Abstract
Objective
To assess the anatomical variations of the pronator teres muscle (PTM) and its implication in the compression of the median nerve, which passes through the humeral and ulnar heads of the PTM.
Methods
For the present study, 100 upper limbs from human cadavers from the anatomy laboratory were dissected. Forty-six specimens were male and four, female, whose aged ranged from 28 to 77 years; 27 were white and 23, non-white. A pilot study consisting of six hands from three fresh cadaver dissections was conducted to familiarize the authors with the local anatomy; these were not included in the present study.
Results
The humeral and ulnar heads of PTM were present in 86 limbs. In 72 out of the 86 limbs, the median nerve was positioned between the two heads of the PTM; in 11, it passed through the muscle belly of ulnar head of the PTM, and in three, posteriorly to both heads of the PTM. When both heads were present, the median nerve was not observed as passing through the muscle belly of the humeral head of PTM. In 14 out of the 100 dissected limbs, the ulnar head of the PTM was not observed; in this situation, the median nerve was positioned posteriorly to the humeral head in 11 limbs, and passed through the humeral head in three. In 17 limbs, the ulnar head of PTM was little developed, with a fibrous band originating from the ulnar coronoid process, associated with a distal muscle component near the union with the humeral head. In four limbs, the ulnar head of the MPR was represented by a fibrous band. In both limbs of one cadaver, a fibrous band was observed between the supinator muscle and the humeral head of the PTM, passing over median nerve.
Conclusion
The results suggest that these anatomical variations in relationship median nerve and PTM are potential factors for median nerve compression, as they narrow the space through which the median nerve passes.
Keywords: Pronation, Median nerve, Nerve compression syndromes
Resumo
Objetivo
Analisar as variações anatômicas do músculo pronador redondo (MPR) e suas implicações na compressão do nervo mediano, que passa entre as cabeças umeral e ulnar do MPR.
Método
Foram dissecados 100 membros superiores de cadáveres adultos pertencentes ao laboratório de anatomia; 46 cadáveres eram do sexo masculino e quatro do feminino. A idade variou entre 28 e 77 anos; 27 eram da etnia branca e 23, não branca. Um estudo piloto que incluiu três cadáveres frescos foi feito, para familiarização dos autores com a anatomia regional. Esses não foram incluídos no estudo.
Resultados
Em 86 membros, observou-se a presença das cabeças umeral e ulnar do MPR. Em 72 dos 86 membros, o nervo mediano estava posicionado entre as cabeças umeral e ulnar do MPR; em 11, esse encontrava-se através da massa muscular da cabeça ulnar do MPR e em três, o nervo mediano estava posicionado posteriormente às duas cabeças do MPR. Nos casos em que as duas cabeças do músculo estavam presentes, não se observou o nervo mediano passando através da massa muscular da cabeça umeral do MPR. Em 14 dos 100 membros dissecados, a cabeça ulnar do MPR não estava presente. Nessa situação, o nervo mediano posicionava-se posteriormente à cabeça umeral em 11 membros e através da cabeça umeral em três membros. Em 17 membros, a cabeça ulnar estava muito pouco desenvolvida, com conformação fibrosa em sua origem no processo coronoide da ulna, associada a um componente muscular distal, próximo a sua união com a cabeça umeral. Em quatro membros, a cabeça ulnar do MPR estava representada apenas por uma banda fibrosa. Nos dois membros de um cadáver, observou-se uma expansão fibrosa que saía do músculo supinador para a cabeça umeral do MPR, passando como uma cinta sobre o nervo mediano.
Conclusões
Esses resultados sugerem que as variações anatômicas na relação nervo mediano e MPR representam fatores potenciais para compressão nervosa, por estreitar o espaço no qual passa o nervo mediano.
Palavras-chave: Pronação, Nervo mediano, Síndromes de compressão nervosa
Introduction
There are several anatomical structures that can compress the median nerve near the elbow joint. From proximal to distal, the compression may be caused by the Struthers’ ligament1, 2 with or without the supracondylar process of the humerus, by aponeurotic expansion of the biceps brachii muscle (Lacertus fibrosus),3, 4 between the humeral and ulnar heads of the pronator teres muscle (PTM),5, 6 by the vascular network of the region,7 and by the arch formed by the two insertions of the superficial flexor muscle of the fingers.8
Regardless of these sites where compression occurs, this condition is termed pronator teres syndrome, because the compression occurs most frequently between the two heads of this muscle.9, 10, 11 The main causes are the anatomic variations of the PTM. The normal anatomical pattern described by the classical anatomy studies12, 13, 14 is that the PTM is constituted by two heads. The humeral head, more extensive, originates in the supracondylar process of the humerus and adjacencies. The ulnar head originates in the coronoid process of the ulna. The two portions unite for insertion into the diaphysis of the radius, contouring to it. The median nerve is positioned between the two heads of the PTM. However, the relationship between the median nerve and the humeral and ulnar heads of the PTM is subject to numerous variations.4, 6, 15, 16 This study aimed to analyze, through anatomical dissections, the relationship between the PTM and median nerve and thus contribute to a better understanding of the causes of the pronator teres syndrome.
Material and methods
One hundred upper limbs of 50 adult cadavers from the anatomy department of this institution were dissected for this study, 46 cadavers were male and four were female. The age ranged from 28 to 77 years; 27 were white and 23, non-white. Cadavers whose forearms were deformed by traumas, malformations, and scars were excluded. A pilot study that included three fresh cadavers was conducted so that the authors could familiarize themselves with the local anatomy. These were not included in this study.
The dissection was performed through a medial incision across the forearm and lower third of the arm. The skin and the subcutaneous tissue were folded to the radial and ulnar sides, respectively. The median nerve was identified in the medial margin of the biceps brachii muscle, approximately 10 cm proximal to the intercondylar line of the humerus; at this location, it was positioned medially in relation to the brachial artery. The dissection proceeded distally until reaching the bicipital aponeurosis, which was sectioned, allowing the visualization of the proximal margin of the PTM. The presence of variations in the surface head and fibrous bands at the site was recorded. Subsequently, the superficial head of the PTM was sectioned transversely to allow the visualization of the deep head, whose presentation was varied; it was absent in 14 of the 100 dissected limbs. The median nerve was distally dissected until it passed through the arch formed by the proximal insertions of the flexor digitorum superficialis muscles. In all dissected limbs, the first branch of the median nerve in the forearm was always towards the superficial head of the PTM. All forearm muscles were dissected; their innervation, the presence of communication among the forearm nerves (Martin-Gruber anastomosis), the relationship between the median nerve and the bicipital aponeurosis, and the relationship of the median and anterior interosseous nerves with the arch of origin of the three heads of the flexor digitorum superficialis muscle were analyzed. The anatomical variations were annotated and photographed. A Keller 2.5 X magnifying glass was used for magnification. This study was approved by the hospital's ethics committee under the CAAE No. 1.356.351.
Results
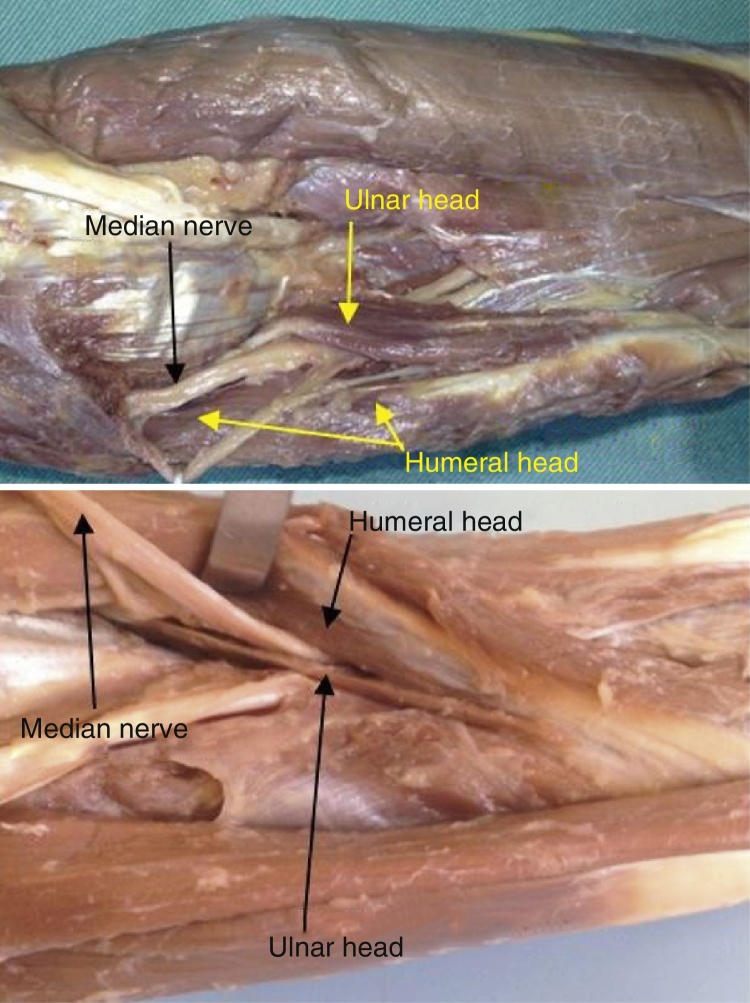
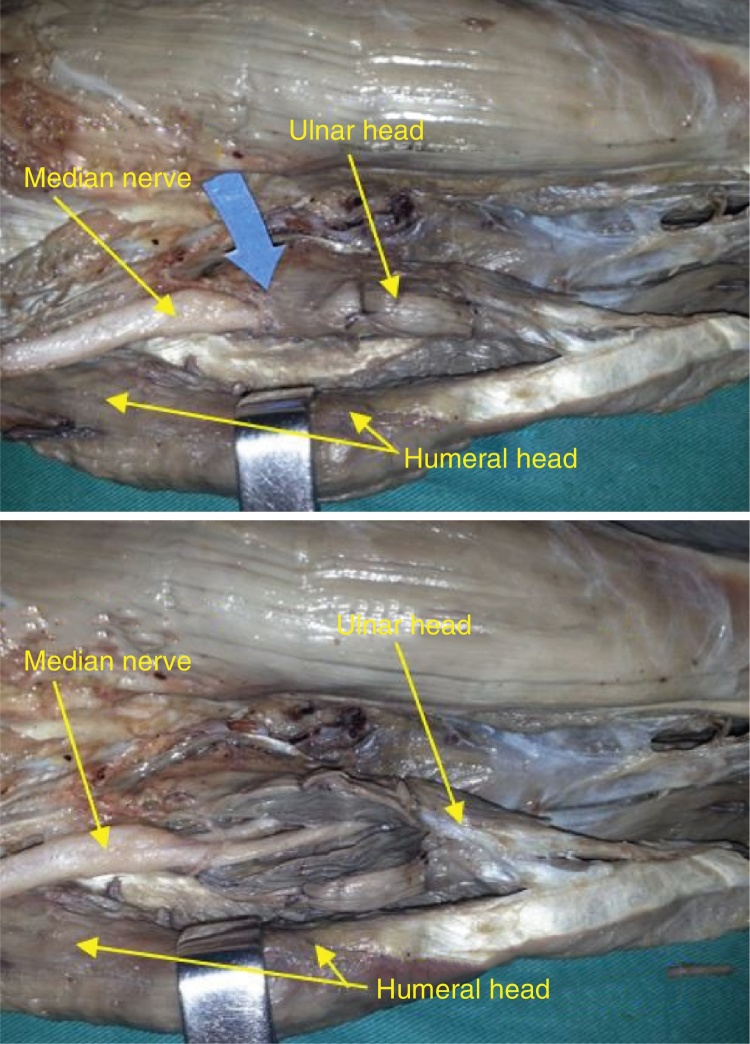
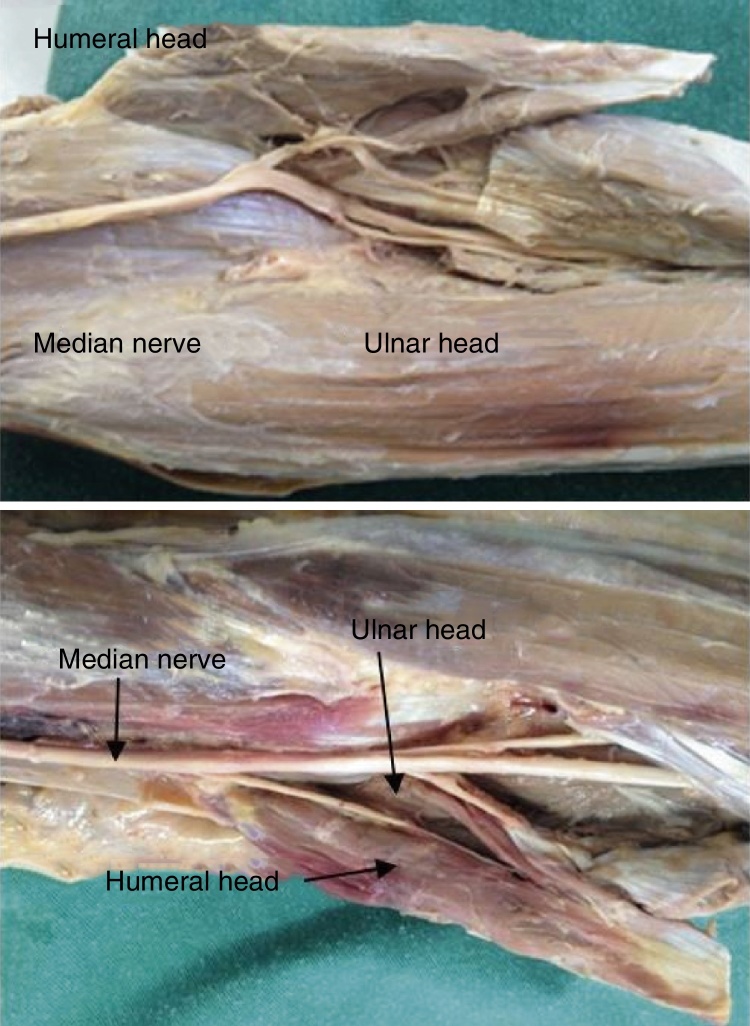
In 86 dissected limbs, the humeral and ulnar heads of the PTM were well individualized, consisting of two distinct muscular portions that joined to insert through an enlarged tendon, contouring to and inserting in the middle third of the diaphysis of the radius (Fig. 1). In 72 of the 86 limbs, the median nerve was positioned between the humeral and ulnar heads of the PTM (Fig. 1). In 11 limbs (four bilaterally), it was positioned through the muscular mass of the ulnar head of the PTM (Fig. 2). In three forearms (one bilaterally), the median nerve was positioned posteriorly to the two heads of the PTM (Fig. 3). When both heads of the muscle were present, no cases of the median nerve passing through the muscle mass of the humeral head of the PTM were observed. In 14 of the 100 limbs, the ulnar head of the PTM was absent. In this situation, the median nerve was positioned posteriorly to the humeral head in 11 limbs (Fig. 4) and through the humeral head in three limbs (Fig. 5).
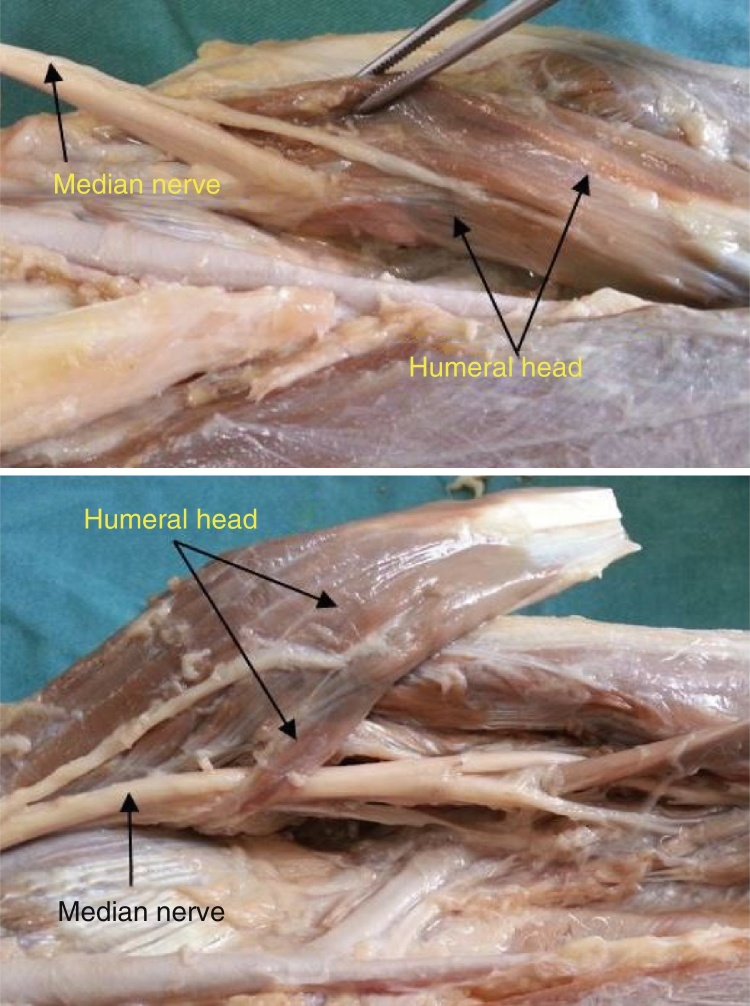
Fig. 1.
In 86 limbs, the humeral and ulnar heads of the PR muscle were well individualized.
Fig. 2.
In nine limbs (three bilaterally), the median nerve crossed the muscle mass of the ulnar head of the PTM.
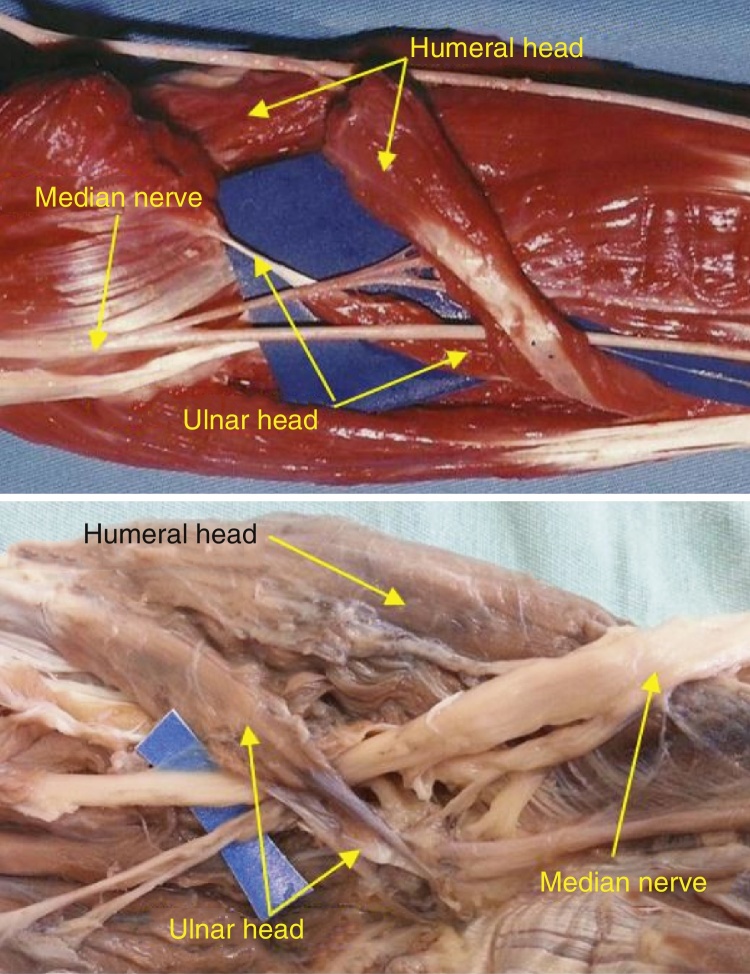
Fig. 3.
In three forearms (one bilaterally), the median nerve was positioned posteriorly to the two heads of the PTM.
Fig. 4.
Absence of the ulnar head of the PTM. In this situation, the median nerve was positioned posteriorly to the humeral head in 11 limbs.
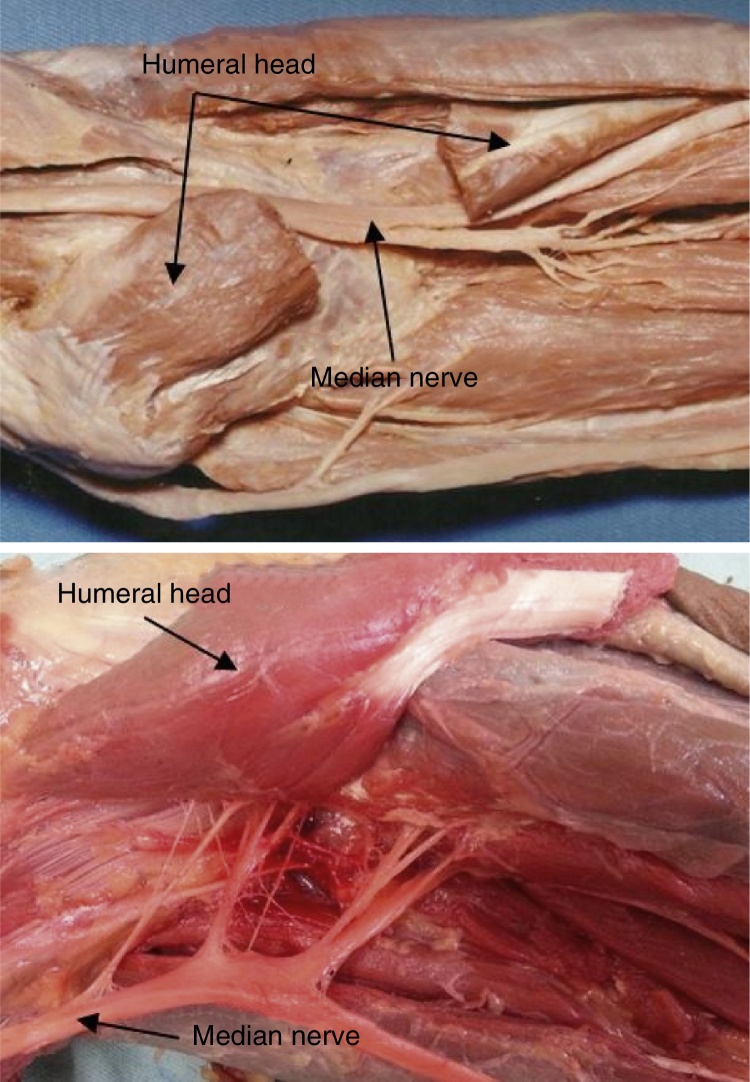
Fig. 5.
Absence of the ulnar head of the PTM. In this situation, the median nerve passed through the humeral head in three limbs.
The humeral head was larger than the ulnar head (Fig. 1). A poorly developed ulnar head was observed in 17 limbs, with a fibrous conformation in its origin in the coronoid process of the ulna, associated with a distal muscular component, close to its union with the humeral head (Fig. 6). The ulnar head of the PTM was represented by a fibrous band not associated with a muscular component in only four limbs (Fig. 7A). On both limbs of a single corpse, a fibrous expansion extending from the supinator muscle to the humeral head of the PTM, passing as a band over the median nerve, was observed (Fig. 7B). In five limbs, the ulnar head was inserted alongside the Gantzer muscle, in the coronoid process of the ulna. In eight limbs, a high insertion of the humeral head PTM ranging from 2.8 to 3.5 cm proximal to the medial epicondyle was observed (Fig. 7A and B; Table 1).
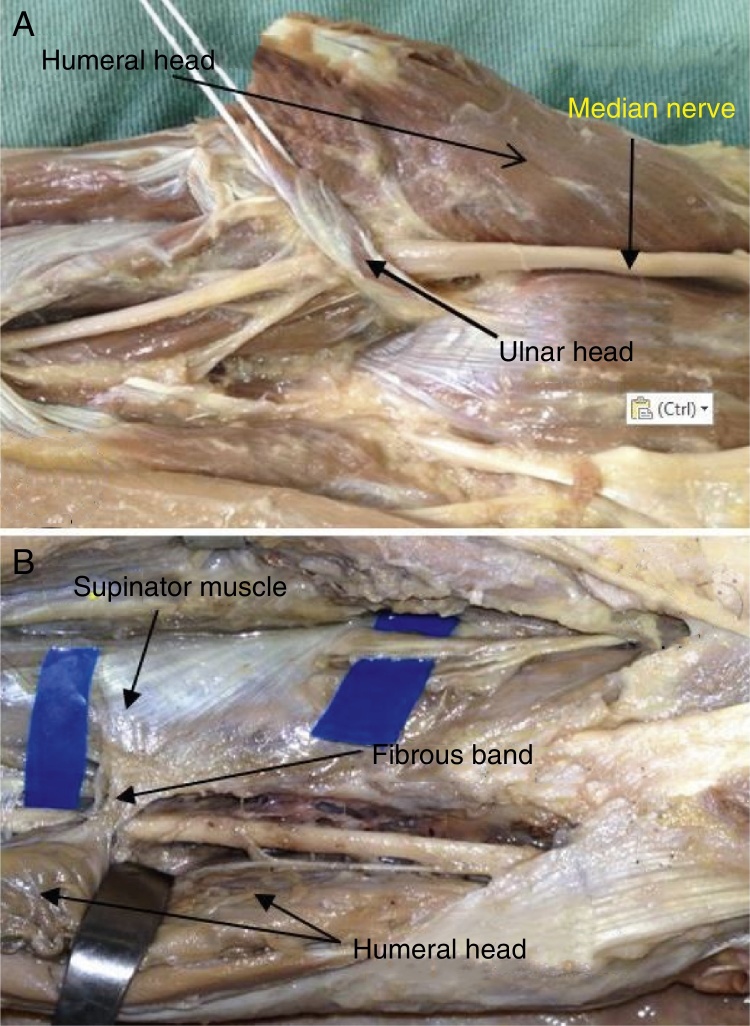
Fig. 6.
In 11 limbs, a poorly developed ulnar head was observed, with a fibrous conformation in its origin in the coronoid process of the ulna, associated with a distal muscular component, close to its union with the humeral head.
Fig. 7.
(A) In four limbs, the ulnar head of the PTM was represented by a fibrous band not associated with a muscle component; (B) in two limbs, a fibrous expansion extended from the supinator muscle to the humeral head of the PTM, passing as a band over the median nerve.
Table 1.
Evaluation of the humeral and ulnar heads of PTM and their relationships with the median nerve in 100 dissected limbs.
| Pronator teres | Location of the median nerve | Percentage | % Total |
|---|---|---|---|
| Humeral and ulnar heads present | Between the two heads of the PTM | 72 | 86 |
| Posteriorly to the two heads of the PTM | 3 | ||
| Through the ulnar head of the PTM | 11 | ||
| Through the humeral head of the PTM | 0 | ||
| Absent ulnar head | Through the humeral head of the PTM | 3 | 14 |
| Posteriorly to the humeral head of the PTM | 11 | ||
| Absent humeral head | Not recorded | 0 | 0 |
| Total | 100 | 100 | |
Discussion
In 86 of the 100 dissected limbs (86%), the humeral and ulnar heads of the PTM were present, which is in agreement with the results reported by Stabille et al.6 (83.5%), Jamieson and Anson15 (81%), and Hollinshead17 (91%). Other authors observed different percentages: Hofer and Hofer,18 56%, and Nebot-Cegarra et al.,19 68%. In 74 of these 86 limbs, the median nerve was positioned between the humeral and ulnar heads of the PTM; in 11, the median nerve passed through the musculature of the ulnar head of the PTM. In three limbs, the median nerve was positioned posteriorly to both PTM heads. In cases in which both heads of the PTM were present, no cases of the median nerve passing through the muscular mass of the humeral head of the PTM were observed.
The PTM ulnar head was absent in 14% of the dissected limbs. In the study by Stabille et al.,6 it was observed in 15%; in that by Hollinshead,17 in 9%, and in that by Nebot-Cegarra et al.,19 in 21.7%. Kaplan20 and Zancolli21 reported that the absence of the ulnar head is frequent. Testut and Latarjet12 and Chiarugi14 also observed this absence, but did not record how often this anatomical variation may occur.
Testut and Latarjet12 and Le Double and Anatole22 described that a tendon segment may replace the ulnar head of the PTM; Spinner23 considers that this variation occurs frequently. Stabille et al.6 observed the ulnar head represented by a fibrous band in 9% of the cases. In the present study, 17 limbs had a poorly developed ulnar head, with a fibrous component in its proximal portion in the coronoid process of the ulna, but associated with a muscular component in the distal portion, before joining the humeral head. In only four limbs, the ulnar head of the PTM was represented by a fibrous band, not associated with a muscular component. In agreement with all the studies analyzed, no cases of absent humeral head of the PTM were observed.
Testut and Latarjet12 and Le Double and Anatole22 also described that the humeral and ulnar head of the PTM may be completely separate, with distal insertions at different sites. In the present study, in agreement with Stabille et al.,6 in the 86 limbs in which both heads were present, these were united before their insertion into the middle-third of the radial diaphysis.
Barret,24 in 200 dissected cases, observed in one of them an additional portion of the humeral head, terming it the third head of the PTM. He also reported that Buchanan had observed a third head of the PTM, which originated from the supracondylar process of the humerus. Caetano et al.2 published a case in which there was median nerve compression caused by the insertion of the humeral head of the PTM in supracondylar humeral process. In the present study, the insertion of the humeral head (2.8–3.5 cm) proximal to the medial epicondyle of the humerus was observed in eight cases.
The positioning of the median nerve posteriorly to both heads of the PTM, described by Jamieson and Anson15 in 6% of limbs and by Di Dio and Dangelo16 in 2.5%, was observed in three forearms (3%) in the present study.
The present results are in agreement with those by Stabille et al.6 and Gessini et al.25 The most frequent anatomical variation was the absence of the ulnar head of the PTM. The authors are in agreement with the conclusion of these two studies that anatomical variations and the presence of fibrous bands between the two heads of the PTM can result in narrowing of the space through which the median nerve passes, thus causing nerve compression and the motor and sensory symptoms observed in pronator teres syndrome. The authors are also in agreement with Spinner23 and Stabille et al.,6 who stipulated that the proximal fibrous component that is part of the coronoid process of the ulna may be responsible for nerve compression. In the present study, the median nerve passed through the muscular mass of the ulnar head of the PTM in 11 limbs (three bilaterally; Fig. 2). The nerve passed through the humeral head in three limbs (in the absence of the ulnar head), but this was not observed when both muscle heads were present; Stabille et al.6 observed this situation in 2% of their cases, and Tulwa et al.,26 in one case in which the median nerve was positioned medially near the medial epicondyle. In the present study, in limbs in which the median nerve passed through the muscles of the ulnar head of the PTM, the authors had the same observation as Stabille et al.6: that this is a very narrow space, thus more subject to nerve compression.
Surgeons should be aware of the anatomical variations that can be observed in the elbow region, as they change the position of the noble structures, putting them at risk during arthroscopic procedures and open surgical approaches in the region.
Conclusion
The anatomical variations of the humeral and ulnar heads of the PTM in relation to their constitution and frequency can alter the positioning of the median nerve. The most frequently observed variation was absence of the ulnar head. In the presence of fibrous bands, especially when the median nerve extends close to the coronoid process of the ulna where the ulnar head of the PTM has a fibrous constitution, nerve compression can occur due to a narrowing of the nerve passage space. It is clear that the passage of the nerve through the muscle mass of the PTM is not only a place with greater potential to cause pronator teres syndrome, but also alters the normal course of the median nerve.
Conflicts of interest
The authors declare no conflicts of interest.
Footnotes
Study conducted at the Pontifícia Universidade Católica de São Paulo, Faculdade de Ciências Médicas e da Saúde, Disciplinade Ortopedia e Traumatologia, Sorocaba, SP, Brazil.
References
- 1.Sener E., Takka S., Cila E. Supracondylar process syndrome. Arch Orthop Trauma Surg. 1998;117(6–7):418–419. doi: 10.1007/s004020050284. [DOI] [PubMed] [Google Scholar]
- 2.Caetano E.B., Brandi S., Lee H.J. Compressão do nervo mediano por processo supracondilar do úmero. Rev Bras Ortop. 1989;24(9):323–326. [Google Scholar]
- 3.Spinner R.J., Carmichael S.W., Spinner M. Partial median nerve entrapment in the distal arm because of an accessory bicipital aponeurosis. J Hand Surg. 1991;16(2):236–244. doi: 10.1016/s0363-5023(10)80103-0. [DOI] [PubMed] [Google Scholar]
- 4.Seitz W.H., Jr., Matsuoka H., McAdoo J., Sherman G., Stickney D.P. Acute compression of the median nerve at the elbow by the Lacertus fibrosus. J Shoulder Elbow Surg. 2007;16(1):91–94. doi: 10.1016/j.jse.2006.04.005. [DOI] [PubMed] [Google Scholar]
- 5.Hartz C.R., Linscheid R.L., Gramse R.R., Daube J.R. The pronator teres syndrome: compressive neuropathy of the median nerve. J Bone Joint Surg Am. 1981;63(6):885–890. [PubMed] [Google Scholar]
- 6.Stabille S.R., Duarte E., Carvalho V.C. Pronator teres muscle: anatomical variations and predisposition for the compression of the median nerve. Acta Sci Biol Sci. 2008;24:631–637. [Google Scholar]
- 7.Pires P.R., Andrade R.P. Síndromes compressivas no membro superior. In: Pardini A., Freitas A., editors. Cirurgia da mão: lesões não traumáticas. 2ª ed. Medbook; Rio de Janeiro: 2008. pp. 263–297. [Google Scholar]
- 8.Dellon A.L., Mackinnon S.E. Musculoaponeurotic variations along the course of the median nerve in the proximal forearm. J Hand Surg Edinb Scotl. 1987;12(3):359–363. doi: 10.1016/0266-7681_87_90189-6. [DOI] [PubMed] [Google Scholar]
- 9.Johnson R.K., Spinner M., Shrewsbury M.M. Median nerve entrapment syndrome in the proximal forearm. J Hand Surg. 1979;4(1):48–51. doi: 10.1016/s0363-5023(79)80104-5. [DOI] [PubMed] [Google Scholar]
- 10.Eversmann W.W. Proximal median nerve compression. Hand Clin. 1992;8(2):307–315. [PubMed] [Google Scholar]
- 11.Bayerl W., Fischer K. The pronator teres syndrome. Clinical aspects, pathogenesis, and therapy of a non-traumatic median nerve compression syndrome in the space of the elbow joint. Handchirurgie. 1979;11(2):91–98. [PubMed] [Google Scholar]
- 12.Testut L., Latarjet A. Salvat; Barcelona: 1947. Tratado de anatomia humana. [Google Scholar]
- 13.Tandler J. 2ª ed. Salvat; Barcelona: 1928. Tratado de anatomia sistematica. [Google Scholar]
- 14.Chiarugi G. 7a ed. Sovete; Milano: 1949. Istituzioni di anatomia dell’uomo. [Google Scholar]
- 15.Jamieson R.W., Anson B.J. The relation of the median nerve to the heads of origin of the pronator teres muscle, a study of 300 specimens. Q Bull Northwest Univ Med Sch. 1952;26(1):34–35. [PMC free article] [PubMed] [Google Scholar]
- 16.Di Dio J.A., Dangelo J.G. Nervus medianus piercing the caput humerale of the m. pronator teres. Anat Anz. 1963;112:385–388. [PubMed] [Google Scholar]
- 17.Hollinshead W.H. Hoeber Harper; New York: 1958. Anatomy for surgeons. [Google Scholar]
- 18.Hofer K., Hofer G. Ueberden Verlauf der arteria brachialis mit dem nervus medianus zwischen den beiden kopfen des musculus pronator teres. Anat Anzeles. 1910;36:510. [Google Scholar]
- 19.Nebot-Cegarra J., Perez-Berruezo J., Reina de la Torre F. Variations of the pronator teres muscle: predispositional role to median nerve entrapment. Arch Anat Histol Embryol. 1991–1992;74:35–45. [PubMed] [Google Scholar]
- 20.Kaplan E.B. Artecnica; Buenos Aires: 1961. Anatomia functional y quirurgica de la mano. [Google Scholar]
- 21.Zancolli E. 2nd ed. Lippincott; Philadelphia: 1979. Structural and dynamic bases of hand surgery. [Google Scholar]
- 22.Le Double A.F., Anatole F. Schleicher Frères; Paris: 1897. Traité des variations du système musculaire de l’homme et de leur signification au point de vue de l’anthropologie zoologique. [Google Scholar]
- 23.Spinner M. 2nd ed. WB Saunders; Philadelphia: 1978. Injuries to the major branches of peripheral nerves of the forearm. [Google Scholar]
- 24.Barrett J.H. An additional (third and separate) head of the pronator teres muscle. J Anat. 1936;70(Pt 4):577–578. [PMC free article] [PubMed] [Google Scholar]
- 25.Gessini L., Jandolo B., Pietrangeli A. Entrapment neuropathies of the median nerve at and above the elbow. Surg Neurol. 1983;19(2):112–116. doi: 10.1016/0090-3019(83)90405-6. [DOI] [PubMed] [Google Scholar]
- 26.Tulwa N., Limb D., Brown R.F. Median nerve compression within the humeral head of pronator teres. J Hand Surg Br Eur. 1994;19(6):709–710. doi: 10.1016/0266-7681(94)90241-0. [DOI] [PubMed] [Google Scholar]