Abstract
Background
Asthma and obliterative bronchiolitis (OB) cases have occurred among styrene-exposed workers. We aimed to investigate styrene as a risk factor for non-malignant respiratory disease (NMRD).
Methods
From a literature review, we identified case reports and assessed cross-sectional and mortality studies for strength of evidence of positive association (i.e., strong, intermediate, suggestive, none) between styrene exposure and NMRD-related morbidity and mortality.
Results
We analyzed 55 articles and two unpublished case reports. Ten OB cases and eight asthma cases were identified. Six (75%) asthma cases had abnormal styrene inhalation challenges. Thirteen (87%) of 15 cross-sectional studies and 12 (50%) of 24 mortality studies provided at least suggestive evidence that styrene was associated with NMRD-related morbidity or mortality. Six (66%) of nine mortality studies assessing chronic obstructive pulmonary disease-related mortality indicated excess mortality.
Conclusions
Available evidence suggests styrene exposure is a potential risk factor for NMRD. Additional studies of styrene-exposed workers are warranted.
Keywords: styrene, vinylbenzene, styrol, non-malignant respiratory disease, asthma, occupational asthma, obliterative bronchiolitis, bronchiolitis obliterans, occupational lung disease
Introduction
Asthma and obliterative bronchiolitis (OB) cases have occurred among workers exposed to styrene [Moscato et al., 1987; Cullinan et al., 2013]. OB is a rare and irreversible lung disease often associated with exposure to inhalational toxins, and frequently characterized by a short latency and insidious onset of dyspnea, non-productive cough, and airway obstruction [Epler, 2007; Kreiss, 2013; Barker et al., 2014; Cummings and Kreiss, 2015]. We sought to assess the available evidence for the risk of non-malignant respiratory disease (NMRD) among workers in industries using styrene.
Styrene (C8H8) is a colorless liquid and volatile organic compound that occurs naturally in small quantities in certain plants and foods [Agency for Toxic Substances & Disease Registry, 2012]. Commercially produced since the 1920s, styrene is an important industrial component used in the manufacturing of reinforced plastics and synthetic rubbers [International Agency for Research on Cancer, 2002]. Industries that commonly use styrene include boat and automobile manufacturing, plastics, food packaging, wind energy, and others [Agency for Toxic Substances & Disease Registry, 2010; Styrene Information & Research Center, 2014; McCague et al., 2015]. In 2008, over 12 billion pounds of styrene were produced in the United States [Agency for Toxic Substances & Disease Registry, 2010].
An estimated 90,000 U.S. workers are potentially exposed to styrene [Occupational Safety & Health Administration, 2016]. Work-related exposure most commonly occurs through inhalation and skin contact [Agency for Toxic Substances & Disease Registry, 2010]. The amount of styrene workers are exposed to varies by industry, job, presence of environmental controls, and use of personal protective equipment. The Occupational Safety and Health Administration (OSHA) permissible exposure limit over an 8-hr time-weighted average (TWA) is 100 ppm, the National Institute for Occupational Safety and Health (NIOSH) recommended exposure limit is 50 ppm, and the American Conference of Governmental Industrial Hygienists (ACGIH) [2015] threshold limit value for an 8-hr TWA is 20 ppm [Agency for Toxic Substances & Disease Registry, 2010]. The NIOSH recommended short-term exposure limit over a 15-min TWA is 100 ppm. The highest levels of occupational exposure to styrene have occurred when glass-fiber-reinforced plastics are used in the production of automotive parts, bathtubs, boats, and tanks [National Toxicology Program, 2014]. Occupational exposure to styrene has been associated with deleterious health effects, including mucous membrane irritation, changes in color vision, hearing loss, and neurocognitive impairment [Benignus et al., 2005; Agency for Toxic Substances & Disease Registry, 2010; Morata et al., 2011]. In addition, the International Agency for Research on Cancer [2002] classifies styrene as possibly carcinogenic to humans, and the National Toxicology Program [2014] classifies styrene as reasonably anticipated to be a human carcinogen.
Styrene toxicology studies support the biological plausibility of styrene-induced NMRD in workers. Styrene is a fat-soluble chemical easily absorbed by multiple routes of exposure. Consistent with a possible role for styrene exposure and NMRD in workers, the respiratory epithelium lining airways is damaged by styrene inhalation at high concentrations and in susceptible animal models [Ohashi et al., 1986; Coccini et al., 1997; Cruzan et al., 1997, 2013]. Detailed information on styrene toxicology is included in recent reviews [National Research Council, 2014; National Toxicology Program, 2014].
Materials and Methods
This review was completed using the steps recommended when conducting systematic reviews for occupational safety and health questions [Hempel et al., 2016]. Case reports, cross-sectional studies, and mortality studies on the respiratory health effects of exposure to styrene were identified through searching the published medical literature, reviewing relevant bibliographies, identifying manuscripts in the authors' collections, and obtaining unpublished data. A PubMed search of the scientific literature published from 1949 through October 8, 2015 was conducted.1
An initial collection of 328 citations was retrieved (Fig. 1). Seven duplicates were identified and excluded. The collection was then reduced by one author (RJN) to 41 articles by scanning titles and abstracts and excluding those not deemed relevant. Additional articles were sought from the selected manuscripts' bibliographies (n = 16) and from the authors' collections (n = 3), resulting in a total of 60 articles of interest. Five full-text articles were reviewed and excluded. Two unpublished case reports made available by two authors (KK, YTH) were also included in the analysis, for a total of 57 records of interest. Five relevant articles identified by the PubMed search but not in the English language were translated.
Figure 1.
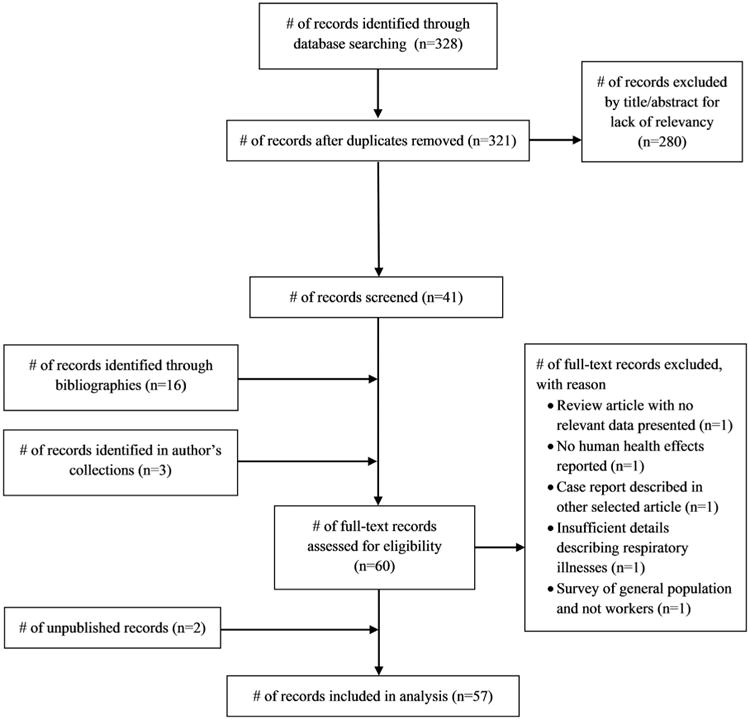
Flow diagram showing process for inclusion of studies exploring the association between occupational styrene exposure and non-malignant respiratory disease.
Study findings were summarized with respect to styrene exposures, spirometry measurements, clinical symptoms or signs, respiratory diagnoses as defined by the original study, or mortality from NMRD. Each cross-sectional and mortality study was evaluated by two of the authors (RJN, JCG) for evidence of a potential association between styrene exposure and development of respiratory symptoms, airflow limitation, NMRD, or NMRD-related mortality. The evidence for positive association between styrene exposure and respiratory morbidity or mortality was characterized as strong, intermediate, or suggestive using a grading rubric developed by three of the authors (RJN, JCG, KK) (Table I). Studies with no evidence were characterized as having no association.
Table I. Criteria Used for Evaluating Strength of Evidence for a Positive Association Between Styrene Exposure and NMRD-Related Morbidity or Mortality.
| Strong (+++) | Intermediate (++) | Suggestive (+) | |
|---|---|---|---|
| Cross-sectional studies | (1) Inclusion of styrene-exposed and comparison groups,a AND | (1) Inclusion of styrene-exposed and comparison groups,a AND | (1) Inclusion of styrene-exposed and comparison groupsa and non-statistically significantb higher prevalence for ≥1 respiratory symptom or ≥1 NMRD, or airflow limitation on spirometry, OR |
| (2) exposure group had statistically significantb higher prevalence for ≥1 respiratory symptom or NMRD, AND | (2) exposure group had statistically significantb higher prevalence for ≥1 respiratory symptom or ≥1 NMRD, or airflow limitation on spirometry | (2) no comparison groupa and the presence of exposed workers with respiratory symptoms or ≥1 NMRD, or airflow limitation on spirometry | |
| (3) exposure group had statistically significant higher prevalenceb for airflow limitation on spirometry | |||
| Mortality studies | (1) Analysis of workers by level of styrene exposure, AND | All workers or a subset of workers had statistically significantb higher SMR for ≥1 NMRD | All workers or a subset of workers had non-statistically significantb higher SMR for ≥1 NMRD |
| (2) workers with high exposure had statistically significantb higher SMR for ≥1 NMRD |
NMRD, non-malignant respiratory disease; SMR, standardized mortality ratio.
Comparison groups determined by environmental exposure data at factories and include groups with either no or comparatively low styrene exposure.
P < 0.05.
Results
Case Reports
In Table II, we summarize 13 articles describing 23 respiratory illness cases and two unpublished respiratory illness cases associated with styrene exposure [Moscato et al., 1987, 1988; Hayes et al., 1991; Shields et al., 1995; Janigan et al., 1997; Occupational Safety and Health Research Institute, 2003; Fernandez-Nieto et al., 2006; Volkman et al., 2006; Ye et al., 2007; Chen et al., 2013; Cullinan et al., 2013; Lee et al., 2013; Arochena et al., 2014]. We reviewed an additional case series by Convery et al. [2001] that was not included in Table II or in the below summary analysis. In this case series, five coal miners and one automotive repairman who were diagnosed with occupational asthma and had exposure to styrene resins had negative inhalation challenges to styrene and were not classified as styrene-related cases, suggesting that styrene is not a non-specific trigger of hyperreactive airways.
Table II. Cases of Respiratory Illness Associated With Styrene Exposure.
| Reference | Age (years)/sex | Industry | Time from first styrene exposure to symptom onset | Findings | Outcome | ||
|---|---|---|---|---|---|---|---|
| Physician-diagnosed obliterative bronchiolitis | |||||||
|
| |||||||
| Janigan et al. [1997] | 37 M | Not applicable | 4 hr | Burned polystyrene and particle board using indoor wood burning stove; presented 11 days later with cough, dyspnea, fever; open lung biopsy, OB | Gradually recovered | ||
| Cullinan et al. [2013] | 25 M | Boat manufacturing | 5 months | FEV1, 0.70 L; FVC, 2.85 L; FEV1/FVC, 0.25; RV, 152% of predicted; kCO, 78% of predicted; lung biopsy, OB | Heart/lung transplant 2 years after presentation; died from complications 17 years later | ||
| 31 M | Boat manufacturing | 7 months | FEV1, 0.88 L; FVC, 2.65 L; FEV1/FVC, 0.33; RV, 333% of predicted; kCO, 117% of predicted; CT chest, OB; lung biopsy, OB | Lung transplant 1 year after presentation | |||
| 42 M | Boat manufacturing | 12 months | FEV1, 1.30 L; FVC, 3.80 L; FEV1/FVC, 0.34; RV, 171% of predicted; kCO, 95% of predicted; took over job of 31 M described above after his lung transplant | Alive 2 years after presentation | |||
| 26 M | Boat manufacturing | 12 months | FEV1, 1.25 L; FVC, 4.44 L; FEV1/FVC, 0.28; RV, 249% of predicted; kCO, 111% of predicted; CT chest, OB; lung biopsy, OB | Alive 4 years after presentation | |||
| 51 M | Boat manufacturing | 4 years | FEV1, 1.81 L; FVC, 4.66 L; FEV1/FVC, 0.39; RV, 109% of predicted; kCO, 96% of predicted; CT chest, bronchial wall thickening | Improved away from work; 6 years after presentation: FEV1, 2.32 L; FVC, 4.58 L | |||
| 26 M | Cooling tower manufacturing | 6 months | FEV1, 0.80 L; FVC, 2.21 L; FEV1/FVC, 0.36; RV, 196% of predicted; kCO, 50% of predicted; CT chest, air trapping around region of right upper lobe and right hilum; central bronchial dilatation; lung biopsy, OB | Died from respiratory failure 2 years after presentation | |||
| Chen et al. [2013] | 35 M | Boat manufacturing | 12 months | Persistent dyspnea; FEV1, 1.28 L; FVC, 2.72 L; FEV1/FVC, 0.47 | Not reported | ||
| 28 M | Water storage tank repair | 2 years | Progressive dyspnea; FEV1, 1.55 L; FVC, 3.56 L; FEV1/FVC, 0.44; irreversible severe obstruction; CT chest, air trapping | Quit job because of dyspnea | |||
| Huang (unpublished) | 32 M | Fiberglass | 1.5 months | Dyspnea on exertion; wheezing; FEV1, 27% of predicted; FVC, 59% of predicted; TLC, 115% of predicted; RV, 292% of predicted; DLCO, 58% of predicted; CT chest, mosaic attenuation | Chronic dyspnea on exertion | ||
|
| |||||||
| Physician-diagnosed asthma | |||||||
|
| |||||||
| Moscato et al. [1987] | 31 M | Plastics manufacturing | 1 month | Acute attacks of dyspnea, chest tightness, and dry cough after starting in polystyrene department; symptoms improved away from work; inhalation challenges using methacholine and styrene caused 15% and 18% decreases in FEV1, respectively; negative inhalation challenge to ethylbenzene | Changed job; no further exposure to styrene; symptoms resolved | ||
| 45 F | Plastic button manufacturing | Not reported | 5-year history of dry cough and chest tightness at workplace; asthma attacks during previous year at work and occasionally at night; symptoms improved during weekends and holidays; inhalation challenge using styrene caused 22% decrease in FEV1; negative inhalation challenges to ethylbenzene and polyester resins | Changed job; no further exposure to styrene; symptoms resolved | |||
| Moscato et al. [1988] | 48 M | Fabric manufacturing | 20 years | 5-month history of dry cough, chest tightness, and dyspnea in afternoons and evenings; chest X-ray normal; baseline spirometry normal; inhalation challenge using styrene caused 37% decrease in FEV1; negative inhalation challenges to lacquer thinner and polystyrene, lacquer thinner and polyester, phthalic anhydride, and epoxy resin | Changed job; no further exposure to styrene; symptoms resolved | ||
| Hayes et al. [1991] | 30 M | Military aviation | Not reported | 20-month history of chest tightness, wheeze, dyspnea, decreased exercise tolerance when exposed to styrene; inhalation challenge using styrene caused >25% decrease in FEV1 | Changed job; felt well 6 months later | ||
| Occupational Safety and Health Research Institute [2003] | 30–39 age category M | Tire manufacturing | 4 years | Job included curing tires; maximum air styrene concentration, 0.19 ppm detected; average PEF decreased from 417.1 L/min on rest days to 361.7 L/min on working days; PEF decreased 15% during work hours compared with rest hours on same day Lee et al. [2013] | Not reported | ||
| Fernandez-Nieto et al. [2006] | 31 M | Automotive repair | 3 years | Dyspnea, dry cough, wheezing while working; symptoms worse at end of shift and resolved away from work; inhalation challenge using styrene caused 22% decrease in FEV1; negative inhalation challenge to hexamethylene diisocyanate | Not reported | ||
| Ye et al. [2007] | 50 M | Automotive repair | 12 years | Cough and dyspnea while working with styrene-containing putty; inhalation challenges using styrene and toluene diisocyanate caused 18% and 48% decrease in FEV1, respectively | Well-controlled asthma with avoidance of styrene and toluene diisocyanate | ||
| Lee et al. [2013] | 47 M | Automotive manufacturing | 4 years | Cough, dyspnea; during hospitalization for asthma exacerbation: FEV1, 46% of predicted and FVC, 57% of predicted; died from asthma exacerbation 40 min after leaving work | Died | ||
|
| |||||||
| Other | |||||||
|
| |||||||
| CDC (unpublished) | 52 M | Yacht manufacturing | 6 months | Worked as a fiberglass painter for 4.5 years; average exposures in molding and production areas were 11.2–120.4 ppm and 2.3–3.6 ppm, respectively; chest tightness, wheezing at least weekly, ∼10 episodes of attacks of shortness of breath and wheezing over 3 years; 23 pack-year history; severe mixed pattern on spirometry (FEV1, 1.69 L; FVC, 2.86 L; FEV1/FVC, 0.59); no clinical diagnosis available | Not reported | ||
| Shields et al. [1995] | 23 M | Not reported | 1 day | Case 1 of 4; exposed to high concentrations of styrene in confined space for 3 months; cough, sore throat; symptoms worsened after leaving job; hospitalized for pneumonia and acute respiratory distress syndrome 2 weeks after leaving job and 3.5 months after first exposure | Ongoing respiratory symptoms 6 years after presentation, FVC 61% of predicted | ||
| 54–66 age category M | Not reported | Not reported | Case 2 of 4; exposed to high concentrations of styrene in confined space for several months; 15 pack-year history; CXR showed hyperinflation; chronic bronchitis (chest tightness, cough, dyspnea) | Ongoing respiratory symptoms several years after exposure cessation | |||
| 54–66 age category M | Not reported | Not reported | Case 3 of 4; exposed to high concentrations of styrene in confined space for several months; 15 pack-year history; chronic bronchitis (chest tightness, cough, dyspnea) | Ongoing respiratory symptoms several years after exposure cessation | |||
| 54–66 age category M | Not reported | Not reported | Case 4 of 4; exposed to high concentrations of styrene in confined space for several months; 15 pack-year history; chronic bronchitis (chest tightness, cough, dyspnea) | Ongoing respiratory symptoms several years after exposure cessation | |||
| Volkman et al. [2006] | 46 F | Yacht manufacturing | 5 years | 2-month history of progressive dyspnea, chest tightness, dry cough; FEV1, 41% of predicted; FVC, 43% of predicted; CXR, mild interstitial prominence; symptoms and spirometry improved following 4 week rest from work and corticosteroid therapy; symptoms returned and spirometry decline occurred 3 weeks after return to work; CT chest, nodular densities; no biopsy performed; diagnosed with hypersensitivity pneumonitis | Removed from work: clinical improvement, normal spirometry and exercise challenge | ||
| Arochena et al. [2014] | 55 M | Automotive repair | 12 years | 10-year history of cough and dyspnea more intense at end of work shift; no symptoms during holidays; after 4 months away from work: (i) spirometry normal, (ii) inhalation challenge using styrene caused no decrease in FEV1; after 10-day trial at work: (a) sputum eosinophil percentage, 15% (twice baseline percentage); diagnosed with eosinophilic bronchitis | Not reported | ||
CDC, Centers for Disease Control and Prevention; CT, computed tomography; CXR, chest X-ray; DLCO, diffusing capacity of the lungs for carbon monoxide; F, female; FEV1, forced expiratory volume in 1s; FVC, forced vital capacity; kCO, diffusing capacity/alveolar volume; M, male; OB, obliterative bronchiolitis; OSHA, Occupational Safety.
In total, we identified nine OB cases, eight asthma cases, one hypersensitivity pneumonitis case, and one eosinophilic bronchitis case among workers exposed to styrene. We also included one case of non-occupational OB occurring in a man who burned polystyrene insulation and particle board in his home's wood burning stove [Janigan et al., 1997]. In addition, Shields et al. [1995] reported four cases of chronic dyspnea following a short-term exposure to styrene in a shared confined space. Another respiratory illness case occurred in a man who began having attacks of shortness of breath and wheezing 6 months after beginning work as a fiberglass painter in a yacht manufacturing plant; he had a severe mixed obstructive and restrictive pattern on spirometry (unpublished).
Of the 10 OB cases, the median age was 31.5 years (range: 25–51 years) at clinical presentation. The median time from first styrene exposure to respiratory symptom onset was 9.5 months (range: 4 hr–4 years), consistent with a short-latency disease. Only three cases were current smokers. Six cases occurred among workers in the boat manufacturing industry. One case occurred in a man after he assumed the job of another worker who had been diagnosed with OB and left his job following a lung transplant [Cullinan et al., 2013]. Five cases were known to have been diagnosed following pathologic analyses of open biopsy (n = 4) and explanted tissue (n = 1) specimens, and five cases were diagnosed based upon clinical findings. Two cases received lung transplants and two cases died (one from complications of a heart and lung transplant, and one from respiratory failure).
Of the eight asthma cases, the median age was 40 years (range: 30–50 years) at clinical presentation. Of the six cases with known time from first styrene exposure to respiratory symptom onset, the median time was 4 years (range: 1 month–20 years). Two cases occurred among workers in the automotive repair industry. Six cases had abnormal inhalational challenges to styrene. Of the six cases with known outcomes, five had improved or resolved symptoms after changing jobs and one died of respiratory failure after developing an acute asthma exacerbation within 2 hr of leaving work.
The four respiratory illness cases described by Shields et al. [1995] occurred among workers not previously exposed to styrene, following 3 months of working in a confined space with exposures to high styrene concentrations that led to neurotoxic effects, and without adequate respiratory protection. One of these cases occurred in a 23-year-old male who began having respiratory symptoms within 1 day of exposure. Worsening cough and respiratory symptoms led to his dismissal within 3 months of beginning his job. Two weeks after leaving his job he was hospitalized for pneumonia and developed acute respiratory distress syndrome. Six years after exposure, he had a forced vital capacity (FVC) of 61% of predicted, indicating chronic airways disease. He and the other three exposed workers suffered chronic dyspnea several years after the initial exposure, consistent with OB or other short-latency and irreversible NMRD.
Cross-Sectional Studies
In Table III, we summarize 16 articles describing 15 cross-sectional studies evaluating the presence of respiratory symptoms, respiratory diagnoses, or airflow limitation among workers exposed to styrene [Chmielewski and Renke, 1975; Lorimer et al., 1976, 1978; Harkonen, 1977; Axelson and Gustavson, 1978; Thiess and Friedheim, 1978; Jedrychowski and Fonte, 1984; Robins et al., 1990; Centers for Disease Control and Prevention (CDC), 1992; Lewin-Kowalik et al., 1994; Tucek et al., 2002; Oner et al., 2004; Sati et al., 2011; Helal and Elshafy, 2013; McCague et al., 2015]. Studies of occupational cohorts varied considerably in size (range: 17–4,717 workers). Ten studies evaluated both respiratory symptoms/diagnoses and spirometry measurements, four spirometry measurements only, and one respiratory symptoms/diagnoses only. Twelve studies included a comparison group of the general population, unexposed workers, or workers exposed to lower concentrations of styrene. Thirteen of 15 studies had at least suggestive evidence of an association between styrene exposure and NMRD-related morbidity. One study had strong evidence.
Table III. Cross-Sectional Prevalence of Respiratory Morbidity Among Cohorts Exposed to Styrene.
| Reference | Industry | No. workers | Symptoms or diagnoses | Findings | Strength of evidencea |
|---|---|---|---|---|---|
| Strong, intermediate, or suggestive evidence | |||||
|
| |||||
| Chmielewski and Renke [1975] | Not reported | 122 | Cough | (i) Chronic cough: 4 (4%) of 101 with short tenure (mean 1 year) and 3 (15%) of 21 with long tenure (mean 10 years); (ii) long-tenured workers: 1 (5%) had chronic bronchitis, 2 (10%) had CXRs that showed “intensified lung structure and fine macular mottling,” and 4 (19%) had FEV1/FVC of 57.1–68.1% | + |
| Lorimer et al. [1976, 1978] | Styrene manufacturing | 488 | Wheezing, chest tightness | (i) Wheezing or chest tightness from styrene vapors: 7% (low-exposure), 19% (high-exposure), P < 0.001; (ii) recurrent wheeze or chest tightness: 5% (low-exposure), 12% (high-exposure), P < 0.01; (iii) acute lower respiratory symptoms for workers with low versus high exposure: 6%, 12%, NS (0.1–7.0 years of exposure); 8%, 25%, P < 0.02 (7.1–20.0); 8%, 18%, P < 0.05 (>20.0); (iv) percentage non-smokers with FEV1/FVC <0.75: 41.4% (with detectable urinary mandelic acidb), 21.0% (with non-detectable urinary mandelic acid), P < 0.05 | ++ |
| Harkonen [1977] | Polyester plastic manufacturing | 98 | Shortness of breath, chronic bronchitis | (i) Frequency of shortness of breath during workday (exposed/unexposed): never (67%/84%); sometimes (30%/13%); often (3%/3%), P < 0.05; (ii) frequency of chronic bronchitis (exposed/unexposed): 28%/12%, P < 0.05, smoking habits did not differ between exposed and unexposed; (iii) 43 subjects had normal FEV1 and FVC measurements (values not provided) | ++ |
| Jedrychowski [1982] | Styrene, methyl methacrylate manufacturing | 1,137 | Asthmatic symptoms, chronic bronchitis | (i) Chronic bronchitis and/or asthma symptoms: 17.8% (exposed) and 19.5% (controls); (ii) FEV1 <80% of predicted: 45.4% (exposed) and 18.0% (controls), P < 0.05; (iii) RR for FEV1 <80% of predicted, 4.7 (95% CI, 2.4–7.0) for exposed non-smokers/ex-smokers compared with unexposed non-smokers/ex-smokers | ++ |
| Jedrychowski and Fonte [1984] | Chemical manufacturing | 4,717 | Bronchial asthma, chronic bronchitis | (i) Workers in one styrene department (observed/expected): asthma/no chronic bronchitis (26/17.7, P < 0.05); asthma/chronic bronchitis (16/9.0, P < 0.05); (ii) obstructive syndrome (observed/expected): department V, 38.0%/52.4%, NS; department VI, 68.0%/35.7%, P < 0.05 | +++ |
| Robins et al. [1990] | Patterns and models manufacturing | 864 | Chronic bronchitis, dyspnea, wheezing | (i) 199 workers known to work most often with plastic; (ii) 10-year increase in plastic-years associated with OR for wheezing, 1.49 (P = 0.04); chronic bronchitis, 1.65 (P = 0.019); dyspnea, 2.23 (P = 0.0004); (iii) no significant change in FEV1, FVC, FEV1/FVC associated with plastic-years or polyester/styrene-years of exposure | ++ |
| CDC [1992] | Yacht manufacturing | 44 | Cough, dyspnea, chest tightness | (i) Air samples 1.0–120.4 ppm; (ii) symptoms: cough, 13 (35%) of 37; dyspnea, 5 (14%) of 36; chest tightness and difficulty breathing, 22 (59%) of 37; (iii) spirometry: obstructive pattern, 4 (10%) of 39; restrictive pattern, 2 (5%); (iv) no relationship detected between exposure to air styrene concentrations >25 ppm and pulmonary function measurements | + |
| Lewin-Kowalik et al. [1994] | Chemical manufacturing | 647 | Not reported | (i) Mean FEV1 among non-smoking males compared with normal values: 2.85 L/3.54 L, P = 0.003 (styrene department) and 2.82 L/3.52 L, P < 0.003 (polystyrene department); (ii) mean FVC among nonsmoking males compared with normal values: 3.70 L/4.46 L, P < 0.02 (styrene department) and 3.89 L/4.26 L, P < 0.05 (polystyrene department) | ++ |
| Tucek et al.[2002] | Acrylic acid esters manufacturing | 1,005 | Upper respiratory symptoms, cough | (i) 280 workers exposed to styrene; (ii) work-related respiratory symptoms (e.g., mucous membrane irritation, cough): exposed, 40%; controls, 20%; (iii) for both smokers and non-smokers, no significant differences in spirometric parameters for exposed versus controls | + |
| Oner et al. [2004] | Furniture manufacturing | 47 | Chest tightness, cough, dyspnea, wheezing | (i) 5 (11%) workers with dyspnea, wheezing, chest tightness, or dry cough associated with styrene exposure; (ii) 3 of these 5 workers with occupational respiratory symptoms had positive methacholine challenges; of these 3 workers, 1 had improvements in PEF when away from work and 0 had positive inhalation challenge to styrene | + |
| Sati et al. [2011] | Plastics manufacturing | 64 | Not reported | (i) Mean FEV1: 2.60 L (exposed) and 3.11 L (controls), P < 0.001; (ii) mean FVC: 2.90 L (exposed) and 3.67 L (controls), P < 0.001; (iii) mean FEV1/FVC percentage: 89.3% (exposed), 85.5% (controls), P = 0.082; (iv) mean FEF25–75%: 3.02 L/s (exposed) and 3.28 L/s (controls), P = 0.31 | ++ |
| Helal and Elshafy [2013] | Plastics manufacturing | 90 | Not reported | (i) Mean percent FEV1 predicted: 76.9% (exposed) and 87.4% (controls), P < 0.001; (ii) mean percent FVC predicted: 77.2% (exposed) and 86.1% (controls), P < 0.001; (iii) mean FEV1/FVC percentage: 74.2% (exposed) and 82.8% (controls), P < 0.001; (iv) negative correlation between blood styrene concentration and FEV1/FVC, r = −0.49, P < 0.05 and MEF25–75%, r = −0.76, P < 0.001 | ++ |
| McCague et al. [2015] | Wind energy | 355 | Chest tightness, cough, shortness of breath, wheezing | (i) Shortness of breath and usual cough less common, and wheezing more common than expected from adjusted comparisons with U.S. adult population; (ii) chest tightness by median current styrene exposure (mg/g creatinine): 5.0% with <53.6, 13.0% with ≥53.6, P ≤ 0.05; (iii) increased cumulative styrene exposure associated with decreased percent predicted MMEF, effect estimate = −0.026, P = 0.011; (iv) 3.5% decrease in FEV1/FVC (P < 0.05) and 5.5% decrease in FeNO (P < 0.05) with cumulative styrene exposure change from 2.5th to 97.5th percentile | ++ |
|
| |||||
| No Association | |||||
|
| |||||
| Axelson and Gustavson [1978] | Glass fiber reinforced products manufacturing | 17 | Not reported | (i) 11 workers with exposure to 8 hrTWA <150 ppm (before work/after work): mean FVC, 103%/101 % of predicted; mean FEV1/FVC, 107%/106% of predicted; (ii) 6 workers with exposure to 8 hTWA >150 ppm (before work/after work): mean FVC, 101 %/101% of predicted; mean FEV1/FVC, 103%/102% of predicted | NA |
| Thiess and Friedheim [1978] | Styrene manufacturing | 177 | Bronchial asthma, chronic bronchitis | (i) Air concentrations generally <1 ppm, occasionally up to 8 ppm, highest excursion was 47 ppm; (ii) urine mandelic acid <50 mg/L in 61 (91%) of 67 styrene or polystyrene workers; (iii) 6 (7%) of 84 styrene workers had chronic bronchitis; 8 (9%) of 93 polystyrene workers had bronchial asthma | NA |
CDC, Centers for Disease Control and Prevention; CXR, chest X-ray; FeNO, fraction of exhaled nitric oxide; FEV1, forced expiratory volume in 1s; FVC, forced vital capacity; h, hour; LOD, limit of detection; MEF, mid-expiratory flow; MMEF, maximal mid-expiratory flow; NA, no association; NS, non-significant (P ≥ 0.05); OB, obliterative bronchiolitis; OR, odds ratio; PEF, peak expiratory flow; ppm, parts per million; RR, relative risk; TWA, time-weighted average
Strength of evidence for positive association: +++, strong; ++, intermediate; +, suggestive; NA, no association; see Table I for definitions.
Presence of urinary mandelic acid indicates metabolism of styrene.
Eleven cross-sectional studies included respiratory symptoms or disease diagnoses. For the eight studies with comparison groups, seven reported a higher prevalence of ≥1 respiratory symptom or disease diagnosis among exposed workers. Symptoms reported at higher prevalence included cough, dyspnea, shortness of breath, wheeze, chest tightness, and recurrent lower respiratory symptoms. Diagnoses reported at higher prevalence included asthma, chronic bronchitis, and asthma or chronic bronchitis.
Fourteen studies reported spirometry measurements; of these, nine demonstrated airflow limitation among workers. Of the 12 studies with a comparison group, eight showed evidence of increased airflow limitation in the exposed groups compared with controls.
Mortality Studies
In Table IV, we summarize 25 articles describing 24 mortality studies of 13 occupational cohorts with 343–35,443 workers [Frentzel-Beyme et al., 1978; Nicholson et al., 1978; Ott et al., 1980; Meinhardt et al., 1982; Bond et al., 1985, 1992; Hodgson and Jones, 1985; Okun et al., 1985; Coggon et al., 1987, 2015; Matanoski and Schwartz, 1987; Matanoski et al., 1990; Wong, 1990; Cowles et al., 1994; Olsen et al., 1994; Wong et al., 1994; Welp et al., 1996; Sathiakumar et al., 1998; Wong and Trent, 1999; Marsh et al., 2001; Burns et al., 2003; Macaluso et al., 2004; Ruder et al., 2004; Sathiakumar and Delzell, 2009; Collins et al., 2013; Ruder et al., 2016]. Required tenure varied by study from ≥1 day to ≥5 years. Four studies required ≥6 months tenure and 13 required ≥1 year. Twelve studies provided at least suggestive evidence of an association between styrene exposure and NMRD-related mortality. Two studies had strong evidence.
Table IV. Mortality From Non-Malignant Respiratory Diseases Within Occupational Cohorts Exposed to styrene.
| Cohort and Reference | Industry | No. workers | Required tenure | Standardized mortality ratio (95%CI) | Findings | Strength of evidencea | |
|---|---|---|---|---|---|---|---|
|
| |||||||
| NMRD | COPD | ||||||
| A—Frentzel-Beyme et al. [1978] | Styrene and polystyrene manufacturing | 1,960 | >1month | 0.46b,c | 0.95d,e (0.05–4.70) | (i) Air sampling performed during 1975: range of styrene concentration in air, <0.01 ppm (limit of detection) to 46.92 ppm Thiess and Friedheim [1978]; (ii) SMR for asthma, 1.49d,e (95%CI, 0.07-735); (iii) SMR for pneumonopathy, 4.13d (95%CI, 0.21– 20.38) | + |
| B—Marsh et al. [2001] | Vitreous fiber manufacturing | 32,110 | ≥1 year | 0.91 (0.62–1.27), 0.69 (0.45–1.01), 0.53 (0.24–0.99)f,g | Not reported | Styrene exposure in 3 of 10 plants included in study; exposure levels not reported | NA |
| C—Ott et al. [1980] | Styrene-based product manufacturing | 2,904 | ≥1 year | 1.59d,h (0.81–2.83) | Not reported | Exposure varied by work role and location; TWAs ranged from 0 to <10 ppm, with excursions reported as high as 88 ppm | + |
| C—Bond et al. [1992] | Styrene-based product manufacturing | 0.55 (0.37–0.79) | 0.85i (0.39–1.61) | RR for NMRD for styrene exposed workers compared with unexposed Michigan manufacturers, 0.75 (95%CI, 0.52–1.08) | NA | ||
| D—Bond et al. [1985] | Chemical manufacturing | 19,608 | ≥1 year | 0.95 (0.82–1.09) | 1.03i (0.78–1.34) | Workers hired 1965–1980 (younger workforce): (i) NMRD, SMR, 1.05 (95%CI, 0.90–1.22); (ii) emphysema, SMR, 1.06 (95%CI, 0.79–1.39); longer duration of employment associated with decreased rate of death from NMRD, P < 0.001 | + |
| D—Olsen et al. [1994] | Chemical manufacturing | 27,040 | 0.97j (0.88–1.08) | 1.19i,j (0.95–1.46) | SMRs among male workers ≥15 years since hire: (i) NMRD, 1.04 (95%CI, 0.94–1.15); (ii) emphysema, 1.26 (95%CI, 1.01–1.55) | ++ | |
| D—Burns and Carson [2003] | Chemical manufacturing | 27,795 | Males, 0.95 (0.87–1.03); females, 0.55 (0.35–0.82) | Not reported | SMR (95%CI) for NMRD by duration of employment: (i) 1–4 years, 1.15 (1.02–1.29); (ii) ≥15 years, SMR, 0.65 (0.56–0.76) | ++ | |
| E—Nicholson et al. [1978] | Styrene and polystyrene manufacturing | 560 | ≥ 5 years | 0.15d (0.0075–0.74) | Not reported | SMRs (95%CI) for NMRD by exposure: (i) high-exposure, 0 deaths; (ii) possibly high-exposure, 0 deaths; low-exposure, 0.67 (0.034–3.31)d | NA |
| F—Meinhardt et al. [1982] | Synthetic rubber manufacturing | 2,756 | ≥6 months | 0.49 (0.23–0.93) | Not reported | (i) Mean estimated TWA: (a) plant A, 0.94 ppm (range: 0.03–6.46 ppm); (b) plant B, 1.99 ppm (range: 0.05–12.3 ppm); (ii) SMR for NMRD: (a) plant A, 0.49 (95%CI, 0.28–1.13); (b) plant B, 0.97, (95%CI, 0.36–2.16) | NA |
| G—Matanoski and Schwartz [1987] | Synthetic rubber manufacturing | 13,920 | ≥1 year | 0.64c | Not reported | Mean estimated 8-hr TWA, 1.3 ppm (all workers) and 0.9–9.4 ppm (different job groups) Macaluso et al. [2004] | NA |
| G—Matanoski, et al. [1990] | Synthetic rubber manufacturing | 12,110 | 0.69 (0.58–0.83) | Not reported | SMRs (95%CI) by worker race: (i) white, 0.68 (0.56–0.82); (ii) black, 0.79 (0.47–1.24) | NA | |
| G—Sathiakumar et al. [1998] | Synthetic rubber manufacturing | 15,649 | 0.71 (0.62–0.81) | Not reported | (i) Ever hourly: SMR, 0.72 (P < 0.05); (ii) never hourly, SMR, 0.61c (P < 0.05); (iii) ≥10 years worked and ≥20 years since hire, SMR, 0.87 (95%CI, 0.71–1.06) | NA | |
| G—Sathiakumar and Delzell [2009] | Synthetic rubber manufacturing | 4,863 | ≥1 day | 0.97 (0.79–1.18) | Not reported | Only females included in study | NA |
| H—Welp et al. [1996] | Reinforced plastics manufacturing | 35,443 | ≥1 day | 0.81 (0.67–0.96) | 0.86h (0.66–1.10) | (i) Mean exposures, ∼200 ppm (early 1960s), 20–40 ppm (late 1980s); (ii) relative risk (RR) (95%CI) for NMRD by average exposure (ppm) using internal comparisons: <20, 1.00 (ref); 20–59, 0.37 (0.16–0.83); 60–119, 0.55 (0.26–1.17); 120–199, 0.67 (0.31–1.47); >200, 0.86 (0.38–1.93), P for trend = 0.08 | NA |
| I—Hodgson and Jones [1985] | Styrene manufacturing | 622 | ≥1 year | 0.49d (0.082–1.61) | Not reported | Exposure levels not reported but believed exposures would have been <100 ppm with isolated excursions to higher levels during certain activities | NA |
| J—Coggon et al. [1987] | Glass-reinforced plastics manufacturing | 7,949 | ≥1 day | 0.70 (0.53–0.90) | Not reported | High-exposure category; mean 8-hr TWA at 5 of the 8 factories after 1975, 40–100 ppm | NA |
| J—Coggon et al. [2015] | Glass-reinforced plastics manufacturing | 7,970 | 0.93 (0.83–1.03) | Not reported | SMRs (95%CI) for respiratory diseases for all workers and workers with more than background exposure to styrene, by time period: (i) 1946–2012, 0.93 (0.83–1.03) and 0.97 (0.85–1.11); (ii) 1991–2012, 1.20 (1.06–1.35) and 1.26 (1.08–1.45) | ++ | |
| K—Wong [1990] | Reinforced plastics and composites manufacturing | 15,908 | ≥6 months | 0.52° (P < 0.05) | 1.18c,i (NS) | (i) SMR for emphysema by duration of employment: <1 year: 1.28, NSc; 1–2 years: SMR, 3.75, NSc; 2–5 years: 0.83, NSc; >5 years: SMR, 0.43, NSc; (ii) SMR for emphysema by level of exposure potential: low-exposure: 1.22, NSc; high-exposure, 1.50, NSc | + |
| K—Wong et al. [1994]; Wong and Trent [1999] | Reinforced plastics and composites manufacturing | 15,826 | 1.21 (0.98–1.48) | 1.27h (0.81–1.91) | (i) SMR for other NMRD, 1.41, (95%CI, 1.05–1.85); (ii) SMR for bronchitis, emphysema, asthma by job category (minimum >2 years): open mold processing, 2.38, NSc; mixing and closed mold processing, 2.62, NSc; finish and assembly, 1.14, NSc; plant office and support, 0.42, NSc; maintenance and preparation, 1.11, NSc; supervisory and professional, 0.90, NSc | ++ | |
| K—Collins et al. [2013] | Reinforced plastics and composites manufacturing | 1.15 (1.05–1.27) | 1.35h (117–1.56) | (i) SMR for emphysema, 1.30 (95%CI, 0.96–1.71); (ii) mortality from bronchitis, emphysema, and asthma not associated with increased days of peak styrene exposure (≥15 min above 100 ppm) | ++ | ||
| L—Okun et al. [1985] | Boat manufacturing | 5,201 | ≥1 day | 0.82d (0.36–1.63) | Not reported | (i) High-exposure (mean exposures, 42.5 ppm [company A], 71.7 ppm [company B]; (ii) low-exposure included workers who never worked in high exposure departments and considered to have minimal exposure; (iii) SMR (95%CI) for NMRD by exposure category: high-exposure, 1.54d (0.26–5.08); low-exposure, 0.69d (0.25–1.54) | + |
| L—Ruder et al. [2004] | Boat manufacturing | 1.14 (0.88–1.46) | Not reported | SMRs (95%CI) for selected diseases among high-exposure cohort: (i) NMRD, 2.07 (1.24–3.23); (ii) pneumoconiosis and other respiratory diseases, 2.54 (1.31–4.44) | +++ | ||
| L—Ruder et al. [2016] | Boat manufacturing | 1,678 | ≥1 year | 0.99 (0.75–1.28) | 1.15 (0.81–1.58) | Using entire 5,201 worker cohort, SMRs (95%CI) for selected diseases among potential high-exposure subcohorts with tenure <1 year and ≥1 year, respectively: (i) NMRD, 1.99 (1.38–2.79) and 1.64 (0.96–2.63); (ii) COPD, 2.60 (1.70–3.81) and 2.02 (1.08–3.46) | +++ |
| M—Cowles et al. [1994] | Plastics and resins manufacturing | 343 | ≥1 year | 0 deaths | Not reported | (i) Research and development facility operational 1962–1975; (ii) no exposure levels reported | NA |
CI, confidence interval; COPD. Chronic obstructive pulmonary disease; NA, no association; NMRD, non-malignant respiratory diseases; NS, non-significant (P ≥ 0.05); ppm, parts per million; RR, relative risk; SMR, standardized mortality ratio; TWA, time-weighted average.
Strength of evidence for positive association: +++, strong; ++, intermediate; +, suggestive; NA, no association; see Table I for definitions.
Proportional mortality ratio calculated using Federal Republic of Germany's general population.
Confidence interval not reported.
Standardized mortality ratio and 95% confidence interval calculated from reported data using http://openepi.com
Standardized mortality ratio calculated for bronchitis.
Standardized mortality ratios presented for 3 of 10 plants included in study where styrene exposure occurred.
Standardized mortality ratio calculated for non-malignant respiratory disease excluding pneumonia and influenza.
Standardized mortality ratio calculated for bronchitis, emphysema, and asthma.
Standardized mortality ratio calculated for emphysema.
Males only when both males and females included in study.
Mortality rates from NMRD for entire cohorts varied considerably. Four studies analyzing their entire cohorts indicated excess mortality from NMRD compared with the general population (see Supplementary Table SI for a listing of diagnostic codes used). Although OB can be misdiagnosed or classified as COPD on death certificates, only nine studies assessed COPD mortality (SMR [standardized mortality ratio] range: 0.85–1.35); of these, six studies assessing three cohorts reported excess mortality. The highest SMR for COPD was described by Ruder et al. [2016] and occurred among a cohort of boat builders in Washington State]. In this cohort, the SMR for COPD among workers characterized as having potentially high-exposure to styrene with tenure ≥1 year was 2.02 (95%CI, 1.08–3.46).
Because OB and asthma are short-latency diseases, they can occur in short-tenured workers. Thus, peak and perhaps average styrene exposures might be more important in the disease process than cumulative exposures. Only four studies analyzing two separate cohorts assessed NMRD-mortality among workers with tenure < 1 year, and each indicated excess mortality. Wong [1990] investigated mortality for 15,908 reinforced plastics workers with tenure ≥6 months and reported the SMR from emphysema in workers with tenure 6 months–1 year was 1.28, although the results were not statistically significant. A later analysis of the same cohort indicated excess mortality for bronchitis, emphysema, and asthma (SMR, 1.96) and other NMRD (SMR 1.80) among workers with tenure 6 months–1 year, but again the results were not statistically significant [Wong et al., 1994; Wong and Trent, 1999]. Ruder et al. [2004] investigated mortality for workers with tenure <1 year and demonstrated an excess mortality from pneumoconiosis and other respiratory diseases (SMR, 2.78 [95%CI, 1.20–5.667]). A later analysis of the same cohort determined the SMRs for respiratory system diseases among workers with tenure <1 year with high and low potential styrene exposures, respectively, were 1.99 (95%CI, 1.38–2.79) and 1.64 (95%CI, 0.96–2.63) [Ruder et al., 2016].
Twelve studies found no positive association between styrene exposure and NMRD-related mortality. Of these, 10 required worker tenure ≥6 months, 10 did not specifically report COPD-related mortality, and nine did not separately assess workers with high-exposure.
Only two mortality studies required worker tenure ≥1 day, assessed workers by level of styrene exposure, and reported COPD-related mortality [Welp et al., 1996; Ruder et al., 2016]. Welp et al. [1996] studied a cohort of 35,443 reinforced plastics workers from 660 European factories. Workers with increasing time since first styrene exposure were more likely to have died from NMRD. Compared with the referents who worked <10 years, the relative risk (RR) (95%CI) for mortality from all respiratory diseases for working 10–19 years was 2.06 (1.20–3.54) and >20 years was 2.50 (1.28–4.89). Workers were also more likely to die from pneumonia with increasing average exposure. Compared with referents exposed to <60 ppm, the RR (95%CI) for pneumonia of those exposed to 60–119 ppm was 2.07 (0.53–8.04), 120–199 ppm was 3.20 (0.79–13.0), and >200 ppm was 6.10 (1.44–25.8). No association was found between mortality from bronchitis, emphysema, or asthma and time since first exposure, duration of exposure, average exposure, or cumulative exposure. In contrast, Ruder et al. [2016] described excess mortality for COPD among boat builders with high styrene exposures and tenure <1 year (SMR, 2.60 [95%CI, 1.70–3.81]) and ≥1 year 2.02 (95%CI, 1.08–3.46).
Discussion
This review found evidence supporting that working in industries using styrene is a potential risk factor for NMRD, including: (i) 10 case reports of OB among persons exposed to styrene, including one case that occurred in a worker who replaced another worker diagnosed with OB, a highly unusual occurrence for a rare pulmonary disease; (ii) eight case reports of occupational asthma among workers exposed to styrene, including six with abnormal inhalation challenges to styrene; (iii) four cases of chronic dyspnea that occurred among workers who had a short-term exposure to high styrene levels in a shared confined space; (iv) 13 of 15 cross-sectional studies of workers provided at least suggestive evidence of an association between styrene exposure and airflow limitation or NMRD; and (v) six of the nine mortality studies analyzing COPD indicated excess COPD-related mortality.
Obliterative Bronchiolitis
Mortality studies focusing on occupational cancer are not optimally designed to assess short-latency lung diseases, such as OB. The reviewed studies were mostly large, the cohorts were often followed for decades, and one-half required tenures ≥1 year. However, workers exposed to styrene might be at-risk for OB that occurs insidiously within weeks to months after beginning employment, but stabilizes once styrene exposure ends [Kreiss, 2013], thus reducing the likelihood of detecting OB-related morbidity using mortality studies of cumulative exposures of long-tenured workers followed for decades for long-latency diseases. Indeed, eight (80%) of the 10 identified OB cases had respiratory symptom onset within ≤12 months of first exposure to styrene. Wong et al. demonstrated a higher SMR from other NMRD for workers with tenure <1 year, and Ruder et al. demonstrated a higher SMR from pneumoconiosis and other respiratory diseases, and COPD for workers with tenures <1 year [Wong, 1990; Wong et al., 1994; Wong and Trent, 1999; Ruder et al., 2004, 2016]. Moreover, Ruder et al. [2016] found a decreased SMR from respiratory system diseases for workers with high exposure when the cohort was limited to those with tenure ≥1 year (SMR, 1.64 [95%CI, 0.96–2.63]) compared with ≥1 day (SMR, 1.99 [95%CI, 1.38–2.79]). Additional studies that include short-term high-exposures and short-tenured workers are required to better describe the risk of respiratory disease mortality among workers with styrene exposure.
An excess of COPD-related mortality was found in six of the nine mortality studies assessing COPD mortality. Although Collins et al. [2013] suggested an observed excess of COPD-related mortality in a cohort of U.S. reinforced plastics workers was likely because of greater tobacco use among those exposed, this hypothesis remains unexamined [Cummings et al., 2014]. The clinical manifestations of OB can be mistaken for those caused by asthma or COPD, which can lead to underreporting [CDC, 2013]. The absence of a medical diagnostic code for OB also increases the probability that deaths caused by OB were classified as COPD. These details raise the likelihood that at least some of the workers with causes of death listed as COPD died instead from OB.
A potential for classification of at least some OB cases as COPD among styrene-exposed workers is highlighted by Ruder et al. [2016] where the authors demonstrated a higher standardized rate ratio (SRR) for COPD between potentially high- and low-exposure styrene subcohorts (SRR, 1.76 [95%CI, 0.80–3.92]) than for lung cancer (SRR, 0.77 [95% CI, 0.42–1.41]), which suggests the additional mortality from COPD in this boatbuilding cohort is not easily attributable to smoking. Further investigation of current workers exposed to styrene who are diagnosed with COPD is warranted to examine the possibility for misdiagnosed OB.
Cross-sectional studies can provide unreliable estimates of the health of a cohort of workers because of the healthy worker effect [Shah, 2009] and likely underestimate the potential respiratory morbidity associated with styrene exposure as ill workers likely leave the workforce earlier. Studies relying upon chest X-rays and spirometry measurements are further limited in their ability to detect workers with OB as neither diagnostic test is a sensitive indicator of disease, and pathologically confirmed cases can have obstructive, restrictive, or mixed spirometry patterns, or even normal spirometry measurements [Markopoulo et al., 2002; Kreiss, 2013; Cummings and Kreiss, 2015]. For example, a study of 38 U.S. soldiers returning from Iraq and Afghanistan who had insidious onset of dyspnea were found to have constrictive bronchiolitis following thoracoscopic lung biopsies; of those, 37 (97%) had normal chest X-rays, 32 (84%) had normal spirometry measurements, and only two (5%) had evidence of obstruction on spirometry [King et al., 2011]. Despite the lack of sensitivity of cross-sectional studies, over 86% of the studies we evaluated provided at least suggestive evidence that styrene was associated with NMRD-related morbidity.
Asthma
Similar to other volatile organic compounds [Nurmatov et al., 2015], available evidence indicates that styrene is an asthmagen. Six published case reports of asthma demonstrated reduced FEV1 following inhalation challenges with styrene among workers who suffered respiratory symptoms when exposed to styrene. Additionally, each of the five living asthma cases with known outcomes had improved or resolved symptoms after changing jobs and eliminating further styrene exposure. Clinical improvement following elimination of styrene exposure also makes it less likely these cases had OB, an irreversible lung disease.
The majority of cross-sectional studies provided evidence suggesting that styrene is a potential cause of occupational asthma. A cohort of U.S. styrene workers with higher exposure levels compared with those who had lower exposures had a higher prevalence of wheezing or chest tightness, and airflow obstruction [Lorimer et al., 1976, 1978]. Similarly, Polish workers exposed to styrene had a higher than expected prevalence of asthma and obstructive syndrome, and exposed non-smokers/ex-smokers were at higher risk of having airway obstruction compared with unexposed non-smokers/ex-smokers [Jedrychowski, 1982; Jedrychowski and Fonte, 1984]. Finally, Egyptian plastics workers compared with controls had reduced percent predicted FEV1 and FVC, reduced mean FEV1/FVC percentage, and a negative correlation between blood styrene concentrations and both FEV1/FVC and maximal mid-expiratory flow rates, an indicator of obstruction of the small airways (<2 mm internal diameter) [Helal and Elshafy, 2013]. Further investigation of styrene as an asthmagen is needed.
Challenges exist in assessing styrene's role in the development of NMRD as workers exposed to styrene are often exposed to multiple chemicals (Supplementary Table SII) [CDC, 2009]. Multiple chemical exposures likely occurred at all workplaces described in this review, but workers at glass reinforced plastics facilities where styrene exposures are highest likely were exposed to fewer chemicals than workers at other facilities [International Agency for Research on Cancer, 2002]. The possibility exists that styrene is a surrogate marker for another chemical exposure that causes an increase in NMRD-related morbidity and mortality among workers exposed to styrene. Interactions are also possible, as demonstrated by a study in mice showing the presence of biologically inert respirable glass fibers enhanced the respiratory toxicity of styrene in causing lower airway damage [Morisset et al., 1979]. The interpretation of published data with respect to exposures to styrene and other chemicals simultaneously was further complicated as exposures for facilities described in the literature reviewed here were often incomplete. Further animal studies would contribute to improved knowledge about the contribution of styrene to respiratory toxicity in the context of concurrent chemical exposures.
This analysis is subject to several limitations. First, considering the widespread global use of styrene across multiple industries, we identified only 25 cases of NMRD associated with exposure. However, the relatively small number of recognized cases might also be related to an underrecognition of both OB as clinical diagnosis and occupational causes of asthma. Second, available cross-sectional studies for review might be biased toward studies reporting a positive association between styrene exposure and NMRD-related morbidity and mortality. Third, workers described in the case reports, cross-sectional studies, and mortality studies were exposed to often unknown or differing concentrations of styrene, had different lengths of exposure, and were exposed to multiple chemicals in the workplace, which potentially confounds the results of primary analyses. Fourth, this review included mortality studies that did not explicitly assess mortality from COPD, which could result in an underestimation of OB-related mortality. When COPD is included with other causes of NMRD, the possible effect of COPD is diluted by other diagnoses not associated with styrene exposure as demonstrated when examining only COPD-related mortality.
In summary, a review of available case reports, cross-sectional studies, and mortality studies suggested occupational exposure to styrene is a potential risk factor for NMRD, and related morbidity and mortality. This review highlighted the need for higher quality data. Additional animal exposure studies using novel humanized rodent models that better mimic human physiology would help address remaining questions regarding the development of lung disease following inhalational exposure to styrene. Additional studies should also include prospective and longitudinal investigations to further describe the risk for respiratory morbidity and mortality among short- and long-tenured workers in industries using styrene, both during and after employment, particularly for those with high styrene exposures. Finally, assessing for styrene and other chemical exposures in future epidemiologic studies could allow for added clarification of the influence styrene has on respiratory toxicity in workers with mixed chemical exposures.
Supplementary Material
Acknowledgments
The authors thank Barbara Landreth, Ju-Hyeong Park, Yeonmi Park, Jacek Mazurek, Cara Halldin, and Kathy Fedan for their invaluable support and contributions, and Patricia Sullivan and Kristin Yeoman for their thoughtful technical reviews.
Funding: This work was supported by intramural funding from the National Institute for Occupational Safety and Health.
Footnotes
Search strategy and keywords: [100-42-5.rn. or “benzene, ethenyl-” or “benzene, vinyl-” or “Bulstren K-525-19” or cinnamene or ethenylbenzene or “ethylene, phenyl-” or phenethylene or phenylethylene or polystyrene* or stirolo or styreen or styren or styrene* or styrol or styrole or styrolene or “styropol SO” or “vinyl benzene” or vinylbenzen or vinylbenzene or vinylbenzol] and [“threshold limit value*” or employee* or facilities or facility or industr* or manufactur* or “maximum allowable concentration*” or occupation* or worker* or workplace*] and [airway* or alveol* or asthma* or bronch* or (bronchiolit* ADJ oblit*) or chest or exp diagnostic techniques, respiratory system/or expiratory or FEV1 or (hypersensit* ADJ pneumon*) or inhal* or laryng* or lung or lungs or pneumo* or pulmon* or respirat* or exp respiratory system/or exp respiratory tract diseases/or spiromet*] and [limited to English language or (abstracts or structured abstracts)].
Authors' Contributions: Jean M. Cox-Ganser and Randall J. Nett participated in study design, scientific literature review, scientific literature grading, manuscript preparation, and manuscript review. Ann F. Hubbs participated in scientific literature review, manuscript preparation, and manuscript review. Avima M. Ruder and Yuh-Chin T. Huang participated in contributing unpublished data, manuscript preparation, and manuscript review. Kristin J. Cummings and Kathleen Kreiss participated in study design, manuscript preparation, and manuscript review.
Disclosure (Authors): The authors declare no conflicts of interest.
Disclosure by Ajim Editor of Record: Rodney Ehrlich declares that he has no competing or conflicts of interest in the review and publication decision regarding this article.
Disclaimer: The findings and conclusions in this report are those of the author(s) and do not necessarily represent the views of the National Institute for Occupational Safety and Health.
Supporting Information: Additional supporting information may be found in the online version of this article at the publisher's website.
References
- Agency for Toxic Substances & Disease Registry. Toxicological profile for styrene. Atlanta, GA: Department of Health and Human Services; 2010. pp. 1–236. [PubMed] [Google Scholar]
- Agency for Toxic Substances & Disease Registry. Public health statement for styrene. Department of Health and Human Services; 2012. [Google Scholar]
- American Conference of Governmental Industrial Hygienists (ACGIH) 2015 TLVs and BEIs. Cincinnati, OH: ACGIH; 2015. [Google Scholar]
- Arochena L, Fernandez-Nieto M, Aguado E, Garcia del Potro M, Sastre J. Eosinophilic bronchitis caused by styrene. J Investig Allergol Clin Immunol. 2014;24:68–69. [PubMed] [Google Scholar]
- Axelson O, Gustavson J. Some hygienic and clinical observations on styrene exposure. Scand J Work Environ Health. 1978;4(Suppl 2):215–219. [PubMed] [Google Scholar]
- Barker AF, Bergeron A, Rom WN, Hertz MI. Obliterative bronchiolitis. N Engl J Med. 2014;370:1820–1828. doi: 10.1056/NEJMra1204664. [DOI] [PubMed] [Google Scholar]
- Benignus VA, Geller AM, Boyes WK, Bushnell PJ. Human neurobehavioral effects of long-term exposure to styrene: A meta-analysis. Environ Health Perspect. 2005;113:532–538. doi: 10.1289/ehp.7518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bond GG, Shellenberger RJ, Fishbeck WA, Cartmill JB, Lasich BJ, Wymer KT, Cook RR. Mortality among a large cohort of chemical manufacturing employees. J Natl Cancer Inst. 1985;75:859–869. doi: 10.1093/jnci/75.5.859. [DOI] [PubMed] [Google Scholar]
- Bond GG, Bodner KM, Olsen GW, Cook RR. Mortality among workers engaged in the development or manufacture of styrene-based products-an update. Scand J Work Environ Health. 1992;18:145–154. doi: 10.5271/sjweh.1594. [DOI] [PubMed] [Google Scholar]
- Burns CJ, Carson ML, Cartmill JB. Cause-specific mortality among employees of a Texas-based chemical manufacturing facility, 1940 through 1996. Tex Med. 2003;99:67–73. [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention (CDC) HETA 88-262-2209. Morgantown, WV: National Institute for Occupational Safety and Health; 1992. [Accessed October 3, 2016]. https://www.cdc.gov/niosh/hhe/reports/pdfs/1988-0262-2209.pdf. [Google Scholar]
- U.S. Department of Health and Human Services, editor. CDC. In-depth survey report: Styrene exposures during fiber reinforced wind blade manufacturing. Cincinnati, OH: 2009. [Google Scholar]
- CDC. Obliterative bronchiolitis in workers in a coffee-processing facility—Texas, 2008–2012. MMWR Morb Mortal Wkly Rep. 2013;62:305–307. [PMC free article] [PubMed] [Google Scholar]
- Chen CH, Tsai PJ, Wang WC, Pan CH, Ho JJ, Guo YL. Obliterative bronchiolitis in workers laying up fiberglass-reinforced plastics with polyester resin and methylethyl ketone peroxide catalyst. Occup Environ Med. 2013;70:675–676. doi: 10.1136/oemed-2013-101594. [DOI] [PubMed] [Google Scholar]
- Chmielewski J, Renke W. Clinical and experimental studies on the pathogenesis of toxic effects of styrene. II. The effect of styrene on the respiratory system. Bull Inst Marit Trop Med Gdynia. 1975;26:299–302. [PubMed] [Google Scholar]
- Coccini T, Fenoglio C, Nano R, De Piceis Polver P, Moscato G, Manzo L. Styrene-induced alterations in the respiratory tract of rats treated by inhalation or intraperitoneally. J Toxicol Environ Health. 1997;52:63–77. doi: 10.1080/00984109708984053. [DOI] [PubMed] [Google Scholar]
- Coggon D, Osmond C, Pannett B, Simmonds S, Winter PD, Acheson ED. Mortality of workers exposed to styrene in the manufacture of glass-reinforced plastics. Scand J Work Environ Health. 1987;13:94–99. doi: 10.5271/sjweh.2067. [DOI] [PubMed] [Google Scholar]
- Coggon D, Ntani G, Harris EC, Palmer KT. Risk of cancer in workers exposed to styrene at eight British companies making glass-reinforced plastics. Occup Environ Med. 2015;72:165–170. doi: 10.1136/oemed-2014-102382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Collins JJ, Bodner KM, Bus JS. Cancer mortality of workers exposed to styrene in the U.S. Reinforced plastics and composite industry. Epidemiology. 2013;24:195–203. doi: 10.1097/EDE.0b013e318281a30f. [DOI] [PubMed] [Google Scholar]
- Convery R, Ward A, Ward R, Bromly CL, Dennis JH, Stenton SC, Bourke SJ, Hendrick DJ. Asthmagenicity of coal mine roof-bolting resins: An assessment using inhalation provocation tests. Occup Med (Oxf) 2001;51:100–106. doi: 10.1093/occmed/51.2.100. [DOI] [PubMed] [Google Scholar]
- Cowles SR, Tsai SP, Gilstrap EL, Ross CE. Mortality among employees at a plastics and resins research and development facility. Occup Environ Med. 1994;51:799–803. doi: 10.1136/oem.51.12.799. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cruzan G, Cushman JR, Andrews LS, Granville GC, Miller RR, Hardy CJ, Coombs DW, Mullins PA. Subchronic inhalation studies of styrene in CD rats and CD-1 mice. Fundam Appl Toxicol. 1997;35:152–165. doi: 10.1006/faat.1996.2273. [DOI] [PubMed] [Google Scholar]
- Cruzan G, Bus J, Hotchkiss J, Sura R, Moore C, Yost G, Banton M, Sarang S. Studies of styrene, styrene oxide and 4-hydroxystyrene toxicity in CYP2F2 knockout and CYP2F1 humanized mice support lack of human relevance for mouse lung tumors. Regul Toxicol Pharmacol. 2013;66:24–29. doi: 10.1016/j.yrtph.2013.02.008. [DOI] [PubMed] [Google Scholar]
- Cullinan P, McGavin CR, Kreiss K, Nicholson AG, Maher TM, Howell T, Banks J, Newman Taylor AJ, Chen CH, Tsai PJ, et al. Obliterative bronchiolitis in fibreglass workers: A new occupational disease? Occup Environ Med. 2013;70:357–359. doi: 10.1136/oemed-2012-101060. [DOI] [PubMed] [Google Scholar]
- Cummings KJ, Kreiss K. Occupational and environmental bronchiolar disorders. Semin Respir Crit Care Med. 2015;36:366–378. doi: 10.1055/s-0035-1549452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cummings KJ, McCague AB, Kreiss K. Nonmalignant respiratory disease mortality in styrene-exposed workers. Epidemiology. 2014;25:160–161. doi: 10.1097/EDE.0b013e3182a70b0f. [DOI] [PubMed] [Google Scholar]
- Epler GR. Constrictive bronchiolitis obliterans: The fibrotic airway disorder. Expert Rev Respir Med. 2007;1:139–147. doi: 10.1586/17476348.1.1.139. [DOI] [PubMed] [Google Scholar]
- Fernandez-Nieto M, Quirce S, Fraj J, del Pozo V, Seoane C, Sastre B, Lahoz C, Sastre J. Airway inflammation in occupational asthma caused by styrene. J Allergy Clin Immunol. 2006;117:948–950. doi: 10.1016/j.jaci.2005.12.1350. [DOI] [PubMed] [Google Scholar]
- Frentzel-Beyme R, Thiess AM, Wieland R. Survey of mortality among employees engaged in the manufacture of styrene and polystyrene at the BASF Ludwigshafen works. Scand J Work Environ Health. 1978;4(Suppl 2):231–239. [PubMed] [Google Scholar]
- Harkonen H. Relationship of symptoms to occupational styrene exposure and to the findings of electroencephalographic and psychological examinations. Int Arch Occup Environ Health. 1977;40:231–239. doi: 10.1007/BF00381410. [DOI] [PubMed] [Google Scholar]
- Hayes JP, Lambourn L, Hopkirk JA, Durham SR, Taylor AJ. Occupational asthma due to styrene. Thorax. 1991;46:396–397. doi: 10.1136/thx.46.5.396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Helal SF, Elshafy WS. Health hazards among workers in plastic industry. Toxicol Ind Health. 2013;29:812–819. doi: 10.1177/0748233712442728. [DOI] [PubMed] [Google Scholar]
- Hempel S, Xenakis L, Danz M. Systematic reviews for occupational safety and health questions. Santa Monica, CA: RAND Corporation; 2016. pp. 1–88. [Google Scholar]
- Hodgson JT, Jones RD. Mortality of styrene production, polymerization and processing workers at a site in northwest England. Scand J Work Environ Health. 1985;11:347–352. doi: 10.5271/sjweh.2214. [DOI] [PubMed] [Google Scholar]
- International Agency for Research on Cancer. IARC monographs on the evaluation of carcinogenic risks to humans—Some traditional herbal medicines, some mycotoxins, naphthalene and styrene. Lyon, France: IARC Press; 2002. pp. 1–590. [PMC free article] [PubMed] [Google Scholar]
- Janigan DT, Kilp T, Michael R, McCleave JJ. Bronchiolitis obliterans in a man who used his wood-burning stove to burn synthetic construction materials. CMAJ. 1997;156:1171–1173. [PMC free article] [PubMed] [Google Scholar]
- Jedrychowski WA, Fonte R. Chronic respiratory symptomatology and obstructive syndrome in workers of a chemical industry. G Ital Med Lav. 1984;6:225–233. [PubMed] [Google Scholar]
- Jedrychowski W. Styrene and methyl methacrylate in the industrial environment as a risk factor of chronic obstructive lung disease. Int Arch Occup Environ Health. 1982;51:151–157. doi: 10.1007/BF00378159. [DOI] [PubMed] [Google Scholar]
- King MS, Eisenberg R, Newman JH, Tolle JJ, Harrell FE, Jr, Nian H, Ninan M, Lambright ES, Sheller JR, Johnson JE. Constrictive bronchiolitis in soldiers returning from Iraq and Afghanistan. N Engl J Med. 2011;365:222–230. doi: 10.1056/NEJMoa1101388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kreiss K. Occupational causes of constrictive bronchiolitis. Curr Opin Allergy Clin Immunol. 2013;13:167–172. doi: 10.1097/ACI.0b013e32835e0282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee JS, Kwak HS, Choi BS, Park SY. A case of occupational asthma in a plastic injection process worker. Ann Occup Environ Med. 2013;25:25. doi: 10.1186/2052-4374-25-25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lewin-Kowalik J, Krause M, Poborska K, Barski JJ, Gorka D, Golka B, Kwiek S, Larysz-Brysz M, Haber-Garlinska J. Occupational exposure of workers in chemical factors and selected parameters of the respiratory system. Med Pr. 1994;45:227–238. [PubMed] [Google Scholar]
- Lorimer WV, Lilis R, Nicholson WJ, Anderson H, Fischbein A, Daum S, Rom W, Rice C, Selikoff IJ. Clinical studies of styrene workers: Initial findings. Environ Health Perspect. 1976;17:171–181. doi: 10.1289/ehp.7617171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lorimer WV, Lilis R, Fischbein A, Daum S, Anderson H, Wolff MS, Selikoff IJ. Health status of styrene-polystyrene polymerization workers. Scand J Work Environ Health. 1978;4(Suppl 2):220–226. [PubMed] [Google Scholar]
- Macaluso M, Larson R, Lynch J, Lipton S, Delzell E. Historical estimation of exposure to 1,3-butadiene, styrene, and dimethyldithio-carbamate among synthetic rubber workers. J Occup Environ Hyg. 2004;1:371–390. doi: 10.1080/15459620490452004. [DOI] [PubMed] [Google Scholar]
- Markopoulo KD, Cool CD, Elliot TL, Lync DA, Newell JD, Jr, Hale VA, Brown KK, Schwarz MI, Tuder RM. Obliterative bronchiolitis: Varying presentations and clinicopathological correlation. Eur Respir J. 2002;19:20–30. doi: 10.1183/09031936.02.00282001. [DOI] [PubMed] [Google Scholar]
- Marsh GM, Youk AO, Stone RA, Buchanich JM, Gula MJ, Smith TJ, Quinn MM. Historical cohort study of US man-made vitreous fiber production workers: I. 1992 fiberglass cohort follow-up: Initial findings. J Occup Environ Med. 2001;43:741–756. doi: 10.1097/00043764-200109000-00004. [DOI] [PubMed] [Google Scholar]
- Matanoski GM, Schwartz L. Mortality of workers in styrene-butadiene polymer production. J Occup Med. 1987;29:675–680. [PubMed] [Google Scholar]
- Matanoski GM, Santos-Burgoa C, Schwartz L. Mortality of a cohort of workers in the styrene-butadiene polymer manufacturing industry (1943–1982) Environ Health Perspect. 1990;86:107–117. doi: 10.1289/ehp.9086107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCague AB, Cox-Ganser JM, Harney JM, Alwis KU, Blount BC, Cummings KJ, Edwards N, Kreiss K. Styrene-associated health outcomes at a windblade manufacturing plant. Am J Ind Med. 2015 doi: 10.1002/ajim.22516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meinhardt TJ, Lemen RA, Crandall MS, Young RJ. Environmental epidemiologic investigation of the styrene-butadiene rubber industry. Mortality patterns with discussion of the hematopoietic and lymphatic malignancies. Scand J Work Environ Health. 1982;8:250–259. doi: 10.5271/sjweh.2469. [DOI] [PubMed] [Google Scholar]
- Morata TC, Sliwinska-Kowalska M, Johnson AC, Starck J, Pawlas K, Zamyslowska-Szmytke E, Nylen P, Toppila E, Krieg E, Pawlas N, et al. A multicenter study on the audiometric findings of styrene-exposed workers. Int J Audiol. 2011;50:652–660. doi: 10.3109/14992027.2011.588965. [DOI] [PubMed] [Google Scholar]
- Morisset Y, P'an A, Jegier Z. Effect of styrene and fiber glass on small airways of mice. J Toxicol Environ Health. 1979;5:943–956. doi: 10.1080/15287397909529803. [DOI] [PubMed] [Google Scholar]
- Moscato G, Biscaldi G, Cottica D, Pugliese F, Candura S, Candura F. Occupational asthma due to styrene: Two case reports. J Occup Med. 1987;29:957–960. [PubMed] [Google Scholar]
- Moscato G, Marraccini P, Dellabianca A, Vinci G, Candura SM. Styrene-induced occupational asthma and rhinitis. G Ital Med Lav. 1988;10:253–259. [PubMed] [Google Scholar]
- National Research Council. Review of the Styrene Assessment in the National Toxicology Program 12th Report on Carcinogens: Workshop Summary. Washington (DC): National Academy of Sciences; 2014. p. 178. [PubMed] [Google Scholar]
- National Toxicology Program. Report on carcinogens. 13th. Research Triangle Park, NC: U.S. Department of Health and Human Services, Public Health Service; 2014. [Google Scholar]
- Nicholson WJ, Selikoff IJ, Seidman H. Mortality experience of styrene-polystyrene polymerization workers. Initial findings. Scand J Work Environ Health. 1978;4(Suppl 2):247–252. [PubMed] [Google Scholar]
- Nurmatov UB, Tagiyeva N, Semple S, Devereux G, Sheikh A. Volatile organic compounds and risk of asthma and allergy: A systematic review. Eur Respir Rev. 2015;24:92–101. doi: 10.1183/09059180.00000714. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Occupational Safety & Health Administration. Styrene. [Accessed August 19, 2016];2016 https://www.osha.gov/SLTC/styrene/
- Occupational Safety and Health Research Institute. Occupational disease casebook Republic of Korea. Korea Occupational Safety and Health Research Agency; 2003. [Google Scholar]
- Ohashi Y, Nakai Y, Ikeoka H, Koshimo H, Nakata J, Esaki Y, Horiguchi S, Teramoto K. Degeneration and regeneration of respiratory mucosa of rats after exposure to styrene. J Appl Toxicol. 1986;6:405–412. doi: 10.1002/jat.2550060605. [DOI] [PubMed] [Google Scholar]
- Okun AH, Beaumont JJ, Meinhardt TJ, Crandall MS. Mortality patterns among styrene-exposed boatbuilders. Am J Ind Med. 1985;8:193–205. doi: 10.1002/ajim.4700080305. [DOI] [PubMed] [Google Scholar]
- Olsen GW, Lacy SE, Cartmill JB, Kravat BA, Chamberlin SR, Spadacene NW, Lipps TE. Half-century of cause-specific mortality experience of chemical manufacturing employees. Am J Ind Med. 1994;26:203–219. doi: 10.1002/ajim.4700260206. [DOI] [PubMed] [Google Scholar]
- Oner F, Mungan D, Numanoglu N, Demirel Y. Occupational asthma in the furniture industry: Is it due to styrene? Respiration. 2004;71:336–341. doi: 10.1159/000079636. [DOI] [PubMed] [Google Scholar]
- Ott MG, Kolesar RC, Scharnweber HC, Schneider EJ, Venable JR. A mortality survey of employees engaged in the development or manufacture of styrene-based products. J Occup Med. 1980;22:445–460. [PubMed] [Google Scholar]
- Robins TG, Haboubi G, Demers RY, Schork MA. Respiratory morbidity of pattern and model makers exposed to wood, plastic, and metal products. Am J Ind Med. 1990;17:173–188. doi: 10.1002/ajim.4700170204. [DOI] [PubMed] [Google Scholar]
- Ruder AM, Ward EM, Dong M, Okun AH, Davis-King K. Mortality patterns among workers exposed to styrene in the reinforced plastic boatbuilding industry: An update. Am J Ind Med. 2004;45:165–176. doi: 10.1002/ajim.10349. [DOI] [PubMed] [Google Scholar]
- Ruder AM, Meyers AR, Bertke SJ. Mortality among styrene-exposed workers in the reinforced plastic boatbuilding industry. Occup Environ Med. 2016;73:97–102. doi: 10.1136/oemed-2015-102990. [DOI] [PubMed] [Google Scholar]
- Sathiakumar N, Delzell E. A follow-up study of mortality among women in the North American synthetic rubber industry. J Occup Environ Med. 2009;51:1314–1325. doi: 10.1097/JOM.0b013e3181bd8972. [DOI] [PubMed] [Google Scholar]
- Sathiakumar N, Delzell E, Hovinga M, Macaluso M, Julian JA, Larson R, Cole P, Muir DC. Mortality from cancer and other causes of death among synthetic rubber workers. Occup Environ Med. 1998;55:230–235. doi: 10.1136/oem.55.4.230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sati PC, Khaliq F, Vaney N, Ahmed T, Tripathi AK, Banerjee BD. Pulmonary function and oxidative stress in workers exposed to styrene in plastic factory: Occupational hazards in styrene-exposed plastic factory workers. Hum Exp Toxicol. 2011;30:1743–1750. doi: 10.1177/0960327111401436. [DOI] [PubMed] [Google Scholar]
- Shah D. Healthy worker effect phenomenon. Indian J Occup Environ Med. 2009;13:77–79. doi: 10.4103/0019-5278.55123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shields PG, McCunney RJ, Chase KH. Confined space hazards: Combined exposure to styrene, fiberglass, and silica. J Occup Environ Med. 1995;37:185–188. doi: 10.1097/00043764-199502000-00017. [DOI] [PubMed] [Google Scholar]
- Styrene Information & Research Center. About styrene. [Accessed August 19, 2016];2014 http://styrene.org/
- Thiess AM, Friedheim M. Morbidity among persons employed in styrene production, polymerization and processing plants. Scand J Work Environ Health. 1978;4(Suppl 2):203–214. [PubMed] [Google Scholar]
- Tucek M, Tenglerova J, Kollarova B, Kvasnickova M, Maxa K, Mohyluk I, Svandova E, Topolcan O, Vlasak Z, Cikrt M. Effect of acrylate chemistry on human health. Int Arch Occup Environ Health. 2002:S67–S72. doi: 10.1007/s00420-002-0381-x. [DOI] [PubMed] [Google Scholar]
- Volkman KK, Merrick JG, Zacharisen MC. Yacht-maker's lung: A case of hypersensitivity pneumonitis in yacht manufacturing. WMJ. 2006;105:47–50. [PubMed] [Google Scholar]
- Welp E, Partanen T, Kogevinas M, Andersen A, Bellander T, Biocca M, Coggon D, Gennaro V, Kolstad H, Lundberg I, et al. Exposure to styrene and mortality from nonmalignant respiratory diseases. Occup Environ Med. 1996;53:499–501. doi: 10.1136/oem.53.7.499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wong O, Trent LS. Mortality from nonmalignant diseases of the respiratory, genitourinary and nervous systems among workers exposed to styrene in the reinforced plastics and composites industry in the United States. Scand J Work Environ Health. 1999;25:317–325. doi: 10.5271/sjweh.441. [DOI] [PubMed] [Google Scholar]
- Wong O, Trent LS, Whorton MD. An updated cohort mortality study of workers exposed to styrene in the reinforced plastics and composites industry. Occup Environ Med. 1994;51:386–396. doi: 10.1136/oem.51.6.386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wong O. A cohort mortality study and a case-control study of workers potentially exposed to styrene in the reinforced plastics and composites industry. Br J Ind Med. 1990;47:753–762. doi: 10.1136/oem.47.11.753. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ye YM, Choi GS, Park HJ, Kim HA, Hur GY, Park HS. Occupational asthma due to styrene and toluene diisocyanate. Korean J Asthma Allergy Clin Immunol. 2007;27:70–73. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


