Abstract
Introduction
Two-dimensional laparoscopy for living donor nephrectomy is the current standard of care. We report the first case of three-dimensional laparoscopy for living-donor nephrectomy with vaginal extraction.
Presentation of case
The procedure was performed in a 66-year-old woman donating his left kidney to her son with the HD S 3D column (Karl Storz, Tuttlingen, Germany). Preoperative computed tomography showed one left renal artery. The warm ischemic time was 2 min 20 s and the operative time was 200 min. There was no loss of blood and no intraoperative or postoperative complications.
Discussion
This report demonstrates the feasibility of using 3D laparoscopy which allows for a more in-depth vision, greater overall definition of planes, better accuracy of dissection and reduced operative times, for nephrectomy with vaginal extraction for kidney donation.
Conclusion
Three-dimensional laparoscopy for living-donor nephrectomy with vaginal extraction is feasible and could become a new standard.
Keywords: 3-dimensional, Laparoscopy, Nephrectomy, Living-donor, Vagina
1. Introduction
Renal transplantation from living donors is now a common surgical procedure due to the shortage in cadaveric donors and the improvements in graft survival. Laparoscopic kidney removal is currently the gold standard and offers the advantages of reduced post-operative pain, limited scarring and a shorter hospital stay. The transvaginal approach for kidney extraction with living donor has previously been emphasized showing advantages in recovery and cosmesis [1].
Three-dimensional laparoscopy was developed several years ago but has not been widely adopted in surgery since it is expensive and often leads to headaches and eye strain for surgeon [2]. Very recently, third generation 3D laparoscopy has become available. It has been shown to produce a more in-depth vision of tissues, with increased definition and better spatial orientation, allowing greater surgical precision, reduced hospital stays and shorter training times [3], [4].
We report the first case of nephrectomy with vaginal extraction for kidney donation using 3D laparoscopy. The work has been reported according to the SCARE criteria [5].
2. Case report
A 66-year-old woman was referred to perform a left nephrectomy to donate a kidney to her son. She had no significant medical history. Preoperative computed tomography showed a left renal artery, a renal vein and a ureter.
The procedure was performed under general anaesthesia using an HD S 3D column (Karl Storz, Tuttlingen, Germany). The patient was placed in the lateral position (Fig. 1) and four trocars were put in place: one 12 mm trocar on a vertical line through the navel, two finger widths from the outside lateral edge of the rectus muscle; one 5 mm trocar at the same horizontal level a finger width under the ribs; one 10 mm trocar midway along the lateral edge of the rectus muscle; and, during surgery, one 5 mm trocar was placed in the left flank symmetrically to the 10 mm trocar.
Fig. 1.
The patient is placed in the lateral position with 30°’ abduction legs.
The procedure was carried out in the usual way, firstly with the left colon being moved to expose the kidney. The gonadal vein was then moved in line with the renal vein. The splenic flexure and pancreas and spleen en bloc were then moved in line with the upper edge of the kidney. The upper edge of the renal vein was then mobilised and the adrenal vein was controlled and severed by thermofusion (Ligasure®, Covidien-Medtronic, USA). The upper pole of the kidney was then mobilised, and the gonadal vein and azygos vein were then controlled and severed by thermofusion. The renal artery was mobilised up to the ostium and the ureter was mobilised up to where it crosses the iliac artery. The kidney was then completely released. An incision of the posterior vaginal cul-de-sac was made laparoscopically after the insertion of a retractor in the vagina and a wound retractor was put in place (Alexis®, Applied medical, Rancho Santa Margarita, CA, USA), into which an endobag was introduced (Fig. 2). After sectioning the ureter between two Hem-o-loks (Teleflex, Wayne, PA, USA) at the point where it crosses the iliac artery, the kidney was placed into the endobag and the artery and the vein were each clamped and then sectioned. The kidney was removed and washed. The vagina was sutured laparoscopically with V-Loc™ (Covidien-Medtronic, USA) and the different incisions were sutured.
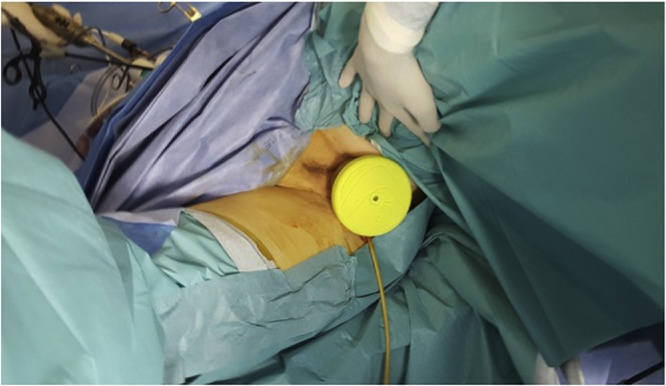
Fig. 2.
A wound retractor was put in the vagina allowing the kidney extraction.
The warm ischemic time was 2 min 20 s and the operative time was 200 min. There was no loss of blood and no intraoperative or postoperative complications. The patient was discharged on the second postoperative day. The transplanted organ behaved as expected, with the recovery of renal function on the same evening as the intervention.
3. Discussion
This report shows the feasibility of using 3D laparoscopy for nephrectomy with vaginal extraction for kidney donation. The value of 3D vision in performing nephrectomies for kidney donation has already been demonstrated for robotic surgery, however this uses older technology than that used here and allows only the operator a three dimensional view, an important limiting factor when operational assistance is required, especially when clamping the vessels. Moreover, the lack of force feedback and its high cost are additional limitations to the wide uptake of this technology.
This is the first report to date showing the use of 3D laparoscopy to perform nephrectomy with vaginal extraction in humans. The new generation 3D laparoscopy used here allows for a more in-depth vision, greater overall definition of tissues and better accuracy of dissection. This is in line with reported results on other urological interventions. For example, when used for adrenalectomy this 3D laparoscopy technology was shown to be superior to standard 2D techniques in terms of better precision, increased definition of tissues and more in-depth vision. For the operator, there was also reduced stress in the upper arms and eyes and a lower risk of headaches [3]. Similar results were reported for cystectomy, with reduced operative times due to the increased definition of tissues [6]. It therefore appears that 3D laparoscopy could gradually replace 2D techniques in urological surgery.
Thus, for nephrectomy with vaginal extraction, and especially in cases of kidney donation, additional studies are now needed to establish the benefits of this technique, which could become standard procedure in future.
Conflicts of interest
No conflict of interest to disclose.
Funding
This study was not supported by any grant.
Ethical approval
Not applicable.
Consent
Written consent from the patient to publish a case report has been obtained.
Author contributions
Xavier Gamé: data collection and writing the paper.
Mouath Binhazzaa: data collection.
Michel Soulié: review the manuscript.
Nassim Kamar: review the manuscript.
Fédérico Sallusto: data collection and review the manuscript.
Registration of research studies
Not required.
Guarantor
Prof Xavier Gamé.
References
- 1.Alcaraz A., Musquera M., Peri L., Izquierdo L., Garcia-Cruz E., Huguet J. Feasibility of transvaginal natural orifice transluminal endoscopic surgery-assisted living donor nephrectomy: is kidney vaginal delivery the approach of the future? Eur. Urol. 2011;59(6):1019–1025. doi: 10.1016/j.eururo.2011.03.021. [DOI] [PubMed] [Google Scholar]
- 2.Sakata S., Watson M.O., Grove P.M., Stevenson A.R. The conflicting evidence of three-dimensional displays in laparoscopy: a review of systems old and new. Ann. Surg. 2016;263(2):234–239. doi: 10.1097/SLA.0000000000001504. [DOI] [PubMed] [Google Scholar]
- 3.Agrusa A., di Buono G., Chianetta D., Sorce V., Citarrella R., Galia M. Three-dimensional (3D) versus two-dimensional (2D) laparoscopic adrenalectomy: a case-control study. Int. J. Surg. 2016;28(Suppl. 1):S114–S117. doi: 10.1016/j.ijsu.2015.12.055. [DOI] [PubMed] [Google Scholar]
- 4.Cicione A., Autorino R., Laguna M.P., De Sio M., Micali S., Turna B. Three-dimensional technology facilitates surgical performance of novice laparoscopy surgeons: a quantitative assessment on a porcine kidney model. Urology. 2015;85(6):1252–1256. doi: 10.1016/j.urology.2015.03.009. [DOI] [PubMed] [Google Scholar]
- 5.Agha R.A., Fowler A.J., Saeta A., Barai I., Rajmohan S., Orgill D.P. The SCARE statement: consensus-based surgical case report guidelines. Int. J. Surg. 2016;34:180–186. doi: 10.1016/j.ijsu.2016.08.014. [DOI] [PubMed] [Google Scholar]
- 6.Tang F.J., Qi L., Jiang H.C., Tong S.Y., Li Y. Comparison of the clinical effectiveness of 3D and 2D imaging systems for laparoscopic radical cystectomy with pelvic lymph node dissection. J. Int. Med. Res. 2016;44(3):613–619. doi: 10.1177/0300060515621445. [DOI] [PMC free article] [PubMed] [Google Scholar]