Supplemental Digital Content is available in the text
Keywords: femoral nerve block, liposomal bupivacaine, meta-analysis, total knee arthroplasty
Abstract
Background:
Periarticular anesthesia (PAI) with liposomal bupivacaine (LB) and femoral nerve block (FNB) were 2 common type of pain management after total knee arthroplasty (TKA). There is no consensus about PAI with LB shows better clinical outcome than FNB. Thus, we performed a systematic review and meta-analysis to compare the efficacy and safety of PAI with LB and FNB for patients prepared for TKA.
Methods:
Randomized controlled trials (RCTs) and non-RCTs from PubMed (1966-2017.2), EMBASE (1980-2017.2), and the Cochrane Central Register of Controlled Trials (CENTRAL, 2017.2), Web of Science (1966-2017.2), and Chinese Wanfang database (1980-2017.2) were searched. Continuous outcomes including visual analogue scale (VAS) at 24, 48, and 72 hours, total morphine consumption, length of hospital, and range of motion (ROM) were reported as the weighted mean difference with 95% and confidence interval (CI) and discontinuous outcomes (the occurrence of postoperative nausea and vomiting [PONV]) were presented as relative risk with 95% CI. Random-effects model was adopted to analyze the relevant data.
Results:
According to the inclusion and exclusion criteria, 8 studies with 2407 patients were eligible and finally included in this meta-analysis (LB = 1114, FNB = 1293). There was no significant difference between VAS at 24, 4, and 72 hours, ROM, and the occurrence of PONV between PAI with LB group versus FNB group (P > 0.05). Compared with the FNB group, PAI with LB was associated with a significant decrease in length of hospital stay by 0.43 day (MD = −0.43; 95% CI −0.60 to −0.27; P = 0.001) and the total dose of total morphine consumption by (MD = −29.32; 95% CI −57.55 to −1.09; P = 0.042).
Conclusions:
The review of trials found that PAI with LB provided a significant beneficial effect over FNB in improving the pain or decreased the total morphine consumption in patients who underwent TKA. However, PAI with LB associated with less LOS than FNB. More high quality RCTs are still needed to identify the effects and optimal dose of LB for pain management after TKA.
1. Introduction
Total knee arthroplasty (TKA) was regarded as an effective surgery for end-stage knee osteoarthritis or rheumatoid arthritis and most patients experience moderate to severe postsurgical pain.[1–3] Postoperative pain control management after TKA is still a concern as it relates to patients satisfaction and functional recovery.[4,5] Adequate postoperative pain management, enhances patient comfort and rapid return to expected functionality, was the current goal for TKA surgeons.[6] Numerous trials have estimated that inappropriate pain control after TKA was associated with a wide range of preventable and undesirable side effects.[7] Many anesthetic regimens and techniques have been explored to decrease postoperative pain and enhance the fast recovery after TKA.[8]
Previous reports have demonstrated that femoral nerve block (FNB) and periarticular anesthesia (PAI) with multimodal anesthetic were 2 alternatives for postoperative pain control.[9] The duration of pain control for FNB may last 48 hours postoperatively. However, FNB may reduce quadriceps muscle strength and results in an increased risk of falls.[10] PAI is another anesthetic technique to provide postoperative pain control while avoiding motor weakness.[11] Bupivacaine is a common and relative long action anesthetic agent for local anesthesia. However, the function time was limited and always lasted for 24 hours.[12] Liposomal bupivacaine (LB) was a prolonged-release formulation of bupivacaine from multivesicular liposomes and tried to administration for pain control after TKA.[13] The structure of LB allows for drug release over several days after administration into the surgical site. Wu et al[14] found that LB as a novel anesthetic formulation performs a positive role for pain control than bupivacaine. It is reported that LB can be released over 72 hours. Although many clinical trials about comparing PAI with LB with FNB for pain control after TKA have been published. There was no evidence revealed that PAI with LB shows better clinical outcome than FNB. Thus, we searched the electronic databases and performed a systematic review and meta-analysis to compare the clinical efficacy and safety of PAI with LB with FNB after TKA.
2. Materials and methods
2.1. Search strategy
Two reviewers (SQL and XC) systematically searched randomized controlled trials (RCTs) and non-RCTs that investigated the use of LB versus FNB for the treatment of postoperative pain after TKA from PubMed (1966-2017.2), EMBASE (1980-2017.2), and the Cochrane Central Register of Controlled Trials (CENTRAL, 2017.2), Web of Science (1966-2017.2), and Chinese Wanfang database (1980-2017.2). Search items in PubMed were shown in Supplement S1. There were no restrictions regarding publication language and date. We also manually retrieved reference lists from the identified studies and relevant review studies for additional studies. Two investigators (CCY and CWW) independently assessed the titles and abstracts of studies, and disagreement was settled by referring to a 3rd reviewer (YQW). A meta-analysis was extracted data from previous published papers and thus no ethic approval was performed.
2.2. Eligibility criteria and exclusion criteria
-
(1)
Participants: Only studies enrolling adult participants with a diagnosis of end-stage of knee osteoarthritis or rheumatoid arthritis and prepared for unilateral TKA.
-
(2)
Interventions: The intervention was administration PAI with LB for pain management after TKA.
-
(3)
Comparisons: The control group was only used an FNB for postoperative pain control.
-
(4)
Outcomes: VAS at 24, 48, and 72 hours, total morphine consumption, length of hospital stay, range of motion (ROM), and the occurrence of postoperative nausea and vomiting (PONV).
-
(5)
Study design: RCTs and non-RCTs were regarded as eligible in our study.
2.3. Data extraction and outcome measures
Two researchers (JCX and SHX) independently extracted the general characteristic and outcomes. Any discrepancy between the 2 authors was solved by discussion.
The primary outcomes measures of interest were VAS at 24, 48, and 72 hours, total morphine consumption, ROM, and length of hospital stay. The secondary outcomes measures comprised the occurrence of nausea. If the mean, standard deviation was not listed in the text, we extracted data from the diagrams by Get Data (version 2.25, Fedorov, China).[15] For a study with numerous doses, we divided the different dose as separate groups and calculated in the final meta-analysis.[15]
2.4. Risk of bias assessment
Two investigators independently measured all of the included studies in accordance to the Cochrane Handbook for Systematic Reviews of Interventions (version 5.3.0).[15] Each of the fields was determined as a low risk of bias, a high risk of bias, or an unclear risk of bias. The risk of bias summary and the risk of bias graph were obtained from Reviewer Manager 5.3.0 (The Cochrane Collaboration, Oxford, UK).
2.5. Statistical analysis
Continuous outcomes (VAS at 24, 48, and 72 hours, total morphine consumption, and the length of hospital stay) were expressed as the weighted mean differences with 95% confidence intervals (CIs). Discontinuous outcomes (the occurrence of PONV) were expressed as relative risk with 95% CI. Relevant data were analyzed by Stata software (version 12.0, Stata Corp., College Station, TX). The I2 value overpass 50% indicated that there was statistically heterogeneity between the studies. Funnel plots and Begg test were created to determine the presence of publication bias.[16] Kappa values were used to measure the degree of agreement between the 2 reviewers and the acceptable threshold value was set as 0.61.[17,18]P < 0.05 was set as the statistically different.
3. Results
3.1. Search results and quality assessment
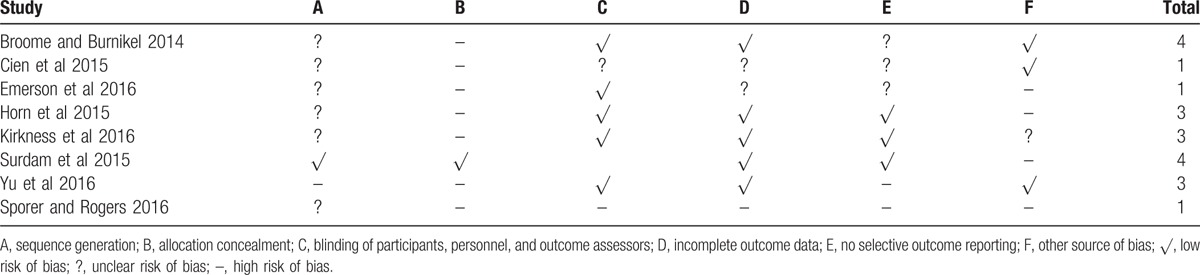
In the initial search, we identified 246 potentially relevant studies (PubMed = 102, EMBASE = 46, CENTRAL = 35, Chinese Wanfang database = 37, and Web of Science = 26), of which 15 duplicates were removed by Endnote Software (Version X7; Thomson Scientific; Connecticut). According to the inclusion criteria, 223 studies were excluded. Finally, we included 8 clinical trials (RCTs = 2 and non-RCTs = 6) with 2407 patients (LB = 1114, FNB = 1293) in the meta-analysis[19–26] (Fig. 1). The detailed information of the patients general characteristic can be seen in Table 1. Seven studies were published in USA and the rest 1 published in India. The quality assessment of included studies can be seen detail in Table 2. Only 1 study refers to the proper random sequence generation[24] and 6 studies were all referred to unknown risk of bias.[19–24,26] The study of Yu et al[25] is with high risk of bias for the random sequence generation.[25] The overall kappa value regarding the evaluation of risk of bias of included RCTs was 0.736, indicating an excellent degree of agreement between the 2 reviewers.
Figure 1.
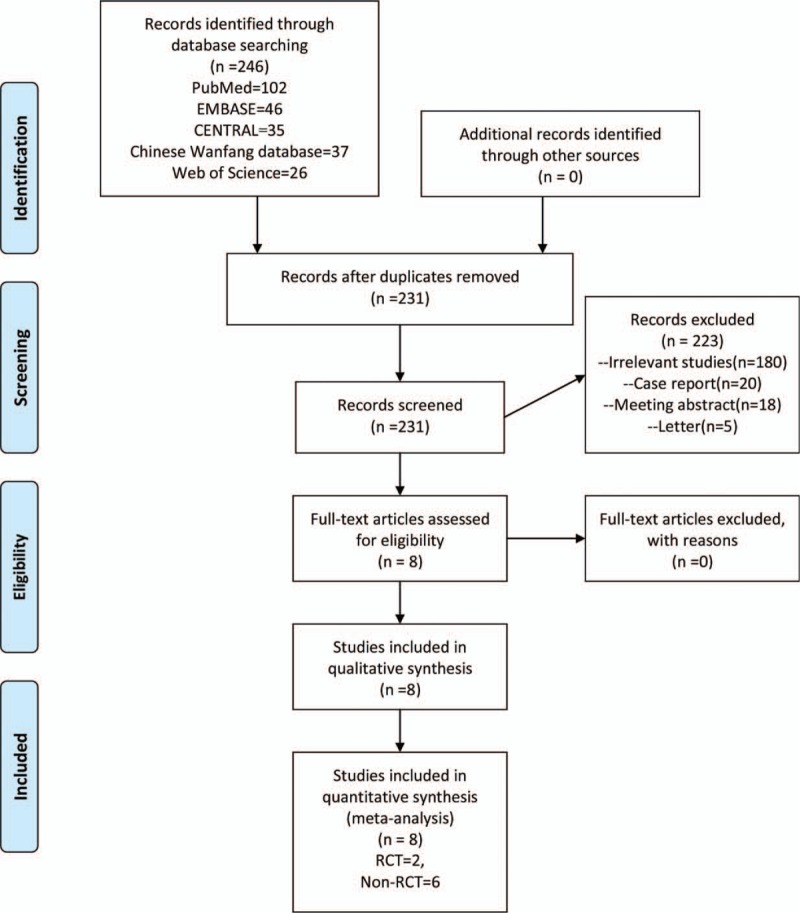
The PRISMA flow chart of retrieved studies.
Table 1.
The general characteristic of the included studies.
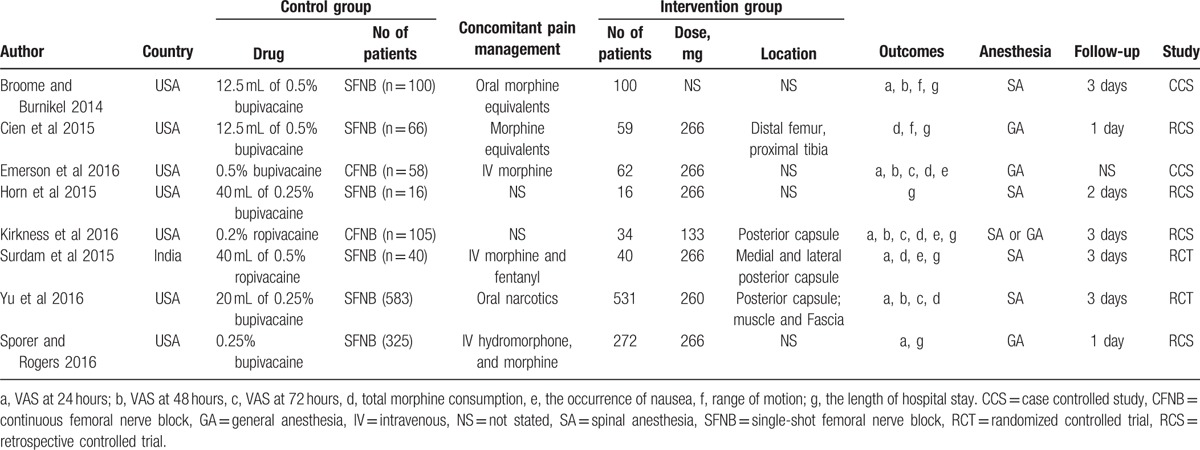
Table 2.
The risk of bias of the included studies.
3.2. Result of meta-analysis
3.2.1. VAS at 24, 48, and 72 hours
Data from 6 studies[19,21,23–26] involving 2250 patients were able to examine the VAS at 24 hours postoperatively; however, final results presented with a large heterogeneity (I2 = 91.5%, P = 0.000). Pooled results revealed that PAI with LB was associated with no superior than FNB in terms of VAS at 24 hours (MD = −3.02; 95% CI −8.55 to 2.51; P = 0.284, Fig. 2A). Funnel plot was then conducted to analyze the publication bias and results indicated that the number of literature is symmetrical and no publication bias was exist (Fig. 2 B). Begg test provided further evidence and showed no publication bias regarding effect of LB versus FNB on the VAS at 24 hours was existed (P = 0.087, Fig. 2C). The sensitivity analysis was then conducted to analyze the source of heterogeneity between the included studies. Result is shown in Fig. 2D. None of the included studies affect the final results.
Figure 2.
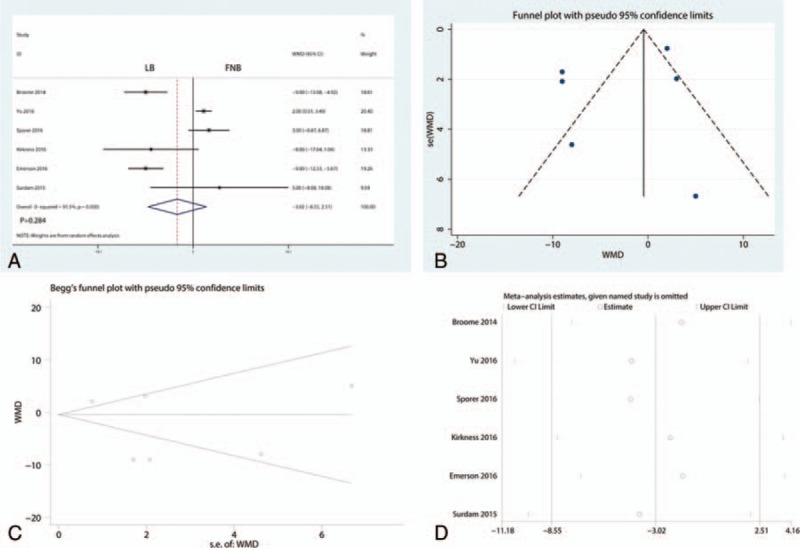
(A) Forest plot that comparing VAS at 24 hours between the 2 groups; (B) funnel plot of VAS at 24 hours; (C) Begg test for VAS at 24 hours; (D) sensitivity analysis for the VAS at 24 hours.
Five studies[19,21,23–25] with 1653 patients were used to carry out a meta-analysis on the VAS at 48 hours and final results revealed that there was no significant difference between VAS at 48 hours (MD = −4.16; 95% CI −8.76–0.43; P = 0.076, Fig. 3A). Meanwhile, included studies were with a large heterogeneity (I2 = 83.3%, P = 0.000) and thus a random-effect model was performed. Funnel plot was then conducted to analyze the publication bias and results indicated that the number of literature is symmetry and no publication bias was exist (Fig. 3B). The sensitivity analysis was then conducted to analyze the source of heterogeneity between the included studies. Result is shown in Fig. 3C. None of the included studies affect the final results.
Figure 3.
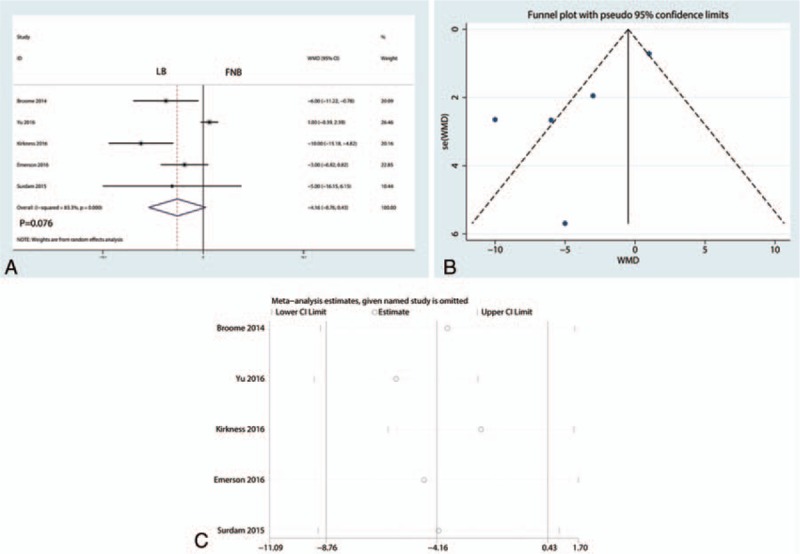
(A) Forest plot of the VAS at 48 hours; (B) funnel plot of VAS at 48 hours; and (C) sensitivity analysis of the VAS at 48 hours.
Only 3 studies[21,23,25] reported the VAS at 72 hours and pooled results indicated that PAI with LB has similar pain control at 72 hours (MD = −0.49; 95% CI −4.22–3.23; P = 0.795, Fig. 4A). Included studies presented with a large heterogeneity (I2 = 61.2%, P = 0.076). Funnel plot was then conducted to analyze the publication bias and results indicated that the number of literature is symmetry and no publication bias was exist (Fig. 4B). The sensitivity analysis was then conducted to analyze the source of heterogeneity between the included studies. Result is shown in Fig. 4C. None of the included studies affect the final results.
Figure 4.
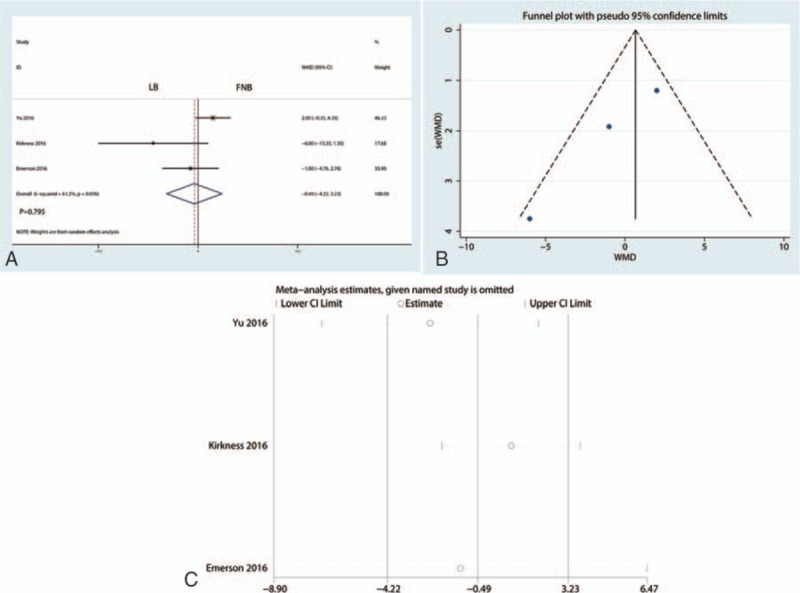
(A) Forest plot of the VAS at 72 hours; (B) funnel plot of VAS at 72 hours; (C) sensitivity analysis of the VAS at 72 hours.
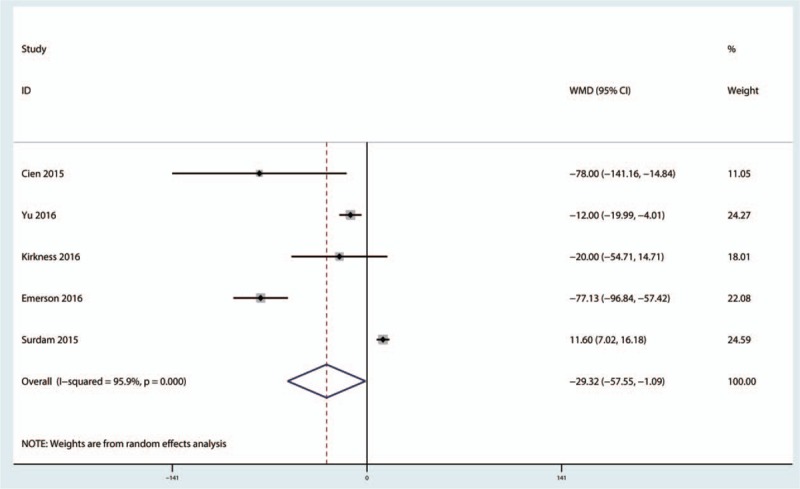
3.2.2. Total morphine consumption
Five studies[19,21,23–25] addressed the total morphine consumption between LB group and FNB group. There was a high heterogeneity between the included studies (I2 = 95.9%, P = 0.000) and thus a random-model was performed. The results indicated that there was no significant difference between LB and FNB group in terms of total morphine consumption (MD = −29.32; 95% CI −57.55 to −1.09; P = 0.042, Fig. 5).
Figure 5.
Forest plot that comparing total morphine consumption between the 2 groups.
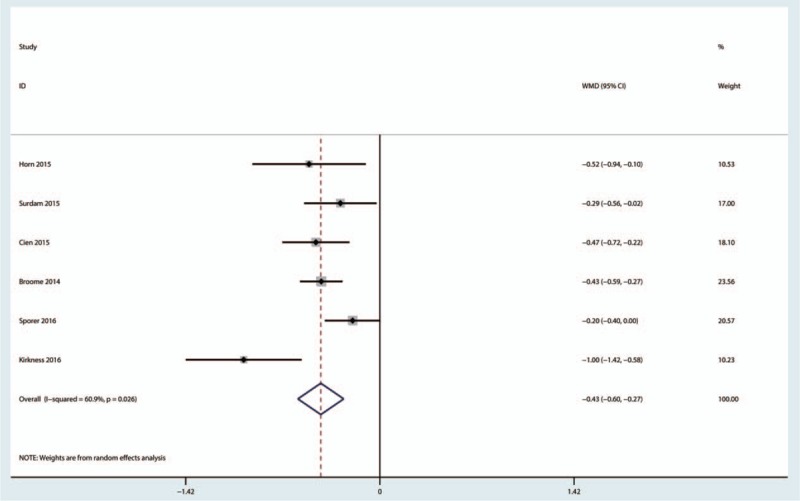
3.2.3. Length of hospital stay
A total of 5 studies[12,19,20,22–24] with 1173 patients addressed the length of hospital between PAI with LB and FNB group. The results indicated that PAI with LB was associated with less length of hospital stay compared with FNB (MD = −0.43; 95% CI −0.60 to −0.27; P = 0.001, Fig. 6) with high heterogeneity (I2 = 60.9%, P = 0.026).
Figure 6.
Forest plot that comparing the length of hospital stay between the 2 groups.
3.2.4. Range of motion
A total of 2 studies[19,24] with 280 patients addressed the ROM between PAI with LB group and FNB group. The results indicated that there was no significant difference between the PAI with LB group with FNB group in terms of ROM (MD = 1.07; 95% CI −14.61–16.75; P = 0.894, Fig. 7) with high heterogeneity (I2 = 96.6%, P = 0.000).
Figure 7.
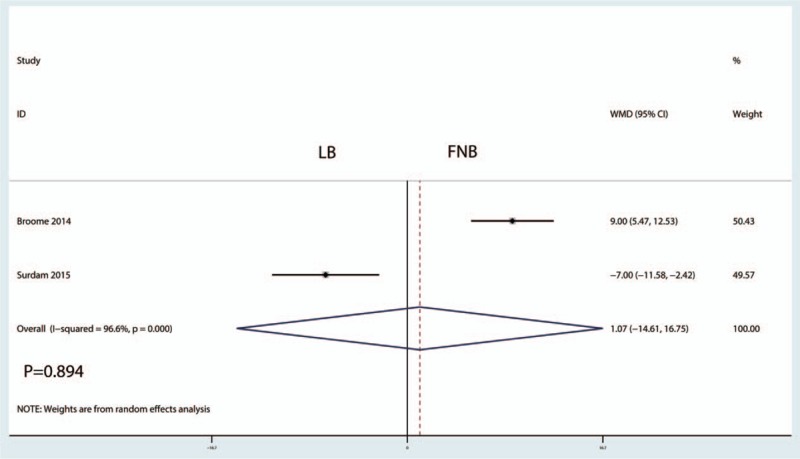
Forest plot that comparing the range of motion between the 2 groups.
3.2.5. The occurrence of PONV
Eight studies involving 339 patients paid close attention to the PONV. The meta-analysis indicated that there was no significant difference between LB group versus FNB group (relative risk, 0.68; 95%CI 0.34–1.34, P = 0.268, Fig. 8) with a low heterogeneity (I2 = 0.0%, P = 0.617).
Figure 8.
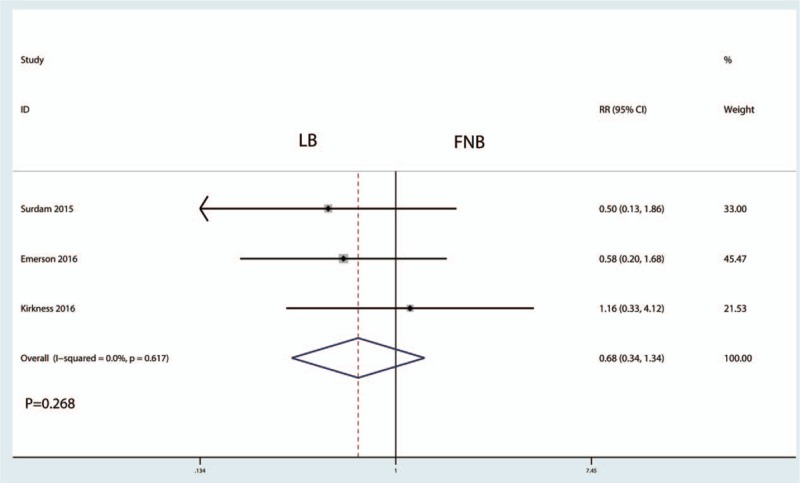
Forest plot that comparing the occurrence of PONV between the 2 groups.
4. Discussion
The results of this meta-analysis indicated that PAI with LB associated with equal pain relief and morphine-sparing effects compared to FNB after TKA. However, LOS in the group of PAI with LB was decreased than FNB group. There was no significant difference between the occurrence of nausea and ROM of the knee. A major strength of the current analysis is the comprehensive search with strict statistical calculations. After comprehensive search, 8 clinical trials (2 RCTs and 6 non-RCTs) with 2407 patients were finally included in this meta-analysis. The quality of the included studies is limited and thus the final results should be treated cautiously. Although a previous meta-analysis was published, but the analysis did not include all available studies.[20] And the ROM between the PAI with LB and FNB group was not compared.
Recently, attention has arisen to the PAI with multimodal anesthetic drugs as it is an easy, relatively safe alternative to decrease the postoperative pain without sacrificing the muscle strength.[27] And when compared with FNB, PAI did not decrease the muscle strength and thus the occurrence of fall is decreased.[9] However, the relative short duration of anesthesia of PAI limited for popularized application. The half-lives of bupivacaine is 3.5 hours and thus the function time is limited.[28] LB encapsulated bupivacaine into multivesicular liposomes, resulting in a slow and controlled release bupivacaine. And this novel long-acting local anesthetic agent was to administration in the surgical site for postoperative pain control.[29] Final results showed that PAI with LB has equal pain relief and morphine-sparing effects with FNB in the 72 hours after TKA. The effects of PAI with LB after TKA are in debated in the published papers. Wu et al[14] preferred LB than standard bupivacaine due to the long duration anesthesia effects. However, Singh et al[30] revealed that the anesthetic effects of LB infiltration need to further identified.
The morphine-sparing effects of PAI with LB and FNB were similar and with statistically significant (MD = −29.32; 95% CI −57.55 to −1.09; P = 0.042). Morphine is a supplement anesthesia for patients who could not tolerate the postoperative pain. The pain intensity between the included studies is equivalent and thus the supplement morphine consumption is also equivalent. The occurrence of nausea was also the common complication of morphine and the difference also with no statistically significant (P > 0.05). And the ROM between PAI with LB and FNB groups was also with no statistically significant (P > 0.05).
Present meta-analysis indicated that LB was associated with shorter length of hospital stay than FNB (MD = −0.43; 95% CI −0.60 to −0.27; P = 0.001). This outcome is inconsistent with previous meta-analysis (SMD = 0.207, 95%CI 0.095–0.319).[30] FNB may delay discharge period due to the motor weakness. Sharma et al[31] recently reported that FNB after TKA is associated with quadriceps weakness and higher rate of postoperative falls, thus delaying patient discharge. When comparing LB with standard bupivacaine, there was no significant difference between the lengths of hospital stay.[30]
There were a total of 4 limitations in this meta-analysis: non-RCTs were included and may have potential selective bias; different volume and dose of LB may provide the heterogeneity between the included studies; continuous FNB and single-shot FNB has potential heterogeneity between included studies; and different drugs for FNB in the included studies may cause the heterogeneity.
5. Conclusions
Present meta-analysis indicated that PAI with LB provided a significant beneficial effect over FNB in improving the pain or decreased the total morphine consumption in patients who underwent TKA. However, PAI with LB associated with less length of hospital stay than FNB. More high quality RCTs are still needed to identify the effects and optimal dose of LB for pain management after TKA.
Supplementary Material
Footnotes
Abbreviations: LB = liposomal bupivacaine, FNB = femoral nerve block, TKA = total knee arthroplasty, CI = confidence interval, PONV = postoperative nausea and vomiting, PAI = periarticular anesthesia, RCT = randomized controlled trial, ROM = range of motion.
The authors have no funding and conflicts of interest to disclose.
Supplemental Digital Content is available for this article.
References
- [1].Wylde V, Rooker J, Halliday L, et al. Acute postoperative pain at rest after hip and knee arthroplasty: severity, sensory qualities and impact on sleep. Orthop Traumatol Surg Res 2011;97:139–44. [DOI] [PubMed] [Google Scholar]
- [2].Sun XL, Zhao ZH, Ma JX, et al. Continuous local infiltration analgesia for pain control after total knee arthroplasty: a meta-analysis of randomized controlled trials. Medicine 2015;94:e2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3].Hamilton TW, Strickland LH, Pandit HG. A meta-analysis on the use of gabapentinoids for the treatment of acute postoperative pain following total knee arthroplasty. J Bone Joint Surg Am 2016;98:1340–50. [DOI] [PubMed] [Google Scholar]
- [4].Shin HJ, Soh JS, Lim HH, et al. In-plane three-step needle insertion technique for ultrasound-guided continuous femoral nerve block after total knee arthroplasty: a retrospective review of 488 cases. Korean J Anesthesiol 2016;69:587–91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].Zhai L, Song Z, Liu K. The effect of gabapentin on acute postoperative pain in patients undergoing total knee arthroplasty: a meta-analysis. Medicine 2016;95:e3673. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].Li J, Deng X, Jiang T. Combined femoral and sciatic nerve block versus femoral and local infiltration anesthesia for pain control after total knee arthroplasty: a meta-analysis of randomized controlled trials. J Orthop Surg Res 2016;11:158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7].Cherian JJ, Muzaffar A, Barrington JW, et al. Liposomal bupivacaine in total knee arthroplasty for better postoperative analgesic outcome and economic benefits. J Knee Surg 2016;29:e2. [DOI] [PubMed] [Google Scholar]
- [8].Cip J, Erb-Linzmeier H, Stadlbauer P, et al. Continuous intra-articular local anesthetic drug instillation versus discontinuous sciatic nerve block after total knee arthroplasty. J Clin Anesth 2016;35:543–50. [DOI] [PubMed] [Google Scholar]
- [9].Lefevre N, Klouche S, de Pamphilis O, et al. Peri-articular local infiltration analgesia versus femoral nerve block for postoperative pain control following anterior cruciate ligament reconstruction: prospective, comparative, non-inferiority study. Orthop Traumatol Surg Res 2016;102:873–7. [DOI] [PubMed] [Google Scholar]
- [10].Dong CC, Dong SL, He FC. Comparison of adductor canal block and femoral nerve block for postoperative pain in total knee arthroplasty: a systematic review and meta-analysis. Medicine 2016;95:e2983. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].Albrecht E, Guyen O, Jacot-Guillarmod A, et al. The analgesic efficacy of local infiltration analgesia vs femoral nerve block after total knee arthroplasty: a systematic review and meta-analysis. Br J Anaesth 2016;116:597–609. [DOI] [PubMed] [Google Scholar]
- [12].Sporer SM, Rogers T. Postoperative pain management after primary total knee arthroplasty: the value of liposomal bupivacaine. J Arthroplasty 2016;31:2603–7. [DOI] [PubMed] [Google Scholar]
- [13].Sakamoto B, Keiser S, Meldrum R, et al. Efficacy of liposomal bupivacaine infiltration on the management of total knee arthroplasty. JAMA Surg 2016;152:90–5. [DOI] [PubMed] [Google Scholar]
- [14].Wu ZQ, Min JK, Wang D, et al. Liposome bupivacaine for pain control after total knee arthroplasty: a meta-analysis. J Orthop Surg Res 2016;11:84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].Higgins JPT GS. Cochrane handbook for systematic reviews of interventions version 5.1.0. 2011; [http://www.cochrane-handbook.org]. [Google Scholar]
- [16].Macaskill P, Walter SD, Irwig L. A comparison of methods to detect publication bias in meta-analysis. Stat Med 2001;20:641–54. [DOI] [PubMed] [Google Scholar]
- [17].Landis JR, Koch GG. An application of hierarchical kappa-type statistics in the assessment of majority agreement among multiple observers. Biometrics 1977;33:363–74. [PubMed] [Google Scholar]
- [18].Landis JR, Koch GG. The measurement of observer agreement for categorical data. Biometrics 1977;33:159–74. [PubMed] [Google Scholar]
- [19].Broome CB, Burnikel B. Novel strategies to improve early outcomes following total knee arthroplasty: a case control study of intra articular injection versus femoral nerve block. Int Orthop 2014;38:2087–9. [DOI] [PubMed] [Google Scholar]
- [20].Cien AJ, Penny PC, Horn BJ, et al. Comparison between liposomal bupivacaine and femoral nerve block in patients undergoing primary total knee arthroplasty. J Surg Orthop Adv 2015;24:225–9. [PubMed] [Google Scholar]
- [21].Emerson RH, Jr, Barrington JW, Olugbode O, et al. Femoral nerve block versus long-acting wound infiltration in total knee arthroplasty. Orthopedics 2016;39:e449–55. [DOI] [PubMed] [Google Scholar]
- [22].Horn BJ, Cien A, Reeves NP, et al. Femoral nerve block vs periarticular bupivacaine liposome injection after primary total knee arthroplasty: effect on patient outcomes. J Am Osteopath Assoc 2015;115:714–9. [DOI] [PubMed] [Google Scholar]
- [23].Kirkness CS, Asche CV, Ren J, et al. Assessment of liposome bupivacaine infiltration versus continuous femoral nerve block for postsurgical analgesia following total knee arthroplasty: a retrospective cohort study. Curr Med Res Opin 2016;1–0. [DOI] [PubMed] [Google Scholar]
- [24].Surdam JW, Licini DJ, Baynes NT, et al. The use of exparel (liposomal bupivacaine) to manage postoperative pain in unilateral total knee arthroplasty patients. J Arthroplasty 2015;30:325–9. [DOI] [PubMed] [Google Scholar]
- [25].Yu S, Szulc A, Walton S, et al. Pain control and functional milestones in total knee arthroplasty: liposomal bupivacaine versus femoral nerve block. Clin Orthop Relat Res 2017;475:110–1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [26].Sporer SM, Rogers T. Postoperative pain management after primary total knee arthroplasty: the value of liposomal bupivacaine. J Arthroplasty 2016. [DOI] [PubMed] [Google Scholar]
- [27].Zhang Y, Lu M, Chang C. Local anesthetic infusion pump for pain management following total knee arthroplasty: a meta-analysis. BMC Musculoskelet Disord 2017;18:32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [28].Ong JC, Chin PL, Fook-Chong SM, et al. Continuous infiltration of local anaesthetic following total knee arthroplasty. J Orthop Surg 2010;18:203–7. [DOI] [PubMed] [Google Scholar]
- [29].Kuang MJ, Du Y, Ma JX, et al. The efficacy of liposomal bupivacaine using periarticular injection in total knee arthroplasty: a systematic review and meta-analysis. J Arthroplasty 2016;[Epub ahead of print]. [DOI] [PubMed] [Google Scholar]
- [30].Singh PM, Borle A, Trikha A, et al. Role of periarticular liposomal bupivacaine infiltration in patients undergoing total knee arthroplasty – a meta-analysis of comparative trials. J Arthroplasty 2017;32:675–88. [DOI] [PubMed] [Google Scholar]
- [31].Sharma S, Iorio R, Specht LM, et al. Complications of femoral nerve block for total knee arthroplasty. Clin Orthop Relat Res 2010;468:135–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


