Abstract
Objectives
There is limited literature about physicians’ adherence to 2010 CDC Sexually Transmitted Diseases Treatment Guidelines specific to specimen collection/testing methods in adolescent females in the emergency setting. The objectives are to 1) Determine physician adherence to CDC guidelines for specimen collection/testing for chlamydia and gonorrhea, 2) Determine physician characteristics associated with guideline adherence and 3) Describe physicians’ knowledge of expedited partner therapy (EPT) laws.
Methods
This is a cross sectional, anonymous, Internet-based survey of physician members of the American Academy of Pediatrics Section of Emergency Medicine. Questions addressed practice patterns and knowledge through clinical scenarios of adolescent females. Descriptive statistics are used to report frequency. Chi square and Fisher’s exact analyses are used to compare physician subgroups: gender, years in practice, practice setting and geographical region.
Results
Overall, 257 physicians responded and 231 were analyzed; 62.4% female; 46.0% in practice for ≤ 7 years; 86.2% in academic medicine. Specimen collection/testing in an asymptomatic patient were consistent with guidelines for 85.6% of respondents, but decreased to 37.4% for a symptomatic patient. Guideline adherence was not different between physician subgroups. Only 30.4% of physicians reported state EPT law knowledge.
Conclusions
Adherence with the CDC guidelines for chlamydia/gonorrhea specimen collection/testing for adolescents in the emergency setting is inadequate and EPT knowledge is poor. With increased ED use by adolescents, it is critical physicians know and implement the current recommendations to improve adolescent health outcomes.
Introduction
Sexually transmitted infections (STIs) are a significant problem among adolescents that may result in considerable morbidity if left untreated. Half of all new cases of STIs diagnosed each year are among adolescents aged 15–24 years.1 The Centers for Disease Control and Prevention (CDC) Sexually Transmitted Diseases Treatment Guidelines contain information on target populations, specimen testing/collection, and treatment.2 The optimal specimen for chlamydia and gonorrhea testing in females is a provider or self-collected vaginal swab.2,3 A first void urine is acceptable, but will detect about 10% fewer infections.2–4 Cervical swabs requiring a more invasive speculum exam, while still acceptable, are no longer routinely recommended and their use should be limited.2,3,5 Indications for a speculum exam include lower abdominal pain and persistent vaginal discharge (Table 1).6 The recommended test is nucleic acid amplification testing (NAAT) because it is more accurate than traditional cultures for detecting chlamydia and gonorrhea genital tract infections.2–4
Table 1.
Indications for a pelvic exam7
| Persistent vaginal discharge |
| Dysuria or urinary tract symptoms in a sexually active female |
| Dysmenorrhea unresponsive to nonsteroidal anti-inflammatory drugs |
| Amenorrhea |
| Abnormal vaginal bleeding |
| Lower abdominal pain |
| Contraceptive counseling for an intrauterine device or diaphragm |
| Perform Pap test |
| Suspected/reported rape or sexual abuse |
| Pregnancy |
Optimal STI treatment is critical for adolescent females given the serious health consequences of untreated infections that include pelvic inflammatory disease and infertility. Adolescents are also known to have high rates of re-infection that are independently associated with the failure to treat their sexual partners.7,8 Providers should discuss with their adolescent patients the treatment of their sexual partners. In 2006, the CDC recommended expedited partner therapy (EPT) for the treatment of heterosexual partners in the past 60 days of patients diagnosed with chlamydia and/or gonorrhea when it is unlikely the partner will seek care.2,9 EPT has been associated with decreased gonorrheal or chlamydial infections in the index patient at follow up compared to standard referral requiring patients to notify partners themselves.10 While state statutes vary regarding this practice, EPT allows providers to either prescribe or dispense medication to their patients to give to their sexual partners without the provider ever examining the partner.9,11
Millions of adolescents use the emergency department (ED) as their primary site for healthcare.12 From 1997 to 2007, ED use increased by 22% among those <18 years old.13 Furthermore, ED utilization increases with increasing adolescent age, especially among females with genitourinary complaints.14 Recent literature estimates the prevalence rate of asymptomatic chlamydia or gonorrhea infections in pediatric ED to be about 5% and as high as 26% in symptomatic females.15–18 Prior research shows it is acceptable and feasible to provide some routine screening in the ED and thus STI screening in the ED may become standard care.18–20 The combination of high burden of adolescent STIs, increasing ED use and push for using the ED to screen asymptomatic patients positions physicians practicing in the pediatric emergency setting to be leaders in improving the testing and treatment of STIs. Doing so requires knowledge of the STI guidelines and proper adherence from physicians.
Translation of CDC recommendations into clinical practice has been shown to be inadequate.21–23 STI screening is infrequently performed in pediatric primary care clinics and a study of emergency medicine providers found only 24% adhered to the CDC pelvic inflammatory disease treatment guidelines in females 12 years and older.21,23 It is not known if physicians practicing pediatric emergency medicine adhere to the specimen collection/testing method portion of the 2010 CDC Sexually Transmitted Diseases Treatment Guidelines (referred throughout as STI collection/testing guidelines) for chlamydia and gonorrhea in adolescent females.
The primary objective of this study is to determine adherence to the STI collection/testing guidelines for chlamydia and use of EPT in adolescent females by physicians practicing in the pediatric emergency setting. Secondary objectives are to determine physician characteristics associated with adherence to the STI collection/testing guidelines and physician knowledge of state EPT laws.
Materials and Methods
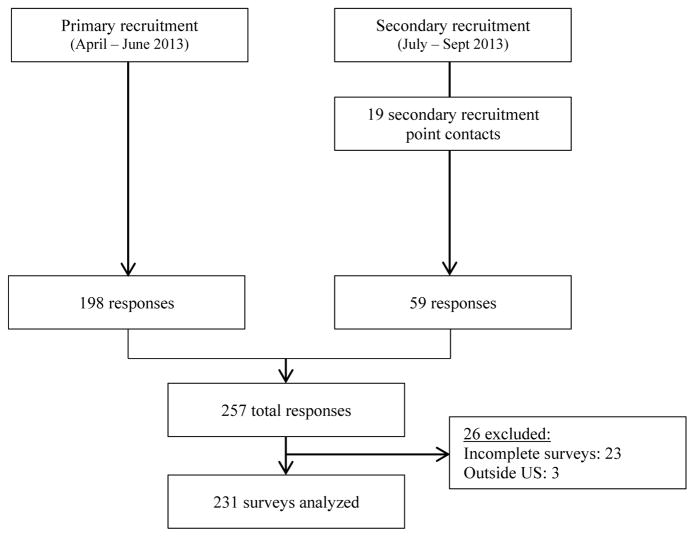
This is a national, anonymous, cross sectional internet-based survey of physicians providing emergency medical care for adolescents. The institutional review board of Children’s Hospital of Wisconsin approved this study. Qualtrics (www.qualtrics.com), an internet based survey tool, was used to create the survey, which was selected and approved by the American Academy of Pediatrics (AAP) Section of Emergency Medicine (SOEM). Any AAP member with an interest in pediatric emergency medicine can be part of the AAP SOEM, therefore respondents included pediatric emergency medicine physicians, emergency medicine physicians and general pediatricians, but membership is not limited to these specialties. As primary recruitment, the survey link was emailed to physician members of the AAP SOEM. Over a 9 week period (April—June 2013), participants received the initial recruitment email in addition to two more reminders. As a secondary recruitment method, 19 colleagues practicing in pediatric emergency departments from across the United States were asked to email the survey link to their practice partners; 242 survey links were distributed to 11 institutions (Figure 1). Physicians were asked to complete the survey if they had not previously done so through the AAP SOEM. This secondary recruitment period (July—September 2013) was also 9 weeks and was performed in a similar manner. Inclusion criteria were 1) English speaking physician and 2) provide care for adolescent females requiring assessment for chlamydia/gonorrhea. Resident physicians and students were excluded from the study population. Incomplete responses (surveys with three or fewer questions answered) and those from respondents outside the United States were excluded from analysis.
Figure 1.
Recruitment flow diagram.
The 10 minute, multiple choice 24-question survey was designed to query adherence with the STI collection/testing guidelines and use of EPT. Survey ideas and concepts were generated and categorized into four domains: specimen collection, specimen testing, use of EPT and EPT laws. After eliminating redundant items, the survey was formatted to develop succinct stems and appropriate response formats.24 Face validity of the survey was affirmed by a multi-disciplinary team of experts in the field, and ease of use and readability was pilot tested with 10 pediatricians. The survey included demographic questions and 4 different clinical adolescent scenarios with questions regarding the providers’ choice of specimen collection method and testing, as well as knowledge and use of expedited partner therapy (Appendix A). In all scenarios, the female adolescent patient had sex with one male partner with intermittent condom use. Scenarios differed by age of the patient and presence of acute discharge in either the patient or partner. Adherence to the STI collection/testing guidelines was defined as obtaining either a vaginal swab (provider or self-collected) or a urine sample and performance of a NAAT. Since obtaining a cervical swab is not routinely recommended and performing a culture is not the standard, for purposes of this study they were considered wrong answers. The survey had polymerase chain reaction (PCR) in the answer instead of NAAT. PCR is a common NAAT and will therefore be referred to NAAT throughout. Participants were only allowed to select one answer per question, but could skip questions if desired. At the completion of the survey, participants were provided a summary of the STI collection/testing and EPT recommendations to facilitate advancement of provider’s practice.
Descriptive statistics were performed to summarize demographic variables, adherence to the STI collection/testing guidelines and use/knowledge of EPT. Use of EPT was not analyzed with adherence to the STI collection/testing guidelines. Physician subgroups of interest included gender, years in practice (≤7 years or ≥8 years), practice type (academic or private) and geographical region (per United States region census).25 To determine the accuracy of the EPT knowledge questions, participants were analyzed according to the legal status of EPT in their state (ie permissible, prohibited, or potentially allowable). Respondents residing in ‘potentially allowable’ states were excluded since the only survey answers allowed were ‘allowed,’ ‘not allowed’ or ‘do not know.’ Chi square test was used to compare categorical variables and in cases of low frequency of groups, Fisher’s Exact test was used for comparison (SAS V 9.2, Cary, IN). An alpha of 0.05 was used for all statistical calculations.
Results
Two hundred fifty-seven (22.3%) responded to the survey, although 23 incomplete (three or less questions answered) surveys and three surveys from respondents outside the United States were excluded from analysis. Two hundred thirty-one surveys were included in the data analysis. Respondent characteristics are described in Table 2 with representation by gender, years in practice, practice type and region of the United States. Almost all the physicians were pediatric trained (96.9%) and practiced in a children’s or general ED (96.9%).
Table 2.
Respondent characteristics (N=231)
| n (%)^ | |
|---|---|
| Female | 141 (62.4) |
| Years in practice | |
| ≤7 years | 103 (46.0) |
| ≥8 years | 120 (54.0) |
| Practice type | |
| Private | 31 (13.8) |
| Academic | 194 (86.2) |
| Region | |
| Midwesta | 77 (35.2) |
| Northeastb | 54 (24.7) |
| Southc | 67 (30.6) |
| Westd | 21 (9.6) |
| Pediatric residency, % yes | 217 (96.9) |
| PEM fellowship, % yes | 187 (83.5) |
| Practice setting | |
| Children’s ED/urgent care | 210 (92.9) |
| General ED/urgent care | 9 (4.0) |
| Primary care clinic | 7 (3.1) |
Missing data is ≤5%. Percentages based on number of responses for each category.
Illinois, Indiana, Iowa, Kansas, Michigan, Minnesota, Missouri, Ohio, Nebraska, North Dakota, South Dakota, and Wisconsin
Connecticut, Maine, Massachusetts, New Hampshire, Rhode Island, Vermont, New Jersey, New York, and Pennsylvania
Alabama, Arkansas, Delaware, District of Columbia, Florida, Georgia, Kentucky, Louisiana, Maryland, Mississippi, North Carolina, Oklahoma, South Carolina, Tennessee, Texas, Virginia, West Virginia
Alaska, Arizona, California, Colorado, Hawaii, Idaho, Montana, Nevada, New Mexico, Oregon, Utah, Washington, Wyoming
Physician management of each scenario is presented in Table 3. Adherence to the STI collection/testing guidelines for asymptomatic females aged 14 and 18 were 87.4% and 85.6%, respectively. Adherence was lower if the partner reported symptoms (85.6% vs 70.4%, p<0.001) and was significantly lower when the patient developed vaginal discharge (85.6% vs 37.4%, p<0.001). Use of the cervical swab specimen was the most common response that did not adhere to the STI collection/testing guidelines. Sixty-one percent of physicians obtained a cervical swab when the patient was symptomatic with acute vaginal discharge. Prescription of EPT was consistently low in each scenario; 15.4% of symptomatic patients were prescribed EPT.
Table 3.
Overall rates of physician adherence to CDC STI collection/testing guidelines and use of expedited partner therapy prescription by scenario (N=231)^
| Scenario | ||||
|---|---|---|---|---|
| 14 year old asymptomatic patient | 18 years old asymptomatic patient | 18 years old asymptomatic patient with partner with penile discharge | 18 years old symptomatic patient with vaginal discharge only | |
| Adhered to CDC collection/testing guidelines (% yes) | 201 (87.4) | 196 (85.6) | 162 (70.4)* | 86 (37.4)* |
| Prescribed EPT (% yes) | 20 (8.8) | 25 (10.9) | 28 (12.3) | 35 (15.4) |
Missing data is ≤5%. Percentages based on number of responses for each category.
p<0.001when compared to the 18 year old asymptomatic patient scenario
No significant difference in proportion of physicians that adhered to the STI collection/testing guidelines was found when comparing subgroups by gender, years in practice, practice type or geographical region there was (Table 4). There was no difference in the proportion of physicians prescribing EPT by gender, years in practice, and practice type (Table 5). The proportion of physicians prescribing EPT was significantly different among geographical regions for the asymptomatic female patient with a symptomatic partner scenario. The Midwest had the lowest use of EPT and the West the highest (Midwest 5.3% vs Northeast 18.9% vs South 6.0% vs West 26.3%, p=0.006).
Table 4.
Rates of adherence to CDC STI collection/testing guidelines by subgroups (N=231)
| Scenario | ||||||||
|---|---|---|---|---|---|---|---|---|
| 14 year old asymptomatic patient | 18 years old asymptomatic patient | 18 years old asymptomatic patient with partner with penile discharge | 18 years old symptomatic patient with vaginal discharge only | |||||
| n (%) | p-value | n (%) | p-value | n (%) | p-value | n (%) | p-value | |
| Gender, n (%) | ||||||||
| Female | 124 (87.9) | 0.97 | 124 (87.9) | 0.44 | 101 (76.6) | 0.68 | 54 (38.3) | 0.98 |
| Male | 74 (88.1) | 70 (84.3) | 58 (69.0) | 32 (38.1) | ||||
| Years in practice, n (%) | ||||||||
| ≤7 years | 94 (91.3) | 0.15 | 91 (88.3) | 0.45 | 74 (71.8) | 0.66 | 39 (37.9) | 0.84 |
| ≥8 years | 102 (85.0) | 101 (84.9) | 83 (69.2) | 47 (39.2) | ||||
| Practice type, n (%) | ||||||||
| Private | 25 (80.6) | 0.23 | 24 (77.4) | 0.15 | 19 (61.3) | 0.20 | 12 (38.7) | 0.97 |
| Academic | 172 (89.1) | 169 (88.0) | 140 (72.5) | 74 (38.3) | ||||
| Region, n (%) | ||||||||
| Midwesta | 67 (87.0) | 0.97 | 68 (88.3) | 0.86 | 55 (71.4) | 0.93 | 23 (29.9) | 0.27 |
| Northeastb | 48 (88.9) | 47 (87.0) | 40 (74.1) | 24 (44.4) | ||||
| Southc | 59 (88.1) | 55 (83.3) | 46 (68.7) | 28 (42.1) | ||||
| Westd | 17 (85.0) | 17 (85.0) | 14 (70.0) | 9 (45.0) | ||||
Illinois, Indiana, Iowa, Kansas, Michigan, Minnesota, Missouri, Ohio, Nebraska, North Dakota, South Dakota, and Wisconsin
Connecticut, Maine, Massachusetts, New Hampshire, Rhode Island, Vermont, New Jersey, New York, and Pennsylvania
Alabama, Arkansas, Delaware, District of Columbia, Florida, Georgia, Kentucky, Louisiana, Maryland, Mississippi, North Carolina, Oklahoma, South Carolina, Tennessee, Texas, Virginia, West Virginia
Alaska, Arizona, California, Colorado, Hawaii, Idaho, Montana, Nevada, New Mexico, Oregon, Utah, Washington, Wyoming
Table 5.
Rates of expedited partner therapy by subgroups (N=231)
| Scenario | ||||||||
|---|---|---|---|---|---|---|---|---|
| 14 year old asymptomatic patient | 18 years old asymptomatic patient | 18 years old asymptomatic patient with partner with penile discharge | 18 years old symptomatic patient with vaginal discharge only | |||||
| n (%) | p-value | n (%) | p-value | n (%) | p-value | n (%) | p-value | |
| Gender, n (%) | ||||||||
| Female | 15 (10.8) | 0.23 | 17 (12.1) | 0.56 | 16 (11.5) | 0.88 | 20 (14.5) | 0.97 |
| Male | 5 (6.0) | 8 (9.5) | 9 (10.8) | 12 (14.3) | ||||
| Years in practice, n (%) | ||||||||
| ≤7 years | 9 (8.7) | 0.86 | 11 (10.7) | 0.82 | 10 (9.8) | 0.50 | 14 (13.9) | 0.79 |
| ≥8 years | 11 (9.4) | 14 (11.7) | 15 (12.7) | 18 (15.1) | ||||
| Practice type, n (%) | ||||||||
| Private | 3 (9.7) | 1.00 | 3 (9.7) | 1.00 | 2 (6.9) | 0.54 | 4 (12.9) | 1.00 |
| Academic | 17 (8.9) | 22 (11.4) | 23 (12.0) | 28 (14.7) | ||||
| Region, n (%) | ||||||||
| Midwesta | 7 (9.2) | 0.52 | 7 (9.1) | 0.31 | 4 (5.3) | 0.006 | 7 (9.2) | 0.20 |
| Northeastb | 7(13.2) | 8 (14.8) | 10 (18.9) | 10 (18.5) | ||||
| Southc | 4 (6.1) | 5 (7.5) | 4 (6.0) | 9 (13.6) | ||||
| Westd | 1 (5.0) | 4 (20.0) | 5 (26.3) | 5 (26.3) | ||||
Illinois, Indiana, Iowa, Kansas, Michigan, Minnesota, Missouri, Ohio, Nebraska, North Dakota, South Dakota, and Wisconsin
Connecticut, Maine, Massachusetts, New Hampshire, Rhode Island, Vermont, New Jersey, New York, and Pennsylvania
Alabama, Arkansas, Delaware, District of Columbia, Florida, Georgia, Kentucky, Louisiana, Maryland, Mississippi, North Carolina, Oklahoma, South Carolina, Tennessee, Texas, Virginia, West Virginia
Alaska, Arizona, California, Colorado, Hawaii, Idaho, Montana, Nevada, New Mexico, Oregon, Utah, Washington, Wyoming
Few respondents, 68 (30.4%), report knowledge of their state EPT laws. Respondents practicing in an academic setting were more likely to self-report knowledge of state EPT laws compared to those in private practice (33.2% vs 13.3%, p=0.03). There was no difference in knowledge of EPT when comparing provider gender (p=0.29), years in practice (p=0.22), or region (p=0.57). We evaluated the accuracy of the 68 participants that reported knowledge of their state’s EPT laws. Thirteen were excluded from this analysis, three did not report a state and ten live in states in which EPT is ‘potentially allowable’ therefore accuracy could not be determined. Fifty-five participants were included in this analysis. Thirty-seven (67.3%) thought their state allows EPT and most, 34 (91.9%), were correct. Eighteen (32.7%) thought their state prohibits EPT and 7 (38.9%) were correct. Overall, 41 (17.7%) of all study participants had correct knowledge of state EPT laws.
Discussion
This study demonstrated adherence to the STI collection/testing guidelines by physicians in the pediatric emergency setting was poor for symptomatic adolescent female patients. Use of a cervical swab instead of a vaginal swab or urine sample was the most common reason for lack of adherence. This is noteworthy because vaginal swabs are as accurate for diagnosis as cervical swabs and are less invasive and anxiety provoking to adolescents.4,26 The high prevalence of chlamydia/gonorrhea among symptomatic adolescent females in the ED and push for screening in the ED highlights the importance of improved STI collection/testing guideline adherence and increased use of EPT.15,17,18
Comparison of physician subgroups found no differences in the STI collection/testing guideline adherence. Review of previous literature, including the use of emergency contraception among physicians in the emergency setting, does not show any consistent trends in adherence to guidelines based on provider characteristics such as gender, years in practice, geographical region or practice type.21,27–29 Therefore our results are not unexpected and support the use of broadly implemented interventions to improve collection/testing adherence instead of targeting specific subgroups.
A lag in knowledge translation may be one reason for discrepancy between the guideline recommendations and the reported physician practice. Knowledge translation is defined as “a dynamic and iterative process that includes the synthesis, dissemination, exchange and ethically sound application of knowledge to improve the health of patients, provide more effective health services and products and strengthen the health care system,” by the Canadian Institutes of Health Research.30 These findings are consistent with the Institute of Health report that it takes 17 years for new knowledge to be translated into clinical practice.31 Prior studies have shown lack of adherence may be multifactorial including a lack of knowledge of the updated guidelines, derivation of guidelines outside of emergency medicine, distrust/disagreement with the recommended collection/testing methods and EPT, multiple/complex recommendation, and hesitancy to change.22,32–36 While our study did not specifically address why there is a lack of adherence to the guidelines, it is not unreasonable to assume these factors play a role in our participant adherence.
Although EPT is effective and supported by the CDC, AAP, Society for Adolescent Health and Medicine, and the American College of Obstetrics and Gynecology,9,37–39 our study highlighted that the physicians we studied rarely prescribe EPT. During study recruitment, EPT was permissible in 32 states by law, potentially allowed in 11 states including District of Columbia, and prohibited in 7 states.11 Cramer et al used data from the STI Surveillance Network and found 9.5% of patients eligible for EPT reported receiving EPT for their partner, similar to what was observed in our study.40 A nine state study of physicians practicing in specialties that treat adolescents, found while 63% of providers support EPT, only 20% reported ever offering EPT.41 Barriers to prescribing EPT have been identified including minimal physician resident education, costs, and legal considerations.40–45 Most of the physicians surveyed in our study did not know state EPT laws and of those who thought EPT was illegal, over half were incorrect. EPT is governed by the state, not national law, and there is wide variation in state practices. For example, in some states the medication can be dispensed, opposed to a prescription for the medication, and in others, if the patient does not know or is unwilling to disclose the partner’s name, the provider is allowed to write ‘expedited partner therapy’ instead of a name on the prescription. Electronic medical record prescribing may also hinder EPT prescription, as it is difficult to electronically prescribe to the partner if he/she is not registered in the medical records.46
This study has limitations. As primary recruitment, the survey was only emailed to members of the AAP which may be a biased sample. But as the largest pediatrician organization with national representation, this sampling provided the optimal cross section of pediatricians working in the emergency setting. The recruitment methodology used may have included non-AAP SOEM physicians, yet all participants in the secondary recruitment were PEM trained. There was no mechanism in place to prohibit physicians from taking the survey multiple times which would reduce the response rate. These results may not be generalized to other physician subspecialties. Those who did participate may have an interest in this topic or may have responded differently from actual practice both of which potentially overestimates adherence to the STI collection/testing guidelines and EPT use/knowledge. Lastly, the survey sent to participants stated ‘PCR’ in the survey answers, instead of ‘NAAT’. As there are other forms of NAATs available, some participants may not have recognized PCR as a form of NAAT.
Our study found poor physician compliance with the STI collection/testing guidelines for chlamydia and gonorrhea in adolescent females. Additionally, use of expedited partner treatment for adolescents in the emergency setting is inadequate. This study highlights the need for improved adherence to the STI collection/testing guidelines, increased EPT knowledge, and appropriate EPT use in the ED setting. Results may inform the development of a novel intervention to optimize care and bridge the gap between knowledge and practice in the pediatric ED setting.
Acknowledgments
Funding Source: This study was supported by the National Center for Advancing Translational Sciences, National Institutes of Health, through Grant Number 8UL1TR000055.
We acknowledge the following people and groups: The Pediatric Emergency Medicine Collaborative Research Committee of the American Academy of Pediatrics Section of Emergency Medicine for selecting and distributing survey. Tao Wang, PhD, biostatistician assisted in data analyses. David Brousseau MD, MS provided critical review of study design. Viday Heffner, MD assisted with the survey development. This publication was supported by the National Center for Advancing Translational Sciences, National Institutes of Health, through Grant Number 8UL1TR000055. Its contents are solely the responsibility of the authors and do not necessarily represent the official views of the NIH.
Appendix A
(Questions with correct responses are bolded)
Q1 What percentage of the population
that you treat is aged 14–18 years?
|
Q2 If appropriate in the context of
the patient visit, do you test/screen for gonorrhea/chlamydia?
|
Q3 During the average month, how often
do you test/screen for gonorrhea or chlamydia in adolescent
female patients, less than 18 years old?
|
Q4 A 14 year old female presents
requesting testing for gonorrhea and chlamydia. She is sexually
active with a male partner. Sometimes they use condoms. Neither
she nor her partner has had any symptoms. How would you collect
a sample for gonorrhea/chlamydia testing for this asymptomatic
14 year old patient?
|
Q5 If treatment is indicated for this
asymptomatic 14 year old female, with regards to her partner, do
you:
|
Q6 A female patient presents with the
same complaints as the previous scenario. Please note the
patient is now an 18 years old female. How would you collect a
sample for gonorrhea/chlamydia testing for this asymptomatic 18
year old female?
|
Q7 If treatment is indicated for this
asymptomatic 18 year old female with regards to her partner, do
you:
|
Q8 The same 18 year old female from
the previous scenario presents requesting testing for gonorrhea
and chlamydia. She remains asymptomatic, but now her male
partner has penile discharge. How would you collect a sample for
gonorrhea/chlamydia testing for this asymptomatic 18 year old
female, with a symptomatic partner?
|
Q9 If treatment is indicated for this
18 year old female with regards to her symptomatic partner, do
you:
|
Q10 The same 18 year old female from
the previous scenario presents requesting testing for gonorrhea
and chlamydia. She was asymptomatic, but now is complaining of
vaginal discharge. How would you collect a sample for
gonorrhea/chlamydia testing for this symptomatic 18 year old
female?
|
Q11 If treatment is indicated for this
symptomatic 18 year old female, with regards to her partner, do
you:
|
Q12 If offered a choice, which method
of collection do you think your female adolescent patients would
prefer?
|
| Q13 What do you think is the biggest
barrier to using the method of collection that your patients
would choose in the previous question? None, I use that method of collection
|
| Q14 In which state does the majority of your clinical practice occur? |
Q15 With regards to treating partners
of patients, the laws of my state in which the majority of my
practice is located:
|
Q16 If your patient does not know or
is unwilling to disclosure her partners’ names, my state
law:
|
Q17 How familiar are you with the most
recent CDC guidelines for gonorrhea/chlamydia?
|
Q18 As diagnostic and treatment
recommendations change for adolescents, what method do you think
best supports implementing evidence based practices?
|
Q19 What is your gender?
|
Q20 What is the setting of your
clinical practice?
|
Q21 How would you describe the
majority of your clinical practice?
|
Q22 What type of residency program did
you complete?
|
Q23 Did you complete fellowship
training?
|
Q24 How many years since you completed
your entire medical training?
|
The original survey sent to participants listed PCR instead of NAAT as an option.
Footnotes
Financial disclosure: The authors have no financial relationships relevant to this article to disclosure.
Conflict of interest: The authors have no conflicts of interest to disclose.
References
- 1.Centers for Disease Control and Prevention. Sexually transmitted disease surveillance. Atlanta: U.S. Department of Health and Human Services; 2013. [Accessed January 27, 2015]. http://www.cdc.gov/std/stats13/surv2013-print.pdf. Updated 2014. [Google Scholar]
- 2.Workowski KA, Berman S. Sexually transmitted diseases treatment guidelines, 2010. MMWR Recomm Rep. 2010;59(RR-12):1–110. [PubMed] [Google Scholar]
- 3.Association of Public Health Laboratories. Laboratory diagnostic testing for Chlamydia trachomatis and Neisseria gonorrhoeae. Expert consultation meeting summary report; Atlanta, GA. January 13–15, 2009; [Accessed January 28, 2013]. http://www.aphl.org/aphlprograms/infectious/std/documents/ctgclabguidelinesmeetingreport.pdf. [Google Scholar]
- 4.Centers for Disease Control and Prevention. Recommendations for the laboratory-based detection of Chlamydia trachomatis and Neisseria gonorrhoeae--2014. MMWR Recomm Rep. 2014;63(RR-02):1–19. [PMC free article] [PubMed] [Google Scholar]
- 5.Murray PJ, Braverman PK, Adelman WP, et al. Screening for nonviral sexually transmitted infections in adolescents and young adults. Pediatrics. 2014;134(1):e302–e311. doi: 10.1542/peds.2014-1024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Braverman PK, Breech L Committee on Adolescence. American Academy of Pediatrics. clinical report--gynecologic examination for adolescents in the pediatric office setting. Pediatrics. 2010;126(3):583–590. doi: 10.1542/peds.2010-1564. [DOI] [PubMed] [Google Scholar]
- 7.Rietmeijer CA, Van Bemmelen R, Judson FN, Douglas JM., Jr Incidence and repeat infection rates of Chlamydia trachomatis among male and female patients in an STD clinic: Implications for screening and rescreening. Sex Transm Dis. 2002;29(2):65–72. doi: 10.1097/00007435-200202000-00001. [DOI] [PubMed] [Google Scholar]
- 8.Scott Lamontagne D, Baster K, Emmett L, et al. Incidence and reinfection rates of genital chlamydial infection among women aged 16–24 years attending general practice, family planning and genitourinary medicine clinics in England: A prospective cohort study by the chlamydia recall study advisory group. Sex Transm Infect. 2007;83(4):292–303. doi: 10.1136/sti.2006.022053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Handsfield HH, Hogben M, Schillinger J, Golden MR, Kissinger P, Sparling PF. Expedited partner therapy in the management of sexually transmitted diseases. Atlanta, GA: Centers for Disease Control and Prevention; 2006. [Google Scholar]
- 10.Golden MR, Whittington WL, Handsfield HH, et al. Effect of expedited treatment of sex partners on recurrent or persistent gonorrhea or chlamydial infection. N Engl J Med. 2005;352(7):676–685. doi: 10.1056/NEJMoa041681. [DOI] [PubMed] [Google Scholar]
- 11.Centers for Disease Control and Prevention. Legal status of expedited partner therapy. Atlanta: U.S. Department of Health and Human Services; [Accessed February 5, 2013]. http://www.cdc.gov/std/ept/legal/default.htm. [Google Scholar]
- 12.Wilson KM, Klein JD. Adolescents who use the emergency department as their usual source of care. Arch Pediatr Adolesc Med. 2000;154(4):361–365. doi: 10.1001/archpedi.154.4.361. [DOI] [PubMed] [Google Scholar]
- 13.Tang N, Stein J, Hsia RY, Maselli JH, Gonzales R. Trends and characteristics of US emergency department visits, 1997–2007. JAMA. 2010;304(6):664–670. doi: 10.1001/jama.2010.1112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ziv A, Boulet JR, Slap GB. Emergency department utilization by adolescents in the United States. Pediatrics. 1998;101(6):987–994. doi: 10.1542/peds.101.6.987. [DOI] [PubMed] [Google Scholar]
- 15.Uppal A, Chou KJ. Screening adolescents for sexually transmitted infections in the pediatric emergency department. Pediatr Emerg Care. 2015;31(1):20–24. doi: 10.1097/PEC.0000000000000322. [DOI] [PubMed] [Google Scholar]
- 16.Miller MK, Dowd MD, Harrison CJ, Mollen CJ, Selvarangan R, Humiston SG. Prevalence of 3 sexually transmitted infections in a pediatric emergency department. Pediatr Emerg Care. 2015;31(2):107–112. doi: 10.1097/PEC.0000000000000284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Goyal M, Hayes K, Mollen C. Sexually transmitted infection prevalence in symptomatic adolescent emergency department patients. Pediatr Emerg Care. 2012;28(12):1277–1280. doi: 10.1097/PEC.0b013e3182767d7c. [DOI] [PubMed] [Google Scholar]
- 18.Goyal MK, Teach SJ, Badolato GM, Trent M, Chamberlain JM. Universal screening for sexually transmitted infections among asymptomatic adolescents in an urban emergency department: High acceptance but low prevalence of infection. J Pediatr. 2016 doi: 10.1016/j.jpeds.2016.01.019. [published online Feb 2, 2016] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Williams JR, Ho ML, Grupp-Phelan J. The acceptability of mental health screening in a pediatric emergency department. Pediatr Emerg Care. 2011;27(7):611–615. doi: 10.1097/PEC.0b013e318222554e. [DOI] [PubMed] [Google Scholar]
- 20.Rhodes KV, Lauderdale DS, Stocking CB, Howes DS, Roizen MF, Levinson W. Better health while you wait: A controlled trial of a computer-based intervention for screening and health promotion in the emergency department. Ann Emerg Med. 2001;37(3):284–291. doi: 10.1067/mem.2001.110818. [DOI] [PubMed] [Google Scholar]
- 21.Shih TY, Gaydos CA, Rothman RE, Hsieh YH. Poor provider adherence to the centers for disease control and prevention treatment guidelines in US emergency department visits with a diagnosis of pelvic inflammatory disease. Sex Transm Dis. 2011;38(4):299–305. doi: 10.1097/OLQ.0b013e31820b8bb4. [DOI] [PubMed] [Google Scholar]
- 22.Kane BG, Degutis LC, Sayward HK, D’Onofrio G. Compliance with the centers for disease control and prevention recommendations for the diagnosis and treatment of sexually transmitted diseases. Acad Emerg Med. 2004;11(4):371–377. doi: 10.1197/j.aem.2003.11.016. [DOI] [PubMed] [Google Scholar]
- 23.Goyal MK, Witt R, Hayes KL, Zaoutis TE, Gerber JS. Clinician adherence to recommendations for screening of adolescents for sexual activity and sexually transmitted infection/human immunodeficiency virus. J Pediatr. 2014;165(2):343–347. doi: 10.1016/j.jpeds.2014.04.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Burns KE, Duffett M, Kho ME, et al. A guide for the design and conduct of self-administered surveys of clinicians. CMAJ. 2008;179(3):245–252. doi: 10.1503/cmaj.080372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.United States Census Bureau. [Accessed October 1, 2013];Census divisions and census regions. www.census.gov/geo/reference/gtc/gtc_census_divreg.html.
- 26.Serlin M, Shafer M, Tebb K, et al. What sexually transmitted disease screening method does the adolescent prefer?: Adolescents’ attitudes toward first-void urine, self-collected vaginal swab, and pelvic examination. Arch Pediatr Adolesc Med. 2002;156(6):588–591. doi: 10.1001/archpedi.156.6.588. [DOI] [PubMed] [Google Scholar]
- 27.McKinlay JB, Link CL, Freund KM, Marceau LD, O’Donnell AB, Lutfey K. Sources of variation in physician adherence with clinical guidelines: Results from a factorial experiment. J Gen Intern Med. 2007;22(3):289–296. doi: 10.1007/s11606-006-0075-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Golden NH, Seigel WM, Fisher M, et al. Emergency contraception: Pediatricians’ knowledge, attitudes, and opinions. Pediatrics. 2001;107(2):287–292. doi: 10.1542/peds.107.2.287. [DOI] [PubMed] [Google Scholar]
- 29.Choudhry NK, Fletcher RH, Soumerai SB. Systematic review: The relationship between clinical experience and quality of health care. Ann Intern Med. 2005;142(4):260–273. doi: 10.7326/0003-4819-142-4-200502150-00008. [DOI] [PubMed] [Google Scholar]
- 30.Canadian Institutes of Health Research. [Accessed September 20, 2014];More about knowledge translation at CIHR. http://www.cihr-irsc.gc.ca/e/39033.html. Updated 2014.
- 31.Institute of Medicine. Committee on Quality of Health Care in America. Crossing the Quality Chasm: A New Health System for the 21st Century [online book] Washington, DC: National Academy Press; 2001. http://books.nap.edu/openbook.php?record_id=10027&page=R1. [Google Scholar]
- 32.Lugtenberg M, Zegers-van Schaick JM, Westert GP, Burgers JS. Why don’t physicians adhere to guideline recommendations in practice? an analysis of barriers among Dutch general practitioners. Implement Sci. 2009;4(54):5908–5904. doi: 10.1186/1748-5908-4-54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Cochrane LJ, Olson CA, Murray S, Dupuis M, Tooman T, Hayes S. Gaps between knowing and doing: Understanding and assessing the barriers to optimal health care. J Contin Educ Health Prof. 2007;27(2):94–102. doi: 10.1002/chp.106. [DOI] [PubMed] [Google Scholar]
- 34.Wahabi HA, Alziedan RA. Reasons behind non-adherence of healthcare practitioners to pediatric asthma guidelines in an emergency department in Saudi Arabia. BMC Health Serv Res. 2012;12 doi: 10.1186/1472-6963-12-226. 226-6963-12-226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Andrews AL, Teufel RJ, 2nd, Basco WT., Jr Initiating inhaled steroid treatment for children with asthma in the emergency room: Current reported prescribing rates and frequently cited barriers. Pediatr Emerg Care. 2013;29(9):957–962. doi: 10.1097/PEC.0b013e3182a219d0. [DOI] [PubMed] [Google Scholar]
- 36.Ebben R, Vloet L, Verhofstad M, Meijer S, Mintjes-de Groot J, van Achterberg T. Adherence to guidelines and protocols in the prehospital and emergency care setting: A systematic review. Scand J Trauma Resusc Emerg Med. 2013;21(9) doi: 10.1186/1757-7241-21-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Burstein GR, Eliscu A, Ford K, et al. Expedited partner therapy for adolescents diagnosed with chlamydia or gonorrhea: A position paper of the society for adolescent medicine. J Adolesc Health. 2009;45(3):303–309. doi: 10.1016/j.jadohealth.2009.05.010. [DOI] [PubMed] [Google Scholar]
- 38.American Academy of Pediatrics. Statement of endorsement—expedited partner therapy for adolescents diagnosed with chlamydia or gonorrhea. Pediatrics. 2009;124:1264. [Google Scholar]
- 39.American College of Obstetricians and Gynecologists. Committee opinion no 506: Expedited partner therapy in the management of gonorrhea and chlamydia by obstetrician-gynecologists. Obstet Gynecol. 2011;118(3):761–766. doi: 10.1097/AOG.0b013e3182310cee. [DOI] [PubMed] [Google Scholar]
- 40.Cramer R, Leichliter JS, Stenger MR, Loosier PS, Slive L SSuN Working Group. The legal aspects of expedited partner therapy practice: Do state laws and policies really matter? Sex Transm Dis. 2013;40(8):657–662. doi: 10.1097/01.OLQ.0000431358.18959.d4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Lee S, Dowshen N, Matone M, Mollen C. Variation in practice of expedited partner therapy for adolescents by state policy environment. J Adolesc Health. 2015;57(3):348–350. doi: 10.1016/j.jadohealth.2015.05.013. [DOI] [PubMed] [Google Scholar]
- 42.Hsii A, Hillard P, Yen S, Golden NH. Pediatric residents’ knowledge, use, and comfort with expedited partner therapy for STIs. Pediatrics. 2012;130(4):705–711. doi: 10.1542/peds.2011-3764. [DOI] [PubMed] [Google Scholar]
- 43.Golden MR, Estcourt CS. Barriers to the implementation of expedited partner therapy. Sex Transm Infect. 2011;87(Suppl 2):ii37–8. doi: 10.1136/sti.2010.047670. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Gift TL, Kissinger P, Mohammed H, Leichliter JS, Hogben M, Golden MR. The cost and cost-effectiveness of expedited partner therapy compared with standard partner referral for the treatment of chlamydia or gonorrhea. Sex Transm Dis. 2011;38(11):1067–1073. doi: 10.1097/OLQ.0b013e31822e9192. [DOI] [PubMed] [Google Scholar]
- 45.McBride KR, Goldsworthy RC, Fortenberry JD. Patient and partner perspectives on patient-delivered partner screening: Acceptability, benefits, and barriers. AIDS Patient Care STDS. 2010;24(10):631–637. doi: 10.1089/apc.2010.0109. [DOI] [PubMed] [Google Scholar]
- 46.Introcaso CE, Rogers ME, Abbott SA, Gorwitz RJ, Markowitz LE, Schillinger JA. Expedited partner therapy in federally qualified health centers--New York City, 2012. Sex Transm Dis. 2013;40(11):881–885. doi: 10.1097/OLQ.0000000000000045. [DOI] [PubMed] [Google Scholar]