Highlights
-
•
Very rare clinical entity.
-
•
Large Association with multiple uro-genital malformation.
-
•
Discovered usually by accident.
-
•
Associated with infertility.
Keywords: Vas deferens, Embryology, Case repot, Urogenital, Rare abnormality
Abstract
Introduction
Congenital absence of the vas deferens (CUAVD) is a rare clinical entity, usually discovered accidently during surgical procedures of the urogenital zone, CUAVD has the prevalence of 0.5–1.0% in male population and it is associated with various forms of congenital genitourinary malformations like renal agenesis. we present a case of a 21 years old, male, managed in our private hospital for varicoceles and discovered to have CUAVD and ectopic kidney.
Presentation of case
A 21 years old male, with no significant medical or surgical history presented to our out-patient clinic complaining of scrotal heaviness and pain. upon physical examination he was discovered to have a bilateral varicocele and was scheduled for a bilateral varicocelectomy, during the procedure he was discovered with left side CUAVD.
Discussion
Congenital unilateral absence of the vas deference is a very rare clinical entity in the male population it has an incidence of 0.5–1.0%. it is usually discovered during evaluation for infertility or surgical procedures of the urogenital zone. Unilateral congenital absence of the vas deference is more associated with renal agenesis (73.3%), compared to the bilateral form (11.8%). CAVD is responsible of 1–2% of male infertility.
Conclusion
Congenital absence of the vas deference is a unique clinical entity due to its great association with a large variety of urogenital abnormalities, we present this case to stress the importance of including scrotal examination in the routine physical exam to reduce the late diagnosis of such abnormality and it associated comorbidities.
1. Introduction
Congenital absence of the vas deferens (CUAVD) is a rare clinical entity, usually discovered accidently during surgical procedures of the urogenital zone, it was first discovered by a Scottish surgeon in 1737 by the name of John Hunter [1], CUAVD has the prevalence of 0.5–1.0% in male population and it is associated with various forms of congenital genitourinary malformations like renal agenesis, in 1870 a Swiss surgeon by the name of Jacques-Louis Reverdin first described the association of CUAVD and renal agenesis on the same side [2]. According to the SCARE criteria [3]; we present a case of a 21 years old, male, managed in our private hospital for varicoceles and discovered to have CUAVD and ectopic kidney.
2. Presentation of case
A 21 years old male, married, with No history of smoking, drug abuse or other systemic disease, presented to our out-patient clinic complaining of scrotal pain and heaviness sensation with mild enlargement and failure to establish pregnancy after three years of trying. Upon physical examination, the scrotum revealed bilateral enlargement of the pampiniform plexuses and minimal scrotal enlargement, scrotal ultrasonography was done and showed bilateral minimal hydrocele, and patient was scheduled for a bilateral varicocelectomy after two days (Fig. 1), patient seminal fluid analysis showed oligospermia.
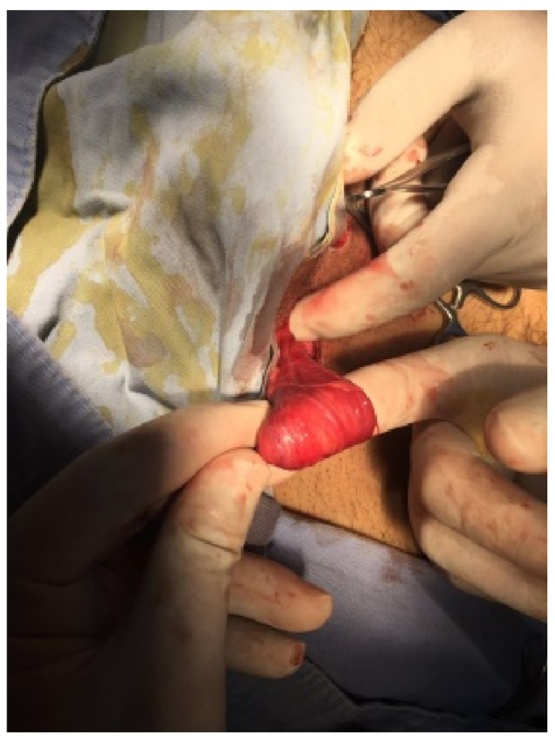
Fig. 1.

Right testicular varicocele, open surgery view.
During the procedure, patient went under general anesthesia and was placed in supine position and a microscopic sub inguinal approach was decided and a 3 cm oblique incision was done centered over the external inguinal ring and camper's and scarpa's fascia were opened and the spermatic cord grasped with a Babcock and place over a piece of gauze, the testicular artery was isolated but the vas deferens was not found the tortuous veins were ligated (Fig. 2). Post operation due to the common association between CUAVD and renal abnormalities, patient was sent for an abdominal-pelvis ultrasonography where he was found to have left ectopic kidney localized in the mid lower abdomen (Fig. 3), patient was discharged after 2 days with no active complains and a followed up after 2 weeks.
Fig. 2.
Absence left vas deferens, open surgery view.
Fig. 3.
Abdominal ultrasonography showing left ectopic kidney in the lower mid abdomen.
3. Discussion
Congenital unilateral absence of the vas deference is a very rare clinical entity in the male population it has an incidence of 0.5–1.0% [4], it is usually discovered during evaluation for infertility or surgical procedures of the urogenital zone. Patients with CUAVD are generally divided into two subgroups upon their fertility status; fertile patients with CUAVD have a high incidence of ipsilateral renal agenesis, and infertile patients who have a normal upper urinary tract but a partially obstructed vas deference of the contralateral side [4]. Left side CUVAD occurs twice as more than right CUAVD.
Unilateral congenital absence of the vas deference is more associated with renal agenesis (73.3%), compared to the bilateral form (11.8%) [4], CUAVD association with renal agenesis is due to an intrinsic defect in the wolffian duct, in course of the development of the urogenital system in embryogenesis, the vas deferens originates from the wolffian duct, which connects the urogenital sinus with the mesonephros, also the ureteral bud starts to develop as the wollfian duct starts to curve to enter the cloaca, the development of the kidney is induced by the penetration of the urethral bud in the metanephrogenic blastema, any defect in this process or interruption before the complete separation of the wolffian duct can lead to CUAVD and renal agenesis where interruption after the separation can lead to an isolated CUAVD [2]. Other reasons may include primary absence of the caudal nephrogenic core, urethral bud malformation, and dysplasia of mesonephric duct [5], [6], [7].
CUAVD has been associated with other anomalies of kidney as ectopic kidney, multicystic kidney, horseshoe kidney and malrotation of the solitary kidney [6], and with anomalies of the ejaculatory ducts, cryptorchidism and the seminal vesicles. Anomalies of the inguinal zone such as inguinal hernia have been also reported [5]. With rare cases of uretrovesical obstruction and vesicoureteric reflux in the contralateral kidney also. There have been cases of adrenal gland agenesis occurring with CUAVD and ipsilateral renal agenesis [7].
CAVD is responsible of 1–2% of male infertility [4], generally caused by CBAVD and a small number caused by CUAVD due to obstruction in the contralateral vas deferens.
There is a close relationship between CUAVD and cystic fibrosis gene(CFTR) as studies showed [8] that about 38% of CUAVD have mutations of the CFTR gene and 45% of CFTR mutations were specific to CAVD and were not found in cystic fibrosis patients, 26% of the CFTR mutations in patients with CAVD were detected by the OLA/PCR mutations detection system, this underlines the importance of CFTR gene analysis in these patients because of the risk of related diseases and cystic fibrosis in their offspring’s [8].
CAVD can be diagnosed by physical examination in the absence of the round, firm, sliding linguini-like vas deferens that is in continuation with the epididymis and can be followed throw out the external inguinal ring, or by the use of transrectal ultrasonography or vasography by the detection of the missing vas. The delay in diagnosing CAVD can lead to increase mortality and morbidity rates associated with this anomaly due to associated abnormalities of the urogenital area as indicated by Weiss [6], that why palpating the vas deferens should by in the routine checkup of male patients. Patient diagnosed with CAVD should undergo obligatory abdominal pelvis ultrasonography to detect further urogenital anomalies and patients with renal agenesis should undergo exploration of the scrotum to detect absence of the vas deferens.
4. Conclusions
Congenital absence of the vas deference is a unique clinical entity due to its great association with a large variety of urogenital abnormalities, we present a case of CUAVD and an ectopic kidney discovered accidentally during a bilateral varicocelectomy, to stress the importance of including scrotal examination in the routine physical exam to reduce the late diagnosis of such abnormality and it associated comorbidities.
Conflicts of interest
No conflict of interest.
Funding
No sources of funding were used in the completion of this case report.
Ethical approval
No ethical approval was needed.
Author contribution
Authors have equal contribution in all related matters.
Guarantor
Dr.Alobaidi Salwan.
Dr.Alhmooze Abdelrahman.
Contributor Information
Alobaidi Salwan, Email: salwanalobaidi@yahoo.com.
Alhmooze Abdelrahman, Email: drabdelrahmanalhmooze@gmail.com.
REFERENCES
- 1.Hunter J. On the glands called vesiculae seminales. In: Palmer J.F., editor. vol. 4. Longman, Reese, Orm, Brown, Green and Longman; London: 1737. p. 23. (Complete Works). [Google Scholar]
- 2.Reverdin M. Absence der rein, de l’uretere, du canal deferent, et de la vesicule seminale du cote gauche: Existence des deux testicules dans les bourses. Bull. Soc. Anat. Paris. 1870;65:325. [Google Scholar]
- 3.Agha R.A., Fowler A.J., Saetta A., Barai I., Rajmohan S., Orgill D.P., SCARE Group The SCARE Statement: consensus-based surgical case report guidelines. Int. J. Surg. 2016;34:180–186. doi: 10.1016/j.ijsu.2016.08.014. [DOI] [PubMed] [Google Scholar]
- 4.Weiske W.H., Sälzler N., Schroeder-Printzen I., Weidner W. Clinical findings in congenital absence of the vasa deferentia. Andrologia. 2000;32(1):13–18. [PubMed] [Google Scholar]
- 5.Kolettis P.N., Sandlow J.I. Clinical and genetic features of patients with congenital unilateral absence of the vas deferens. Urology. 2002;60(6):1073–1076. doi: 10.1016/s0090-4295(02)01973-8. [DOI] [PubMed] [Google Scholar]
- 6.Khan Z.A., Novell J.R. A missing vas. J. R. Soc. Med. 2001;94(11):582–583. doi: 10.1177/014107680109401108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Nakada T., Furuta H., Kazama T., Katayama T. Unilateral renal agenesis with or without ipsilateral adrenal agenesis. J. Urol. 1988;140(5):933–937. doi: 10.1016/s0022-5347(17)41892-1. [DOI] [PubMed] [Google Scholar]
- 8.Casals T., Bassas L., Egozcue S. Heterogeneity for mutations in the CFTR gene and clinical correlations in patients with congenital absence of the vas deferens. Hum. Reprod. 2000;15(7):1476–1483. doi: 10.1093/humrep/15.7.1476. [DOI] [PubMed] [Google Scholar]



