Supplemental Digital Content is available in the text
Keywords: acute intestinal ischemia, D-dimer, diagnostic accuracy, meta-analysis
Abstract
Objective:
The purpose of this meta-analysis is to comprehensively assess the accuracy of serum D-dimer for the diagnosis of acute intestinal ischemia.
Methods:
Diagnostic studies of D-dimer for accurate diagnosis of acute intestinal ischemia were extracted from 6 databases, and prospective and retrospective studies that provided adequate data on sensitivity and specificity were included here. Sensitivity, positive likelihood ratio (PLR), negative likelihood ratio (NLR), and diagnostic odds ratio (DOR) were calculated. The overall diagnostic performance of D-dimer was assessed by plotting a summary receiver operating characteristic curve (SROC) and calculating the area under the curve (AUC).
Results:
A total of 1300 patients with suspected acute intestinal ischemia from 12 studies met the inclusion criteria. The combined sensitivity, specificity, PLR, NLR, and DOR were 0.94 (95% CI: 0.87–0.97), 0.50 (95% CI: 0.40–0.61), 1.9 (95% CI: 1.5–2.3), 0.12 (95% CI: 0.05–0.26), and 16 (95% CI: 7–39), respectively. The AUC was 0.81 (95% CI: 0.78–0.84).
Conclusion:
The results of this meta-analysis suggested that plasma D-dimer detection might be a useful means of identifying patients with acute intestinal ischemia of the abdomen.
1. Introduction
Acute intestinal ischemia is potentially fatal when it occurs in the abdomen, with 67% to 80% mortality as the disease progresses.[1] The numerous causes of acute intestinal ischemia includes arteriovenous thrombosis, arterial embolism, exogenous mesenteric vascular compression, and disproportionate mesenteric vasoconstriction.[2,3] The delayed diagnosis may lead to intestinal necrosis, septic shock, and multiple organ failure, which is life threatening in the acute intestinal ischemia patients. Clinically, accurate diagnosis of acute intestinal ischemia is very difficult even for a highly experienced physician. It is often diagnosed only after being found intraoperatively. Sensitivity and specificity of spiral computed tomography (CT) for the detection of acute mesenteric ischemia are 93.3% and 95.9%, respectively.[4] However, misdiagnosed cases may occur.[5,6] In recent years, some researchers have shown that serum markers such as D-dimer, intestinal fatty acid-binding protein (I-FABP), D-lactate, diaminoxidase (DOA), and citrulline facilitate the diagnosis of acute intestinal ischemia, with considerable accuracy.[3,7,8]
The D-dimer is a cross-linked fibrin degradation product [9] and a highly effective diagnostic tool for deep vein thrombosis, pulmonary embolism, aortic dissection, and other vascular diseases.[10–12] A number of case–control studies have assessed the accuracy of plasma D-dimer for the diagnosis of acute intestinal ischemia in the past decade.[13–35] The reported results have been inconsistent, with the sensitivity varying from 60% to 100% and the specificity ranging from 40% to 90%. Only 2 systematic reviews and meta-analyses have focused on the diagnosis of acute intestinal ischemia using plasma markers are available.[3,36] However, these 2 reports included only a few studies (3[3] and 5,[36] respectively), which limited the reliability and accuracy of the combined sensitivity and specificity results. Here, a meta-analysis was used to summarize the diagnostic studies of acute intestinal ischemia using D-dimer from 6 databases to confirm the accuracy of the diagnosis and to provide more reliable basis for clinical applications.
2. Methods
2.1. Ethical approval
The Medical Ethics Committee of Second Affiliated Hospital of Kunming Medical University informed us that ethical approval was not required. Because the data in the study were retrospective, which were extracted from different studies.
2.2. Data retrieval strategy
This study comprehensively explored the clinical studies (without language restriction) from PubMed, Medline (Ovid), Cochrane Library, the Wily Online Library, Web of Science, and China National Knowledge Infrastructure (CNKI) databases through September 28, 2016. The terms for data browsing included free words and MeSH keywords, including variations of intestine or mesentery (e.g., “intestines,” “intestinal,” “bowel,” “gut,” “mesentery, “mesaraic,” and “mesenteric”), alone, or in combination with various forms of ischemia (e.g., “ischemia,” “ischemic,” and “reperfusion”). These terms were searched individually and in combination (e.g., using “AND” to perform combined search between “sensitivity,” “specificity,” “false positive,” “false negative,” “accuracy,” “predictive value of tests,” “likelihood ratio,” “reference values,” “roc analysis,” and “D-dimer,” and “D-D”). Other forms of related literature were obtained by manually retrieving reference literature and related reviews.
2.3. Criteria for inclusion and exclusion studies
Only original studies were considered for inclusion in this meta-analysis, with the following inclusion criteria: original studies that evaluated D-dimers for the diagnosis of intestinal ischemia; each of the studies included >10 blood samples; and each of the studies provided true positive (TP), false positive (FP), true negative (TN), and false negative (FN) data or sufficient data for creating 2 × 2 tables. Exclusion criteria of this meta-analysis were as follows: studies that did not report accuracy or sensitivity of D-dimers; studies without reference standards for the definition of acute intestinal ischemia diagnosis; studies with methodological errors; and studies that did not report cut-off values. Criteria for the diagnosis of intestinal ischemia were the patients with obvious clinical symptoms such as acute abdominal pain, frequent nausea, vomiting, intestinal obstruction, and hypoactive or absent bowel sounds, which were supported by pathological, radiological, and intraoperative evidence.[37]
2.4. Data extraction and quality evaluation
Duplicate works were removed from the imported literature using literature management software. Two investigators preliminarily and independently screened the literature based on the index. Studies whose inclusion or exclusion were contested were verified after the discussion with a third party researcher. General information (e.g., first author's name, gender and age of the test subjects, and year and country of publication) and D-dimer-related information (e.g., detection method, cut-off value, sensitivity, and specificity) of each of the extracted study were listed in a standard form.
Two investigators independently used a methodological evaluation tool for diagnostic study, QUADAS (Quality Assessment of Diagnostic Accuracy Studies included in systematic reviews), to evaluate the quality of the included studies.[38] QUADAS is a systematic review tool for diagnostic studies in evidence-based medicine. It includes 14 items and can give a maximum score of 14[38] (Table S1).
2.5. Data analysis
The diagnostic accuracy of this meta-analysis was based on a previous study by the present team, Sun et al,[37] and studies of Leeflang et al[39] and Jones et al[40] Sensitivity, specificity, PLR, NLR, positive predictive value, negative predictive value, DOR, and 95% confidence interval (CI) were calculated based on the accuracy data (TP, TN, FP, and FN) extracted from each included study. Meta-Disc 1.4 software (XI Cochrane Colloquium, Barcelona, Spain) was used to calculate the Spearman correlation coefficient to evaluate the heterogeneity generated by the threshold effect. The threshold effect is the difference in sensitivity and specificity because of different cut-off values used according to different definitions of positive test results in different studies. If the analysis showed that the Spearman correlation coefficient to be strong and positive and P <0.05, the results indicated a significant threshold effect. Then, the chi-square-based Q test and inconsistency index I2 were used to detect the nonthreshold-induced heterogeneity. If the results of Q test showed that P <0.05 or I2 >50%, the included studies were believed to have significant heterogeneity. For the included studies with significant heterogeneity, the DerSimonian Laird method was used to calculate the estimated value.[41] Meta-regression was used to explore the source of heterogeneity. The Deek's funnel plot was used to detect the publication bias[42]; P <0.05 was considered indicative of the presence of publication bias. Despite the analysis of threshold effect, other analyses were performed using STATA 13.1 software (Stata Corporation, College Station, TX).
3. Results
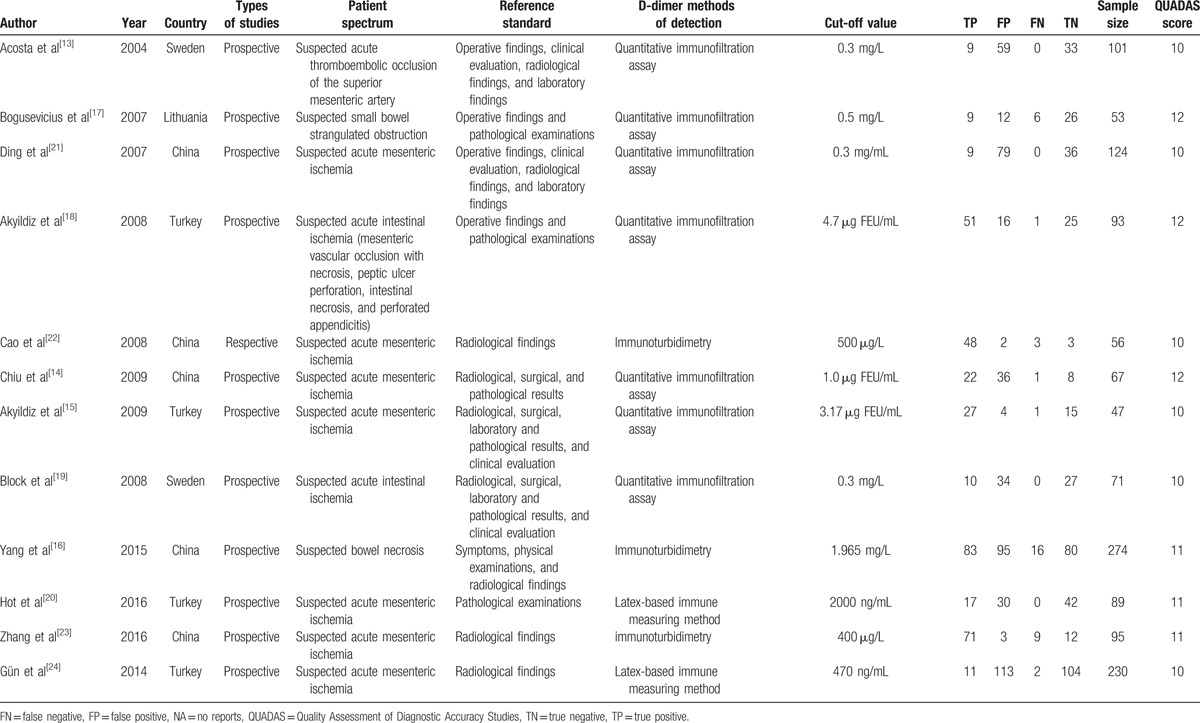
After removal of duplicate publications, the aforementioned browsing strategy was used to identify 82 reported studies. By screening the titles and abstracts, 39 studies were excluded. Then 22 potentially relevant documents remained. For a variety of reasons, 11 reported studies out of the 22 were excluded[25–35] (Fig. 1). Among the 11 excluded studies,[25–35] 6 did not report the sensitivity and specificity of D-dimer[25–30]; 2 were duplicate reports[31,32]; 1 had no definition of diagnostic criteria for acute intestinal ischemia[33]; 1 did not describe the method by which the D-dimer was detected[34]; and 1 did not report the cut-off values of D-dimer[35] Only 12 studies were eventually included in this meta-analysis,[13–24] with the years of publication ranging from 2004 to 2016 and including 1300 patients with suspected acute intestinal ischemia. Only 1 of them was a retrospective study,[22] and the others were prospective studies.[13–21,23,24] Five of the included studies were conducted in Asia,[14,16,21–23] and the remaining 7 included studies were conducted in European countries.[13,15,17–20,24] The types of acute intestinal ischemia in the 12 included studies were reported differently. There were 8 studies of acute mesenteric ischemia,[13–15,20–24] 1 study of acute strangulated intestinal obstruction,[17] 1 study of acute intestinal necrosis,[16] and 2 studies of mixed type of acute intestinal ischemia.[18,19] Diagnostic criteria for acute intestinal ischemia included pathological examinations, intraoperative findings, radiological examination, laboratory test results, and clinical evaluation (Table 1). Most of the studies included here used an immunofiltration assay to detect D-dimer[13–15,17–19,21]: 3 studies used immunoturbidimetry[16,22,23] and 2 studies used Latex-based immune measuring method.[20,24] Supplementary Table S1, summarizes the results of quality evaluation.
Figure 1.
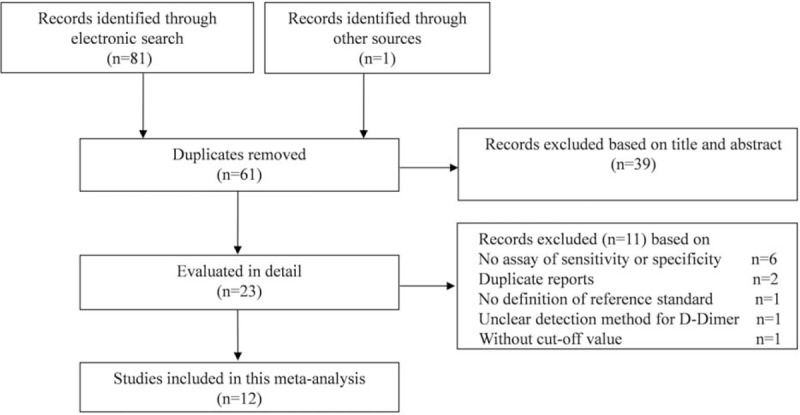
Summary of evidence search and selection.
Table 1.
Characteristics of the included studies.
3.1. Accuracy of plasma D-dimer for the diagnosis of acute intestinal ischemia
Different cut-off values used different studies resulted in the differences of sensitivity and specificity, namely threshold effect. The Spearman correlation coefficient and P values were used in this study to evaluate the threshold effect. The Spearman correlation coefficient of 0.088 and the P value of 0.787 suggested that there was not enough evidence to support the heterogeneity from the threshold effect. The combined sensitivity and specificity of D-dimer diagnosis of acute intestinal ischemia were 0.94 (95% CI: 0.87–0.97) and 0.50 (95% CI: 0.40–0.61), respectively (Fig. 2). The combined positive likelihood ratio (PLP) and negative likelihood ratio (NLR) of plasma D-dimer were 1.9 (95% CI: 1.5–2.3) and 0.12 (95% CI: 0.05–0.26), respectively. The combined diagnostic odds ratio (DOR) of plasma D-dimer was 16 (95% CI: 7–39; Table S2). The area under the curve (AUC) of the summary receiver operating characteristic curve (SROC) was 0.81 (95% CI: 0.78–0.84; Fig. 3), suggesting a high diagnostic accuracy of D-dimer for acute intestinal ischemia.
Figure 2.
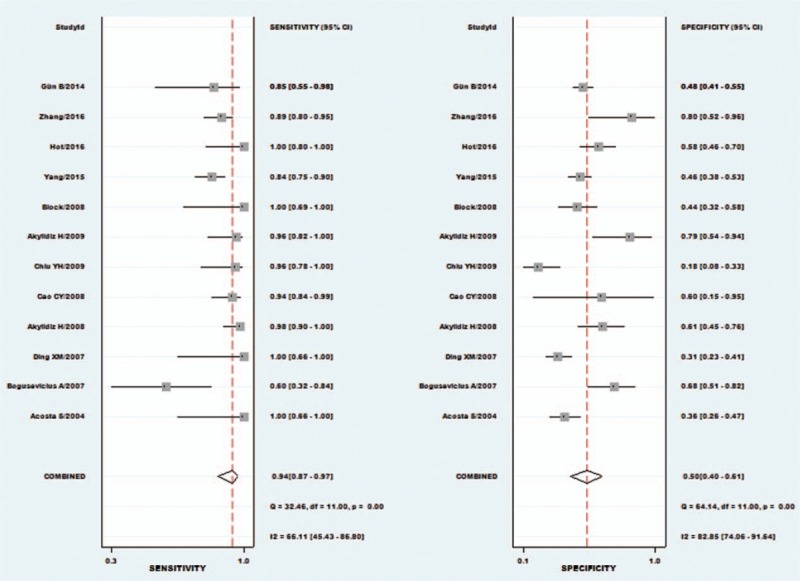
Forest plot of sensitivity and specificity of serum D-dimer.
Figure 3.
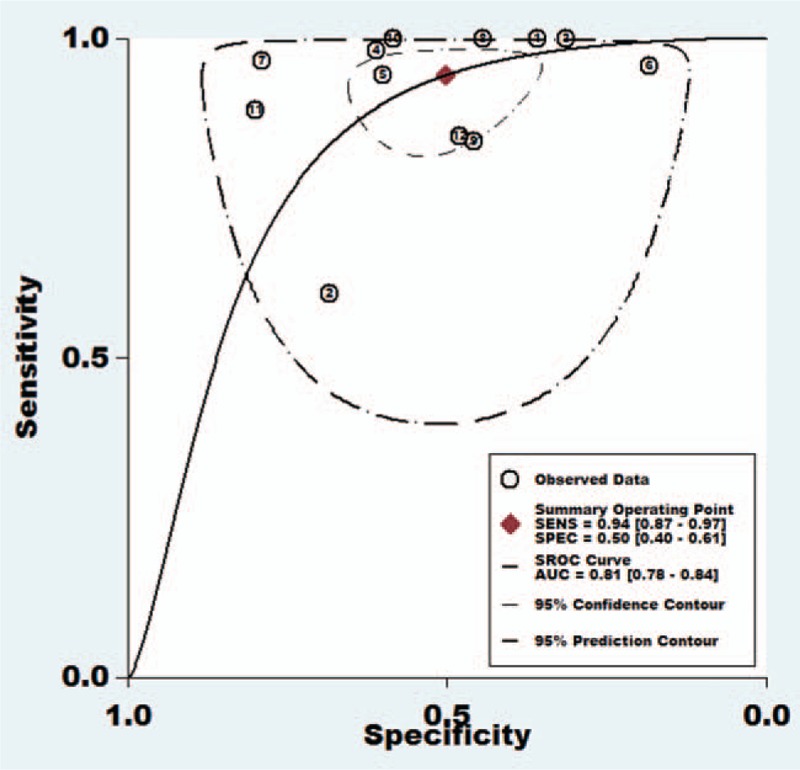
Summary operative receiver characteristic curve indicated high diagnostic accuracy.
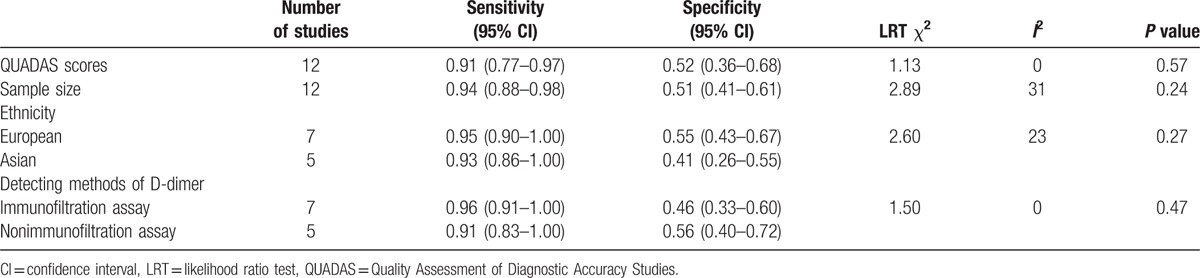
3.2. Meta-regression analysis
According to the forest plots (Fig. 2, S1, and S2), the accuracy for heterogeneity (sensitivity, specificity, PLR, NLR, and DOR) was significant. Meta-regression was performed to investigate the source of heterogeneity, which included continuous variables (QUADAS score and sample size) and dichotomous variables (the continent, such as Asia and Europe; and D-dimer detection assay, such as immunofiltration assay and nonimmunofiltration assay). However, there has not been sufficient evidence to support any association between these variables and the source of heterogeneity (Table 2 and Fig. S3).
Table 2.
Meta-regression results.
3.3. Analyses of sensitivity and publication bias
Sensitivity analysis of the prospective study (a retrospective study was excluded[22]) and only studies of acute mesenteric ischemia (4 studies of mixed types of acute intestinal ischemia and nonmesenteric ischemia were excluded[16–19]) showed similar findings between the combined results and the total analysis (Table S2). Deek's funnel plot was used to assess the publication bias, and the results showed no significant publication bias in this study (P = 0.247 [> 0.05]; Fig. S4). The clinical utility of D-dimer is shown in Fig. S5.
4. Discussion
Although the presence of acute intestinal ischemia can be verified intraoperatively, in pathology, and with angiography, rapid and accurate diagnosis of emergency cases of acute intestinal ischemia of the abdomen is often very difficult. Detection of plasma D-dimer concentration is a more feasible alternative method with minimal invasiveness. Increasing numbers of researchers have studied the diagnostic feasibility of D-dimer in acute intestinal ischemia.[13–35] However, reports of the diagnostic accuracy and specificity of D-dimer for acute intestinal ischemia remains inconsistent; and some studies have not adequately reported the results.[25–35] Summarizing and integrating the existing evidence might help clinicians to apply this method for clinical diagnosis and treatment.
This meta-analysis is the first to determine the diagnostic accuracy of D-dimer for acute intestinal ischemia. The combined sensitivity and specificity of plasma D-dimer assay were 0.94 (95% CI: 0.87–0.97) and 0.50 (95% CI: 0.40–0.61), respectively. In addition, the AUC of 0.81 and DOR of 16 suggested that D-dimer had high diagnostic accuracy for acute intestinal ischemia.
Heterogeneity is an unavoidable challenge to the result interpretation in meta-analysis. The I2 results of the combined sensitivity, specificity, PLR, NLR, and DOR suggested that this study had significant heterogeneity. In the diagnostic studies, the threshold effect produced different cut-off values. Here, the threshold effect is first considered as the primary source of heterogeneity. The differences in detection methods, the effectiveness of different reagent kits, and the differences in testing equipment and operating procedures affect the detection results of D-dimer. For these reasons, we used Spearman correlation analysis to detect the threshold effect. The Spearman correlation coefficient of 0.088 (P = 0.787) did not support the heterogeneity resulting from the threshold effect. Meta-regression was performed, and some possible causes of heterogeneity, including race, QUADAS score, sample size, and D-dimer detection methods, were included. Unfortunately, the results of meta-regression did not indicate that these variables were the source of heterogeneity. Importantly, patient's age was found to affect the D-dimer concentration. Some recent studies on pulmonary embolism and deep venous thrombosis[43,44] used patient's age to adjust the cut-off value of D-dimer and showed that it could increase the sensitivity and specificity of D-dimer. Some of the studies included did not report the age range in detail. Some studies did not even reported the age,[15,16,24] and thus, the subgroup analysis could not be performed. Age-adjusted D-dimer cut-off values can be used in future studies to evaluate the diagnostic accuracy of D-dimer for acute intestinal ischemia.
Because acute intestinal ischemia includes both vascular and nonvascular causes, most previous studies of D-dimer have focused on the vascular diseases.[10–12] Sensitivity analysis included only vascular acute intestinal ischemia, and the results were similar to the meta-analysis of other vascular diseases[10,12], whereas only 2 of the included studies of nonvascular acute intestinal ischemia were involved in evaluation of the diagnostic effect of the D-dimer.[16,17] That was not enough to perform subgroup analysis. Similarly, the only 2 studies of mixed vascular and nonvascular-induced acute intestinal ischemia included in this meta-analysis both included subgroup analysis.[18,19] Therefore, all data, which was not available for the determination of diagnostic accuracy of D-dimer for nonvascular acute intestinal ischemia, will require further studies for verification.
The limitations of this meta-analysis include the following: first, disunity of diagnostic reference standard for acute intestinal ischemia (e.g., pathological examinations, intraoperative findings, radiological examinations, laboratory tests, and clinical assessment). Although the pathological examinations were the most ideal diagnostic criteria, the implementation under emergency conditions was almost impossible. Therefore, the majority of studies used radiological examinations (e.g., CT angiography), laboratory tests, and even clinical assessment as the diagnostic criteria for acute intestinal ischemia, which may have caused overestimation of the diagnostic accuracy of the D-dimer; second, the studies used D-dimer detection assays and cut-off values different from each other, which affected the assessment of diagnostic accuracy; third, more than half of the studies had small sample size (<100 cases), which could have caused overestimation of the diagnostic accuracy of D-dimer for acute intestinal ischemia. Although in the present meta-regression, sample size was the only variable for the analysis, the results showed that sample size did not have much impact on the outcomes. Nevertheless, a large sample, multicenter, high-quality study may be necessary for further verification; fourth, given patients ages affecting the D-dimer detection results. However, most of the studies included here did not include age stratification analysis and did not even report the age range of the patients, so it was not possible to perform subgroup analysis in this study. Thus, it is necessary to consider age an important factor in the future studies.
Despite the limitations of this meta-analysis, the present data supported that D-dimer had the sufficient diagnostic value for the identification of acute intestinal ischemia from acute abdomen in the emergency department. However, this result will need further validation in a high-quality, large-sample, multi-center clinical study.
Supplementary Material
Footnotes
Abbreviations: AUC = area under the curve, CI = confidence interval, DOA = diaminoxidase, DOR = diagnostic odds ratio, FN = false negative, FP = false positive, I-FABP = intestinal fatty acid-binding protein, included in systematic reviews, NLR = negative likelihood ratio, PLR = positive likelihood ratio, QUADAS = Quality Assessment of Diagnostic Accuracy Studies, SROC = summary receiver operating characteristic curve, TN = true negative, TP = true positive.
D-L Sun and S-M Li are co-first authors who contributed equally to this paper.
DLS, SML, WML, and PYX designed this study; DLS, YYC, QWX, YJL, YBS, YXQ, and WML searched databases and collected full-text papers; YYL, TY, LYA, KS, YXQ, and SML extracted and analyzed data; DLS, SML, WML, and PYX composed the manuscript.
Funding: This study was supported by the Foundation of Research Center for Surgical Clinical Nutrition in Yunnan Province and Professor Yang Hua Research Station in Yunnan Province.
The authors have no conflicts of interest to disclose.
Supplemental Digital Content is available for this article.
References
- [1].Martin B. Prevention of gastrointestinal complications in the critically ill patient. AACN Adv Crit Care 2007;18:158–66. [DOI] [PubMed] [Google Scholar]
- [2].Tilsed JV, Casamassima A, Kurihara H, et al. ESTES guidelines: acute mesenteric ischaemia. Eur J Trauma Emerg Surg 2016;42:253–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3].Evennett NJ, Petrov MS, Mittal A, et al. Systematic review and pooled estimates for the diagnostic accuracy of serological markers for intestinal ischemia. World J Surg 2009;33:1374–83. [DOI] [PubMed] [Google Scholar]
- [4].Yikilmaz A, Karahan OI, Senol S, et al. Value of multislice computed tomography in the diagnosis of acute mesenteric ischemia. Eur J Radiol 2011;80:297–302. [DOI] [PubMed] [Google Scholar]
- [5].Angelelli G, Scardapane A, Memeo M, et al. Acute bowel ischemia: CT findings. Eur J Radiol 2004;50:37–47. [DOI] [PubMed] [Google Scholar]
- [6].Kozuch PL, Brandt LJ. Review article: diagnosis and management of mesenteric ischemia with an emphasis on pharmacotherapy. Aliment Pharmacol Ther 2005;21:201–15. [DOI] [PubMed] [Google Scholar]
- [7].Crenn P, Messing B, Cynober L. Citrulline as a biomarker of intestinal failure due to enterocyte mass reduction. Clin Nutr 2008;27:328–39. [DOI] [PubMed] [Google Scholar]
- [8].Cakmaz R, Büyükaşik O, Kahramansoy N, et al. A combination of plasma DAO and citrulline levels as a potential marker for acute mesenteric ischemia. Libyan J Med 2013;8:1–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9].Perrier A, Desmarais S, Goehring C, et al. D-dimer testing for suspected pulmonary embolism in outpatients. Am J Respir Crit Care Med 1997;156:492–6. [DOI] [PubMed] [Google Scholar]
- [10].Watanabe H, Horita N, Shibata Y, et al. Diagnostic test accuracy of D-dimer for acute aortic syndrome: systematic review and meta-analysis of 22 studies with 5000 subjects. Sci Rep 2016;6:26893. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].vanEs N, van der Hulle T, van Es J, et al. Wells rule and D-dimer testing to rule out pulmonary embolism: a systematic review and individual-patient data meta-analysis. Ann Intern Med 2016;165:253–61. [DOI] [PubMed] [Google Scholar]
- [12].Geersing GS, Janssen KJ, Oudega R, et al. Excluding venous thromboembolism using point of care D-dimer tests in outpatients: a diagnostic meta-analysis. BMJ 2009;339:586–1586. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13].Acosta S, Nilsson TK, Björck M. D-dimer testing in patients with suspected acute thromboembolic occlusion of the superior mesenteric artery. Br J Surg 2004;91:991–4. [DOI] [PubMed] [Google Scholar]
- [14].Chiu YH, Huang MK, How CK, et al. D-dimer in patients with suspected acute mesenteric ischemia. Am J Emerg Med 2009;27:975–9. [DOI] [PubMed] [Google Scholar]
- [15].Akyildiz H, Akcan A, Oztürk A, et al. The correlation of the D-dimer test and biphasic computed tomography with mesenteric computed tomography angiography in the diagnosis of acute mesenteric ischemia. Am J Surg 2009;197:429–33. [DOI] [PubMed] [Google Scholar]
- [16].Yang K, Wang W, Zhang WH, et al. The combination of D-dimer and peritoneal irritation signs as a potential indicator to exclude the diagnosis of intestinal necrosis. Medicine (Baltimore) 2015;94:e1564. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [17].Bogusevicius A, Grinkevicius A, Maleckas A, et al. The role of D-dimer in the diagnosis of strangulated small-bowel obstruction. Medicina 2007;43:850–4. [PubMed] [Google Scholar]
- [18].Akyildiz H, Akcan A, Oztürk A, et al. D-dimer as a predictor of the need for laparotomy in patients with unclear non-traumatic acute abdomen. A preliminary study. Scand J Clin Lab Invest 2008;68:612–7. [DOI] [PubMed] [Google Scholar]
- [19].Block T, Nilsson TK, Björck M, et al. Diagnostic accuracy of plasma biomarkers for intestinal ischaemia. Scand J Clin Lab Invest 2008;68:242–8. [DOI] [PubMed] [Google Scholar]
- [20].Hot S, Duraker N, Sari A, et al. The value of D-dimer in diagnosis of acute mesenteric ischemia and differential diagnosis from acute pancreatitis and acute cholecystitis. Dic Med J 2016;43:88–92. [Google Scholar]
- [21].Ding XM, Zhang XC, Zhu LH, et al. Detection and clinical significance of plasma D-dimer in patients with suspected mesenteric artery ischemia. J Surg Concepts Pract (Chinese) 2007;12:72–3. [Google Scholar]
- [22].Cao CY, Fang JZ, Tang WH, et al. The combined application of plasma D-dimer detection and spiral CT angiography in the diagnosis of ischemic bowel disease. Zhejiang Med (Chinese) 2009;31:398–400. [Google Scholar]
- [23].Zhang RR, Wang Y, Gao H, et al. Value of plasma D-dimer in early diagnosis of acute ischemic bowel disease. Int J Lab Med(Chinese) 2016;37:2258–60. [Google Scholar]
- [24].Gün B, Yolcu S, Değerli V, et al. Multi-detector angio-CT and the use of D-dimer for the diagnosis of acute mesenteric ischemia in geriatric patients. Ulus Travma Acil Cerrahi Derg 2014;20:376–81. [DOI] [PubMed] [Google Scholar]
- [25].Acosta S, Björck M. Acute thrombo-embolic occlusion of the superior mesenteric artery: a prospective study in a well defined population. Eur J Vasc Endovasc Surg 2003;26:179–83. [DOI] [PubMed] [Google Scholar]
- [26].Tan WW, Zhang M. Clinical value of D-dimer for early diagnosis and severity of ischemic bowel disease. Lab Med Clin 2016;13:1497–9. [Google Scholar]
- [27].Wang ZM, Zhang YD, He JT. Clinical significance of C-reactive protein and D-dimer in diagnosis and prognosis of acute mesentedearte isehemia. J Hunan Normal Univ (Med Sci) (Chinese) 2013;10:48–50. [Google Scholar]
- [28].Ma C, Fang XD, Lu GQ, et al. Early diagnosis and treatment of the acute mesenteric ischemia disease. Chin J Lab Diagn (Chinese) 2000;4:262–4. [Google Scholar]
- [29].Ma C, Fang XD, Lu GQ, et al. Selective angiography and D-dimer examination in the diagnosis and treatment of acute mesenteric ischemia. Chin J Mod Med (Chinese) 2001;11:68–9. [Google Scholar]
- [30].Feng JB. The value of D-dimer in the diagnosis and prognosis of patients with ischemic bowel disease. Chin Med Pharm (Chinese) 2012;2:111–2. [Google Scholar]
- [31].Zhang XC, Zhang XC, Zhu LH, Shi L, D-dimer in early diagnosis of acute ischemic bowel disease, The Second Conference of Vascular Surgery in Jiangsu Province (Chinese), 2015, 42–4. [Google Scholar]
- [32].Ding XM, Zhang XC, Zhu LH, et al. D-dimer test in patients with suspected acute mesenteric artery ischemia. Clin Med Chin (Chinese) 2007;12:23–5. [Google Scholar]
- [33].Icoz G, Makay O, Sozbilen M, et al. Is D-dimer a predictor of strangulated intestinal hernia? World J Surg 2006;30:2165–9. [DOI] [PubMed] [Google Scholar]
- [34].Güzel M, Sözüer EM, Salt Ö, et al. Value of the serum I-FABP level for diagnosing acute mesenteric ischemia. Surg Today 2014;44:2072–6. [DOI] [PubMed] [Google Scholar]
- [35].Chen JP. Value of plasma D-dimer in early diagnosis of acute ischemic bowel disease. Med Innovat Chi(Chinese) 2015;12:48–50. [Google Scholar]
- [36].Cudnik MT, Darbha S, Jones J, et al. The diagnosis of acute mesenteric ischemia: a systematic review and meta-analysis. Acad Emerg Med 2013;20:1087–100. [DOI] [PubMed] [Google Scholar]
- [37].Sun DL, Cen YY, Li SM, et al. Accuracy of the serum intestinal fatty-acid-binding protein for diagnosis of acute intestinal ischemia: a meta-analysis. Sci Rep 2016;6:34371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [38].Whiting P, Rutjes AW, Reitsma JB, et al. The development of QUADAS: a tool for the quality assessment of studies of diagnostic accuracy included in systematic reviews. BMC Med Res Methodol 2003;3:25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [39].Leeflang MM, Deeks JJ, Gatsonis C, et al. Systematic reviews of diagnostic test accuracy. Ann Intern Med 2008;149:889–97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [40].Jones C, Ashrafian H, Skapinakis P, et al. Diagnostic accuracy meta-analysis: a review of the basic principles of interpretation and application. Int J Cardiol 2010;140:138–44. [DOI] [PubMed] [Google Scholar]
- [41].Higgins JP, Thompson SG, Deeks JJ, et al. Measuring inconsistency in meta-analyses. BMJ 2003;327:557–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [42].Deeks JJ, Macaskill P, Irwig L. The performance of tests of publication bias and other sample size effects in systematic reviews of diagnostic test accuracy was assessed. J Clin Epidemiol 2005;58:882–93. [DOI] [PubMed] [Google Scholar]
- [43].Righini M, Van Es J, Den Exter PL, et al. Age-adjusted D-dimer cutoff levels to rule out pulmonary embolism The ADJUST-PE Study. JAMA 2014;311:1117–24. [DOI] [PubMed] [Google Scholar]
- [44].Schouten HJ, Geersing GJ, Koek HL, et al. Diagnostic accuracy of conventional or age adjusted D-dimer cut-off values in older patients with suspected venous thromboembolism: systematic review and meta-analysis. BMJ 2013;346:964–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


