Abstract
Importance
Sleep is vital to children’s bio-psycho-social development. Inadequate sleep quantity and quality is a public health concern with an array of detrimental health outcomes. Portable mobile and media device have become a ubiquitous part of children’s lives and may impact children’s sleep duration and quality.
Objective
This systematic review was conducted to examine the effect of portable media devices (e.g. mobile phones, and tablet devices) on sleep outcomes
Data Sources
A search strategy was developed and searches of the published and grey literature were conducted across 12 databases from January 1st 2011 to June 15th, 2015. No language restriction was applied.
Study Selection
We included randomized controlled trials; cohort; and cross sectional study designs. Of 467 studies identified, 20 cross-sectional studies were assessed for quality
Data Extraction and Synthesis
Data extraction and quality assessment was independently carried out by two reviewers and disagreements resolved by a third. Data was pooled in a random-effects meta-analysis, and an individual participant meta-analysis was carried out where possible.
Main Outcomes and Measures
The primary outcomes were: inadequate sleep quantity; poor sleep quality; and excessive daytime sleepiness, carried out following an a priori protocol.
Results
Twenty studies were included and quality assessed, involving 125,198 children, 50.1% were male. There was a strong and consistent association between bedtime media device use and: inadequate sleep quantity (OR =2.17; 95%CI 1.42-3.32); poor sleep quality (OR=1.46; 95%CI 1.14-1.88); and excessive daytime sleepiness (OR=2.72; 95%CI 1.32-5.61). Additionally, children who had access to (but did not use) media devices at night were more likely to have inadequate: sleep quantity (OR=1.79; 95%CI 1.39-2.31); sleep quality (OR=1.53; 95%CI 1.11-2.10); and daytime sleepiness (OR=2.27; 95%CI 1.54-3.35).
Conclusions and relevance
This was the first meta-analysis of the effect of access and use of media device on sleep outcomes. Bedtime access and use of media devices was significantly associated with inadequate sleep quantity; poor sleep quality; and excessive daytime sleepiness. An integrated approach between teachers, healthcare providers and parents is needed to minimize device access at bedtime, and future research is needed to evaluate the impact on sleep hygiene and outcomes.
Keywords: Media devices, Mobile devices, inadequate sleep, meta-analysis, sleepiness
Introduction
Sleep is crucial to the development of physically and psychologically healthy children. Sleep disturbance in childhood is known to lead to adverse physical and mental health consequences. Short and long term detrimental health outcomes include: poor diet; sedative behavior; obesity; reduced immunity; stunted growth; mental health issues (such as depression and suicidal tendencies); and substance abuse (1-3).
Despite its importance to health, insufficient sleep and resultant daytime sleepiness is prevalent amongst the pediatric population, and increases throughout adolescence (4, 5). In the USA, 75% of 17-18 year olds report insufficient sleep, which is consistent with other developed countries (6). The American Academy of Pediatrics highlight factors such as electronic media device use, early school start times and increasing caffeine consumption, contribute substantially to this trend of insufficient and deteriorating sleep in the pediatric population (4, 5).
Studies over the last decade have demonstrated that conventional electronic devices such as televisions, gaming consoles and computers negatively impact sleep (7, 8). Newer portable mobile and media devices including smart phones and tablet devices with broader capabilities, such as internet and social networking, provide a different type of exposure, as they allow real-time interaction and therefore continuous stimulation for children unlike older stationary devices (8). Herein, these newer portable mobile and media devices will be defined as ‘media devices’.
It has been found that media devices are almost ubiquitous amongst children: 72% of all children and 89% of adolescents have at least one device in their sleeping environment, and most are used near bedtime (3, 6). Such devices are hypothesized to adversely impact sleep through a variety of pathways (7, 8). First, they may negatively affect sleep through directly displacing, delaying or interrupting sleep time. Second, the content can be psychologically stimulating, and finally the light-emitted from devices impact circadian timing, sleep physiology, and alertness (9). However, the association between media devices and poor sleep outcomes has been relatively under-explored, as the speed at which these devices have been developed has outpaced research capabilities (8, 9). A previous literature review reported a suspected association between screen-time and poor sleep outcomes, and raised debate to assess the quality of evidence and quantify the magnitude of the potential association (7, 8). We present the first systematic review to quantify the impact of media device use on sleep outcomes in a meta-analysis.
Methods
Study selection
This review was conducted following PRISMA guidelines (10) and carried out following an a priori protocol (available on request). All experimental and observational study designs, in any language, published between January 1st, 2011 and June 15th, 2015 were included. The time frame was selected to reflect the interactive nature of media device currently used. Access to and use of media device were included as pragmatic exposures. The inclusion criteria included studies of children and adolescents of school age between 6 to 19 years of age. The exclusion criteria were studies of stationary exposures such as televisions or desktop/personal computers, or those investigating electromagnetic radiation.
Data sources and search strategy
A search strategy consisting of 24 MeSH terms was developed in Medline Ovid and adapted for other databases (available on request). Searches of the published literature were conducted across eleven databases (British Education Index; NAHL; Cochrane Library; ERIC; International Biography of Social Sciences; Medline via Ovid [EMBASE, Medline, Psych INFO]; Pubmed; Science Direct; Scopus; Web of Science) on June 15th 2015. The grey literature was searched using the Open Grey online database. Bibliographies of included studies and conference abstracts were hand searched and authors of included studies were contacted to identify any ongoing or unpublished studies.
Device exposure categories and sleep outcomes
Cohorts of children with access to media devices less than three times a week were combined with children who had no media device access, and are defined as having ‘no access to a media device’. Children with bedtime access to a media device at least three times a week were categorized as ‘having access to a media device’. Children who used media device around bedtime were categorized as those who ‘used a media device around bedtime’.
Outcomes were the proportion of children who experienced: inadequate sleep quantity (less than 10 and 9 hours of daily sleep for children and adolescents respectively (5); inadequate sleep quality (defined as frequent difficulty in sleep initiation and/or sleep maintenance and/or non-refreshing sleep (11)); and daytime sleepiness (defined as poor daytime functioning as a result of both sleep quantity and quality (12)).
Study screening and quality assessment
Titles and abstracts identified from searches were screened for relevance and duplicates were excluded. The full texts of all relevant articles were retrieved, and their eligibility for inclusion was assessed. Two reviewers (MP and DB) independently assessed the methodological quality of all full text articles and discrepancies were resolved by a third reviewer (BC). The quality assessment tool consisted of 13 domains that appraised the overall evidence of the study (13). Each domain was determined as having a low risk of bias (RoB), unclear RoB or high RoB. If a study was found to have all domains with a low RoB the study was assessed as good quality. If a study was found with at least one domain with a high RoB it was assessed as low quality. Alternatively if a study was assessed with a combination of low and unclear RoB domains it was determined to have an unclear quality. Methodologically flawed studies were excluded, and the reason(s) for exclusion stated. A grading of recommendations assessment, development and evaluation (GRADE) was carried out on all findings (14).
Data extraction
Two reviewers independently extracted data (MP and PR) and a third reviewer resolved discrepancies (BC). Study authors were contacted if incomplete data had been reported and to provide aggregate or individual participant data (IPD).
Measures of effect of a media device on sleep
Included studies measured the association between exposure to a media device and impact on sleep using either: linear regression slopes (β); correlation co-efficient (r); or odds ratio (OR). To ensure consistency in interpretation only studies that reported dichotomous data, or logistic regression analyzes were pooled in a meta-analysis.
Data synthesis
If study design, population, intervention, and outcome were deemed to be sufficiently clinically homogenous, study data were pooled in a random effects meta-analysis using a Mantel-Haenszel method (15, 16). Where dichotomous data was not available, but study analysis were reported, the analysis were pooled with the dichotomous data using a generalized inverse variance approach (17). Where individual participant data (IPD) were available and determined to have external validity, a logistic regression model was fitted, accounting for the study as the random effect, and adjusted for participant age (18).
Assessment of subgroups and statistical heterogeneity
Statistical heterogeneity was assessed using the I2 statistic. Heterogeneity over 85% was explored using subgroup analyses (17). All meta-analyses were presented as an OR along with their associated 95% confidence intervals (95% CI), P-values and I2 summary data. Pre-specified subgroups to explore heterogeneity were: quality assessment (high quality, versus unclear and low quality studies); age of children (6 to 11, versus 12 to 15 and 16 to 18 age of children); and type of media device (cell phone; versus tablet).
Results
Identified studies and quality assessment
A total of 467 records were identified, 69 full texts were reviewed, leading to 49 excluded (Figure 1). Of the 20 studies that were assessed for methodological quality, 17 were included and three studies were excluded due to poor methodological conduct or reporting (19-21), see Supplementary Table 1 for further details. Two studies were of good quality (11, 22), six studies were of low quality (3, 23-27) and nine had unclear quality (28-36), see Supplementary Table 1.
Figure 1.
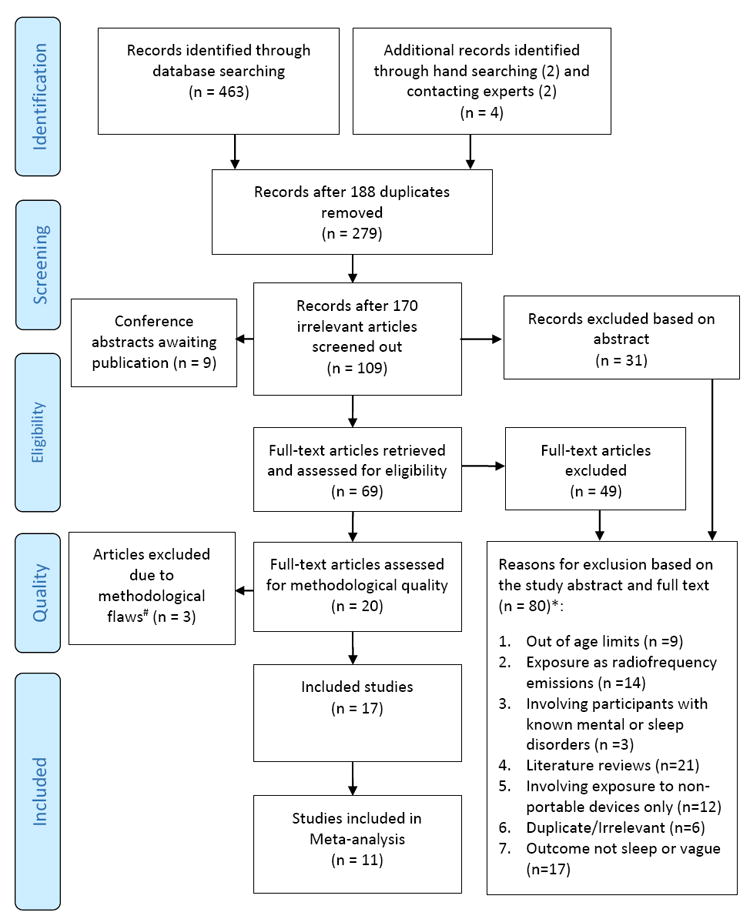
*Some studies satisfied more than one criteria
#For further details see Supplementary Table 1
Characteristics of included studies
Included studies were conducted in: Europe (n=7) (11, 25, 26, 28, 31, 33, 36); North America (n=4) (3, 23, 24, 29); Asia (n=3) (22, 34, 35); and Australasia (n=3) (27, 30, 32), for a comparison of the included study characteristics see Supplementary Table 2. Six studies assessed the association between media device and sleep during weekday periods only (11, 22, 24, 25, 28, 31, 34). Five studies assessed children’s sleep separately on weekdays and weekends (3, 23, 26, 30, 32) and six studies aggregated weekly data (27, 29, 33-36)
Media device exposure categorizes
Media device were categorized into two exposure groups: studies that reported the use of media device around bedtime (3, 11, 22, 25, 26, 28-31, 33, 35, 36); and the presence of a device in the sleep environment (3, 23-25, 29, 30, 33). One study presented data on the use of media device throughout the entire day, which is not reported here (34). Individual study results are presented in Supplementary Table 3, grouped by device exposure.
The effect of using a media device near bedtime, compared to not having access to a device
We found 12 studies that investigated the use of media device near bedtime and the individual study results are summarized in Supplementary Table 3. Eight studies reported that media device use was significantly associated with increase in inadequate sleep quantity (P<0.05). Seven studies reported an association between media device and an increase in inadequate sleep quality (P<0.05) and one study reported that media device use was associated with improved sleep quality (33). All four studies that presented data on excess daytime sleepiness exhibited statistical significance (P<0.05).
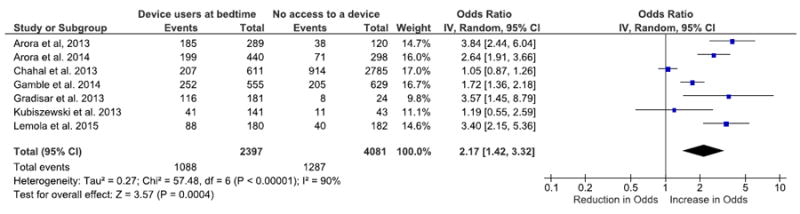
Inadequate sleep quantity
Seven studies were pooled in a meta-analysis (3, 11, 25, 28-30, 33), the OR of inadequate sleep quantity was 2.17 (95% CI 1.42-3.33; P<0.001; I2= 90%; Figure 2). There was an increased odds of inadequate sleep quantity by over double in those children that used a media device near bedtime. The severe heterogeneity was due to Chahal et al (2013) recruiting only 10 and 11 year olds: after this study was excluded the OR was 2.52 (95% CI 1.79-3.55; P<0.001; I2= 72%). Two studies (3, 25) were included in an individual participant data meta-analysis (IPD) and the age adjusted odds ratio (aOR) was 3.06 (95% CI 2.01-4.70; P<0.001).
Figure 2.
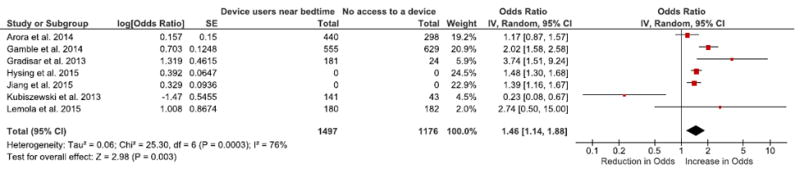
Poor sleep quality
Five studies reported dichotomous data (3, 11, 25, 30, 33), and two studies reported the OR from a logistic regression (25, 33). The pooled OR of poor sleep quality in those who used a media device was 1.46 (95% CI 1.14-1.88; P=0.003; I2= 76%; Figure 3). There was an increased odds of poor sleep quality of 46% in those children that used a media device near bedtime. The IPD meta-analysis aOR was 1.92 (95% CI 1.27-2.90; P=0.002) from two studies (3, 25).
Figure 3.
Excess daytime sleepiness
Two studies reported dichotomous data on the use of device near bedtime and excessive daytime sleepiness (3, 30). The pooled OR was 2.72 (95% CI 1.32-5.61; P=0.007; I2= 50%, Supplementary Figure 1). There was an increased odds of excessive daytime sleepiness by over double, in those children who used a media device near bedtime.
The effect of the presence of a media device in the sleeping environment near bedtime, compared to not having access to a device
Most studies reported statistical evidence of an association between the presence of a media device in the sleep environment near bedtime and: inadequate quantity (six of seven studies); poor sleep quality (four of six studies) and excess daytime sleepiness (three of four studies), see Supplementary Table 3.
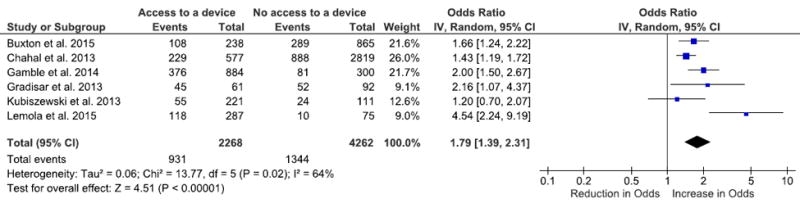
Inadequate sleep quantity
There was data from six studies (3, 23, 25, 29, 30, 33) investigating the presence of a media device in the sleep environment near bedtime and inadequate sleep quantity, the OR was 1.79 (95% CI 1.39-2.31; P<0.001; I2= 64%, Figure 4). There was an increased odds of 79% of inadequate sleep quantity, in those children that had access to a media device near bedtime. The IPD meta-analysis aOR was 1.88 (95% CI 1.46-2.42; P<0.001) from two studies (3, 25).
Figure 4.
Poor sleep quality
Dichotomous data was available from four studies (3, 23, 25, 30), and the OR for was extracted from two studies (24, 33). The pooled OR for poor sleep quality was 1.53 (95% CI 1.11-2.10; P=0.009; I2= 74%, Supplementary Figure 2). There was an increased odds of 53% of poor sleep quality, in those children that had access to a media device in the sleep environment near bedtime.
Excess daytime sleepiness
Dichotomous data was available from three studies (3, 23, 30) and an OR was extracted from a further study (33). The pooled OR of excessive daytime sleepiness was 2.27 (95% CI 1.54-3.35; P<0.001; I2= 24%; Supplementary Figure 3). There was an increased odds of over double of excessive daytime sleepiness, in those children that had access to a media device in the sleep environment near bedtime.
Subgroup analyses
There was no subgroup effects found due to: the quality of the included studies; age of the children (although the majority were aged between 10 and 18); or type of media device.
GRADE assessment
The GRADE assessment of included studies was low, due to their non-randomized nature. The assessment of the findings were upgraded due to the large effect sizes found, but downgraded due to the substantial heterogeneity. Therefore the level of evidence for all findings is low, meaning that the findings may change on publication of further evidence.
DISCUSSION
Summary of findings
This is the first systematic review to quantify the effect of media device access and use on children’s sleep. We found that bedtime device use was associated with an increase in the odds of: inadequate sleep quantity; poor sleep quality; and excessive daytime sleepiness. Media device presence in the bedroom (even without use) was also associated with increased odds of detrimental sleep outcomes.
This is the first systematic review to include a robust quality assessment that quantified the association between media device access and use and poor sleep outcomes (8). This review provides supporting evidence for an interaction between media device and psychophysiological arousal as a key mechanism of effect (31). Our findings support recommendations that interventions should be developed and evaluated to reduce media device access and use at bedtime. Specifically, we support age specific guidance for media device access and use (31); and parent-led initiatives to reduce device access and use in collaboration with health providers, and teachers (37).
Our findings support current clinical opinion that media device access and use results in poorer sleep outcomes. The limitations of research in this area include: measurement error of self-reported data; difficulty in ascertaining causality; isolating the effects of specific exposures; technology outpacing research; and weaknesses inherent to observational study designs. Substantial heterogeneity was found in many of the meta-analyses, and is likely a reflection of the included non-randomized studies. Therefore, a degree of caution is needed when interpreting these findings.
Implications for policy and practice
The deleterious effect of screen-based media on children and adolescents’ sleep is a major public health concern. Given the evolving technological landscape and the replacement of textbooks with media devices in schools, access to and use of screen-based media devices is likely to rise. It is imperative that clinicians, parents, teachers, and children are educated about the damaging impact of device use on sleep. Policy led population level health promotion to not stigmatize individual children, but guide communities to promote the importance of sleep hygiene is needed. Additionally, we encourage screening of children during routine clinical visits (by health visitors, school nurses, or family physicians) to identify those with inadequate sleep, in order to explore device use as a potential cause, and target sleep hygiene promotion.
Implications for research
Multidisciplinary interventions to improve sleep hygiene have been investigated (38, 39), however pragmatic studies are needed to understand the mechanism of action and causal pathway between device usage and sleep, using objective data collection methods. Interventions could be delivered by family physicians as a part of routine care for those presenting with health concerns, and teachers who introduce devices into education (39). Device technologists should investigate software and parent-led interventions such as automatic time switches to restrict access to media device near bedtime. Interventions and policies must be developed, evaluated and implemented at the population level to raise awareness of the potential health hazard to improve sleep hygiene through an integrated approach involving teachers, healthcare providers and parents.
CONCLUSIONS
Media device access and use at bedtime is significantly associated with detrimental sleep outcomes, and lead to poor health outcomes. We recommend that interventions to minimize device access and use are needed to be developed and evaluated. Interventions should include a multidisciplinary approach from teachers and healthcare workers to empower parents to minimize the deleterious impact on child health.
Supplementary Material
Key Messages.
This is the first systematic review and meta-analysis of the effect of media device access and use on children’s sleep.
Access and use of media devices at bedtime increased inadequate sleep quantity, inadequate sleep quality and excess daytime sleepiness.
Parents need an integrated approach from policy makers, healthcare providers and teachers, to minimize bedtime media device access and use
Acknowledgments
This research is funded in part by a grant (R01HD073352) from the Eunice Kennedy Shriver National Institute for Child Health and Human Development to LH.
Footnotes
Contributions of authors
BC – Drafted the protocol, analyzed and interpreted the data, drafted the manuscript, is guarantor of this review
DB – Extracted data, agreed the manuscript
LH – Drafted the manuscript, agreed the manuscript
MP – Drafted the protocol, searched the literature, extracted the data, analyzed and interpreted the data, agreed the manuscript
PR – Drafted the manuscript, extracted data, agreed the manuscript
Conflicts of interest
No funding was received for this study for authors BC, DB, MP and PR.
References
- 1.Calamaro CJ, Mason Tb, Ratcliffe SJ. Adolescents living the 24/7 lifestyle: effects of caffeine and technology on sleep duration and daytime functioning. Pediatrics 2009 20090601 DCOM- 20090617. 2009 Jun;123(6):e1005–10. doi: 10.1542/peds.2008-3641. (1098-4275 (Electronic)). eng. [DOI] [PubMed] [Google Scholar]
- 2.Gangwisch JE, Babiss La, Malaspina D, Turner JB, Zammit GK, Posner K. Earlier parental set bedtimes as a protective factor against depression and suicidal ideation. Sleep 2010 20100203 DCOM- 20100308. 2010 Jan;33(1):97–106. doi: 10.1093/sleep/33.1.97. (0161-8105 (Print)). eng. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Gradisar M, Wolfson AR, Harvey AG, Hale L, Rosenberg R, Czeisler CA. The sleep and technology use of Americans: findings from the National Sleep Foundation’s 2011 Sleep in America poll. Journal of clinical sleep medicine : JCSM : official publication of the American Academy of Sleep Medicine. 2013;9(12):1291–9. doi: 10.5664/jcsm.3272. Epub 2013/12/18. eng. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Gruber R, Carrey N, Weiss SK, Frappier JY, Rourke L, Brouillette RT, et al. Position statement on pediatric sleep for psychiatrists. J Can Acad Child Adolesc Psychiatry. 2014;23(3):174–95. [PMC free article] [PubMed] [Google Scholar]
- 5.Owens J Committee aASWG. Insufficient Sleep in Adolescents and Young Adults: An Update on Causes and Consequences. Pediatrics. 2014;134(3):e921–31. doi: 10.1542/peds.2014-1696. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Sleep in america poll, 2014: Summary of findings 2014. 2015 Jul 17; Available from: http://sleepfoundation.org/sites/default/files/2014-NSF-Sleep-in-America-poll-summary-of-findings---FINAL-Updated-3-26-14-.pdf.
- 7.Cain N, Gradisar M. Electronic media use and sleep in school-aged children and adolescents: A review. Sleep Medicine. 2010:735–42. doi: 10.1016/j.sleep.2010.02.006. [DOI] [PubMed] [Google Scholar]
- 8.Hale L, Guan S. Screen time and sleep among school-aged children and adolescents: a systematic literature review. Sleep Med Rev. 2015;21:50–8. doi: 10.1016/j.smrv.2014.07.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Chang AM, Aeschbach D, Duffy J, C C. Evening use of light-emitting eReaders negatively affects sleep, circadian timing, and next-morning alertness. Proceedings of the National Academy of Sciences. 2015;112:1232–7. doi: 10.1073/pnas.1418490112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. BMJ : British Medical Journal. 2009 Jul 21;339:b2535. doi: 10.1136/bmj.b2535. 06/05/accepted; [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Arora T, Broglia E, Thomas GN, Taheri S. Associations between specific technologies and adolescent sleep quantity, sleep quality, and parasomnias. Sleep Medicine Vol 2014. 2014;15(2):240–7. doi: 10.1016/j.sleep.2013.08.799. [DOI] [PubMed] [Google Scholar]
- 12.Young T. Epidemiology of Daytime Sleepiness: Definitions, Symptomatology, and Prevalence. J Clin Psychiatry. 2004;65(16):12–6. [PubMed] [Google Scholar]
- 13.Study" CpF. [02/01/2016];Methodological Quality Criteria. 2014 Available from: http://www.core-info.cardiff.ac.uk/wp-content/uploads/2012/03/Critical-appraisal-form-2014.pdf.
- 14.Schunemann H, Brozek J, Guyatt G, Oxman A. GRADE handbook for grading quality of evidence and strength of recommendation. [9th March, 2016];2013 Last updated 2016 http://gdt.guidelinedevelopment.org/central_prod/_design/client/handbook/handbook.html.
- 15.Deeks JJ, Higgins JP, Altman D. Analysing Data and Undertaking Meta-Analyses, in Cochrane Handbook for Systematic Reviews of Interventions. In: Green JPHaS., editor. Cochrane Book Series. Chichester, UK: John Wiley & Sons, Ltd; 2008. [Google Scholar]
- 16.Reeves BC, Deeks JJ, Higgins JP, Wells G. Including Non-Randomized Studies, in Cochrane Handbook for Systematic Reviews of Interventions. In: Green JPHaS., editor. Cochrane Book Series. Chichester, UK: John Wiley & Sons, Ltd; 2008. [Google Scholar]
- 17.Higgins JPT, Green S. Cochrane Handbook for Systematic Reviews of Interventions: The Cochrane Collaboration. 2011;2011 [Google Scholar]
- 18.Riley RD, Lambert PC, Abo-Zaid G. Meta-analysis of individual participant data: rationale, conduct, and reporting. BMJ. 2010;340:c221. doi: 10.1136/bmj.c221. [DOI] [PubMed] [Google Scholar]
- 19.Adachi-Mejia AM, Edwards PM, Gilbert-Diamond D, Greenough GP, Olson A. TXT me I’m only sleeping: adolescents with mobile phones in their bedroom. Fam Community Health. 2014;37(4):252–7. doi: 10.1097/FCH.0000000000000044. [DOI] [PubMed] [Google Scholar]
- 20.Nathan N, Zeitzer J. A survey study of the association between mobile phone use and daytime sleepiness in California high school students. BMC Public Health. 2013;13(840) doi: 10.1186/1471-2458-13-840. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Pea R, Nass C, Meheula L, Rance M, Kumar A, Bamford H, et al. Media use, face-to-face communication, media multitasking, and social well-being among 8- to 12-year-old girls. Dev Psychol. 2012;48(2):327–36. doi: 10.1037/a0027030. [DOI] [PubMed] [Google Scholar]
- 22.Jiang X, Hardy LL, Baur LA, Ding D, Wang L, Shi H. Sleep duration, schedule and quality among urban Chinese children and adolescents: associations with routine after-school activities. PloS one. 2015;10(1):e0115326. doi: 10.1371/journal.pone.0115326. Epub 2015/01/23. eng. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Buxton OM, Chang A-M, Spilsbury JC, Bos T, Emsellem H, Knutson KL. Sleep in the modern family: protective family routines for child and adolescent sleep. Sleep Health. 2015;1(1):15–27. doi: 10.1016/j.sleh.2014.12.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Falbe J, Davison KK, Franckle RL, Ganter C, Gortmaker SL, Smith L, et al. Sleep duration, restfulness, and screens in the sleep environment. Pediatrics. 2015 Feb;135(2):e367–75. doi: 10.1542/peds.2014-2306. Epub 2015/01/07. eng. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Lemola S, Perkinson-Gloor N, Brand S, Dewald-Kaufmann JF, Grob A. Adolescents’ electronic media use at night, sleep disturbance, and depressive symptoms in the smartphone age. Journal of Youth and Adolescence Vol 2015. 2015;44(2):405–18. doi: 10.1007/s10964-014-0176-x. [DOI] [PubMed] [Google Scholar]
- 26.Pieters D, De Valck E, Vandekerckhove M, Pirrera S, Wuyts J, Exadaktylos V, et al. Effects of pre-sleep media use on sleep/wake patterns and daytime functioning among adolescents: The moderating role of parental control. Behavioral Sleep Medicine Vol 2014. 2014;12(6):427–43. doi: 10.1080/15402002.2012.694381. [DOI] [PubMed] [Google Scholar]
- 27.Redmayne M, Smith E, Abramson M. The relationship between adolescents’ well-being and their wireless phone use: a cross-sectional study. Environ Health. 2013;12(90) doi: 10.1186/1476-069X-12-90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Arora T, H S, Lam H, Yao L, Thomas N, T S. Exploring the complex pathways among specific types of technology, self-reported sleep duration and body mass index in UK adolescents. International Journal of Obesity. 2013;37(9):1254–60. doi: 10.1038/ijo.2012.209. [DOI] [PubMed] [Google Scholar]
- 29.Chahal H, Fung C, Kuhle S, Veugelers PJ. Availability and night-time use of electronic entertainment and communication devices are associated with short sleep duration and obesity among Canadian children. Pediatric obesity. 2013 Feb;8(1):42–51. doi: 10.1111/j.2047-6310.2012.00085.x. Epub 2012/09/11. eng. [DOI] [PubMed] [Google Scholar]
- 30.Gamble AL, D’Rozario AL, Bartlett DJ, Williams S, Bin YS, Grunstein RR, et al. Adolescent sleep patterns and night-time technology use: results of the Australian Broadcasting Corporation’s Big Sleep Survey. PloS one. 2014;9(11):e111700. doi: 10.1371/journal.pone.0111700. Epub 2014/11/13. eng. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Hysing M, Pallesen S, Stormark KM, Jakobsen R, Lundervold AJ, Sivertsen B. Sleep and use of electronic devices in adolescence: Results from a large population-based study. BMJ Open. 2015;5(1) doi: 10.1136/bmjopen-2014-006748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.King DL, Delfabbro PH, Zwaans T, D K. Clinical features and axis I comorbidity of Australian adolescent pathological Internet and video game users. Aust N Z J Psychiatry. 2013;47(11) doi: 10.1177/0004867413491159. [DOI] [PubMed] [Google Scholar]
- 33.Kubiszewski V, Fontaine R, Rusch E, Hazouard E. Association between electronic media use and sleep habits: an eight-day follow-up study. International Journal of Adolescence and Youth 2013. 2014 Jul 03;19(3):395–407. [Google Scholar]
- 34.Mak YW, Sau Ting Wu C, Wing Shun Hui D, Lam SP, Tse HY, Yu WY, et al. Association between screen viewing duration and sleep duration, Sleep quality, And excessive daytime sleepiness among adolescents in Hong Kong. International Journal of Environmental Research and Public Health. 2014 Oct;11(11):11201–19. doi: 10.3390/ijerph111111201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Munezawa T, Kaneita Y, Osaki Y, Kanda H, Minowa M, Suzuki K, et al. The association between use of mobile phones after lights out and sleep disturbances among Japanese adolescents: A nationwide cross-sectional survey. Sleep: Journal of Sleep and Sleep Disorders Research Vol 2011 1. 2011;34(8):1013–20. doi: 10.5665/SLEEP.1152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Peiro-Velert C, Valencia-Peris A, Gonzalez LM, Garcia-Masso X, Serra-Ano P, Devis-Devis J. Screen media usage, sleep time and academic performance in adolescents: clustering a self-organizing maps analysis. PloS one. 2014;9(6):e99478. doi: 10.1371/journal.pone.0099478. Epub 2014/06/19. eng. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Royal College of Peadiatrics and Child Health. Mums launch parenting products to help manage children’s screen time. 2016 [updated 11th Feburary, 2016]. Available from: http://www.rcpch.ac.uk/news/mums-launch-parenting-products-help-manage-childrens-screen-time.
- 38.Quach J, Hiscock H, Ukoumunne O, M W. A Brief Sleep Intervention Improves Outcomes in The School Entry Year: A Randomized Controlled Trial Oct. Pediatrics. 2011;128(4):692–701. doi: 10.1542/peds.2011-0409. [DOI] [PubMed] [Google Scholar]
- 39.Hiscock H, Sciberras E, Mensah F, Gerner B, Efron D, Khano S, et al. Impact of a behavioural sleep intervention on symptoms and sleep in children with attention deficit hyperactivity disorder, and parental mental health: randomised controlled trial. BMJ. 2015;350(65) doi: 10.1136/bmj.h68. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


