Abstract
Background
To study the incidence of and factors influencing “neck shortening” in elderly patients treated for femoral neck fractures using multiple cancellous screws.
Material/Methods
Of the 197 femoral neck fracture cases treated via closed reduction and cancellous screws fixation from January 2006 to February 2010, 110 were followed up. Patient age, gender, operative time, implantation method, reduction quality, fracture type, bone mineral density, loading time, length of hospital stay, and Harris hip score 12 months after operation were recorded. The patients were divided into two groups (shortening and non-shortening) based on their X-ray performance during follow-up. The healing rates and Harris hip scores of the two groups were compared, and the influencing factors of femoral neck shortening were analyzed.
Results
Of the 110 cases followed up, 94.5% (104/110) were healed and neck shortening occurred in 41.8% (46/110) within 12.5 months (mean) after treatment. The Harris hip score of the shortening group was lower than that of the non-shortening group (78±17 vs. 86±23, p=0.048). The fracture healing rates of the two groups were not significantly different (p=0.068). The factors influencing neck shortening were significantly correlated with bone mineral density, patient age, gender, and type of fracture.
Conclusions
The incidence of neck shortening in elderly patients treated for femoral neck fracture using cancellous screws was high. Bone mineral density, patient age, gender, and type of fracture were the influencing factors of neck shortening.
MeSH Keywords: Bone Screws, Femoral Neck Fractures, Internal Fixators, Neck Pain
Background
Femoral neck fractures are associated with high mortality rates at one year after surgery, and profound temporary and sometimes permanent impairment of independence and quality of life. Options for managing femoral neck fractures include non-operative and operative management with either internal fixation or arthroplasty. In recent years, operation on femoral neck fractures was the main treatment [1,2]. Options for internal fixation include the use of various implants such as sliding compression cancellous screws, which have been reported to have good clinical results. However, this surgical technique allows dynamic compression at the fracture site during weight bearing; thus, shortening of the femoral neck might occur. Many studies have investigated the complications of this procedure [3–9]. However, the incidence of and factors influencing neck shortening in patients given this treatment have rarely been assessed. In the current study, we tried to better ascertain the incidence of and clinical predictors associated with femoral neck shortening, and to determine the influence of using sliding compression cancellous screws on the functional outcome of patients.
Material and Methods
Patients
In this prospective cohort study, the protocol conformed to the ethical guidelines of the Declaration of Helsinki and was approved by the ethics committee of Beijing Army General Hospital (Beijing, China). Informed consent was obtained from all patients before our study started.
A consecutive series of 197 patients with femoral neck fractures treated via closed reduction and cancellous screw fixation in our hospital from January 2010 to February 2014 were included when they fulfilled the following criteria: age ≥60 years and with clinical and imaging diagnoses of femoral neck fractures. Exclusion criteria were pathologic fracture combined with other fractures or injuries, femoral head necrosis, and fixation failure after surgery. All the patients were treated using three parallel cancellous screws or via strong oblique fixation (oblique angle) after closed reduction. Operations were performed 2 to 13 days (mean, 3.6 days) after the injury was sustained.
All the patients were followed up clinically and radiologically by one of the three operating surgeons at 1, 3, 12, and 24 months after the operation; the mean period of follow-up was 12.5 months (range, 3 to 39 months). Outcomes were analyzed at the end of the follow-ups.
A total of 110 patients (35 males and 75 females; mean age, 75 years) completed the follow-ups. A total of 68 cases sustained a fracture of the left hip, and 42 cases sustained the injury at the right hip. With respect to the Garden classification of femoral neck fractures, 7 type I, 25 type II (including intercalation), 49 type III, and 29 type IV fractures were identified. Of the 110 patients, 92 (83.6%) had more than one other systemic complication, mainly hypertension, coronary heart disease, diabetes, chronic bronchitis, and atrial fibrillation.
Methods
Trabecular bone density of the contralateral proximal femur was evaluated in all the patients after hospital admission. The estimated average bone density was −2.8 (T-score). Before operation, a skin or skeletal traction was generally performed.
Standard techniques were used for fracture stabilization. Operations were performed under image-intensifier control using anteroposterior (AP) and lateral views, with the patients in a supine position on a traction table. Displaced fractures were mostly reduced via traction, with the hip in neutral flexion and internal rotation and approximately 10° abduction.
Non-displaced fractures were fixed in situ. The goal of correcting the angulation was to obtain a position as close as possible to a Garden index of 160° in the AP plane and 180° in the lateral plane, although slight valgus angulation was accepted. Screws were percutaneously placed across the femoral neck via parallel implantation or strong oblique implantation. The length of the screws was determined in such a way that the tips would reach the subchondral bone of the femoral head.
All the patients were encouraged to sit up the day after operation. Perioperative AP and lateral radiographs were taken on the first day after operation. The quality of fracture reduction was determined according to the Garden alignment index on AP and lateral views. Results were follows: Garden grade I, 39 cases; grade II, 30 cases; grade III, 35 cases; and grade IV, 6 cases.
Follow-ups were performed 1, 3, 12, and 24 months after the operation. All the patients underwent clinical and radiographic examinations to determine the length of weight-bearing time. The clinical course of each patient was documented and their Harris hip scores were determined 12 months after surgery. Due to poor patient compliance, 36 patients were followed up for 10 to 14 months, and the follow-up period of 19 patients was fewer than 10 months; hence, their Harris hip scores were not included in the analysis. Fracture healing was evaluated during the last follow-up according to clinical and radiographic examination results. During the follow-up period, the patients were divided into two groups, shortening and non-shortening, based on their X-ray images. The incidence of neck shortening in all the patients was determined, and the rate of fracture healing and hip function (Harris hip scores) of the shortening and non-shortening groups were compared. The predictors of neck shortening were further identified.
Statistical analysis
The observed indicators – patient age, gender, surgical time, implantation method, reduction quality, fracture type, bone density, weight-bearing time, and length of hospitalization – were considered as independent variables. The occurrence of neck shortening was used as a dependent variable. Parametric data were analyzed using the χ2 test or Fisher’s exact test. All variables with a p value <0.5 in the bivariate analysis were included in the multivariate model. Multivariate logistic regression analysis was performed to identify the predictors of neck shortening. A two-tailed p value <0.05 was considered significant. All data analyses were conducted using SPSS 16.0 statistical software.
Results
Incidence of neck shortening, rate of fracture healing, and hip function based on Harris hip score
Overall, 110 patients were considered for analysis. Neck shortening occurred in 46 of these patients as determined radiographically; the occurrence rate was 41.8% and average loading time was 1.8 months (range, 1 to 3 months). Moreover, 104 fracture cases were healed, and the healing rate was 94.5%. The average Harris hip score of the 110 patients was 72.4 points (range, 22 to 97 points). There was no significant difference observed between the fracture healing rates of the shortening and non-shortening groups. However, the Harris hip score of the shortening group was significantly lower than that of the non-shortening group (Table 1).
Table 1.
A comparison of fracture healing and hip function after operation between shortening group and non-shortening group.
| Incidence | Healing rate | Harris score | |
|---|---|---|---|
| Neck shortening group | 41.8% (46 cases) | 95.7% (44/46) | 78 ± 17 |
| Non-neck shortening group | 58.2% (64 cases) | 93.7% (60/64) | 86 ± 23 |
| χ2 value | – | 3.343 | – |
| t value | – | – | −1.998 |
| P value | – | 0.068 | 0.048 |
Factors that influenced the occurrence of neck shortening
Based on the univariate analyses, age (>70 years), gender (female), type of fracture (types III and IV), bone mineral density (T ≤–2.5), and fracture reduction quality were significantly associated with the occurrence of neck shortening. Bone mineral density (T ≤–2.5) and fracture reduction quality were more relevant to neck shortening than age (>70 years) and gender (female). Operative time (≤4 days), implantation method (parallel or strong oblique), loading time after surgery (≤2 months), and length of hospital stay (≤7 days) were not associated with the occurrence of neck shortening (Tables 2 and 3).
Table 2.
General comparison between shortening group and non-shortening group.
| Cases | Shortening N=46 | Non-shortening N=64 | χ2 value | P | |
|---|---|---|---|---|---|
| Age | |||||
| >70 y | 66 | 34 | 32 | 6.370 | 0.012 |
| ≤70 y | 44 | 12 | 32 | ||
| Gender | |||||
| Male | 32 | 7 | 25 | 7.734 | 0.007 |
| Female | 78 | 39 | 39 | ||
| Operative time | |||||
| ≤4 d | 60 | 20 | 40 | 3.960 | 0.048 |
| >4 d | 50 | 26 | 24 | ||
| Implantation method | |||||
| Parallel implantation | 62 | 32 | 30 | 5.602 | 0.018 |
| Strong oblique implantation | 48 | 14 | 34 | ||
| Reduction quality | |||||
| Grade I, II | 69 | 16 | 53 | 26.407 | 0.000 |
| Grade III, IV | 41 | 30 | 11 | ||
| Fracture type | |||||
| Type I, II | 42 | 10 | 32 | 9.056 | 0.003 |
| Type III, IV | 68 | 36 | 32 | ||
| Bone mineral density | |||||
| T ≤–2.5 | 80 | 40 | 40 | 8.017 | 0.004 |
| T >–2.5 | 30 | 6 | 24 | ||
| Loading time | |||||
| ≤2 months | 57 | 36 | 21 | 22.142 | 0.000 |
| >2 months | 53 | 10 | 43 | ||
| Length of hospital stay | |||||
| ≤7 d | 53 | 34 | 19 | 20.160 | 0.000 |
| >7 d | 57 | 12 | 45 | ||
Table 3.
Multiple regression analyses of the influencing factors of “neck shortening”.
| Influencing factors | B | S.E. | Wald | Exp (B) | 95% CI | P |
|---|---|---|---|---|---|---|
| Age | ||||||
| >70 years | 3.490 | .506 | 11.66 | 10.23 | 3.87–17.43 | 0.006 |
|
| ||||||
| Gender | ||||||
| Female | 2.765 | .543 | 7.998 | 9.13 | 2.45–15.54 | 0.003 |
|
| ||||||
| Fracture type | ||||||
| Garden III, IV | 3.095 | .258 | 9.379 | 10.28 | 5.87–21.56 | 0.000 |
|
| ||||||
| BMD | ||||||
| T ≤–2.5 | 5.612 | .487 | 14.284 | 28.34 | 6.35–44.15 | 0.000 |
|
| ||||||
| Reduction quality | ||||||
| Grade III, IV | 2.006 | .543 | 6.610 | 15.22 | 5.34–29.27 | 0.000 |
Discussion
Femoral neck fractures can be treated via immediate prosthetic replacement (total hip arthroplasty or hemiarthroplasty) or internal fixation using pins or screws [10–14]. Several studies have suggested that fracture reduction and fixation are associated with a lower rate of morbidity and mortality than treatment via prosthetic replacement [15,16]. Some reports emphasized that the multiple cannulated screws procedure is associated with low operative mortality and morbidity and a high rate of fracture union. The surgical procedure used in the present study was based on their principle [15,17]. However, some problems that still exist in the treatment are worth noting, such as during the follow-up period, femoral neck shortening occurred in a substantial number of patients based on imaging. Other issues of less concern include imaging performance, effect of the described procedure on joint function after surgery, and occurrence rate of and factors influencing neck shortening.
Incidence of neck shortening
The incidence of neck shortening after cancellous screw fixation is rarely reported in the current literature. In a study by Zlowodzki et al., the incidence of neck shortening was about 31% [18]; our present study revealed an incidence of 42% (Figure 1). This discrepancy may be explained by the different characteristics of the subjects investigated. The former examined more type I and II fractures, whereas the latter examined more type III and IV fractures and older (on average) patients. We also found that neck shortening generally occurs one to three months after surgery, and rarely after three months. Femoral neck shortening may be partly attributed to bone resorption during fracture healing and partly to sliding compression between fracture blocks during cancellous screw fixation. In our study, we observed that neck shortening mostly occurred early after surgery, even immediately in some cases, according to follow-up X-rays (Figure 2). In these cases, fractures were often comminuted, and shortening may occur immediately after fracture owing to the loss of bone density in the fracture site. Although the neck is restored to some length via traction during the operation, the sliding compression of the screws acting on the fracture site did not maintain the length of the femoral neck by controlling the move that occurred in the fracture site.
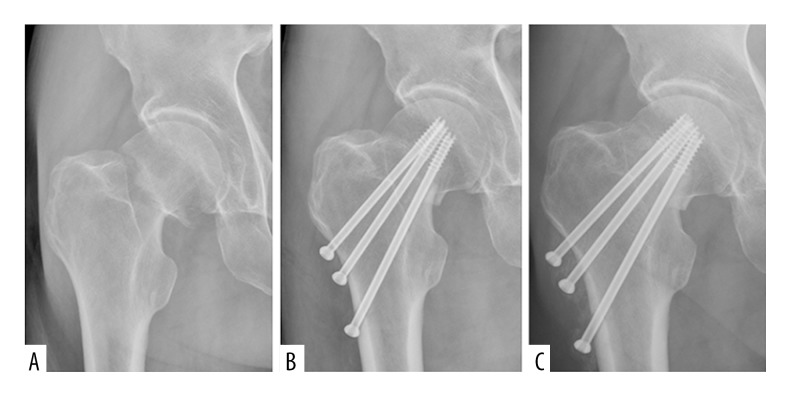
Figure 1.
Male, 64 years old, Garden type III fracture. (A) Preoperative X-ray film; (B) Postoperative X-ray film; (C) X-ray film after 1 year; Harris hip score (obtained 1 year after surgery), 72 points.
Figure 2.
Female, 76 years, Garden type III fracture. (A) Preoperative X-ray film; (B) Postoperative X-ray film; (C) X-ray film after 1 year; Harris hip score (obtained 1 year after surgery), 80 points.
Factors influencing neck shortening
There are few studies covering the factors that influence neck shortening. A few key variables were selected and investigated to study the occurrence of neck shortening. Based on logistic regression analyses, the occurrence of neck shortening was mostly associated with bone mineral density (T ≤–2.5) and fracture reduction quality, and was least associated with the type of fracture, patient age, gender, and so on. Low bone mineral density may have indicated that bone quantity at the fracture site was significantly reduced, which may have consequently weakened the effect of internal fixation on the fracture and the strength of the fracture against axial compression. A biomechanical study by Alves et al. has confirmed this explanation; they observed that injecting hydroxyapatite (to increase local bone quantity) into the fracture site increases the holding power of cancellous screws in the fracture, as well as strengthens the resistance of the site to axis pressure, which results in the effective reduction of the incidence of neck shortening [19].
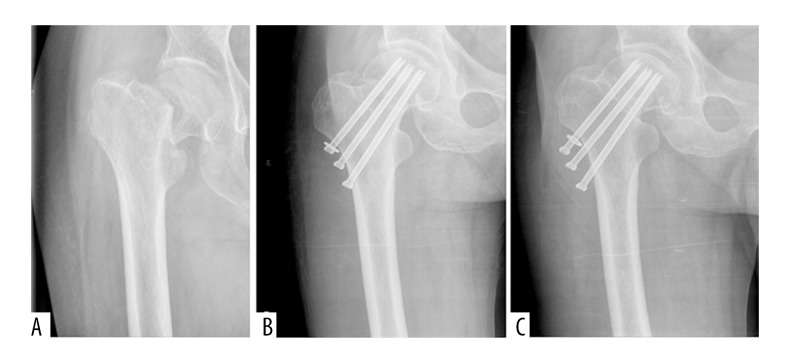
The fracture reduction quality was highly correlated with the incidence of neck shortening. This finding indicates that good reduction is helpful in improving local blood circulation and restoring favorable stress in the fracture fragments, which could decrease the incidence of aseptic necrosis and bone resorption at the fracture site, consequently reducing the incidence of neck shortening. In our study, gender and patient age were also correlated with femoral neck shortening. Actually, the close correlation between these two factors and bone density was not difficult to establish. In general, elderly females have a more serious degree of osteoporosis than males, and with increasing age, the loss of bone quantity increases. This result affects the incidence of neck shortening. Currently, we have not yet seen a report that discusses the relationship between patient age, gender, and incidence of neck shortening after internal fixation. Concerning the relationship between the incidence of neck shortening and fracture type in a group of 56 patients, Zlowodzki et al. observed no significant difference between the incidence of neck shortening in displaced fractures and non-displaced fractures (27% vs. 31%) [18]. This finding was not in agreement with our study, wherein the occurrence rate of neck shortening in Garden type I and II fracture patients (23.8% [10/42]) was significantly lower than that in Garden type III and IV fracture patients (52.9% [36/68]). This difference may be attributed to the difference between the studies in terms of sample size and statistical criteria used for the classification of fracture types. Moreover, the relatively higher rate of neck shortening in Garden type III and IV fractures compared with the other types indicates that joint replacement may be a more ideal treatment for unstable femoral neck fractures, which is consistent with the results of some studies. Compression at the fracture site and internal fixation are two of the principal aspects of treatment, but whether there is a certain relationship between axial pressure caused by body mass (weight bearing) and the incidence of neck shortening needs further exploration. Some authors think that although sliding compression in the fracture fragments [19,20], generated during cancellous screw fixation, can promote healing and improve healing rates, it may also increase the incidence of neck shortening. In some patients, the cancellous screws were fully screwed during fixation, producing a certain fixed pressure that acted on the fracture fragments and prevented the occurrence of shortening by increasing the control of the fracture site. However, neck shortening was still detected six months after fixation (Figure 3). Although neck shortening was observed in only a small number of cases, its occurrence indicated that pressure was not its main cause, and bone mineral density, fracture type, and reduction quality play more important roles in its development.
Figure 3.
Male, 80 years, Garden type III fracture. (A) Preoperative X-ray film; (B) After 1 d, X-ray showed neck shortening; (C) X-ray film after 6 months; Harris hip score (obtained 1 year after surgery), 86 points.
Relationship between neck shortening and fracture healing and joint function
How neck shortening after cancellous screw fixation affects fracture healing is an important concern. In our study, the healing rate was 95.7% (44/46) in the shortening group and 93.7% (60/64) in the non-shortening group; a significant difference was not found (p>0.05). Although neck shortening did not influence fracture healing significantly, it had a significantly negative impact on the patients’ physical functioning. A multicenter study by Zlowodzki et al. involving 660 cases showed that hip joint function and quality of life are significantly reduced in patients who develop neck shortening [20]. Another study by Zlowodzki et al. revealed that 89% of doctors believe that neck shortening affects hip joint abduction [21], and 69% believe that it reduces hip joint function. Our study also suggested that neck shortening adversely affects postoperative joint function; the average Harris hip scores (obtained during a follow-up 12 months after surgery) of the shortening and non-shortening groups were 78 and 86, respectively. Limping and poor abduction strength were the main adverse effects of neck shortening on hip function. The main hip abductor muscles are the gluteus medius and gluteus minimus, and the abductor muscles counteract the central vertical forces rendered by body weight and stabilize the pelvis during the single-leg stance phase of the gait cycle. Both the gluteus medius and gluteus minimus insert on the greater trochanter; consequently, femoral neck shortening decreases the moment arm of the abductor muscles and directly influences their function. A decrease in the abductor moment arm increases the abductor muscle force and joint reaction force required for walking.
In our study, the number of patients followed up was relatively small, and some patients were not followed up during the set schedule. Differences among the doctors who performed data collection, in terms of their understanding of the criteria used, may have also existed, thus affecting the results.
Conclusions
The occurrence of neck shortening is most closely associated with bone mineral density, slightly associated with fracture type and reduction quality, and least associated with patient age and gender. The results of this study remind us that we should pay attention to the aforementioned factors when considering treatment methods. Although the use of cancellous screws for the treatment of femoral neck fractures is effective, there is still room for improvement. The technique used in the treatment of femoral neck fracture results in a high healing rate, but it also results in a high incidence of neck shortening, which adversely affects joint function. Therefore, the selection of treatment indications for individual patients and the reduction of the incidence of neck shortening are important issues that must be considered.
Footnotes
Conflict of interests
None.
Source of support: Self financing
References
- 1.Ahmad T, Ashraf U, Irfan O, et al. Trends in management of neck of femur fracture. J Pak Med Assoc. 2015;65(11 Suppl 3):S163–65. [PubMed] [Google Scholar]
- 2.Grund S, Roos M, Duchene W, et al. Treatment in a center for geriatric traumatology. Dtsch Arztebl Int. 2015;112(7):113–19. doi: 10.3238/arztebl.2015.0113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Thein R, Herman A, Kedem P, et al. Osteosynthesis of unstable intracapsular femoral neck fracture by dynamic locking plate or screw fixation: early results. J Orthop Trauma. 2014;28(2):70–76. doi: 10.1097/BOT.0b013e3182a225fa. [DOI] [PubMed] [Google Scholar]
- 4.Manohara R, Liang S, Huang D, et al. Cancellous screw fixation for undisplaced femoral neck fractures in the elderly. J Orthop Surg (Hong Kong) 2014;22(3):282–86. doi: 10.1177/230949901402200303. [DOI] [PubMed] [Google Scholar]
- 5.Cornwall R, Gilbert MS, Koval KJ, et al. Functional outcomes and mortality vary among different types of hip fractures: A function of patient characteristics. Clin Orthop Relat Res. 2004;(425):64–71. doi: 10.1097/01.blo.0000132406.37763.b3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Warschawski Y, Sharfman ZT, Berger O, et al. Dynamic locking plate vs. simple cannulated screws for nondisplaced intracapsular hip fracture: A comparative study. Injury. 2016;47(2):424–27. doi: 10.1016/j.injury.2015.10.054. [DOI] [PubMed] [Google Scholar]
- 7.Blomfeldt R, Tornkvist H, Ponzer S, et al. Internal fixation versus hemiarthroplasty for displaced fractures of the femoral neck in elderly patients with severe cognitive impairment. J Bone Joint Surg Br. 2005;87:523–29. doi: 10.1302/0301-620X.87B4.15764. [DOI] [PubMed] [Google Scholar]
- 8.Parker MJ, Ali SM. Short versus long thread cannulated cancellous screws for intracapsular hip fractures: A randomised trial of 432 patients. Injury. 2010;41(4):382–84. doi: 10.1016/j.injury.2009.10.008. [DOI] [PubMed] [Google Scholar]
- 9.Halm EA, Wang JJ, Boockvar K, et al. The effect of perioperative anemia on clinical and functional outcomes in patients with hip fracture. J Orthop Trauma. 2004;18:369–74. doi: 10.1097/00005131-200407000-00007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Tan WL, Low SL, Shen L, et al. Osteoporotic hip fractures: 10-year review in a Singaporean hospital. J Orthop Surg (Hong Kong) 2015;23(2):150–54. doi: 10.1177/230949901502300206. [DOI] [PubMed] [Google Scholar]
- 11.Inngul C, Blomfeldt R, Ponzer S, et al. Cemented versus uncemented arthroplasty in patients with a displaced fracture of the femoralneck: A randomised controlled trial. Bone Joint J. 2015;97-B(11):1475–80. doi: 10.1302/0301-620X.97B11.36248. [DOI] [PubMed] [Google Scholar]
- 12.Wang F, Zhang H, Zhang Z, et al. Comparison of bipolar hemiarthroplasty and total hip arthroplasty for displaced femoral neck fractures in the healthy elderly: A meta-analysis. BMC Musculoskelet Disord. 2015;16:229. doi: 10.1186/s12891-015-0696-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Lin JC, Liang WM. Outcomes after fixation for undisplaced femoral neck fracture compared to hemiarthroplasty for displaced femoral neck fracture among the elderly. BMC Musculoskelet Disord. 2015;16:199. doi: 10.1186/s12891-015-0671-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Han SK, Song HS, Kim R, et al. Clinical results of treatment of garden type 1 and 2 femoral neck fractures in patients over 70-year old. Eur J Trauma Emerg Surg. 2016;42(2):191–96. doi: 10.1007/s00068-015-0528-6. [DOI] [PubMed] [Google Scholar]
- 15.Johansson T. Internal fixation compared with total hip replacement for displaced femoral neck fractures: A minimum fifteen-year follow-up study of a previously reported randomized trial. J Bone Joint Surg Am. 2014;96(6):e46. doi: 10.2106/JBJS.K.00244. [DOI] [PubMed] [Google Scholar]
- 16.Cao L, Wang B, Li M, et al. Closed reduction and internal fixation versus total hip arthroplasty for displaced femoral neckfracture. Chin J Traumatol. 2014;17(2):63–68. [PubMed] [Google Scholar]
- 17.Kain MS, Marcantonio AJ, Iorio R. Revision surgery occurs frequently after percutaneous fixation of stable femoral neck fractures in elderly patients. Clin Orthop Relat Res. 2014;472(12):4010–14. doi: 10.1007/s11999-014-3957-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Zlowodzki M, Ayieni O, Petrisor BA, et al. Femoral neck shortening after fracture fixation with multiple cancellous screws: incidence and effect on function. J Trauma. 2008;64:163–69. doi: 10.1097/01.ta.0000241143.71274.63. [DOI] [PubMed] [Google Scholar]
- 19.Alves T, Neal JW, Weinhold PS, et al. Biomechanical comparison of 3 possible fixation strategies to resist femoral neck shortening after fracture. Orthopedics. 2010;16:233–37. doi: 10.3928/01477447-20100225-07. [DOI] [PubMed] [Google Scholar]
- 20.Zlowodzki M, Jönsson A, Paulke R, et al. Shortening after femoral neck fracture fixation: is there a solution? Clin Orthop Relat Res. 2007;(461):213–18. doi: 10.1097/BLO.0b013e31805b7ec4. [DOI] [PubMed] [Google Scholar]
- 21.Zlowodzki M, Brink O, Switzer J, et al. The effect of shortening and varus collapse of the femoral neck on function after fixation of intracapsular fracture of the hip: A multi-centre cohort study. J Bone Joint Surg (Br) 2008;90:1487–94. doi: 10.1302/0301-620X.90B11.20582. [DOI] [PubMed] [Google Scholar]