Abstract
Rationale:
Peliosis hepatis (PH) is a rare tumor-like liver lesion composed of multiple blood-filled cavities within the liver parenchyma. It is hard to differentiate PH from other liver lesions by imaging, such as carcinoma, metastases, or abscess.
Patient concerns:
Here, we reported 2 cases that presented with liver lesions under ultrasound and computed tomography (CT) scanning, without any history of liver diseases or drug usage traced back.
Diagnoses:
Liver biopsy and laparoscopy were processed, and the lesions were eventually diagnosed as PH by histopathology, which microscopically presented with multiple sinusoidal dilatations with blood-filled cystic spaces.
Interventions:
After the liver biopsy or laparoscopy, the patients were discharged and followed up in the clinic.
Outcomes:
Both patients were followed up for at least 1 year with good recovery.
Lessons:
PH should always be recognized in the differentiation of liver lesions, particularly indistinctive lesion(s) without any history of liver-related diseases.
Keywords: differential diagnosis, imaging, liver lesions, peliosis hepatis
1. Introduction
Peliosis hepatis (PH) is a rare condition characterized by tumor-like liver lesions composed of multiple blood-filled cavities. The etiology and pathogenesis of PH are not clear. Reported data showed that PH might be associated with numerous causes, such as cytotoxic drug, gamma-ray, bacterial or viral infection, immunodeficiency, and so on.[1] The imageology of PH resembles primary hepatic carcinoma, liver metastases, or liver abscess. Therefore, it is hard to be differentiated from the other similar diseases. In this study, we reported 2 unusual cases presented with liver lesions in imaging without a history of liver disease and were eventually diagnosed as PH by histopathology.
2. Case report
2.1. Case 1
A 64-year-old female, with 2 months history of fatigue, anorexia, and abdominal distention, was admitted to our hospital. She had elevated levels of alkaline phosphatase (AKP 792 U/L) and gamma-glutamyltransferase (GGT 607 U/L). An upper abdominal contrast-enhanced computed tomography (CT) scanning at the local hospital identified an incrassate and dropsical gallbladder wall, by which an acute episode of chronic cholecystitis was diagnosed initially. In addition to the gallbladder abnormality, hepatosplenomegaly and multiple lower-density lesions within the liver were found. Medical record showed no history of viral hepatitis or bacterial infections in the liver.
Abdominal palpation revealed a slight discomfort in the right upper quadrant, as well as hepatosplenomegaly. The patient was sensitive to percussion on the hepatic region with negative Murphy sign. Thrombocytopenia was identified with a platelet count of 6.2 × 1010/L. Other laboratory examinations witnessed normal white blood cell count, hemoglobin, blood electrolytes, and prothrombin time. The results of liver chemistry were as follows: aspartate aminotransferase (AST) 45 U/L, alanine aminotransferase (ALT) 25 U/L, total bilirubin (TBil) 28.3 μmol/L, and direct bilirubin (DBil) 14 μmol/L, AKP 266 U/L, GGT 292 U/L, alpha fetoprotein (AFP) < 20 μg/L. Hepatitis B virus (HBV) serology was negative with an undetectable level of HBV DNA. The level of carbohydrate antigen (CA) 19-9 was normal, but carcinoembryonic antigen (CEA) concentration was elevated to 5.2 μg/L, and the level of CA125 was elevated to 128 U/mL. Human immunodeficiency virus (HIV), antinuclear antibody (ANA), and anti-neutrophil cytoplasmic antibodies (ANCA) were negative, and thyroid function was normal. The ultrasonography and indolent enteroscope were processed to exclude the possibility of gynecological or colorectal malignancies. During the hospitalization, the patient's platelet counts went down progressively (from 55 × 109/L to 47 × 109/L), but the bone marrow examination and parasite antibody determination were proved to be normal. The diagnosis of acute cholecystitis was evidenced by a 3-week effective anti-infection treatment with disappeared symptoms and decreased liver functions. However, the hepatic lesions were still a mystery. Hepatocellular carcinoma (HCC), liver abscess, or liver benign tumors should be differentiated.
To approach to the nature of the multiple intrahepatic lesions, the patient underwent another liver contrast-enhanced CT and magnetic resonance cholangiopancreatography (MRCP). Mild fatty liver and hepatosplenomegaly with several lower-density lesions were found (Fig. 1A–C). Nevertheless, lesions were somewhat poorly defined. Finally, after the signing of a written informed consent, an ultrasound-guided liver biopsy was performed. Typical PH with mild hepatic fibrosis was recognized by histopathology (Fig. 2).
Figure 1.

(A) Arterial phase of contrast-enhanced computed tomography (CT) in Case 1; (B) Portal phase of contrast-enhanced CT showed the lesion (arrows) with heterogeneous enhancement, but the lesions were somewhat poorly defined; (C) Magnetic resonance cholangiopancreatography (MRCP) in case 1 showed hepatosplenomegaly on T2 weight.
Figure 2.
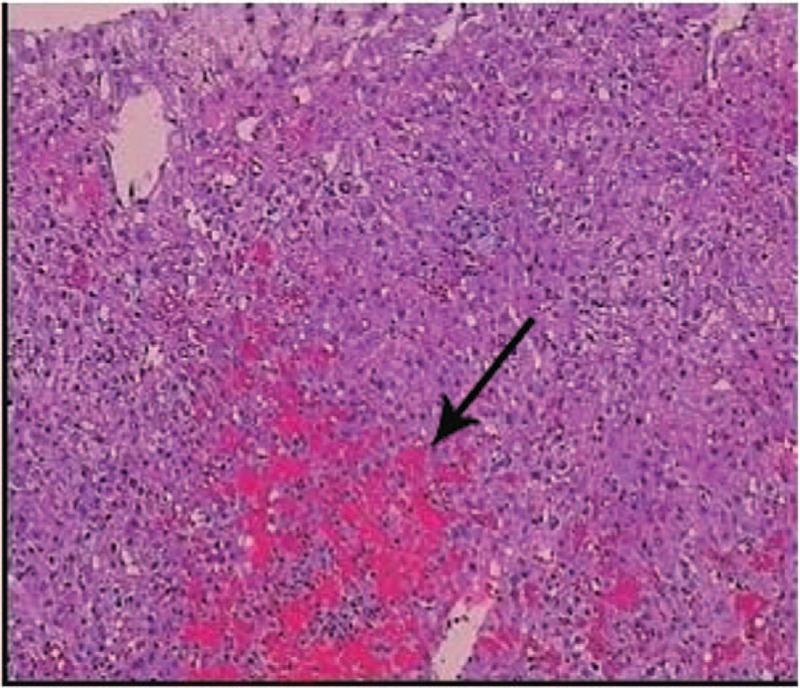
Histology of the liver lesion in case1 indicated a typical feature of peliosis hepatis presenting with multiple sinusoidal dilatations together with blood-filled cystic spaces (arrow). (H&E, x100).
2.2. Case 2
A 47-year-old man came into our clinic due to a liver lesion in the right lobe found during his routine annual check-up. A hepatic magnetic resonance imaging (MRI) was performed at a local hospital, suggesting that the lesion might be an inflammatory pseudo tumor, but HCC could not be excluded. The patient had no history of liver disease, tumor, or any drug-taken. The results of physical examination and laboratory tests were normal, except for an increase of CEA level from 6.5 mmol/L to 7.9 mmol/L during 4-week duration. The ultrasound demonstrated an inhomogeneous echo and calcification plaque in the liver parenchyma (Fig. 3). Gastroendoscopes were processed to exclude gastrointestinal tumors. Eventually, the patient chose surgical operation to remove the hepatic neoplasm. Laparoscopy was conducted to partially resect the right hepatic lobe. The final histopathology of the lesion demonstrated PH (Fig. 4). The patient got a good recovery, and was discharged a week after the surgery.
Figure 3.

Liver ultrasound in Case 2 demonstrated a clear heterogeneous echo (38 mm × 35 mm) in the right lobe of liver.
Figure 4.
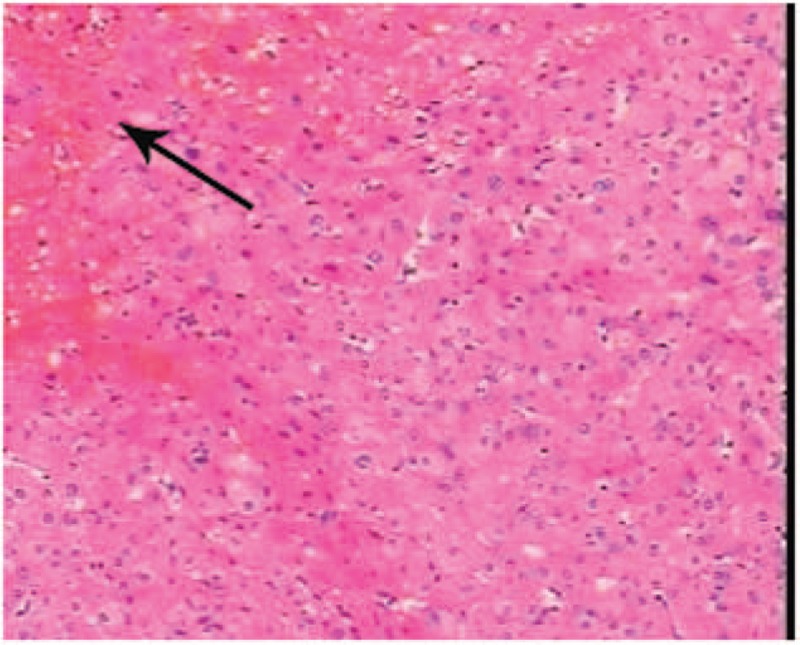
Liver histology in case 2. Peliosis hepatis is morphologically recognized as the formation of “blood lake” due to vascular dilation mixed with focal bleeding (arrow). (H&E, x100).
3. Discussion
As an uncommon benign vascular disease, PH is usually asymptomatic. It could occur in any age, but is more common in adults.[1] PH has always been somewhat confused with liver neoplasm. The size of lesions ranges from a few millimeters to several centimeters, and even occupied most part of liver. In a few cases, the number or size of PH lesions could increase in a short period and disseminate throughout the liver, resembling the progress of liver carcinoma or metastases.[2]
The etiology of PH remains unclear. Literatures have suggested that prolonged use of various kinds of drugs might be associated with PH. The related drugs include anabolic steroids, diethylstilbestrol, corticosteroids, immunosuppressant,[3,4] tamoxifen,[5] androgen,[6] thiopurine,[7] and oral contraceptives.[8,9] In addition, a variety of infectious diseases, such as Bartonella henselae,[10] tuberculosis,[11] acquired immunodeficiency syndrome,[12] gummatous syphilis[13] are reported to be associated with PH. Moreover, PH has been recognized to be concomitant with HCC[14] and hematological malignancies[15] in some cases. However, no evidence could support a direct relationship between the above factors and the development of PH.
In this study, the patients had no obvious immune deficiency, no history of significant infection, no documented family history of vascular diseases or cancer, and no drug usage that may be related to PH. Their hepatic lesions were found coincidently by imaging during the evaluation for other disease or medical check-up. This benign liver lesion is difficult to differentiate from other hepatic mass or malignancy by medical history taking, routine laboratory tests, or imaging.
PH often presented asymptomatically like the patient in case 2. However, the patient with PH in case 1 was complicated with biliary tract infection. Reported cases described the common concomitant manifestations of PH including hepatomegaly, ascites, portal hypertension, cholestasis, and even hepatic failure. In a few cases, a severe abdominal pain resulting from the rupture of lesions, intraperitoneal hemorrhage, and spontaneous intrahepatic hemorrhage occurred.[16] Furthermore, the bacillary peliosis might present with fever, weight loss, anorexia, diarrhea, hepatosplenomegaly, and so on. In this case, bacillary peliosis could be ruled out because of no typical findings of lymphadenopathy with Bartonella henselae or neurologic symptoms with Bartonella quintana infection.[5]
PH is characterized by blood-filled cavities distributing randomly throughout the liver. The lesions can be focal, segmental, or diffusely disseminated in hepatic sinusoids. Therefore, the imaging features of PH are nonspecific and differ from one another,[5] leading to the difficulty for diagnosis and differential diagnosis. A missed, delayed, or an incorrect diagnosis seems to be very common. In our cases, abdominal ultrasound, CT scanning, MRI, and MRCP were processed to distinguish the lesions from malignancies, but all of them failed to make a definite diagnosis. Histopathology represents the golden standard. The histopathologic results of liver biopsy or hepatolobectomy witnessed dilated sinusoidal spaces with congestion in the liver parenchyma (Figs. 2–4).
The pathogenesis of PH remains unclear. Researchers made a hypothesis that the obstruction of hepatic sinusoidal outflow contributes to the dilatation of the hepatic central vein and the subsequent hepatocellular necrosis, thus leading to cavity formation. The results of the histopathology in 2 cases both demonstrated multiple sinusoidal dilatations together with blood-filled cystic spaces, which might support this hypothesis (Figs. 2–4).
PH is frequently an occasional finding during abdominal scanning of ultrasound, CT, or MRI. Subsequent angiography could be considered. A typical imaging of PH presents with multiple accumulations of the contrast media, which is most prominent during the parenchyma and venous phase. However, these features did not manifest in our cases. Helical CT may tell multiple peripheral low-density regions with foci of spontaneous high-density regions, indicating the presence of blood component. MRI can reveal multiple peripheral lesions with hypo-intense on T1-weighted and hyper-intense on T2-weighted images with bright foci on all sequences, suggesting subacute blood flow.[17]
Liver biopsy remains the most reliable method in the diagnosis of PH, though it is an invasive manipulation, carrying the risk of bleeding. In Case 1, the MAX-CORE Disposable Core Biopsy Instrument (Bard Peripheral Vascular, Inc. Mexico, USA; Length of sample size 1.9 cm, gauge size and needle length 16 g ∗ 16 cm, penetration depth 22 mm) was used for liver biopsy. The sample of the specimen was sufficient for the histopathological diagnosis; a larger-size needle biopsy may increase the risk of complications.[8]
In summary, although PH is a rare disease, it should always be kept in mind for the differential diagnosis in newly discovered liver lesions. Imaging assessment is insufficient. Clinicians and radiologists should be aware of this disorder for the accurate and timely diagnosis, and to exclude malignancy. As it is considered the most reliable diagnostic tool, liver biopsy should be recommended, but the risk of hemorrhage must be alert.
Footnotes
Abbreviations: AFP = alpha fetoprotein, AKP = alkaline phosphatase, ALT = alanine aminotransferase, ANA = antinuclear antibody, ANCA = anti-neutrophil cytoplasmic antibodies, AST = aspartate aminotransferase, CA = carbohydrate antigen, CEA = carcinoembryonic antigen, CT = computed tomography, DBil = direct bilirubin, GGT = gamma-glutamyltransferase, HBV = Hepatitis B virus, HCC = hepatocellular carcinoma, HIV = Human immunodeficiency virus, MRCP = magnetic resonance cholangiopancreatography, MRI = magnetic resonance imaging, PH = peliosis hepatis, TBil = total bilirubin.
YND and ZZR contributed equally to this work.
The authors have declared that no conflict of interest exists.
References
- [1].Hidaka H, Ohbu M, Nakazawa T, et al. Peliosis hepatis disseminated rapidly throughout the liver in a patient with prostate cancer: a case report. J Med Case Rep 2015;9:194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [2].Terlizzi JP, Azizi R, Chow MD, et al. Peliosis hepatis in a child with myotubular myopathy: successful treatment using hepatic artery embolization. J Pediatr Surg 2013;48:e9–12. [DOI] [PubMed] [Google Scholar]
- [3].Elsing C, Placke J, Herrmann T. Alcohol binging causes peliosis hepatis during azathioprine. World J Gastroenterol 2007;13:4646–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].Yu CY, Chang LC, Chen LW, et al. Peliosis hepatis complicated by portal hypertension following renal transplantation. World J Gastroenterol 2014;20:2420–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].Iannaccone R, Federle MP, Brancatelli G, et al. Peliosis hepatis: spectrum of imaging findings. AJR Am J Roentgenol 2006;187:W43–52. [DOI] [PubMed] [Google Scholar]
- [6].Neri M, Bello1 S, Bonsignore A, et al. Anabolic androgenic steroids abuse and liver toxicity. Mini-Rev Med Chem 2011;11:430–7. [DOI] [PubMed] [Google Scholar]
- [7].Calabrese E, Hanauer SB. Assessment of non-cirrhotic portal hypertension associated with thiopurine therapy in inflammatory bowel disease. J Crohn's Colitis 2011;5:48–53. [DOI] [PubMed] [Google Scholar]
- [8].Grønlykke L, Tarp B, Dutoit SH, Wilkens R. Peliosis hepatis: a complicating finding in a case of biliary colic. BMJ Case Rep 2013;2013:pii: bcr2013200539. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9].Testa G, Panaro F, Sankary H, et al. Peliosis hepatis in a living related liver transplantation donor candidate. J Gastroenterol Hepatol 2006;21:1075–7. [DOI] [PubMed] [Google Scholar]
- [10].Biswas S, Rolain J-M. Bartonella infection: treatment and drug resistance. Future Microbiol 2010;5:1719–31. [DOI] [PubMed] [Google Scholar]
- [11].Sanz-Canalejas L, Gomez-Mampaso E, Canton-Moreno R, et al. Peliosis hepatis due to disseminated tuberculosis in a patient with AIDS. Infection 2014;42:185–9. [DOI] [PubMed] [Google Scholar]
- [12].Sandrasegaran K, Hawes DR, Matthew G. Hepatic peliosis (bacillary angiomatosis) in AIDS: CT findings. Abdom Imaging 2005;30:738–40. [DOI] [PubMed] [Google Scholar]
- [13].Chen JF, Chen WX, Zhang HY, Zhang WY. Peliosis and gummatous syphilis of the liver: a case report. World J Gastroenterol 2008;14:1961–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].Hoshimoto S, Morise Z, Suzuki K, et al. Hepatocellular carcinoma with extensive peliotic change. J Hepatobiliary Pancreat Surg 2009;16:566–70. [DOI] [PubMed] [Google Scholar]
- [15].Kleger A, Bommer M, Kunze M, et al. First reported case of disease: peliosis hepatis as cardinal symptom of Hodgkin's lymphoma. Oncologist 2009;14:1088–94. [DOI] [PubMed] [Google Scholar]
- [16].Charatcharoenwitthaya P, Tanwandee T. Education and imaging: hepatobiliary and pancreatic: spontaneous intrahepatic hemorrhage from peliosis hepatis: an uncommon complication of a rare liver disorder. J Gastroenterol Hepatol 2014;29:1754. [DOI] [PubMed] [Google Scholar]
- [17].Atila K, Çoker A, Uçar D, et al. A rare clinical entity misdiagnosed as a tumor: peliosis hepatis. Ulus Travma Acil Cerrahi Derg 2007;13:149–53. [PubMed] [Google Scholar]


