Abstract
Background
Disorganized attachment is an important early risk factor for socio-emotional problems throughout childhood and into adulthood. Prevailing models of the etiology of disorganized attachment emphasize the role of highly dysfunctional parenting, to the exclusion of complex models examining the interplay of child and parental factors. Decades of research have established that extreme child birth weight may have long-term effects on developmental processes. These effects are typically negative, but this is not always the case. Recent studies have also identified the dopamine D4 receptor (DRD4) as a moderator of childrearing effects on the development of disorganized attachment. However, there are inconsistent findings concerning which variant of the polymorphism (7-repeat long-form allele or non 7-repeat short form) is most likely to interact with caregiving in predicting disorganized versus organized attachment. In this study we examined possible 2- and 3-way interactions between child DRD4 polymorphisms and birth weight and maternal caregiving at age 6 months in longitudinally predicting attachment disorganization at 36 months.
Method
Our sample is from the Maternal Adversity, Vulnerability and Neurodevelopment (MAVAN) project, a sample of 650 mother-child dyads. Birth weight was cross-referenced with normative data to calculate birth weight percentile. Infant DRD4 was obtained with buccal swabs and categorized according to the presence of the putative allele 7-Repeat. Macro-analytic and a micro-analytic measures of maternal behavior were extracted from a videotaped session of 20-minutes of non-feeding interaction followed by a 10-minute divided attention maternal task at 6 months. Attachment was assessed at 36 months using the Strange Situation Procedure, and categorized into disorganized attachment and others.
Results
Results indicated that a main effect for DRD4 and a two-way interaction of birth weight and 6 month maternal attention (frequency of maternal looking away behaviour) and sensitivity predicted disorganized attachment in robust logistic regression models adjusted for social demographic covariates. Specifically, children in the midrange of birth weight were more likely to develop a disorganized attachment when exposed to less attentive maternal care. The association however reversed with extreme birth weight (low and high). The DRD4 7R allele was associated with less D (protective), while non-7R children were more likely to be classified D.
Conclusion
Implications for understanding inconsistencies in the literature about which DRD4 genotype is the risk direction are also considered. Suggestions for intervention with families with infants at different levels of biological risk and caregiving risk are also discussed.
INTRODUCTION
Disorganized attachment, characterized by lack of a coherent strategy to deal with the stress of separation and reunion with the mother during the strange situation (Main & Solomon, 1986), is an important early risk factor for socio-emotional problems throughout childhood and into adulthood (Carlson, 1998; Moss, Cyr, & Dubois-Comtois, 2004; van IJzendoorn, Schuengel, & Bakermans-Kranenburg, 1999). Disorganization can be defined as a dysfunction in emotional regulation, including the experience of fear (Carlson, 1998). The caregiver serves as a source of fear to the child as well as the biologically based, expectable source of reassurance which leads to the concurrent activation of both the fear and attachment systems (Carlson, 1998; Main & Solomon, 1986, 1990). These conflicting motivations within the child lead to maintenance of extreme arousal at a time when child capabilities are inadequate to ensure self-regulation. Such conflict and premature reliance on individual organization during a developmental period when dyadic child-caregiver regulation is normative is believed to interfere with the development of effective relational capabilities, communication and internal organizational skills related to emotion regulation.
Between preschool and school-age, two-thirds of children showing disorganized attachment adopt a role-reversed controlling attachment pattern with the caregiver (Moss, et al., 2004). The increase in controlling behaviour with the caregiver during the preschool period may be linked to attempts by disorganized children to reduce stress levels, which cannot be regulated through child dependency on the caregiver (Moss, St-Laurent, Tarabulsy, & Bureau, 2011). However, the controlling child’s strategy of orienting away from seeking comfort, protection, and the meeting of their own needs and toward maintaining engagement with the parent on the parent’s terms increases the likelihood of child internalizing and externalizing psychopathology (Moss, et al., 2004). Thus, despite their superficial “organized” attachment strategy, controlling children, like those who continue to manifest behavioral disorganization, are at significant risk for maladaptation between early childhood and young adulthood. Although characteristics of parenting are greatly associated with the risk for disorganized attachment, few attachment studies consider more complex models of the etiology of disorganized attachment which account for the influence of multiple child factors.
Disorganization and early maternal care
Traditional models of the etiology of disorganized attachment emphasize the role of atypical and highly dysfunctional parenting. Helpless or hostile caregiving places the child in a “fright without solution” paradox (Lyons-Ruth, Melnick, Bronfman, Sherry, & Llanas, 2004; Main & Solomon, 1986, 1990), undermining the infant’s primary attachment strategy and causing him/her to behave in ways that are not obviously aimed at proximity with the caregiver, despite his/her need for comfort.
Beyond helpless/hostile caregiving, highly insensitive maternal care is also related to disorganization (Bakermans-Kranenburg & van Ijzendoorn, 2011; Laucht, Esser, & Schmidt, 2001; Moss, St-Laurent, et al., 2011), both in its own right and over and above the contribution made by atypical maternal behaviour (Moran, Forbes, Evans, Tarabulsy, & Madigan, 2008). Maternal sensitivity, defined as a mother’s ability to perceive her child’s signals appropriately and respond to them promptly and contingently (Ainsworth, Blehar, Waters, & Wall, 1978) is an important precursor to secure attachment (Ainsworth, et al., 1978; Atkinson, Niccols, et al., 2000; de Wolff & van IJzendoorn, 1997; Jaffe, Beebe, Feldstein, Crown, & Jasnow, 2001; van den Boom, 1994) and affects social-emotional development as it scaffolds neurobiological development (e.g., the stress regulatory systems (Glaser, 2000; Gunnar & Quevedo, 2007)). Sensitive maternal care promotes the moderation of physiological stress by young children (Atkinson et al., 2013; Derryberry & Rothbart, 1984), and is associated with fewer behavioural problems (Feldman & Eidelman, 2004).
Of particular importance in the context of attachment generally and maternal sensitivity and disorganization more specifically, is the issue of controlled attention, the ability to concentrate focus on consciously selected stimuli and inhibit focus on potential distractors. Attention is considered central to attachment theory (Atkinson et al., 2009) because the whereabouts of the attachment figure is continuously monitored by all children (Bretherton, 1980; Maier et al., 2005), with variance in attention underlying the unique nature of each attachment pattern (Atkinson et al., 2009). For example, “[A]ttention is fluid in secure babies … and liable to dysregulation or collapse in disorganized babies” ((Main, 1995), p. 427). Similar considerations pertain to attachment at the preschool age. Moss and St. Laurent (2001) showed that disorganized pre-schoolers, who focus attention on coping with parental figures who induce fear or feelings of abandonment in them, have fewer cognitive and attentional resources available for learning and exploration.
Furthermore, attentional capacity is a necessary (although not a sufficient) condition for sensitive parenting, insofar as excessive orienting away from the infant precludes response to infant signals. Thus, mothers who self-report a tendency to orient away from stressful stimuli also show lower sensitivity in interaction with their infants (Atkinson et al., 1995). Pederson et al. (1990) pointed out, “mothers of more secure infants were more frequently characterized as noticing their babies’ signals [italics added] and using these signals to direct behavior” (p. 1974); “sensitivity involves an openness to signals” (p. 1976). Indeed, meta-analytic evidence indicates that the prediction of infant attachment security from observations of maternal responsiveness is significantly stronger when the mother is experimentally induced to divide her attention between infant and another task, as compared to when the mother’s attention is not experimentally divided (Atkinson, Niccols, et al., 2000). Mileva et al. (2013) showed that less sensitive mothers tend to orient away from the infant more frequently and for longer durations than do more sensitive mothers. They also found a significant negative correlation between infant-directed vocalizing and frequency of orienting away from the infant. Mileva et al. (2012) also showed that maternal orienting away is significantly negatively related to infant activity. Hence, there is a relation between maternal attention and infant behaviour (although the direction of the causality is not reflected in this correlation). Atkinson, Paglia, et al. (2000) concluded that “effective attention allocation … lie[s] at the core of sensitive interaction” (p. 49).
Maternal attention has also been linked directly to disorganized attachment in infants (Atkinson, et al., 2009). Administered an emotional Stroop task, disorganized mothers/mothers of disorganized infants were less adept at disengaging from negative emotion/negative attachment stimuli than from neutral stimuli, a selective attention deficit not exhibited by disorganized mothers/mothers of organized infants. Thus, disorganized mothers and the mothers of disorganized infants showed a less controlled attentional focus than the mothers of infants with organized attachment patterns.
Based on the above review, we investigate mothering behaviour in two ways in the present study. One involves assessing maternal sensitivity through observational rating scales, as developed by Ainsworth et al. (1978) and typically used in attachment research. The second assessment strategy focuses more specifically on the issue of maternal attention to the child. This strategy is more akin to the ethological approach used in studies of maternal behaviour in other animals, where we have been interested in the psychobiology of mothering. This strategy involves determining the frequency and duration of specific behaviours emitted by the mother and the infant during their interactions. This micro “ethological” measure provides an alternative way of looking at mothering “motivation” or intensity. The major focus of this study is maternal attention, given our interest in dopamine, as explained in more detail below. But as mentioned, maternal attention is a necessary but insufficient condition for maternal sensitivity. Therefore, we supplemented analyses with formalized attachment rating scales (Ainsworth, et al., 1978).
Genetic influences
Attachment theory has not, for the most part, included more complex models of the development of disorganized attachment that allow for the interplay of particular child factors with parenting characteristics in the prediction of disorganization. This approach is illustrated by van IJzendoorn and Bakermans-Kranenburg (Van IJzendoorn & Bakermans-Kranenburg, 2006), who showed that maternal unresolved loss or trauma, a distal feature of environmental risk, is associated with infant disorganization, but only in the presence of the DRD4 7-repeat polymorphism. In the present study, we assess the interplay of two environmental risk factors (specifically maternal sensitivity and birth weight) and DRD4 as they relate to infant disorganization at 36 months.
Recent advances in molecular genotyping permit the incorporation of genetic variation into models of developmental risk. Recent studies have identified the dopamine D4 receptor (DRD4) to be of particular salience in the pathway to disorganized attachment. Dopamine is expressed in pathways mediating reward related to social interaction, including mother-child interaction (Insel, 2003). Dopamine is also expressed in the amygdala and amygdala prefrontal circuits involved in cognitive processes (Wang, Zhong, Gu, & Yan, 2003) and anxiety-related behaviour such as the stress response (Armbruster et al., 2009; LeDoux, 2000; Phelps & LeDoux, 2005). The encoding gene for the DRD4 receptor has a number of functional variants including a 48-base pair variable number tandem repeats (VNTR) in exon 3 ranging from 2 to 11 copies. The most common functional variants are the 4-repeat (4R) and the 7-repeat (7R). The longer variants (6R to 10R) are associated with lower dopamine receptor efficiency. The DRD4 expression is also influenced by an upstream regulatory region, the functional single nucleotide polymorphism (SNP) -521C/T. The C variant is associated with greater novelty seeking and extraversion (Munafo, Yalcin, Willis-Owen, & Flint, 2008).
Curiously, studies have reported contradictory findings about which variant of the polymorphism is most likely to predict disorganized attachment. Three studies from the same Hungarian low-risk middle class community sample have found an increased risk for disorganized attachment in 12 month old infants with at least one 7R allele (Lakatos et al., 2000), an association strengthened with at least one -521 SNP T allele (CT or TT) (Lakatos et al., 2002). After examining parental genotypes, these authors also concluded that carrying neither the 7R nor the T allele was a resilience factor for the development of early (secure) attachment (Gervai et al., 2005). On the other hand, Cicchetti et al. (2011) reported a greater likelihood of disorganization and stability of disorganization (age 1–2 years) in the 7-absent group. Three studies (Bakermans-Kranenburg & Van Ijzendoorn, 2004; Luijk et al., 2010; Spangler, Johann, Ronai, & Zimmermann, 2009) did not find an association between disorganized attachment and DRD4, -521 C/T or both genotypes, and a meta-analysis only found a small effect size (0.05) (Bakermans-Kranenburg & van Ijzendoorn, 2011). The inconsistency in the association between DRD4 and disorganized attachment suggests other factors may serve as moderators.
Consistent with the etiological hypotheses of disorganized attachment proposed by Main and Hesse (Main & Solomon, 1986), the moderating effect of early caregiving has been examined in several studies including a meta-analysis (Bakermans-Kranenburg & van Ijzendoorn, 2011). However studies report paradoxical findings about which DRD4 allele constitutes the risk or susceptibility allele. Bakermans-Kranenburg & van Ijzendoorn (2011) report that in conditions of adverse caregiving environments, children with the 7R variant have higher levels of disorganized attachment than children without this variant. For example, maternal unresolved attachment, an adult attachment category predictive of infant disorganization, interacts with DRD4 7R to predict disorganized attachment (Van IJzendoorn & Bakermans-Kranenburg, 2006). On the contrary, Gervai et al. (2007) found that disruptive maternal affective behaviour interacts with the short form, the 4R, to predict disorganized attachment, and that the 7R mutes the infant’s responsiveness to adverse care. Cicchetti et al (2011), examined how the outcome of an intervention study with maltreating mothers and their infants is moderated by genetic factors. For maltreated children receiving the intervention, having the 7R allele predicts less disorganized attachment and lower stability of disorganized attachment post-intervention. On the other hand, for the control (non-maltreated) children, the 7R allele predicts more disorganized attachment post-intervention.
Birth Weight
The theory of the Biological Sensitivity to Context suggests that developmental risk, such as perinatal risk, interacts with postnatal influences to prepare the infant to match or calibrate their biological and behavioural systems to their postnatal environment (Ellis & Boyce, 2008). Perinatal risk may interact with other biological and environmental factors in predicting outcomes (Belsky & Pluess, 2009). Child birth weight, as an indication of intra-uterine growth retardation (IUGR), is one of the major risk factors for infant morbidity and mortality and has long-term effects on developmental processes. Several factors affect foetal growth, including foetal, maternal, and placental features, as well as their interactions (Valero De Bernabe et al., 2004).
Children with IUGR, because of a fragile or less developed nervous system, have a reduced ability to regulate their response to the environment. With reduced internal regulatory capacity, such children may be particularly vulnerable to adverse parental experiences but also more receptive to very positive experiences. For example, Nomura et al. (2007) found that children with low birthweight AGA and child maltreatment are at higher risk for delinquency at adolescence and poor emotional wellbeing and depression in adulthood relative to those with neither risk factor. Whiteside-Mansell et al. (2009) confirmed this vulnerability to adversity, regarding family conflict. Conversely, two studies have reported that early maternal sensitivity interacts with low birthweight to predict positive outcomes. For example, Laucht et al (2001) found that children with low birthweight exposed to high maternal sensitivity show decreased internalizing and hyperkinetic problems at the ages of 2, 4.5 and 8 compared to those exposed to lower levels of sensitivity. Weiss et al (2000) reported that vulnerable children with low birthweight and/or perinatal risk are more likely to develop a secure attachment when exposed to nurturing maternal touch. Only in the study by Nomura et al.(2007) is birthweight adjusted for gestational age. No study though has examined disorganized attachment as an outcome.
While the majority of research has emphasized the deleterious neurological and cognitive outcomes such as learning and attention, recent studies have explored the association between IUGR (as measured by weight adjusted for gestational age (AGA) and socio-emotional development. For example, birthweight AGA is linked in longitudinal studies with the development of anxious and depressive psychopathology in early adolescence (Costello, Worthman, Erkanli, & Angold, 2007; Rice, Harold, & Thapar, 2006; Smolla, Béliveau, Lépine, Lévesque, & Martin, 2009). Rice et al (2006) found that birthweight AGA predicts parent-rated depressive symptoms when controlling for other known risk factors. Similarly, Costello et al (2007) found that low birthweight predicts a five-fold increase in female adolescent depression. Such findings suggest that, in a process consistent with fetal programming, fetal growth predicts childhood development. In utero events affect the development of neural systems that regulate emotional and cognitive development. Increased fetal glucocorticoid levels have been associated with impaired fetal growth, altered neural development, and increased expression of genes associate with behavioural and endocrine stress responses (Challis et al., 2001; Maccari et al., 2003; Meaney, Szyf, & Seckl, 2007; Seckl & Holmes, 2007).
There is also modest evidence that genetic factors moderate the association between birth weight and the development of attachment. For example, Rice, Harold and Thapar (2006) reported that low birth weight AGA interacts with genetic risk (as measured by twin status) in the prediction of depressive symptoms in 8 to 17 year olds. More specifically, Broekman et al (2011) reported that birth weight AGA interacts with genotype in numerous serotonergic genes to predict internalizing symptoms in a sample of children aged 8 to 12 years of age.
Consistent with evidence for other disorders such as diabetes (Wei et al., 2007), emerging research suggests that an increased susceptibility to psychopathology may not be restricted to infants born small. Foetal growth across the entire gradient predicts the risk for psychopathology with reverse or J-shaped associations between birth weight and a number of disorders. Several studies have shown that macrosomia (excessive birth weight) is a significant predictor of later psychiatric disorder, internalizing and externalizing (Van Lieshout & Boyle, 2011). Two studies demonstrate a curvilinear relationship between birthweight and attention problem scores (van Mil et al., 2015) as well as with anxiety and depressive scores (Broekman et al., 2011), such that birthweight at either end of the measure pose higher risks.
In the area of attachment and birth weight, in particular, studies have been imprecise in two respects. First, for the most part, they have not uncoupled the effect of birth weight from that of prematurity. This means that some subjects in these low birth weight studies might not actually have IUGR but rather low birth weight, because gestation had been prematurely ended. Few studies have uncoupled the effects of intra-uterine growth constraints from those associated with the complications of early birth, such as immature organ development and early parent-child separation. The second source of imprecision in these studies is that many of them were conducted before the development of the disorganized attachment classification (Main & Solomon, 1986, 1990) or were based on instrumentation that does not assess Disorganization (i.e., Attachment Q-set, AQS (Waters & Deane, 1985).
One study found that vulnerable children (with low birth weight (LBW = <2500 grams), preterm birth and/or perinatal complications) are more likely to be insecurely attached at 12 months, according to the AQS (Weiss, et al., 2000). Results of a study examining children separated at birth from parents (because of preterm birth or severe illness), did not show an association between birth weight and attachment organization at 12–19 months (Rode, Chang, Fisch, & Sroufe, 1981).
Studies of exclusively preterm children yield contradictory findings. Plunkett, Klein, and Meisels (1988) found that preterm LBW children are more likely to be insecurely attached at 24 months, whereas Frodi et al (1983) reported no association with attachment security at 52 weeks. Concerning very low birth weight (VLBW = <1500 grams) preterm children, Mangelsdorf et al. (1996) found that VLBW preterm children were more likely to be insecurely attached at 14 (AQS) and at 19 months (Strange Situation; assessments included a variant of disorganization). Brisch et al. (2005), using an attachment system that included disorganization, found more insecure attachment at 24 months only in children who were neurologically impaired. On the other hand, Goldberg, Perotta, Minde and Corter (1986) found no association between birth weight and attachment security at 12 months past term. Easterbrooks et al. (1989), although using the disorganized attachment classification, reported no association between VLBW preterm status and attachment security at 13 and 20 months. There is a paucity of studies examining the role of birth weight in non-preterm children on the development of attachment and especially on the less studied, disorganized subtype.
Although the reviewed literature suggests that birth weight might interact with caregiving quality and child genetic variables (DRD4) in predicting disorganized attachment, the direction of the association seems less predictable. To our knowledge, no study has yet examined the combined effects of constitutional risk, molecular genetics and relevant environmental influences on the development of child attachment disorganization.
Objectives and hypotheses
Specifically, we examined: (1) Whether birthweight AGA predicts child disorganized attachment at 36 months; (2) Whether the association between birthweight is linear or curvilinear; (3) Whether the association between birthweight AGA is moderated by the child’s DRD4 genotype, in a GxE model; (4) Whether the association between birthweight AGA is moderated by early maternal sensitivity at 6 months; and, (5) Whether in a three way interaction, birthweight AGA, child DRD4 genotype and early maternal care at 6 months predict child disorganized attachment at 36 months.
We hypothesized that birthweight would operate with a curvilinear effect and that children with extreme birth weight (low and high) AGA and 7R DRD4 would be more likely to have disorganized attachment. We also hypothesized that the risk factors of birth weight and DRD4 would interact, such that children with extreme birth weight (low and high) and the 7R would be more likely to have disorganized attachment when exposed to less sensitive maternal care.
METHOD
Participants
Participants were mother-child pairs from the ongoing longitudinal Maternal Adversity, Vulnerability and Neurodevelopment (MAVAN) project. The MAVAN is a Canadian community-based birth cohort composed of more than 650 women recruited from Montreal (Qc.) and Hamilton (On.). Women 18–43 years of age were recruited between 2003 and 2009 during routine ultrasound examinations and from prenatal care clinics in maternity hospitals. Eligibility criteria for women were age 18 years of age or over at the expected date of delivery, less than 24 weeks gestational age, singleton and term pregnancy (≥ 37 weeks), and fluency in English or French. Exclusion criteria were the presence of severe chronic maternal illness, past obstetrical complications or major foetal/infant anomaly. Children exhibiting significant developmental delays, identified with the Bayley scale, were excluded from the study. Greater details are available elsewhere (O’Donnell et al., 2014).
Retention rates for the MAVAN subjects are 97.4% at 6 months, 84.0% at 18 months and 80.6% at 36 months, with the majority of subjects dropping out when the parent returned to work. Compared to mothers who remained in the study, mothers who left the study did not differ significantly on measures of age at delivery, depression, or education. Compared to children who remained in the study, children lost to follow-up did not differ significantly on measures of birth weight. The present study includes 650 mother-child dyads included in the final imputation model.
There were slightly more boys than girls. Mothers were on average 30.6 years of age at recruitment, and approximately half were in the “University graduate” or higher category (Table 1). Unstandardized prenatal depression scores ranged from 0 to 49 (M = 12.28, SD = 10, α = .92). The demographic and socioeconomic distribution of women in this study was similar to that of women from the Generation R Study and the Avon Longitudinal Study of Parents and their Children, two comparable prenatal cohort studies (Van Batenburg-Eddes et al., 2013).
Table 1.
Descriptive statistics of MAVAN mother and child at 36 months (N = 650 pairs)
| Demographic Characteristics of subjects from MAVAN included in 36 months analyses | ||
|---|---|---|
| Variables | Montreal (N = 388) | Hamilton (N = 262) |
| Mothers | ||
| Age* | M = 29.8, SD = 5.01 | M = 31.2, SD = 5.09 |
| Education | ||
| High school or less and Partial College | 18.8% | 17.6% |
| Completed college or some university | 29.9% | 38.3% |
| University graduate or more | 51.3% | 44.1% |
| Income* | ||
| <15,000 | 11.8% | 3.9% |
| 15,00–<30,000 | 17.3% | 10.6% |
| 30,000–<50,000 | 23.6% | 20.0% |
| 50,000–<80,000 | 20.0% | 27.5% |
| >80,000 | 27.3% | 38.0% |
| Genotype DRD4 | ||
| No 7 repeat | 62.4% | 64.0% |
| 7 repeat | 37.6% | 36.0% |
| Post Natal Depression 36 Months | M = 11.4, SD = 8.74 | M = 11.4, SD = 10.3 |
| Prenatal CES-D* | M = 12.1, SD = 8.57 | M = 13.9, SD = 11.4 |
| Children | ||
| Gender* | ||
| Male | 49.2% | 40.1% |
| Female | 50.8% | 59.9% |
| Birth Weight* (percentile) | M = 41.4, SD = 26.04 | M = 52.4, SD = 27.8 |
| Genotype DRD4 | ||
| No 7 repeat | 66.5% | 61.4% |
| 7 repeat | 33.5% | 38.6% |
| Ainsworth sensitivity scale | M = 5.65, SD = 1.91 | M = 5.4, SD = 2.1 |
| Looking away frequency* | M =19.2, SD = 10.63 | M = 23.5, SD = 13.2 |
| Looking away duration* | M = 121, SD = 131 | M = 152, SD =155 |
| Attachment style | ||
| Avoidant | 6.43% | 6.9% |
| Secure | 53.2% | 57.2% |
| Ambivalent | 15.2% | 13/0% |
| Disorganized | 25.2% | 22.9% |
Significant difference between Montreal and Hamilton
Procedure
Women consenting to participate were interviewed at 24–36 weeks of pregnancy to obtain data on demographic, medical and obstetric history, stressors, social support, and pregnancy. Birth outcomes were extracted from the chart of the birthing unit. Mothers and their children were seen at each study time point (i.e., 3, 6, 12 and 18 months and yearly from age 24 months onward). Mothers were assessed using extensive socio-demographic and psychological measures while children were assessed using neurodevelopmental and socio-emotional measures. Early maternal care was assessed at 6 months in a 20-minute videotaped, non-feeding and unstructured home interaction session followed by a 10-minute divided attention task. Mothers were asked to interact normally with their infants. During the last 10-minute period, mothers completed scales while still caring for the infant. The purpose of this task was to place the mother in a situation that divides attention. Behaviour under these conditions augments the predictive capacity of sensitivity ratings (Atkinson, Paglia, Coolbear, Niccols, Poulton, et al., 2000). A macro-analytic (Ainsworth sensitivity scales) and a micro-analytic (Behavioural Evaluation Strategies and Taxonomies - BEST) measure of maternal behaviour were used to code observed maternal behaviour.
Measures
Birth weight
As fetal growth may differ by race, gender, socioeconomic environment, geographical area and altitude, birth weight from the chart was cross-referenced with Canadian normative data (M.S. Kramer et al., 2001) to calculate birth weight Adjusted for Gestational Age (AGA), measured as a percentile. Infant birthweight ranged from 2.19kg to 5.34kg (M = 3.37kg, SD = .47kg), while birthweight AGA ranged from 0 to 100 percentile (M = 46.53, SD = 27.64).
DRD4 genotype
Child and maternal genotypes were obtained with the use of buccal swabs, using the TaqMan methods on the ABI-7000 for Single Nucleotide Polymorphism (SNP) markers and ABI-3100 for repeat polymorphisms. To ensure a clear result, any ambiguous genotypes were discarded and the subjects were re-genotyped until the results were unambiguous. Each 20th marker was re-genotyped to check for error rates (0.5%). DRD4 was coded dichotomous as the presence or absence of 7R, the lowest expressing genotype, and others. The genotype distribution represented that of a predominantly white population sample. For both the Montreal and Hamilton samples the distribution of DRD4 conformed to the Hardy Weinberg equilibrium (p = .58; p = .95, respectively). There were no gender differences (χ2(1) = .01, p = .92; χ2(1) = .4, p = .52) (lab of J Kennedy). For DRD4, 65.2% of the children and 67.0% of the mothers were carriers of the 7-repeat allele.
Maternal Sensitivity
The Ainsworth Maternal Sensitivity Scales are a reliable and validated (Ainsworth, et al., 1978) gold-standard measure of sensitivity. The measure includes four nine-point Likert rating scales: Cooperation, Accessibility, Acceptance, and Sensitivity. Video-taped mother-child interactions were coded by research assistants and then compared to videos coded by an expert coder. Interclass correlation for the Ainsworth mean score at 6 months, which we use in this study, was 0.88 (N=28) (lab of L Atkinson). The mean Ainsworth maternal sensitivity scale was 5.61 (SD 2.0).
Maternal behaviour
Second by second behaviours observed during mother-infant interaction were coded using the BEST coding system (Educational Consulting, Inc. Florida, US) (S & K NorPark Computer Design, Toronto). This analysis generated duration and frequency data for multiple maternal behaviours by use of a computer keyboard with keys indexed for each behaviour. Coded behaviours include frequency and duration of looking away from the infant, vocalizing to the infant (quiet talk, motherese, singing, adult talk), and instrumental caregiving (burping, wiping face, adjusting blanket, grooming the infant). These behaviours and coding scheme have been used in our past research (Giardino, Gonzalez, Steiner, & Fleming, 2008; Krpan, Coombs, Zinga, Steiner, & Fleming, 2005; Mileva-Seitz et al., 2011). Inter-rater reliability was obtained by having two observers code the same 18 videos of mother-infant interactions twice. Inter-rater reliability was high, with r values ranging from 0.67 to 0.96 across all behaviours, and 0.74 to 0.90 for looking away frequency and duration. Also, intra-rater reliability was computed, based on the second observer independently coding 10 videotapes of mothers interacting with their infants on two separate occasions. All of the behaviours analyzed were highly correlated, with r values ranging from 0.821 to 1.0 (lab of A Fleming). On average mothers looked away 21.5 times and for a total of 133.2 seconds during the videotape interaction.
These looking away scores have been validated against dimensional ratings of maternal sensitivity, as described above (Mileva-Seitz, et al., 2013). As well, dopamine DRD1 SNPs are associated with maternal orienting away (Mileva-Seitz, et al., 2012). ANOVAs with Tukey’s post hoc tests showed the heterozygote group oriented away from the infant significantly less frequently compared with the other homozygous genotypes in rs265981 and rs686, and trended in the same direction for rs4532. Mileva et al (2012) showed with respect to DRD1 that mothers carrying one copy of haplotype 1 and one copy of haplotype 12 had lower levels of orienting away. Mileva et al. (2012) concluded that orienting away, infant-directed vocalizing, and sensitivity are likely separate but overlapping components of the complex maternal phenotype, akin to endophenotypes in psychiatric research. Mileva et al. (2012) argued that lower rates of orienting away are indicative of lesser maternal distractibility and greater maternal sustained attention on the infant, an argument strengthened by the negative correlation between orienting away and maternal sensitivity (Mileva-Seitz, et al., 2013).
In general frequency and duration of looking away are correlated with one another and tend to show effects in the same direction (Table 2). Frequency was a more direct measure of mothers’ inattention.
Table 2.
Correlation table for variables predicting Disorganized attachment
| CESD (Prenatal) | Birth size (Percentile) | Birth size squared (Percentile) | DRD4 | Ainsworth sensitivity (6 months) | Look away from baby (Frequency) | Look away from baby (Duration) | Maternal age at birth | CESD (36 months) | |
|---|---|---|---|---|---|---|---|---|---|
| CESD (Prenatal) | 1.00000 | 0.06208 | −0.08623 | −0.08596 | −0.09456 | −0.07620 | 0.03850 | −0.07560 | 0.50442 |
| 0.4144 | 0.2565 | 0.1220 | 0.2314 | 0.3162 | 0.6130 | 0.3200 | <.0001 | ||
| Birth size (Percentile) | 0.06208 | 1.00000 | −0.18430 | 0.05203 | 0.12504 | −0.01909 | 0.09780 | 0.09430 | 0.12722 |
| 0.4144 | 0.0130 | 0.3111 | 0.1063 | 0.7987 | 0.1903 | 0.2067 | 0.0879 | ||
| Birth size squared (Percentile) | −0.08623 | −0.18430 | 1.00000 | 0.02586 | −0.05241 | 0.00297 | −0.01732 | −0.06164 | −0.01191 |
| 0.2565 | 0.0130 | 0.6149 | 0.4998 | 0.9683 | 0.8170 | 0.4098 | 0.8736 | ||
| DRD4 | −0.08596 | 0.05203 | 0.02586 | 1.0000 | 0.01131 | −0.03868 | −0.00299 | 0.08582 | −0.09371 |
| 0.1220 | 0.3111 | 0.6149 | 0.8420 | 0.5269 | 0.9611 | 0.1180 | 0.0912 | ||
| Ainsworth sensitivity | −0.09456 | 0.12504 | −0.05241 | 0.01131 | 1.00000 | −0.14019 | −0.13677 | 0.05123 | −0.02843 |
| 0.2314 | 0.1063 | 0.4998 | 0.8420 | 0.0699 | 0.0771 | 0.5096 | 0.7145 | ||
| Look-away from baby frequency | −0.07620 | −0.01909 | 0.00297 | −0.03868 | −0.14019 | 1.00000 | 0.43159 | −0.00323 | −0.07358 |
| 0.3162 | 0.7987 | 0.9683 | 0.5269 | 0.0699 | <.0001 | 0.9656 | 0.3249 | ||
| Look-away from baby duration | 0.03850 | 0.09780 | −0.01732 | −0.00299 | −0.13677 | 0.43159 | 1.00000 | −0.06779 | 0.08445 |
| 0.6130 | 0.1903 | 0.8170 | 0.9611 | 0.0771 | <.0001 | 0.3646 | 0.2584 | ||
| Maternal age | −0.07560 | 0.09430 | −0.06164 | 0.08582 | 0.05123 | −0.00323 | −0.06779 | 1.00000 | −0.12585 |
| 0.3200 | 0.2067 | 0.4098 | 0.1180 | 0.5096 | 0.9656 | 0.3646 | 0.0914 | ||
| CESD (36 months) | 0.50442 | 0.12722 | −0.01191 | −0.09371 | −0.02843 | −0.07358 | 0.08445 | −0.12585 | 1.00000 |
| <.0001 | 0.0879 | 0.8736 | 0.0912 | 0.7145 | 0.3249 | 0.2584 | 0.0914 |
Spearman Correlation Coefficients, with probability > |r|
Attachment
The modified separation–reunion procedure described by Cassidy and Marvin with the MacArthur Working Group on Attachment (1992) for preschool-age children was followed. It consists of four episodes lasting 5 min each: (a) separation between mother and child; (b) reunion; (c) second separation; and (d) second reunion. During both separations, the child was left alone. Following the separations, the mother was told to rejoin the child but received no specific instructions concerning the reunions. The separation-reunion sequence took place in a room in which age-appropriate toys were scattered. The attachment classifications (secure, avoidant, ambivalent, disorganized) were based on behaviour observed in both reunions, with details of coding criteria for each classification provided in (Moss, Bureau, Cyr, Mongeau, & St-Laurent, 2004). The criteria for identifying disorganized attachment at preschool age are similar to those identified in Main and Solomon (1990) with the additional criteria of role-reversed behavior with the caregiver of a punitive or caregiving type. Children are subclassified as behaviorally disorganized if they display inexplicable, contradictory or odd behavior in the presence of the caregiver similar to infant disorganized behaviors. Children are subclassified as controlling-punitive if they attempt to control their parent’s behavior in a hostile, role-reversed punitive manner. Those who show role-reversal in a helpful, attentive, caregiving manner are subclassified as controlling-caregiving. Because children in all three disorganized subclassifications lack a coherent strategy to organize emotions and behaviors toward the caregiver at the time of the reunion, they are typically combined with the disorganized group for analyses (Moss et al., 2005).
Overall agreement between the two coders for the major classifications (A, B, C, D) was calculated on 20% of the tapes and excellent inter-rater reliability was obtained (89%, κ = .83, p < .01). Coding is based on information gathered from five modalities: physical proximity and contact, body positioning, speech, gaze and affect. The validity of this procedure for classifying attachment behaviour in children of this age range has been demonstrated in several studies (Moss et al., 2004; Moss et al., 2005, NICHD Early Child Care Network, 2001). In many studies primarily focused on disorganization, A, B and C categories are combined into an organized category (based on the assumption that they involve organized attachment strategies for seeking proximity to the caregiver) enabling a dichotomous comparison with the D (disorganized) group. Attachment was available for 301 children as follows: 166 secure, 40 ambivalent, 20 avoidant and 75 disorganized. Breakdown of the disorganized group in the behaviorally-disorganized, controlling-punitive, and controlling-caregiving groups was 53, 3, and 19, respectively. As is common practice, children in all three disorganized subclassifications were combined into one group. This was justified based on both sample size limitations and the idea that for both behaviorally disorganized and controlling children, the internal working model underlying the behavioral strategy is characterized by disorganization in socio-emotional regulation as evidenced by performance on doll-play and other representational measures of attachment (Moss, St-Laurent, et al., 2011). Missing values were imputed for the logistic regression (see below).
Covariates
The Bayley Scales of Infant Development-Second Edition (Bayley, 1993) was administered at 6, 12 and 18 months of age. The Mental Developmental Index (MDI) and Psychomotor Developmental Index (PDI) were extracted.
Other covariates were obtained from the Health and Well Being of Mothers and their Newborns questionnaire (M. S. Kramer et al., 2009) administered prenatally and at 6, 12, 24 and 36 months postnatally. Postnatal depression was assessed with the CES-D at 6, 12, 24 and 36 months. The Center for Epidemiologic Studies Depression Scale (CES-D), a 20-item self-report measure of depressive symptomatology (Radloff, 1977) validated for pregnancy (e.g.(Davis, Glynn, Waffarn, & Sandman, 2011)). The CES-D items are rated on a 4-point Likert-scale that ranges from “rarely or none of the time” to “most or all of the time.” The highest score is 60 and a score of 16 or higher is suggestive of a depressive disorder. Scores were centered to facilitate interpretation of regression coefficients. Maternal education, assessed prenatally, was dichotomized as ‘University graduate or higher’ or ‘others’. The original categories (Table 1) were collapsed into two groups in light of small sized categories.
Analyses
Logistic Regression
Intraclass correlation (ICC), which depicts the proportion of variance in attachment accounted for by site of recruitment, was estimated to 0 in all analyses. Accordingly, a mixed model was not used. Furthermore, site was not correlated with disorganized attachment. All assumptions for regression were respected. Outliers were assessed with the use of standardized Pearson residual values and were removed if their value was greater than 2.8 (or smaller than −2.8) or greater than 2.00 (or smaller than −2) with a combined leverage larger than 2p/n (Hoaglin & Welsch, 1978).
A logistic regression model was created, with birth weight, child DRD4 genotype and maternal care (separate models for Ainsworth sensitivity, Looking away frequency and Looking away duration), and disorganized attachment as the outcome. Birth weight AGA was treated as a continuous variable (percentile), even when transformed (squared) to reflect a better fitting curvilinear (J-shaped) association. Maternal care variables were treated as continuous and were centered. To assess the effect size of our models we used a McFadden R2. To assess the accuracy of our models we used the area under the curve (AUC), which is the probability of correctly determining which children are disorganized or not. A value between .9 and 1 is considered outstanding, a value between 0.8 and 0.9 is considered excellent, a value between .7 and .8 is considered acceptable and a value below than 0.7 is considered poor.
Covariates were identified by preliminary analyses driven by theoretical conception. Variables were retained as covariates for the final analyses when they were associated with both a predictor and the outcome. This included maternal postnatal depression and maternal education. Child gender and maternal age were retained as a priori covariates. Variables considered as covariates but not retained for the final analyses were maternal alcohol use (not associated) and family income (not as robust a predictor as maternal education). Since allele frequency distributions can differ across ethnic groups (Kidd et al., 1998) and heterogeneous ancestry samples can reduce power (Tian, Gregersen, & Seldin, 2008), ancestry was also considered. We ran our models with and without the non-white Caucasian subjects. We also examined a model where white race was entered as a covariate. The results were similar in all cases. All results are for the entire sample and are adjusted for the relevant covariates.
Multiple imputation
Missing values were imputed for the logistic regression using the MICE (multivariate imputation by chained equations) algorithm (van Buuren & Groothuis-Oudshoorn, 2011). The imputation model was used to explain the pattern of missing data and to obtain imputed values for these missing data and included the following variables: all variables used in the regression including maternal prenatal CESD, prenatal income, prenatal alcohol intake and the use of psychotropic medication during pregnancy. No variable had to be removed because of excessive missing data. Imputed values were based on regression estimates. As recommended, five imputed data sets were created. The quality of the imputations depends on the amount of missing data. When the amount of missing data does not exceed 50%, 5 imputations are enough to obtain valid estimates (Schafer, 1999). R software (version 2.7.2; The R Foundation for Statistical Computing, Vienna, Austria) was used to perform imputation; all other analyses were performed using SPSS statistical software (version 15.0; SPSS Inc, Chicago, Illinois). Estimates were not biased by the imputation since executing the models with the subset of subject with complete measures yielded the same results and even a model with a slightly better fit. Both models (with and without imputed data) are presented.
RESULTS
Covariates of D
Gender was not associated with D (χ2 = .93, df = 1, p = .33). As expected, there were significant effects for maternal education (χ2, df =6, 21.070, p=0.0014), with higher D in children whose mothers had less than university education. Income was also associated with D (χ2, df = 12, 28.852, p=0.0041), such that children from lower income homes were more likely to be disorganized. There was no association with maternal age, prenatal alcohol consumption or prenatal maternal depression. However children with D had higher maternal depression scores on the CESD (14.9 (SD=10.7)) at the 36 month time point of attachment than children without D (10.9 (SD=9.57); p=0.0068)
Gene-environment correlation
There was no significant association between birthweight AGA (percentile) and maternal care at 6 months, be it Ainsworth sensitivity (r=0.047, p=0.3149), frequency of looking away behaviour (r=−0.012, p=0.8091) or duration of looking away behaviour (r=0.082, p= 0.1266). This also applied for DRD4, with no association between the presence of 7R and Ainsworth sensitivity (r=0.011, p=0.8420), frequency of looking away behaviour (r=−0.039, p=0.5269) or duration of looking away behaviour (r=−0.003, p= 0.9611). Therefore, we have no reason to suspect that the child’s constitutional factors evoked the observed variations in maternal care, albeit only DRD4 was tested. There was also no relation between mother’s DRD4 and measures of maternal care, suggesting maternal DRD4 genotype did not better explain the association between maternal care and child disorganized attachment.
Main effect of birth weight
There was no association between birthweight AGA and disorganized attachment (D), using a categorical (r = −.08, p = .3) measure of D. Actually none of the analyses reported here were significant when birthweight AGA was entered, without transformation. Consistent with recent publications (Alati et al., 2009; Broekman, et al., 2011; van Mil, et al., 2015) reporting a curvilinear relationship between birthweight and psychopathology, birthweight was centered and squared ((birthweight – 50)2). All analyses with birthweight hitherto refer to birthweight transformed (centered and squared). This allowed for high and low value of birthweight (e.g. - 30th percentile and 70th percentile) to be treated equally. There was no association between the transformed birthweight AGA and D (t = .41, df = 179, p = .68).
Moderation of birthweight by genotype
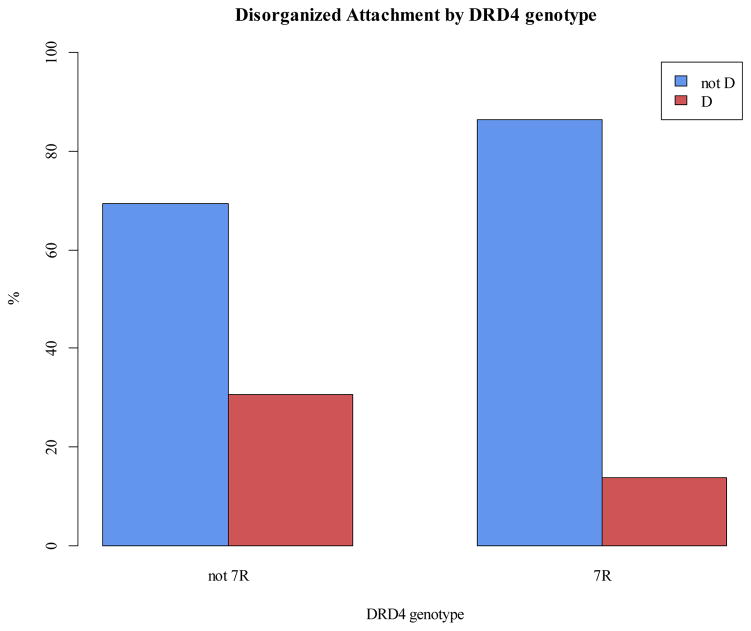
There was a strong negative association between 7R and D (χ2 = 16.88, df = 1, p < .0001). Almost all cases of D were found in children without a 7R (Figure 1). In a two-way interaction model (χ2 = 14.49, df = 3, p = .002) examining the prediction of D from birthweight AGA and DRD4, the interaction term of birthweight AGA and DRD4 was not significant (β = −.0007, p = .24). The lack of a moderation of birthweight by genotype was found consistently across all our models.
Figure 1.
Disorganized attachment by DRD4 genotype
Moderation of the effects of birthweight by maternal care
There was no main effect of maternal care as measured by maternal looking away frequency and duration, and Ainsworth maternal sensitivity. The two-way interaction model (F(4,557) = 5.07, p < .0001) examining the prediction of D from birthweight AGA and maternal looking away frequency was significant (Table 3, Step 2). Although there were trends for maternal looking away duration, and Ainsworth maternal sensitivity, maternal looking away frequency produced the best model (lowest AIC). Increased looking away frequency was associated with increased probability of D in children with lower birthweight (squared) AGA. Adding covariates to the model (Table 3, Step 3) did not change the results, the model remained significant (F(9,1056) = 4.96, p < .0001) and the parameters of DRD4 (β = −1.06; p, .01), and the interaction between birthweight and maternal looking away remained significant (β = −.00004; p < .05).
Table 3.
The prediction of Disorganized Attachment from the interactions of birth weight x looking away frequency, birth weight x looking away duration and birth weight x Ainsworth sensitivity
| Predictors | Looking away frequency | Looking away frequency | Looking away frequency | Looking away duration | Ainsworth sensitivity |
|---|---|---|---|---|---|
| Step 1 | Step 2 | Step 3 | Step 3 | Step 3 | |
| Birth weight (centered and squared) | −.0002 | .001* | .001* | .0009* | −.001 |
| Maternal sensitivity/behaviour | .02 | .07** | .08** | .007* | −.25t |
| DRD4 | −2.57*** | −2.75*** | −2.69*** | −2.24*** | −2.33** |
| Birth weight (centered and squared) X frequency of looking away | - | −.00006* | −.00007** | −.00001** | .0002 |
| Covariates | |||||
| Postnatal depression | - | - | .02 | .01 | .03t |
| Maternal education – College | - | - | −1.51* | −1.38* | −1.22* |
| Maternal education – University | - | - | −.63 | −.61 | −.57 |
| Gender | - | - | −.01 | .16 | −.08 |
| Mother age of birth | - | - | −.01 | .00009 | −.05 |
| McFadden R2 | .13 | .17 | .21 | .18 | .16 |
| AUC | .72 | .78 | .8 | .8 | .78 |
Note: In looking away frequency step 1 χ2(3) = 23.95***, in looking away frequency step 2 χ2(4) = 30.8***, in looking away frequency step 3 χ2(9) = 38.75***, in looking away duration step 3 χ2(9) = 34.85*** and in Ainsworth sensitivity step 3 χ2(9) = 34.64***,
p < .10,
p < .05,
p < .01,
p < .001
Three way interaction/Best model
The three-way interaction model (χ2 = 36.93, df = 7, p < .0001) did not better explain our results. There was no significant interaction between birthweight AGA, DRD4 and maternal care. The data were best explained by a model which included the two-way interaction of birthweight and maternal looking away frequency as well as the main effect of DRD4 (Table 3). Analyses with imputed data revealed a similar model (Table 4).
Table 4.
The prediction of Disorganized Attachment from the interaction of birth weight and looking away frequency using Multiple Imputation.
| Predictors | Step 1 | Step 2 | Step 3 |
|---|---|---|---|
| Birth weight (centered and squared) | .00006 | .0008* | .0008* |
| Frequency of looking away | .02 | .05** | .05** |
| DRD4 | −.94** | −.97** | −1.08** |
| Birth weight (centered and squared) X frequency of looking away | - | −.00004* | −.00004* |
| Covariates | |||
| Postnatal depression | - | - | .03 |
| Maternal education – College | - | - | −1.91*** |
| Maternal education – University | - | - | −1.33** |
| Gender | - | - | .06 |
| Mother age of birth | - | - | −.02 |
| McFadden R2 | .04 | .06 | .17 |
Note: In step 1 F(3,435) = 4.29**, in step 2 F(4,589) = 4.65** and in step 3 F(9,1147) = 4.87***,
p < .10,
p < .05,
p < .01,
p < .001
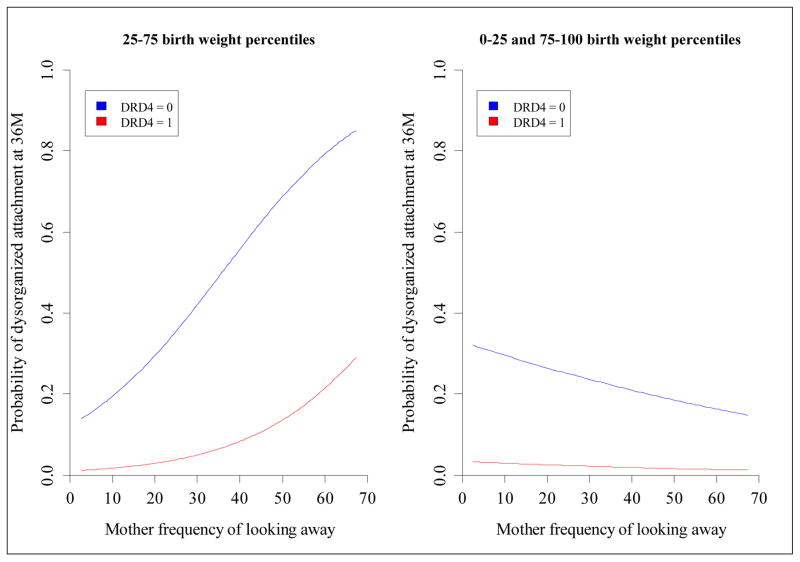
Figure 2 depicts how looking away frequency differentially influences the probability of D as a function of birthweight AGA. To better characterize the interaction we conducted simple slope analyses (Aiken & West, 1991), the birthweight AGA variable was evenly divided into midrange (25th to 75th percentile) and extreme range (<25th and >75th percentile). Translating this back to untransformed birthweight, children with birthweight AGA in the midrange were more likely to develop a disorganized attachment when exposed to less sensitive maternal care, in the form of more frequent looking away (simple slope analysis: β = 0.064, p = 0.0055). However, for children at either extremity of the birthweight range, there was no association, such that the probability of D remained the same, irrespective of looking away behaviour (simple slope: β = −0.0436, p = 0.1393). Other measures of maternal attunement moderated birthweight AGA less significantly (duration of maternal looking away behaviour) or not at all (Ainsworth sensitivity or frequency/duration of vocalizations).
Figure 2.
The prediction of Disorganized Attachment at 36 months from Mother looking away frequency at 6 months and DRD4 7R allele status, for average birth weight and extreme birth weight children
The results in Figure 2 are presented separately for DRD4 7R and non-7R to underline how significant the main effect of DRD4, sometimes up to three-fold, in spite of the absence of a three-way interaction. In the final model, having a 7R allele was associated with a decreased probability of D. Maternal education was also associated with a decreased probability of D (β = −1.51; p = .02). The AUC of our final model was very good (AUC = .8, se = .04). Around 80% of the children where correctly assigned as disorganized or not based on our model. Therefore our model has good accuracy.
DISCUSSION
Our findings suggest that a main effect of DRD4 polymorphism and an interaction effect of birthweight (adjusted for gestational age) and maternal care at 6 months, specifically maternal looking away behaviour, predict disorganized attachment at 36 months. These unique findings are strengthened by a prenatal longitudinal design, independent and objective measurements of all the variables, detailed measures of maternal care as well as complementary and novel analyses.
Three findings stand out. First, we did not find a main effect of birthweight or of maternal care as measured by looking away behaviour on disorganized attachment. Second, we did find that birthweight and maternal care interacted to predict disorganized attachment. Specifically, the effect of birthweight on D at 36 months of age was moderated by the how much the mother looked away from her infant at 6 months of age. This is consistent with evidence that prenatal experience significantly influences child development and socio-emotional functioning. It is already established that birthweight is associated with an increased risk for cardiovascular and endocrine conditions (Barker, 2004) as well as psychopathology (Schlotz & Phillips, 2009). This is the first evidence that birthweight predicts the child’s attachment organization in certain contexts of maternal care. One wonders whether the organism with greater growth associated pressures (at either end), might be affected similarly in how it experiences the environment. Although the role of child factors in the prediction of D is not a novel finding, much of the literature has focused on the role of genotype. This is the first study to our knowledge to consider the role of birthweight.
The role of maternal behaviour in the prediction of disorganized attachment is also consistent with the extant literature (Hesse & Main, 2006). Extreme parental insensitivity, (Bakermans-Kranenburg & van Ijzendoorn, 2011; Laucht, et al., 2001; Moss, St-Laurent, et al., 2011), attentional inflexibility (Atkinson, et al., 2009) and lack of comforting maternal-infant contact (Weiss, et al., 2000) have been associated with development of disorganized attachment. Our findings suggest that the effect of maternal care is contingent on an important child factor, i.e. birthweight. Maternal care and specifically maternal looking away frequency, was associated with disorganized attachment only when birthweight was within the midrange. This suggests that the effect of maternal behaviour and early environmental experiences do not operate independently of the child.
Of particular interest is the finding that child birthweight moderated the effect of maternal care, such that poorer care predicted disorganisation only for children with normal range birthweight. Whereas we had hypothesized that extremes of birthweight would more likely be associated with higher D, we found the reverse association. Children with midrange birthweight had a greater probability of disorganized attachment when maternal looking away behaviour increased. Children in the extreme ranges however were influenced minimally by maternal looking away behaviour. It is possible that with greater birthweight pressures, these extreme birthweight children are less susceptible to interactive influences on development of social-emotional and cognitive processes at that period (6 months) but may be so at a later point in development.
Another interesting hypothesis is that more neglectful parental behaviour may prepare the extreme birthweight offspring for adverse surroundings by causing elevated levels of glucocorticoids, fearfulness, and vigilance that promote detection of potential threat and avoidance learning. These mechanisms are potentially helpful in an environment where one must struggle for survival (Avinun & Knafo, in press; Evans, 2004). However, for normally-developing children this is the beginning of the period (6–12 months) when the attachment system develops rapidly and particular secure/insecure patterns emerge. These patterns emerge from the degree of synchronization of maternal care with the infant’s need to maintain equilibrium between dependency and exploratory needs. In this sense, high levels of maternal looking away behaviour are an indication of the disrupted parental affective communication which has been shown to predict disorganized attachment by 12 months of age (Lyons-Ruth & Jacobvitz, 2008).
Third, we found, across all models, that DRD4 7R was protective against D. In contrast, in the literature, the 7R variant is either not associated with D or is associated with an increased probability of D, as was reported by Lakatos (2002) in the Hungarian sample or by Cicchetti et al. (2011) for children with no maltreatment history. Even in GxE studies where DRD4 is reported to interact with maternal care (Bakermans-Kranenburg & van Ijzendoorn, 2006) or unresolved trauma (Van IJzendoorn & Bakermans-Kranenburg, 2006), the 7R variant has been the susceptible allele. The 7R variant has only been associated with a decreased risk for D in maltreated children (Cicchetti, et al., 2011), or in those exposed to disruptive maternal affective behaviours (Gervai, et al., 2007), the explanation being that the 7R genotype was less relevant when children experienced extremely adverse environments. It is unlikely that our finding is explained by levels of maltreatment in our low risk sample (not considered in our models) or disruptive maternal behaviours (considered in our models). There is evidence nonetheless for the protective role of Dopamine 7R in a community sample. Ebstein et al (1998) found the 7R variant is associated with better infant orientation and state regulation. Our findings add to the complexity of the literature about the association of DRD4 with disorganized attachment, especially as one extends the developmental model into the preschool age. The inclusion of a significant child co-factor (ie child birthweight) seems to increase the complexity of the interpretation but underscores the idea that GxE interactions must be interpreted in light of specific characteristics of the child.
Overall, results are most parsimoniously interpreted in the context of attention, a construct considered central to attachment theory (Atkinson, et al., 2009). The whereabouts of the attachment figure are continuously monitored by all infants (Bretherton, 1980; Maier, et al., 2005) and the variance among them is explained by the attachment patterns they adopt. Furthermore, dopamine has been implicated in the relation between maternal attention and disorganized attachment (Atkinson, et al., 2009). Dopamine is involved in selective attention (which involves simultaneous inhibition and direction of attentional processes) and in suppressing irrelevant responses and selecting newly appropriate behaviours (Winstanley, Theobald, Dalley, & Robbins, 2005). Disorganized individuals show a breakdown of both attentional (Atkinson, et al., 2009) and behavioural systems. With respect to the latter, disorganization is defined as the collapse of attachment strategy under conditions of stress; under such conditions, disorganized individuals select a set of behaviours that are irrelevant to their need for downregulation of discomfort (Hesse & Main, 2006). Moreover, dopamine plays an important role in consolidating stimulus traces under conditions of extreme stress (Oades, 1985), chronically experienced by disorganized babies, and interferes with future function under stress conditions. More specifically, and based in part on evidence that the DRD4 gene is implicated in attentional, cognitive and emotional processes, several studies (Gervai, et al., 2005; Lakatos, et al., 2002; Lakatos, et al., 2000; Van IJzendoorn & Bakermans-Kranenburg, 2006) support DRD4 involvement in attachment disorganization, as discussed above.
Moreover, in the context of mother-child behaviour, “looking away” serves as a fundamental, behavioural instantiation of attention. It has been argued that inattention (avoidance) is a sufficient condition for maternal insensitivity, given that it precludes perception of infant signals (Atkinson, et al., 1995; David R. Pederson et al., 1990). Of interest in the present study, maternal looking away behaviour modified the impact of birth weight more strongly than a fuller measure of maternal sensitivity, a particularly interesting phenomenon given that the interaction was studied in the context of a dopamine gene known to influence attention.
Finally, there is the issue of prenatal programming as it pertains to disorganization. The question is, why would a fetus prepare itself for disorganization? Given the disruptions to controlled attention, discussed above, what could the possible advantages of disorganization be? Atkinson et al. (2009) made the following argument. The disorganized infant feels him/herself to be under threat because the caregiver is either frightened or frightening. Under such conditions of threat, it may be advantageous to shut down controlled processing in favor of habitual, environmentally dependent processes that have ensured survival in the past (Arnsten, 1998). In fact, controlled processes, attentional flexibility foremost among them, are often downgraded during stress while automatic processes are enhanced, especially under conditions where the individual has little control, as would be the case for the infant under conditions of helpless/hostile caregiving. Furthermore, dopamine plays a particularly important role in the selection of controlled versus automatic processing (Arnsten, 1998). Overall, these considerations may explain why the infant prepares him/herself for disorganization prenatally, why the DRD4 gene plays an important role in the disorganization outcome, and why maternal behaviour provides the context necessary to this outcome.
Conceptualizing our findings within the context of attention also helps link the processes described here to psychopathology more broadly (Atkinson, et al., 2009). Attentional deficits serve to cause and maintain emotional disturbance (Posner & Rothbart, 2000). Williams et al. (1996) proposed that attentional bias contributes to an iterative process whereby slight increases in emotional difficulty increase the salience of particular stimuli, which in turn, magnifies the emotional power of those stimuli. It seems likely, then, that the automatic attentional bias of disorganized individuals toward negative attachment experiences magnifies concern about these experiences such that they increasingly preclude broader attention allocation and become psychopathological. The present data show that these processes are not driven by maternal behaviour alone, but by aspects of the child, including genetic and prenatal biological factors, in interaction with maternal factors, in a cycle of mutual influence.
Limitations
The interpretation of our findings should be made in light of certain limitations. Our results indicate that maternal care and birthweight interacted to predict D. Although many confounding pathways were not significant in our analyses, it still remains possible that other unmeasured aspects of the child evoked changes in maternal behaviour (identified or not) thus leading to disorganized attachment. Moreover, in future research with larger samples, it will be interesting to delineate the pathways leading to the different sub-types of disorganization seen at preschool and early school-age ie. controlling-punitive, controlling-caregiving and behaviorally disorganized.
When compared to other genetic studies, the MAVAN has a relatively smaller number of participants. Our power, however, is strengthened by the accuracy of our genotyping method (Wong, Day, Luan, Chan, & Wareham, 2003), precise functional sub-categorization of the DRD4 allele (7R or not), and observational measures of maternal care. Nonetheless, meaningful G×E effects might have been undetected in this study as a result of insufficient statistical power. Conversely the risk of Type I errors can emerge from the use of three operationalizations of caregiving quality and two operationalizations of birth weight (linear and curvilinear). Although the risk was minimized by theory driven analysis, sparse models with specified analytic steps, and the convergence of the findings across three slightly different measures of the parenting construct, the replication of such striking findings will be essential.
Finally, we only examine a monogenic model. There is growing evidence for the interaction of genes (GxG) and specifically the association of DRD4 with 5HTTLPR (Ebstein, et al., 1998) but also with MAO (Serretti et al., 2002) and COMT (Olsson et al., 2007). One interesting possibility, for example, would involve norepenephrine-related genes, given that norepenephrine acts in concert with dopamine to influence attentional processes and likely attachment disorganization (Atkinson, et al., 2009).
Future Directions for Translating Research on the Influential Child into Preventive Interventions
These results highlight the importance of considering the complex interplay of parenting and child factors in understanding the complex pathways toward psychopathology. They also highlight the importance of individualizing intervention efforts in order to prevent the onset of disorganization in early childhood. In this respect, intervention programs oriented directly at increasing the predictability, consistency and warmth of parental behaviour toward the child which have been shown to reduce disorganization (eg. (Cicchetti, Rogosch, & Toth, 2006; Moss et al., 2011)) must be implemented with an eye on developmental timing and particular child needs. Two findings stand out in providing more precise directions as the population such interventions should target. One, the absence of the 7R allele of DRD4 increased the risk for D. Two, the presence of higher looking away behaviours in children in mid-ranges of birthweight also increased the risk for D. However, since both of these findings are novel, they would have to be reproduced before they could be instrumentalized into more precise strategies of prevention.
With approaches such as video feedback (Juffer, Bakermans-Kranenburg, & van Ijzendoorn, 2008; Moss et al., 2014), parents are coached in becoming attentive to child responses to their interventions which guide them in adjusting their behaviour in an individualized child-sensitive manner. Our findings also suggest that outcomes of such programs must always be assessed using child measures over time, rather than parental measures such as stress-reduction. Given that the pathway towards disorganized attachment appears to be complex involving interplay of biological, genetic and parenting factors, successful prevention programs must address the particular needs of the child. Accordingly, research is also needed on the impact of such programs with children with different birthweight status and genetic dispositions. Considering multiple child factors instead of single factors may yield different interpretations of the efficacy of such programs for individual children.
Acknowledgments
This research was made possible by grants from the Canadian Institutes of Health Research, the March of Dimes Foundation and the Fonds de Research du Quebec. The MAVAN project has been supported by funding from the McGill Faculty of Medicine, the Blema & Arnold Steinberg Family Foundation, and the Canadian Institutes for Health Research
We would like to thank all members and participants of the Maternal Adversity, Vulnerability, and Neurodevelopment (MAVAN) project for their time and commitment to this research. We would also like to thank David Brownlee, Vincent Jolivet, Amber Rieder and Patricia Szymkow for their contributions.
Footnotes
No Conflicts of Interest to Report
References
- Ainsworth M, Blehar M, Waters E, Wall S. Patterns of attachment: A psychological study of the Strange Situation. Hillsdale NJ: Erlbaum; 1978. [Google Scholar]
- Alati R, Najman JM, O’Callaghan M, Bor W, Williams GM, Clavarino A. Fetal growth and behaviour problems in early adolescence: findings from the Mater University Study of Pregnancy. International journal of epidemiology. 2009;38(5):1390–1400. doi: 10.1093/ije/dyp252. [DOI] [PubMed] [Google Scholar]
- Armbruster D, Mueller A, Moser DA, Lesch KP, Brocke B, Kirschbaum C. Interaction effect of D4 dopamine receptor gene and serotonin transporter promoter polymorphism on the cortisol stress response. Behavioral neuroscience. 2009;123(6):1288–1295. doi: 10.1037/a0017615. [DOI] [PubMed] [Google Scholar]
- Arnsten AF. Catecholamine modulation of prefrontal cortical cognitive function. Trends in cognitive sciences. 1998;2(11):436–447. doi: 10.1016/s1364-6613(98)01240-6. [DOI] [PubMed] [Google Scholar]
- Atkinson L, Gonzalez A, Kashy DA, Santo Basile V, Masellis M, Pereira J, et al. Maternal sensitivity and infant and mother adrenocortical function across challenges. Psychoneuroendocrinology. 2013;38(12):2943–2951. doi: 10.1016/j.psyneuen.2013.08.001. [DOI] [PubMed] [Google Scholar]
- Atkinson L, Leung E, Goldberg S, Benoit D, Poulton L, Myhal N, et al. Attachment and selective attention: disorganization and emotional Stroop reaction time. Development and psychopathology. 2009;21(1):99–126. doi: 10.1017/S0954579409000078. [DOI] [PubMed] [Google Scholar]
- Atkinson L, Niccols A, Paglia A, Coolbear J, Parker HKC, Poulton L, et al. A Meta-Analysis of Time between Maternal Sensitivity and Attachment Assessments: Implications for Internal Working Models in Infancy/Toddlerhood. Journal of Social and Personal Relationships. 2000;17(6):791–810. [Google Scholar]
- Atkinson L, Paglia A, Coolbear J, Niccols A, Parker KC, Guger S. Attachment security: a meta-analysis of maternal mental health correlates. Clinical psychology review. 2000;20(8):1019–1040. doi: 10.1016/s0272-7358(99)00023-9. [DOI] [PubMed] [Google Scholar]
- Atkinson L, Paglia A, Coolbear J, Niccols A, Poulton L, Leung E, et al. L’ évaluation de la sensibilité maternelle dans le contexte de la sécurité d’attachment: Une méta-analyse. [Assessing maternal sensitivity in the context of attachment security: A meta-analysis.] In: Tarabulsy GM, Larose S, Pederson DR, Moran G, editors. Attachement et développement: Le rôle des premieres relations dans le développement humain. [Attachment and development: The role of first relationships in human development.] Québec, Canada: Presses de l’Université du Québec; 2000. pp. 27–56. [Google Scholar]
- Atkinson L, Scott B, Chisholm V, Blackwell J, Dickens S, Tam F, et al. Cognitive coping, affective distress, and maternal sensitivity: Mothers of children with Down syndrome. Developmental psychology. 1995;31(4):668–676. [Google Scholar]
- Avinun R, Knafo A. Socialization, Genetics and their Interplay in Development. In: Grusec JE, Hastings P, editors. Handbook of Socialization. Guilford; (in press) [Google Scholar]
- Bakermans-Kranenburg MJ, Van Ijzendoorn MH. No association of the dopamine D4 receptor (DRD4) and -521 C/T promoter polymorphisms with infant attachment disorganization. Attachment & human development. 2004;6(3):211–218. doi: 10.1080/14616730412331281584. discussion 219–222. [DOI] [PubMed] [Google Scholar]
- Bakermans-Kranenburg MJ, van Ijzendoorn MH. Gene-environment interaction of the dopamine D4 receptor (DRD4) and observed maternal insensitivity predicting externalizing behavior in preschoolers. Developmental psychobiology. 2006;48(5):406–409. doi: 10.1002/dev.20152. [DOI] [PubMed] [Google Scholar]
- Bakermans-Kranenburg MJ, van Ijzendoorn MH. Differential susceptibility to rearing environment depending on dopamine-related genes: new evidence and a meta-analysis. Development and psychopathology. 2011;23(1):39–52. doi: 10.1017/S0954579410000635. [DOI] [PubMed] [Google Scholar]
- Barker DJ. The developmental origins of adult disease. Journal of the American College of Nutrition. 2004;23(6 Suppl):588S–595S. doi: 10.1080/07315724.2004.10719428. [DOI] [PubMed] [Google Scholar]
- Bayley N. Bayley Scales of Infant Development: Administering and scoring manual. New York: Psychological Corporation; 1993. [Google Scholar]
- Belsky J, Pluess M. The Nature (and Nurture?) of Plasticity in Early Human Development. Persp on Psychol Sci. 2009;4(4):345–351. doi: 10.1111/j.1745-6924.2009.01136.x. [DOI] [PubMed] [Google Scholar]
- Bretherton I. Young Children in Stressful Situations: The Supporting Role of Attachment Figures and Unfamiliar Caregivers. In: Coelho G, Ahmed P, editors. Uprooting and Development. Springer US; 1980. pp. 179–210. [Google Scholar]
- Brisch KH, Bechinger D, Betzler S, Heinemann H, Kachele H, Pohlandt F, et al. Attachment Quality in Very Low-Birthweight Premature Infants in Relation to Maternal Attachment Representations and Neurological Development. Parenting. 2005;5(4):311–331. [Google Scholar]
- Broekman BF, Chan YH, Goh L, Fung D, Gluckman PD, Saw SM, et al. Influence of birth weight on internalizing traits modulated by serotonergic genes. [Research Support, Non-U.S. Gov’t] Pediatrics. 2011;128(5):e1250–1258. doi: 10.1542/peds.2010-3714. [DOI] [PubMed] [Google Scholar]
- Carlson EA. A prospective longitudinal study of attachment disorganization/disorientation. Child development. 1998;69(4):1107–1128. [PubMed] [Google Scholar]
- Challis JR, Sloboda D, Matthews SG, Holloway A, Alfaidy N, Patel FA, et al. The fetal placental hypothalamic-pituitary-adrenal (HPA) axis, parturition and post natal health. Molecular and cellular endocrinology. 2001;185(1–2):135–144. doi: 10.1016/s0303-7207(01)00624-4. [DOI] [PubMed] [Google Scholar]
- Cicchetti D, Rogosch FA, Toth SL. Fostering secure attachment in infants in maltreating families through preventive interventions. Development and psychopathology. 2006;18(3):623–649. doi: 10.1017/s0954579406060329. [DOI] [PubMed] [Google Scholar]
- Cicchetti D, Rogosch FA, Toth SL. The effects of child maltreatment and polymorphisms of the serotonin transporter and dopamine D4 receptor genes on infant attachment and intervention efficacy. Development and psychopathology. 2011;23(2):357–372. doi: 10.1017/S0954579411000113. [DOI] [PubMed] [Google Scholar]
- Costello EJ, Worthman C, Erkanli A, Angold A. Prediction from low birth weight to female adolescent depression: a test of competing hypotheses. Archives of General Psychiatry. 2007;64(3):338–344. doi: 10.1001/archpsyc.64.3.338. [DOI] [PubMed] [Google Scholar]
- Davis EP, Glynn LM, Waffarn F, Sandman CA. Prenatal maternal stress programs infant stress regulation. Journal of child psychology and psychiatry, and allied disciplines. 2011;52(2):119–129. doi: 10.1111/j.1469-7610.2010.02314.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- de Wolff MS, van IJzendoorn MH. Sensitivity and attachment: A meta-analysis on parental antecedents of infant attachment. Child Development. 1997;68:571–591. [PubMed] [Google Scholar]
- Derryberry D, Rothbart MK. Emotion, attention, and temperament. In: Izard C, Kagan J, Zajonc R, editors. Emotion, cognition, and behavior. Cambridge: Cambridge University Press; 1984. pp. 132–166. [Google Scholar]
- Easterbrooks MA. Quality of Attachment to Mother and to Father: Effects of Perinatal Risk Status. Child development. 1989;60(4):825–830. [Google Scholar]
- Ebstein RP, Levine J, Geller V, Auerbach J, Gritsenko I, Belmaker RH. Dopamine D4 receptor and serotonin transporter promoter in the determination of neonatal temperament. Molecular psychiatry. 1998;3(3):238–246. doi: 10.1038/sj.mp.4000363. [DOI] [PubMed] [Google Scholar]
- Ellis BJ, Boyce WT. Biological Sensitivity to Context. Current Directions in Psychological Science. 2008;17(3):183–187. [Google Scholar]
- Evans GW. The Environment of Childhood Poverty. American Psychologist. 2004;59(2):77–92. doi: 10.1037/0003-066X.59.2.77. [DOI] [PubMed] [Google Scholar]
- Feldman R, Eidelman AI. Parent-infant synchrony and the social-emotional development of triplets. Dev Psychol. 2004;40(6):1133–1147. doi: 10.1037/0012-1649.40.6.1133. [DOI] [PubMed] [Google Scholar]
- Frodi A. Attachment behavior and socialibility with strangers in premature and fullterm infants. Infant Mental Health Journal. 1983;4(1):13–22. [Google Scholar]
- Gervai J, Nemoda Z, Lakatos K, Ronai Z, Toth I, Ney K, et al. Transmission disequilibrium tests confirm the link between DRD4 gene polymorphism and infant attachment. [Research Support, Non-U.S. Gov’t] American journal of medical genetics Part B, Neuropsychiatric genetics: the official publication of the International Society of Psychiatric Genetics. 2005;132B(1):126–130. doi: 10.1002/ajmg.b.30102. [DOI] [PubMed] [Google Scholar]
- Gervai J, Novak A, Lakatos K, Toth I, Danis I, Ronai Z, et al. Infant genotype may moderate sensitivity to maternal affective communications: attachment disorganization, quality of care, and the DRD4 polymorphism. Social neuroscience. 2007;2(3–4):307–319. doi: 10.1080/17470910701391893. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Giardino J, Gonzalez A, Steiner M, Fleming AS. Effects of motherhood on physiological and subjective responses to infant cries in teenage mothers: a comparison with non-mothers and adult mothers. Horm Behav. 2008;53(1):149–158. doi: 10.1016/j.yhbeh.2007.09.010. [DOI] [PubMed] [Google Scholar]
- Glaser D. Child Abuse and Neglect and the Brain—A Review. Journal of Child Psychology and Psychiatry. 2000;41(1):97–116. [PubMed] [Google Scholar]
- Goldberg S, Perrotta M, Minde K, Corter C. Maternal behavior and attachment in low-birth-weight twins and singletons. Child development. 1986;57(1):34–46. doi: 10.1111/j.1467-8624.1986.tb00004.x. [DOI] [PubMed] [Google Scholar]
- Gunnar M, Quevedo K. The Neurobiology of Stress and Development. Annual Review of Psychology. 2007;58(1):145–173. doi: 10.1146/annurev.psych.58.110405.085605. [DOI] [PubMed] [Google Scholar]
- Hesse E, Main M. Frightened, threatening, and dissociative parental behavior in low-risk samples: Description, discussion, and interpretations. Development and psychopathology. 2006;18(2):309–343. doi: 10.1017/S0954579406060172. [DOI] [PubMed] [Google Scholar]
- Hoaglin DC, Welsch RE. The hat matrix in regression and anova. The American Statistician. 1978;32:17–22. [Google Scholar]
- Insel TR. Is social attachment an addictive disorder? Physiology & behavior. 2003;79(3):351–357. doi: 10.1016/s0031-9384(03)00148-3. [DOI] [PubMed] [Google Scholar]
- Jaffe J, Beebe B, Feldstein S, Crown CL, Jasnow MD. Rythms of Dialogue in Infancy. Monographs of the Society for Research in Child Development. 2001:66. [PubMed] [Google Scholar]
- Juffer F, Bakermans-Kranenburg MJ, van Ijzendoorn MH. Promoting positive parenting: An attachment-based intervention (2008) Promoting positive parenting: An attachment-based intervention. New York, NY: Taylor & Francis Group/Lawrence Erlbaum Associates; 2008. p. xix.p. 238. [Google Scholar]
- Kidd KK, Morar B, Castiglione CM, Zhao H, Pakstis AJ, Speed WC, et al. A global survey of haplotype frequencies and linkage disequilibrium at the DRD2 locus. Human genetics. 1998;103(2):211–227. doi: 10.1007/s004390050809. [DOI] [PubMed] [Google Scholar]
- Kramer MS, Lydon J, Seguin L, Goulet L, Kahn SR, McNamara H, et al. Stress pathways to spontaneous preterm birth: the role of stressors, psychological distress, and stress hormones. American journal of epidemiology. 2009;169(11):1319–1326. doi: 10.1093/aje/kwp061. [DOI] [PubMed] [Google Scholar]
- Kramer MS, Platt RW, Wen SW, Joseph KS, Allen A, Abrahamowicz M, et al. A new and improved population-based Canadian reference for birth weight for gestational age. Pediatrics. 2001;108:E35. doi: 10.1542/peds.108.2.e35. [DOI] [PubMed] [Google Scholar]
- Krpan KM, Coombs R, Zinga D, Steiner M, Fleming AS. Experiential and hormonal correlates of maternal behavior in teen and adult mothers. Horm Behav. 2005;47(1):112–122. doi: 10.1016/j.yhbeh.2004.08.006. [DOI] [PubMed] [Google Scholar]
- Lakatos K, Nemoda Z, Toth I, Ronai Z, Ney K, Sasvari-Szekely M, et al. Further evidence for the role of the dopamine D4 receptor (DRD4) gene in attachment disorganization: interaction of the exon III 48-bp repeat and the -521 C/T promoter polymorphisms. Molecular psychiatry. 2002;7(1):27–31. doi: 10.1038/sj.mp.4000986. [DOI] [PubMed] [Google Scholar]
- Lakatos K, Toth I, Nemoda Z, Ney K, Sasvari-Szekely M, Gervai J. Dopamine D4 receptor (DRD4) gene polymorphism is associated with attachment disorganization in infants. [Research Support, Non-U.S. Gov’t] Molecular psychiatry. 2000;5(6):633–637. doi: 10.1038/sj.mp.4000773. [DOI] [PubMed] [Google Scholar]
- Laucht M, Esser G, Schmidt M. Differential development of infants at risk for psychopathology: the moderating role of early maternal responsivity. Dev Med Child Neurol. 2001;43:292–300. doi: 10.1017/s0012162201000561. [DOI] [PubMed] [Google Scholar]
- LeDoux JE. Emotion circuits in the brain. Annual review of neuroscience. 2000;23:155–184. doi: 10.1146/annurev.neuro.23.1.155. [DOI] [PubMed] [Google Scholar]
- Luijk MPCM, Saridjan N, Tharner A, van Ijzendoorn MH, Bakermans-Kranenburg MJ, Jaddoe VWV, et al. Attachment, depression, and cortisol: Deviant patterns in insecure-resistant and disorganized infants. Developmental Psychobiology. 2010;52(5):441–452. doi: 10.1002/dev.20446. [DOI] [PubMed] [Google Scholar]
- Lyons-Ruth K, Jacobvitz D. Handbook of attachment: Theory, research, and clinical applications. 2. New York, NY: Guilford Press; US; 2008. Attachment disorganization: Genetic factors, parenting contexts, and developmental transformation from infancy to adulthood; pp. 666–697. [Google Scholar]
- Lyons-Ruth K, Melnick S, Bronfman E, Sherry S, Llanas L. Attachment issues in psychopathology and intervention. Mahwah, NJ: Lawrence Erlbaum Associates Publishers; US; 2004. Hostile-Helpless Relational Models and Disorganized Attachment Patterns Between Parents and Their Young Children: Review of Research and Implications for Clinical Work; pp. 65–94. [Google Scholar]
- Maccari S, Darnaudery M, Morley-Fletcher S, Zuena AR, Cinque C, Van Reeth O. Prenatal stress and long-term consequences: implications of glucocorticoid hormones. Neuroscience and biobehavioral reviews. 2003;27(1–2):119–127. doi: 10.1016/s0149-7634(03)00014-9. [DOI] [PubMed] [Google Scholar]
- Maier MA, Bernier A, Pekrun R, Zimmermann P, Strasser K, Grossmann KE. Attachment state of mind and perceptual processing of emotional stimuli. Attachment & human development. 2005;7(1):67–81. doi: 10.1080/14616730500039606. [DOI] [PubMed] [Google Scholar]
- Main M. Attachment theory: Social, developmental, and clinical perspectives. Hillsdale, NJ: Analytic Press, Inc; US; 1995. Recent studies in attachment: Overview, with selected implications for clinical work; pp. 407–474. [Google Scholar]
- Main M, Solomon J. Affective development in infancy. Westport, CT: Ablex Publishing; US; 1986. Discovery of an insecure-disorganized/disoriented attachment pattern; pp. 95–124. [Google Scholar]
- Main M, Solomon J. Attachment in the preschool years: Theory, research, and intervention. Chicago, IL: University of Chicago Press; US; 1990. Procedures for identifying infants as disorganized/disoriented during the Ainsworth Strange Situation; pp. 121–160. [Google Scholar]
- Mangelsdorf SC, Plunkett JW, Dedrick CF, Berlin M, Meisels SJ, McHale JL, et al. Attachment security in very low birth weight infants. Developmental psychology. 1996;32(5):914–920. [Google Scholar]
- Meaney MJ, Szyf M, Seckl JR. Epigenetic mechanisms of perinatal programming of hypothalamic-pituitary-adrenal function and health. Trends in molecular medicine. 2007;13(7):269–277. doi: 10.1016/j.molmed.2007.05.003. [DOI] [PubMed] [Google Scholar]
- Mileva-Seitz V, Fleming AS, Meaney MJ, Mastroianni A, Sinnwell JP, Steiner M, et al. Dopamine receptors D1 and D2 are related to observed maternal behavior. Genes, Brain and Behavior. 2012;11(6):684–694. doi: 10.1111/j.1601-183X.2012.00804.x. [DOI] [PubMed] [Google Scholar]
- Mileva-Seitz V, Kennedy J, Atkinson L, Steiner M, Levitan R, Matthews SG, et al. Serotonin transporter allelic variation in mothers predicts maternal sensitivity, behavior and attitudes toward 6-month-old infants. Genes, Brain and Behavior. 2011;10(3):325–333. doi: 10.1111/j.1601-183X.2010.00671.x. [DOI] [PubMed] [Google Scholar]
- Mileva-Seitz V, Steiner M, Atkinson L, Meaney MJ, Levitan R, Kennedy JL, et al. Interaction between oxytocin genotypes and early experience predicts quality of mothering and postpartum mood. [Research Support, Non-U.S. Gov’t] PloS one. 2013;8(4):e61443. doi: 10.1371/journal.pone.0061443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moran G, Forbes L, Evans E, Tarabulsy G, Madigan S. Both Maternal Sensitivity and Atypical Maternal Behavior Independently Predict Attachment Security and Disorganization in Adolescent Mother–infant Dyads. Paper presented at the The International Conference on Infant Studies; 2008. [DOI] [PubMed] [Google Scholar]
- Moss E, Cyr C, Dubois-Comtois K. Attachment at early school age and developmental risk: examining family contexts and behavior problems of controlling-caregiving, controlling-punitive, and behaviorally disorganized children. Developmental psychology. 2004;40(4):519–532. doi: 10.1037/0012-1649.40.4.519. [DOI] [PubMed] [Google Scholar]
- Moss E, Dubois-Comtois K, Cyr C, Tarabulsy GM, St-Laurent D, Bernier A. Efficacy of a home-visiting intervention aimed at improving maternal sensitivity, child attachment, and behavioral outcomes for maltreated children: A randomized control trial. Development and psychopathology. 2011;23(1):195–210. doi: 10.1017/S0954579410000738. [DOI] [PubMed] [Google Scholar]
- Moss E, St-Laurent D. Attachment at school age and academic performance. [Research Support, Non-U.S. Gov’t] Developmental psychology. 2001;37(6):863–874. [PubMed] [Google Scholar]
- Moss E, St-Laurent D, Tarabulsy GM, Bureau J-F. Disorganized attachment and caregiving. New York, NY: Guilford Press; US; 2011. Understanding disorganized attachment at preschool and school age: Examining divergent pathways of disorganized and controlling children; pp. 52–79. [Google Scholar]
- Moss E, Tarabulsy GM, St-Georges R, Dubois-Comtois K, Cyr C, Bernier A, et al. Videofeedback intervention with maltreating parent-child dyads. Attachment & Human Development. 2014;16(4):329–342. doi: 10.1080/14616734.2014.912486. [DOI] [PubMed] [Google Scholar]
- Munafo MR, Yalcin B, Willis-Owen SA, Flint J. Association of the dopamine D4 receptor (DRD4) gene and approach-related personality traits: meta-analysis and new data. Biological psychiatry. 2008;63(2):197–206. doi: 10.1016/j.biopsych.2007.04.006. [DOI] [PubMed] [Google Scholar]
- Nomura Y, Chemtob CM. Conjoined effects of low birth weight and childhood abuse on adaptation and well-being in adolescence and adulthood. Archives of pediatrics & adolescent medicine. 2007;161(2):186–192. doi: 10.1001/archpedi.161.2.186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- O’Donnell KA, Gaudreau H, Colalillo S, Steiner M, Atkinson L, Moss E, et al. The maternal adversity, vulnerability and neurodevelopment project: theory and methodology. Canadian journal of psychiatry Revue canadienne de psychiatrie. 2014;59(9):497–508. doi: 10.1177/070674371405900906. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oades RD. The role of noradrenaline in tuning and dopamine in switching between signals in the CNS. Neuroscience & Biobehavioral Reviews. 1985;9(2):261–282. doi: 10.1016/0149-7634(85)90050-8. [DOI] [PubMed] [Google Scholar]
- Olsson CA, Byrnes GB, Anney RJL, Collins V, Hemphill SA, Williamson R, et al. COMT Val158Met and 5HTTLPR functional loci interact to predict persistence of anxiety across adolescence: results from the Victorian Adolescent Health Cohort Study. Genes, Brain and Behavior. 2007;6(7):647–652. doi: 10.1111/j.1601-183X.2007.00313.x. [DOI] [PubMed] [Google Scholar]
- Pederson DR, Moran G, Sitko C, Campbell K, Ghesquire K, Acton H. Maternal Sensitivity and the Security of Infant-Mother Attachment: A Q-Sort Study. Child development. 1990;61(6):1974–1983. doi: 10.1111/j.1467-8624.1990.tb03579.x. [DOI] [PubMed] [Google Scholar]
- Pederson DR, Moran G, Sitko C, Campbell KGK, Acton H. Maternal sensitivity and the security of infant-mother attachment: a Q-sort study. [Research Support, Non-U.S. Gov’t] Child development. 1990;61(6):1974–1983. doi: 10.1111/j.1467-8624.1990.tb03579.x. [DOI] [PubMed] [Google Scholar]
- Phelps EA, LeDoux JE. Contributions of the amygdala to emotion processing: from animal models to human behavior. Neuron. 2005;48(2):175–187. doi: 10.1016/j.neuron.2005.09.025. [DOI] [PubMed] [Google Scholar]
- Plunkett JW, Klein T, Meisels SJ. The relationship of preterm infant-mother attachment to stranger sociability at 3 years. Infant Behavior and Development. 1988;11(1):83–96. [Google Scholar]
- Posner MI, Rothbart MK. Developing mechanisms of self-regulation. Development and psychopathology. 2000;12(3):427–441. doi: 10.1017/s0954579400003096. [DOI] [PubMed] [Google Scholar]
- Radloff LS. The CES-D scale: A self-report depression scale for research in the general population. Applied Psychological Measurement. 1977;1(3):385–401. [Google Scholar]
- Rice F, Harold GT, Thapar A. The effect of birth-weight with genetic susceptibility on depressive symptoms in childhood and adolescence. Eur Child Adolesc Psychiatry. 2006;15:383–391. doi: 10.1007/s00787-006-0545-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rode SS, Chang P-n, Fisch RO, Sroufe L. Attachment patterns of infants separated at birth. Developmental psychology. 1981;17(2):188–191. [Google Scholar]
- Schafer JL. Multiple imputation: a primer. Statistical methods in medical research. 1999;8(1):3–15. doi: 10.1177/096228029900800102. [DOI] [PubMed] [Google Scholar]
- Schlotz W, Phillips DI. Fetal origins of mental health: evidence and mechanisms. Brain, behavior, and immunity. 2009;23(7):905–916. doi: 10.1016/j.bbi.2009.02.001. [DOI] [PubMed] [Google Scholar]
- Seckl JR, Holmes MC. Mechanisms of disease: glucocorticoids, their placental metabolism and fetal ‘programming’ of adult pathophysiology. Nature clinical practice Endocrinology & metabolism. 2007;3(6):479–488. doi: 10.1038/ncpendmet0515. [DOI] [PubMed] [Google Scholar]
- Serretti A, Cristina S, Lilli R, Cusin C, Lattuada E, Lorenzi C, et al. Family-based association study of 5-HTTLPR, TPH, MAO-A, and DRD4 polymorphisms in mood disorders. American Journal of Medical Genetics. 2002;114(4):361–369. doi: 10.1002/ajmg.10356. [DOI] [PubMed] [Google Scholar]
- Smolla N, Béliveau MJ, Lépine S, Lévesque A, Martin V. Intrauterine Growth Retardation among young psychiatric patients born full-term with birth weights over. 2009;2:500g. (Poster): 30th Congress of the Society of Behavioral Medicine, Montréal. [Google Scholar]
- Spangler G, Johann M, Ronai Z, Zimmermann P. Genetic and environmental influence on attachment disorganization. Journal of Child Psychology and Psychiatry. 2009;50(8):952–961. doi: 10.1111/j.1469-7610.2008.02054.x. [DOI] [PubMed] [Google Scholar]
- Tian C, Gregersen PK, Seldin MF. Accounting for ancestry: population substructure and genome-wide association studies. Human molecular genetics. 2008;17(R2):R143–150. doi: 10.1093/hmg/ddn268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Valero De Bernabe J, Soriano T, Albaladejo R, Juarranz M, Calle ME, Martinez D, et al. Risk factors for low birth weight: a review. [Review] European journal of obstetrics, gynecology, and reproductive biology. 2004;116(1):3–15. doi: 10.1016/j.ejogrb.2004.03.007. [DOI] [PubMed] [Google Scholar]
- Van Batenburg-Eddes T, Brion MJ, Henrichs J, Jaddoe VW, Hofman A, Verhulst FC, et al. Parental depressive and anxiety symptoms during pregnancy and attention problems in children: a cross-cohort consistency study. Journal of child psychology and psychiatry, and allied disciplines. 2013;54(5):591–600. doi: 10.1111/jcpp.12023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- van Buuren S, Groothuis-Oudshoorn K. mice: Multivariate Imputation by Chained Equations in R. Journal of Statistical Software. 2011;45(3) [Google Scholar]
- van den Boom DC. The influence of temperament and mothering on attachment and exploration: An experimental manipulation of sensitive responsiveness among lower-class mothers with irritable infants. Child Development. 1994;65:1457–1477. doi: 10.1111/j.1467-8624.1994.tb00829.x. [DOI] [PubMed] [Google Scholar]
- Van IJzendoorn MH, Bakermans-Kranenburg MJ. DRD4 7-repeat polymorphism moderates the association between maternal unresolved loss or trauma and infant disorganization. Attachment & human development. 2006;8(4):291–307. doi: 10.1080/14616730601048159. [DOI] [PubMed] [Google Scholar]
- van IJzendoorn MH, Schuengel C, Bakermans-Kranenburg MJ. Disorganized attachment in early childhood: meta-analysis of precursors, concomitants, and sequelae. Development and psychopathology. 1999;11(2):225–249. doi: 10.1017/s0954579499002035. [DOI] [PubMed] [Google Scholar]
- Van Lieshout RJ, Boyle MH. Canadian Youth Born Large or Small for Gestational Age and Externalizing and Internalizing Problems. [Article] Naître gros ou petit pour I’âge gestationnel et les problèmes d’externalisation et d’internalisation dans une cohorte de jeunes canadiens. 2011;56(4):227–234. doi: 10.1177/070674371105600406. [DOI] [PubMed] [Google Scholar]
- van Mil NH, Steegers-Theunissen RPM, Motazedi E, Jansen PW, Jaddoe VWV, Steegers EAP, et al. Low and High Birth Weight and the Risk of Child Attention Problems. The Journal of pediatrics. 2015 doi: 10.1016/j.jpeds.2014.12.075. (in press) [DOI] [PubMed] [Google Scholar]
- Wang X, Zhong P, Gu Z, Yan Z. Regulation of NMDA receptors by dopamine D4 signaling in prefrontal cortex. The Journal of neuroscience: the official journal of the Society for Neuroscience. 2003;23(30):9852–9861. doi: 10.1523/JNEUROSCI.23-30-09852.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Waters E, Deane KE. Growing Points of Attachment Theory and Research. Monographs of the Society for Research in Child Development. 1985;50(1/2):41–65. [PubMed] [Google Scholar]
- Wei JN, Li HY, Sung FC, Lin CC, Chiang CC, Li CY, et al. Birth Weight Correlates Differently with Cardiovascular Risk Factors in Youth. Obesity. 2007;15(6):1609–1616. doi: 10.1038/oby.2007.190. [DOI] [PubMed] [Google Scholar]
- Weiss SJ, Wilson P, Hertenstein MJ, Campos R. The tactile context of a mother’s caregiving: implications for attachment of low birth weight infants. Infant Behavior and Development. 2000;23(1):91–111. [Google Scholar]
- Whiteside-Mansell L, Bradley RH, Casey PH, Fussell JJ, Conners-Burrow NA. Triple risk: do difficult temperament and family conflict increase the likelihood of behavioral maladjustment in children born low birth weight and preterm? J Pediatr Psychol. 2009;34(4):396–405. doi: 10.1093/jpepsy/jsn089. [DOI] [PubMed] [Google Scholar]
- Williams JM, Mathews A, MacLeod C. The emotional Stroop task and psychopathology. Psychological bulletin. 1996;120(1):3–24. doi: 10.1037/0033-2909.120.1.3. [DOI] [PubMed] [Google Scholar]
- Winstanley CA, Theobald DE, Dalley JW, Robbins TW. Interactions between serotonin and dopamine in the control of impulsive choice in rats: therapeutic implications for impulse control disorders. Neuropsychopharmacology: official publication of the American College of Neuropsychopharmacology. 2005;30(4):669–682. doi: 10.1038/sj.npp.1300610. [DOI] [PubMed] [Google Scholar]
- Wong MY, Day NE, Luan JA, Chan KP, Wareham NJ. The detection of gene-environment interaction for continuous traits: should we deal with measurement error by bigger studies or better measurement? International journal of epidemiology. 2003;32(1):51–57. doi: 10.1093/ije/dyg002. [DOI] [PubMed] [Google Scholar]