulnerability (Clark et al., 1999; Williams & Mohammed, 2009). Notably, subjective measures of social class or status have been shown to be more strongly and consistently related to psychological functioning, health outcomes, and disease risk factors (e.g., self-rated health, heart rate, sleep latency) as compared to objective indicators of social status (Demakakos, Nazroo, Breeze, & Marmot, 2008; Freeman, Bauldry, Volpe, Shanahan, & Shanahan, 2016; Singh-Manoux , Marmot, & Adler, 2005). Consistent with previous research examining social class or status via subjective social class identity categories (Jackman, 1979; Ostrove & Long, 2007), participants in the present study were instructed to indicate their subjective social status by selecting one of five possible categorical descriptors (i.e., 1 = Lower Class, 2 = Working Class, 3= Lower Middle Class, 4 = Upper Middle Class, 5= Upper/Higher Class).
Statistical analysis
Descriptive statistics were computed to characterize the sample. Pearson’s correlations (r) were computed to quantify associations between the study variables. Whereas mediation analysis is commonly associated with testing causal relationships, this statistical methodology or approach may also be applied to test theoretically derived hypotheses regarding the conditional or process-oriented relationships among a set of variables (Hayes 2012; Hayes, 2013; Preacher & Hayes, 2008). We employed the PROCESS computational macro designed by Hayes (2013) to test the hypothesis that worry (M1) and rumination (M2) would mediate the association between RD (X) and sleep (Y). PROCESS is a flexible model estimation utility that incorporates many standard methods (e.g., Baron & Kenny, 1986; MacKinnon, 2008) for testing conditional effects using an Ordinary Least Squares (OLS) regression approach. Point and interval estimates for direct effects (X→Y) are automatically generated in PROCESS, which further applies boot-strapping with replacement in the generation of the 95% confidence intervals (CIs) for the indirect effects (X→M→Y). Using bias-corrected bootstrap CIs is ideal, as the sampling distribution may not be normal (Hayes, 2013). To examine the potential mediating roles of worry and rumination while also accounting for their shared association, we simultaneously tested both candidate mediators using the PROCESS parallel mediator model (Model 4). There would be evidence of mediation if the product of the X→M1 coefficient (path a1) and the M1→Y coefficient (path b1) or the X→M2 coefficient (path a2) and the M2→Y coefficient (path b2) produces a bootstrapped coefficient (a1b1; a2b2) whose CI does not straddle zero. Age, gender, and social class were included as covariates in all analyses.
RESULTS
Descriptive statistics and correlations are reported in Table 1. We note that one person was missing data for the PEDQ-CV, three people were missing data for the PSQI, and one person was missing data for the PSWQ and RRS. These individuals were not included in the statistical analyses. A majority (95.6%) of the participants reported having experienced RD. The sample generally comprised low to moderate trait worriers and ruminators. Approximately two thirds (67.7%) of the sample scored above a 5 on the PSQI, suggesting that the sample generally had clinically significant poor sleep quality.
TABLE 1.
Descriptive Statistics and Correlations for Racial Discrimination, Mediators, Sleep Quality, and Covariates
| Correlations | |||||||
|---|---|---|---|---|---|---|---|
|
| |||||||
| Variable | M (SD) | 1 | 2 | 3 | 4 | 5 | 6 |
| 1. Age | 20.18 (2.93) | – | |||||
| 2. Class | 3.01 (0.95) | −.32** | – | ||||
| 3. Discrimination | 31.52 (10.03) | .00 | −.15 | – | |||
| 4. Worry | 48.96 (13.32) | .13 | −.04 | .18 | – | ||
| 5. Rumination | 43.90 (13.02) | .26* | –.18 | .36** | .56** | – | |
| 6. Sleep quality | 6.98 (3.41) | .31* | −.30* | .35** | .25* | .51** | – |
Note.
Participants’ self-reported social class: 1 = Lower Class (5.9%), 2 = Working Class (22.1%), 3 = Lower Middle Class (41.2%), 4 = Upper Middle Class (26.5%), 5 = Upper/Higher Class (4.4%).
p = .05,
p = .001.
There were no gender differences in RD exposure , subjective sleep quality , worry , or rumination .
Age was positively correlated with sleep quality (r = .31, p = .011) and rumination (r = .26, p = .037), but was uncorrelated with RD (r ≤ .001, p = .999) and worry (r = .13, p = .283). Social class was negatively correlated with sleep quality (r = −.30, p = .016), but was uncorrelated with RD (r = −.15, p = .225), rumination (r = −.18, p = .139), and worry (r = −.04, p = .769). Worry and rumination were moderately correlated (r = .56, p = <.001).
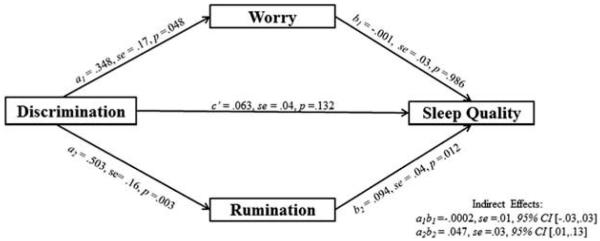
Results for our main analyses are reported in Table 2 and in Figure 1. The results revealed a significant total effect of RD on subjective sleep quality, b = .110, SE = .04, p = .008 (path c). We found that RD was positively associated with both worry, b = .348, SE = .17, p = .048 (path a1), and rumination, b = .503, SE = .16, p = .003 (path a2). Rumination, b = .094, SE = .04, p = .012 (path b2), but not worry, b = −.001, SE = .03, p = .986 (path b1), was positively associated with subjective sleep quality. We also found no significant indirect effect of RD on subjective sleep quality through worry, as the bootstrapped CIs straddled zero (a1b1 = −.0002, Bias-Corrected 95% CI [−.031, .026]). Conversely, there was a significant indirect effect of RD on subjective sleep quality through rumination, as the bootstrapped CI did not include zero (a2b2 = .047, Bias-Corrected 95% CI [.008, .125]).
TABLE 2.
Regression Coefficients, Standard Errors, and Model Summary Information for the Parallel Mediator Model
| Outcome | ||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
|
||||||||||||||||
| Worry | Rumination | Sleep Qualitya | Sleep Qualityb | |||||||||||||
|
|
|
|
|
|||||||||||||
| Predictor | Coefficien | SE | P | Coefficient | SE | P | Coefficient | SE | P | Coefficient | SE | P | ||||
| Discrimination | a1 | .35 | .17 | .048 | a2 | .50 | .16 | .003 | c’ | .06 | .04 | .132 | c | .11 | .04 | .008 |
| Worry | - | - | - | - | - | - | b1 | −.001 | .03 | .986 | - | - | - | |||
| Rumination | - | - | - | - | - | - | b2 | .09 | .04 | .012 | - | - | - | |||
| Age | .65 | .17 | .266 | 1.06 | .54 | .055 | .19 | .13 | .143 | .29 | .14 | .034 | ||||
| Gender | −7.07 | 3.42 | .043 | −1.91 | 3.18 | .551 | .43 | .78 | .586 | .25 | .80 | .754 | ||||
| Class | 1.00 | 1.82 | .589 | −.60 | 1.69 | .722 | −.56 | .40 | .166 | −.62 | .42 | .147 | ||||
| R2 =.12, p =.119 | R2 = .21, p =.008 | R2 = .36, p =.0002 | R2 =.25, p = .002 | |||||||||||||
Note.
= indirect effect model;
= direct effect model.
FIGURE 1.
A Effect of racial discrimination on subjective sleep quality.
B Indirect effect of racial discrimination on subjective sleep quality through PC.
DISCUSSION
The present study is among the first to examine PC as a functional mechanism in the association between RD and subjective sleep quality. Our results corroborate and build upon the findings of previous research demonstrating that RD is associated with poorer subjective sleep quality in African Americans. Consistent with our first hypothesis, we found that more frequent RD exposure was associated with poorer subjective sleep quality. In support of our second hypothesis, we found a significant indirect effect of RD on subjective sleep quality through rumination. Surprisingly and counter to previous research (i.e., Beatty et al., 2011), we did not find a significant indirect effect for worry. There are key differences that may account for this divergence. First, we utilized a measure of RD whereas Beatty and colleagues (2011) employed a measure of unfair treatment attributable to a number of factors (e.g., race, gender), and not race exclusively. Second, we assessed general or trait worry, not nighttime sleep-related worry. Research documents that nighttime sleep-related worry and stress near bedtime are associated with sleep impairment (Åkerstedt et al., 2012; Lancee, Eisma, van Zantem, & Topper, 2015), which in turn, may increase presleep arousal (Yeh, Wung, & Lin, 2015) that persists into and disrupts sleep. Based on this pattern, it is possible that African Americans engage both in reflection on previous discrimination experiences and worry about future experiences of discrimination at the end of the day. Future research examining both the intrusiveness and affective content of nighttime-related thoughts among African Americans would be illuminative.
In context, our findings are consistent with mounting evidence that rumination may be the more salient component of PC in the association between stressors and sleep impairment. In a recent investigation in college students with moderate depression, Pillai et al. (2014) examined the association between actigraphy-based sleep across a seven-day period and presleep rumination, which was retrospectively assessed each morning via a daily diary. These researchers found that presleep rumination significantly predicted longer actigraphy- and diary-based sleep onset latency (Pillai et al., 2014). Other research documents that individuals with higher levels of trait rumination experience more presleep intrusive thoughts and poorer self-reported sleep quality (Guastella & Moulds, 2007). Despite these findings, there is also evidence that both domains of PC mediate the impact of daily stress on sleep. For example, in a three-day ambulatory study, Dutch EMS helicopter pilots wore actigraphs and completed diary measures of work-related distress, worry and rumination (i.e., single items), and sleep quality. Work-shift related distress significantly predicted sleep onset latency, but this association was fully attenuated by the combined worry and rumination items (Radstaak et al., 2014). We posit that variations in measures used to assess rumination, worry, and sleep may account for some of the discrepancy across research studies. As the literature on PC and sleep continues to mature, it will become further evident whether it is rumination or worry alone, or their synergistic influence that drives the relationship between daily stressors and sleep. Irrespective of these mixed findings, one major implication of this previous work is that when PC is assessed may be as important as how (i.e., trait versus diary versus single-item measures).
There are several limitations of the present study that can inform future research. First, our sample comprises African American college students. Thus, our findings may have limited generalizability to the larger African American population with regard to variations in socioeconomic status, relative developmental stage, and controllability of other secondary factors that might influence sleep. It is further acknowledged that college students generally have poorer sleep hygiene and quality than noncollege samples (Hershner & Chervin, 2014); however, African American college students may not be any more or less likely than other African Americans to encounter RD, or to ponder and reflect upon these experiences. Second, although we employed mediation to test the theoretical function of PC, the present study is cross-sectional. Consequently, the data are limited in informing causal ordering in the association between RD and sleep quality. Longitudinal investigations are needed to assess temporality of the interrelations among RD, PC, and sleep quality over time and the long-term accumulative burden of RD on sleep. Finally, we only included self-reported sleep data. As PSG is the gold standard of sleep measurement, future studies may examine the interrelations among RD, PSG-measured sleep, and PC.
Limitations notwithstanding, our findings raise several considerations for research, practice, and intervention. Cognitive behavioral methods have been shown to be effective in improving some aspects of sleep (i.e., chronic insomnia; Trauer, Qian, Doyle, Rajaratnam, & Cunnington, 2015). However, it is unclear whether these findings extend to African Americans, who remain underrepresented in and are less likely to voluntarily participate in the clinical trials that develop and evaluate the efficacy of these treatments. Fortunately, there has been increasing attention to identifying and addressing such barriers (e.g., George, Duran, & Norris, 2014; Luebbert & Perez, 2016). This work may be of particular interest to researchers seeking to determine whether standard sleep interventions are effective in improving African Americans’ sleep.
Additionally, it may be important for practitioners working with African Americans both within and beyond sleep medicine contexts to further consider the exacerbating role of RD on broader mental health. RD is associated with a greater risk for depression among African Americans (for review, see, Lewis, Cogburn, & Williams, 2015), and African Americans may employ more ruminative coping, a common strategy used among individuals with depression, for race-related events as compared to non–race-related events (Hoggard, Byrd, & Sellers, 2012). There is also growing interest in the parallels between aspects of the qualitative experience of RD and features of clinical anxiety (e.g., Earl & Williams, 2009; Hunter & Schmidt, 2010; Soto, Dawson-Andoh, & BeLue, 2011). Paramount among these is hypervigilance, whose presence is well documented in generalized anxiety (GAD) and posttraumatic stress disorder (PTSD). Scholars have increasingly recognized that the constant anticipation of encountering future RD (i.e., vigilance) may be one of the most salient aspects of race-related stress (e.g., Hicken et al., 2013).
Although care should be taken to avoid pathologizing what is for many a chronic daily experience, it may be critical that clinicians and counselors aid their African American patients in identifying and minimizing the use of maladaptive coping strategies (e.g., rumination; worry) and developing more adaptive mechanisms for coping with RD. For example, several culturally based coping models have underscored the effectiveness of social support seeking (Harrell, 2000; Shorter-Gooden, 2004), Africultural coping (Utsey, Adams, & Bolden, 2000), and racial and ethnic identity development (Banks & Kohn-Wood, 2007; Helms, 1990). Other research indicates that values- and affirmations-based interventions, which encourage individuals to write about their experiences, values, and beliefs, may also be effective in improving coping among African Americans (for review, see Lewis et al., 2015). Testing the effectiveness of these interventions is a worthwhile endeavor, as they may be easily implemented in individual and community-based clinical and research settings.
CONCLUSION
Our findings suggest that the association between RD and sleep quality among African Americans may be twofold, both through a greater frequency of exposure as well as through reflection on past experiences of RD. Given the global importance of optimal sleep for maintaining and promoting mental and physical health, it is essential that the influence(s) of RD be addressed as a unique and pervasive stressor underlying disparities in sleep and other domains.
ACKNOWLEDGMENTS
We thank Giselle Corbie-Smith for her assistance with editing the introduction.
FUNDING
This research was supported by funding from The Ohio State University Office of Diversity & Inclusion, The Todd Anthony Bell National Resource Center on the African American Male, The Ohio State University Graduate School, The Ohio State University College of Social, Behavioral and Economic Sciences, the National Institute on Aging (5T32AG000029) and the National Heart, Lung, and Blood Institute (R01HL121708) to the second author [L.K.H.]). The first author (L.S.H.) was supported by funding from the National Science Foundation (537597).
Contributor Information
Lori S. Hoggard, Center for Health Equity Research, Department of Social Medicine and School of Medicine, University of North Carolina at Chapel Hill, Chapel Hill, North Carolina Institute of African American Research, University of North Carolina at Chapel Hill, Chapel Hill, North Carolina.
LaBarron K. Hill, Department of Psychiatry and Behavioral Sciences, Duke University Medical Center, Durham, North Carolina Center for Biobehavioral Health Disparities Research, Duke University, Durham, North Carolina; Center for the Study of Aging and Human Development, Duke University Medical Center, Durham, North Carolina.
REFERENCES
- Åkerstedt T, Orsini N, Petersen H, Axelsson J, Lekander M, Kecklund G. Predicting sleep quality from stress and prior sleep: A study of day-to-day covariation across six weeks. Sleep Medicine. 2012;13(6):674–679. doi: 10.1016/j.sleep.2011.12.013. [DOI] [PubMed] [Google Scholar]
- Banks KH, Kohn-Wood LP, Spencer M. An examination of the African American experience of everyday discrimination and symptoms of psychological distress. Community Mental Health Journal. 2006;42(6):555–570. doi: 10.1007/s10597-006-9052-9. [DOI] [PubMed] [Google Scholar]
- Banks KH, Kohn-Wood LP. The influence of racial identity profiles on the relationship between racial discrimination and depressive symptoms. Journal of Black Psychology. 2007;33(3):331–354. [Google Scholar]
- Baron RM, Kenny DA. The moderator-mediator variable distinction in social psychological research: Conceptual, strategic and statistical considerations. Journal of Personality and Social Psychology. 1986;51:1173–1182. doi: 10.1037//0022-3514.51.6.1173. [DOI] [PubMed] [Google Scholar]
- Beatty DL, Hall MH, Kamarck TA, Buysse DJ, Owens JF, Reis SE, Matthews KA. Unfair treatment is associated with poor sleep in African American and Caucasian adults: Pittsburgh SleepSCORE project. Health Psychology. 2011;30(3):351–359. doi: 10.1037/a0022976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Borkovec TD, Ray WJ, Stober J. Worry: A cognitive phenomenon intimately linked to affective, physiological, and interpersonal behavioral processes. Cognitive Therapy and Research. 1998;22(6):561–576. [Google Scholar]
- Brondolo E, Kelly KP, Coakley V, Gordon T, Thompson S, Levy E, Contrada RJ. The Perceived Ethnic Discrimination Questionnaire: Development and preliminary validation of a community version. Journal of Applied Social Psychology. 2005;35(2):335–365. [Google Scholar]
- Brosschot JF. Markers of chronic stress: Prolonged physiological activation and (un) conscious perseverative cognition. Neuroscience & Biobehavioral Reviews. 2010;35:46–50. doi: 10.1016/j.neubiorev.2010.01.004. [DOI] [PubMed] [Google Scholar]
- Brosschot JF, Gerin W, Thayer JF. The perseverative cognition hypothesis: A review of worry, prolonged stress-related physiological activation, and health. Journal of Psychosomatic Research. 2006;60:113–124. doi: 10.1016/j.jpsychores.2005.06.074. [DOI] [PubMed] [Google Scholar]
- Brosschot JF, Pieper S, Thayer JF. Expanding stress theory: Prolonged activation and perseverative cognition. Psychoneuroendocrinology. 2005;30(10):1043–1049. doi: 10.1016/j.psyneuen.2005.04.008. [DOI] [PubMed] [Google Scholar]
- Brosschot JF, Van Dijk E, Thayer JF. Daily worry is related to low heart rate variability during waking and the subsequent nocturnal sleep period. International Journal of Psychophysiology. 2007;63(1):39–47. doi: 10.1016/j.ijpsycho.2006.07.016. [DOI] [PubMed] [Google Scholar]
- Brosschot JF, Verkuil B, Thayer JF. Conscious and unconscious perseverative cognition: Is a large part of prolonged physiological activity due to unconscious stress? Journal of Psychosomatic Research. 2010;69(4):407–416. doi: 10.1016/j.jpsychores.2010.02.002. [DOI] [PubMed] [Google Scholar]
- Buysse DJ, Reynolds CF, Monk TH, Berman SR, Kupfer DJ. The Pittsburgh Sleep Quality Index: A new instrument for psychiatric practice and research. Psychiatry Research. 1989;28(2):193–213. doi: 10.1016/0165-1781(89)90047-4. [DOI] [PubMed] [Google Scholar]
- Clark R, Anderson NB, Clark VR, Williams DR. Racism as a stressor for African Americans: A biopsychosocial model. American Psychologist. 1999;54(10):805–816. doi: 10.1037//0003-066x.54.10.805. [DOI] [PubMed] [Google Scholar]
- Demakakos P, Nazroo J, Breeze E, Marmot M. Socioeconomic status and health: The role of subjective social status. Social Science & Medicine. 2008;67(2):330–340. doi: 10.1016/j.socscimed.2008.03.038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Durrence HH, Lichstein KL. The sleep of African Americans: A comparative review. Behavioral Sleep Medicine. 2006;4(1):29–44. doi: 10.1207/s15402010bsm0401_3. [DOI] [PubMed] [Google Scholar]
- Earl TR, Williams DR. Black Americans and mental health status: Complexities and new developments. In: Neville Helen A., Tynes Brendesha M., Utsey Shawn O., editors. Handbook of African American psychology. Sage; Thousand Oaks, CA: 2009. pp. 335–350. [Google Scholar]
- Freeman JA, Bauldry S, Volpe VV, Shanahan MJ, Shanahan L. Sex differences in associations between subjective social status and C-reactive protein in young adults. Psychosomatic Medicine. 2016;78(5):542–551. doi: 10.1097/PSY.0000000000000309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Friedman M, Bliznikas D, Klein M, Duggal P, Somenek M, Joseph NJ. Comparison of the incidences of obstructive sleep apnea-hypopnea syndrome in African Americans versus Caucasian Americans. Otolaryngology–Head and Neck Surgery. 2006;134:545–550. doi: 10.1016/j.otohns.2005.12.011. [DOI] [PubMed] [Google Scholar]
- Gallicchio L, Kalesan B. Sleep duration and mortality: A systematic review an meta-analysis. Journal of Sleep Research. 2009;18:148–158. doi: 10.1111/j.1365-2869.2008.00732.x. [DOI] [PubMed] [Google Scholar]
- George S, Duran N, Norris K. A systematic review of barriers and facilitators to minority research participation among African Americans, Latinos, Asian Americans, and Pacific Islanders. American Journal of Public Health. 2014;104(2):e16–e31. doi: 10.2105/AJPH.2013.301706. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gottlieb DJ, Redline S, Nieto FJ, Baldwin CM, Newman AB, Resnick HE, Punjabi NM. Association of usual sleep duration with hypertension: The Sleep Heart Health Study. Sleep. 2006;29(8):1009–1014. doi: 10.1093/sleep/29.8.1009. [DOI] [PubMed] [Google Scholar]
- Grandner MA, Hale L, Jackson N, Patel NP, Gooneratne NS, Troxel WM. Perceived racial discrimination as an independent predictor of sleep disturbance and daytime fatigue. Behavioral Sleep Medicine. 2012;10(4):235–249. doi: 10.1080/15402002.2012.654548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grandner MA, Patel NP, Gehrman PR, Perlis ML, Pack AI. Problems associated with short sleep: Bridging the gap between laboratory and epidemiological studies. Sleep Medicine Reviews. 2010;14:239–247. doi: 10.1016/j.smrv.2009.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grandner MA, Patel NP, Gehrman PR, Xie D, Sha D, Weaver T, Gooneratne N. Who gets the best sleep? Ethnic and socioeconomic factors related to sleep complaints. Sleep Medicine. 2010;11(5):470–478. doi: 10.1016/j.sleep.2009.10.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guastella AJ, Moulds ML. The impact of rumination on sleep quality following a stressful life event. Personality and Individual Differences. 2007;42(6):1151–1162. [Google Scholar]
- Hall M, Buysse DJ, Dew MA, Prigerson HG, Kupfer DJ, Reynolds CF., III. Intrusive thoughts and avoidance behaviors are associated with sleep disturbances in bereavement-related depression. Depression and Anxiety. 1997;6:106–112. [PubMed] [Google Scholar]
- Hall MH, Matthews KA, Kravitz HM, Gold EB, Buysse DJ, Bromberger JT, Sowers MF. Race and financial strain are independent correlates of sleep in midlife women: The Swan sleep study. Sleep. 2009;32:73–82. [PMC free article] [PubMed] [Google Scholar]
- Harrell SP. A multidimensional conceptualization of racism-related stress: Implications for the well-being of people of color. American Journal of Orthopsychiatry. 2000;70(1):42–57. doi: 10.1037/h0087722. [DOI] [PubMed] [Google Scholar]
- Hayes AF. PROCESS: A versatile computational tool for observed variable mediation, moderation, and conditional process modeling. 2012 [White paper]. Retrieved from http://www.afhayes.com/public/process2012.pdf.
- Hayes AF. Introduction to mediation, moderation, and conditional process analysis: A regression-based approach. Guilford Press; New York, NY: 2013. [Google Scholar]
- Helms JE. Black and White racial identity: Theory, research, and practice. Greenwood Press; New York, NY: 1990. [Google Scholar]
- Hershner SD, Chervin RD. Causes and consequences of sleepiness among college students. Nature and Science of Sleep. 2014;6:73–84. doi: 10.2147/NSS.S62907. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hicken MT, Lee H, Ailshire J, Burgard SA, Williams DR. “Every shut eye, ain’t sleep”: The role of racism-related vigilance in racial/ethnic disparities in sleep difficulty. Race and Social Problems. 2013;5(2):100–112. doi: 10.1007/s12552-013-9095-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hill LK, Hoggard LS, Richmond AS, Gray DL, Williams DP, Thayer JF. Examining the association between perceived discrimination and heart rate variability in African Americans. Cultural Diversity and Ethnic Minority Psychology. doi: 10.1037/cdp0000076. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hoggard LS, Byrd CM, Sellers RM. Comparison of African American college students’ coping with racially and nonracially stressful events. Cultural Diversity and Ethnic Minority Psychology. 2012;18(4):329–339. doi: 10.1037/a0029437. [DOI] [PubMed] [Google Scholar]
- Hunter LR, Schmidt NB. Anxiety psychopathology in African American adults: Literature review and development of an empirically informed sociocultural model. Psychological Bulletin. 2010;136(2):211–235. doi: 10.1037/a0018133. [DOI] [PubMed] [Google Scholar]
- Jackman MR. The subjective meaning of social class identification in the United States. Public Opinion Quarterly. 1979;43(4):443–462. [Google Scholar]
- Kelly WE. Worry and sleep length revisited: Worry, sleep length, and sleep disturbance ascribed to worry. The Journal of Genetic Psychology. 2002;163(3):296–304. doi: 10.1080/00221320209598685. [DOI] [PubMed] [Google Scholar]
- Kim EJ, Dimsdale JE. The effect of psychosocial stress on sleep: A review of polysomnographic evidence. Behavioral Sleep Medicine. 2007;5(4):256–278. doi: 10.1080/15402000701557383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kochanek KD, Arias E, Anderson RN. How did cause of death contribute to racial differences in life expectancy in the United States in 2010. NCHS Data Brief. 2013;125:1–8. [PubMed] [Google Scholar]
- Knutson KL, Van Cauter E, Rathouz PJ, DeLeire T, Lauderdale DS. Trends in the prevalence of short sleepers in the USA: 1975–2006. Sleep. 2010;33(1):37–45. doi: 10.1093/sleep/33.1.37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lancee J, Eisma MC, van Zanten KB, Topper M. When thinking impairs sleep: Trait, daytime and nighttime repetitive thinking in insomnia. Behavioral Sleep Medicine. 2015:1–17. doi: 10.1080/15402002.2015.1083022. [DOI] [PubMed] [Google Scholar]
- Lewis TT, Troxel WM, Kravitz HM, Bromberger JT, Matthews KA, Hall MH. Chronic exposure to everyday discrimination and sleep in a multiethnic sample of middle-aged women. Health Psychology. 2013;32(7):810–819. doi: 10.1037/a0029938. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lewis TT, Cogburn CD, Williams DR. Self-reported experiences of discrimination and health: scientific advances, ongoing controversies, and emerging issues. Annual Review of Clinical Psychology. 2015;11:407–440. doi: 10.1146/annurev-clinpsy-032814-112728. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Luebbert R, Perez A. Barriers to clinical research participation among African Americans. Journal of Transcultural Nursing. 2016;27(5):456–463. doi: 10.1177/1043659615575578. [DOI] [PubMed] [Google Scholar]
- MacKinnon DP. Introduction to statistical mediation analysis. Erlbaum; Mahwah, NJ: 2008. [Google Scholar]
- Meyer TJ, Miller ML, Metzger RL, Borkovec TD. Development and validation of the Penn State worry questionnaire. Behaviour Research and Therapy. 1990;28(6):487–495. doi: 10.1016/0005-7967(90)90135-6. [DOI] [PubMed] [Google Scholar]
- Mezick EJ, Matthews KA, Hall M, Strollo PJ, Jr., Buysse DJ, Kamarck TW, Reis SE. Influence of race and socioeconomic status on sleep: Pittsburgh Sleep SCORE project. Psychosomatic Medicine. 2008;70(4):410–416. doi: 10.1097/PSY.0b013e31816fdf21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miniño AM. Death in the United States. US Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Health Statistics; Hyattsville, MD: 2013. 2011. pp. 1–8. [Google Scholar]
- Nolen-Hoeksema S. Responses to depression and their effects on the duration of depressive episodes. Journal of Abnormal Psychology. 1991;100(4):569–582. doi: 10.1037//0021-843x.100.4.569. [DOI] [PubMed] [Google Scholar]
- Nolen-Hoeksema S. The role of rumination in depressive disorders and mixed anxiety/depressive symptoms. Journal of Abnormal Psychology. 2000;109(3):504–511. [PubMed] [Google Scholar]
- Nolen-Hoeksema S, Morrow J. A prospective study of depression and posttraumatic stress symptoms after a natural disaster: the 1989 Loma Prieta Earthquake. Journal of Personality and Social Psychology. 1991;61(1):115–121. doi: 10.1037//0022-3514.61.1.115. [DOI] [PubMed] [Google Scholar]
- Nota JA, Coles ME. Duration and timing of sleep are associated with repetitive negative thinking. Cognitive Therapy and Research. 2014:1–9. [Google Scholar]
- Ostrove JM, Long SM. Social class and belonging: Implications for college adjustment. The Review of Higher Education. 2007;30(4):363–389. [Google Scholar]
- Ottaviani C, Medea B, Lonigro A, Tarvainen M, Couyoumdjian A. Cognitive rigidity is mirrored by autonomic inflexibility in daily life perseverative cognition. Biological Psychology. 2015;107:24–30. doi: 10.1016/j.biopsycho.2015.02.011. [DOI] [PubMed] [Google Scholar]
- Pillai V, Steenburg LA, Ciesla JA, Roth T, Drake CL. A seven day actigraphy-based study of rumination and sleep disturbance among young adults with depressive symptoms. Journal of Psychosomatic Research. 2014;77(1):70–75. doi: 10.1016/j.jpsychores.2014.05.004. [DOI] [PubMed] [Google Scholar]
- Preacher KJ, Hayes AF. Asymptotic and resampling strategies for assessing and comparing indirect effects in multiple mediator models. Behavior Research Methods. 2008;40(3):879–891. doi: 10.3758/brm.40.3.879. [DOI] [PubMed] [Google Scholar]
- Radstaak M, Geurts SA, Beckers DG, Brosschot JF, Kompier MA. Work stressors, perseverative cognition and objective sleep quality: A longitudinal study among Dutch Helicopter Emergency Medical Service (HEMS) pilots. Journal of Occupational Health. 2014;56:469–477. doi: 10.1539/joh.14-0118-OA. [DOI] [PubMed] [Google Scholar]
- Redline S, Kirchner HL, Quan SF, Gottlieb DJ, Kapur V, Newman A. The effects of age, sex ethnicity, and sleep disordered breathing on sleep architecture. Archives of Internal Medicine. 2004;164:406–418. doi: 10.1001/archinte.164.4.406. [DOI] [PubMed] [Google Scholar]
- Sellers RM, Shelton NJ. The role of racial identity in perceived discrimination. Journal of Personality and Social Psychology. 2003;84(5):1079–1092. doi: 10.1037/0022-3514.84.5.1079. [DOI] [PubMed] [Google Scholar]
- Shorter-Gooden K. Multiple resistance strategies: How African American women cope with racism and sexism. Journal of Black Psychology. 2004;30:406–425. [Google Scholar]
- Singh-Manoux A, Marmot MG, Adler NE. Does subjective social status predict health and change in health status better than objective status? Psychosomatic Medicine. 2005;67(6):855–861. doi: 10.1097/01.psy.0000188434.52941.a0. [DOI] [PubMed] [Google Scholar]
- Slopen N, Lewis TT, Williams DR. Discrimination and sleep: A systematic review. Sleep Medicine. 2016;18:88–95. doi: 10.1016/j.sleep.2015.01.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Slopen N, Williams DR. Discrimination, other psychosocial stressors, and self-reported sleep duration and difficulties. Sleep. 2014;37(1):147–156. doi: 10.5665/sleep.3326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Soto JA, Dawson-Andoh NA, BeLue R. The relationship between perceived discrimination and generalized anxiety disorder among African Americans, Afro Caribbeans, and non-Hispanic Whites. Journal of Anxiety Disorders. 2011;25(2):258–265. doi: 10.1016/j.janxdis.2010.09.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Steffen PR, Bowden M. Sleep disturbance mediates the relationship between perceived racism and depressive symptoms. Ethnicity and Disease. 2006;16:16–21. [PubMed] [Google Scholar]
- Takano K, Sakamoto S, Tanno Y. Repetitive thought impairs sleep quality: An experience sampling study. Behavior Therapy. 2014;45(1):67–82. doi: 10.1016/j.beth.2013.09.004. [DOI] [PubMed] [Google Scholar]
- Thomas KS, Bardwell WA, Ancoli-Israel S, Dimsdale JE. The toll of ethnic discrimination on sleep architecture and fatigue. Health Psychology. 2006;25:635–642. doi: 10.1037/0278-6133.25.5.635. [DOI] [PubMed] [Google Scholar]
- Trauer JM, Qian MY, Doyle JS, Rajaratnam SM, Cunnington D. Cognitive behavioral therapy for chronic insomnia: A systematic review and meta-analysis. Annals of Internal Medicine. 2015;163(3):191–204. doi: 10.7326/M14-2841. [DOI] [PubMed] [Google Scholar]
- Utsey S, Adams E, Bolden M. Development and initial validation of the Africultural coping systems inventory. Journal of Black Psychology. 2000;26:194–215. [Google Scholar]
- U.S. Department of Health and Human Services Office of Disease Prevention and Health Promotion, Healthy people 2020. Sleep Health. 2016 Retrieved from https://www.healthypeople.gov/2020/topics-objectives/topic/sleep-health.
- Williams DR, Mohammed SA. Discrimination and racial disparities in health: Evidence and needed research. Journal of Behavioral Medicine. 2009;32:20–47. doi: 10.1007/s10865-008-9185-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yang TC, Park K. To what extent do sleep quality and duration mediate the effect of perceived discrimination on health? Evidence from Philadelphia. Journal of Urban Health. 2015;92(6):1024–1037. doi: 10.1007/s11524-015-9986-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yeh ZT, Wung SK, Lin CM. Pre-sleep arousal as a mediator of relationships among worry, rumination, and sleep quality. International Journal of Cognitive Therapy. 2015;8(1):21–34. [Google Scholar]
- Zoccola PM, Dickerson SS, Lam S. Rumination predicts longer sleep onset latency after an acute psychosocial stressor. Psychosomatic Medicine. 2009;71(7):771–775. doi: 10.1097/PSY.0b013e3181ae58e8. [DOI] [PubMed] [Google Scholar]