Abstract
Objective
Although numerous studies among adults have shown a U-shaped association between sleep duration and health outcomes, fewer studies have investigated the theory that children also have an optimal sleep duration range, with both lower and upper limits. We evaluated whether children's sleep duration at ages 5 and 9 has a U-shaped association with both behavioral problems and physical health at age 9.
Method
We analyzed data from 1,965 participants in a longitudinal birth cohort, the Fragile Families and Child Wellbeing Study. This sample of children was 52% male and approximately 22% non-Hispanic white, 52% non-Hispanic black, 23% Hispanic, and 3% some other race/ethnicity. The child's primary caregiver reported the predictor of interest: sleep duration at age 5 and age 9. Both children and primary caregivers reported on outcomes of the child's behavior problems (internalizing and externalizing) and overall physical health.
Results
We found that the association between children's sleep duration and wellbeing was typically nonlinear and U-shaped. Adjusting for their sleep duration at age 5, children who sleep either too much or too little at age 9 had higher levels of behavior problems and scored lower on a global measure of physical health. These non-linear patterns were similar whether children or primary caregivers reported child outcomes, with the exception that there was a linear and increasing association of longer sleep duration and caregiver-rated child health.
Conclusions
This study highlights that both short and long sleep duration may be risk factors for adverse behavioral and health outcomes in school-aged children.
Keywords: Sleep Duration, Child Health, Child Behavioral Problems, Sleep, Health Disparities
Introduction
Sleep is part of a complex internally regulated homeostatic system (Borbély & Achermann, 1999; Saper, Cano, & Scammell, 2005). Theoretically, therefore, there is an optimal duration of sleep to maintain the right balance between sleep and wakefulness. In such a model, any sleep duration that is outside of this optimal range would be either too short or too long for optimal health and wellbeing. Indeed, prior research has found a U-shaped association between habitual sleep duration and health in numerous studies of adults. For example, regularly sleeping either too little or too much has been associated with a higher risk of obesity, cardiovascular disease, and all-cause mortality in adults (Buxton & Marcelli, 2010; Grandner, Hale, Moore, & Patel, 2010; Taheri et al., 2004). The mechanisms that have been suggested to explain the association between short sleep duration and poor health have included metabolic, immunological, and endocrine pathways (Grandner et al., 2010). However, the mechanisms though which overly long sleep duration has been associated with poor health are less well understood (Grandner & Drummond, 2007; Hossin 2016). One possibility is that long sleep duration directly produces poor outcomes; alternatively, the association between long sleep and poor health may be due to reverse causality or underlying conditions producing both longer sleep duration and poor health.
If the association between sleep duration and wellbeing comes about through biological mechanisms that do not change over the life course, a U-shaped association of sleep and wellbeing should be found among both adults and children. To our knowledge, however, only a few studies have evaluated whether the association between sleep duration and children's outcomes takes this nonlinear form. One study has modeled a nonlinear effect of sleep duration at ages 3-7.9 on children's BMI and overweight status four to seven years later by measuring sleep duration with indicators of whether the child sleeps less than 8 hours, 8-8.9 hours, 9-9.9 hours (reference), 10-10.9 hours, or 11 hours or more each night (Snell et al., 2007). This study has found that children who sleep for 11 hours or more each night have an elevated risk of higher BMI and being overweight as compared to children who sleep 9-9.9 hours per night. Another study has allowed for nonlinearities in an exploratory graphical examination of the association of children's sleep duration with physical and mental health measures, but has concluded there are no nonlinearities (Price, Quach, Wake, Bittman, & Hiscock, 2015).
Given the theoretical expectation of a nonlinear association of sleep duration with wellbeing, and the lack of studies evaluating such a pattern in children, in this paper we asked whether sleep duration is associated with behavioral and physical health outcomes in a U-shaped pattern for a large sample of 9-year-old children. We measured sleep duration both contemporaneously to the outcomes (when children are age 9) and at the prior study wave (when children are age 5). We hypothesized that both current and prior measures of sleep duration may have independent associations with behavioral and physical health outcomes. The association between age 9 sleep duration and the outcomes may reflect short-term associations, whereas sleep duration from an earlier age may indicate the lasting effects of problematic sleep duration during an earlier developmental period.
Prior Research
School-age children's sleep duration and behavioral problems
Prior studies evaluating how children's sleep duration is associated with behavioral problems have shown mixed results. One study has indicated that the objectively-measured sleep duration of a small sample of elementary school children was associated with conduct problems but not hyperactivity or emotional problems (Holley, Hill, & Stevenson, 2011). Another study has shown that sleeping for less than 9 hours per night was associated with higher emotional lability for a group of Australian 7-year-olds (Nixon et al., 2008). In addition, in a large sample of American children the odds of inadequate sleep have been shown to be higher among 6-11 year olds with depressive symptoms than those without depressive symptoms (Smaldone, Honig, & Byrne, 2007). Finally, cross-sectional analyses of Australian children have shown that children with low psychosocial quality of life at ages 6-7 slept more than their peers without this clinical level of problematic behavior; there were no statistically significant associations of sleep duration with behavior at ages 4-5 or 8-9 (Price et al., 2015). While the final study (Price et al., 2015) has included preliminary graphical exploration of raw data which could capture nonlinearities, these analyses were not adjusted for any confounders, and neither this study nor the others has tested whether a model which allows for a U-shaped relationship between children's sleep duration and behavior problems is supported by the data.
School-age children's sleep duration and health outcomes
A substantial literature has documented a significant negative – and in some cases U-shaped – association between children's sleep duration and weight gain, overweight, and obesity (Bagley, Kelly, & El-Sheikh, 2015; Cappuccio et al., 2008; Chen, Beydoun, & Wang, 2008; Magee & Hale, 2012; Nixon et al., 2008; Snell, Adam, & Duncan, 2007; Price et al., 2015). However, less research has considered the potential association between sleep duration and global measures of child health. One exception, which uses the same dataset as the present study, has found that the sleep duration of 5-year-old children is not associated with having good, fair, or poor health relative to excellent or very good health after adjusting for the presence of language-based bedtime routines at age 3 and other family factors (Hale, Berger, LeBourgeois, & Brooks-Gunn, 2011). Similarly, Price et al. (2015) have found no association of sleep duration with low levels of physical health among 4-9 year old Australian children. As with the literature on children's sleep durations and behavioral problems, none of these prior studies on the association between children's sleep duration and global measures of health have analyzed whether long sleep duration is associated with poorer health or if there is a U-shaped association of sleep with health.
Biological pathways between sleep and wellbeing
Sleep duration has been theorized to relate to behavior and health via a number of biological pathways. For behavioral outcomes, sleep deprivation in adults has been shown to limit prefrontal cortex and amygdala connectivity and to make negative emotional stimuli more salient (Yoo, Gujar, Hu, Jolesz, & Walker, 2007). For physical health, the mechanisms through which insufficient sleep is problematic for overweight and obesity have been especially well documented. Sleep deprivation has been shown to decrease levels of leptin, an appetite-suppressing hormone, and increase levels of ghrelin, an appetite-enhancing hormone (Taheri, Lin, Austin, Young, & Mignot, 2004); these hormonal changes have been associated with increased appetite and consuming more calories after a sleep-deprived night (Brondel, Romer, Nougues, Touyarou, & Davenne, 2010). Beyond weight status, short sleep duration (less than 7.7 hours) has been associated with higher waking and peak cortisol levels than those for average sleep duration (7.7-9.3 hours) in a sample of 8-year-old Finnish children (Räikkönen et al., 2010). In addition, emerging evidence has suggested that sleep and immune system function may have a circular relationship, whereby sickness impairs sleep and sleep problems contribute to illness (Bryant, Trinder, & Curtis, 2004). Relatively little of this research has been conducted on pediatric populations, however.
Contributions
We are unaware of any longitudinal population-based studies that have investigated whether children's behavioral problems and physical health have a non-linear association with sleep duration. Therefore, we tested a model of sleep homeostasis in which both short and long sleep durations are associated with poorer outcomes than sleep durations between these extremes. By leveraging a longitudinal design, we were able to evaluate to what extent children's sleep duration was associated with their wellbeing in middle childhood; we tested this association both when sleep duration was measured contemporaneously to the outcome and at a prior study wave. This study also improved upon prior work on sleep and child wellbeing by using a large and diverse sample of children. Finally, this study considered the behavior and physical health of children as assessed via both self-report and caregiver-report.
Method
We analyzed data from the Fragile Families and Child Wellbeing Study (FFCWS), a population-based longitudinal study of children born in large American cities (population > 200,000) between 1998 and 2000, with an oversample of non-marital births.1 Using a multi-stage probability sample procedure, participants were recruited in hospitals at the time of the child's birth. Interviews with mothers and fathers (or other primary caregivers)2 occurred at the child's birth and again when the child was ages 1, 3, 5, and 9. Children were interviewed at age 9. Study topics included parental relationships, child outcomes, and the impact of contextual and policy conditions on families and children. FFCWS included child and primary caregiver reports of behavior problems and physical health, as well as the primary caregiver's report of the child's sleep duration.
Of the 4,898 participants enrolled in FFCWS at the child's birth, 2,503 participated in the three surveys beyond the baseline (in-home interview at age 5, primary caregiver interview at age 9, and child interview at age 9) necessary to provide the outcome and key predictor variables in these analyses. The analytic sample included 79% of these cases, or 1,965 participants in the FFCWS (see Table 1 for sample description). The 21% of missing cases who did participate in the relevant survey waves came from the following sources. First, 33 cases had unusable data on sleep duration: 21 cases were missing sleep duration at age 5, 1 other case was missing sleep duration at age 9, and an additional 12 cases had extreme sleep durations and were dropped from the analyses (see Measures: Sleep duration). Second, 360 cases had missing values for one or more of the outcomes of interest. Third, an additional 144 cases were missing demographic or control variable information. Though we have presented the results of analyses employing listwise deletion to address this missing data, we have replicated the analyses using multiple imputation for missing control variables and find the results to be substantively unchanged in that sample (N=2,109).
Table 1. Analytic sample description (N = 1,965).
| Mean or proportion | Range | |
|---|---|---|
| Child's age in monthsˆ | 111.63 | 105-129 |
| Child low birth weight (< 2,500 grams) | 0.10 | 0-1 |
| Child male | 0.52 | 0-1 |
| Child's puberty scoreˆ | 1.46 | 1.0-3.2 |
| Mother non-Hispanic white, native born | 0.22 | 0-1 |
| Mother non-Hispanic black, native born | 0.52 | 0-1 |
| Mother Hispanic, native born | 0.23 | 0-1 |
| Mother other race/ethnicity, native born | 0.03 | 0-1 |
| Father same race/ethnicity as mother | 0.86 | 0-1 |
| Mother foreign born | 0.11 | 0-1 |
| Mother's ageˆˆ | 30.05 | 19-50 |
| Mother has less than high school education | 0.31 | 0-1 |
| Mother has high school diploma or GED | 0.31 | 0-1 |
| Mother attended some college | 0.27 | 0-1 |
| Mother is a college graduate | 0.11 | 0-1 |
| Household incomeˆˆ | $38,045.22 | $0-$688,444 |
| Biological parents marriedˆˆ | 0.32 | 0-1 |
| Biological parents cohabitingˆˆ | 0.12 | 0-1 |
| Number of children in homeˆˆ | 2.50 | 0-10 |
| Hours of sleep – age 9ˆ | 9.44 | 6-14 |
| Hours of sleep – age 5ˆˆ | 8.95 | 6-15 |
| Child's self-rated internalizing behavior (SDQ)ˆ | 9.25 | 0-24 |
| PCG's rating of child's internalizing behavior (CBCL)ˆ | 3.73 | 0-42 |
| Child's self-rated externalizing behavior (SDQ)ˆ | 5.53 | 0-18 |
| PCG's rating of child's externalizing behavior (CBCL)ˆ | 6.28 | 0-70 |
| Child's self-rated physical healthˆ | 4.10 | 1-5 |
| PCG's rating of child's physical healthˆ | 4.40 | 1-5 |
Note:
measured at age 9;
measured at age 5;
other characteristics measured at baseline.
Compared to the baseline Fragile Families cohort, children included in analyses were in somewhat better circumstances. Mothers of children in the analytic sample were more likely to be native-born non-Hispanic blacks (52%) and less likely to be native-born Hispanics (23%), native-borns of some other race/ethnicity (3%), or foreign-born (11%) than were mothers in the baseline cohort (48%, 27%, 4%, and 11% respectively). In addition, mothers of children in the analytic sample had on average more education than do mothers in the baseline cohort; in the analytic sample 31% had less than a high school education (35% in the baseline cohort), 31% had a high school diploma or GED (30% in the baseline cohort), 27% had some college education 24% in the baseline cohort), and 11% had a college degree (11% in the baseline cohort). However, there was no difference between our analytic sample and the baseline cohort in the proportion of children who were born with a low birth weight, male, or have mothers and fathers of the same race/ethnicity. It is unclear whether the pattern of missing data will lead to under- or over-estimates of the associations between sleep duration and wellbeing.
Measures
Child behavior problems and health
Both children and primary caregivers assed child behavior problems and health at age 9.
Children evaluated their behavior problems using the internalizing and externalizing subscales of the Self Description Questionnaire (SDQ) (Marsh, 1990). Children rated to what extent a set of statements described their feelings and behaviors at school and home on a scale of 0 (“not at all true”), 1 (“a little bit true”), 2 (“mostly true”), and 3 (“very true”). Internalizing behavior included actions directed toward the self, such as depressive and anxious tendencies. There were 8 items in the internalizing subscale, with a potential score ranging from 0 to 24.3 Externalizing behavior included other-directed actions, such as conduct disorder and acting out. There were 6 items in the externalizing subscale, with a potential score ranging from 0 to 18.4 Primary caregivers appraised children's behavior problems using the Child Behavior Checklist (CBCL). Primary caregivers rated how much a series of behaviors were representative of the child's typical behavior on a scale of 1 (“not true”), 2 (“somewhat or sometimes true”), and 3 (“very true or often true”). Internalizing behavior summed the withdrawn/depressed5 and anxious/depressed6 subscales for a total of 21 items with potential scores ranging from 21 to 63. Externalizing behavior summed the aggressive7 and rule-breaking8 subscales for a total of 35 items with potential scores ranging from 35 to 105.
Both children and primary caregivers reported on the child's general physical health at the 9-year survey wave. Health ratings included 1 (“Poor”), 2 (“Fair”), 3 (“Good”), 4 (“Very good”), and 5 (“Excellent”).
Sleep duration
Primary caregivers reported how many hours of sleep their children typically got per night during the week in both the age 5 and age 9 survey waves. In the analytic sample, hours of sleep ranged from 0 to 17 at age 5 and 4 to 14 at age 9. To adjust for implausible sleep durations, we dropped the 12 cases with implausibly short (less than 6 hours) or long (more than 15 hours) nightly sleep durations using listwise deletion; this method has been previously used by Price et al. (2015). As an alternative, we also employed another method for dealing with the extreme cases in which we bottom- and top-coded extreme sleep durations such that less than 6 hours per night was recoded to 6 hours per night (bottom-coded) and greater than 15 hours per night was recoded to 15 hours per night (top-coded). Results were similar with either approach, but for a conservative estimate we showed results from the models without the extreme cases.
Child characteristics
Child characteristics included the child's age in months at the time of the 9-year interview, whether the child had a low birth weight (< 2,500 grams, assessed at birth), and whether the child was male or female (recorded at birth). The child's pubertal development was reported at age 9 by the child's primary caregiver and was a scale ranging from 1 to 4 that indicates the degree to which the child had experienced a height growth spurt, hair growth, skin changes, a deepening voice (boys), facial hair growth (boys), breast growth (girls) or menarche (girls). We included these variables because they have been shown in prior studies to be associated with both child sleep and child wellbeing.
Parent characteristics
Mothers reported their race/ethnicity, nativity, and educational attainment at the time of the child's birth. Whether the father was of the same race/ethnicity as the child's mother was also measured at the child's birth. Both parents' race/ethnicity was self-reported and included categories for white (non-Hispanic), black (non-Hispanic), Hispanic, and some other race/ethnicity. Nativity indicated whether or not the mother was born in the United States. Maternal educational attainment was measured with categories for whether the mother had obtained less than high school education, a high school diploma or GED, some college education, or a college degree. Mothers reported their age, household income, relationship (married, cohabiting, or no relationship) with the biological father, and household composition at the 5-year interview. Household income, in dollars, was logged in analyses. Household composition indicated how many children, in addition to the focal child, live in the home at the 5-year interview. Again, these variables were included to avoid confounding influences of other variables known to be associated with both child sleep and child wellbeing.
Analytic Strategy
We estimated the extent to which children's sleep duration sat ages 5 and 9 was associated with their self-rated and primary-caregiver-rated behavior problems and physical health at age 9. In the following analyses, α was the model intercept, X1 was sleep duration, X2 was a vector of child and family characteristics (control variables with the vector of coefficients β2), and X3 was a non-linear, quadratic term for sleep duration (i.e. hours of sleep, squared).
Behavior problems were evaluated using ordinary least squares regression (OLS). Physical health was modeled using ordered logit models. There were three outcomes – internalizing behavior, externalizing behavior, and physical health – reported separately by mothers and children for a total of six models (see Table 2). Each analysis had the same set of control variables, whose measurement was described in the prior section: the child's age in months at age 9, whether the child was born with a low birth weight (< 2,500 grams), child sex, the child's pubertal progression score at age 9, maternal race/ethnicity and nativity, whether the father was the of the same race/ethnicity as the mother, the mother's age at the 5-year interview, maternal educational attainment at the child's birth, household income at the 5-year interview, biological parents' relationship at the 5-year interview, and the number of children in the home at the 5-year interview.
Table 2. Selected coefficients and standard errors (in parentheses) from OLS models of child behavior and exponentiated coefficients and standard errors (in parentheses) from ordered logit models of child health (N=1,965).
| OLS | Ordered logit | |||||
|---|---|---|---|---|---|---|
|
| ||||||
| Internalizing behavior | Externalizing behavior | Physical health | ||||
|
| ||||||
| Child report | PCG report | Child report | PCG report | Child report | PCG report | |
|
| ||||||
| (1) | (2) | (3) | (4) | (5) | (6) | |
|
|
||||||
| Intercept | 26.536** (8.310) | 14.074* (6.804) | 29.192*** (6.391) | 35.319** (10.897) | ||
| Hours of sleep age 9 | -2.611* (1.220) | -2.084* (0.999) | -2.368* (0.938) | -5.495*** (1.600) | 1.934* (0.332) | 1.108* (0.043) |
| (Hours of sleep age 9)2 | 0.139* (0.067) | 0.101+ (0.055) | 0.129* (0.051) | 0.275** (0.088) | 0.968+ (0.018) | |
| Hours of sleep age 5 | 0.515 (1.144) | -0.267 (0.937) | -0.978 (0.880) | 0.161 (1.501) | 1.427 (0.316) | 1.022 (0.039) |
| (Hours of sleep age 5)2 | -0.020 (0.060) | 0.014 (0.049) | 0.051 (0.046) | -0.018 (0.079) | 0.982 (0.017) | |
| Control Variables | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ |
|
| ||||||
| R2 | 0.076 | 0.029 | 0.096 | 0.061 | ||
| AIC | 4,888.678 | 4,038.714 | ||||
Note:
p<0.10;
p<0.05;
p<0.01;
p<0.001.
These analyses also account for the child's age in months at age 9, whether the child was born with a low birth weight (< 2,500 grams), child sex, the child's pubertal progression score at age 9, maternal race/ethnicity and nativity, whether the father is the of the same race/ethnicity as the mother, the mother's age at the 5-year interview, maternal educational attainment at the child's birth, maternal household income at the 5-year interview, biological parents' relationship at the 5-year interview, and the number of children in the home at the 5-year interview.
Results
Children's sleep durations in the primary school years were associated with their wellbeing, with both shorter and longer sleep durations associated with worse outcomes than sleep durations between these extremes. Using the child's sleep duration at ages 5 and 9 as predictors, Table 2 displays coefficients for OLS models which tested the association of these variables with behavior problems at age 9 and exponentiated coefficients (odds ratios) for ordered logit models which tested the association of these variables with physical health at age 9. These models allowed for both a linear effect of sleep duration and a nonlinear (quadratic or U-shaped) effect of sleep duration on the outcomes via the term hours of sleep, squared.
For internalizing behavior, there was a statistically significant association of behavior problems with the child's sleep duration and the nonlinear term for sleep duration even when models were adjusted for a number of control variables. This pattern was true whether the child reported his or her own internalizing behavior (Model 1) or the primary caregiver reported the child's internalizing behavior problems (Model 2). The pattern of findings was the same for the child's externalizing behavior problems, whether reported by the child (Model 3) or the child's primary caregiver (Model 4), as well as the child's own report of his or her physical health (Model 5). For the primary caregiver's report of the child's physical health (Model 6), the nonlinear terms for sleep duration were not significantly associated with the outcome. Therefore, these terms were not included in the model presented here.
None of the models of child behavior or physical health indicated that sleep duration when the child was 5 years old had a statistically significant association with behavior problems or health at age 9. Thus, concurrent sleep patterns were more strongly associated with the child's own and his or her primary caregiver's report of behavior problems and physical health than were the child's sleep duration in the previous survey wave.
Nonlinear Association between Sleep Duration and Child Behavior
Figures 1 and 2 present predicted levels of behavior problems and physical health for children with different sleep durations, based on the models of child behavior presented in Table 2. These figures hold other covariates at their mean or modal levels.9 For reference, the recommended range of 9-11 hours of sleep for school age children, as recommended by the National Sleep Foundation (NSF) (Hirshkowitz et al., 2015), is denoted by the shaded area.
Figure 1. Hours of sleep and predicted self-reported behavior, age 9.
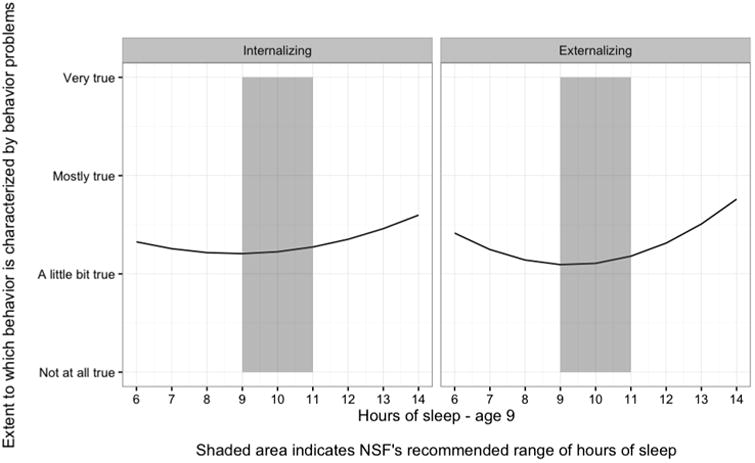
Figure 2. Hours of sleep and predicted PCG-reported behavior, age 9.
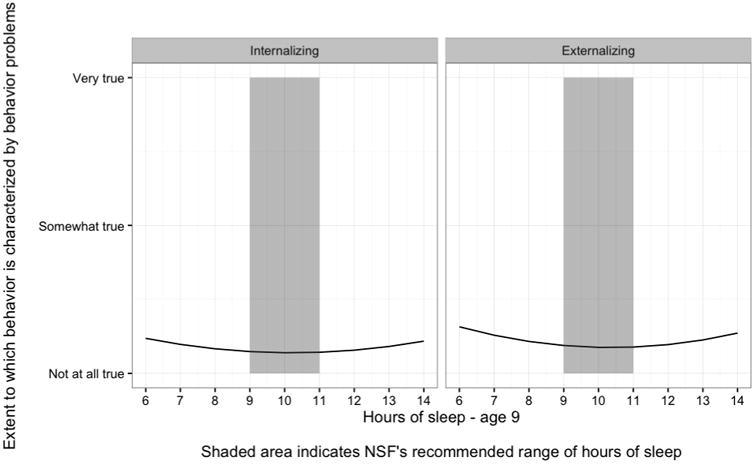
Figures 1 and 2 display the nonlinear association of sleep duration at age 9 with the child's behavior problems, as reported by the child and the primary caregiver, respectively. For each reporter, the left column is internalizing behavior problems and the right column is externalizing behavior problems. The horizontal axis of these plots corresponds to the child's sleep duration. The shaded area indicates the NSF's range of recommended sleep duration for school age children (9-11 hours) (Hirshkowitz et al., 2015). The vertical axis of these plots corresponds to the level of child behavior problems; higher scores indicate worse child behavior. Rather than showing the numeric value for levels of behavior problems, these axes denote to what extent the child's behavior was characterized by the given type of behavior problems, ranging from “not at all true” to “somewhat true” and “very true” in primary caregiver reports and from “not at all true” to “a little bit true”, “mostly true”, and “very true” in child reports.
Overall, there was a U-shaped association between child's sleep duration at age 9 and behavior problems. Children who slept a very small or very large number of hours per night reported the highest levels of behavior problems. This broad effect held for both child and primary caregiver-reported internalizing and externalizing behavior problems, though there were small differences by reporter. Children reported on average higher levels of behavior problems than do their primary caregivers, and the most dramatic curvilinear associations were found for children's reported behavior problems and their sleep duration. The lowest levels of behavior problems mirrored the NSF's recommended sleep duration for school age children (9-11 hours) (Hirshkowitz et al., 2015) in primary caregiver reports. However, the lowest level of behavior problems as reported by the child corresponded to a slightly shorter sleep duration, in the range of 8-10 hours of sleep per night.
Nonlinear Association between Sleep Duration and Physical Health
Figure 3 displays the association between sleep duration and the probability that the child was rated to have a given level of physical health, based on the models for child health in Table 2. The plot on the left is the child's rating, the plot on the right is the primary caregiver's rating, the horizontal axis corresponds to the child's nightly sleep duration at age 9, and the shaded area denotes recommended sleep duration for school age children. The vertical axis is the probability of reporting that the child was rated to have a given level of physical health. As in the figures for child behavior, these figures hold other covariates at their mean or modal levels, and the shaded area indicates the recommended range of 9-11 hours of sleep for school age children.
Figure 3. Hours of sleep and predicted child health, age 9.
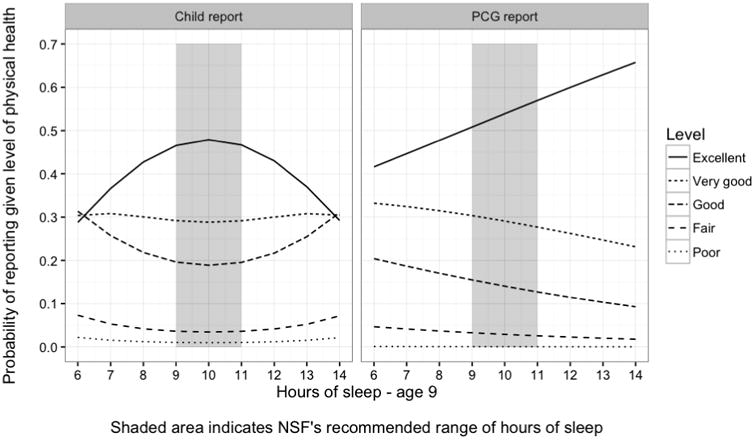
The association of sleep duration with physical health differed by who reported the child's physical health. When children reported their physical health, there was a U-shaped association with sleep duration, as shown in the solid line in Figure 3, which corresponds to a rating of excellent physical health. The highest probability of the child reporting excellent physical health was found within the NSF's recommended sleep duration for school age children (9-11 hours) (Hirshkowitz et al., 2015), and children who sleep low or high numbers of hours each night had lower probabilities of reporting excellent physical health. In contrast, the primary caregiver's assessment of the child's physical health did not have the same nonlinear association; the best model of fit was a linear model which did not include the term for a nonlinear effect of the child's hours of sleep. Figure 3 shows that children who slept the least had the lowest probability of having a primary caregiver who reported excellent physical health. As the number of hours the child slept at age 9 increased, the probability that the primary caregiver rated the child as being in excellent physical health increased.
Robustness checks
The results shown in the focal analyses were robust to an alternative specification that included a control for the child's having a bedtime in the prior (age 5) and current (age 9) survey waves. These bedtime indicators did not have a statistically significant association with the outcomes of interest, and the association of sleep duration and child outcomes did not differ meaningfully from models without these controls. Thus, for parsimony, the final results did not account for whether or not the child has a bedtime at ages 5 or 9.
Discussion
There was a nonlinear association between children's sleep duration and their concurrent behavior problems and physical health even after adjusting for their sleep duration in an earlier study wave. Children who slept the least or the most had the highest levels of behavior problems and the lowest self-rated physical health. For behavior problems, this pattern was consistent regardless of whether the child or the parent reported the child's behavior problems – though the gradient was more dramatic when children report their behavior problems. In contrast, who evaluates child health made a difference for its association with sleep duration. When children rated their physical health, there was a U-shaped association of sleep duration with health. When the primary caregiver rated the child's health, the association was linear and increasing.
These findings suggest that future research on the association between children's sleep duration and wellbeing should follow two recommendations. First, future studies should consider the full range of child sleep durations. Measuring only whether or not the child sleeps more or less than a recommended number of hours does not capture the full range of child experiences, and grouping children who sleep an adequate amount with those who sleep too much may mask important differences in these groups. Analyses utilizing the full range of child sleep durations should also consider using a nonlinear specification when modeling the association between sleep duration and child wellbeing. Second, subsequent research should be particularly attentive to who reports child outcomes. This study finds that the association between a child's sleep duration and his or her behavior problems is largely consistent regardless of whether the outcome of interest is evaluated by the child or the primary caregiver. Thus, both reporters are reliable when considering how sleep duration is related to child behavior. In contrast, the association of sleep and health differs when the child and the primary caregiver report the child's physical health.
These analyses are among the first to use longitudinal, population-based data to evaluate the extent to which there is a nonlinear association between children's sleep duration and multiple reports of their behavior problems and physical health. However, this study does have several significant limitations. First, the study design did not allow us to rule out a reverse causal explanation or a bidirectional relationship between sleep duration and wellbeing. Not all outcomes are measured at multiple data waves, so we did not control for prior behavior problems or health status in the models. Second, the models explain a low but non-trivial portion of the variance in the outcomes of interest. While we have attempted to produce models which adjust for a variety of factors known to be associated with both children's nightly sleep duration and wellbeing, child health and behavior are complex phenomena produced by many interactive social, psychological, and biological inputs. Other, unmeasured factors that may also matter for this association include additional health and behavior conditions, other stressful life experiences, and genetic factors. Third, the primary predictor – the report of children's sleep duration – comes from a report by their primary caregiver, rather than a more objective estimate (e.g., actigraphy, polysomnography). Any error in primary caregiver reports of child sleep duration, compared to the child's actual nightly sleep duration, may be influenced by the primary caregiver's impressions of the child's behavior problems and physical health. In general, the presence of this type of measurement error tends to attenuate the associations between observed variables and thus underestimate true effect sizes. Additionally, our sleep measure included only one question about children's typical sleep duration, which does not indicate the variability of children's sleep across nights. While these analyses were not able to address these biases directly, future work should integrate more objective estimates of sleep duration into population-based studies to improve accuracy and eliminate any underlying caregiver-specific factor that influences both the report of the child's sleep duration. Finally, while FFCWS is a population-based sample of children born in large American cities, study participants are overall more disadvantaged than American children as a whole; it is not clear if these results would generalize to children from rural areas, born in a different time period, or who were more advantaged.
Despite its limitations, this research has important clinical implications and suggests potential areas for practitioner intervention. First, this study reiterates prior consensus that short sleep duration is associated with poor outcomes. Short sleep is more prevalent than long sleep in children, and practitioners should intervene to help families ensure that children get sufficient sleep for optimal health and wellbeing. Second, this study is the first to highlight that long sleep duration, already shown to be associated with adverse health outcomes in adults, is also potentially a concern for school-aged children. As with adults, underlying factors that are in themselves problematic for behavior and health may be causing children to sleep for longer durations. Nevertheless, clinicians should take note of particularly long nightly sleep durations in children, which may be indicators of or precursors to an underlying condition. Finally, clinicians should be reassured by the finding that concurrent but not past sleep duration is associated with child outcomes, indicating that sleep and wellbeing have short-term but not long-term associations. This pattern suggests that the association of sleep duration with problematic behavior and health outcomes may be mitigated with contemporaneous interventions.
In conclusion, sleep duration is a risk factor for the wellbeing of children who sleep either too much or too little. Future research should investigate both the clinical implications and the broader social consequences of these findings.
Appendix A. Coefficients and standard deviations from OLS models of child behavior and exponentiated coefficients and standard errors (in parentheses) from ordered logit models of child health (N = 1,965).
| OLS | Ordered logit | |||||
|---|---|---|---|---|---|---|
|
| ||||||
| Internalizing behavior | Externalizing behavior | Physical health | ||||
|
| ||||||
| Child report | PCG report | Child report | PCG report | Child report | PCG report | |
|
| ||||||
| (1) | (2) | (3) | (4) | (5) | (6) | |
|
|
||||||
| Intercept | 26.536** (8.310) | 14.074* (6.804) | 29.192*** (6.391) | 35.319** (10.897) | ||
| Hours of sleepage9 | -2.611* (1.220) | -2.084* (0.999) | -2.368* (0.938) | -5.495*** (1.600) | 1.934* (0.332) | 1.108* (0.043) |
| (Hours of sleep age 9)2 | 0.139* (0.067) | 0.101+ (0.055) | 0.129* (0.051) | 0.275** (0.088) | 0.968+ (0.018) | |
| Hours of sleepage 5 | 0.515 (1.144) | -0.267 (0.937) | -0.978 (0.880) | 0.161 (1.501) | 1.427 (0.316) | 1.022 (0.039) |
| (Hours of sleep age 5)2 | -0.020 (0.060) | 0.014 (0.049) | 0.051 (0.046) | -0.018 (0.079) | 0.982 (0.017) | |
| Child's age in months | -0.030 (0.032) | 0.031 (0.026) | -0.044+ (0.025) | 0.041 (0.042) | 1.010 (0.010) | 1.007 (0.012) |
| Child low birth weight (ref: >2,500 grams) | 0.812* (0.406) | -0.151 (0.332) | 0.073 (0.312) | -0.752 (0.532) | 0.941 (0.142) | 0.908 (0.147) |
| Child male (ref: female) | 0.403 (0.253) | 0.250 (0.207) | 1.328*** (0.194) | 1.288*** (0.332) | 1.026 (0.088) | 0.852+ (0.094) |
| Child's puberty score | 0.215 (0.358) | 0.747* (0.293) | 0.341 (0.275) | 0.368 (0.469) | 0.680** (0.124) | 0.958 (0.132) |
| Mother non-Hispanic black, native born (ref: white, native born) | 1.134** (0.363) | -1.261*** (0.297) | 0.869** (0.279) | -1.410** (0.476) | 0.994 (0.123) | 0.783+ (0.135) |
| Mother Hispanic, native born (ref: white, native born) | 0.551 (0.410) | -0.314 (0.336) | -0.325 (0.315) | -1.583** (0.538) | 0.736* (0.140) | 0.740* (0.152) |
| Mother other race/ethnicity, native born (ref: white, native born) | -0.768 (0.820) | 0.891 (0.672) | 0.163 (0.631) | 0.802 (1.076) | 1.667+ (0.285) | 1.198 (0.317) |
| Father same race/ethnicity as mother (ref: father not same race/ethnicity) | 0.051 (0.370) | 0.202 (0.303) | -0.098 (0.285) | -0.094 (0.486) | 1.001 (0.126) | 1.118 (0.136) |
| Mother foreign born | -0.370 (0.448) | 0.091 (0.367) | -0.955** (0.345) | -0.846 (0.588) | 0.921 (0.154) | 0.724* (0.164) |
| Mother's age when child age 5 | -0.080*** (0.023) | -0.003 (0.019) | -0.021 (0.018) | -0.053+ (0.031) | 0.992 (0.008) | 0.990 (0.009) |
| Mother has high school diploma or GED (ref: less than high school education) | -0.531+ (0.316) | -0.245 (0.259) | 0.001 (0.243) | -0.230 (0.414) | 1.053 (0.110) | 0.765* (0.116) |
| Mother attended some college (ref: less than high school education) | -0.901* (0.355) | -0.376 (0.291) | -0.329 (0.273) | -0.564 (0.465) | 1.190 (0.124) | 0.984 (0.132) |
| Mother is a college graduate (ref: less than high school education) | -1.085* (0.534) | -0.018 (0.437) | -0.217 (0.411) | -0.173 (0.700) | 1.165 (0.183) | 0.933 (0.202) |
| Log of household income when child age 5 | -0.370** (0.113) | -0.251** (0.092) | -0.406*** (0.087) | -0.527*** (0.148) | 0.988 (0.040) | 1.078+ (0.041) |
| Biological parents married when child age 5 (ref: no relationship) | -0.241 (0.319) | -0.358 (0.261) | -0.237 (0.245) | -0.992* (0.418) | 0.915 (0.110) | 1.250+ (0.118) |
| Biological parents cohabiting when child age 5 (ref: no relationship) | -1.007** (0.390) | -0.086 (0.319) | -0.545+ (0.300) | -0.697 (0.511) | 0.990 (0.135) | 1.084 (0.142) |
| Number of children in home when child age 5 | 0.265** (0.095) | 0.030 (0.078) | 0.040 (0.073) | 0.378** (0.125) | 1.002 (0.033) | 0.998 (0.035) |
|
| ||||||
| R2 | 0.076 | 0.029 | 0.096 | 0.061 | ||
| AIC | 4,888.678 | 4,038.714 | ||||
Note:
p<0.10;
p<0.05;
p<0.01;
p<0.001
Acknowledgments
Research reported in this publication was supported by the Eunice Kennedy Shriver National Institute of Child Health and Human Development (NICHD) of the National Institutes of Health under award numbers R01HD073352, R01HD36916, R01HD39135, R01HD40421, and P2CHD047879; and a consortium of private foundations. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Footnotes
Detailed information on study procedures is available at http://www.fragilefamilies.princeton.edu/
Primary caregivers were mothers at both the age 5 and age 9 survey waves in 95% of cases in the analytic sample; mothers were assumed to be the primary caregiver where the child's mother and father lived together or for single mothers.
In the FFCWS age 9 sample, the SDQ internalizing subscale has a Cronbach's alpha of 0.78 and mean 1.15 (SD = 0.70).
In the FFCWS age 9 sample, the SDQ externalizing subscale has a Cronbach's alpha of 0.76 and mean 0.92 (SD = 0.72).
In the FFCWS age 9 sample, the CBCL withdrawn/depressed subscale has a Cronbach's alpha of 0.70.
In the FFCWS age 9 sample, the CBCL anxious/depressed subscale has a Cronbach's alpha of 0.78.
In the FFCWS age 9 sample, the CBCL aggressive subscale has a Cronbach's alpha of 0.89.
In the FFCWS age 9 sample, the CBCL rule-breaking subscale has a Cronbach's alpha of 0.77.
That is, these figures make predictions for a child who is 111.62 months old at the age 9 interview, not low birth weight, male, has a pubertal development score of 1.46 at age 9, and lives in a household with 2.5 other children at age 5; has a black mother and father who are not co-resident when the child is age 5; and whose mother is a native-born woman 30.05 years old at the age 5 interview with a high school diploma or GED whose household income was $38,0435.22 when the child was age 5.
Contributor Information
Sarah James, Department of Sociology, Office of Population Research, Princeton University.
Lauren Hale, Department of Family, Population, and Preventive Medicine, Program in Public Health, Stony Brook Medicine.
References
- Bagley EJ, Kelly RJ, El-Sheikh M. Longitudinal relations between children's sleep and body mass index: the moderating role of socioeconomic risk. Sleep Health. 2015;1(1):44–49. doi: 10.1016/j.sleh.2014.12.001. http://doi.org/10.1016/j.sleh.2014.12.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Borbély AA, Achermann P. Sleep homeostasis and models of sleep regulation. Journal of Biological Rhythms. 1999;14(6):557–568. doi: 10.1177/074873099129000894. [DOI] [PubMed] [Google Scholar]
- Brondel L, Romer MA, Nougues PM, Touyarou P, Davenne D. Acute partial sleep deprivation increases food intake in healthy men. American Journal of Clinical Nutrition. 2010;91(6):1550–1559. doi: 10.3945/ajcn.2009.28523. http://doi.org/10.3945/ajcn.2009.28523. [DOI] [PubMed] [Google Scholar]
- Bryant PA, Trinder J, Curtis N. Sick and tired: Does sleep have a vital role in the immune system? Nature Reviews Immunology. 2004;4(6):457–467. doi: 10.1038/nri1369. http://doi.org/10.1038/nri1369. [DOI] [PubMed] [Google Scholar]
- Buxton OM, Marcelli E. Short and long sleep are positively associated with obesity, diabetes, hypertension, and cardiovascular disease among adults in the United States. Social Science & Medicine. 2010;71(5):1027–1036. doi: 10.1016/j.socscimed.2010.05.041. http://doi.org/10.1016/j.socscimed.2010.05.041. [DOI] [PubMed] [Google Scholar]
- Cappuccio FP, Taggart FM, Kandala NB, Currie A, Peile E, Stranges S, Miller MA. Meta-Analysis of Short Sleep Duration and Obesity in Children and Adults. Sleep. 2008;31(5):619–626. doi: 10.1093/sleep/31.5.619. Retrieved from http://wrap.warwick.ac.uk/30144/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen X, Beydoun MA, Wang Y. Is sleep duration associated with childhood obesity? A systematic review and meta-analysis. Obesity. 2008;16(2):265–274. doi: 10.1038/oby.2007.63. http://doi.org/10.1038/oby.2007.63. [DOI] [PubMed] [Google Scholar]
- Grandner MA, Drummond SP. Who are the long sleepers? Towards an understanding of the mortality relationship. Sleep Medicine Reviews. 2007;11(5):341–360. doi: 10.1016/j.smrv.2007.03.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grandner MA, Hale L, Moore M, Patel NP. Mortality associated with short sleep duration: The evidence, the possible mechanisms, and the future. Sleep Medicine Reviews. 2010;14(3):191–203. doi: 10.1016/j.smrv.2009.07.006. http://doi.org/10.1016/j.smrv.2009.07.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hale L, Berger LM, LeBourgeois MK, Brooks-Gunn J. A Longitudinal Study of Preschoolers' Language-Based Bedtime Routines, Sleep Duration, and Well-Being. Journal of Family Psychology. 2011;25(3):423–33. doi: 10.1037/a0023564. http://doi.org/10.1037/a0023564. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hirshkowitz M, Whiton K, Albert SM, Alessi C, Bruni O, DonCarlos L, et al. Adams Hillard PJ. National Sleep Foundation's sleep time duration recommendations: methodology and results summary. Sleep Health. 2015;1(1):40–43. doi: 10.1016/j.sleh.2014.12.010. http://doi.org/10.1016/j.sleh.2014.12.010. [DOI] [PubMed] [Google Scholar]
- Hossin MZ. From habitual sleep hours to morbidity and mortality: existing evidence, potential mechanisms, and future agenda. Sleep Health. 2016;2(2) doi: 10.1016/j.sleh.2016.01.006. [DOI] [PubMed] [Google Scholar]
- Holley S, Hill CM, Stevenson J. An hour less sleep is a risk factor for childhood conduct problems. Child: Care, Health and Development. 2011;37(4):563–570. doi: 10.1111/j.1365-2214.2010.01203.x. http://doi.org/10.1111/j.1365-2214.2010.01203.x. [DOI] [PubMed] [Google Scholar]
- Magee L, Hale L. Longitudinal associations between sleep duration and subsequent weight gain: A systematic review. Sleep Medicine Reviews. 2012;16(3):231–41. doi: 10.1016/j.smrv.2011.05.005. http://doi.org/10.1016/j.smrv.2011.05.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marsh HW. Self-Description Questionnaire Manual. Campbelltown N. S. W. Australia; University of Western Sydney, Macarthur: 1990. [Google Scholar]
- Nixon GM, Thompson JMD, Han DY, Becroft DM, Clark PM, Robinson E, et al. Mitchell EA. Short Sleep Duration in Middle Childhood: Risk Factors and Consequences. Sleep. 2008;31(1):71–78. doi: 10.1093/sleep/31.1.71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Price AMH, Quach J, Wake M, Bittman M, Hiscock H. Cross-sectional sleep thresholds for optimal health and well-being in Australian 4-9-year-olds. Sleep Medicine. 2015 doi: 10.1016/j.sleep.2015.08.013. http://doi.org/10.1016/j.sleep.2015.08.013. [DOI] [PubMed]
- Räikkönen K, Matthews KA, Pesonen AK, Pyhälä R, Paavonen EJ, Feldt K, et al. Kajantie E. Poor Sleep and Altered Hypothalamic-Pituitary-Adrenocortical and Sympatho-Adrenal-Medullary System Activity in Children. Journal of Clinical Endocrinology and Metabolism. 2010;95(5):2254–2261. doi: 10.1210/jc.2009-0943. http://doi.org/10.1210/jc.2009-0943. [DOI] [PubMed] [Google Scholar]
- Saper CB, Cano G, Scammell TE. Homeostatic, circadian, and emotional regulation of sleep. Journal of Comparative Neurology. 2005;493(1):92–98. doi: 10.1002/cne.20770. [DOI] [PubMed] [Google Scholar]
- Smaldone A, Honig JC, Byrne MW. Sleepless in America: Inadequate Sleep and Relationships to Health and Well-being of Our Nation's Children. Pediatrics. 2007;119(Supplement 1):S29–S37. doi: 10.1542/peds.2006-2089F. http://doi.org/10.1542/peds.2006-2089F. [DOI] [PubMed] [Google Scholar]
- Snell EK, Adam EK, Duncan GJ. Sleep and the Body Mass Index and Overweight Status of Children and Adolescents. Child Development. 2007;78(1):309–323. doi: 10.1111/j.1467-8624.2007.00999.x. http://doi.org/10.1111/j.1467-8624.2007.00999.x. [DOI] [PubMed] [Google Scholar]
- Taheri S, Lin L, Austin D, Young T, Mignot E. Short Sleep Duration is Associated with Reduced Leptin, Elevated Ghrelin, and Increased Body Mass Index. PLoS Medicine. 2004;1(3):e62. doi: 10.1371/journal.pmed.0010062. http://doi.org/10.1371/journal.pmed.0010062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yoo SS, Gujar N, Hu P, Jolesz FA, Walker MP. The human emotional brain without sleep - a prefrontal amygdala disconnect. Current Biology. 2007;17(20):877–878. doi: 10.1016/j.cub.2007.08.007. http://doi.org/10.1016/j.cub.2007.08.007. [DOI] [PubMed] [Google Scholar]


