Dear Editor,
Osteosarcoma is a frequently occurring primary malignant bone tumor, characterized by osteoid producing atypical cells.[1] Brain metastases are rare, with a reported incidence of 1.8–5.6%, and associated with prior pulmonary metastasis, with the hypothesis of lung tumor emboli invading the brain.[2,3] We present a case of osteosarcoma of the femur in a middle-aged female with a long disease-free survival of more than 7 years, later presenting with brain metastases.
A 36-year-old woman presented with swelling in the lower lateral aspect of left thigh for about 6 months duration in 2005. She was diagnosed as a case of osteosarcoma and underwent resection. Hisptopathological examination (HPE) of the resected tissue was suggestive of fibroblastic osteosarcoma. She received 6 cycles of iphosphamide, adriamycin, and cisplatin-based chemotherapy until March 2006. She was kept on follow-up and was asymptomatic for 6 years until December 2012 when she presented with cough and left sided chest pain. She was evaluated with a positron emission tomography-computed tomography (CT) scan that showed left pulmonary metastatic mass invading the left pulmonary vein. She underwent left pnuemonectomy and intercostal muscle flap cover in February 2013. HPE confirmed the diagnosis of metastatic osteosarcoma. In view of the long disease-free survival after first platinum-based adjuvant treatment, she was planned and given 6 cycles of iphosphamide and cisplatin-based chemotherapy until July 2013. Postchemotherapy CT chest done in August 2013 showed postpnuemonectomy status with no evidence of disease and was kept on follow-up. She was asymptomatic for about 15 months but later presented to the hospital in November 2014 with complaints of progressive left sided weakness of 1 week duration. Her higher mental functions and cranial nerves were normal. Motor examination revealed left hemiparesis (power left upper limb 4/5, left lower limb 2/5). There was no other focal neurological deficit.
She was further evaluated in detail and magnetic resonance imaging brain with contrast revealed a solitary large space occupying lesion in the right posterior frontal parasagittal region with intralesional calcification and perilesional edema [Figure 1]. After informed consent, she was taken up for surgery in November 2014 and right fronto-parietal craniotomy and decompression of the lesion was done. Postsurgery, she improved neurologically and regained full power on the left side. Histopathology report of the lesion was suggestive of metastatic deposit of osteosarcoma.
Figure 1.
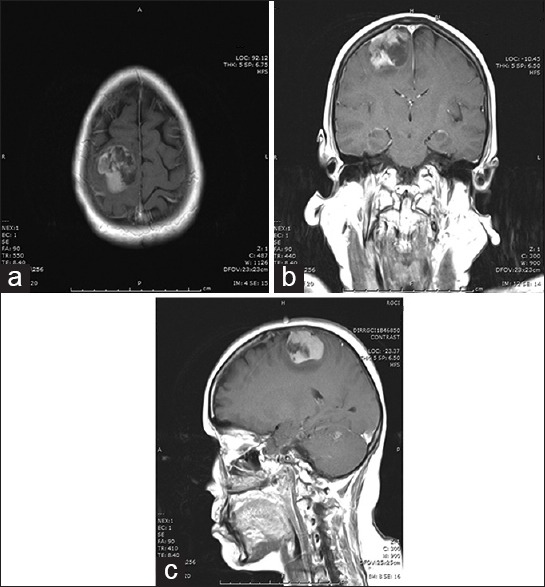
Contrast enhanced T1-weighted spin-echo image showing enhancing lesion in right frontal lobe (a) axial (b) coronal (c) sagittal
Breast cancer, nonsmall cell lung cancer, and melanoma have shown a penchant for brain involvement.[4,5] Brain metastases are approximately 10 times more common than primary brain tumors.[4,5,6,7] It is estimated that 3% of all brain metastases develop from sarcomas and 1–8% of all sarcoma patients may develop brain metastases.[6,7] The only exception is patients with alveolar soft part sarcoma in whom the incidence is 33%.[8] Unlike many other brain metastases, sarcomas tend to be highly radio and chemo-resistant, with surgical resection being the main basis for management.[6] Mechanisms of sarcoma spread to the brain are through hematogenous dissemination into brain parenchyma and contiguous extension of metastases in bones of the skull into intracranial structures.[9] As in other brain metastases, those from osteosarcoma typically locate through the anterior circulation to the gray-white matter junction.[10]
There is an increase in the incidence of brain metastases in soft tissue and bony sarcomas due to new chemotherapeutic and radiotherapeutic treatments that prolong survival through systemic disease control but without effective intracranial control.[4,5,7] An increased risk of brain metastases with metastatic disease at presentation or with recurrence at 1 year has been reported.[4] Mean interval to brain metastases from initial diagnosis was approximately 20 months from diagnosis of the primary.[11] Yonemoto et al. recommended performing brain imaging periodically in patients with known active pulmonary metastasis.[12] This was echoed by Marina et al. for those with metastatic disease at diagnosis or in whom recurrence develops within 12 months, though whether routine imaging will improve outcomes is debatable.[13] Multimodality treatment is often involved, though no consensus on treatment exists.[11] Brain metastases management almost always involves surgical resection followed by whole brain radiation therapy and/or chemotherapy in select cases.[11] As many of these lesions are solitary, surgical excision has been the standard of care, with chemotherapy and RT for palliative measures.
As a commonly diagnosed musculoskeletal cancer in children and young adults, osteosarcoma, when metastatic, mainly spreads to the lungs and other bones and rarely to the brain. As such, it is difficult to form consensus guidelines on treatment once brain metastases occur.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Betzler M. Klassifikation der Knochentumoren verbindet Kliniker und Pathologen. Klinikarzt. 1983;12:959–71. [Google Scholar]
- 2.Link MP, Gebhardt MC, Meyers PA. Principles and Practice of Pediatric Oncology. 5th ed. Lippincott Williams and Wilkins; 2005. Osteosarcoma; pp. 1075–113. [Google Scholar]
- 3.Deutsch M, Orlando S, Wollman M. Radiotherapy for metastases to the brain in children. Med Pediatr Oncol. 2002;39:60–2. doi: 10.1002/mpo.10042. [DOI] [PubMed] [Google Scholar]
- 4.Kebudi R, Ayan I, Görgün O, Agaoglu FY, Vural S, Darendeliler E. Brain metastasis in pediatric extracranial solid tumors: Survey and literature review. J Neurooncol. 2005;71:43–8. doi: 10.1007/s11060-004-4840-y. [DOI] [PubMed] [Google Scholar]
- 5.Chou YS, Liu CY, Chen WM, Chen TH, Chen PC, Wu HT, et al. Brain, the last fortress of sarcoma: Similar dismal outcome but discrepancy of timing of brain metastasis in bone and soft tissue sarcoma. J Surg Oncol. 2011;104:765–70. doi: 10.1002/jso.22011. [DOI] [PubMed] [Google Scholar]
- 6.Fox BD, Patel A, Suki D, Rao G. Surgical management of metastatic sarcoma to the brain: Clinical article. J Neurosurg. 2009;110:181–6. doi: 10.3171/2008.4.17505. [DOI] [PubMed] [Google Scholar]
- 7.Salvati M, D'Elia A, Frati A, Santoro A. Sarcoma metastatic to the brain: A series of 35 cases and considerations from 27 years of experience. J Neurooncol. 2010;98:373–7. doi: 10.1007/s11060-009-0085-0. [DOI] [PubMed] [Google Scholar]
- 8.Lieberman PH, Brennan MF, Kimmel M, Erlandson RA, Garin-Chesa P, Flehinger BY. Alveolar soft-part sarcoma. A clinico-pathologic study of half a century. Cancer. 1989;63:1–13. doi: 10.1002/1097-0142(19890101)63:1<1::aid-cncr2820630102>3.0.co;2-e. [DOI] [PubMed] [Google Scholar]
- 9.Postovsky S, Ash S, Ramu IN, Yaniv Y, Zaizov R, Futerman B, et al. Central nervous system involvement in children with sarcoma. Oncology. 2003;65:118–24. doi: 10.1159/000072336. [DOI] [PubMed] [Google Scholar]
- 10.Singh SK, Leeds NE, Ginsberg LE. MR imaging of leptomeningeal metastases: Comparison of three sequences. AJNR Am J Neuroradiol. 2002;23:817–21. [PMC free article] [PubMed] [Google Scholar]
- 11.Shweikeh F, Bukavina L, Saeed K, Sarkis R, Suneja A, Sweiss F, et al. Brain metastasis in bone and soft tissue cancers: A review of incidence, interventions, and outcomes. Sarcoma. 2014;2014:475175. doi: 10.1155/2014/475175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Yonemoto T, Tatezaki S, Ishii T, Osato K, Takenouchi T. Longterm survival after surgical removal of solitary brain metastasis from osteosarcoma. Int J Clin Oncol. 2003;8:340–2. doi: 10.1007/s10147-003-0341-9. [DOI] [PubMed] [Google Scholar]
- 13.Marina NM, Pratt CB, Shema SJ, Brooks T, Rao B, Meyer WH. Brain metastases in osteosarcoma. Report of a long-term survivor and review of the St. Jude children's research hospital experience. Cancer. 1993;71:3656–60. doi: 10.1002/1097-0142(19930601)71:11<3656::aid-cncr2820711130>3.0.co;2-l. [DOI] [PubMed] [Google Scholar]


