Abstract
Evidence from recent pre-exposure prophylaxis (PrEP) trials has demonstrated its safety and efficacy in significantly reducing the risk of HIV acquisition for those who are at considerable risk of acquiring HIV infection. With a rapid increase in the amount of research on the efficacy of PrEP for HIV prevention, complementary research on the willingness to use PrEP has grown, especially among MSM, but limited research has been focused among people who use drugs (PWUD). As part of the formative process, we utilized the Information-Motivation-Behavioral Skills (IMB) model of health behavior change to characterize and guide intervention development for promoting willingness to use PrEP among high-risk PWUD. The analysis included 400 HIV-negative high-risk PWUD enrolled in a community-based methadone maintenance treatment who reported drug- and/or sex-related HIV risk behaviors in the past 6-months. Analyses revealed support for the IMB model as PrEP-related behavioral skills were found to mediate the influence of PrEP-related information and motivation on willingness to use PrEP. The results provide evidence as to the utility of the IMB model to increase willingness to use PrEP among high-risk PWUD. It therefore makes an important contribution to our understanding of the applicability of theoretically-grounded models of willingness to use PrEP among high-risk PWUD, who are one of the key risk populations who could benefit from the use of PrEP.
Keywords: Pre-exposure prophylaxis, people who use drugs, substance use, IMB model, HIV, structural equation modeling
Introduction
Despite a number of evidence-based interventions, HIV incidence in the US has been unchanged for the past 15 years [1]. People who use drugs (PWUD) continue to account for a substantial proportion of new HIV infections, which occurs through preventable injection-drug use and sexual risk behaviors [2–7]. A recent advancement with enormous potential for high-risk PWUD involves Pre-Exposure Prophylaxis (PrEP) – the routine self-administration of the antiretroviral medication, Truvada™ (Tenofovir/emtricitabine) – as a means to foster primary HIV prevention [8]. PrEP is an HIV prevention method that involves high risk HIV-uninfected individuals taking antiretroviral therapy (ART) in anticipation of potential HIV exposure in order to reduce the risk of HIV infection [9].
Evidence from recent PrEP trials has demonstrated its safety and efficacy in significantly reducing the risk of HIV acquisition for those who are at considerable risk of acquiring HIV infection, such as men who have sex with men (MSM), people who inject drugs (PWID), sex workers, and transgender people [10–14]. For instance, Choopanya et al. (2013) demonstrated a 48.9% decrease in the risk of acquiring HIV among PWID in Bangkok, Thailand. In a separate analysis, the risk was reduced by approximately 74% reduction in participants with detectable levels of tenofovir in their blood. Consistent with the results of other PrEP trials [10–13], this trial did not identify any significant safety concerns associated with daily PrEP use [14]. Thus, the Centers for Disease Control and Prevention (CDC) and the World Health Organization (WHO) have recommended the use of PrEP as part of a comprehensive set of HIV prevention services, identifying PWUD as one of the key populations that could benefit from its use [8, 15]. This has provided unprecedented opportunities in our public health response to curtail the HIV epidemic.
With a rapid increase in the amount of research on the efficacy of PrEP for HIV prevention, complementary research on the willingness to use PrEP and its uptake has gained prominence [16–19]. In the US, there has been considerable increase in studies assessing willingness to use PrEP, especially among MSM, but limited research has been focused among PWUD [20–27]. With regard to PWID, two studies have been published so far, which showed that very few people (7% – 13%) were aware of PrEP and fairly low willingness to use PrEP for HIV prevention (~ 50%), compared to MSM [23, 26]. This is alarming since PWUD frequently report engaging in high-risk behaviors across both sexual and drug use domains and could greatly benefit from the use of PrEP.
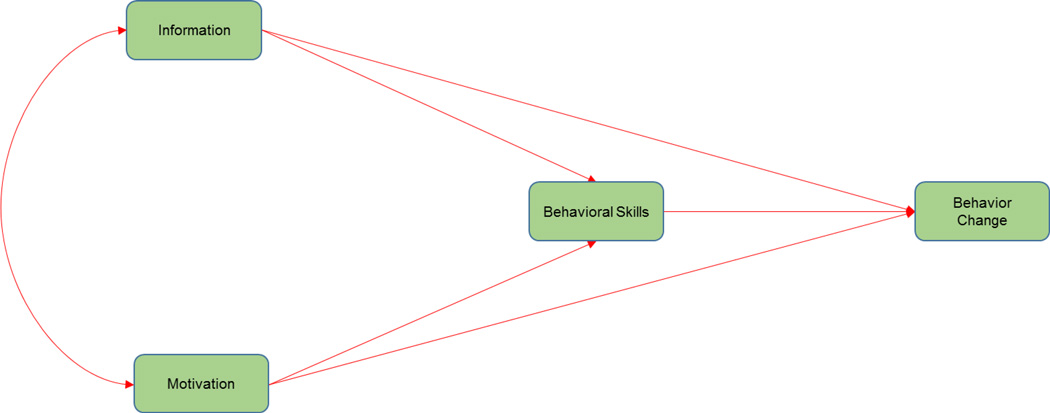
An application of a theory-based model to understand willingness to use PrEP can help researchers to identify the critical dynamics of this underserved population, and to develop tailored interventions to promote PrEP uptake and adherence. As part of the formative process, we utilized the Information-Motivation-Behavioral Skills (IMB) model of health behavior change [28, 29] to characterize and guide intervention development for promoting willingness to use PrEP among high-risk PWUD. In brief, the IMB model asserts that information, motivation, and behavioral skills are important determinants of health behavior change. Information and motivation work mainly through behavioral skills to influence change in behavior. The model also specifies that information and motivation may have direct effects on behavior change (Figure 1).
Figure 1.
IMB model of health behavior change [28]
While the IMB model has been successfully utilized as a theoretical framework for the design and evaluation of a wide range of intervention strategies across different behaviors, populations, and contexts [30–37], it has not yet been applied to PrEP usage. In the present study, we therefore tested a theory-based model using constructs from the IMB model [28, 29] and applied it to PrEP use as HIV prevention among opioid-dependent persons at risk for HIV. Aligned with the IMB model, we hypothesized that information (e.g., knowledge of PrEP effectiveness, side effects, monitoring) and motivation (e.g., personal and/or social motivation toward PrEP use) would be significantly associated with behavioral skills (e.g., adherence self-efficacy, side effect management, PrEP negotiation, sustained PrEP adherence). In turn, behavioral skills were hypothesized to mediate the influence of information and motivation on willingness to use PrEP. Further, we expect that information and motivation would be directly associated with willingness to use PrEP.
Methods
Participants and procedures
A cross-sectional study was conducted among high-risk PWUD enrolled in a community-based methadone maintenance program (MMP) in New Haven, Connecticut that provides drug treatment and clinical care to opioid-dependent PWUD [38]. Individuals in the MMP were eligible to participate in the study, if they were: i) 18 years or older, ii) HIV-negative, iii) reported drug- or sex-related HIV risk behaviors in the past 6 months, iv) and met DSM-V criteria for opioid use disorders.
Between June and July 2016, a total of 400 participants were recruited using a convenience sampling process. Potential participants were recruited via flyers, peers, word-of-mouth, and direct referral from their counselors at the MMP. Potential participants were screened in-person in a private room or by phone using a screening form. Individuals who met inclusion criteria, and who were willing to participate, were provided a description of the study and invited to provide informed consent, followed by the survey. Participants were assessed using an audio computer assisted self-interview (ACASI) that has demonstrated sound psychometric properties in prior studies [39]. All participants were reimbursed for the time and effort needed to participate in the survey. The study protocol was approved by the Investigational Review Board at the [BLINDED FOR REVIEW] and received board approval from the MMP (APT Foundation Inc.).
Measures
Socio-demographic variables included self-reported measures of age, gender, sexual orientation, ethnicity, marital status, educational status, employment status, and income. Participants’ self-report measure of drug use and sex-related HIV risk behaviors during the past 30 days were assessed using an adapted version of the HIV risk-taking behavior scale (HRBS) [40]. We utilized four out of the eleven items from the original scale to measure risk behaviors among our sample (Table 1).
Table 1.
Characteristics of the participants (N = 400)
| Variable | Frequency | % |
|---|---|---|
| Age: Mean (±SD) | 40.9 (11.1) | |
| Gender | ||
| Male | 234 | 58.5 |
| Female | 166 | 41.5 |
| Sexual orientation | ||
| Heterosexual or straight | 345 | 86.3 |
| Homosexual, gay, or lesbian | 16 | 4.0 |
| Bisexual | 39 | 9.7 |
| Ethnicity | ||
| White | 253 | 63.2 |
| African American | 70 | 17.5 |
| Hispanic or Latino | 61 | 15.3 |
| Other | 16 | 4.0 |
| Marital status | ||
| Married | 83 | 20.8 |
| Divorced | 111 | 27.8 |
| Widowed | 14 | 3.5 |
| Single | 192 | 48.0 |
| High school graduate | 293 | 73.3 |
| Employed | 69 | 17.3 |
| Income | ||
| < $10,000 | 312 | 78.0 |
| $10,000 – $19,999 | 57 | 14.2 |
| ≥ $20,000 | 31 | 7.8 |
| Injected illicit drugs (past 30 days) | 230 | 57.5 |
| Shared needles/works (past 30 days) | n = 230 | |
| No | 80 | 34.8 |
| Yes | 150 | 65.2 |
| Ever been sexually active (past 30 days) | 328 | 82.0 |
| Number of sexual partners (past 30 days) | n = 328 | |
| 1 | 197 | 60.0 |
| 2 – 5 | 116 | 35.4 |
| ≥ 6 | 15 | 4.6 |
| Always used condom with casual partner | n = 328 | |
| No casual partner | 64 | 19.5 |
| No | 215 | 65.6 |
| Yes | 49 | 14.9 |
| Heard about PrEP | 72 | 18.0 |
| Willing to use PrEP | 251 | 62.7 |
SD: standard deviation; PrEP: pre-exposure prophylaxis
Awareness and acceptability of PrEP use
Participants were asked about their awareness about PrEP prior to participating in the survey using, “Before participating in this survey, have you ever heard about PrEP?” Additionally, their willingness to use PrEP was assessed after providing a brief description of PrEP (Appendix). After reviewing this description, participants were asked to respond to a statement, “I would be interested in taking PrEP to reduce my current risk of HIV infection” on a five-point Likert scale of: “strongly disagree” to “strongly agree”. For data analysis, willingness to use PrEP was further dichotomized into “Yes” (strongly agree and agree) and “No” (strongly disagree, disagree, neutral) [41].
IMB Measures
Consistent with the IMB model [28, 32], participants completed an assessment that included following domains: information, motivation, and behavioral skills. IMB measures related to PrEP was developed based on feedback from focus group sessions with target population (high-risk PWUD) and treatment providers (e.g., physicians, nurses, substance abuse counselors), existing literature on PrEP, and adaptation of HIV-related IMB measures used in prior studies [29, 39]. We then performed an initial exploration of each construct’s measurement model to further inform out item selection decisions. Responses were analyzed as continuous measures, or dichotomized into an IMB strengths/deficits-based approaches. All responses were recoded and summed up so that higher values indicated higher levels of information, motivation, and behavioral skills. Each IMB construct consisted of several associated observable variables that could be directly measured. Structural equation modelling (SEM) was used to estimate the structural coefficients between constructs or latent variables. A specific description of the measures included in the IMB model constructs are described below:
Information
Participants’ PrEP related knowledge (e.g., knowledge of PrEP effectiveness, side effects, monitoring) was measured with twelve items with “yes”, “no” or “do not know” as answers (e.g., “When on PrEP, I don’t need to use new or clean needles”; “PrEP provides protection against other sexually transmitted infections”; “When on PrEP, I don’t need to use condoms”; “While I’m on PrEP, I will need to go for regular doctor visits”; “The short-term side-effects of PrEP may include nausea and dizziness”). Positive responses were scored as one, and negative responses were assigned a score of zero. Higher scores indicated more information about PrEP.
Motivation
Sixteen items were used to examine participants' motivation about PrEP use (e.g., personal and/or social motivation toward PrEP use). Questions included, “I think I would be less worried about HIV infection if I were on PrEP”; “If I were on PrEP, I would not be concerned about the potential side-effects of PrEP”; “If I disclose that I’m on PrEP to my sex partner, he/she will be comfortable with it.”; “I have a responsibility to contribute to HIV prevention efforts by using PrEP”; “I would take PrEP if I know someone (e.g., friend, family member) who is currently taking it”; “I have family members or friends to encourage me to take PrEP properly.” Answers for motivation items were measured on a five-point Likert scale (0 “Strongly disagree” and 4 “Strongly agree”).
HIV behavioral skills
Eleven items were used to assess participants' behavioral skills (e.g., adherence self-efficacy, side effect management, PrEP negotiation, sustained PrEP adherence) about PrEP use (e.g., “How confident are you that you would stick to your PrEP medication even if you have some side-effects (e.g., nausea)?”; “How confident are you that you could make PrEP part of your daily routine?”; “How confident are you that you could get PrEP refills before you run out?”; “How confident are you that you could continue with your PrEP regimen even if getting to your clinic appointments is a major hassle?”; “How confident are you that you would stop sharing needles or works while on PrEP?”; “How confident are you that you would use condoms while on PrEP?”). Answers for these items were constructed on a five-point Likert scale (0 “not at all confident” and 4 “completely confident”).
Data analysis
All IMB items were evaluated for any missing data. All available data were included via maximum likelihood estimation, a preferred method for handling missing data when assumed missing-at-random [42]. Analyses were carried out in Mplus Version 7.31 [43], which includes the capability to test models using a full information (direct) maximum likelihood estimator to account for missing data [44]. Model fit was assessed with the chi-square statistics (χ2) [45], the comparative fit index (CFI) [46], the Tucker-Lewis index (TLI) [47], Root Mean Square Error of Approximation (RMSEA) [48], and the Standardized Root Mean Square Residual (SRMR) [49, 50]. Non-significant χ2, values of 0.95 or greater for the CFI and TLI, 0.08 or below for the RMSEA, and below 0.05 for the SRMR were generally regarded as indicative of good fit.
Measurement Models
First, we conducted confirmatory factor analysis (CFA) to test the fit of each of the IMB constructs. For each measurement model, the best fitting model was assessed by evaluating a single latent construct for each IMB construct. The full item set for each construct was then loaded on to its respective latent variables. Individual items were removed from the scale if they had a non-significant factor loading (p > 0.05) or if unstandardized factor loading estimate was < 0.40. Individual error variances were considered to be significantly correlated if they had a modification index > 10 and if they were theoretically related items. This process of excluding items and correlating errors was iteratively repeated until the best fitting measurement model was obtained (i.e., non-significant χ2, CFI > 0.95, TLI > 0.95, RMSEA < 0.08, SRMR < 0.05).
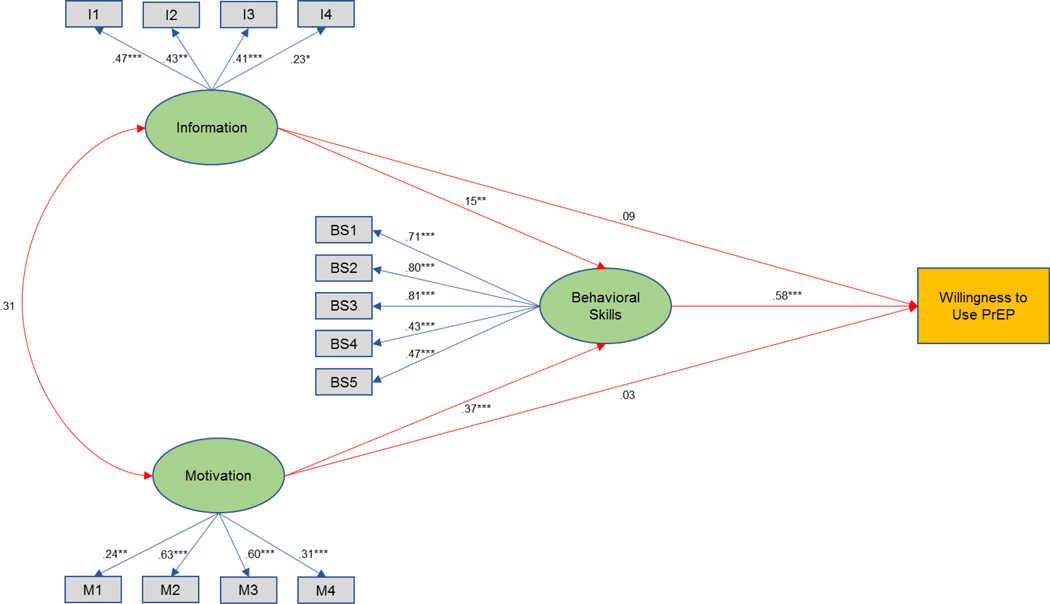
Path models
Once the factor structure was confirmed, we evaluated the full IMB model of acceptability of PrEP use (Figure 2) in which four construct (information, motivation, behavioral skills, and PrEP acceptability) were used in a structural equation model. Consistent with IMB model [28], information and motivation were related to behavioral skills, and behavioral skills were related to acceptability of PrEP use (mediation effect). Information and motivation were each also permitted to relate directly to acceptability of PrEP use (direct effect). The parameter estimates, in terms of path loadings and significance levels, and fit indices were used for evaluating the full IMB model.
Figure 2.
An empirical test of the IMB model of willingness to use PrEP using SEM with standardized path coefficients
Note: Coefficients are standardized path coefficients.
Overall model fit, χ2 (72, N = 400) = 113.08, p = 0.024, CFI = 0.95, TLI = 0.93 RMSEA = 0.09 (90% CI: 0.05 – 0.14) SRMR = 0.045.
For tests of significance of individual paths, *p < 0.05, **p < 0.01 and ***p < 0.001. Legend: PrEP: pre-exposure prophylaxis
Results
Participant characteristics
A total of 400 participants completed the questionnaire. The average age of the participants was 40.9 ± 11.1 years and 58.5% were male. The majority of participants identified as heterosexual or straight (86.3%), White (63.2%), high school graduates (73.2%), not employed (82.8%), and reported an income at or below $10,000 per year (78%). Self-reported HIV risk behaviors were highly prevalent. Over half of the participants (57.5%) reported injecting illicit drugs and two-third reported sharing needles/works in the past 30 days. Of those who were sexually active (82.0%), the majority reported having multiple sexual partner (39.9%); however, only 14.9% reported having consistently used a condom with casual sexual partners. Only 18% of participants had heard of PrEP as a method to prevent HIV infection. When presented with information about PrEP, however, almost two-thirds of participants (62.7%) reported that they would be interested in using PrEP to reduce their risk of contracting HIV infection (Table 1).
Measurement model
Table 2 presents the tests of significance and estimated CFA with parameters of the IMB constructs. The mean knowledge score of the information component for this sample was 3.61 (SD = .699) on a scale of 0 to 4. The mean motivation score was 10.12 (SD = 2.519) on a scale of 0 – 16. The mean behavioral skills score was 10.88 (SD = 4.207) on a scale of 0 – 20. The reliability of the IMB constructs ranged from good to acceptable (αI = 0.892; αM = 0.763; αBS = 0.811), and all factor loadings were significant (p < 0.05).
Table 2.
Constructs for PrEP related Information, Motivation, and Behavioral Skills (N = 400)
| Constructs | Items | β | p | SE | Mean | SD | CFS/TLI | RMSEA | SRMR | α | |
|---|---|---|---|---|---|---|---|---|---|---|---|
|
Information (0 – 4) |
I-1 | When on PrEP, I don’t need to use new or clean needles. |
.438 | <.0001 | .103 | 3.61 | .699 | 1.000 / 1.000 |
.072 | .012 | .892 |
| I-2 | PrEP provides protection against other sexually transmitted infections. |
.461 | <.0001 | .128 | |||||||
| I-3 | When on PrEP, I don’t need to use condoms. | .408 | <.0001 | .114 | |||||||
| I-4 | The short-term side-effects of PrEP may include nausea and dizziness. |
.245 | .008 | .092 | |||||||
|
Motivation (0 – 16) |
M-1 | It is important to me to not to get HIV in the next year. |
.260 | .002 | .085 | 10.12 | 2.519 | .969 / .907 |
.051 | .022 | .763 |
| M-2 | I think I would be less worried about HIV infection if I were on PrEP. |
.659 | <.0001 | .127 | |||||||
| M-3 | If I were on PrEP, I would not be concerned about the potential side-effects of PrEP. |
.578 | <.0001 | .103 | |||||||
| M-4 | I have a responsibility to contribute to HIV prevention efforts by using PrEP. |
.282 | .001 | .083 | |||||||
|
Behavioral Skills (0 – 20) |
BS-1 | How confident are you that you would stick to your PrEP medication even if you have some side-effects (e.g., nausea)? |
.717 | <.0001 | .041 | 10.88 | 4.207 | .971 / .942 |
.075 | .032 | .811 |
| BS-2 | How confident are you that you could make PrEP part of your daily routine? |
.806 | <.0001 | .034 | |||||||
| BS-3 | How confident are you that you could get PrEP refills before you run out? |
.797 | <.0001 | .038 | |||||||
| BS-4 | How confident are you that you could continue with your PrEP regimen even if getting to your clinic appointments is a major hassle? |
.432 | <.0001 | .050 | |||||||
| BS-5 | How confident are you that you would stop sharing needles or works while on PrEP? |
.459 | <.0001 | .051 | |||||||
SE: standard error; SD: standard deviation; CFS/TLI: Comparative Fit Index/Tucker-Lewis Index; RMSEA: Root Mean Square Error of Approximation; SRMR: Standardized Root Mean Square Residual; PrEP: pre-exposure prophylaxis
In fitting the initial constructs of the IMB model [28], the a priori measurement models did not have an acceptable fit to the data. The CFA yielded a reduced number of items for each of the measures, which resulted in an acceptable to good fit for all three domains of the IMB model. The CFA model for the information construct resulted in retaining four items with a good fitting model [χ2 (2, N = 400) = 0.689, p = 0.708, CFI = 1.000, TLI = 1.000, RMSEA = 0.072, SRMR = 0.012]. The reduced four-factor model of motivation yielded a good fitting model on a single latent construct [χ2 (2, N = 400) = 4.114, p = 0.127, CFI = 0.969, TLI = 0.907, RMSEA = 0.051, SRMR = 0.022]. Similarly, the CFA model for behavioral skills yielded a good fitting model [χ2 (5, N = 400) = 16.109, p = 0.006, CFI = 0.971, TLI = 0.942, RMSEA = 0.975, SRMR = 0.032] with five items (Table 2).
Path model
As indicated in Figure 2, the path coefficients for the full (mediated) IMB model supported our hypotheses. As expected, information and motivation were not significantly related to one another. Paths from information to behavioral skills (β = 0.15, p = 0.016) and from motivation to behavioral skills (β = 0.37, p < 0.001) were significant and in the predicted direction. Also as predicted by the IMB model, the path from behavioral skills to willingness to use PrEP was significant (β = 0.58, p < 0.001) and in the anticipated direction. The overall fit of the model was good according to standard model fit indices: χ2 (72, N = 400) = 113.08, p = 0.024, CFI = 0.95, TLI = 0.93, RMSEA = 0.09 (90% CI: 0.05 – 0.14), SRMR = 0.045), with the model accounting for approximately 36.6% of the variability in willingness to use PrEP.
Discussion
This is the first study to apply a theory-based framework using constructs adapted from the IMB model [28] to conceptualize the determinants of willingness to use PrEP among high-risk PWUD. Specifically, we evaluated the IMB model’s central propositions that PrEP-related information and motivation were each significantly associated with behavioral skills related to PrEP which, in turn, would be related to willingness to use PrEP. Using structural measured and latent variable modeling techniques, we found support for each of the propositions of the IMB model of willingness to use PrEP. This indicates that the enhancement of PrEP-related information and motivation positively influences behavioral skills related to PrEP use. A higher degree of HIV behavioral skills, in turn, was associated with increased willingness to use PrEP. The results thus demonstrate the utility of the IMB framework of willingness to use PrEP to inform future interventions to increase PrEP uptake among high-risk PWUD.
The results obtained from the final IMB model showed that willingness to use PrEP was mainly predicted by behavioral skills, and there was no significant direct pathway from PrEP-related information and motivation to willingness to use PrEP. This finding was inconsistent with the classic IMB model [28]. This result is, however, consistent with the findings from prior studies of the adapted IMB model of ART adherence [51–53], diabetes medication adherence [35, 54], intention to smoke [55], and medication prescribing behaviors among the doctors [56]. It is suggested that information and motivation may have no direct effect on change in behavior when the behavior itself is very complex or requires multiple behavioral skills to accomplish. In the context of this study, the willingness to use PrEP is multifaceted, which depends not only on individuals themselves (e.g., knowledge about PrEP, social motivation for taking medications, barriers to personal motivation), health care providers (e.g., health care providers’ attitude toward PrEP, risk assessment), and national policies, but also requires multiple behavioral skills (e.g., sustained PrEP adherence, side-effect management, PrEP negotiation) to initiate and maintain the uptake of PrEP. Overall, the results suggest that willingness to use PrEP is associated with more accurate information about PrEP, stronger personal and social motivation for taking PrEP, and stronger behavioral skills to take PrEP on a regular basis.
Although there is a considerable increase in a number of PrEP demonstration projects among MSM, to date, very little if any attention has been given to incorporate PrEP into HIV prevention approaches targeting PWUD. Therefore, a key purpose of this study was to characterize and to develop a theory-grounded PrEP intervention specifically tailored toward high-risk PWUD. Our results lend support to the growing body of literature and recommendations of tailoring health promotion interventions to the knowledge, motivation, and behavioral skills needs of specific high risk groups. Based on the findings of this study, and consistent with the IMB model [28], intervention to enhance PrEP uptake may be most effective if intervention components target: 1) PrEP-related information (e.g., knowledge about PrEP effectiveness, side effects, adherence, perceived affordability, risk compensation, effect of continued drug use on PrEP efficacy), 2) personal motivation (e.g., sexual expectancies, acceptability, anticipated HIV stigma, safe sex initiation, safe drug use practices, perceived and controlled risk of HIV, benefit of substance abuse treatment program) and social motivation (e.g., prevention altruism, peer values and medication use, peer sex and drug use norms, dyadic decision making, role of substance abuse counselors and the clinic), and 3) the development of practical behavioral skills in adhering to PrEP medications (e.g., taking it with methadone), managing side effects, negotiating PrEP use, sustaining motivation, and safer sex and drug use practices in the context of PrEP. Such interventions are likely to be more effective in increasing individuals’ willingness to use PrEP and also adhering to it.
This study has a number of potential limitations that should also be acknowledged. First, issues surrounding cross-sectional nature of the data is noteworthy. As with all cross-sectional study design, the modelling result from this study is only able to assess associations, rather than causal relationships, between IMB constructs and acceptability of PrEP use. Second, the use of self-report measures in the current study may be prone to reporting bias and thus may have reduced our ability to precisely detect some variables (e.g., information, acceptability of PrEP use). Third, a brief description of PrEP was provided prior to assessing IMB measures, which could have influenced participants’ responses to subsequent questions. Fourth, although a brief explanation about PrEP was provided, we do not know the extent to which participants understood every aspects of PrEP (e.g., effectiveness, cost, side-effects, dispensing venue, adherence, etc.) while providing responses regarding willingness to use PrEP. Fourth, the participants in this study were high-risk PWUD enrolled in MMP; thus, our findings may not be generalizable to all risk groups. Fifth, the use of a convenience sampling strategy to recruit participants may limit the potential external validity of the results. Sixth, the measure of behaviors skills used in the study focused on the perceived self-efficacy in performing various skills (e.g., adherence, side effect management, PrEP negotiation). The IMB theory specifies the use of enactment of behaviors necessary to change health behavior, in addition to self-efficacy. Thus, it is not clear how the omission of actual behavioral skills from our measures may have influenced the results. Finally, it is possible that people who have injected within the past 6 months may have different attitudes toward PrEP than their counterparts, however, exploring this differential impact was beyond the scope of this study. Thus, future studies would benefit from the comparative assessment of injection history on PrEP attitudes among this sample.
Conclusions
This study is the first to empirically test the IMB model of willingness to use PrEP and to offer a more comprehensive understanding of the elements that should be incorporated in future PrEP interventions. The results provide support for the IMB model as PrEP-related behavioral skills were found to mediate the influence of PrEP-related information and motivation on willingness to use PrEP. This test of the IMB model, a prominent theoretical model of health behavior change [28], provides evidence as to the utility of the IMB model to increase willingness to use PrEP among high-risk PWUD. It therefore makes an important contribution to our understanding of the applicability of theoretically-grounded models of willingness to use PrEP among high-risk PWUD, who are one of the key risk populations who could benefit from the use of PrEP.
Acknowledgments
Source of Funding: This work was supported by grants from the National Institute on Drug Abuse for research (R01 DA025943 to FLA) and for career development (K24 DA017072 to FLA; K02 033139 to MMC).
Appendix
Brief description of pre-exposure prophylaxis (PrEP) provided to the participants
“There is a new way to prevent HIV infection for people who may be exposed to the virus. It is called Pre-Exposure Prophylaxis or PrEP. It involves an HIV-negative person taking a pill daily, on an ongoing basis (starting before an exposure and continuing after for as long as the person is at risk) to reduce their risk of HIV infection. Research suggests that PrEP is generally safe and is highly effective (over 90%) in preventing HIV infection if taken every day. It is much less effective if not taken every day and does not protect against other sexually transmitted infections. Taking PrEP would require a visit to a doctor every three months in order to be tested for HIV, STIs and side effects.”
Footnotes
Conflicts of Interest: The authors have no conflicts of interest to disclose.
Ethical approval
The study protocol was approved by the Investigational Review Board (IRB) at the University of Connecticut and received board approval from APT Foundation Inc. All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Compliance with Ethical Standards
Informed consent
Informed consent was obtained from all individual participants included in the study.
References
- 1.CDC. HIV surveillance report: Diagnoses of HIV infection in the United States and dependent areas, 2015. Vol. 27. Atlanta, GA: 2016. [Google Scholar]
- 2.Arasteh K, Jarlais DCD, Perlis TE. Alcohol and HIV sexual risk behaviors among injection drug users. Drug & Alcohol Dependence. 2008;95(1):54–61. doi: 10.1016/j.drugalcdep.2007.12.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Marshall BDL, Friedman SR, Monteiro JFG, Paczkowski M, Tempalski B, Pouget ER, Lurie MN, Galea S. Prevention And Treatment Produced Large Decreases In HIV Incidence In A Model Of People Who Inject Drugs. Health Affairs. 2014;33(3):401–409. doi: 10.1377/hlthaff.2013.0824. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Strathdee SA, Hallett TB, Bobrova N, Rhodes T, Booth R, Abdool R, Hankins CA. HIV and risk environment for injecting drug users: the past, present, and future. The Lancet. 2010;376(9737):268–284. doi: 10.1016/S0140-6736(10)60743-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Volkow ND, Montaner J. The urgency of providing comprehensive and integrated treatment for substance abusers with HIV. Health affairs (Project Hope) 2011;30(8):1411–1419. doi: 10.1377/hlthaff.2011.0663. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Shrestha R, Krishnan A, Altice FL, Copenhaver M. A non-inferiority trial of an evidence-based secondary HIV prevention behavioral intervention compared to an adapted, abbreviated version: Rationale and intervention description. Contemporary Clinical Trials. 2015;44:95–102. doi: 10.1016/j.cct.2015.08.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Shrestha R, Copenhaver M. The Influence of Neurocognitive Impairment on HIV Risk Behaviors and Intervention Outcomes among High-Risk Substance Users: A Systematic Review. Frontiers in Public Health. 2016;4(16) doi: 10.3389/fpubh.2016.00016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.CDC. Preexposure prophylaxis for the prevention of HIV infection in the United States—2014: a clinical practice guideline. Washington, DC: Department of Health and Human Services USA—Centers for Disease Control and Prevention; 2014. [Google Scholar]
- 9.Kelesidis T, Landovitz RJ. Preexposure Prophylaxis for HIV Prevention. Current HIV/AIDS Reports. 2011;8(2):94–103. doi: 10.1007/s11904-011-0078-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Grant RM, Lama JR, Anderson PL, McMahan V, Liu AY, Vargas L, Goicochea P, Casapía M, Guanira-Carranza JV, Ramirez-Cardich ME, et al. Preexposure Chemoprophylaxis for HIV Prevention in Men Who Have Sex with Men. The New England journal of medicine. 2010;363(27):2587–2599. doi: 10.1056/NEJMoa1011205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Baeten JM, Donnell D, Ndase P, Mugo NR, Campbell JD, Wangisi J, Tappero JW, Bukusi EA, Cohen CR, Katabira E, et al. Antiretroviral Prophylaxis for HIV Prevention in Heterosexual Men and Women. New England Journal of Medicine. 2012;367(5):399–410. doi: 10.1056/NEJMoa1108524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Thigpen MC, Kebaabetswe PM, Paxton LA, Smith DK, Rose CE, Segolodi TM, Henderson FL, Pathak SR, Soud FA, Chillag KL, et al. Antiretroviral Preexposure Prophylaxis for Heterosexual HIV Transmission in Botswana. New England Journal of Medicine. 2012;367(5):423–434. doi: 10.1056/NEJMoa1110711. [DOI] [PubMed] [Google Scholar]
- 13.Van Damme L, Corneli A, Ahmed K, Agot K, Lombaard J, Kapiga S, Malahleha M, Owino F, Manongi R, Onyango J, et al. Preexposure Prophylaxis for HIV Infection among African Women. New England Journal of Medicine. 2012;367(5):411–422. doi: 10.1056/NEJMoa1202614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Choopanya K, Martin M, Suntharasamai P, Sangkum U, Mock PA, Leethochawalit M, Chiamwongpaet S, Kitisin P, Natrujirote P, Kittimunkong S, et al. Antiretroviral prophylaxis for HIV infection in injecting drug users in Bangkok, Thailand (the Bangkok Tenofovir Study): a randomised, double-blind, placebo-controlled phase 3 trial. The Lancet. 2013;381(9883):2083–2090. doi: 10.1016/S0140-6736(13)61127-7. [DOI] [PubMed] [Google Scholar]
- 15.WHO. Guideline on when to start antiretroviral therapy and on pre-exposure prophylaxis for HIV. Geneva, Switzerland: 2015. [PubMed] [Google Scholar]
- 16.Young I, McDaid L. How acceptable are antiretrovirals for the prevention of sexually transmitted HIV?: A review of research on the acceptability of oral pre-exposure prophylaxis and treatment as prevention. AIDS Behav. 2014;18(2):195–216. doi: 10.1007/s10461-013-0560-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.King HL, Keller SB, Giancola MA, Rodriguez DA, Chau JJ, Young JA, Little SJ, Smith DM. Pre-Exposure Prophylaxis Accessibility Research and Evaluation (PrEPARE Study) AIDS and behavior. 2014;18(9):1722–1725. doi: 10.1007/s10461-014-0845-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Cohen SE, Vittinghoff E, Bacon O, Doblecki-Lewis S, Postle BS, Feaster DJ, Matheson T, Trainor N, Blue RW, Estrada Y, et al. High Interest in Preexposure Prophylaxis Among Men Who Have Sex With Men at Risk for HIV Infection: Baseline Data From the US PrEP Demonstration Project. JAIDS Journal of Acquired Immune Deficiency Syndromes. 2015;68(4):439–448. doi: 10.1097/QAI.0000000000000479. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Hood JE, Buskin SE, Dombrowski JC, Kern DA, Barash EA, Katzi DA, Golden MR. Dramatic increase in preexposure prophylaxis use among MSM in Washington state. AIDS. 2016;30(3):515–519. doi: 10.1097/QAD.0000000000000937. [DOI] [PubMed] [Google Scholar]
- 20.Peng B, Yang X, Zhang Y, Dai J, Liang H, Zou Y, Luo J, Peng H, Zhong X, Huang A. Willingness to use pre-exposure prophylaxis for HIV prevention among female sex workers: a cross-sectional study in China. HIV/AIDS (Auckland, NZ) 2012;4:149–158. doi: 10.2147/HIV.S33445. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Hoagland B, De Boni RB, Moreira RI, Madruga JV, Kallas EG, Goulart SP, Cerqueira N, Torres TS, Luz PM, Fernandes NM, et al. Awareness and Willingness to Use Pre-exposure Prophylaxis (PrEP) Among Men Who Have Sex with Men and Transgender Women in Brazil. AIDS and Behavior. 2016 doi: 10.1007/s10461-016-1516-5. [DOI] [PubMed] [Google Scholar]
- 22.Goedel WC, Halkitis PN, Greene RE, Duncan DT. Correlates of Awareness of and Willingness to Use Pre-exposure Prophylaxis (PrEP) in Gay, Bisexual, and Other Men Who Have Sex with Men Who Use Geosocial-Networking Smartphone Applications in New York City. AIDS and Behavior. 2016;20(7):1435–1442. doi: 10.1007/s10461-016-1353-6. [DOI] [PubMed] [Google Scholar]
- 23.Kuo I, Olsen H, Patrick R, Phillips G, II, Magnus M, Opoku J, Rawls A, Peterson J, Hamilton F, Kharfen M, et al. Willingness to use HIV pre-exposure prophylaxis among community-recruited, older people who inject drugs in Washington, DC. Drug & Alcohol Dependence. 2016;164:8–13. doi: 10.1016/j.drugalcdep.2016.02.044. [DOI] [PubMed] [Google Scholar]
- 24.Young I, Li J, McDaid L. Awareness and Willingness to Use HIV Pre-Exposure Prophylaxis amongst Gay and Bisexual Men in Scotland: Implications for Biomedical HIV Prevention. PLoS One. 2013;8(5):e64038. doi: 10.1371/journal.pone.0064038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Gredig D, Uggowitzer F, Hassler B, Weber P, Nideröst S. Acceptability and willingness to use HIV pre-exposure prophylaxis among HIV-negative men who have sex with men in Switzerland. AIDS Care. 2016;28(sup1):44–47. doi: 10.1080/09540121.2016.1146212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Stein M, Thurmond P, Bailey G. Willingness to use HIV pre-exposure prophylaxis among opiate users. AIDS and Behavior. 2014;18(9):1694–1700. doi: 10.1007/s10461-014-0778-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Ferrer L, Folch C, Fernandez-Davila P, Garcia A, Morales A, Belda J, Susperregui A, Casabona J. Awareness of Pre-exposure Prophylaxis for HIV, Willingness to Use It and Potential Barriers or Facilitators to Uptake Among Men Who Have Sex with Men in Spain. AIDS and Behavior. 2016:1–11. doi: 10.1007/s10461-016-1379-9. [DOI] [PubMed] [Google Scholar]
- 28.Fisher JD, Fisher WA. Changing AIDS-risk behavior. Psychological bulletin. 1992;111(3):455–474. doi: 10.1037/0033-2909.111.3.455. [DOI] [PubMed] [Google Scholar]
- 29.Fisher JD, Fisher WA, Amico KR, Harman JJ. An information-motivationbehavioral skills model of adherence to antiretroviral therapy. Health psychology : official journal of the Division of Health Psychology, American Psychological Association. 2006;25(4):462–473. doi: 10.1037/0278-6133.25.4.462. [DOI] [PubMed] [Google Scholar]
- 30.Bian C, Xu S, Wang H, Li N, Wu J, Zhao Y, Li P, Lu H. A study on the application of the information-motivation-behavioral skills (IMB) model on rational drug use behavior among second-level hospital outpatients in Anhui, China. PloS one. 2015;10(8):e0135782. doi: 10.1371/journal.pone.0135782. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Fisher JD, Fisher WA, Bryan AD, Misovich SJ. Information-motivation-behavioral skills model-based HIV risk behavior change intervention for inner-city high school youth. Health Psychol. 2002;21(2):177–186. [PubMed] [Google Scholar]
- 32.Fisher JD, Fisher WA, Williams SS, Malloy TE. Empirical tests of an information-motivation-behavioral skills model of AIDS-preventive behavior with gay men and heterosexual university students. Health Psychology. 1994;13(3):238–250. doi: 10.1037//0278-6133.13.3.238. [DOI] [PubMed] [Google Scholar]
- 33.Ezeabogu I, Copenhaver MM, Potrepka J. The influence of neurocognitive impairment on HIV treatment outcomes among drug-involved people living with HIV/AIDS. AIDS Care. 2012;24(3):386–393. doi: 10.1080/09540121.2011.608794. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Rongkavilit C, Naar-King S, Kaljee LM, Panthong A, Koken JA, Bunupuradah T, Parsons JT. Applying the Information-Motivation-Behavioral Skills Model in Medication Adherence Among Thai Youth Living with HIV: A Qualitative Study. AIDS Patient Care and STDs. 2010;24(12):787–794. doi: 10.1089/apc.2010.0069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Mayberry LS, Osborn CY. Empirical validation of the information-motivation-behavioral skills model of diabetes medication adherence: a framework for intervention. Diabetes care. 2014;37(5):1246–1253. doi: 10.2337/dc13-1828. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Chang SJ, Choi S, Kim S-A, Song M. Intervention Strategies Based on Information-Motivation-Behavioral Skills Model for Health Behavior Change: A Systematic Review. Asian Nursing Research. 2014;8(3):172–181. [Google Scholar]
- 37.Huedo-Medina TB, Shrestha R, Copenhaver M. Modeling a Theory-Based Approach to Examine the Influence of Neurocognitive Impairment on HIV Risk Reduction Behaviors Among Drug Users in Treatment. AIDS and Behavior. 2016;20(8):1646–1657. doi: 10.1007/s10461-016-1394-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Shrestha R, Huedo-Medina T, Krishnan A, Altice F, Copenhaver M. Examining the Acceptability of mHealth Technology in HIV Prevention among High-risk Drug Users in Treatment. AIDS and Behavior. 2016 doi: 10.1007/s10461-016-1637-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Copenhaver MM, Lee IC, Baldwin P. A randomized controlled trial of the community-friendly health recovery program (CHRP) among high-risk drug users in treatment. AIDS and Behavior. 2013;17(9):2902–2913. doi: 10.1007/s10461-013-0539-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Ward J, Darke S, Hall W. The HIV risk-taking behaviour scale (HRBS) manual. National Drug and Alcohol Research Centre, University of New South Wales Sydney; 1990. [Google Scholar]
- 41.Shrestha R, Huedo-Medina T, Altice F, Karki P, Copenhaver M. Correlates of willingness to use Pre-Exposure Prophylaxis (PrEP) and the likelihood of practicing safer drug- and sex-related risk behaviors while on PrEP among high-risk drug users in treatment. Drug & Alcohol Dependence. 2016 doi: 10.1016/j.drugalcdep.2016.12.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Schafer JL, Graham JW. Missing data: our view of the state of the art. Psychological methods. 2002;7(2):147–177. [PubMed] [Google Scholar]
- 43.Muthén BO, Muthén LK. Mplus User’s Guide. Seventh. Los Angeles, CA: Muthén & Muthén; 2012. [Google Scholar]
- 44.Arbuckle JL, Marcoulides GA, Schumacker RE. Full information estimation in the presence of incomplete data. Advanced structural equation modeling: Issues and techniques. 1996;243:277. [Google Scholar]
- 45.Barrett P. Structural equation modelling: Adjudging model fit. Personality and Individual differences. 2007;42(5):815–824. [Google Scholar]
- 46.Bentler PM. Comparative fit indexes in structural models. Psychol Bull. 1990;107(2):238–246. doi: 10.1037/0033-2909.107.2.238. [DOI] [PubMed] [Google Scholar]
- 47.Tucker L, Lewis C. A reliability coefficient for maximum likelihood factor analysis. Psychometrika. 1973;38(1):1–10. [Google Scholar]
- 48.Steiger JH. Structural Model Evaluation and Modification: An Interval Estimation Approach. Multivariate Behavioral Research. 1990;25(2):173–180. doi: 10.1207/s15327906mbr2502_4. [DOI] [PubMed] [Google Scholar]
- 49.Byrne BM. Structural equation modeling with LISREL, PRELIS, and SIMPLIS: Basic concepts, applications, and programming. Psychology Press; 2013. [Google Scholar]
- 50.Diamantopoulos A, Siguaw JA, Siguaw JA. Introducing LISREL: A guide for the uninitiated. Sage; 2000. [Google Scholar]
- 51.Santillán Torres Torija C, Villagrán Vázquez G, Robles Montijo SS, Eguiluz Romo LdL. The Information and Motivation and Behavioral Skills Model of ART Adherence among HIV-Positive Adults in Mexico. Journal of the International Association of Providers of AIDS Care (JIAPAC) 2015;14(4):335–342. doi: 10.1177/2325957415581903. [DOI] [PubMed] [Google Scholar]
- 52.Starace F, Massa A, Amico KR, Fisher JD. Adherence to antiretroviral therapy: an empirical test of the information-motivation-behavioral skills model. Health Psychol. 2006;25(2):153–162. doi: 10.1037/0278-6133.25.2.153. [DOI] [PubMed] [Google Scholar]
- 53.Amico KR, Barta W, Konkle-Parker DJ, Fisher JD, Cornman DH, Shuper PA, Fisher WA. The Information–Motivation–Behavioral Skills Model of ART Adherence in a Deep South HIV+ Clinic Sample. AIDS and behavior. 2009;13(1):66–75. doi: 10.1007/s10461-007-9311-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Osborn CY, Egede LE. Validation of an Information-Motivation-Behavioral Skills model of diabetes self-care (IMB-DSC) Patient education and counseling. 2010;79(1):49–54. doi: 10.1016/j.pec.2009.07.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Zhu C, Cai Y, Ma J, Li N, Zhu J, He Y, Redmon P, Qiao Y. Predictors of intention to smoke among junior high school students in Shanghai, China: an empirical test of the information-motivation-behavioral skills (IMB) model. PLoS One. 2013;8(11):e80482. doi: 10.1371/journal.pone.0080482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Zhao Y-W, Wu J-Y, Wang H, Li N-N, Bian C, Xu S-M, Li P, Lu H, Xu L. A Cross-sectional Study Assessing Predictors of Essential Medicines Prescribing Behavior Based on Information-motivation-behavioral Skills Model among County Hospitals in Anhui, China. Chinese Medical Journal. 2015;128(21):2887–2895. doi: 10.4103/0366-6999.168046. [DOI] [PMC free article] [PubMed] [Google Scholar]