Abstract
Background
Although 3D motion capture is considered the “gold standard” for recording and analyzing kinematics, 2D video analysis may be a more reasonable, inexpensive, and portable option for kinematic assessment during pre-participation screenings. Few studies have compared quantitative measurements of lower extremity functional tasks between 2D and 3D.
Purpose
To compare kinematic measurements of the trunk and lower extremity in the frontal and sagittal planes between 2D video camera and 3D motion capture analyses obtained concurrently during a SLS.
Study Design
Descriptive laboratory study.
Methods
Twenty-six healthy, recreationally active adults volunteered to participate. Participants performed three trials of the single leg squat on each limb, which were recorded simultaneously by three 2D video cameras and a 3D motion capture system. Dependent variables analyzed were joint displacement at the trunk, hip, knee, and ankle in the frontal and sagittal planes during the task compared to single leg quiet standing.
Results
Dependent variables exhibited moderate to strong correlations between the two measures in the sagittal plane (r = 0.51–.093), and a poor correlation at the knee in the frontal plane (r = 0.308) at (p ≤ 0.05) All other dependent variables revealed non-significant results between the two measures. Bland-Altman plots revealed strong agreement in the average mean difference in the amount of joint displacement between 2D and 3D in the sagittal plane (trunk = 1.68 º, hip = 2.60 º, knee = 0.74 º, and ankle = 3.12 º). Agreement in the frontal plane was good (trunk = 7.92 °, hip = -8.72 º, knee = -6.62 º, and ankle = 3.03 °).
Conclusion
Moderate to strong relationships were observed between 2D video camera and 3D motion capture analyses at all joints in the sagittal plane, and the average mean difference was comparable to the standard error of measure with goniometry. The results suggest that despite the lack of precision and ability to capture rotations, 2D measurements may provide a pragmatic method of evaluating sagittal plane joint displacement for assessing gross movement displacement and therein risk of lower extremity injury.
Level of Evidence
3
Keywords: Movement pattern, sagittal plane, screening, single leg squat
INTRODUCTION
Many athletic movement patterns, including decelerating, cutting, pivoting, and landing from a jump, have been linked to an increased risk of lower extremity injury.1–4 Dynamic knee valgus (DKV) is often described in the literature as a biomechanical risk factor for lower extremity injury, and it has been reported to prospectively contribute to anterior cruciate ligament (ACL) injury as well as to the development of patellofemoral pain (PFP).5–7 Furthermore, deficits in dynamic stability of the trunk8 and lower extremity asymmetries7,9 have been purported as mechanisms that initiate this faulty position and contribute to injury risk.
Functional assessments such as the Functional Movement Screen™,10 Selective Functional Movement Assessment,10 Star Excursion Balance Test,11 and the Landing Error Scoring System12 all have the ability to identify discrepancies in movement quality. Common clinical limitations among these assessments are the lack of measurable kinematic output, the training required for testing, and the time involved with test administration. While some observational screenings have been shown to be valid and reliable,12–14 others have exhibited poor reliability,15 and inadequate sensitivity.16 Previous literature has identified that rater experience,15 perception,17 and visual acuity17 may play a significant role in the standardization of observational screenings. The ability to easily identify quantifiable kinematic risk factors for lower extremity injury may allow sports medicine professionals to intervene more effectively and enable them to educate athletes about sport-specific, at-risk positions. The single leg squat (SLS) has been used as a qualitative measure to evaluate lower extremity injury risk.18,19 While this task is simple, and can identify unilateral dysfunction,20 kinematic evaluation is not commonly included in the SLS assessment.
Laboratory-based 3-Dimensional (3D) motion capture systems are considered the “gold standard” in the evaluation of biomechanical risk factors.21 These systems are reliable22,23 during many functional tasks and can accurately determine multi-planar and dimensional kinematics, including rotational forces across joints. However, 3D motion capture systems have limited application in the clinical setting due to the high-priced equipment and time consuming set-up, application of multiple electromagnetic sensors that do not always relate well to the performance of functional tasks, and difficulty to incorporate into pre-season screenings. Video screenings are a potential solution to the current limitations (e.g. portability, time and cost effectiveness, and standardization) in the aforementioned clinical movement assessments. Video assessments can take place in a physical therapy clinic or physician's office and results can be readily discussed using phone or tablet applications. Additionally, these 2-dimensional (2D) video systems are portable, time and cost effective, and require little training.21 Since the majority of knee injury risk factors occur in the cardinal planes of movement, it was hypothesized that video analysis in the sagittal and frontal planes would be comparable to the same kinematic measures using 3D motion capture. Currently, limited research has addressed the relationship between 2D and 3D methods of kinematic analysis during functional tasks. Gwynne et al reported moderate to strong correlations between 2D and 3D analyses at the knee in frontal plane during the SLS (r = 0.64–0.78).24 The study, however, did not compare data from the two systems collected during the same session. Similarly, Ayala et al found a strong relationship between 2D and 3D analyses at the knee in the frontal plane during the drop vertical jump (r = 0.82–0.97).25 A limitation of both of these studies was the absence of a sagittal plane evaluation during the functional task. Therefore, the purpose of this study was to compare kinematic measurements of the trunk and lower extremity in the frontal and sagittal planes between 2D video camera and 3D motion capture analyses obtained concurrently during a SLS.
METHODS
This was a descriptive laboratory study with a single session of data collection. The independent variable was observation method at two levels: 2D video camera analysis and 3D motion capture. The dependent variables included joint displacement at the trunk, hip, knee, and ankle in the frontal and sagittal planes. These variables were calculated as the displacement between the kinematic value at quiet standing and the corresponding kinematic value at peak knee flexion, for each joint.
Participants
Twenty-six healthy and recreationally active adults (age: 22.26 ± 2.99 years, height: 1.70 ± 0.12 meters, mass: 67.43 ± 12.24 kilograms) were recruited as a volunteer sample of convenience from a University setting and the surrounding community. An a priori sample size estimate was performed based on previously published data26 exhibiting a correlation coefficient of 0.36 and effect size of 0.60 between 2D and 3D measurements of knee valgus during a side jump task. It was estimated that 26 total subjects would be sufficient to find statistically significant differences at an α level of 0.05, and power (1-β) of 0.80. Participants were excluded from the study if they reported a history of lower extremity surgery, history of lower extremity injury within the last year, or any lower extremity or balance condition that may have affected the participant's ability to complete the task. The study was approved by the University of Virginia's Institutional Review Board and each participant provided written informed consent prior to the start of data collection.
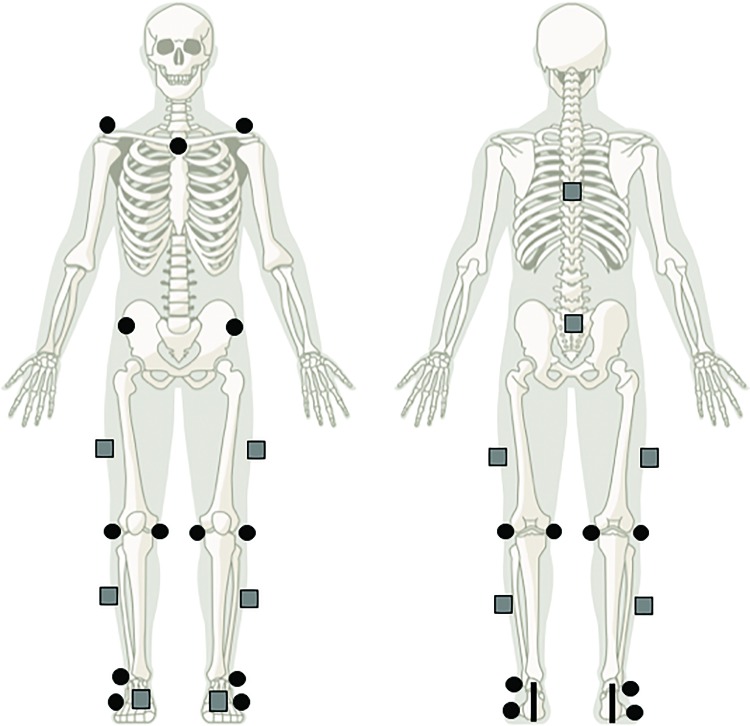
Three-Dimensional Motion Capture
Lower extremity joint kinematics were recorded with the Flock of Birds 6 degrees-of-freedom electromagnetic tracking system (Ascension Technology Inc., Burlington, VT, USA) and integrated with the Motion Monitor Software (version 8.85, Innovative Sports Training, Inc., Chicago, IL, USA). Ten electromagnetic sensors were secured with double-sided adhesive tape and non-adhesive elastic wrap to the subject's skin: one on each calcaneus, one on the dorsal aspect of each foot, one on the middle third of each lateral shank, one on the middle third of each lateral thigh, one over the sacrum, and one at T1 (Figure 1). Height, mass, and joint centers were subsequently calibrated using the stylus. Sensors were secured and digitized by the same clinician for each participant. Kinematic data were collected at a sampling rate of 144 Hz.
Figure 1.
2D retroreflective marker (black circles) and 3D electromagnetic sensor (gray squares) locations.
Two-Dimensional Video Camera
Fifteen anatomical landmarks were identified with retroreflective markers and secured with double-sided adhesive tape to the subject's skin: one at the sternoclavicular notch, one on each acromioclavicular joint, one on each anterior superior iliac spine, one on each medial joint line of the knee, one on each lateral joint line of the knee, one on each medial malleolus, one on each lateral malleolus, and one on each base of the fifth metatarsal (Figure 1). Retroreflective markers were affixed by the same clinician for each participant, with a level of accuracy of less than 8mm. Two-dimensional videos of the SLS were captured using three Canon Vixia HF R42 digital cameras (Canon USA, Inc., Melville, NY, USA). Each camera was placed on a tripod at a height of 1.2 meters from the floor, and at a distance of 2.4 meters from the participant. One camera was placed in the sagittal plane, and two were placed in the frontal plane (one anterior, one posterior). Each camera was leveled using the Bubble Level application (version 2.1, Lemondo Entertainment, www.lemondo.com) on the clinician's smartphone. Two-dimensional data were collected at a sampling rate of 60 frames per second.
Data Collection Procedures
The participants performed three trials of a SLS on each leg (order randomized), for a total of six trials. Participants received verbal standardized instructions on the performance of the SLS maneuver20 from the researcher and were permitted up to three practice trials per leg. Each participant was instructed to look straight ahead, stand on the test limb with the opposite knee flexed to approximately 90°, and fold his or her arms across their chest. They were then asked to squat down as far as comfortably possible without losing balance, and to return to the starting position. Each SLS task was recorded individually, capturing the quiet single leg stance through the self-selected peak knee flexion, and back to the starting position. A trial was discarded if: the participant lost balance during the movement; the clinician determined that the movement was uncontrolled; a reflective marker or sensor fell off; or the trial was interrupted. The participant was permitted as much rest as they felt necessary between repetitions, and after three successful trials the participant repeated the process on the opposite limb.
3D Data Processing
Kinematic data was collected at 144 Hz for the ankle, knee, hip, and trunk during the six total trials of the SLS task for each participant. Lower extremity joint rotations were calculated using the Euler rotation method in the following order: Y (flexion-extension axis) X (abduction-adduction axis), Z (internal-external rotation axis). The hip joint center of rotation was determined using the Bell method.27 Data was filtered using a 4th order low-pass Butterworth filter at 6 Hz. For each trial, one virtual event marker was placed at quiet standing, and one virtual event marker was placed at peak knee flexion. Kinematic values at each joint that corresponded with peak knee flexion were extracted and compared with quiet standing to determine joint displacement.
2D Data Processing
Two-dimensional videos were processed using Kinovea Software (version 0.8.15, Kinovea Open Source Project, www.kinovea.org). For each trial, two still images were created in the frontal and sagittal planes (one at quiet standing, one at peak knee flexion). On each still image, the clinician measured joint angles at the trunk, hip, knee, and ankle using the retroreflective markers, and calculated the joint displacement between quiet standing and peak knee flexion. All angles were measured by the same clinician.
In the sagittal plane, trunk flexion was measured as the angle between a vertical line (perpendicular to the ground) bisecting the sacrum and a line bisecting the thoracic spine.28 Hip flexion was measured as the angle between the AC joint and lateral knee joint with the greater trochanter serving as the fulcrum. Knee flexion was measured as the angle between the greater trochanter and lateral malleolus with lateral knee joint serving as the fulcrum. Ankle dorsiflexion was measured as the angle between a line from the lateral knee joint through the lateral malleolus and a line parallel with the fifth metatarsal.
In the frontal plane, lateral trunk flexion was measured as the angle between a vertical line bisecting the contralateral ASIS (perpendicular to the ground) and a line from the ASIS to the AC joint marker.29 Hip abduction was measured as the angle between a vertical line bisecting the ipsilateral ASIS (perpendicular to the ground) and a line from the ASIS to the point half the distance between the two knee joint markers. Knee abduction was measured as the angle connecting three points: one bisecting the malleoli of the ankle, one bisecting the femoral condyles, and one on the proximal thigh parallel to the ASIS.30 Ankle abduction was measured as the angle between a line bisecting the calcaneus and a line bisecting the distal 1/3 of the lower leg, using a rear foot view.
STATISTICAL ANALYSIS
The mean of the three trials on each limb and for each system were used for statistical analysis. Pearson product moment correlation coefficients were utilized to assess linear relationships between mean 2D and 3D displacement measures at the trunk, hip, knee, and ankle in the frontal and sagittal planes. The strength of the correlation (r) was interpreted as poor (0 to 0.49), moderate (0.50 to 0.75), and strong ( > 0.75).31 Bland-Altman plots with average mean difference (AMD) and 95% limits of agreement (LOA) were used to evaluate agreement between 2D and 3D measurements for each dependent variable. Left and right average mean differences were combined for an overall analysis. The presentation of the LOA allows for the visual judgment of how well the two techniques agree. The smaller the range between the upper and lower limits, the stronger the agreement is. Statistical analyses were performed using SPSS software Version 23.0 (IBM Corporation, Chicago, IL, USA). Bland Altman plots were generated using the Microsoft Excel® software (Version 14.4.0, Microsoft Corporation, Redmond WA, USA). Alpha was set a priori at p ≤ 0.05)
RESULTS
Dependent variables were all significantly correlated between the two measures in the sagittal plane at the trunk (r = 0.53, 95% CI: 0.30–0.70, moderate), hip (r = 0.93, 95% CI: 0.88–0.96, strong), knee (r = 0.86, 95% CI: 0.77–0.92, strong) , and ankle (r = 0.51, 95% CI: 0.28–0.69, moderate), and in the frontal plane at the knee (r = 0.31, 95% CI: 0.04–0.54, poor). Correlations between 2D and 3D analyses were not significant in the frontal plane at the trunk, hip, or ankle (Table 1).
Table 1.
Pearson's correlation coefficients and associated 95% confidence intervals between 2D and 3D analysis. Statistical significance denoted as p ≤ 0.05.
| Plane | Joint | r | 95% CI | p |
|---|---|---|---|---|
| Sagittal | Trunk | 0.53 | 0.30, 0.70 | <.001* |
| Hip | 0.93 | 0.88, 0.96 | <.001* | |
| Knee | 0.86 | 0.77, 0.92 | <.001* | |
| Ankle | 0.51 | 0.28, 0.69 | <.001* | |
| Frontal | Trunk | 0.16 | −0.12, 0.41 | .27 |
| Hip | 0.15 | −0.13, 0.41 | .28 | |
| Knee | 0.31 | 0.04, 0.54 | .03* | |
| Ankle | 0.12 | −0.16, 0.38 | .39 |
Denotes significance at p≤0.005
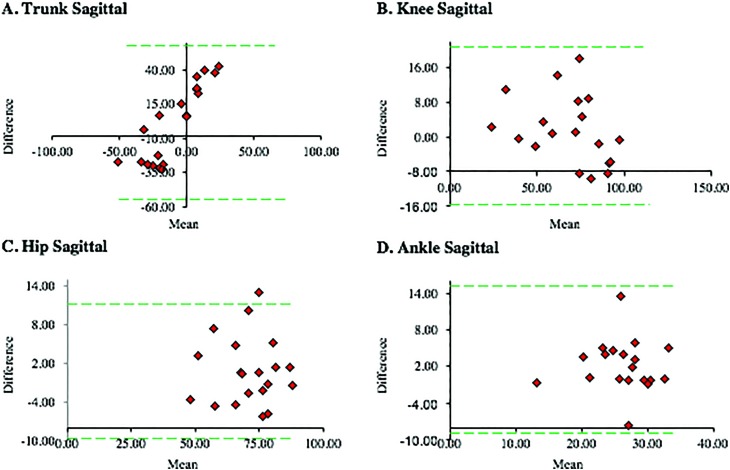
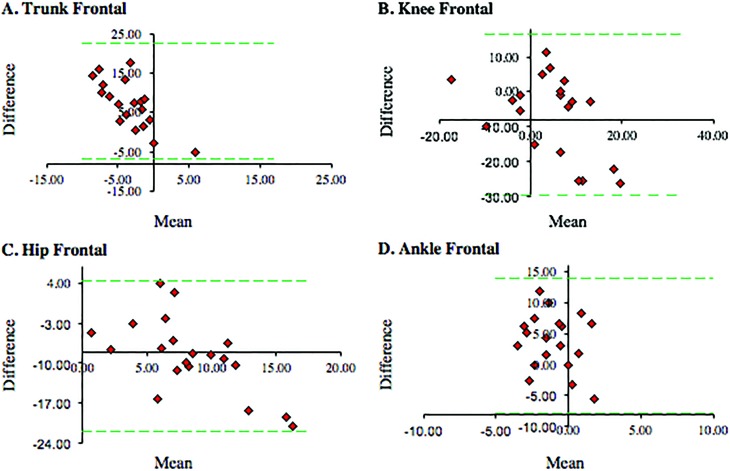
Bland-Altman plots revealed agreement in the AMD between 2D and 3D measurement techniques in the sagittal plane at the trunk (1.68°; LOA −54.45 to 57.81; Figure 2a), hip (2.60°; LOA −15.48 to 20.68; Figure 2b), knee (0.74°; LOA −9.70 to 11.19; Figure 2c), and ankle (3.12°; LOA −8.89 to 15.14; Figure 2d). Agreement in the frontal plane at the trunk (7.92°; LOA −6.65 to 22.50; Figure 3a), hip (-8.72°; LOA −21.90 to 4.45; Figure 3b), knee (-6.62°; LOA −29.83 to 16.59; Figure 3c), and ankle (3.03°; LOA −7.96 to 14.02; Figure 3d) was not as strong. A positive value indicates that the 2D analysis measured larger displacement than 3D analysis, whereas a negative value indicates that the 3D analysis measured larger displacement than the 2D analysis.
Figure 2.
Bland Altman plots comparing 2D and 3D analyses of the SLS in the sagittal plane with 95% limits of agreement (dashed lines). The difference between the 2D and 3D measurement score plotted against the mean of the two measurements for each dependent variable.
Figure 3.
Bland Altman plots comparing 2D and 3D analyses of the SLS in the frontal plane with 95% limits of agreement (dashed lines). The difference between the 20 and 30 measurement score plotted against the mean of the two measurements for each dependent variable.
DISCUSSION
The relationship and agreement between two methods of commonly used biomechanical analyses: 2D video camera and 3D motion capture were evaluated. Utilizing both Pearson's correlation coefficients and Bland Altman plots when comparing two measurement techniques allows for a more robust evaluation of consistency between measures by providing both linear association and agreement. The strongest relationships between the two measurement systems in the sagittal plane were observed at the hip and at the knee. This is consistent with previous literature, where Norris et al evaluated the relationship between a similar 2D measurement technique and goniometry in the sagittal plane during mechanical lifting.32 During this bilateral and foundational task, the researchers were able to observe near perfect reliability at both the hip (r = 0.99, 95% CI: 0.98–0.99) and at the knee (r = 0.98, 95% CI: 0.96–0.99), with a standard error of measurement of 0.75° and 1.4°, respectively. The SLS task that this study utilized requires a greater degree of postural control and proprioception than double-legged foundational tasks, which could could account for this slight decrease in reliability. In support of this theory, Gribble et al evaluated sagittal plane joint angle measurements between a 2D video method and standard goniometry during a SLS. The authors reported a difference of < 4° for the knee and < 11° for the hip, with strong reliability (r = 0.76–0.89).33
While significant relationships between 2D and 3D techniques were observed at all four joints in the sagittal plane, the only significant correlation observed in the frontal plane was at the knee, which was considered poor. Although previous studies have evaluated the reliability between 2D and 3D analyses, the systems are frequently just compared at the knee in the frontal plane. Similar to these findings, the side-step (r = 0.40), and the side-jump (r = 0.32) also exhibited poor reliability between the two techniques when evaluating knee varus/valgus motion.26 In contrast, moderate to strong reliability has been observed during the SLS (r = 0.64–0.78), and drop vertical jump (r = 0.82–0.97).25 A potential explanation for the lack of clinically relevant findings in the frontal plane could be related to the decision to allow participants to self-select their SLS depth. Eltoukhy et al found similar results at the knee in the frontal plane when utilizing a self-selected SLS depth in their comparison between the Kinect camera and 3D motion capture (r = 0.144).34 As a result, this variation could allow individuals to utilize multiple movement strategies to complete the task – in particular the incorporation of transverse plane motion both proximal and distal to the knee at the hip and ankle.
Bland Altman plots allowed for the quantification of the agreement between these two clinical measurement techniques. The AMD between the two measures was less than 4° at each joint in the sagittal plane and less than 7° in the frontal plane. Previous literature reports interrater standard error of measurement of goniometry for the lower extremity ranging between 0.62° and 7.8°.35–39 While the 2D and 3D measurements had stronger agreement in the sagittal plane, it is important to note that both planes of motion exhibited an AMD that is clinically acceptable. Additionally, although there were no patterns in regards to which system consistently measured greater joint angles, and wide LOA were observed (particularly at the trunk). This finding could be the result of transverse plane motion that could not be accounted for in the 2D video assessment.40
It has been suggested that sagittal plane body positions affect lower extremity biomechanics and the risk of knee injuries.41 Landing with the body in a more erect position increases vertical ground reaction forces attenuated through the entire kinetic chain, which is believed to increase both acute and chronic knee injury risk.42,43 At the deepest landing position, hip flexion has been significantly related to knee flexion moment in a drop vertical jump as well as a single leg drop vertical jump.42 Subjects who used less hip flexion in the sagittal plane upon landing relied more heavily on frontal plane knee moments to decelerate their center of mass.42 Similarly, it has been demonstrated that females perform the SLS with less trunk flexion, greater knee abduction, and greater hip adduction when compared to males.40 While it is known that increased moments in the frontal plane lead to a significant increased risk for injury,5 an erect position coupled with the medial collapse at the knee has been suggested as a faulty movement pattern that predisposes an individual to non-contact ACL injury.44 The ability for clinicians to effectively measure sagittal plane kinematics during functional tasks adds a valuable component to functional assessments and risk factor screenings.
Clinical Relevance
Although poor movement quality exhibited during functional tasks may be attributed to deficits in lower extremity neuromuscular control, specific kinematic variables have been highlighted as primary risk factors for knee injury.7,20,21 There is evidence that peak knee flexion is the strongest predictor of SLS performance,20 and that males perform the task with greater knee flexion than females.20,45 While SLS depth was not standardized in this study in an effort to maintain clinical applicability, we may consider this modification in the future if comparing kinematics between sexes. The ability to detect these faulty movements during the SLS task in 2D provides clinicians with a valuable kinematic measurement tool to utilize in screenings and during rehabilitation.
Limitations
It is anticipated that the method of 2D measurement utilized may have contributed to the results of this study. The points utilized to construct the joint angles were each explicitly identified by a retroreflective marker in the sagittal plane, whereas sets of anatomical landmarks were bisected to identify several points in the frontal plane. Although these methods are consistent with the literature,28–30 they could also potentially explain more variation in the identification of the frontal plane angles, as the clinician visually identified several points that comprised the joint angles (i.e. at the knee and at the ankle).
One factor that must be considered is that 2D methods are unable to measure rotation. Rotation of the trunk, hip, and tibia are included in the definition of DKV,46 and contribute to other biomechanical abnormalities that were unable to be analyzed. Previous authors have indicated that frontal plane movements during 2D video analysis may not be a true representation of 3D kinematics, as rotation cannot be measured.30,47 Indeed this presented a problem in this study, as those who had greater discrepancies between the two methods of measurement visually appeared to show more trunk rotation. This finding is supported by previous authors,26,48 who suggest that joint rotations at the hip and knee contribute to the appearance of 2D frontal plane kinematics. Another limitation to this study is that the maximal values for the calculation of joint displacement were taken at peak knee flexion. Recent data has shown that the deepest part of a squat or landing is a comparable position to an athletic task,7,49 however, discrepancies in movement and visible weaknesses may occur throughout the task.
CONCLUSION
The results of this study indicate that 2D video analysis is comparable to 3D motion capture when evaluating sagittal plane joint displacement during a SLS. Clinically, a valid 2D analysis may help health care professionals identify at-risk athletes and apply targeted interventions to these athletes, especially when they do not have access to a 3D motion analysis system, or the financial means to acquire one.29 Future studies should evaluate the use of mobile technology in the quantification of lower extremity kinematics during functional tasks, in an effort to move towards an even more expedient and efficient method of assessment.
REFERENCES
- 1.Boden BP, Dean GS, Feagin JA, Garrett WE. Mechanisms of anterior cruciate ligament injury. Orthopedics. 2000;23(6):573-578. [DOI] [PubMed] [Google Scholar]
- 2.Ford KR, Myer GD, Toms HE, Hewett TE. Gender differences in the kinematics of unanticipated cutting in young athletes. Med Sci Sport Exer. 2005;37(1):124-129. [PubMed] [Google Scholar]
- 3.Besier TF, Lloyd DG, Ackland TR, Cochrane JL. Anticipatory effects on knee joint loading during running and cutting maneuvers. Med Sci Sport Exer. 2001;33(7):1176-1181. [DOI] [PubMed] [Google Scholar]
- 4.Myklebust G, Engebretsen L, Braekken IH, Skjolberg A, Olsen OE, Bahr R. Prevention of anterior cruciate ligament injuries in female team handball players: A prospective intervention study over three seasons. Clin J Sport Med. 2003;13(2):71-78. [DOI] [PubMed] [Google Scholar]
- 5.Myer GD, Ford KR, Di Stasi SL, Foss KDB, Micheli LJ, Hewett TE. High knee abduction moments are common risk factors for patellofemoral pain (PFP) and anterior cruciate ligament (ACL) injury in girls: Is PFP itself a predictor for subsequent ACL injury? Brit J Sport Med. 2014;49(2):118-122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Nakagawa TH, Uehara Moriya ET, Maciel CD, Serrao FV. Frontal plane biomechanics in males and females with and without patellofemoral pain. Med Sci Sport Exer. 2012;44(9):1747-1755. [DOI] [PubMed] [Google Scholar]
- 7.Hewett TE, Myer GD, Ford KR, Heidt RS, Colosimo AJ, McLean SG, van den Bogert AJ, Paterno MV, Succop P. Biomechanical measures of neuromuscular control and valgus loading of the knee predict anterior cruciate ligament injury risk in female athletes: A prospective study. Am J Sports Med. 2005;33(4):492-501. [DOI] [PubMed] [Google Scholar]
- 8.Zazulak BT, Hewett TE, Reeves NP, Goldberg B, Cholewicki J. Deficits in neuromuscular control of the trunk predict knee injury risk: A prospective biomechanical-epidemiologic study. Am J Sports Med. 2007;35(7):1123-1130. [DOI] [PubMed] [Google Scholar]
- 9.Pappas E, Carpes FP. Lower extremity kinematic asymmetry in male and female athletes performing jump-landing tasks. J Sci Med Sport. 2012;15(1):87-92. [DOI] [PubMed] [Google Scholar]
- 10.Cook G, Burton L, Hoogenboom BJ, Voight M. Functional movement screening: The use of fundamental movements as an assessment of function - part 1. Int J Sports Phys Ther. 2014;9(3):396-409. [PMC free article] [PubMed] [Google Scholar]
- 11.Plisky PJ, Rauh MJ, Kaminski TW, Underwood FB. Star Excursion Balance Test as a predictor of lower extremity injury in high school basketball players. J Orthop Sports Phys Ther. 2006;36(12):911-919. [DOI] [PubMed] [Google Scholar]
- 12.Padua DA, Marshall SW, Boling MC, Thigpen CA, Garrett WEJ, Beutler AI. The Landing Error Scoring System (LESS) Is a Valid and Reliable Clinical Assessment Tool of Jump-Landing Biomechanics. Am J Sports Med. 2009;37(10):1996-2002. [DOI] [PubMed] [Google Scholar]
- 13.Whatman C, Hume P, Hing W. The reliability and validity of physiotherapist visual rating of dynamic pelvis and knee alignment in young athletes. Phys Ther Sport. 2013;13(2):87-96. [DOI] [PubMed] [Google Scholar]
- 14.Harris-Hayes M, Steger-May K, Koh C, Royer NK, Graci V, Salsich GB. Classification of lower extremity movement patterns based on visual assessment: Reliability and correlation with 2-dimensional video analysis. J Athl Train. 2014;49(3):304-310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Eastlack ME, Arvidson J, Snyder-Mackler L, Danoff JV, McGarvey CL. Interrater reliability of videotaped observational gait-analysis assessments. Phys Ther. 1991;71(6):465-472. [DOI] [PubMed] [Google Scholar]
- 16.Ekegren CL, Miller WC, Celebrini RG, Eng JJ, Macintyre DL. Reliability and validity of observational risk screening in evaluating dynamic knee valgus. J Orthop Sports Phys Ther. 2009;39(9):665-674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Knudson D. Validity and reliability of visual ratings of the vertical jump. Percept Mot Skills. 1999;89(2):642-648. [DOI] [PubMed] [Google Scholar]
- 18.Almangoush A, Herrington L, Jones R. A preliminary reliability study of a qualitative scoring system of limb alignment during single leg squat. Phys Ther Rehabil. 2014;1(1):2-7. [Google Scholar]
- 19.Kennedy MD, Burrows L, Eric P. Intrarater and interrater reliability of the single-leg squat test. Athlet Ther Today. 2010;15(6):32-36. [Google Scholar]
- 20.Weeks BK, Carty CP, Horan SA. Kinematic predictors of single-leg squat performance. BMC Musculoskelet Disord. 2012;13(1):207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Munro A, Herrington L, Carolan M. Reliability of 2-dimensional video assessment of frontal-plane dynamic knee valgus during common athletic screening tasks. J Sport Rehabil. 2012;21(1):7-11. [DOI] [PubMed] [Google Scholar]
- 22.Nakagawa TH, Uehara Moriya ET, Maciel CD, Serrao FV. Test–retest reliability of three-dimensional kinematics using an electromagnetic tracking system during single-leg squat and stepping maneuver. Gait Posture. 2014;39(1):141-146. [DOI] [PubMed] [Google Scholar]
- 23.Ford KR, Myer GD, Hewett TE. Reliability of landing 3D motion analysis: Implications for longitudinal analyses. Med Sci Sport Exer. 2007;39(11):2021-2028. [DOI] [PubMed] [Google Scholar]
- 24.Gwynne CR, Curran SA. Quantifying frontal plane knee motion during single limb squats: reliability and validity of 2-dimensional measures. Int J Sports Phys Ther. 2014;9(7):898-906. [PMC free article] [PubMed] [Google Scholar]
- 25.Figueroa Ayala CN, Seda Díaz AH, Rodríguez Lafontaine A, Rosario M. Concurrent validity between two-dimensional and three dimensional motion systems for evaluation of frontal plane knee kinematics during a drop vertical jump task. [master's thesis]. San Juan, Puerto Rico: University of Puerto Rico; 2013. [Google Scholar]
- 26.McLean SG, Walkter K, Ford KR, Myer GD, Hewett TE, van den Bogert AJ. Evaluation of a two dimensional analysis method as a screening and evaluation tool for anterior cruciate ligament injury. Brit J Sport Med. 2005;39(6):355-362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Bell AL, Brand RA, Pedersen DR. Prediction of hip joint centre location from external landmarks. Hum Movement Sci. 1989;8(1):3-16. [Google Scholar]
- 28.Walusz HJ, Blackburg JT, Hirth C, Boling MC, McGrath ML, Padua DA. The relationship between knee flexion, hip flexion, and trunk flexion angles and anterior tibial shear force during a jump-landing task. [master's thesis]. Chapel Hill, NC: University of North Carolina; 2007. [Google Scholar]
- 29.DiCesare CA, Bates NA, Myer GD, Hewett TE. The validity of 2-dimensional measurement of trunk angle during dynamic tasks. Int J Sports Phys Ther. 2014;9(4):420-427. [PMC free article] [PubMed] [Google Scholar]
- 30.Willson JD, Davis IS. Utility of the frontal plane projection angle in females with patellofemoral pain. J Orthop Sports Phys Ther. 2008;38(10):606-615. [DOI] [PubMed] [Google Scholar]
- 31.Portney LG, Watkins MP. Foundations of Clinical Research: Applications to Practice. 3rd ed. Philadelphia, PA: F.A. Davis Company; 2015. [Google Scholar]
- 32.Norris BS, Olson SL. Concurrent validity and reliability of two-dimensional video analysis of hip and knee joint motion during mechanical lifting. Physiother Theory Pract. 2011;27(7):521-530. [DOI] [PubMed] [Google Scholar]
- 33.Gribble P, Hertel J, Denegar C, Buckley W. Reliability and validity of a 2-D video digitizing system during a static and a dynamic task. J Sport Rehabil. 2005. [Google Scholar]
- 34.Eltoukhy M, Kelly A, Kim C-Y, Jun H-P, Campbell R, Kuenze C. Validation of the Microsoft Kinect® camera system for measurement of lower extremity jump landing and squatting kinematics. Sports Biomechanics. February 2016:1-14. [DOI] [PubMed] [Google Scholar]
- 35.Clapis PA, Davis SM, Davis RO. Reliability of inclinometer and goniometric measurements of hip extension flexibility using the modified Thomas test. Physiother Theory Pract. 2009;24(2):135-141. [DOI] [PubMed] [Google Scholar]
- 36.Brosseau L, Tousignant M, Budd J, et al. Intratester and Intertester Reliability and Criterion Validity of the Parallelogram and Universal Goniometers for Active Knee Flexion in Healthy Subjects. Physiother Res Int. 1997;2(3):150-166. [DOI] [PubMed] [Google Scholar]
- 37.Menadue C, Raymond J, Kilbreath SL, Refshauge KM, Adams R. Reliability of two goniometric methods of measuring active inversion and eversion range of motion at the ankle. BMC Musculoskelet Disord. 2006;7(1). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Van Gheluwe B, Kirby KA, Roosen P, Phillips RD. Reliability and accuracy of biomechanical measurements of the lower extremities. J Am Podiatr Med Assoc. 2002;92(6):317-326. [DOI] [PubMed] [Google Scholar]
- 39.Nussbaumer S, Leunig M, Glatthorn JF, Stauffacher S, Gerber H, Maffiuletti NA. Validity and test-retest reliability of manual goniometers for measuring passive hip range of motion in femoroacetabular impingement patients. BMC Musculoskelet Disord. 2010;11(1):194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Nakagawa TH, Uehara Moriya ET, Maciel CD, Serrao FV. Trunk, pelvis, hip, and knee kinematics, hip strength, and gluteal muscle activation during a single-leg squat in males and females with and without patellofemoral pain syndrome. J Orthop Sports Phys Ther. 2012;42(6):491-501. [DOI] [PubMed] [Google Scholar]
- 41.Blackburn JT, Padua DA. Influence of trunk flexion on hip and knee joint kinematics during a controlled drop landing. Clin Biomech. 2008;23(3):313-319. [DOI] [PubMed] [Google Scholar]
- 42.Dingenen B, Malfait B, Vanrenterghem J, Verschueren SMP, Staes FF. The reliability and validity of the measurement of lateral trunk motion in two-dimensional video analysis during unipodal functional screening tests in elite female athletes. Phys Ther Sport. 2014;15(2):117-123. [DOI] [PubMed] [Google Scholar]
- 43.Powers CM. The influence of abnormal hip mechanics on knee injury: A biomechanical perspective. J Orthop Sports Phys Ther. 2010;40(2):42-51. [DOI] [PubMed] [Google Scholar]
- 44.Griffin LY, Agel J, Albohm MJ, Arendt EA, Dick RW, Garrett WE, Garrick JG, Hewett TE, Hustin L, Ireland ML, Johnson RJ, Kibler WB, Lephart S, Lewis JL, Lindenfeld TN, Mandelbaum BR, Marchak P, Teitz CC, Wojtys EM. Noncontact anterior cruciate ligament injuries. J Am Acad Orthop Surg. 2000;8(3):141. [DOI] [PubMed] [Google Scholar]
- 45.Dwyer MK, Boudreau SN, Mattacola CG, Uhl TL, Lattermann C. Comparison of lower extremity kinematics and hip muscle activation during rehabilitation tasks between sexes. J Athl Train. 2010;45(2):181-190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Graci V, Salsich GB. Trunk and lower extremity segment kinematics and their relationship to pain following movement instruction during a single-leg squat in females with dynamic knee valgus and patellofemoral pain. J Sci Med Sport. 2015;18(3):343-347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Ageberg E, Bennell KL, Hunt MA, Simic M, Roos EM, Creaby MW. Validity and inter-rater reliability of medio-lateral knee motion observed during a single-limb mini squat. BMC Musculoskelet Disord. 2010;11(1):265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Ford KR, Myer GD, Hewett TE. Valgus knee motion during landing in high school female and male basketball players. Med Sci Sport Exer. 2003;35(10):1745-1750. [DOI] [PubMed] [Google Scholar]
- 49.Paterno MV, Schmitt LC, Ford KR, et al. Biomechanical measures during landing and postural stability predict second anterior cruciate ligament injury after anterior cruciate ligament reconstruction and return to sport. Am J Sports Med. 2010;38(10):1968-1978. [DOI] [PMC free article] [PubMed] [Google Scholar]