Abstract
Introduction:
Childhood malignancy, although a rare phenomenon, is still the leading cause of mortality in the pediatric population. Early diagnosis and treatment are imperative for the achievement of optimal prognosis. The study of factors facilitating the delay in diagnosis is thus of utmost importance, to both shorten the diagnostic delay and allow for early therapeutic intervention, facilitating a higher prognosis.
Objective:
To assess the referral pattern and the identification of potential delays in the diagnosis of childhood malignancy in a developing country.
Methodology:
The study was conducted in the Pediatric Hematology and Oncology department of Sri Ramachandra University, Chennai, India. The study included randomly selected 70 pediatric patients diagnosed with a hematological malignancy, from July 2012-August 2013. The parents were interviewed using a prepared questionnaire about patient symptomatology, interaction with healthcare providers, final diagnosis, and referral details. Data were statistically analyzed using Statistica® (STATsoft).
Results:
70 patients were included in the study (69% boys, 31% girls). The diagnostic delay was primarily due to the delay experienced in the healthcare system, with a mean delay of 26 days (Median: 18; Range: 5-39). Those from a lower socioeconomic background and whom opted for a non-allopathic treatment approach experienced higher diagnostic delays. Diagnostic time was significantly shorter for those who visited a pediatrician versus the patients who visited a general physician or super specialties (P = 0.043).
Conclusions:
Diagnostic delay is often associated with an extensive disease presentation, an aggressive therapeutic approach, and has a negative impact on patient prognosis. To lower mortality rate and facilitate a favourable prognosis, diagnosis requires a high degree of clinical suspicion and immediate intervention.
Key words: Childhood cancer, developing country, diagnostic delay, road to diagnosis
Introduction
Childhood malignancy is the second leading causes of mortality in the pediatric population in developed countries, with a diagnostic age-adjusted incidence of approximately 105–150/million.[1] Mirroring the increase in the incidence of childhood malignancy in developed countries, developing nations also show a rise in pediatric cancers. In a study conducted by Satyanarayana et al., it has been estimated that the incidence of pediatric malignancy in India from 2006 to 2011 ranged from approximately 18.6 to 159.6/million in boys and 11.3 to 112.4/million in girls.[2] The rising incidence of the pathology thus requires a more effective and time-sensitive approach to the diagnosis and intervention. The early diagnosis of cancer facilitates ample opportunity and time to allow for treatment, optimizing patient prognosis. Although there has been significant progress in oncological management over the past few decades, the consistently rising case fatality rates indicate ineffective management, possibly due to the delayed diagnosis of the condition. It has been estimated that up to 70% of pediatric malignancies are treatable, provided adequate access to medical personnel in established tertiary medical centers.[3] Given that the majority of the pediatric population is situated in developing countries, approximately only 20% have adequate access to medical facilities.[3,4] Various factors, including the complexity of pathology, patient's socioeconomic status, healthcare provider, and the bureaucracy of the healthcare system, may contribute to the diagnostic delay. A thorough understanding of the factors contributing to the diagnostic delay is thus mandated to ensure immediate and effective treatment. This study aims to identify the various factors delaying the diagnosis, as perceived by the patient and patient's families, and will include a literature review in light of the similarities and differences in diagnostic delay pertaining to pediatric hematological malignancies, internationally.
Materials and Methods
Participants
The parents or informants of 70 randomly selected pediatric patients, with a hematological malignancy, undergoing cancer treatment in Sri Ramachandra Hospital, between July 2012 and August 2013, were selected and interviewed based on a predesigned questionnaire. An informed consent was obtained from each informant before the commencement of the study. The research protocol was approved by the Ethics Committee. The questionnaire used for the study was validated by two pediatric researchers. The data were extracted and compiled on Microsoft Excel 2009 for comparison, and Statistica®(StatSoft) Version 12 was used for statistical analysis and interpretation.
Interview
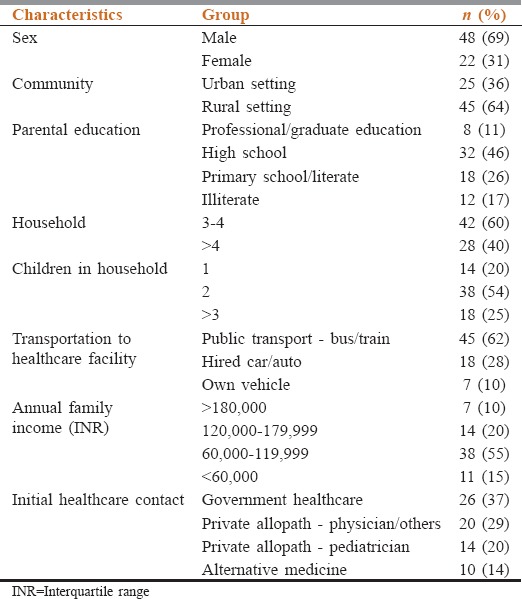
A semi-structured questionnaire was used which included demographic statistics, including guardian employment and socioeconomic status, patient symptomatology, their interaction with healthcare providers and facilities, diagnosis, and treatment and referral patterns. To minimize the possibility of recall bias, prescriptions, medical bills, and referral slips were collected for additional information and verification. The interview lasted for approximately 45–60 min. Table 1 outlines the basic demographic characteristics of the study participants.
Table 1.
Patient characteristics and demographics
Conceptual framework
Our study aims to identify factors associated with the diagnostic delay of malignancy, and thus encompasses the variables that are hypothesized to affect the diagnostic course: Patient demographics and socioeconomic status, the pathological extent of the disease, and healthcare bureaucracy involved in patient referral, diagnosis, and treatment. “Patient delay” refers to the time interval between the onset of patient symptoms and the patient's first visit to the allopathic healthcare system. “Physician delay” or “healthcare system delay” is the delay between the first healthcare visit and the pathological diagnosis of malignancy. “Total delay,” otherwise defined as “lag time” by Martin et al.,[5] is the time interval between the presentation of patient symptomatology and signs, and the pathological confirmation of an existing malignancy. For simplicity, the delay has been measured in days.
Results
Of the 70 patients with hematological malignancies, with 69% boys and 31% girls, the mean age was 7.8 ± 2.2 years. The diagnostic delay, in most patients, was attributed to healthcare system delay with a median delay of 18 days (mean 26, range 5–39). The parental delay was significantly higher with patients from rural areas (n = 43, P = 0.046) and whose parents had lower levels of education (highest being 44 days). Patients who approached alternative practices (herbal home remedies [n = 3], alternative medicine [n = 5], religious practices [n = 2]) for their first mode of care had significantly higher diagnostic delays (P = 0.019). Other reasons for patient's delay exceeding more than 1 week, viz., symptoms temporarily alleviated by supportive measures (n = 5), lack of financial means (n = 4) and parents thought symptoms were caused by a preexisting condition (n = 7). Age of onset did not have a significant influence on patient delay or total delay. A trend of increasing patient delay was noticed among children over 9.5 years (P = 0.139, n = 16), albeit once variables such as family income, household size and approach to alternative medicine as the first contact were controlled for the analysis, age was no longer statistically significant predictor of patient delay (P = 0.84). In the median total diagnostic delay (including patient delay, first contact delay and specialist delay) was of 59 days (mean 41 days, range 18–69). Diagnosis and first contact delay were relatively shorter for patients who visited a pediatrician than for patients whose first health contact was a general physician or physicians of other specialties (P = 0.043). Pediatric-oncologists were never approached as the first contact. Number of different contacts and hospital admissions in the health system was a significant factor causing a delay in diagnosis. The median number of healthcare visits by parents was 4 and an average number of days of admission was 9 days, before they were evaluated by a specialist. In 52 of 70 patients interviewed, information about the primary diagnosis by the first contact physician was available. Of which 18 patients were suspected to have malignancy and were referred to a tertiary care. Most common misdiagnosis was tuberculosis (TB) in various forms (TB lymph node, pulmonary/peritoneal TB) (n = 11) followed by anemia (n = 9), acute gastroenteritis (n = 3), juvenile arthritis/autoimmune (n = 4) and unnamed infection (n = 7). The most common treatment given was antibiotics followed by nonsteroidal anti-inflammatory drugs and nutritional supplements. Geographical distance from access to tertiary healthcare is also positively associated with diagnostic delay. There was no significance impact on delays based on gender, religion, parental profession, type of family, and number of siblings. Correlation between the stage and severity of the disease at presentation and its impact on diagnostic delay could not be assessed using the study data.
Discussion
This retrospective study attempts to analyze the factors involved in the diagnostic delay of pediatric hematological malignancies. Although numerous articles pertaining to malignancy in the pediatric population have been published in developed countries, very few have studied the causality of diagnostic delay in the developing nations, particularly India. A thorough understanding of the variables contributing to this delay is mandated, for early diagnosis and intervention, and to lower patient mortality. In this study, delays were considered intervals in the path of healthcare management of pediatric patients with hematological cancers, without implying any value in terms of clinical acceptability.
Patient age, sex, and religion were analyzed for significance in delayed referral and diagnosis, but no correlation was found in our study. Surprisingly, the study conducted by Abdelkhalek et al. demonstrated a significant correlation between patient age and diagnostic delay: Patients 5–10 years of age experienced a mean diagnostic delay of 25 days (P = 0.01).[6] Similar results were found in numerous studies, including a retrospective study conducted by Araz and Guler.[7]
Parental delay demonstrated reciprocity to the level of parental education, socioeconomic status, and geographical location: Patients with parents of primary level education and increased the geographical distance from healthcare facilities experienced a greater parental delay. Similar findings were observed in the previously mentioned study.[6] However, no relationship was found in our study between parental occupation and diagnostic delay. Interestingly, this contradicts findings from the study conducted by Ramesh et al.[8] In addition, patients with parents of primary educational levels were found to practice initially religious home remedies, or approach alternative healthcare such as Homeopathy or Siddha. These practices may also be attributable to the socioeconomic status and health care accessibility of patients, in addition to the educational level. In addition, the parental delay was also due to the incurrence of medical expenses, primarily in those of lower socioeconomic status. The financial burden is further increased when taking into account nonmedical expenses, in the form of travel, accommodation, and diet. To minimize parental delay, adequate parental education, and social support systems should ideally be provided. Public awareness of the disease presentation and symptomatology, and financial aid for both the medical and nonmedical treatment expenses could lead to a decrease in a parental delay in diagnosis.
Once within the healthcare system, the delay may be attributable to the expertise of the provider, administrative processes within the system, or availability of appropriate diagnostic instrumentation, and are collectively referred to as “healthcare system delays.” Physician's clinical acumen and expertise are difficult to measure quantitatively, and previous studies and malignancy protocols have emphasized the importance of clinical suspicion when faced with constitutional symptoms.[9] The common occurrence of misdiagnoses in developing countries mandate a high degree of clinical suspicion, facilitating a decrease delay times and providing a favorable patient prognosis. Additionally, the supportive treatment of malignant symptomatology, in forms including antipyretics, steroids, blood transfusions, and antibiotics, further facilitate the delay in diagnosis. Paradoxically, the delayed diagnosis of malignancy predominantly presents with increased symptomatology, facilitating the diagnostic process. However, due to the extensive, and possibly, metastatic pathology, it merits aggressive and toxic chemotherapy, limits the interventional capacity of the physician, and negatively impacts survival outcome. Regular and continued medical education programs on the current situation of pediatric malignancies in India, for physicians in both the government and private sectors, must be conducted to reduce first contact delays. Additionally, extensive and more effective protocols for the diagnosis and management of pediatric neoplasia must be defined and nationally established. Further studies are merited to confirm and consolidate the current understanding of factors contributing to the diagnostic delay in malignancy within the pediatric population.
Study limitations
Our study is retrospective, with a relatively smaller sample size (n = 70), decreasing the validity and reliability of the results. It is based out of a single institution, and may not be representative of the entire pediatric population. Second, only malignancies of the hematological variety were included in the study; solid malignancies were not included. Third, disease staging was not taken into account when studying factors contributing to the diagnostic delay. Additionally, due to the chronicity of the disease, recall bias may have possibly influenced the patient's recollection of symptomatology. Finally, our study faces challenges in methodology and a lack of interpretative standards.
Conclusion
The delayed diagnosis of neoplastic disorders is often associated with extensive and metastatic pathologies, and high patient morbidity and mortality. It is thus imperative to practice increased vigilance when encountered with vague constitutional symptoms. Further quantitative studies, with larger sample sizes, are mandated to consolidate our understanding. Finally, effective and standardized protocols should be nationally established to ensure that a treatable condition, such as pediatric cancer, is not allowed to progress to death.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgment
This study was supported and funded by Chancellor Summer Research Fellowship for medical students, Sri Ramachandra University, Porur, Chennai, Tamil Nadu, India. We extend our heartfelt thanks to the parents and all the beautiful children waging a war against cancer who contributed to this study.
References
- 1.Stiller CA, Marcos-Gragera R, Ardanaz E, Pannelli F, Almar Marqués E, Cañada Martinez A, et al. Geographical patterns of childhood cancer incidence in Europe, 1988-1997.Report from the automated childhood cancer information system project. Eur J Cancer. 2006;42:1952–60. doi: 10.1016/j.ejca.2006.05.017. [DOI] [PubMed] [Google Scholar]
- 2.Satyanarayana L, Asthana S, Labani SP. Childhood cancer incidence in India: A review of population-based cancer registries. Indian Pediatr. 2014;51:218–20. doi: 10.1007/s13312-014-0377-0. [DOI] [PubMed] [Google Scholar]
- 3.Chirdan LB, Bode-Thomas F, Chirdan OO. Childhood cancers: Challenges and strategies for management in developing countries. Afr J Paediatr Surg. 2009;6:126–30. doi: 10.4103/0189-6725.54783. [DOI] [PubMed] [Google Scholar]
- 4.Stefan DC, Baadjes B, Kruger M. Incidence of childhood cancer in Namibia: The need for registries in Africa. Pan Afr Med J. 2014;17:191. doi: 10.11604/pamj.2014.17.191.3830. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Martin S, Ulrich C, Munsell M, Taylor S, Lange G, Bleyer A. Delays in cancer diagnosis in underinsured young adults and older adolescents. Oncologist. 2007;12:816–24. doi: 10.1634/theoncologist.12-7-816. [DOI] [PubMed] [Google Scholar]
- 6.Abdelkhalek E, Sherief L, Kamal N, Soliman R. Factors associated with delayed cancer diagnosis in egyptian children. Clin Med Insights Pediatr. 2014;8:39–44. doi: 10.4137/CMPed.S16413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Araz NC, Guler E. Delays in diagnosis of childhood cancer in Southeastern Turkey and the associated factors. Pediatr Hematol Oncol. 2015;32:153–63. doi: 10.3109/08880018.2013.874511. [DOI] [PubMed] [Google Scholar]
- 8.Ramesh PM, Marwaha RK, Anish TS. Childhood cancer in developing society: A roadmap of health care. Indian J Med Paediatr Oncol. 2011;32:30–3. doi: 10.4103/0971-5851.81887. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Haimi M, Peretz Nahum M, Ben Arush MW. Delay in diagnosis of children with cancer: A retrospective study of 315 children. Pediatr Hematol Oncol. 2004;21:37–48. [PubMed] [Google Scholar]


