Abstract
The incidence of laryngeal sarcoma is exceedingly low with osteosarcomas of the larynx being rarer still, comprising less than 1% of all associated malignancies. To date, only 32 cases have been reported since this pathologic entity was first described in 1942. In this article, we discuss the most recent case of laryngeal osteosarcoma in a patient presenting with respiratory distress found to be due to a tumor mass arising from her cricoid cartilage. We further summarize current knowledge regarding the epidemiology, presentation, and diagnosis of this uncommon disease. Lastly, we synthesize all available information regarding treatment and outcomes of the 32 previously described cases of osteosarcoma of the larynx as well as the presently described case in an attempt to offer some insight regarding optimal treatment in future cases.
Key words: Larynx, Osteosarcoma, Chemoradiation, Surgery
Competing interest statement
Conflict of interest: the authors declare no potential conflict of interest.
Introduction
Osteosarcomas of the head and neck account for a minority of all head and neck malignancies. Compared to its more frequently involved subsites, the mandible and maxilla,1 osteosarcomas make up <1% of all laryngeal cancers with the largest review citing only 26 cases since first reported in 1942.2,3 Treatment of this rare disease has ranged from total laryngectomy to definitive radiation as extrapolated from paradigms of common osteosarcomas as well as more common malignancies of the head and neck. This report provides the most comprehensive review of reported cases (Table 1) and in-depth analysis to date. The findings are conveyed in conjunction with the most recent case to be reported.
Table 1.
Presenting symptoms in patients diagnosed with osteosarcoma of the larynx.
| Symptoms | N (%) |
|---|---|
| Hoarseness | 20(61) |
| Dyspnea | 15(45) |
| Dysphagia | 5(15) |
| Odynophagia | 4(12) |
| Stridor | 3(9) |
| Hemoptysis | 2(6) |
| Neck mass | 2(6) |
| Acute airway obstruction | 2(6) |
| Non-specific symptoms | 1(3) |
| Cough | 1(3) |
| Otalgia | 1(3) |
| Globus Sensation | 1(3) |
Case Report
A 48 year-old female never-smoker initially noticed some shortness of breath and increased work of breathing in the autumn of 2013. She was evaluated at her nearby Emergency Department in early November of 2013 and treated for an upper respiratory infection and asthma exacerbation with azithromycin and a short course of prednisone. Her symptoms persisted until January of 2014 when computed tomography (CT) of the chest was unremarkable. At this time she also had associated hemoptysis and stridor. Upon evaluation by pulmonology, her symptoms were felt to be more consistent with vocal cord dysfunction as opposed to lung pathology. On January 29, 2014, she presented with acute respiratory distress and otolaryngology was consulted. A flexible laryngoscopy demonstrated a friable appearing erythematous mass inferior to the level of the true vocal cords at the posterior commissure. CT of the neck showed a mass in the left cricoid cartilage with invasion into the surrounding strap musculature (Figure 1A). Tracheostomy was performed simultaneously with biopsy of the mass; pathology revealed high grade osteosarcoma. Staging positron emission tomography with CT (PET/CT) showed the cricoid mass to be hypermetabolic with suspicious left level IIA and V PET avid lymph nodes (Figure 1B and C). She was evaluated for neoadjuvant chemotherapy and completed 3 cycles of cisplatin (100 mg/m2 on day 1) and doxorubicin (25 mg/m2 on days 1-3) with dose reduction of cisplatin to 80 mg/m2 on the third cycle, which finished on April 12, 2014. On April 30, 2014, a post-chemotherapy PET/CT showed interval decrease in size and FDG uptake in the left-sided cricoid mass (Figure 2). The previously seen suspicious lymph nodes were no longer hypermetabolic. On May 27, 2014, she was taken to the operating room for a total laryngectomy and left thyroid lobectomy. Intraoperative frozen sections reported negative margins, however, final surgical pathology revealed residual disease at the deep tracheal margin. There was no tumor necrosis present. As demonstrated on CT, the tumor appeared to arise from the cricoid cartilage and extended beneath the subglottic mucosa focally into the skeletal muscle. On June 2, 2014, she was taken back to the operating room for re-resection of the tracheal margin, the tissue revealed no evidence of sarcoma.
Figure 1.
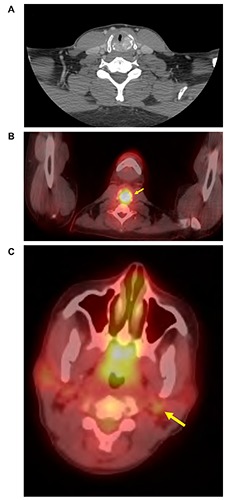
Initial imaging from the from the currently presented case including: A) computed tomography (CT) of the neck revealing a mass in the left cricoid cartilage with invasion of surrounding musculature, B) Initial positron emission tomography with CT fusion (PET/CT) revealing a hypermetabolic mass originating from the left cricoid cartilage; C) Initial PET/CT revealing a suspicious hypermetabolic cervical level IIA lymph node. An additional hypermetabolic level V node was also revealed (not shown).
Figure 2.
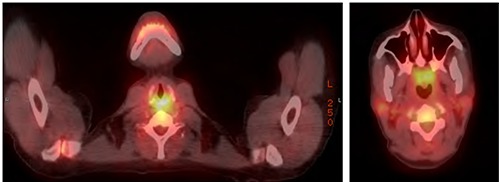
Positron emission tomography/computed tomography following 3 cycles of cisplatin and doxorubicin revealing the patient’s left cricoid mass to be reduced in size and the previously suspicious lymph nodes in cervical nodal levels IIA and V to no longer be hypermetabolic.
Her case was discussed at the multidisciplinary head and neck tumor board. Due to the initial positive margin, high grade pathology and poor response to chemotherapy, post-operative radiation was recommended. On August 20, 2014, she finished a course of post-operative radiation with 6000 cGy delivered in 30 fractions to the surgical bed using volumetric modulated arc therapy (VMAT). Her subsequent follow-up has consisted of clinical visits with appropriate labs and imaging of the neck every 3 months. On September 9, 2016 her most recent CT scan showed stable postsurgical changes of the neck without evidence of recurrent or residual neoplastic disease. Her CT scans of the chest have also remained unremarkable.
Epidemiology
The first case of laryngeal osteosarcoma was described by Jackson & Jackson in 1942. It has proved to be an exceedingly rare diagnosis with only 33 cases reported to date. It predominantly affects males with only 3 of the 33 reported cases in females (9%). Due to the low incidence, risk factors are extrapolated from other sarcomas of the head and neck region, as well as more common presentations of osteosarcomas. Kassir et al. proposed that skeletal Paget’s disease, fibrous dysplasia, retinoblastoma, and previous radiation were possible risk factors.4 There have been 3 cases (9%) of laryngeal osteosarcomas that developed after radiation to the neck for previous nasopharyngeal cancer, squamous cell carcinoma of the supraglottic larynx, and carcinoma in-situ of the true vocal cords. Other suggested factors include laryngeal framework ossification5 and dedifferentiated chondrosarcomas.5-8 Though smoking and alcohol are well established factors in carcinosarcoma/sarcomatoid carcinomas of the larynx,9,10 the reporting of these two factors are incomplete among case reports in osteosarcoma thus any association is currently inconclusive. Patients tend to present after the 6th decade of life, with a median age at diagnosis of 61 years and a reported age range of 38-84 years. Of the 33 published cases to date, 29 were at least 50 years old with age not provided in a single reported case.11
Presentation and diagnosis
As would be expected for malignancies originating in the larynx, dyspnea and hoarseness are common presentations. Of the 33 reported cases, 15 (45%) reported dyspnea at presentation and 20 (61%) reported hoarseness with an additional 5 (15%) reporting general dysphonia not specified as hoarse voice. Other reported presenting symptoms include dysphagia in 5 (15%), odynophagia in 4 (12%), stridor in 3 (9%), painless mass in 2 (6%), hemoptysis in 2 (6%), acute airway obstruction in 2 (6%), cough in 1 (3%), otalgia in 1 (3%), and globus sensation in 1 (3%) (Table 1).
On physical exam, all of the patients with reported laryngoscopies (direct or indirect) had abnormal findings. The majority of the tumors arose from the true vocal cords (13 patients, 39%). The anterior commissure and thyroid cartilage were the next most common sites with 4 cases (12%) each. Two cases (6%) reported tumor arising from the post cricoid space and two from the cricoid. The remaining 8 (24%) were not otherwise specified (Table 2). CT scans showed infiltrating masses often with calcifications.
Table 2.
Location of tumor origin in patients diagnosed with osteosarcoma of the larynx.
| Location | N (%) |
|---|---|
| Cricoid/postcricoid | 4(12) |
| True vocal cord | 13(39) |
| Anterior commissure | 4(12) |
| Thyroid cartilage | 4(12) |
| Not otherwise specified | 8(24) |
Once tissue is obtained, the histologic diagnosis continues to be elusive. Sampling errors can increase the false negative rate. Further, fixation, antibody characterization and antigen retrieval can also misconstrue false positive or false negative immunohistochemical findings. Pathologists must also sufficiently identify malignant osteoid production and exclude epithelial differentiation to preclude the diagnosis of carcinosarcomas.12 Additionally, multiple histologic subtypes have been reported with osteoblastic osteosarcoma being the most common but with fibroblastic, chondroid, telengectatic, small cell and well-differentiated variants also reported. Due to location, presentation, and appearance both on imaging and histologically, the differential for this diagnosis may include spindle cell sarcoma, carcinosarcoma, metastases from a primary sarcoma, and other malignant tumors with osseous metaplasia.13
Treatment
The exceedingly low incidence of the tumor precludes strong evidence-based decision making. Therapies have been extrapolated both from principles of laryngeal cancer as well as osteosarcoma such that surgery maintains its principle role for curative treatment. Thirty of the 33 patients reported underwent some form of surgery comprising of 24 total laryngectomies, 4 partial laryngectomies and 2 local excisions (Supplementary Table S1). Three patients underwent primary radiation therapy in lieu of surgical intervention despite the fact that osteosarcomas are generally thought to be radioresistant. Additionally, 7 patients had postoperative radiation and 6 had chemotherapy incorporated into their primary treatment. In total, ten patients received salvage therapy with 2 receiving local excision for skin-only recurrences, 5 receiving salvage radiation therapy, and 4 receiving chemotherapy after recurrence.
Outcomes
Recurrence free and overall survivals appear to be mixed in patients diagnosed with osteosarcoma of the larynx (Figure 3 and Supplementary Table S1). Of the 33 published cases, 12 patients (36%) had not succumbed to their disease at the time of last follow-up which ranged from 4 to 96 months following diagnosis. Further, durable disease-free survival after initial treatment was achieved in 9 reported patients (28%) with follow-up again ranging from 4 to 96 months. Of note, a single patient died from unrelated causes at 12 months following diagnosis and 2 additional patients did not have any reported post-treatment follow-up. Importantly, all patients who remained recurrence free and/or alive at the time of last follow-up underwent surgical resection as the primary mode of therapy with 9 undergoing a total laryngectomy, 2 undergoing partial laryngectomy, and 1 receiving local excision only. Of the patients who recurred, the majority (13 patients, 39%) failed distantly with local recurrence in 4 (12%) and regional recurrence in 7 (21%). Regional failure consisted of recurrence in the soft-tissues of the neck either with or without associated cervical lymph node involvement. Two reported cases were noted to have recurrence without specification regarding type or location. Notably, recurrence both locoregionally and distantly tend to occur early, with the majority of patients failing within 12 months of initial diagnosis with median times to recurrence being 5 months and 12 months, respectively (Figure 3a-b). Of the four patients who recurred locally, all were initially treated with surgical resection with 2 receiving post-op radiation therapy and one receiving chemotherapy as part of their initial treatments. Upon local recurrence, the two patients who received prior radiation therapy were treated with salvage surgery with or without chemotherapy and remained without disease recurrence at 60 months while the remaining 2 patients were treated with salvage radiation with or without further resection and survived 14 and 3 months, respectively. Regional recurrence in the neck was rarely seen without concurrent uncontrolled local or distant failure as well, with information regarding salvage therapy being generally sparse. Almost invariably, patients with regional failure ultimately died from their disease though 2 of the 7 reported cases did not provide follow-up information following disease recurrence.
Figure 3.
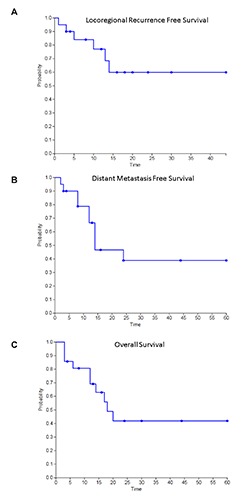
Kaplan-Meyer curves (in months) for A) locoregional recurrence-free survival; B) distant recurrence-free survival; C) overall survival in patients diagnosed with osteosarcoma of the larynx.
Distant failure appears most commonly in the lungs (present in 9 cases reported), followed by bone (2 cases) and mediastinum (1 case). In 2 cases, location of distant failure was not reported.
Patient outcomes based on treatment were notably heterogeneous as well (Table 3). Of the 22 patients who received surgery alone as initial treatment for their disease, 3 (13.6%) failed locally, 6 (27.3%) failed regionally, and 10 (45.5%) failed distantly while 8 (36.4%) remained disease-free at the time of last follow-up. As would be expected, total laryngectomy was associated with less local failure when compared to smaller surgeries with 1 patient (5.6%) failing locally following total laryngectomy only while 2 of the reported 4 patients who underwent local excision or subtotal laryngectomy alone suffered local relapse. Of the 6 patients treated with a combination of surgical resection and radiation therapy, 4 (66.7%) remained disease-free at the time of last follow-up with a single patient recurring locally and another recurring distantly. Only one reported patient was treated initially with a combination of surgical resection and chemotherapy and was noted to suffer early distant failure at 3 months postresection, precluding further assessment of durable local response with this combination. Interestingly, upfront trimodality therapy did not appear to further improve patient outcomes in the three reported cases, with one patient failing locally, one failing distantly, and the currently reported patient remaining without recurrence at 25 months following initial diagnosis.
Conclusions
Osteosarcoma of the head and neck remains a rare diagnosis with only 33 cases reported since it was initially described in 1942. Due to this dearth of cases, no consensus exists regarding optimal treatment or expected outcomes. In this review, we report on the most recent known case of this unusual disease and provide the most comprehensive information regarding past cases, treatments provided, and outcomes observed to date. While the presented data remains sparse, we hope that it may provide a guide for future treating clinicians.
References
- 1.Mendenhall WM, Fernandes R, Werning JW, et al. Head and neck osteosarcoma. Am J Otolaryngol 2011;32:597-600. [DOI] [PubMed] [Google Scholar]
- 2.Jackson C, Jackson C. CH XXV-malignant diseases of the larynx. Diseases and injuries of the larynx. New York: Macmillan Publishing Company; 1942. [Google Scholar]
- 3.Mosalleum E, Afrogheh A, Stofberg S, et al. A review of primary osteosarcoma of the larynx and case report. Head Neck Pathol 2015;9:158-64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kassir RR, Rassekh CH, Kinsella JB, et al. Osteosarcoma of the head and neck: meta-analysis of nonrandomized studies. Laryngoscope 1997;107:56-61. [DOI] [PubMed] [Google Scholar]
- 5.Athre RS, Vories A, Mudrovich S, Ducic Y. Osteosarcomas of the larynx. Laryngoscope 2005;115:74-7. [DOI] [PubMed] [Google Scholar]
- 6.Ulusan M, Yilmazer R, Ozluk Y, et al. Radiation-induced osteosarcoma of the larynx: Case report and literature review. Ear Nose Throat J 2012;91:E22-5. [PubMed] [Google Scholar]
- 7.Sheen TS, Wu CT, Hsieh T, Hsu MM. Postirradiation laryngeal osteosarcoma: case report and literature review. Head Neck 1997;19:57-62. [DOI] [PubMed] [Google Scholar]
- 8.Laskin WB, Silverman TA, Enzinger FM. Postradiation soft tissue sarcomas. an analysis of 53 cases. Cancer 1988;62:2330-40. [DOI] [PubMed] [Google Scholar]
- 9.Thompson LD, Wieneke JA, Miettinen M, Heffner DK. Spindle cell (sarcomatoid) carcinomas of the larynx: a clinicopathologic study of 187 cases. Am J Surg Pathol 2002;26:153-70. [DOI] [PubMed] [Google Scholar]
- 10.Roy S, Purgina B, Seethala RR. Spindle cell carcinoma of the larynx with rhabdomyoblastic heterologous element: a rare form of divergent differentiation. Head Neck Pathol 2013;7:263-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Rydzewski B, Matusiak M. Osteosarcoma of the larynx. Otolaryngol Pol 2005;59:285-8. [PubMed] [Google Scholar]
- 12.Arslan M, Orhan-Kizilkaya H, Yalcin B, et al. Larynx osteosarcoma: case report. J B U ON 2008;13:437-9. [PubMed] [Google Scholar]
- 13.Bhatt NR, Kakked GA, Merchant R, Bhatt R. Extraskeletal osteosarcoma of the larynx: An extremely unusual tumour. BMJ Case Rep 2014;2014: 206759. [DOI] [PMC free article] [PubMed] [Google Scholar]


