Abstract
Purpose
To quantify the influence of the length of the look-back period on misclassification of heart failure (HF) incidence in Medicare claims available for participants of a population-based cohort.
Methods
Atherosclerosis Risk in Communities (ARIC) participants with ≥3 years of continuous fee-for-service Medicare enrollment from 2000–2012 was assigned an index date 36 months after enrollment separating the time-in-observation into the look-back and the incidence periods. Incident HF events were identified using ICD-9-CM code algorithms as the first observed hospitalization claim or the second of two HF outpatient claims occurring within 12 months. Using 36 months as a referent, the look-back period was reduced by 6-months increments. For each look-back period, we calculated the incidence rate, percent of prevalent HF events misclassified as incident, and loss in sample size.
Results
We identified 9,568 ARIC participants at risk for HF. For hospitalized and outpatient HF, the number of events misclassified as incident increased and the total number of incident events decreased with increased length of the look-back period. The incident rate (per 1,000 person years) decreased with increased length of the look-back period from 6 to 36 months and had a greater impact on outpatient HF; for example, from 11.2 to 10.6 for ICD-9-CM 428.xx hospitalization in the primary position and 10.5 to 7.9 for outpatient HF.
Conclusion
Our estimates can be used to optimize trade-offs between the degree of misclassification and number of events in the estimation of incident HF from administrative claims data, as pertinent to different study questions.
Keywords: Heart failure, misclassification, hospitalizations, outpatient, administrative claims
Background
Administrative healthcare data, such as the Centers for Medicare and Medicaid Services (CMS) claims, are widely used in epidemiologic research. Claims data can be used to estimate incidence, prevalence, and associations of chronic and acute conditions1–5. A limitation of claims data in this regard is the paucity of patients’ disease history and laboratory findings, patient-reported outcomes data, age restrictions, such as those encountered with the CMS Medicare data, and changes in enrollment status due to mandatory annual re-enrollment. Thus, identifying initial occurrences, i.e., true incident events, from administrative claims data can pose challenges.
Establishing incidence of heart failure (HF) is particularly challenging as this complex condition can be diagnosed in the inpatient as well as the outpatient setting, using a range of diagnostic criteria. Repeated outpatient visits and hospital admissions are common for individuals with chronic diseases, and notably in patients living with chronic HF, while the identification of incident events requires a look-back period sufficient to identify the incident nature of an event and to exclude prevalent cases. Consequently, in analyses of administrative claims data a time has to be set as the start of enrollment, or the at risk period of incidence, to differentiate incident events from prevalent events whose onset preceded the look-back period.
No standards for the optimal length of a look-back period in identifying incident HF from administrative claims data have been established. A one-year or shorter look-back period has been commonly used in research to date6–10 although this conventional time frame may be insufficient to avoid misclassification of incident HF11. Furthermore, the varying lengths of look-back periods used by investigators may contribute to conflicting estimates of incidence. To accurately classify incident HF, lengthening the look-back period may be necessary, but the impact of the length of the look-back period on the accuracy of the estimation of HF incidence has not been thoroughly examined.
The objective of this study was to characterize the impact of varying lengths of the look-back period on the observed incidence and misclassification of HF diagnosed in the inpatient and outpatient setting using Medicare administrative claims data linked with the Atherosclerosis Risk in Communities (ARIC) study.
Methods
Study Participants
The cohort component of the ARIC study is a community-based prospective study of cardiovascular disease among individuals sampled from 4 U.S. communities: Forsyth County, North Carolina; Jackson, Mississippi; Washington County, Maryland; and the northwest suburbs of Minneapolis, Minnesota12. Recruitment occurred in 1987–89 and included 15,792 mostly Caucasian and African American participants aged 45–64 years at baseline. Institutional Review Boards at each participating institution approved the study and all participants provided written informed consent at each examination.
Data for ARIC cohort participants were linked with Medicare claims for the years 1991–2012 using a finder file that included participants’ social security numbers, gender, and date of birth. From the total number of study participants with available social security numbers (n=15,744), 238 died before 1991 and 607 died after 1991 but before reaching the Medicare eligibility age of 65 years, leaving 14,899 eligible ARIC study participants. A crosswalk file was used to identify ARIC cohort participants eligible for Medicare coverage. The crosswalk file between the ARIC study finder file and the Medicare Beneficiary Summary file yielded 14,702 ARIC cohort IDs for analyses (98.7% match).
Information concerning ARIC study participant enrollment in fee-for-service (FFS) Medicare was obtained from monthly indicators of enrollment in Part A, Part B, and Medicaid buy-in available from annual Medicare Beneficiary Summary files. Continuous enrollment periods were created to indicate uninterrupted FFS Medicare coverage, defined as enrollment in Medicare Part A and Part B as well as the lack of enrollment in a Medicare Advantage (HMO) plan. Study participants with continuous Medicare Advantage enrollment or less than 36 months of continuous Medicare FFS enrollment were excluded from the study. We included the last enrollment period extending ≥36 months for participants with gaps in coverage resulting from the discontinuation of enrollment FFS, enrollment in a Medicare Advantage plan, or from missing enrollment information. All inpatient and outpatient claims were linked.
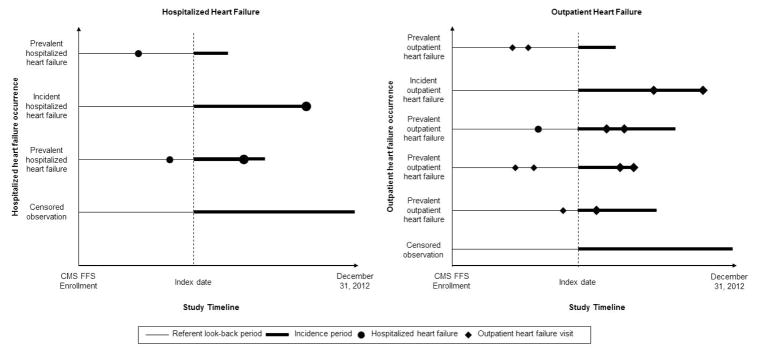
Observation Period
Due to limited number of HF events from 1991–1999, we included participants with Medicare claims for the years 2000–2012 and followed participants from the date of FFS enrollment to FFS disenrollment, death, or December 31, 2012, whichever came first. Each participant was assigned an index date exactly 36 months after enrollment. The index date separated the time-in-observation into two phases: the look-back and incidence periods (Figure 1). The referent look-back period was defined as the first 36 months of FFS enrollment prior to the index date and used to identify prevalent cases of heart failure. The incidence period was defined as the time in FFS enrollment after the index date.
Figure 1.
Study participant’s hospitalized and outpatient heart failure classification scheme, ARIC cohort members enrolled in Medicare Fee-for-Service, 2000–2012
Two outpatient heart failure visits occurring within 12 consecutive months are considered a diagnosis of heart failure in the outpatient setting. An outpatient heart failure diagnosis can be considered prevalent if preceded by either an outpatient heart failure diagnosis or a heart failure hospitalization in the look-back period.
HF Events
HF identified from an ICD-9-CM code in the primary position has high specificity but poor sensitivity; thus, ICD-9-CM code 428.xx in the primary position probably underestimates numbers of true HF hospitalizations13. Indeed, hospitalizations with a non-primary ICD-9-CM code 428.xx are three times more common than those with a primary code of 428.xx14,15 and codes other than 428.xx may also identify patients with HF13,16. Therefore, hospitalized HF was identified from annual Medicare Provider Annual Review (MedPAR) records using three International Classification of Disease, 9th Edition Clinical Modification (ICD-9-CM) code definitions for HF: ICD-9-CM code of 428.xx in the primary position; ICD-9-CM code of 428.xx in any position; and the Chronic Condition Data Warehouse (CCW) chronic condition algorithm for HF (ICD-9-CM codes: 398.91, 402.01, 402.11, 402.91, 404.01, 404.11, 404.91, 404.03, 404.13, 404.93, and 428.xx) in any position. An incident hospitalized HF was defined as the first observed hospitalization claim in the incidence period, following the index date (Figure 1).
Outpatient HF was identified from claims with Evaluation and Management service codes for new and established outpatient visits (99201–99205), consultations (99241–99245), and established preventive medicine visits (99395–99397) matched with date of service found in the Carrier (Part B) claims as well as claims for outpatient services provided through the Federally Qualified Healthcare Center (520–521). Similar to inpatient HF, outpatient HF events were identified using HF-specific ICD-9-CM codes 428.xx in any position in the medical record. A diagnosis of HF in the outpatient setting was defined as the presence of two outpatient HF claims within 12 consecutive months. The date of the first of those two HF outpatient claims was considered as the date of outpatient HF diagnosis (Figure 1)1,2. A 30-day interval between the two outpatient encounters was used to ensure that the two outpatient encounters were separate events. An incident outpatient HF was defined as the first observed outpatient HF diagnosis in the incidence period following the index date.
Analysis
ARIC study participants were included in analyses if they had at least one MedPAR hospitalization record or at least one outpatient claim. Misclassification of HF incidence was estimated separately for hospitalized and outpatient HF. The referent look-back period was defined as 36 months following enrollment.
For identification of incident and prevalent hospitalized and outpatient HF, each participant was classified as having one of four HF incidence and prevalence conditions, based on the 36 month referent look-back period: (1) a HF event in the look-back and incidence periods, (2) a HF event in in the look-back period only, (3) a HF event in the incidence period only, or (4) neither (Figure 1). Similar classifications have been used in previous studies11. Participants with a HF event in the incidence period only were considered as having “true incident HF events”. The incidence rate (IR, per 1,000 person-years) was calculated as the number of true HF events divided by the total person-time for all participants at risk. Participants were considered at risk for a heart failure event if they did not have a HF event in the defined look-back period. Participants’ person-time was measured from the index date to (1) an incident HF event, (2) death, (3) disenrollment, or (4) December 31, 2012, whichever came first. Participants with a HF event in both the look-back and incidence period and participants with a HF event in the look-back period only were excluded from the IR analyses.
The look-back period was progressively reduced in 6-month intervals, from the referent 36 months to a minimum 6 months before the index date. When the look-back period was reduced, membership in the “neither”, “look-back only”, “incidence only”, and “both” categories changed based on the dates of their HF events. The incident HF events observed among participants who were moved to the “incidence only” group in the process of reducing the look-back period were considered to be “false positives”. When assessing outpatient HF, a hospitalized HF or outpatient HF diagnosis in the look-back period reclassified a participant as “look-back only” or “both” from the “neither” or “incidence only” category, respectively. For each shortened look-back period, we recalculated the IR of HF events, calculated the percent of prevalent HF events misclassified as incident, percent of false positives, and the resulting loss in events. Participants with a HF event in both the look-back and incidence period or with a HF event in the look-back period only were excluded from all analyses. Misclassification of HF incidence was calculated as the proportion of the number of true incident HF events among the incident HF events in a given look-back period. False positives were calculated as 1-positive predicted value (the number of true incident HF events divided by the total number of reported incident HF events).
All analyses were conducted using SAS V9.3 (SAS Inc. Cary, North Carolina).
Results
Among the 14,702 ARIC cohort participants whose records were matched to Medicare claims, we identified 9,568 participants with a hospitalization or outpatient claim who were enrolled in FFS Medicare for at least 36 months from January 1, 2000 to December 31, 2012 and met aforementioned inclusion criteria. The average age of participants at the index date was 71 (SD=4.2) years (Table 1). The average length of the FFS Medicare enrollment for participants at risk was 106 months. Fifty-eight percent of participants were female and 27% were African American. There were 617 participants who had a HF hospitalization with an ICD-9-CM code 428.xx in primary position after the index date. We also observed 1,290 and 1,366 participants who had a HF hospitalization with ICD-9-CM code 428.xx in any position or an ICD-9-CM code corresponding to the HF CCW algorithm occurring after the index date respectively. Claims for HF diagnoses in the outpatient setting occurring after the index date were observed among 729 participants. Within the first 12 months following the index date and a non-event outpatient claim, 261 (2.7%) and 138 (1.4%) participants died, respectively.
Table 1.
Participant characteristics, ARIC cohort members enrolled in Medicare Fee-for-Service, 2000–2012
| Characteristic | CMS enrolled ARIC participants (N = 9568) |
|---|---|
| Mean (SD)
|
|
| Age at index date (years) | 71.1 (4.2) |
| Length in enrollment (months) | 105.5 (100.2)
|
| N (%)
|
|
| % Female | 5558 (58.1) |
| % African American | 2564 (26.8) |
| Study region | |
| Forsyth County, North Carolina | 1989 (20.8) |
| Jackson, Mississippi | 2315 (24.2) |
| Minneapolis, Minnesota | 2160 (22.6) |
| Washington County, Maryland | 3104 (32.4) |
| Hospitalized events | |
| ICD-9-CM code of 428.xx in the primary position | 617 (6.4) |
| ICD-9-CM code of 428.xx in any position | 1290 (13.5) |
| CCW ICD-9-CM code algorithm for heart failure | 1366 (14.3) |
| Outpatient events | |
| ICD-9-CM code of 428.xx | 766 (8.0) |
Abbreviations: Atherosclerosis Risk in Communities (ARIC), Centers for Medicare and Medicaid Services (CMS), standard deviation (SD)
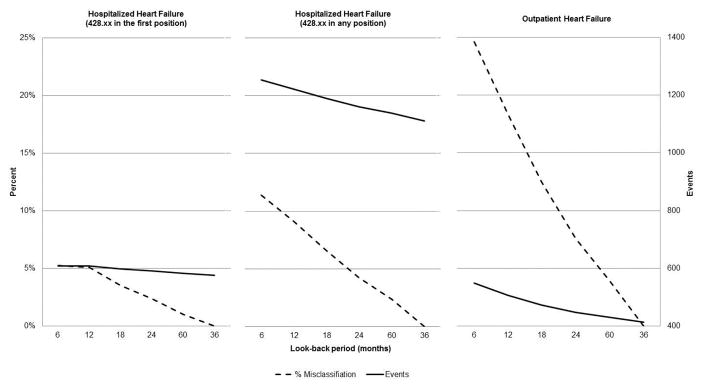
Hospitalized HF (428.xx in the primary position)
Using the referent look-back period of 36 months, we observed 577 HF events classified as incident hospitalized HF (IR = 10.6 per 1,000 person-years, Table 2). Under this referent condition, 414 participants were classified as having an incident event (Figure 2). As the length of the look-back period was progressively shortened the number of HF hospitalizations classified as prevalent decreased and the numbers of HF hospitalizations misclassified as incident increased with a subsequent increase of classified HF events (Figure 2). For example, when the look-back period was shortened to 24 months, 26 (4.2%) of the putatively incident events were excluded as prevalent HF cases. The misclassification of 14 prevalent hospitalized HF events as incident (2.4% false positives) resulted in an overestimation of the IR by 2.4% from 10.6 to 10.9 events per 1,000 person-years. Further shortening the look-back period to 12 months led to the exclusion of 9 (1.5%) participants as having prevalent HF, thus resulting in 31 (5.1%) false positive incident HF hospitalizations and an overestimation of the IR by 5.3% (IR = 11.2 per 1,000 person-years).
Table 2.
Incidence of hospitalized and outpatient heart failure by length of look-back period, ARIC cohort members enrolled in Medicare Fee-for-Service, 2000–2012 (N = 9568)
| Look-back period (monthsb) | Hospitalized heart failure | Outpatient heart failure | ||||
|---|---|---|---|---|---|---|
|
| ||||||
| 428.xx in the primary position | 428.xx in any position | Observed incident outpatient HF | Incidence ratec | |||
|
| ||||||
| Observed incident hospitalized HF | Incidence ratec | Observed incident hospitalized HF | Incidence ratec | |||
| 6 | 609 | 11.20 | 1255 | 24.15 | 549 | 10.46 |
| 12 | 608 | 11.18 | 1223 | 23.54 | 507 | 9.67 |
| 18 | 598 | 11.00 | 1190 | 22.91 | 473 | 9.03 |
| 24 | 591 | 10.87 | 1161 | 22.37 | 448 | 8.56 |
| 30 | 583 | 10.72 | 1139 | 21.95 | 431 | 8.24 |
| 36a | 577 | 10.61 | 1112 | 21.44 | 414 | 7.92 |
Referent
Months available prior to index date
Per 1,000 person years
Figure 2.
Proportion of false positives and number of events for hospitalized and outpatient heart failure, ARIC cohort members enrolled in Medicare Fee-for-Service, 2000–2012
The look-back period is used to exclude patients with prevalent heart failure prior to the index date. Proportion of false positives was calculated as the proportion of incident HF events in a given look-back period relative to the number of true incident HF events.
Hospitalized HF (428.xx in any position)
Using the referent look-back period of 36 months we observed 1,112 incident hospitalized HF events with the ICD-9-CM code of 428.xx in any position (IR = 21.4 per 1,000 person-years, Table 2), leading to the classification of 178 (13.8%) participants as having prevalent HF (Figure 2). As the length of the look-back period was shortened, the number of hospitalized HF events misclassified as incident increased (Figure 2), similar to what was observed using the more restrictive definition of HF based on the presence of ICD-9-CM code 428.xx in the primary position. Shortening the look-back period to 24 months resulted in the exclusion of 129 (10.0%) participants with prevalent hospitalized HF (7.8% false positives). Thus, incidence was overestimated by 4.5% from 21.4 to 22.4 events per 1,000 person-years, about double the overestimation observed when using a HF code in the primary position. When the look-back period was further shortened to 12 months, 67 (5.2%) participants were excluded as prevalent cases and the incidence was overestimated by 8.9% (IR = 23.5 events per 1,000 person-years). This resulted in 111 (9.1%) false positive incident hospitalized HF events.
Results were similar when assessing the CCW chronic condition algorithm for HF (Supplementary Table and Figure).
Outpatient HF
Using the referent look-back period of 36 months we observed 414 incident outpatient HF events (7.92 events per 1,000 person-years, Table 2). Similar to estimates obtained for hospitalized HF, the incidence of outpatient HF increased as the look-back period length was reduced (Figure 2) although the increase in the number of events was more substantial: under the referent condition, 352 (46%) participants were categorized as having prevalent HF (Figure 2). Shortening of the look-back period to 24 months resulted in the exclusion from analyses of 318 (42%) participants with prevalent outpatient HF. Incidence was overestimated by 7.5% from 7.92 to 8.56 events per 1,000 person-years and 34 prevalent outpatient HF events were misclassified as incident. When the look-back period was shortened to 12 months, 259 (33.8%) participants were excluded to account for prevalent outpatient HF, and the overestimation of incidence increased by 18.1% (9.67 events per 1,000 person-years). This resulted in 135 false positive incident outpatient HF events.
Discussion
Evaluations of the impact of the length of the look-back period employed in the estimation of incident events from administrative claims are uncommon, and none specific to HF have been reported to our knowledge. Consistent with a previous report7, our results suggest that lengthening a look-back period to exclude pre-existing HF from the risk set when using Medicare claims decreases the misclassification of prevalent HF events as incident. The use of short look-back periods thus tends to overestimate the incidence of HF by incorporating prevalent events; however, the impact is low for hospitalized HF.
By examining the effect of the length of look-back periods on misclassification of hospitalized HF as well as outpatient HF we contribute new information on misclassification of HF in administrative claims. The misclassification of outpatient HF was approximately double that of the misclassification observed for hospitalized HF using a more specific definition, and five times compared to observed misclassification of hospitalized HF defined by an ICD-9-CM code of 428.xx in any position. The greater impact of the look-back period on misclassification of outpatient, as compared to hospitalized HF, likely stems from the definition of an outpatient diagnosis requiring two HF claims within 12 consecutive months. This differential misclassification suggests that there is value in separately addressing the incidence of outpatient and hospitalized HF.
We compared different conventions commonly used for identification of HF events in claims data, i.e. the use of a HF code (428.xx) in the primary position versus more inclusive definitions such as 428.xx any position and the CCW chronic condition algorithm for HF. Our data suggest that if misclassification is of concern, the use of a more specific code algorithm (e.g. 428.xx in the primary position) may be desirable to reduce the number of false positives.
While misclassification is reduced as the length of the look-back period increases, the number of events is also reduced, particularly in the estimation of the incidence of outpatient HF. Misclassification bias is thus reduced when the length of the look-back period is increased although the resulting loss in the number of events likely affects precision. In general, a look-back period that is not congruent with the natural history of the event under consideration, or the risk characteristic of the population under study, may select observations that are not representative of the population of cases from which the events arise. As our results suggest, a choice of the desirable length of a look-back period would be informed by a trade-off between the costs assigned to misclassification bias vs. the loss of events, which would be influenced by the study question being addressed. If a short look-back period is necessary and the loss in study size is substantial the source of administrative claims used may not be a suitable resource.
Detailed medical record information is not available in administrative claims, nor is anamnestic information that would allow for the assessment of prior events or a time course for the event recorded as a claim. The inability to validate events as true incident events requires that the investigator establish a look-back period to identify and exclude prevalent events. In the absence of established standards for a look-back period we examined the impact of a practical range of lengths of look-back periods on misclassification of HF events as incident and the association reduction in the number of events. For comparability to previous evaluations of look-back periods, we defined as “true” incident HF events those preceded by a 36-month look-back period. While our definition of “true” incident HF events is not calibrated to a gold standard, the average time between HF hospitalizations and outpatient visits in this population was observed to be <1 year and <6 months respectively.
The trade-off between misclassification and the impact on precision of a reduced number of events can be an important consideration when assessing the merit of various look-back periods. Thus, we present information that can assist researchers in gauging the divergent effects of length of the look-back period by comparing misclassification and precision, as best suited to a study question. We also infer from our results that the short look-back periods commonly used in the analysis of administrative claims data may overestimate HF incidence.
Conclusion
Estimating hospitalized or outpatient HF using Medicare claims requires the use of a look-back period predating a HF event to exclude prior events and thus avoid misclassification bias. The length of the look-back period can substantially influence misclassification of prevalent hospitalized and outpatient HF as incident, as well as the size of the population available for study. Our results, coupled with other evaluations11 suggest that published reports of the incidence of HF derived from administrative claims may be overestimated as a result of the short lengths of prevalent periods used. An optimal trade-off between protection against misclassification bias and loss of events in the estimation of incident HF from administrative claims can be informed by the results presented in this report, and adjusted to different study questions as appropriate.
Supplementary Material
Supplementary Figure. Proportion of false positives and number of events for hospitalized heart failure (CCW), ARIC cohort members enrolled in Medicare Fee-for-Service, 2000–2012
Footnote: The Chronic Conditions Data Warehouse (CCW) chronic condition algorithm for heart failure includes International Classification of Disease, 9th Edition Clinical Modification codes 398.91, 402.01, 402.11, 402.91, 404.01, 404.11, 404.91, 404.03, 404.13, 404.93, 428.0, 428.1, 428.20, 428.21, 428.22, 428.23, 428.30, 428.31, 428.32, 428.33, 428.40, 428.41, 428.42, 428.43, 428.9 in any position. The look-back period is used to exclude patients with prevalent heart failure prior to the index date. Proportion of false positives was calculated as the proportion of incident HF events in a given look-back period relative to the number of true incident HF events.
Supplementary Table. Incidence of hospitalized heart failure (CCW) by length of look-back period, ARIC cohort members enrolled in Medicare Fee-for-Service, 2000–2012 (N = 9568)
Key Points.
Estimating incidence of HF using administrative claims requires the use of a look-back period predating a HF event to exclude prevalent events
Implementation of a look-back period will decrease the amount of bias created by misclassification
The length of the look-back period influences misclassification of prevalent HF events as incident
An optimal trade-off between protection against misclassification bias and loss of events can be based on information presented in this report and adjusted to the study question as appropriate
Acknowledgments
The authors thank the staff and participants of the ARIC study for their important contributions. The Atherosclerosis Risk in Communities Study is carried out as a collaborative study supported by National Heart, Lung, and Blood Institute contracts (HHSN268201100005C, HHSN268201100006C, HHSN268201100007C, HHSN268201100008C, HHSN268201100009C, HHSN268201100010C, HHSN268201100011C, and HHSN268201100012C) with the ARIC carotid MRI examination funded by U01HL075572-01. RC was supported by the National Heart, Lung, and Blood Institute GRS Diversity Supplement (HHSN268201100007C).
Funding
The Atherosclerosis Risk in Communities Study is carried out as a collaborative study supported by National Heart, Lung, and Blood Institute contracts (HHSN268201100005C, HHSN268201100006C, HHSN268201100007C, HHSN268201100008C, HHSN268201100009C, HHSN268201100010C, HHSN268201100011C, and HHSN268201100012C) with the ARIC carotid MRI examination funded by U01HL075572-01. RC was supported by the National Heart, Lung, and Blood Institute GRS Diversity Supplement (HHSN268201100007C).
Footnotes
Conflict of Interests
R. Camplain declares that she has no conflicts of interest; A. Kucharska-Newton declares that she has no conflicts of interest; C. Cuthbertson declares that she has no conflicts of interest; J. Wright declares that she has no conflicts of interest; A. Alonso declares that he has no conflicts of interest; G. Heiss declares that he has no conflicts of interest
Prior Presentations
This work was presented at the American Heart Association EPI/Lifestyle Scientific Sessions (formally EPI/NPAM) annual conference in Baltimore, Maryland, March 2015. http://circ.ahajournals.org/content/131/Suppl_1/AMP56.abstract
Contributor Information
Ricky Camplain, The University of North Carolina at Chapel Hill, Department of Epidemiology, 137 E. Franklin St., Suite 303A, Chapel Hill, NC, USA 27514.
Anna Kucharska-Newton, The University of North Carolina at Chapel Hill, Department of Epidemiology.
Carmen Cuthbertson, The University of North Carolina at Chapel Hill, Department of Epidemiology.
Jacqueline Wright, National Heart, Lung, and Blood Institute, National Institutes of Health.
Alvaro Alonso, Emory University, Department of Epidemiology.
Gerardo Heiss, The University of North Carolina at Chapel Hill, Department of Epidemiology.
References
- 1.Blais C, Dai S, Waters C, et al. Assessing the burden of hospitalized and community-care heart failure in Canada. The Canadian journal of cardiology. 2014 Mar;30(3):352–358. doi: 10.1016/j.cjca.2013.12.013. [DOI] [PubMed] [Google Scholar]
- 2.Yeung DF, Boom NK, Guo H, Lee DS, Schultz SE, Tu JV. Trends in the incidence and outcomes of heart failure in Ontario, Canada: 1997 to 2007. CMAJ : Canadian Medical Association journal = journal de l’Association medicale canadienne. 2012 Oct 2;184(14):E765–773. doi: 10.1503/cmaj.111958. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Akushevich I, Kravchenko J, Ukraintseva S, Arbeev K, Yashin AI. Age patterns of incidence of geriatric disease in the U.S. elderly population: Medicare-based analysis. Journal of the American Geriatrics Society. 2012 Feb;60(2):323–327. doi: 10.1111/j.1532-5415.2011.03786.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Neri L, Rocca Rey LA, Lentine KL, et al. Joint association of hyperuricemia and reduced GFR on cardiovascular morbidity: a historical cohort study based on laboratory and claims data from a national insurance provider. American journal of kidney diseases : the official journal of the National Kidney Foundation. 2011 Sep;58(3):398–408. doi: 10.1053/j.ajkd.2011.04.025. [DOI] [PubMed] [Google Scholar]
- 5.Joynt KE, Orav EJ, Jha AK. The association between hospital volume and processes, outcomes, and costs of care for congestive heart failure. Annals of internal medicine. 2011 Jan 18;154(2):94–102. doi: 10.1059/0003-4819-154-2-201101180-00008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Goyal A, Norton CR, Thomas TN, et al. Predictors of incident heart failure in a large insured population: a one million person-year follow-up study. Circulation. Heart failure. 2010 Nov;3(6):698–705. doi: 10.1161/CIRCHEARTFAILURE.110.938175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Curtis JR, Kramer JM, Martin C, et al. Heart failure among younger rheumatoid arthritis and Crohn’s patients exposed to TNF-alpha antagonists. Rheumatology. 2007 Nov;46(11):1688–1693. doi: 10.1093/rheumatology/kem212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Shafazand S, Yang Y, Amore E, O’Neal W, Brixner D. A retrospective, observational cohort analysis of a nationwide database to compare heart failure prescriptions and related health care utilization before and after publication of updated treatment guidelines in the United States. Clinical therapeutics. 2010 Aug;32(9):1642–1650. doi: 10.1016/j.clinthera.2010.08.002. [DOI] [PubMed] [Google Scholar]
- 9.Bertoni AG, Hundley WG, Massing MW, Bonds DE, Burke GL, Goff DC., Jr Heart failure prevalence, incidence, and mortality in the elderly with diabetes. Diabetes care. 2004 Mar;27(3):699–703. doi: 10.2337/diacare.27.3.699. [DOI] [PubMed] [Google Scholar]
- 10.Kociol RD, Hammill BG, Fonarow GC, et al. Generalizability and longitudinal outcomes of a national heart failure clinical registry: Comparison of Acute Decompensated Heart Failure National Registry (ADHERE) and non-ADHERE Medicare beneficiaries. Am Heart J. 2010 Nov;160(5):885–892. doi: 10.1016/j.ahj.2010.07.020. [DOI] [PubMed] [Google Scholar]
- 11.Griffiths RI, O’Malley CD, Herbert RJ, Danese MD. Misclassification of incident conditions using claims data: impact of varying the period used to exclude pre-existing disease. BMC medical research methodology. 2013;13:32. doi: 10.1186/1471-2288-13-32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.The Atherosclerosis Risk in Communities (ARIC) Study: design and objectives. The ARIC investigators. American journal of epidemiology. 1989 Apr;129(4):687–702. [PubMed] [Google Scholar]
- 13.Goff DC, Jr, Pandey DK, Chan FA, Ortiz C, Nichaman MZ. Congestive heart failure in the United States: is there more than meets the I(CD code)? The Corpus Christi Heart Project. Archives of internal medicine. 2000 Jan 24;160(2):197–202. doi: 10.1001/archinte.160.2.197. [DOI] [PubMed] [Google Scholar]
- 14.Blecker S, Paul M, Taksler G, Ogedegbe G, Katz S. Heart failure-associated hospitalizations in the United States. Journal of the American College of Cardiology. 2013 Mar 26;61(12):1259–1267. doi: 10.1016/j.jacc.2012.12.038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Fang J, Mensah GA, Croft JB, Keenan NL. Heart failure-related hospitalization in the U.S., 1979 to 2004. Journal of the American College of Cardiology. 2008 Aug 5;52(6):428–434. doi: 10.1016/j.jacc.2008.03.061. [DOI] [PubMed] [Google Scholar]
- 16.Khand AU, Shaw M, Gemmel I, Cleland JG. Do discharge codes underestimate hospitalisation due to heart failure? Validation study of hospital discharge coding for heart failure. European journal of heart failure. 2005 Aug;7(5):792–797. doi: 10.1016/j.ejheart.2005.04.001. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary Figure. Proportion of false positives and number of events for hospitalized heart failure (CCW), ARIC cohort members enrolled in Medicare Fee-for-Service, 2000–2012
Footnote: The Chronic Conditions Data Warehouse (CCW) chronic condition algorithm for heart failure includes International Classification of Disease, 9th Edition Clinical Modification codes 398.91, 402.01, 402.11, 402.91, 404.01, 404.11, 404.91, 404.03, 404.13, 404.93, 428.0, 428.1, 428.20, 428.21, 428.22, 428.23, 428.30, 428.31, 428.32, 428.33, 428.40, 428.41, 428.42, 428.43, 428.9 in any position. The look-back period is used to exclude patients with prevalent heart failure prior to the index date. Proportion of false positives was calculated as the proportion of incident HF events in a given look-back period relative to the number of true incident HF events.
Supplementary Table. Incidence of hospitalized heart failure (CCW) by length of look-back period, ARIC cohort members enrolled in Medicare Fee-for-Service, 2000–2012 (N = 9568)