Martínez and Blasco review the molecular mechanisms underlying diseases associated with telomere dysfunction, including telomeropathies, age-related disorders, and cancer. Current and future therapeutic strategies to treat and prevent these diseases, including preclinical development of telomere-targeted therapies using mouse models, are discussed.
Abstract
Telomeres, the protective ends of linear chromosomes, shorten throughout an individual’s lifetime. Telomere shortening is proposed to be a primary molecular cause of aging. Short telomeres block the proliferative capacity of stem cells, affecting their potential to regenerate tissues, and trigger the development of age-associated diseases. Mutations in telomere maintenance genes are associated with pathologies referred to as telomere syndromes, including Hoyeraal-Hreidarsson syndrome, dyskeratosis congenita, pulmonary fibrosis, aplastic anemia, and liver fibrosis. Telomere shortening induces chromosomal instability that, in the absence of functional tumor suppressor genes, can contribute to tumorigenesis. In addition, mutations in telomere length maintenance genes and in shelterin components, the protein complex that protects telomeres, have been found to be associated with different types of cancer. These observations have encouraged the development of therapeutic strategies to treat and prevent telomere-associated diseases, namely aging-related diseases, including cancer. Here we review the molecular mechanisms underlying telomere-driven diseases and highlight recent advances in the preclinical development of telomere-targeted therapies using mouse models.
Telomeres, telomerase, and shelterins
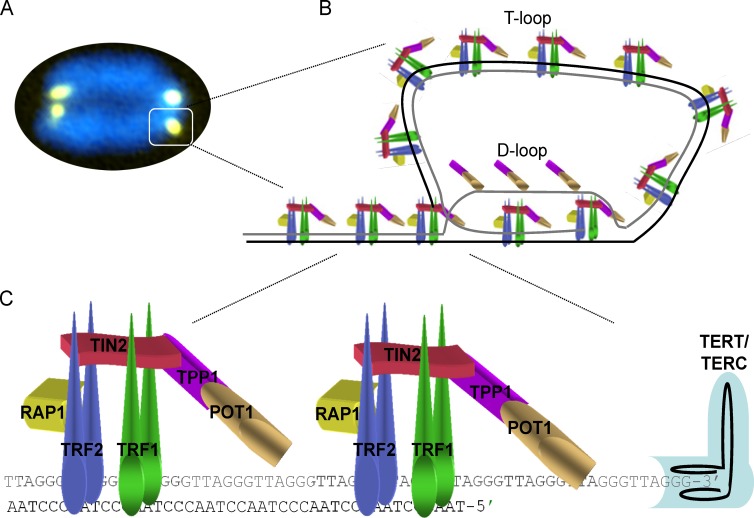
Telomeres form a special heterochromatic structure at the end of linear chromosomes that protects them from degradation and DNA repair and recombination activities. Thus, telomeres are essential to ensure chromosome stability (Blasco, 2005; Palm and de Lange, 2008). Mammalian telomeres comprise several kilobases, between 10 and 15 kb in humans and 25 and 50 kb in mice, of tandem TTAGGG DNA repeats (Blasco, 2005). Telomeres are characterized by the presence of a 30–400-nucleotide-long 3′ overhang of a G-rich strand, known as the G-strand overhang. The G-strand overhang can fold back and invade the double-stranded telomeric region, forming the so-called T-loop and generating a displacement loop, or D-loop. The T-loop structure has been proposed to protect chromosome ends from degradation and DNA repair activities as well as from telomerase activity (Fig. 1, A and B; Griffith et al., 1999; Doksani et al., 2013). Telomeres are bound by a specialized complex known as shelterin that has crucial functions in telomere length regulation and in the protection of telomeres from the DNA damage response (DDR) by masking the chromosome ends from the DNA repair machinery through repression of the ATM and ATR signaling pathways (Palm and de Lange, 2008; Fig. 1 C). The shelterin complex is composed of six proteins: telomeric repeat binding factors 1 and 2 (TRF1 and TRF2), TRF1-interacting protein 2 (TIN2), protection of telomeres protein 1 (POT1), TIN2, POT1-interacting protein (TPP1), and repressor/activator protein 1 (RAP1; Fig. 1 C; de Lange, 2005; Martínez and Blasco, 2010, 2011).
Figure 1.
The shelterin complex and the structure of telomeres. (A) Representative image of a metaphasic chromosome stained with DAPI (blue) and the telomeric DNA–specific peptide nucleic acid probe (yellow). (B) Schematic model of the shelterin complex bound to a telomere in a T-loop configuration. Telomeres contain a double-stranded region of TTAGGG repeats and a 150–200-nucleotide-long single-stranded DNA overhang of a G-rich strand. The G-strand overhang (gray) invades the telomeric double-stranded DNA region to form a protective T-loop, with a displacement D-loop at the invasion site. (C) Schematic representation of telomere-bound proteins, the shelterin complex, and telomerase. The shelterin complex is composed of the telomeric repeat binding factor 1 (TRF1, also known as TERF1), TRF2 (also known as TERF2), repressor-activator protein 1 (RAP1, also known as TERF2IP1), POT1-TIN2 organizing protein (TPP1, also known as ACD), TIN2 (also known as TIFN2), and protection of telomeres protein 1 (POT1). TRF1, TRF2, and POT1 bind directly to telomeric DNA repeats, with TRF1 and TRF2 binding to telomeric double-stranded DNA and POT1 to the 3′ single-stranded G-overhang. TIN2 binds TRF1 and TRF2 through independent domains and recruits the TPP1–POT1 complex, constituting the bridge among the different shelterin components. Telomerase is a two-partner enzyme, the catalytic subunit (TERT) and the RNA template (TERC), that recognizes the 3′-OH at the end of the G-strand overhang and elongates the telomere.
Telomeres shorten with each cell division as a result of the incomplete replication of linear DNA molecules by conventional DNA polymerases, which is called the end-replication problem (Watson, 1972; Olovnikov, 1973). Telomerase compensates for telomere attrition through de novo addition of TTAGGG repeats onto chromosome ends in those cells where it is normally expressed, such as pluripotent stem cells and adult stem cell compartments (Liu et al., 2007; Flores et al., 2008; Marion et al., 2009). Telomerase is composed of a reverse transcriptase subunit (TERT) as well as an associated RNA component (Terc), which is used as a template for the de novo addition of telomeric repeats (Fig. 1 C; Greider and Blackburn, 1985). Although telomerase is expressed in adult stem cell compartments, this is not sufficient to counteract telomere attrition associated with cell division throughout life, and therefore telomeres shorten with age in vitro and in vivo (Harley et al., 1990; Hastie et al., 1990; Lindsey et al., 1991; Collado et al., 2007; Liu et al., 2007; Flores et al., 2008; Marion et al., 2009). This progressive telomere shortening eventually leads to critically short telomeres that can impair the regenerative capacity of tissues and has been proposed as one of the molecular hallmarks of aging (López-Otín et al., 2013). In mice, it has been shown that the rate of increase in the percentage of short telomeres, rather than the rate of telomere shortening throughout life, is a significant predictor of life span (Vera et al., 2012). Shortened telomeres induce a DDR that leads to a growth arrest, during which cells attempt to repair the damage and, if DNA damage is irreparable, triggers replicative senescence (Zou et al., 2004; Fumagalli et al., 2012). Senescent cells progressively accumulate during life and secrete factors that influence age-associated diseases (Tchkonia et al., 2013). Indeed, senescence has been proposed as a mechanism that evolved to protect from cancer, with the drawback of promoting age-associated diseases (Shay, 2016). Therapeutic interventions based on either chemical activators of telomerase or telomerase-based gene therapy are currently being investigated in mouse models for their potential to improve health and extend life span, and as a treatment for short telomere syndromes (Bernardes de Jesus et al., 2011; Bär et al., 2014, 2015; Bär and Blasco, 2016).
Aging-associated diseases and telomeropathies
Telomeres shorten progressively throughout an individual’s lifetime (Cawthon et al., 2003; López-Otín et al., 2013; Sanders and Newman, 2013). Telomere attrition in stem cell compartments impairs their tissue and self-renewal capacity and is considered to be one of the primary molecular causes of aging and the onset of aging-associated diseases (Flores et al., 2005; Sharpless and DePinho, 2007). The first demonstration that telomere shortening is at the origin of age-related pathologies and is a determinant of longevity came from the study of telomerase-deficient mice, which show premature aging phenotypes in both low-proliferating (heart, brain) and high-proliferating compartments (bone marrow [BM], gut, skin, and testis; Blasco et al., 1997; Lee et al., 1998; Herrera et al., 1999; Leri et al., 2003; Ferrón et al., 2004). Telomere shortening with age has also been observed in several mouse stem cell compartments from different tissues independently of high or low tissue proliferation rates (Flores et al., 2008). Telomerase-deficient mice show a worsening of phenotypes with increasing mouse generations owing to inherited progressively shorter telomeres, with the later generations showing severe phenotypes and premature death at pre-reproductive ages (Lee et al., 1998; Herrera et al., 1999; García-Cao et al., 2002). This phenomenon first indicated genetic anticipation associated with telomerase deficiency. However, and in support of critical telomere shortening being a determinant of aging and longevity, increased TERT expression in the context of cancer-resistant transgenic mice was sufficient to delay aging and extend mouse longevity by 40% (Tomás-Loba et al., 2008). More recently, these findings have been translated into a potential therapeutic strategy by using adeno-associated vectors (AAVs) to transiently activate telomerase in adult tissues (Bernardes de Jesus et al., 2012; Bär et al., 2014). Telomeropathies or telomere syndromes develop when telomere attrition occurs prematurely as a consequence of germline mutations in genes coding for factors involved in telomere maintenance and repair (Table 1). Human telomeropathies are mainly associated with Hoyeraal-Hreidarsson syndrome (HHS), dyskeratosis congenita (DC), aplastic anemia, and pulmonary and liver disease and are nowadays considered more as a spectrum disorder than distinct diseases (see Clinical features of telomeropathies; Holohan et al., 2014; Stanley and Armanios, 2015). Although these diseases show a wide and complex range of clinical symptoms, all of them are characterized by presenting with critically short telomeres. The age of onset and the severity of clinical manifestations vary among individuals. These syndromes are characterized by premature loss of the regenerative capacity of tissues, affecting tissues with both high and low proliferation rates (Armanios and Blackburn, 2012; Holohan et al., 2014). As in mice, disease anticipation is also found in human families with telomere syndromes, with the mutation generally first manifesting in adults with pulmonary fibrosis (PF), and the more severe phenotypes appearing in pediatric populations (immunodeficiency) and young adults (aplastic anemia) from the next generations (Armanios and Blackburn, 2012).
Table 1. Genes known to cause telomeropathies when defective, as well as the telomere-related processes and protein complexes in which they are involved.
| Process/protein complex | Genes | Telomeropathies |
|---|---|---|
| Telomerase core components | TERC | DC, IPF, aplastic anemia, liver disease |
| TERT | DC, HHS, IPF, aplastic anemia, liver disease | |
| Telomerase biogenesis | DKC1 | DC, HHS, IPF, aplastic anemia |
| NOP10 | DC, IPF, aplastic anemia | |
| NHP2 | DC, IPF, aplastic anemia | |
| Telomerase trafficking | TCBA1 | DC |
| Shelterin components | TIN2 | DC, HHS |
| TPP1 | DC, HHS, aplastic anemia | |
| Telomeric DNA synthesis | RTEL1 | HHS, IPF |
| CTC1 | DC | |
| TERC RNA processing | PARN | DC, IPF |
| NAF1 | IPF |
The diseases found associated with the mutated genes are indicated (Calado et al., 2009a; Holohan et al., 2014; Glousker et al., 2015; Stanley and Armanios, 2015; Stanley et al., 2016).
Clinical features of telomeropathies
Aplastic anemia: Aplastic anemia is a BM failure state characterized by low blood counts and an insufficiency of hematopoietic cells in the BM (Fogarty et al., 2003).
Idiopathic pulmonary fibrosis (IPF): IPF is characterized by cough, dyspnea, impaired gas exchange, and reduced lung volume. Pathologically, there is patchy fibrosis of the lungs and interstitial inflammation, normal lung alternating with fibrosis, inflammation, and collagen deposition (Armanios et al., 2007).
Liver disease: Liver disease associated with telomere shortening consists of mainly fibrosis with inflammation and nodular regenerative hyperplasia, a leading cause of noncirrhotic portal hypertension (Calado et al., 2009a).
Dyskeratosis congenita (DC): DC is classically diagnosed by the presence of the mucocutaneous triad of nail dysplasia, skin pigmentation, and oral leukoplakia or the presence of one feature of the triad in combination with BM failure and two other DC-associated findings. Patients with DC are at very high risk of BM failure, PF, liver fibrosis, stenosis, premature hair graying, leukemia, and squamous cell cancer of the head, neck, or anogenital regions (Ballew and Savage, 2013).
Hoyeraal-Hreidarsson syndrome (HHS): HHS is a multisystem genetic disorder characterized by very short telomeres (less than first percentile for age) and is considered a clinically severe variant of DC. Patients with HHS present in early childhood with cerebellar hypoplasia, microcephaly, immunodeficiency, BM failure, and intrauterine growth retardation. The DC-associated mucocutaneous triad is also a trait of HHS (Glousker et al., 2015).
In addition to telomere-mediated replicative senescence, telomere length can have an impact on human diseases by regulating gene expression through telomere position effects (TPEs). TPEs involve the spreading of telomeric heterochromatin to silence nearby genes. In human cells, it has been shown that gene expression is affected by telomere length (Stadler et al., 2013; Robin et al., 2014). In particular, genes located near the telomere at chromosome 4q are progressively up-regulated with decreasing telomere length, and this occurs long before terminal telomere shortening would induce replicative senescence (Stadler et al., 2013). Interestingly, among the genes analyzed, the effect of TPE is most prominent with DUX4, the one located nearest to the 4q telomere. Expression of DUX4, encoding a toxic double-homeobox protein, has been linked to facioscapulohumeral muscular dystrophy, a disease presenting with progressive atrophy and weakness of the facial, scapular, and upper arm muscles (Stadler et al., 2013). This disease has highly variable clinical manifestation, and delayed onset that can be explained by age-associated telomere shortening (Stadler et al., 2013). Thus, facioscapulohumeral muscular dystrophy constitutes the first human disease to demonstrate a potential contribution of TPE to the age-associated diseases.
Mouse models for PF, aplastic anemia, DC, and HHS
The study of mouse models genetically deficient in telomerase and telomeric proteins has been crucial to understanding the role of telomere biology in human telomeropathies. In particular, the telomerase knockout, Pot1 knockout, and Trf1 conditional knockout mouse models have recently served as proofs-of-principle of the causal role of DNA damage stemming from dysfunctional telomeres in DC, idiopathic PF (IPF), and aplastic anemia (see text box; Hockemeyer et al., 2008; He et al., 2009; Martínez et al., 2009b; Beier et al., 2012). Recently, mutant mice expressing p53 lacking the C-terminal domain, a protein that is not directly involved in telomere maintenance, have been shown to be remarkable models for human telomeropathies, in particular for HHS (see text box; Simeonova et al., 2013).
Aplastic anemia mouse models
The aplastic anemia phenotypes in mouse (see text box) are provoked either by partially depleting TRF1 in the BM stem cell and progenitor compartments (hematopoietic stem/progenitor cells [HSPCs]) or by transplanting irradiated wild-type mice with BM from late-generation telomerase-deficient Tert knockout mice presenting with short telomeres (Beier et al., 2012; Bär and Blasco, 2016). Partial depletion of the Trf1 gene in the BM causes a persistent DDR at telomeres that leads to a fast clearance of those HSPCs lacking TRF1. Compensatory hyperproliferation of the remaining HSPCs to regenerate the BM results in a concomitant rapid attrition of telomeres (Beier et al., 2012). The short telomeres in BM of both mouse models faithfully recapitulate human acquired and congenital forms of aplastic anemia characterized by peripheral pancytopenia and marrow hypoplasia.
PF mouse models
Among the telomere syndromes, IPF is the most common condition associated with telomere dysfunction in humans (see text box; Armanios and Blackburn, 2012). Mutations in telomere genes have been found in up to 25% of familial and 1–3% of sporadic IPF patients (Armanios et al., 2007; Alder et al., 2008; Cogan et al., 2015; Kannengiesser et al., 2015; Stuart et al., 2015; Stanley et al., 2016). Sporadic cases of IPF, not associated with mutations in telomere maintenance genes, also show shorter telomeres compared with age-matched controls, with 10% of the patients showing telomeres as short as those of the telomerase mutation carriers (Alder et al., 2008). In spite of PF and emphysema being the most frequent manifestations of telomere defects in humans, telomerase-deficient mice with critically short telomeres do not spontaneously develop pulmonary disease. Telomere dysfunction in telomerase-deficient mice induces senescence in alveolar progenitor cells and recapitulates the regenerative defects, inflammatory responses, and susceptibility to injury that are characteristic of human telomere-mediated lung disease, although no IPF was reported in these mouse models (Alder et al., 2015a). Exposure to cigarette smoke, which is known to accelerate PF onset in humans, induces emphysema but not PF in telomerase-deficient mice (Alder et al., 2011). These findings suggested that additional damages, or a telomere damage of higher severity, might be required for PF onset in mice. This was demonstrated in work from our laboratory, whereby we generated two independent mouse models that develop PF. In one of them, treatment of late-generation telomerase-deficient mice presenting short telomeres with low doses of bleomycin, which normally does not lead to PF in wild-type mice, results in full-blown progressive PF in telomerase-deficient mice (Povedano et al., 2015). In the second mouse model, severe PF was developed by induction of telomere dysfunction in the absence of telomere shortening specifically in the lungs, by genetically deleting the shelterin component Trf1 from epithelial type II alveolar cells (Povedano et al., 2015). In both models, we observed activation of the p53/p21 and p19ARF pathways, resulting in cell senescence and apoptosis. Both TERT and TRF1 deficiencies were previously shown to lead to a decreased ability of stem cells to regenerate tissues (Flores et al., 2005; Schneider et al., 2013). Thus, increased lung cell loss associated with severe telomere dysfunction triggers aberrant lung healing by fibroblasts, eventually leading to scar formation and PF. We showed that a DNA-damaged burden above a certain threshold, combined with defective stem cell regeneration ability, lead to the development of PF (Povedano et al., 2015). The TRF1-interacting shelterin protein TIN2 has also been found to be mutated in telomere syndromes (Savage et al., 2008; Alder et al., 2015b; Hoffman et al., 2016). Interestingly, a TIN2 mutation in its TRF1-interacting domain has recently been identified in a patient with sporadic PF who showed normal telomere length in the peripheral blood compartment, underlining the importance of telomere protection proteins and not only telomere length in human telomere syndromes (Hoffman et al., 2016).
DC and HHS mouse models
DC and HHS share a common etiology, are typically caused by germline mutations in telomere biology genes, and are characterized by very short telomeres (see text box; Glousker et al., 2015). In mice, double deletion of Pot1b and Terc gives rise to some DC features such as hyperpigmentation and BM failure (Hockemeyer et al., 2008; He et al., 2009). HHS is considered a clinically severe variant of DC (Glousker et al., 2015). Telomeres in HHS patients are shorter than those of age-matched patients with classic DC (Alter et al., 2012). Although exceedingly short telomeres are considered the main cause of HHS, it is likely that other telomeric or nontelomeric defects also contribute to the pathology of HHS, perhaps distinguishing it from DC (Glousker et al., 2015). Indeed, to our knowledge, the only mouse mutant that faithfully models human HHS does not harbor mutations in any of the known telomere maintenance genes associated with these diseases, but rather a mutation in TP53 gene (Simeonova et al., 2013). p53Δ31/Δ31 mice, homozygous mutant mice expressing a truncated p53 protein lacking the C-terminal domain, suffer from aplastic anemia and PF as well as other phenotypic traits associated with DC and its severe variant, HHS (Simeonova et al., 2013). Thus, p53Δ31/Δ31 mice are born at the expected Mendelian ratio, but most die 14–43 d after birth because of aplastic anemia and heart failure, develop PF, and present cutaneous hyperpigmentation, nail dystrophy, and oral leukoplakia as in DC. In addition, some mice also present HHS features such as small size, hypogonadism, and cerebellar hypoplasia. The p53Δ31 protein shows increased p53 activity leading to down-regulation of genes involved in telomere metabolism such as Dkc1, Rtel1, Tin2, and Trf1, thereby explaining the appearance of phenotypes related to human telomere syndromes (Simeonova et al., 2013).
Therapeutic strategies in the treatment of telomere syndromes
Despite the growing understanding of the molecular defects associated with telomeropathies, the only current interventions to treat these diseases involve organ transplantation; i.e., BM, liver, and lung (Holohan et al., 2014; Stanley and Armanios, 2015). Although organ transplantation improves the physical condition of patients, it does not address the underlying cause of the symptoms, which is short telomeres. Patients diagnosed with interstitial lung disease presenting with short telomeres also showed subclinical BM and liver abnormalities, in some cases in the absence of clinical manifestations in peripheral blood count and liver dysfunction (George et al., 2015). These observations clearly favor a telomerase-activating therapy against other alternatives, such as organ transplant for the treatment of telomeropathies, because it also addresses the molecular defects of other affected organs. Indeed, the use of telomerase activators in the treatment of aging-associated conditions has raised commercial interest. Among telomerase chemical activators, TA-65, a small molecule derived from Astragalus membranaceus extracts, is the most widely studied. The telomerase activator TA-65 has been shown to lead to moderate telomere lengthening and improvement of some aging-related parameters in mice and humans, although no effect on longevity has been observed (Fig. 2; Bernardes de Jesus et al., 2011; Harley et al., 2013). In addition, androgen therapy has been applied as a treatment for aplastic anemia for many years without knowing its mechanism of action (Fig. 2; Shahidi and Diamond, 1961; Jaime-Pérez et al., 2011). It was subsequently reported that sex hormones activate TERT transcription (Calado et al., 2009b). Indeed, testosterone therapy in mice suffering from aplastic anemia was shown to up-regulate telomerase expression, rescue telomere attrition, and extend the life span of these mice (Fig. 2; Bär et al., 2015). In humans, administration of a synthetic androgen, danazol, to patients with telomeropathies resulted in telomere elongation in circulating leukocytes in association with hematologic improvement (Townsley et al., 2016). However, endogenous telomerase reactivation strategies are applicable only in those clinical cases not associated with mutations in telomere maintenance genes such as TERT or TERC. In this regard, therapeutic interventions based on telomerase-based gene therapy are currently being investigated in mouse models for their potential to improve health and extend life span, and as a treatment for short telomere syndromes (Bär and Blasco, 2016).
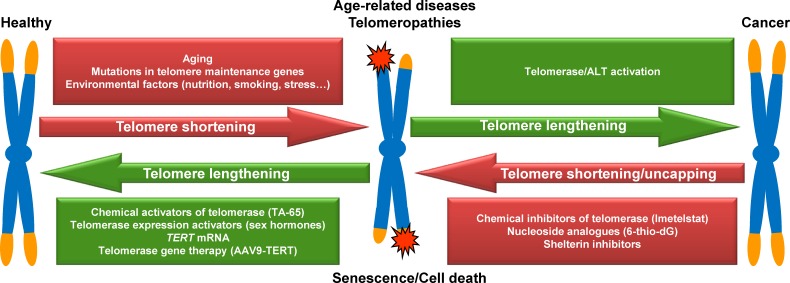
Figure 2.
Natural factors and therapeutic interventions affecting telomere-mediated diseases. Telomere shortening naturally occurs as a consequence of cell division throughout life, whose pace can be influenced by genetic and environmental factors. Shortened unprotected telomeres elicit a DDR that induces cellular senescence, impacting the regenerative capacity of tissues and giving rise to a whole range of age-associated diseases as well as the so-called telomeropathies, in which tissue degeneration occurs prematurely as a consequence of inherited defects in telomere maintenance. Several therapeutic interventions are being assessed to counteract telomere shortening: among others, chemical activators of telomerase (TA-65), activators of the telomerase reverse transcription (TERT) transcription (sex hormones), intracellular administration of TERT mRNA, and telomerase gene therapy (AAV9-TERT). Spontaneous mutations that activate telomerase expression or ALT result in telomere lengthening that, if occurring in genetically unstable checkpoint deficient cells, allows them to divide unlimitedly and eventually become cancer cells. Several therapeutic strategies based on chemical induction of telomere dysfunction have been assessed as anticancer therapies. Among others, we highlight the use of a chemical inhibitor of telomerase (imetelstat), a nucleoside analogue (6-thio-dG), and the use of molecules that inhibit shelterin components.
We have developed a therapeutic strategy by using AAVs to transiently activate telomerase in adult tissues (Fig. 2; Bernardes de Jesus et al., 2012; Bär et al., 2014). Treatment with Tert gene therapy using nonintegrative, replication-incompetent AAV9 vectors of adult mice was able to delay aging and increase longevity by decreasing age-related pathologies such as osteoporosis and glucose intolerance, as well as neuromuscular and cognitive decline. Furthermore, the onset of cancer was delayed in the TERT-treated mice (Bernardes de Jesus et al., 2012). Interestingly, AAV9-Tert delivery specifically to the heart was sufficient to significantly increase mouse survival and heart function upon myocardial infarction. AAV9-Tert after infarct treatment led to lower fibrotic scarring of the heart and increased cardiac myocyte proliferation concomitant with transcriptional changes suggestive of a regenerative signature (Bär et al., 2014). These findings support the notion that telomere shortening is at the origin of age-related diseases and that, by reverting this process with telomerase expression, it is possible to delay and more effectively treat age-associated pathologies, such as cardiovascular diseases. In addition, TERT gene therapy is particularly attractive for the clinical treatment of human telomere syndromes associated with telomerase mutations and short telomeres. Indeed, by using the mouse preclinical model of aplastic anemia provoked by short telomeres in the BM, we demonstrate that AVV9-Tert rescues aplastic anemia and mouse survival by inducing telomere lengthening in peripheral blood and BM cells as well as increasing blood counts (Bär et al., 2016). We are currently investigating the feasibility of AVV9-Tert therapy in the treatment of PF, with positive results so far (unpublished data). An alternative nonintegrative method to transiently express TERT based on TERT mRNA delivery into human cells in culture has been developed, although it has not yet been tested in vivo (Fig. 2; Ramunas et al., 2015).
Telomerase activation strategies should be taken with caution given their potential off-target effects and their ability to promote cancer (Bär and Blasco, 2016). Nevertheless, recent data from our group demonstrated that chimeric mice presenting hyperlong telomeres showed neither disadvantageous effects nor enhanced predisposition for cancer development compared with control chimeric mice presenting normal telomere length, indicating that long telomeres do not cause negative consequences to the organism (Varela et al., 2016). Indeed, in chimeric mice with hyperlong telomeres, cells in compartments with high rates of renewal retain longer telomeres and accumulate fewer short telomeres, less DNA damage burden, and lower levels of p53 with age (Varela et al., 2016). Thus, up to date experimental data in preclinical settings provide proof of concept for the viability of telomerase activation strategies to counteract telomere shortening and its associated consequences. In particular, the use of TERT gene therapy constitutes a promising candidate in the prevention and treatment of human telomeropathies mediated by TERT mutations and deserves further research efforts for clinical implementation. It should be noted that TERT gene therapy in the treatment of telomeropathies mediated by mutations in other genes associated with telomere metabolism (TERC, DKC1, NOP10, NHP2, TCAB1, TIN2, TPP1, RTEL1, CTC1, PARN, and NAF1) may, however, not be effective.
Telomeres and malignant transformation
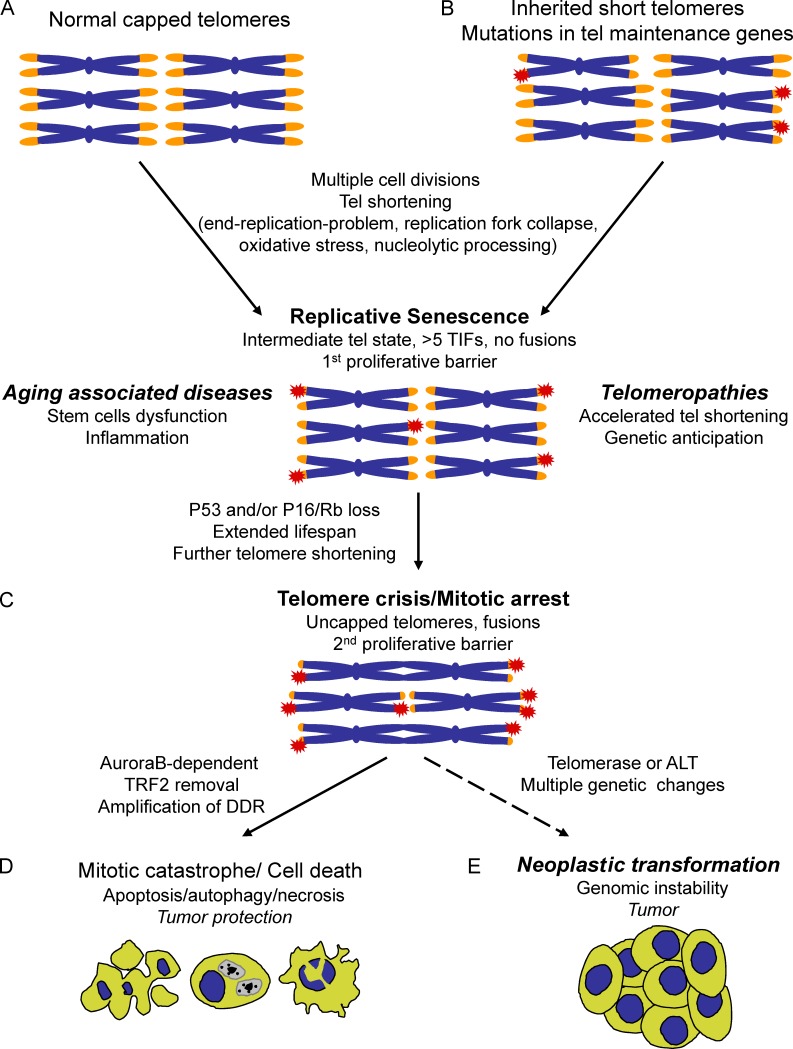
Telomere shortening throughout life is a natural consequence of cell division because of the end replication problem, replication fork collapse, oxidative stress, and nucleolytic processing. Critically shortened telomeres trigger replicative senescence that causes stem cell dysfunction and inflammation, in turn causing aging-associated diseases (Fig. 3 A; Jafri et al., 2016). In the situation of acquired germline mutations in genes coding for factors involved in telomere maintenance and repair, telomere shortening is accelerated, and replicative senescence occurs prematurely, giving rise to telomeropathies (Fig. 3 B; Holohan et al., 2014). In mammalian cells, replicative senescence can be bypassed by acquisition of loss-of-function mutations in tumor suppressor genes that permit further proliferation during a period of time that has been named the extended life span period (Fig. 3 C; Wright and Shay, 1992; Shay and Wright, 2005; Shay, 2016). Proliferation of premalignant cells during the extended life span period results in further telomere shortening. Eventually, cells enter the so-called crisis state, during which short telomeres contribute to genomic instability. Recent work has unraveled how dysfunctional telomeres govern cell fate during senescence, crisis, and transformation in human cells. Replicative senescence is triggered when at least five telomeres become dysfunctional, a critical damage threshold to elicit a DDR characterized by p53 activation (Fig. 3, A and B; Kaul et al., 2011). At that point, named the intermediate telomere state, telomeres are too short to be fully functional and are presumably unable to form the T-loop structure but retain sufficient protective shelterin to inhibit end-to-end fusions (Cesare et al., 2009, 2013; Kaul et al., 2011; Cesare and Karlseder, 2012). Upon loss of p53 and retinoblastoma protein (Rb), cells bypass senescence and continue to grow despite having more than five G1-phase intermediate state telomeres, experiencing further telomere shortening and entering the uncapped state, when they do not retain any protective properties and fuse (Fig. 3 C). A few fused telomeres is sufficient to lead to spindle assembly checkpoint–independent mitotic arrest, during which telomere dysfunction is amplified through Aurora B–dependent removal of TRF2, causing cell death during crisis, a second proliferative barrier (Fig. 3 D; Hayashi et al., 2012, 2015). Cell death in mitosis, also known as mitotic catastrophe (MC), occurs as a consequence of failure to complete mitosis. MC is driven by a complex and poorly understood signaling cascade that antecedes apoptosis, necrosis, senescence, or autophagy (Levine and Kroemer, 2008; Vitale et al., 2011). The molecular mechanisms that underlie MC, especially those that sense mitotic failure to engage the apoptotic, autophagy, or necrotic machinery, remain to be elucidated. It is tempting to speculate that structural and epigenetic changes experienced by multicentric chromosomes could serve as the signal for MC induction. Cell death during crisis thereby constitutes the second blockade against transformation in cells that bypassed the first barrier of senescence (Fig. 3 D). Reactivation of either telomerase activity or the alternative lengthening of telomeres (ALT) allows these premalignant cells to escape crisis, undergo unlimited divisions (immortalization), and evolve into a fully transformed cancerous state (Fig. 3 E; Pickett and Reddel, 2015; Shay, 2016). Indeed, ∼90% of human cancers present telomerase activity (Kim et al., 1994). To date, several mechanisms underlying reactivation of telomerase in cancer cells have been described: notably, mutations in TERT promoter, alterations in the alternative splicing of TERT pre-mRNA, gene amplification, epigenetic changes, alterations in regulatory factors, and /or disruption of TPE (Jafri et al., 2016). Whether telomerase reactivation is an early or late event during tumorigenesis is still a debated question. Recent data showing that TERT promoter mutations are found at early stages of carcinogenesis in most tumor types support the hypothesis that telomerase reactivation occurs at early time points during neoplastic transformation (Kinde et al., 2013; Allory et al., 2014; Hurst et al., 2014; Baerlocher et al., 2015; Chan et al., 2015; Huang et al., 2015; Tefferi et al., 2015; Jafri et al., 2016). However, it is still under debate whether telomerase or ALT reactivation is the driver or simply a facilitator of postcrisis cell growth. It is possible that other molecular events may be required to facilitate the escape from crisis. Studies on telomere dynamics and karyotype analyses in a broad range of human tumor types at early stages underpin telomere crisis as a key event driving genomic instability and clonal evolution during progression to malignancy (Shih et al., 2001; Meeker et al., 2004; Lin et al., 2010; Davoli and de Lange, 2011; Roger et al., 2013). Fused chromosomes in postcrisis cells lead to large-scale genomic rearrangements through breakage-fusion-bridges cycles (B-F-B), aneuploidy, tetraploidization, nonreciprocal translocations, chromothripsis, and kataegis, which promote acquisition of oncogenic mutations and malignant traits required for a fully malignant phenotype (Artandi and DePinho, 2010; Martínez and Blasco, 2010; Davoli and de Lange, 2012; Maciejowski et al., 2015).
Figure 3.
Impact of telomere shortening on aging-associated diseases, telomeropathies, and cancer. (A) Young, healthy cells contain long, fully protected telomeres that progressively shorten with increased cell divisions because of the end replication problem, replication fork collapse, nucleolytic processing, and oxidative stress. This progressive telomere shortening eventually leads to some critically short deprotected telomeres that have been termed intermediate-state telomeres. In this intermediate state of deprotection, telomeres retain enough shelterin to inhibit fusions but induce a DDR characterized by formation of the so-called telomere-induced focus (TIF). Replicative senescence is triggered when at least five telomeres become dysfunctional (more than five telomere-induced focuses), a critical damage threshold to elicit a DDR characterized by p53 activation. Telomere attrition in stem cell compartments impairs their tissue and self-renewal capacity and is considered to be one of the primary molecular causes of aging and the onset of aging-associated diseases. (B) Telomeropathies or telomere syndromes develop when telomere attrition occurs prematurely as a consequence of germline mutations in genes coding for factors involved in telomere maintenance and repair. Successive telomere shortening across generations exhibits genetic anticipation, whereby diseases show a progressively earlier age of onset and an aggravation of symptoms. (C) Senescence can be bypassed by acquisition of loss-of-function mutations in p53 and p16/Rb tumor suppressor genes that permit further proliferation during a period of time that has been named the extended life span period, during which cells experience further telomere shortening, eventually entering the uncapped state, when they do not retain any protective properties and fuse. (D) Fused telomeres lead to a mitotic arrest checkpoint during which telomere dysfunction is amplified by Aurora B–dependent TRF2 removal, causing cell death through apoptosis, necrosis, or autophagy in crisis, a second proliferative barrier that protects against tumor development. (E) Reactivation of either telomerase activity or ALT in some very rare crisis cells allows these premalignant cells to escape crisis and divide unlimitedly (immortalization). Fused chromosomes in postcrisis cells lead to large-scale genomic rearrangements that promote acquisition of oncogenic mutations and malignant traits required for a fully malignant phenotype, cancer.
Mouse models for telomere-driven cancer development
In vivo studies with transgenic mouse models of telomere dysfunction in combination with loss-of-function mutations in tumor suppressor genes strongly underscore the statement that telomere dysfunction leads to genomic rearrangements that are permissive for cancer initiation and progression (Table 2; Martínez and Blasco, 2011). Thus, mice doubly deficient for p53 and telomerase, the Terc−/− p53−/− mouse model, present a reduced tumor latency compared with single p53−/− mice, and Terc−/− p53+/− mice are prone to develop epithelial cancers typically observed in older humans (Chin et al., 1999). In addition, deficiency in the mismatch repair protein MSH2 abolishes the tumor-suppressor effects of short telomeres and prevents degenerative pathologies in Terc−/− Msh2−/− mice (Martinez et al., 2009a). Similarly, and despite the fact that constitutive deletion of either Trf1 or Pot1a results in embryonic lethality, tissue-specific conditional deletion of these genes in combination with p53-null mutation leads to tumorigenesis (Martínez et al., 2009b; Pinzaru et al., 2016). Thus, Trf1lox/lox K5-cre p53−/− mice lacking TRF1 in stratified epithelia spontaneously develop invasive and genetically unstable squamous cell carcinomas in the tail and ear skin (Martínez et al., 2009b). Depletion of POT1a and p53 in common lymphoid progenitor cells, Pot1alox/lox p53lox/lox hCD2-iCre mice, induces genetic instability, accelerates the onset, and increases the severity of T cell lymphomas (Table 2; Pinzaru et al., 2016). Similarly, simultaneous inactivation of Pot1a and p53 in endometrial epithelium, Pot1alox/lox p53lox/lox Sprr2f-Cre mice, results in invasive metastatic endometrial adenocarcinomas presenting nuclear atypia and tetraploid genomes (Akbay et al., 2013). In line with defects in shelterin components as drivers of genome instability, mice harboring a hypomorphic mutation in TPP1 in a p53−/− background show increased carcinomas (Else et al., 2009). Interestingly, complete TPP1 and p53 abrogation in stratified epithelia, the Tpp1lox/lox K5-cre p53−/− mouse model, does not lead to epithelial carcinomas, most likely because TPP1 is required to recruit telomerase to chromosome ends, mimicking the tumor-resistant phenotype of telomerase-deficient mice (Table 2; Tejera et al., 2010).
Table 2. Examples of mouse models underscoring telomere dysfunction as either a driving force in cancer development or as a cancer suppressor.
| Genotype | Cancer phenotype | Reference |
|---|---|---|
| Terc−/− p53−/− | Earlier onset lymphoma/sarcoma, epithelial carcinoma | Chin et al., 1999 |
| Terc−/− Msh2−/− | Lymphoma/carcinoma | Martinez et al., 2009a |
| Trf1lox/lox K5-cre p53−/− | Squamous cell carcinoma | Martínez et al., 2009b |
| Pot1alox/lox p53lox/lox hCD2-iCre | T cell lymphomas | Pinzaru et al., 2016 |
| Pot1alox/lox p53lox/lox Sprr2f-Cre | Endometrial adenocarcinomas | Akbay et al., 2013 |
| Tpp1Acd p53−/− | Carcinomas | Else et al., 2009 |
| Tpp1lox/lox K5-cre p53−/− | Cancer suppressor | Tejera et al., 2010 |
| Terc−/− Ink4a/Arf−/− | Delayed lymphoma/fibrosarcoma onset | Khoo et al., 2007 |
| Trf1lox/lox p53−/− K-RasLSLG12V | Growth impairment of lung carcinoma | García-Beccaria et al., 2015 |
The effects of telomere dysfunction in cancer-prone mouse models depend on the status of DNA damage surveillance mechanisms, acting oncogenes, and tissue-specific factors.
It should be noted that similar mutations in a different genetic context give rise to opposing outcomes resulting in cancer phenotype suppression. For example, late generation of mice doubly deficient for telomerase and the tumor suppressor INK4a/ARF, Terc−/− Ink4a/Arf−/− mice, show a cancer suppression phenotype and increase survival (Khoo et al., 2007). Trf1lox/lox p53−/− K-RasLSLG12V mice constitute an example of shelterin depletion as a cancer protective mechanism. Thus, simultaneous expression of K-RASG12V and TRF1 depletion upon Cre recombinase expression in the lungs impairs the growth of lung carcinomas and increases mouse survival independently of telomere length (Table 2; García-Beccaria et al., 2015). These studies clearly revealed that the neoplastic outcome of telomere dysfunction depends on the status of the DNA damage surveillance mechanisms, acting oncogenes, as well as on tissue-specific factors.
Role of shelterins in human cancer development and progression
Mutations in shelterin components have also been found in cancer. Several studies have reported up-regulation of the shelterin complex TRF1 and TRF2 in lung, gastric, breast, and renal cancers, suggesting that their overexpression might confer proliferative advantages to tumor cells (Miyachi et al., 2002; Saito et al., 2002; Nakanishi et al., 2003; Diehl et al., 2011; Pal et al., 2015). However, the role of TRF1 and TRF2 in cancer development and progression is still unknown. One possible explanation could be that high level of TRF2 in tumor cells decreases their ability to recruit and activate natural killer cells, thereby contributing to the bypass of innate immunosurveillance (Biroccio et al., 2013). Interestingly, TRF1 is highly expressed in pluripotent stem cells and adult stem cells (Boué et al., 2010; Varela et al., 2011; Schneider et al., 2013). TRF1 is essential for both induction and maintenance of pluripotency in a telomere length–independent manner (Schneider et al., 2013). TRF1 is a direct transcriptional target of the pluripotency factor OCT3/4, which binds the TRF1 promoter to up-regulate TRF1 expression, providing a mechanistic link between TRF1 and pluripotency (Schneider et al., 2013). Although TRF1 is clearly essential for IPSC generation and the maintenance of pluripotency, the mechanisms by which TRF1 impacts stemness and carcinogenesis have yet to be elucidated. It is tempting to speculate that TRF1 favors the proliferative capacity of stem and cancer cells.
Mutations in the shelterin component POT1 that disrupt proper telomere capping and result in telomere aberrations have been linked to familial melanoma, familial glioma, Li-Fraumeni–like syndrome, mantle cell lymphoma, parathyroid adenoma, and chronic lymphocytic leukemia (Newey et al., 2012; Ramsay et al., 2013; Bainbridge et al., 2014; Robles-Espinoza et al., 2014; Shi et al., 2014; Zhang et al., 2014; Calvete et al., 2015). Importantly, all the identified POT1 variants conferred a telomere-lengthening effect, suggesting that telomere elongation in combination with the telomere aberrations induced by these mutations favors tumor development. Introduction of POT1 mutations found in cutaneous T cell lymphoma in human and mouse cells showed that inhibition of POT1 results in defective telomere replication caused by impaired CST (CTC1-STN1-TEN1) function at telomeres and activates ATR-dependent DNA damage signaling (Pinzaru et al., 2016). Attenuation of the ATR kinase pathway allows cancer cells lacking POT1 to proliferate, suggesting that POT1-mediated tumorigenesis may be accompanied by concomitant compensatory mechanisms that down-regulate the ATR-dependent DDR (Pinzaru et al., 2016). It is intriguing that specific POT1 variants give rise to different cancer types. Future work warrants elucidation of the molecular mechanisms that determine the specificity of certain specific disease-associated mutations in shelterin components.
Mutations in TPP1 and RAP1 have also been found to be associated with familial melanoma (Aoude et al., 2014). In addition, families carrying TPP1 and RAP1 mutations were enriched with other cancer types, suggesting that these variants also cause predisposition to a broader spectrum of tumors than just melanoma. Although the telomeric phenotypes induced by these mutations have not been addressed, the observation that four of the five mutations found in TPP1 clustered in the POT1-binding domain suggests that POT1 recruitment to telomeres is disrupted, thereby causing similar phenotypes as observed in POT1 variants discussed earlier (Liu et al., 2004). More intriguing is the finding of RAP1 variants co-segregating with melanoma because RAP1 is dispensable for telomere function (Martinez et al., 2010; Sfeir et al., 2010). A possible explanation for the role of RAP1 in cancer could be either through its role in repressing homology-directed repair at telomeres (Martinez et al., 2010; Sfeir et al., 2010) or through its role in telomere maintenance in the absence of telomerase (Martínez et al., 2016).
Telomeres as anticancer targets
Given that most tumors (85–90%) present telomerase activity, whereas telomerase is absent in most normal tissues, or is strictly regulated in transient-amplifying stem cells, inhibition of telomerase is an attractive target for cancer therapy (Kim et al., 1994; Shay, 2016). Different approaches have been designed in the search for telomerase inhibitors: small-molecule inhibitors, antisense oligonucleotides, G-quadruplex stabilizers, immunotherapy, gene therapy using telomerase promoter-driven expression of a suicide gene, and chemicals that block telomerase biogenesis (Harley, 2008; Agrawal et al., 2012; Buseman et al., 2012; Jafri et al., 2016). Among all antitelomerase compounds developed, the oligonucleotide imetelstat (GRN163L) appears to be the most promising telomerase inhibitor and the one most extensively evaluated in clinical trials. Imetelstat sequence binds to a complementary oligonucleotide region of hTR at the active site of telomerase holoenzyme, leading to complete inhibition of enzyme activity (Fig. 2; Jafri et al., 2016). However, inhibition of telomere maintenance by targeting telomerase in cancer has showed effectiveness in only some myeloid tumors but has largely failed in solid tumors (Baerlocher et al., 2015; Tefferi et al., 2015; Jafri et al., 2016). The reasons underlying the lack of success are likely that therapeutic strategies based on telomerase inhibition to treat cancer will be effective only when telomeres shorten below a minimum length, implying a long lag period before cell death. Indeed, telomerase activity is dispensable for transformation of cells with long telomeres (Seger et al., 2002), and studies with telomerase inhibitors indicate that they are effective preferentially in cells with short telomeres (Wang et al., 2004; Buseman et al., 2012). In line with this idea, telomerase abrogation in the context of cancer-prone mouse models, including the K-Ras+/G12D lung tumorigenesis mouse model, showed antitumorigenic activity only after several mouse generations in the absence of telomerase when telomeres reached a critically short length (Chin et al., 1999; Greenberg et al., 1999; González-Suárez et al., 2000; Perera et al., 2008). Moreover, these antitumorigenic effects of short telomeres owing to telomerase deficiency are abrogated in the absence of p53 (Chin et al., 1999).
Alternative therapeutic approaches that target telomeres in a telomere length–independent manner are starting to emerge. In contrast to telomerase inhibition, telomere uncapping has been shown to cause rapid induction of cell death and/or senescence in a manner that is independent of telomerase activity and telomere length (Karlseder et al., 1999; Martínez et al., 2009b). Thus, given that telomere dysfunction can be achieved independently of telomere length, telomere uncapping strategies emerge as a more universal way to rapidly impair the growth of dividing cells. One of these alternative approaches consists of a telomere-targeted telomerase-dependent potential anticancer therapy that uses a nucleoside analogue, 6-thio-2′-deoxyguanosine (6-thio-dG). 6-Thio-dG is recognized by telomerase and incorporated into de novo synthesized telomeres, leading to telomere dysfunction solely in telomerase-expressing cells (Fig. 2). Treatment with 6-thio-dG leads to rapid cell death in most of the cancer cell lines assayed and to telomere dysfunction in in vivo xenograft models (Mender et al., 2015). Targeting telomerase recruitment to telomeres has also been proposed as a potential anticancer treatment (Nakanishi et al., 2003).
We have recently developed a novel telomerase-independent and telomere length–independent strategy to induce telomere dysfunction by targeting TRF1 (Fig. 2; García-Beccaria et al., 2015). Genetic Trf1 deletion impaired the growth of p53-null KRas(G12V)-induced lung carcinomas and increased mouse survival independently of telomere length. Chemical inhibition of TRF1 binding to telomeres by small molecules blocked the growth of already established lung carcinomas by inducing a rapid DDR and without affecting mouse survival or tissue function, supporting induction of acute telomere uncapping as a promising therapeutic target for lung cancer and very likely for many other cancer types (García-Beccaria et al., 2015). Chemical inhibition of TRF2 dimerization has also been achieved by targeted peptide synthesis that directly binds to the TRFH dimerization domain of TRF2 (Di Maro et al., 2014). Treatment of HeLa cells with TRF2-binding chemotypes did not affect TRF2 telomeric localization but induced rapid DDR activation, end-to-end fusions, and cell death indicative of telomere dysfunction (Di Maro et al., 2014). Although further clinical research is needed to ultimately address the efficacy of telomere-uncapping chemical inhibition in human cancer, these strategies provide novel opportunities for the development of anticancer agents.
Outstanding questions in telomere-related diseases and cancer
Although telomere biology has been extensively studied, our knowledge of the implications of telomeres and telomere proteins in human disease has considerably improved in recent years. Current research efforts focus on how our knowledge of telomere biology and its connection with human disease can be translated into the clinic to improve human health. Although some telomere-based therapies have already reached clinical trials, the path is still long. The fact that telomere dysfunction may have different and even opposing outcomes in aging and cancer makes the goal of developing telomere-based anti-aging and anticancer therapies a delicate challenge that requires a highly controllable technology. Results obtained in mouse models with telomerase gene therapy as a treatment for aging-associated diseases and telomere syndromes, as well as shelterin chemical inhibition as anticancer therapy treatment, constitute promising opportunities for further clinical development. However, additional studies are needed to determine the undesired long-term effects associated with exogenous reexpression of telomerase and shelterin inhibition.
The molecular mechanisms underlying the specificity of certain specific disease-associated mutations/variants in shelterins are yet an open field of research. For example, specific POT1 variants give rise to chronic lymphocytic leukemia, whereas other amino acid substitutions predispose to familial melanoma, cardiac angiosarcomas, or gliomas. Several shelterin mutations associated with different tumor types have recently been found, and presumably many more shelterin mutations are yet to be identified in human cancer. These observations further support the use of shelterins as cancer targets and raise the question of the potential translational applications of shelterin gene therapy as preventive treatment in mutation carriers.
In summary, the works discussed in this review provide proof of concept for the feasibility of telomere-targeted therapeutic approaches for the prevention and treatment of telomere dysfunction–mediated diseases in animal models and pave the way for their development and implementation in the clinic.
Acknowledgments
Research in the Blasco laboratory is funded by the Spanish Ministry of Economy and Competitiveness and Fondo Europeo de Desarrollo Regional project RETOS (grant SAF2013-45111-R), the European Research Council project TEL STEM CELL (grant ERC-2008-AdG/232854), and Fundación Botín.
The authors declare no competing financial interests.
Footnotes
Abbreviations used:
- 6-thio-dG
- 6-thio-2′-deoxyguanosine
- AAV
- adeno-associated vector
- ALT
- alternative lengthening of telomeres
- BM
- bone marrow
- DC
- dyskeratosis congenita
- DDR
- DNA damage response
- HHS
- Hoyeraal-Hreidarsson syndrome
- HSPC
- hematopoietic stem/progenitor cell
- IPF
- idiopathic PF
- MC
- mitotic catastrophe
- PF
- pulmonary fibrosis
- TPE
- telomere position effect
References
- Agrawal A., Dang S., and Gabrani R.. 2012. Recent patents on anti-telomerase cancer therapy. Recent Patents Anticancer. Drug Discov. 7:102–117. 10.2174/157489212798357958 [DOI] [PubMed] [Google Scholar]
- Akbay E.A., Peña C.G., Ruder D., Michel J.A., Nakada Y., Pathak S., Multani A.S., Chang S., and Castrillon D.H.. 2013. Cooperation between p53 and the telomere-protecting shelterin component Pot1a in endometrial carcinogenesis. Oncogene. 32:2211–2219. 10.1038/onc.2012.232 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alder J.K., Chen J.J., Lancaster L., Danoff S., Su S.C., Cogan J.D., Vulto I., Xie M., Qi X., Tuder R.M., et al. 2008. Short telomeres are a risk factor for idiopathic pulmonary fibrosis. Proc. Natl. Acad. Sci. USA. 105:13051–13056. 10.1073/pnas.0804280105 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alder J.K., Guo N., Kembou F., Parry E.M., Anderson C.J., Gorgy A.I., Walsh M.F., Sussan T., Biswal S., Mitzner W., et al. 2011. Telomere length is a determinant of emphysema susceptibility. Am. J. Respir. Crit. Care Med. 184:904–912. 10.1164/rccm.201103-0520OC [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alder J.K., Barkauskas C.E., Limjunyawong N., Stanley S.E., Kembou F., Tuder R.M., Hogan B.L., Mitzner W., and Armanios M.. 2015a Telomere dysfunction causes alveolar stem cell failure. Proc. Natl. Acad. Sci. USA. 112:5099–5104. 10.1073/pnas.1504780112 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alder J.K., Stanley S.E., Wagner C.L., Hamilton M., Hanumanthu V.S., and Armanios M.. 2015b Exome sequencing identifies mutant TINF2 in a family with pulmonary fibrosis. Chest. 147:1361–1368. 10.1378/chest.14-1947 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Allory Y., Beukers W., Sagrera A., Flández M., Marqués M., Márquez M., van der Keur K.A., Dyrskjot L., Lurkin I., Vermeij M., et al. 2014. Telomerase reverse transcriptase promoter mutations in bladder cancer: high frequency across stages, detection in urine, and lack of association with outcome. Eur. Urol. 65:360–366. 10.1016/j.eururo.2013.08.052 [DOI] [PubMed] [Google Scholar]
- Alter B.P., Rosenberg P.S., Giri N., Baerlocher G.M., Lansdorp P.M., and Savage S.A.. 2012. Telomere length is associated with disease severity and declines with age in dyskeratosis congenita. Haematologica. 97:353–359. 10.3324/haematol.2011.055269 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aoude L.G., Pritchard A.L., Robles-Espinoza C.D., Wadt K., Harland M., Choi J., Gartside M., Quesada V., Johansson P., Palmer J.M., et al. 2014. Nonsense mutations in the shelterin complex genes ACD and TERF2IP in familial melanoma. J. Natl. Cancer Inst. 107:dju408 10.1093/jnci/dju408 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Armanios M., and Blackburn E.H.. 2012. The telomere syndromes. Nat. Rev. Genet. 13:693–704. 10.1038/nrg3246 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Armanios M.Y., Chen J.J., Cogan J.D., Alder J.K., Ingersoll R.G., Markin C., Lawson W.E., Xie M., Vulto I., Phillips J.A. III, et al. 2007. Telomerase mutations in families with idiopathic pulmonary fibrosis. N. Engl. J. Med. 356:1317–1326. 10.1056/NEJMoa066157 [DOI] [PubMed] [Google Scholar]
- Artandi S.E., and DePinho R.A.. 2010. Telomeres and telomerase in cancer. Carcinogenesis. 31:9–18. 10.1093/carcin/bgp268 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baerlocher G.M., Oppliger Leibundgut E., Ottmann O.G., Spitzer G., Odenike O., McDevitt M.A., Röth A., Daskalakis M., Burington B., Stuart M., and Snyder D.S.. 2015. Telomerase inhibitor imetelstat in patients with essential thrombocythemia. N. Engl. J. Med. 373:920–928. 10.1056/NEJMoa1503479 [DOI] [PubMed] [Google Scholar]
- Bainbridge M.N., Armstrong G.N., Gramatges M.M., Bertuch A.A., Jhangiani S.N., Doddapaneni H., Lewis L., Tombrello J., Tsavachidis S., Liu Y., et al. Gliogene Consortium . 2014. Germline mutations in shelterin complex genes are associated with familial glioma. J. Natl. Cancer Inst. 107:dju384 10.1093/jnci/dju384 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ballew B.J., and Savage S.A.. 2013. Updates on the biology and management of dyskeratosis congenita and related telomere biology disorders. Expert Rev. Hematol. 6:327–337. 10.1586/ehm.13.23 [DOI] [PubMed] [Google Scholar]
- Bär C., and Blasco M.A.. 2016. Telomeres and telomerase as therapeutic targets to prevent and treat age-related diseases. F1000 Res . 5:89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bär C., Bernardes de Jesus B., Serrano R., Tejera A., Ayuso E., Jimenez V., Formentini I., Bobadilla M., Mizrahi J., de Martino A., et al. 2014. Telomerase expression confers cardioprotection in the adult mouse heart after acute myocardial infarction. Nat. Commun. 5:5863 10.1038/ncomms6863 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bär C., Huber N., Beier F., and Blasco M.A.. 2015. Therapeutic effect of androgen therapy in a mouse model of aplastic anemia produced by short telomeres. Haematologica. 100:1267–1274. 10.3324/haematol.2015.129239 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bär C., Povedano J.M., Serrano R., Benitez-Buelga C., Popkes M., Formentini I., Bobadilla M., Bosch F., and Blasco M.A.. 2016. Telomerase gene therapy rescues telomere length, bone marrow aplasia, and survival in mice with aplastic anemia. Blood. 127:1770–1779. 10.1182/blood-2015-08-667485 [DOI] [PubMed] [Google Scholar]
- Beier F., Foronda M., Martinez P., and Blasco M.A.. 2012. Conditional TRF1 knockout in the hematopoietic compartment leads to bone marrow failure and recapitulates clinical features of dyskeratosis congenita. Blood. 120:2990–3000. 10.1182/blood-2012-03-418038 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bernardes de Jesus B., Schneeberger K., Vera E., Tejera A., Harley C.B., and Blasco M.A.. 2011. The telomerase activator TA-65 elongates short telomeres and increases health span of adult/old mice without increasing cancer incidence. Aging Cell. 10:604–621. 10.1111/j.1474-9726.2011.00700.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bernardes de Jesus B., Vera E., Schneeberger K., Tejera A.M., Ayuso E., Bosch F., and Blasco M.A.. 2012. Telomerase gene therapy in adult and old mice delays aging and increases longevity without increasing cancer. EMBO Mol. Med. 4:691–704. 10.1002/emmm.201200245 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Biroccio A., Cherfils-Vicini J., Augereau A., Pinte S., Bauwens S., Ye J., Simonet T., Horard B., Jamet K., Cervera L., et al. 2013. TRF2 inhibits a cell-extrinsic pathway through which natural killer cells eliminate cancer cells. Nat. Cell Biol. 15:818–828. 10.1038/ncb2774 [DOI] [PubMed] [Google Scholar]
- Blasco M.A. 2005. Telomeres and human disease: Ageing, cancer and beyond. Nat. Rev. Genet. 6:611–622. 10.1038/nrg1656 [DOI] [PubMed] [Google Scholar]
- Blasco M.A., Lee H.W., Hande M.P., Samper E., Lansdorp P.M., DePinho R.A., and Greider C.W.. 1997. Telomere shortening and tumor formation by mouse cells lacking telomerase RNA. Cell. 91:25–34. 10.1016/S0092-8674(01)80006-4 [DOI] [PubMed] [Google Scholar]
- Boué S., Paramonov I., Barrero M.J., and Izpisúa Belmonte J.C.. 2010. Analysis of human and mouse reprogramming of somatic cells to induced pluripotent stem cells. What is in the plate? PLoS One. 5:e12664 10.1371/journal.pone.0012664 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buseman C.M., Wright W.E., and Shay J.W.. 2012. Is telomerase a viable target in cancer? Mutat. Res. 730:90–97. 10.1016/j.mrfmmm.2011.07.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Calado R.T., Regal J.A., Kleiner D.E., Schrump D.S., Peterson N.R., Pons V., Chanock S.J., Lansdorp P.M., and Young N.S.. 2009a A spectrum of severe familial liver disorders associate with telomerase mutations. PLoS One. 4:e7926 10.1371/journal.pone.0007926 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Calado R.T., Yewdell W.T., Wilkerson K.L., Regal J.A., Kajigaya S., Stratakis C.A., and Young N.S.. 2009b Sex hormones, acting on the TERT gene, increase telomerase activity in human primary hematopoietic cells. Blood. 114:2236–2243. 10.1182/blood-2008-09-178871 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Calvete O., Martinez P., Garcia-Pavia P., Benitez-Buelga C., Paumard-Hernández B., Fernandez V., Dominguez F., Salas C., Romero-Laorden N., Garcia-Donas J., et al. 2015. A mutation in the POT1 gene is responsible for cardiac angiosarcoma in TP53-negative Li-Fraumeni-like families. Nat. Commun. 6:8383 10.1038/ncomms9383 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cawthon R.M., Smith K.R., O’Brien E., Sivatchenko A., and Kerber R.A.. 2003. Association between telomere length in blood and mortality in people aged 60 years or older. Lancet. 361:393–395. 10.1016/S0140-6736(03)12384-7 [DOI] [PubMed] [Google Scholar]
- Cesare A.J., and Karlseder J.. 2012. A three-state model of telomere control over human proliferative boundaries. Curr. Opin. Cell Biol. 24:731–738. 10.1016/j.ceb.2012.08.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cesare A.J., Kaul Z., Cohen S.B., Napier C.E., Pickett H.A., Neumann A.A., and Reddel R.R.. 2009. Spontaneous occurrence of telomeric DNA damage response in the absence of chromosome fusions. Nat. Struct. Mol. Biol. 16:1244–1251. 10.1038/nsmb.1725 [DOI] [PubMed] [Google Scholar]
- Cesare A.J., Hayashi M.T., Crabbe L., and Karlseder J.. 2013. The telomere deprotection response is functionally distinct from the genomic DNA damage response. Mol. Cell. 51:141–155. 10.1016/j.molcel.2013.06.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chan A.K., Yao Y., Zhang Z., Chung N.Y., Liu J.S., Li K.K., Shi Z., Chan D.T., Poon W.S., Zhou L., and Ng H.K.. 2015. TERT promoter mutations contribute to subset prognostication of lower-grade gliomas. Mod. Pathol. 28:177–186. 10.1038/modpathol.2014.94 [DOI] [PubMed] [Google Scholar]
- Chin L., Artandi S.E., Shen Q., Tam A., Lee S.L., Gottlieb G.J., Greider C.W., and DePinho R.A.. 1999. p53 deficiency rescues the adverse effects of telomere loss and cooperates with telomere dysfunction to accelerate carcinogenesis. Cell. 97:527–538. 10.1016/S0092-8674(00)80762-X [DOI] [PubMed] [Google Scholar]
- Cogan J.D., Kropski J.A., Zhao M., Mitchell D.B., Rives L., Markin C., Garnett E.T., Montgomery K.H., Mason W.R., McKean D.F., et al. 2015. Rare variants in RTEL1 are associated with familial interstitial pneumonia. Am. J. Respir. Crit. Care Med. 191:646–655. 10.1164/rccm.201408-1510OC [DOI] [PMC free article] [PubMed] [Google Scholar]
- Collado M., Blasco M.A., and Serrano M.. 2007. Cellular senescence in cancer and aging. Cell. 130:223–233. 10.1016/j.cell.2007.07.003 [DOI] [PubMed] [Google Scholar]
- Davoli T., and de Lange T.. 2011. The causes and consequences of polyploidy in normal development and cancer. Annu. Rev. Cell Dev. Biol. 27:585–610. 10.1146/annurev-cellbio-092910-154234 [DOI] [PubMed] [Google Scholar]
- Davoli T., and de Lange T.. 2012. Telomere-driven tetraploidization occurs in human cells undergoing crisis and promotes transformation of mouse cells. Cancer Cell. 21:765–776. 10.1016/j.ccr.2012.03.044 [DOI] [PMC free article] [PubMed] [Google Scholar]
- de Lange T. 2005. Shelterin: The protein complex that shapes and safeguards human telomeres. Genes Dev. 19:2100–2110. 10.1101/gad.1346005 [DOI] [PubMed] [Google Scholar]
- Diehl M.C., Idowu M.O., Kimmelshue K.N., York T.P., Jackson-Cook C.K., Turner K.C., Holt S.E., and Elmore L.W.. 2011. Elevated TRF2 in advanced breast cancers with short telomeres. Breast Cancer Res. Treat. 127:623–630. 10.1007/s10549-010-0988-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Di Maro S., Zizza P., Salvati E., De Luca V., Capasso C., Fotticchia I., Pagano B., Marinelli L., Gilson E., Novellino E., et al. 2014. Shading the TRF2 recruiting function: A new horizon in drug development. J. Am. Chem. Soc. 136:16708–16711. 10.1021/ja5080773 [DOI] [PubMed] [Google Scholar]
- Doksani Y., Wu J.Y., de Lange T., and Zhuang X.. 2013. Super-resolution fluorescence imaging of telomeres reveals TRF2-dependent T-loop formation. Cell. 155:345–356. 10.1016/j.cell.2013.09.048 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Else T., Trovato A., Kim A.C., Wu Y., Ferguson D.O., Kuick R.D., Lucas P.C., and Hammer G.D.. 2009. Genetic p53 deficiency partially rescues the adrenocortical dysplasia phenotype at the expense of increased tumorigenesis. Cancer Cell. 15:465–476. 10.1016/j.ccr.2009.04.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ferrón S., Mira H., Franco S., Cano-Jaimez M., Bellmunt E., Ramírez C., Fariñas I., and Blasco M.A.. 2004. Telomere shortening and chromosomal instability abrogates proliferation of adult but not embryonic neural stem cells. Development. 131:4059–4070. 10.1242/dev.01215 [DOI] [PubMed] [Google Scholar]
- Flores I., Cayuela M.L., and Blasco M.A.. 2005. Effects of telomerase and telomere length on epidermal stem cell behavior. Science. 309:1253–1256. 10.1126/science.1115025 [DOI] [PubMed] [Google Scholar]
- Flores I., Canela A., Vera E., Tejera A., Cotsarelis G., and Blasco M.A.. 2008. The longest telomeres: A general signature of adult stem cell compartments. Genes Dev. 22:654–667. 10.1101/gad.451008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fogarty P.F., Yamaguchi H., Wiestner A., Baerlocher G.M., Sloand E., Zeng W.S.. Read E.J., Lansdorp P.M., and Young N.S.. 2003. Late presentation of dyskeratosis congenita as apparently acquired aplastic anaemia due to mutations in telomerase RNA. Lancet. 362:1628–1630 [DOI] [PubMed] [Google Scholar]
- Fumagalli M., Rossiello F., Clerici M., Barozzi S., Cittaro D., Kaplunov J.M., Bucci G., Dobreva M., Matti V., Beausejour C.M., et al. 2012. Telomeric DNA damage is irreparable and causes persistent DNA-damage-response activation. Nat. Cell Biol. 14:355–365. 10.1038/ncb2466 [DOI] [PMC free article] [PubMed] [Google Scholar]
- García-Beccaria M., Martínez P., Méndez-Pertuz M., Martínez S., Blanco-Aparicio C., Cañamero M., Mulero F., Ambrogio C., Flores J.M., Megias D., et al. 2015. Therapeutic inhibition of TRF1 impairs the growth of p53-deficient K-RasG12V-induced lung cancer by induction of telomeric DNA damage. EMBO Mol. Med. 7:930–949. 10.15252/emmm.201404497 [DOI] [PMC free article] [PubMed] [Google Scholar]
- García-Cao I., García-Cao M., Martín-Caballero J., Criado L.M., Klatt P., Flores J.M., Weill J.C., Blasco M.A., and Serrano M.. 2002. “Super p53” mice exhibit enhanced DNA damage response, are tumor resistant and age normally. EMBO J. 21:6225–6235. 10.1093/emboj/cdf595 [DOI] [PMC free article] [PubMed] [Google Scholar]
- George G., Rosas I.O., Cui Y., McKane C., Hunninghake G.M., Camp P.C., Raby B.A., Goldberg H.J., and El-Chemaly S.. 2015. Short telomeres, telomeropathy, and subclinical extrapulmonary organ damage in patients with interstitial lung disease. Chest. 147:1549–1557. 10.1378/chest.14-0631 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Glousker G., Touzot F., Revy P., Tzfati Y., and Savage S.A.. 2015. Unraveling the pathogenesis of Hoyeraal-Hreidarsson syndrome, a complex telomere biology disorder. Br. J. Haematol. 170:457–471. 10.1111/bjh.13442 [DOI] [PMC free article] [PubMed] [Google Scholar]
- González-Suárez E., Samper E., Flores J.M., and Blasco M.A.. 2000. Telomerase-deficient mice with short telomeres are resistant to skin tumorigenesis. Nat. Genet. 26:114–117. 10.1038/79089 [DOI] [PubMed] [Google Scholar]
- Greenberg R.A., Chin L., Femino A., Lee K.H., Gottlieb G.J., Singer R.H., Greider C.W., and DePinho R.A.. 1999. Short dysfunctional telomeres impair tumorigenesis in the INK4a(delta2/3) cancer-prone mouse. Cell. 97:515–525. 10.1016/S0092-8674(00)80761-8 [DOI] [PubMed] [Google Scholar]
- Greider C.W., and Blackburn E.H.. 1985. Identification of a specific telomere terminal transferase activity in Tetrahymena extracts. Cell. 43:405–413. 10.1016/0092-8674(85)90170-9 [DOI] [PubMed] [Google Scholar]
- Griffith J.D., Comeau L., Rosenfield S., Stansel R.M., Bianchi A., Moss H., and de Lange T.. 1999. Mammalian telomeres end in a large duplex loop. Cell. 97:503–514. 10.1016/S0092-8674(00)80760-6 [DOI] [PubMed] [Google Scholar]
- Harley C.B. 2008. Telomerase and cancer therapeutics. Nat. Rev. Cancer. 8:167–179. 10.1038/nrc2275 [DOI] [PubMed] [Google Scholar]
- Harley C.B., Futcher A.B., and Greider C.W.. 1990. Telomeres shorten during ageing of human fibroblasts. Nature. 345:458–460. 10.1038/345458a0 [DOI] [PubMed] [Google Scholar]
- Harley C.B., Liu W., Flom P.L., and Raffaele J.M.. 2013. A natural product telomerase activator as part of a health maintenance program: Metabolic and cardiovascular response. Rejuvenation Res. 16:386–395. 10.1089/rej.2013.1430 [DOI] [PubMed] [Google Scholar]
- Hastie N.D., Dempster M., Dunlop M.G., Thompson A.M., Green D.K., and Allshire R.C.. 1990. Telomere reduction in human colorectal carcinoma and with ageing. Nature. 346:866–868. 10.1038/346866a0 [DOI] [PubMed] [Google Scholar]
- Hayashi M.T., Cesare A.J., Fitzpatrick J.A., Lazzerini-Denchi E., and Karlseder J.. 2012. A telomere-dependent DNA damage checkpoint induced by prolonged mitotic arrest. Nat. Struct. Mol. Biol. 19:387–394. 10.1038/nsmb.2245 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hayashi M.T., Cesare A.J., Rivera T., and Karlseder J.. 2015. Cell death during crisis is mediated by mitotic telomere deprotection. Nature. 522:492–496. 10.1038/nature14513 [DOI] [PMC free article] [PubMed] [Google Scholar]
- He H., Wang Y., Guo X., Ramchandani S., Ma J., Shen M.F., Garcia D.A., Deng Y., Multani A.S., You M.J., and Chang S.. 2009. Pot1b deletion and telomerase haploinsufficiency in mice initiate an ATR-dependent DNA damage response and elicit phenotypes resembling dyskeratosis congenita. Mol. Cell. Biol. 29:229–240. 10.1128/MCB.01400-08 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Herrera E., Samper E., Martín-Caballero J., Flores J.M., Lee H.W., and Blasco M.A.. 1999. Disease states associated with telomerase deficiency appear earlier in mice with short telomeres. EMBO J. 18:2950–2960. 10.1093/emboj/18.11.2950 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hockemeyer D., Palm W., Wang R.C., Couto S.S., and de Lange T.. 2008. Engineered telomere degradation models dyskeratosis congenita. Genes Dev. 22:1773–1785. 10.1101/gad.1679208 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hoffman T.W., van der Vis J.J., van Oosterhout M.F., van Es H.W., van Kessel D.A., Grutters J.C., and van Moorsel C.H.. 2016. TINF2 gene mutation in a patient with pulmonary fibrosis. Case Rep. Pulmonol. 2016:1310862 10.1155/2016/1310862 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holohan B., Wright W.E., and Shay J.W.. 2014. Telomeropathies: An emerging spectrum disorder. J. Cell Biol. 205:289–299. 10.1083/jcb.201401012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huang D.S., Wang Z., He X.J., Diplas B.H., Yang R., Killela P.J., Meng Q., Ye Z.Y., Wang W., Jiang X.T., et al. 2015. Recurrent TERT promoter mutations identified in a large-scale study of multiple tumour types are associated with increased TERT expression and telomerase activation. Eur. J. Cancer. 51:969–976. 10.1016/j.ejca.2015.03.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hurst C.D., Platt F.M., and Knowles M.A.. 2014. Comprehensive mutation analysis of the TERT promoter in bladder cancer and detection of mutations in voided urine. Eur. Urol. 65:367–369. 10.1016/j.eururo.2013.08.057 [DOI] [PubMed] [Google Scholar]
- Jafri M.A., Ansari S.A., Alqahtani M.H., and Shay J.W.. 2016. Roles of telomeres and telomerase in cancer, and advances in telomerase-targeted therapies. Genome Med. 8:69 10.1186/s13073-016-0324-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jaime-Pérez J.C., Colunga-Pedraza P.R., Gómez-Ramírez C.D., Gutiérrez-Aguirre C.H., Cantú-Rodríguez O.G., Tarín-Arzaga L.C., and Gómez-Almaguer D.. 2011. Danazol as first-line therapy for aplastic anemia. Ann. Hematol. 90:523–527. 10.1007/s00277-011-1163-x [DOI] [PubMed] [Google Scholar]
- Kannengiesser C., Borie R., Ménard C., Réocreux M., Nitschké P., Gazal S., Mal H., Taillé C., Cadranel J., Nunes H., et al. 2015. Heterozygous RTEL1 mutations are associated with familial pulmonary fibrosis. Eur. Respir. J. 46:474–485. 10.1183/09031936.00040115 [DOI] [PubMed] [Google Scholar]
- Karlseder J., Broccoli D., Dai Y., Hardy S., and de Lange T.. 1999. p53- and ATM-dependent apoptosis induced by telomeres lacking TRF2. Science. 283:1321–1325. 10.1126/science.283.5406.1321 [DOI] [PubMed] [Google Scholar]
- Kaul Z., Cesare A.J., Huschtscha L.I., Neumann A.A., and Reddel R.R.. 2011. Five dysfunctional telomeres predict onset of senescence in human cells. EMBO Rep. 13:52–59. 10.1038/embor.2011.227 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Khoo C.M., Carrasco D.R., Bosenberg M.W., Paik J.H., and Depinho R.A.. 2007. Ink4a/Arf tumor suppressor does not modulate the degenerative conditions or tumor spectrum of the telomerase-deficient mouse. Proc. Natl. Acad. Sci. USA. 104:3931–3936. 10.1073/pnas.0700093104 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim N.W., Piatyszek M.A., Prowse K.R., Harley C.B., West M.D., Ho P.L., Coviello G.M., Wright W.E., Weinrich S.L., and Shay J.W.. 1994. Specific association of human telomerase activity with immortal cells and cancer. Science. 266:2011–2015. 10.1126/science.7605428 [DOI] [PubMed] [Google Scholar]
- Kinde I., Munari E., Faraj S.F., Hruban R.H., Schoenberg M., Bivalacqua T., Allaf M., Springer S., Wang Y., Diaz L.A. Jr., et al. 2013. TERT promoter mutations occur early in urothelial neoplasia and are biomarkers of early disease and disease recurrence in urine. Cancer Res. 73:7162–7167. 10.1158/0008-5472.CAN-13-2498 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee H.W., Blasco M.A., Gottlieb G.J., Horner J.W. II, Greider C.W., and DePinho R.A.. 1998. Essential role of mouse telomerase in highly proliferative organs. Nature. 392:569–574. 10.1038/33345 [DOI] [PubMed] [Google Scholar]
- Leri A., Franco S., Zacheo A., Barlucchi L., Chimenti S., Limana F., Nadal-Ginard B., Kajstura J., Anversa P., and Blasco M.A.. 2003. Ablation of telomerase and telomere loss leads to cardiac dilatation and heart failure associated with p53 upregulation. EMBO J. 22:131–139. 10.1093/emboj/cdg013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Levine B., and Kroemer G.. 2008. Autophagy in the pathogenesis of disease. Cell. 132:27–42. 10.1016/j.cell.2007.12.018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lin T.T., Letsolo B.T., Jones R.E., Rowson J., Pratt G., Hewamana S., Fegan C., Pepper C., and Baird D.M.. 2010. Telomere dysfunction and fusion during the progression of chronic lymphocytic leukemia: Evidence for a telomere crisis. Blood. 116:1899–1907. 10.1182/blood-2010-02-272104 [DOI] [PubMed] [Google Scholar]
- Lindsey J., McGill N.I., Lindsey L.A., Green D.K., and Cooke H.J.. 1991. In vivo loss of telomeric repeats with age in humans. Mutat. Res. 256:45–48. 10.1016/0921-8734(91)90032-7 [DOI] [PubMed] [Google Scholar]
- Liu D., Safari A., O’Connor M.S., Chan D.W., Laegeler A., Qin J., and Songyang Z.. 2004. PTOP interacts with POT1 and regulates its localization to telomeres. Nat. Cell Biol. 6:673–680. 10.1038/ncb1142 [DOI] [PubMed] [Google Scholar]
- Liu L., Bailey S.M., Okuka M., Muñoz P., Li C., Zhou L., Wu C., Czerwiec E., Sandler L., Seyfang A., et al. 2007. Telomere lengthening early in development. Nat. Cell Biol. 9:1436–1441. 10.1038/ncb1664 [DOI] [PubMed] [Google Scholar]
- López-Otín C., Blasco M.A., Partridge L., Serrano M., and Kroemer G.. 2013. The hallmarks of aging. Cell. 153:1194–1217. 10.1016/j.cell.2013.05.039 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maciejowski J., Li Y., Bosco N., Campbell P.J., and de Lange T.. 2015. Chromothripsis and kataegis induced by telomere crisis. Cell. 163:1641–1654. 10.1016/j.cell.2015.11.054 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marion R.M., Strati K., Li H., Tejera A., Schoeftner S., Ortega S., Serrano M., and Blasco M.A.. 2009. Telomeres acquire embryonic stem cell characteristics in induced pluripotent stem cells. Cell Stem Cell. 4:141–154. 10.1016/j.stem.2008.12.010 [DOI] [PubMed] [Google Scholar]
- Martinez P., Siegl-Cachedenier I., Flores J.M., and Blasco M.A.. 2009a MSH2 deficiency abolishes the anticancer and pro-aging activity of short telomeres. Aging Cell. 8:2–17. 10.1111/j.1474-9726.2008.00441.x [DOI] [PubMed] [Google Scholar]
- Martinez P., Thanasoula M., Carlos A.R., Gómez-López G., Tejera A.M., Schoeftner S., Dominguez O., Pisano D.G., Tarsounas M., and Blasco M.A.. 2010. Mammalian Rap1 controls telomere function and gene expression through binding to telomeric and extratelomeric sites. Nat. Cell Biol. 12:768–780. 10.1038/ncb2081 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martínez P., and Blasco M.A.. 2010. Role of shelterin in cancer and aging. Aging Cell. 9:653–666. 10.1111/j.1474-9726.2010.00596.x [DOI] [PubMed] [Google Scholar]
- Martínez P., and Blasco M.A.. 2011. Telomeric and extra-telomeric roles for telomerase and the telomere-binding proteins. Nat. Rev. Cancer. 11:161–176. 10.1038/nrc3025 [DOI] [PubMed] [Google Scholar]
- Martínez P., Thanasoula M., Muñoz P., Liao C., Tejera A., McNees C., Flores J.M., Fernández-Capetillo O., Tarsounas M., and Blasco M.A.. 2009b Increased telomere fragility and fusions resulting from TRF1 deficiency lead to degenerative pathologies and increased cancer in mice. Genes Dev. 23:2060–2075. 10.1101/gad.543509 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martínez P., Gómez-López G., Pisano D.G., Flores J.M., and Blasco M.A.. 2016. A genetic interaction between RAP1 and telomerase reveals an unanticipated role for RAP1 in telomere maintenance. Aging Cell. 15:1113–1125. 10.1111/acel.12517 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meeker A.K., Hicks J.L., Iacobuzio-Donahue C.A., Montgomery E.A., Westra W.H., Chan T.Y., Ronnett B.M., and De Marzo A.M.. 2004. Telomere length abnormalities occur early in the initiation of epithelial carcinogenesis. Clin. Cancer Res. 10:3317–3326. 10.1158/1078-0432.CCR-0984-03 [DOI] [PubMed] [Google Scholar]
- Mender I., Gryaznov S., Dikmen Z.G., Wright W.E., and Shay J.W.. 2015. Induction of telomere dysfunction mediated by the telomerase substrate precursor 6-thio-2′-deoxyguanosine. Cancer Discov. 5:82–95. 10.1158/2159-8290.CD-14-0609 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miyachi K., Fujita M., Tanaka N., Sasaki K., and Sunagawa M.. 2002. Correlation between telomerase activity and telomeric-repeat binding factors in gastric cancer. J. Exp. Clin. Cancer Res. 21:269–275. [PubMed] [Google Scholar]
- Nakanishi K., Kawai T., Kumaki F., Hiroi S., Mukai M., Ikeda E., Koering C.E., and Gilson E.. 2003. Expression of mRNAs for telomeric repeat binding factor (TRF)-1 and TRF2 in atypical adenomatous hyperplasia and adenocarcinoma of the lung. Clin. Cancer Res. 9:1105–1111. [PubMed] [Google Scholar]
- Newey P.J., Nesbit M.A., Rimmer A.J., Attar M., Head R.T., Christie P.T., Gorvin C.M., Stechman M., Gregory L., Mihai R., et al. 2012. Whole-exome sequencing studies of nonhereditary (sporadic) parathyroid adenomas. J. Clin. Endocrinol. Metab. 97:E1995–E2005. 10.1210/jc.2012-2303 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Olovnikov A.M. 1973. A theory of marginotomy. The incomplete copying of template margin in enzymic synthesis of polynucleotides and biological significance of the phenomenon. J. Theor. Biol. 41:181–190. 10.1016/0022-5193(73)90198-7 [DOI] [PubMed] [Google Scholar]
- Pal D., Sharma U., Singh S.K., Kakkar N., and Prasad R.. 2015. Over-expression of telomere binding factors (TRF1 & TRF2) in renal cell carcinoma and their inhibition by using SiRNA induce apoptosis, reduce cell proliferation and migration invitro. PLoS One. 10:e0115651 10.1371/journal.pone.0115651 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Palm W., and de Lange T.. 2008. How shelterin protects mammalian telomeres. Annu. Rev. Genet. 42:301–334. 10.1146/annurev.genet.41.110306.130350 [DOI] [PubMed] [Google Scholar]
- Perera S.A., Maser R.S., Xia H., McNamara K., Protopopov A., Chen L., Hezel A.F., Kim C.F., Bronson R.T., Castrillon D.H., et al. 2008. Telomere dysfunction promotes genome instability and metastatic potential in a K-ras p53 mouse model of lung cancer. Carcinogenesis. 29:747–753. 10.1093/carcin/bgn050 [DOI] [PubMed] [Google Scholar]
- Pickett H.A., and Reddel R.R.. 2015. Molecular mechanisms of activity and derepression of alternative lengthening of telomeres. Nat. Struct. Mol. Biol. 22:875–880. 10.1038/nsmb.3106 [DOI] [PubMed] [Google Scholar]
- Pinzaru A.M., Hom R.A., Beal A., Phillips A.F., Ni E., Cardozo T., Nair N., Choi J., Wuttke D.S., Sfeir A., and Denchi E.L.. 2016. Telomere replication stress induced by POT1 inactivation accelerates tumorigenesis. Cell Reports. 15:2170–2184. 10.1016/j.celrep.2016.05.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Povedano J.M., Martinez P., Flores J.M., Mulero F., and Blasco M.A.. 2015. Mice with pulmonary fibrosis driven by telomere dysfunction. Cell Reports. 12:286–299. 10.1016/j.celrep.2015.06.028 [DOI] [PubMed] [Google Scholar]
- Ramsay A.J., Quesada V., Foronda M., Conde L., Martínez-Trillos A., Villamor N., Rodríguez D., Kwarciak A., Garabaya C., Gallardo M., et al. 2013. POT1 mutations cause telomere dysfunction in chronic lymphocytic leukemia. Nat. Genet. 45:526–530. 10.1038/ng.2584 [DOI] [PubMed] [Google Scholar]
- Ramunas J., Yakubov E., Brady J.J., Corbel S.Y., Holbrook C., Brandt M., Stein J., Santiago J.G., Cooke J.P., and Blau H.M.. 2015. Transient delivery of modified mRNA encoding TERT rapidly extends telomeres in human cells. FASEB J. 29:1930–1939. 10.1096/fj.14-259531 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Robin J.D., Ludlow A.T., Batten K., Magdinier F., Stadler G., Wagner K.R., Shay J.W., and Wright W.E.. 2014. Telomere position effect: Regulation of gene expression with progressive telomere shortening over long distances. Genes Dev. 28:2464–2476. 10.1101/gad.251041.114 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Robles-Espinoza C.D., Harland M., Ramsay A.J., Aoude L.G., Quesada V., Ding Z., Pooley K.A., Pritchard A.L., Tiffen J.C., Petljak M., et al. 2014. POT1 loss-of-function variants predispose to familial melanoma. Nat. Genet. 46:478–481. 10.1038/ng.2947 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roger L., Jones R.E., Heppel N.H., Williams G.T., Sampson J.R., and Baird D.M.. 2013. Extensive telomere erosion in the initiation of colorectal adenomas and its association with chromosomal instability. J. Natl. Cancer Inst. 105:1202–1211. 10.1093/jnci/djt191 [DOI] [PubMed] [Google Scholar]
- Saito K., Yagihashi A., Nasu S., Izawa Y., Nakamura M., Kobayashi D., Tsuji N., and Watanabe N.. 2002. Gene expression for suppressors of telomerase activity (telomeric-repeat binding factors) in breast cancer. Jpn. J. Cancer Res. 93:253–258. 10.1111/j.1349-7006.2002.tb02166.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sanders J.L., and Newman A.B.. 2013. Telomere length in epidemiology: A biomarker of aging, age-related disease, both, or neither? Epidemiol. Rev. 35:112–131. 10.1093/epirev/mxs008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Savage S.A., Giri N., Baerlocher G.M., Orr N., Lansdorp P.M., and Alter B.P.. 2008. TINF2, a component of the shelterin telomere protection complex, is mutated in dyskeratosis congenita. Am. J. Hum. Genet. 82:501–509. 10.1016/j.ajhg.2007.10.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schneider R.P., Garrobo I., Foronda M., Palacios J.A., Marión R.M., Flores I., Ortega S., and Blasco M.A.. 2013. TRF1 is a stem cell marker and is essential for the generation of induced pluripotent stem cells. Nat. Commun. 4:1946 10.1038/ncomms2946 [DOI] [PubMed] [Google Scholar]
- Seger Y.R., García-Cao M., Piccinin S., Cunsolo C.L., Doglioni C., Blasco M.A., Hannon G.J., and Maestro R.. 2002. Transformation of normal human cells in the absence of telomerase activation. Cancer Cell. 2:401–413. 10.1016/S1535-6108(02)00183-6 [DOI] [PubMed] [Google Scholar]
- Sfeir A., Kabir S., van Overbeek M., Celli G.B., and de Lange T.. 2010. Loss of Rap1 induces telomere recombination in the absence of NHEJ or a DNA damage signal. Science. 327:1657–1661. 10.1126/science.1185100 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shahidi N.T., and Diamond L.K.. 1961. Testosterone-induced remission in aplastic anemia of both acquired and congenital types. Further observations in 24 cases. N. Engl. J. Med. 264:953–967. 10.1056/NEJM196105112641901 [DOI] [PubMed] [Google Scholar]
- Sharpless N.E., and DePinho R.A.. 2007. How stem cells age and why this makes us grow old. Nat. Rev. Mol. Cell Biol. 8:703–713. 10.1038/nrm2241 [DOI] [PubMed] [Google Scholar]
- Shay J.W. 2016. Role of telomeres and telomerase in aging and cancer. Cancer Discov. 6:584–593. 10.1158/2159-8290.CD-16-0062 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shay J.W., and Wright W.E.. 2005. Senescence and immortalization: Role of telomeres and telomerase. Carcinogenesis. 26:867–874. 10.1093/carcin/bgh296 [DOI] [PubMed] [Google Scholar]
- Shi J., Yang X.R., Ballew B., Rotunno M., Calista D., Fargnoli M.C., Ghiorzo P., Bressac-de Paillerets B., Nagore E., Avril M.F., et al. French Familial Melanoma Study Group . 2014. Rare missense variants in POT1 predispose to familial cutaneous malignant melanoma. Nat. Genet. 46:482–486. 10.1038/ng.2941 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shih I.M., Zhou W., Goodman S.N., Lengauer C., Kinzler K.W., and Vogelstein B.. 2001. Evidence that genetic instability occurs at an early stage of colorectal tumorigenesis. Cancer Res. 61:818–822. [PubMed] [Google Scholar]
- Simeonova I., Jaber S., Draskovic I., Bardot B., Fang M., Bouarich-Bourimi R., Lejour V., Charbonnier L., Soudais C., Bourdon J.C., et al. 2013. Mutant mice lacking the p53 C-terminal domain model telomere syndromes. Cell Reports. 3:2046–2058. 10.1016/j.celrep.2013.05.028 [DOI] [PubMed] [Google Scholar]
- Stadler G., Rahimov F., King O.D., Chen J.C., Robin J.D., Wagner K.R., Shay J.W., Emerson C.P. Jr., and Wright W.E.. 2013. Telomere position effect regulates DUX4 in human facioscapulohumeral muscular dystrophy. Nat. Struct. Mol. Biol. 20:671–678. 10.1038/nsmb.2571 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stanley S.E., and Armanios M.. 2015. The short and long telomere syndromes: Paired paradigms for molecular medicine. Curr. Opin. Genet. Dev. 33:1–9. 10.1016/j.gde.2015.06.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stanley S.E., Gable D.L., Wagner C.L., Carlile T.M., Hanumanthu V.S., Podlevsky J.D., Khalil S.E., DeZern A.E., Rojas-Duran M.F., Applegate C.D., et al. 2016. Loss-of-function mutations in the RNA biogenesis factor NAF1 predispose to pulmonary fibrosis-emphysema. Sci. Transl. Med. 8:351ra107 10.1126/scitranslmed.aaf7837 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stuart B.D., Choi J., Zaidi S., Xing C., Holohan B., Chen R., Choi M., Dharwadkar P., Torres F., Girod C.E., et al. 2015. Exome sequencing links mutations in PARN and RTEL1 with familial pulmonary fibrosis and telomere shortening. Nat. Genet. 47:512–517. 10.1038/ng.3278 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tchkonia T., Zhu Y., van Deursen J., Campisi J., and Kirkland J.L.. 2013. Cellular senescence and the senescent secretory phenotype: Therapeutic opportunities. J. Clin. Invest. 123:966–972. 10.1172/JCI64098 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tefferi A., Lasho T.L., Begna K.H., Patnaik M.M., Zblewski D.L., Finke C.M., Laborde R.R., Wassie E., Schimek L., Hanson C.A., et al. 2015. A pilot study of the telomerase inhibitor imetelstat for myelofibrosis. N. Engl. J. Med. 373:908–919. 10.1056/NEJMoa1310523 [DOI] [PubMed] [Google Scholar]
- Tejera A.M., Stagno d’Alcontres M., Thanasoula M., Marion R.M., Martinez P., Liao C., Flores J.M., Tarsounas M., and Blasco M.A.. 2010. TPP1 is required for TERT recruitment, telomere elongation during nuclear reprogramming, and normal skin development in mice. Dev. Cell. 18:775–789. 10.1016/j.devcel.2010.03.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tomás-Loba A., Flores I., Fernández-Marcos P.J., Cayuela M.L., Maraver A., Tejera A., Borrás C., Matheu A., Klatt P., Flores J.M., et al. 2008. Telomerase reverse transcriptase delays aging in cancer-resistant mice. Cell. 135:609–622. 10.1016/j.cell.2008.09.034 [DOI] [PubMed] [Google Scholar]
- Townsley D.M., Dumitriu B., Liu D., Biancotto A., Weinstein B., Chen C., Hardy N., Mihalek A.D., Lingala S., Kim Y.J., et al. 2016. Danazol treatment for telomere diseases. N. Engl. J. Med. 374:1922–1931. 10.1056/NEJMoa1515319 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Varela E., Schneider R.P., Ortega S., and Blasco M.A.. 2011. Different telomere-length dynamics at the inner cell mass versus established embryonic stem (ES) cells. Proc. Natl. Acad. Sci. USA. 108:15207–15212. 10.1073/pnas.1105414108 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Varela E., Muñoz-Lorente M.A., Tejera A.M., Ortega S., and Blasco M.A.. 2016. Generation of mice with longer and better preserved telomeres in the absence of genetic manipulations. Nat. Commun. 7:11739 10.1038/ncomms11739 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vera E., Bernardes de Jesus B., Foronda M., Flores J.M., and Blasco M.A.. 2012. The rate of increase of short telomeres predicts longevity in mammals. Cell Reports. 2:732–737. 10.1016/j.celrep.2012.08.023 [DOI] [PubMed] [Google Scholar]
- Vitale I., Galluzzi L., Castedo M., and Kroemer G.. 2011. Mitotic catastrophe: A mechanism for avoiding genomic instability. Nat. Rev. Mol. Cell Biol. 12:385–392. 10.1038/nrm3115 [DOI] [PubMed] [Google Scholar]
- Wang E.S., Wu K., Chin A.C., Chen-Kiang S., Pongracz K., Gryaznov S., and Moore M.A.. 2004. Telomerase inhibition with an oligonucleotide telomerase template antagonist: In vitro and in vivo studies in multiple myeloma and lymphoma. Blood. 103:258–266. 10.1182/blood-2003-02-0546 [DOI] [PubMed] [Google Scholar]
- Watson J.D. 1972. Origin of concatemeric T7 DNA. Nat. New Biol. 239:197–201. 10.1038/newbio239197a0 [DOI] [PubMed] [Google Scholar]
- Wright W.E., and Shay J.W.. 1992. The two-stage mechanism controlling cellular senescence and immortalization. Exp. Gerontol. 27:383–389. 10.1016/0531-5565(92)90069-C [DOI] [PubMed] [Google Scholar]
- Zhang J., Jima D., Moffitt A.B., Liu Q., Czader M., Hsi E.D., Fedoriw Y., Dunphy C.H., Richards K.L., Gill J.I., et al. 2014. The genomic landscape of mantle cell lymphoma is related to the epigenetically determined chromatin state of normal B cells. Blood. 123:2988–2996. 10.1182/blood-2013-07-517177 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zou Y., Sfeir A., Gryaznov S.M., Shay J.W., and Wright W.E.. 2004. Does a sentinel or a subset of short telomeres determine replicative senescence? Mol. Biol. Cell. 15:3709–3718. 10.1091/mbc.E04-03-0207 [DOI] [PMC free article] [PubMed] [Google Scholar]