Abstract
Spinal schwannomas are benign intradural extramedullary tumors arising from spinal nerve root sheath. They are usually solid or heterogeneously solid. Totally cystic schwannomas are rare entities. Herein, we report a 60-year-old male presenting with backache radiating along the chest wall and weakness of both lower limbs. He had spastic paraparesis. Magnetic resonance imaging revealed a cystic mass in the thoracic region. At operation, the cystic mass was seen to be attached to D4 dorsal rootlets. It was excised in toto and histopathology confirmed it to be a schwannoma. The relevant literature is reviewed.
Keywords: Cystic, intradural-extramedullary, schwannoma
Introduction
Schwannoma is a benign slow-growing encapsulated tumor that arises from myelinated nerve sheath. Total cystic change is rare in these tumors. Schwannomas are the most common benign intradural-extramedullary spinal tumors arising from the sheaths of the spinal roots. Most spinal schwannomas are solitary and solid and some present with a dumbbell shape. The lumbar region is the commonest site for the occurrence of spinal schwannomas. Although schwannomas located in the thoracic region are not rare, totally cystic schwannomas in this region are very rare and hence the present case is being reported.
Case Report
A 60-year-old male was admitted with backache radiating along the chest wall and weakness of both lower limbs of 8-month duration. Weakness initially involved the left lower limb and then progressed to involve the right lower limb. Urinary dribbling was present for the last two months. On examination, he had spastic paraparesis with power being grade 0 on the left side at all joints and grade 3 to 4 in the right lower limb. Deep tendon jerks were exaggerated and plantars were extensor bilaterally. Sensations were diminished up to D6 level. Plain X-ray of the thoracic spine was normal. MRI revealed a well-delineated lesion, hypointense on T1WI, and hyperintense on T2WI [Figure 1]. Thoracic laminectomy was performed and per-operatively the lesion was found to be totally cystic and attached to the filament of the D4 dorsal root [Figure 2]. The cyst contained xanthochromic fluid and it was excised in toto. The patient recovered completely and has no clinical evidence of recurrence over the last 2 years and 9 months of follow-up. Histopathological examination revealed the lesion to be a cystic schwannoma [Figure 3].
Figure 1.
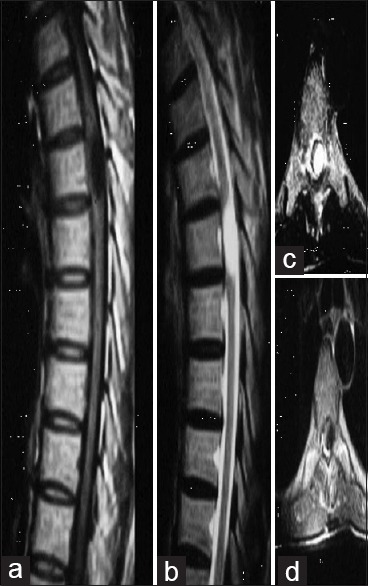
MRI scan showing intradural extramedullary lesion hypointense on T1WI sagittal (a) and axial (d), and hyperintense on T2WI sagittal (b) and axial (c) at the D4-5 level
Figure 2.
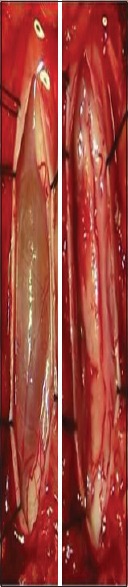
Intraoperative photograph showing a cystic lesion on left side displacing the cord to right
Figure 3.
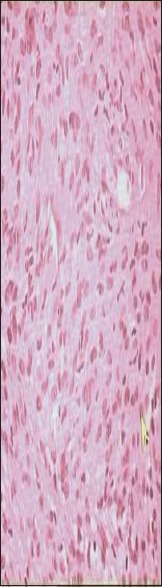
Microphotograph showing spindle shaped cells with elongated nuclei arranged in a palisading fashion (H and E, ×100)
Discussion
Schwannomas are slow-growing benign tumors. They are usually encapsulated and rarely undergo malignant transformation. Schwannomas are more frequent in patients with neurofibromatosis type-2. They are mostly solid or heterogeneously solid tumors.[1] Intradural extramedullary cystic schwannomas are rare.[2,3,4,5,6] Jaiswal et al. could find only 10 cases with predominantly cystic changes reported in the literature.[7] Cystic schwannomas are most common in the lumbar region and occur rarely in the thoracic region. In a review of literature, we could find only two totally cystic schwannomas of the thoracic region reported in the English language. First being by Shen et al., in 1992 and second by Karatas et al., in 2007.[2,8] Schwannomas arise from the embryonic neural crest cells of the nerve sheaths of peripheral and cranial nerves. Schwannomas and neurofibromas account for 30% of all intra-spinal masses.[9] Spinal schwannomas are well-delineated intradural or extradural lesion or intra-extradural and rarely intramedullary. These tumors have a predilection for lumbar, lower cervical and thoracolumbar junction and upper thoracic location is less common as was seen in our case as well.[10]
Schwannoma may become symptomatic at any age, but peak incidence is between fourth and fifth decades.[1,9,10] Clinical symptoms are usually due to compression of the spinal cord or roots. Local pain, paraesthesia, numbness and motor weakness may be present. Tumors arising in the cauda and cervical region can become larger than those at thoracic region because of spacious canal at these levels.
MRI is the mainstay of diagnosis. Schwannomas generally have low to intermediate signal intensity on T1WI. On T2-weighted images, they may be heterogeneous with focal areas of hyperintensity, which indicates cyst within the tumor. Totally cystic tumor as seen in our case is hypointense on T1 and hyperintense on T2-weighted images and has to be differentiated from Tarlov cyst, arachnoid cyst, neurenteric cyst, epidermoid cyst, and cystic teratoma.[11,12,13]
Cystic schwannoma have a well-enhancing wall compared to other cystic lesions mentioned above that usually lack this structure.[11] Epidermoids are slightly hypointense to CSF on T1W images and hyperintense on T2W images. Dermoid cysts may have associated sinus tract and hyperintense areas on T1W and T2W images due to fat. Neurenteric cysts extend through long levels and are usually located anterior to the cord. Teratomas are usually mixed intensity lesions. Definitive diagnosis is based on histopathology. Schwannomas consist of spindle-shaped cells with pale eosinophilic cytoplasm. Cells are arranged in compact fashion in Antoni A type and loosely arranged in Antony B type. In our case, the patient had brought the MRI from outside without contrast injection. Repeat MRI with contrast was not asked for in this hospital considering the cost factor. Treatment consists of radical excision.
In our case, complete excision was easily possible by separating it from the filament of the posterior root from which it was arising and the patient has had no recurrence in the last 2 years and 9 months.
Cystic changes in schwannomas have been attributed to degeneration of Antoni B portion of a neurinoma or ischemic necrosis caused by tumor growth resulting in cyst formation.[1]
Conclusion
Intradural extramedullary cystic schwannoma should be considered in the differential diagnosis of any cystic mass. The lesion should be excised completely to avoid recurrence of the tumor. The rootlets to which it is attached may be sacrificed in the thoracic region as it does not lead to any deficit because of overlapping of the skin supplied by the adjacent roots.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Parmar H, Patkar D, Gadani S, Shah J. Cystic lumbar nerve sheath tumors: MRI features in five patients. Australas Radiol. 2001;45:123–7. doi: 10.1046/j.1440-1673.2001.00891.x. [DOI] [PubMed] [Google Scholar]
- 2.Karatas A, Is M, Yildirim U, Akyuz F, Gezen Fl. Thoracic intradural cystic schwannoma: A case report. Turk Neurosurg. 2007;17:193–6. [PubMed] [Google Scholar]
- 3.Kasliwal MK, Kale SS, Sharma BS, Suri V. Totally cystic intradural extramedullary schwannoma. Turk Neurosurg. 2008;18:404–6. [PubMed] [Google Scholar]
- 4.Albert AF, Kirkman MA, du Plessis D, Sacho R, Cowie R, Tzerakis NG. Giant solitary cystic schwannoma of the cervical spine: A case report. Clin Neuron Neurosurg. 2012;114:396–8. doi: 10.1016/j.clineuro.2011.10.039. [DOI] [PubMed] [Google Scholar]
- 5.Hsich CT, Tsai WC, Liu MY. Intradural lumbar cystic schwannoma. Neurosciences (Riyadh) 2011;16:366–8. [PubMed] [Google Scholar]
- 6.Vikram M, Pande A, Vasudevan MC, Ravi R. Cervical long segment cystic schwannoma. Br J Neurosurg. 2010;24:208–10. doi: 10.3109/02688690903301557. [DOI] [PubMed] [Google Scholar]
- 7.Jaiswal A, Shetty AP, Rajasekaran S. Giant cystic intradural schwannoma in the lumbosacral region: A case report. J Orthop Surg. 2008;16:102–6. doi: 10.1177/230949900801600124. [DOI] [PubMed] [Google Scholar]
- 8.Shen WC, Lee SK, Chang CY, Ho WL. Cystic spinal neurilemmoma on magnetic resonance imaging. Neuroradiology. 1992;34:447–8. doi: 10.1007/BF00596514. [DOI] [PubMed] [Google Scholar]
- 9.Conti P, Pansini G, Mouchaty H, Capuano C, Conti R. Spinal neurinomas: Retrospective analysis and long-term outcome of 179 consecutively operated cases and review of literature. Surg Neurol. 2004;61:34–43. doi: 10.1016/s0090-3019(03)00537-8. [DOI] [PubMed] [Google Scholar]
- 10.Seppala MT, Haltia MJ, Sankila RJ, Jaaskelainen JE, Heiskanen O. Long term outcome after removal of spinal schwannoma: A clinic-pathological study of 187 cases. J Neurosurg. 1995;83:621–6. doi: 10.3171/jns.1995.83.4.0621. [DOI] [PubMed] [Google Scholar]
- 11.Beall DP, Googe DJ, Emery RL, Thompson DB. Extramedullary intradural spinal tumors: A pictorial review. Curr Probl Diagn Radiol. 2007;36:185–98. doi: 10.1067/j.cpradiol.2006.12.002. [DOI] [PubMed] [Google Scholar]
- 12.Scarrow AM, Levy EL, Gerszten PC, Kulich SM, Chu CT, Welch WC. Epidermoid cyst of the thoracic spine: Case history. Clin Neurol Neurosurg. 2001;103:220–2. doi: 10.1016/s0303-8467(01)00156-1. [DOI] [PubMed] [Google Scholar]
- 13.Stevens QE, Kattner KA, Chen YH, Rahman MA. Intradural extramedullary mature cystic teratoma: Not only a childhood disease. J Spinal Disord Tech. 2006;19:213–6. doi: 10.1097/01.bsd.0000188664.54014.c4. [DOI] [PubMed] [Google Scholar]


