Abstract
Background
The use of foam rollers to provide tissue massage is a commonly used intervention by rehabilitation professionals for their patients and clients. Currently, there is no consensus on the optimal foam rolling treatment approach. Of particular interest are the effects of different instructional methods of foam rolling, as individuals ultimately perform these interventions independently outside of formal care. Finding the optimal instructional method may help improve the individual's understanding of the technique, allowing for a safe and effective intervention.
Purpose
The purpose of this study was to compare the effects of video-guided, live instructed, and self-guided foam roll interventions on knee flexion Range of Motion (ROM) and pressure pain thresholds.
Methods
Forty-five healthy adults were recruited and randomly allocated to one of three intervention groups: video-guided, live-instructed, and self-guided. Each foam roll intervention lasted a total of 2 minutes. Dependent variables included knee flexion ROM and pressure pain threshold of the left quadriceps. Statistical analysis included subject demographic calculations and appropriate parametric and non-parametric tests to measure changes within and between intervention groups.
Results
Each intervention group showed significant gains in knee flexion ROM (p ≤ 0.003) and pressure pain thresholds (p < 0.001). An approximate 5 degree increase of knee flexion and a 150 kPa increase in pressure pain threshold was observed at the posttest measure for all groups. There was no significant difference (p=0.25) found between intervention groups.
Conclusion
All three foam roll interventions showed short-term increases in knee flexion ROM and pressure pain thresholds. The two instructional methods (video and live instruction) and the self-guided method produced similar outcomes and can be used interchangeably. Individuals can benefit from various types of instruction and in cases of limited resources video may offer an alternative or adjunct to live instruction or an existing self-guided program.
Level of Evidence
2c
Keywords: exercise instruction, myofascial rolling, perceived pain, muscle soreness, recovery
Introduction
The use of foam rollers to provide tissue massage is a commonly used intervention by rehabilitation professionals for patients and clients. Foam rollers come in several sizes and densities. Commercial foam rollers are typically available in two lengths 36 inch and 18 inch.1,2 The structure of foam rollers vary from a mild density foam to a more rigid solid plastic cyllinder with a dense foam outer covering. Reseachers have shown that higher density foam rollers produce more pressure to the target tissues and may have a stonger effect on the tissues than softer density foam rollers, which could be a potential benefit.3 However, patient tolerance is a factor that must be considered when using higher density foam rolls.
The current research suggests that foam rolling may offer short-term benefits for increasing joint range of motion (ROM) at the hip, knee, and ankle without affecting muscle performance.1,2 These findings further suggest that foam rolling for one to five minutes may be beneficial for enhancing joint flexibility as a pre-exercise warm-up and cool down due to identified short-term benefits ( ≤ 10 minutes).1 After intense exercise, decrements in muscle performance and delayed onset muscle soreness (DOMS) may be attenuated after foam rolling for 10 to 20 minutes.1,2,4 Continued foam rolling (20 minutes per day) over a period of three days may further decrease a patient's pain level and may be beneficial as a post-exercise intervention.1 Research has shown that foam rolling can increase posttreatment pressure pain thresholds,5 reduce arterial stiffness, and improve vascular endothelial function, all which are associated with increased flexibility.6
Due to the popularity of this intervention, foam rollers are commonly used in outpatient rehabilitation, fitness facilities, and as a home-based intervention. Currently, there is no consensus on the optimal foam rolling treatment time, cadence, and technique, amount of force, foam roller density, or instructional strategy.1,2 Of particular interest are the effects of different instructional methods for foam rolling. Finding the optimal instructional method may help improve the patient's performance of the technique, allowing for a safe and effective intervention. One method to improve patient adherence may by to use an Internet based instructional video to reinforce the foam roller techniques prescribed by the clinician. To date, no studies have compared the efficacy of an Internet based instructional video to live-instruction for learning the methods to perform foam rolling. The purpose of this study was to compare the effects of video-guided, live instructed, and self-guided foam rolling interventions on knee flexion ROM and pressure pain thresholds.
METHODS
This pretest, posttest randomized controlled trial was approved by the university Institutional Review Board (IRB# 16-180).
Subjects
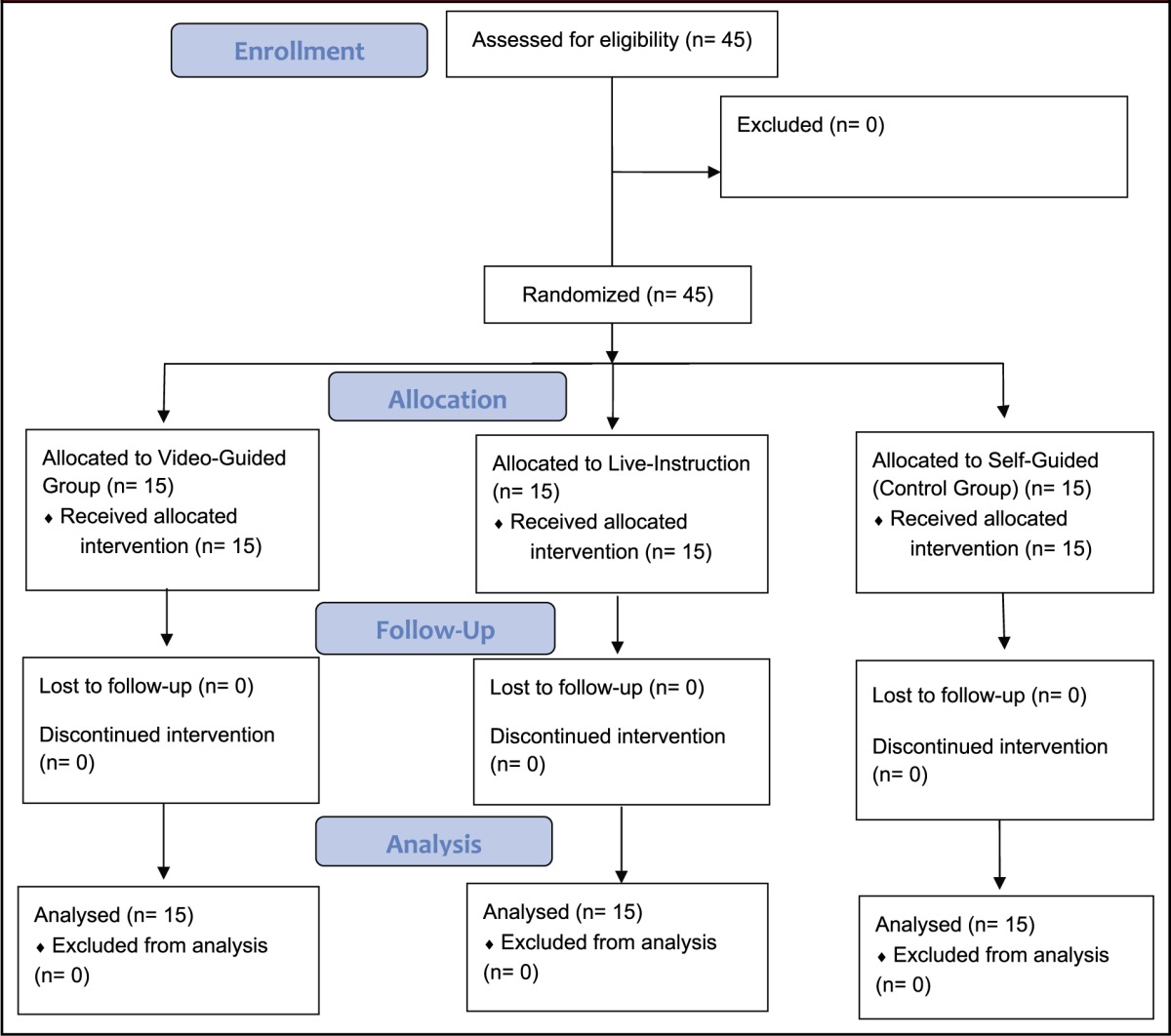
Forty-five healthy adults (28 males, 17 females) (age = 26 ± 6.5 years, height = 1.68 ± 0.1m; body mass=74.1 ± 17.6; body mass index (BMI)=26.1 ± 5.3) were recruited via convenience sampling (e.g. flyers). Descriptive demographic information is provided in Table 1. Volunteers were randomly allocated into three groups of 15 subjects: (1) video-guided intervention, (2) live instructed intervention, and (3) self-guided intervention. The self-guided intervention was considered the control group for this investigation. Exclusion criteria included the presence of any musculoskeletal, systemic, or metabolic disease that would affect lower extremity joint range of motion or tolerance to pressure pain threshold testing and the inability to avoid medications that may have had an effect on testing (Table 2).
Table 1.
Subject demographics.
| characteristics | age (years) | height (m) | mass (kg) | bmi (kg/m2) |
|---|---|---|---|---|
|
video-guided (n=15) |
28.0 ± 9.5 (range 21-54) |
1.66 ± 0.1(range 1.5-1.9) | 74.0 ± 18.5 (range 43.1-101.2) |
25.3 ± 3.8 (range 19.2-31.4) |
|
live instruction (n=15) |
25.5 ± 3.8 (range 20-33) |
1.68 ± 0.1 (range 1.4-1.8) |
75.1 ± 16.2 (range 51.3-111.1) |
26.5 ± 5.0 (range 19.4-36.3) |
|
self-guided (n=15) |
26.4 ± 5.1 (range 21-39) |
1.66 ± 0.1 (range 1.5-1.8) |
73.2 ± 19.2 (range 50.1-113.3) |
26.7 ± 7.0 (range 19.1-46.5) |
data reported as mean ± sd; range (min-max); m=meters; bmi = body mass index; kg/m2 = kilograms-meter squared
Table 2.
Consort flow diagram.
 |
Instruments
Two measurement instruments were used in this investigation. First, the baseline digital inclinometer (Fabrication Enterprises, White Plains, NY, USA) was used to measure passive knee flexion ROM. This device has been shown to be valid and reliable for measuring lower extremity ROM (Figure 1).7–10 Second, the JTECH (Midvale, UT) Tracker Freedom® wireless algometer (Figure 2) was used with the accompanying Tracker 5® Windows® based software to measure pressure pain threshold. Algometry is a valid and reliable tool for measuring pressure pain thresholds.5,11–13
Figure 1.
Baseline digital inclinometer.
Figure 2.
JTECH algometer.
Instructional Video and Foam Roll
A commercial Internet based video and accompanied foam roller (GRID) were used in this investigation (Trigger Point Technologies, Austin, TX, USA). The short foam rolling instructional video demonstrated the use of the 18-inch size GRID foam roller on the left quadriceps muscle group. The GRID foam roll is a rigid solid plastic cyllinder with a dense foam outer covering which has been used in prior research (Figure 3).14 More details of the video instructions are discussed in the procedures section.
Figure 3.
GRID foam roll.
Outcome Measures
Two outcome measures were used for the pretest and posttest measures. For passive knee flexion, subjects lay prone on a yoga mat. The examiner grasped the left ankle and passively moved the left knee to the end of the available flexion ROM to the point where the knee could no long be passively moved without providing overpressure,15–17a measurement was then taken by the examiner. The examiner monitored for any compensatory movement through the lower extremity and pelvis. This testing technique was chosen since it replicated the same hip position and knee movements that occurred during the foam roll interventions and has been used in prior research.15–17 For pressure pain threshold, the left quadriceps group was tested with the subject in the relaxed standing position (two measurements).18 The 1.0-cm2 probe of the algometer was placed into the midline of the left quadriceps (rectus femoris) midway between the iliac crest and superior border of the patella. The graded force was applied at a constant rate of 50-60 kilopascals per second (kPa/sec) until the subject indicated the presence of pain.18
Pilot Study
Prior to data collection, a two session pilot training was conducted to establish intrarater reliability and practice testing procedures for all interventions. Two examiners were involved with data collection. The primary investigator took all the measurements while a second investigator participated in the live-instruction intervention. The primary investigator was a licensed physical therapist with over 12 years of experience and board certified in orthopedics. Ten independent subjects were recruited and tested for the pilot portion of the study. The intrarater reliability was calculated using the Intraclass Correlation Coefficient (ICC model 3, k). Good intrarater reliability was established for passive knee flexion measurements (ICC = 0.95; 95% CI 0.83-0.99) and pressure algometry (ICC = 0.94; 95% CI 0.61-0.90). 19 These coefficients are in accordance with the minimum threshold of ≥ 0.90 for ICC values postulated to be acceptable for clinical decision making.19
Procedures
All eligible participants were given an IRB approved consent form to read and sign before testing. Participants then completed a questionnaire to provide demographic information. All participants were tested by one investigator and were blinded from the results and other participants enrolled in the study. A second investigator participated in the live-instruction group procedures but was blinded to the testing results. Testing was conducted between the hours of 10 A.M. and 2 P.M. and subjects were instructed to refrain from any strenuous activity three hours prior to testing and from taking any medication that would interfere with testing. The intervention was performed on the left quadriceps for all groups. All subjects underwent pretest measures, followed by the instruction and rolling intervention, then immediate posttest measures. The specific procedures for each intervention are discussed below.
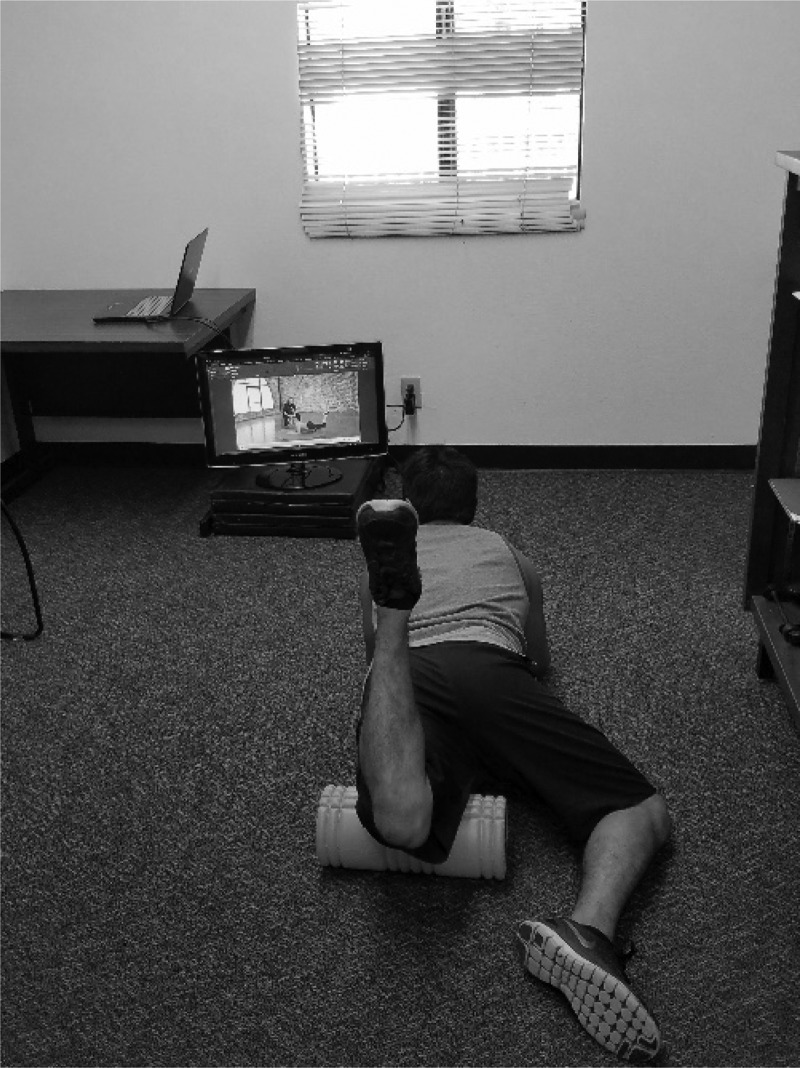
For the video-guided intervention, subjects followed an instructional video that demonstrated the use of the foam roll on the left quadriceps muscle group. Subjects had their own foam roll and followed the video with no feedback from the observing primary investigator (Figure 4). The instructor in the video provided a brief introduction and then discussed the foam rolling technique. The instructor divided the left quadriceps into zone one: top of patella to middle of the quadriceps and zone two: middle quadriceps to anterior superior iliac spine. The model in the video was instructed to get in the plank position allowing moderate weight bearing to the anterior thigh. Then to position the roller above the left patella and roll back and forth in zone one, four times at a cadence of one inch per second. The model was then instructed to stop at the top of zone one followed by four knee bends to 90 degrees. This sequence was repeated for zone two. The intervention portion lasted a total of two minutes.
Figure 4.
Video-guided intervention.
For the live-instruction intervention, subjects followed the examiner's instructions which were the same as the video-guided intervention. The video was transcribed into a text-based script that the examiner followed while teaching the foam rolling technique. The examiner began by demonstrating the foam rolling sequence for zone one and zone two of the left quadriceps then had the subject perform the two-minute sequence of rolling and knee bends. The examiner was observed by the primary investigator during the intervention to ensure accuracy and consistency of the teachings.
For the self-guided or control intervention, the primary investigator demonstrated the plank position and placement of the roller under the left quadriceps group. Subjects performed their own preferred method of foam rolling on the left leg for two minutes. The investigator monitored the intervention time and did not provide any feedback.
Statistical Analysis
Statistical analyses were performed using SPSS version 24.0 (IBM SPSS, Chicago, IL, USA). Subject descriptive data was calculated and reported as the mean and standard deviation (SD) for age, height, body mass, and body mass index (BMI) (Table 1). Group differences were calculated using the ANOVA test for continuous level data and the Kruskal Wallis test for ordinal level data. A factorial repeated ANOVA was used to compare pretest and posttest knee flexion ROM and pressure pain threshold for all three intervention groups. Post hoc testing was conducted using the Tukey post hoc test. The mean of two PPT measures was used for the statistical analysis.20,21 Statistical significance was considered when p < 0.05.
RESULTS
Forty-five subjects aged 20-54 (age = 26 ± 6.5) years completed the study. There were no adverse events and no subjects withdrew during data collection. Statistical analysis of the descriptive data revealed no significant differences between the three groups for age (p=0.57), height (p=0.74), body mass (p=0.96), and BMI (p=0.75) (Table 1).
Within Group Comparison
For passive knee flexion ROM, a significant time effect was found for the video-guided [F (1,14)=118.5, p < 0.001, partial η2=0.89], live-instruction [F (1,14)=112.3, p<0.001, partial η2=0.89], and the self-guided intervention [F(1,14)=12.9, p=0.003, partial η2=0.48]. Post hoc testing revealed a mean increase of approximately five degrees (p ≤ 0.003) from pretest to posttest for all three groups (Table 3).
Table 3.
Pretest, posttest descriptive results.
| Pretest | Posttest | Change | P-Value | |
|---|---|---|---|---|
| Video-Guided | ||||
| Knee ROM (degrees) | 135.3 ± 8.8 | 140.2 ± 7.8 | 4.9 ± 1.7 | <0.001 |
| Pressure Pain Threshold (kPa) | 1123.3 ± 312.9 | 1268.0 ± 268.6 | 145.3 ± 77.4 | <0.001 |
| Live Instruction | ||||
| Knee ROM (degrees) | 140.4 ± 7.7 | 145.3 ± 7.7 | 4.9 ± 1.8 | <0.001 |
| Pressure Pain Threshold (kPa) | 1185.3 ± 312.9 | 1268.7 ± 268.6 | 119.3 ± 72.8 | <0.001 |
| Self-Guided | ||||
| Knee ROM (degrees) | 134.5 ± 13.6 | 139.6 ± 14.2 | 5.1 ± 5.5 | 0.003 |
| Pressure Pain Threshold (kPa) | 940 ± 319.3 | 1124.2 ± 365.6 | 184.2 ± 115.8 | <0.001 |
*IR: inter Data reported as mean ± SD, kPa = kilopascals; statistical significance considered p<.05
For pressure pain threshold, a significant time effect was found for the video-guided [F (1,14)=52.8, p < 0.001, partial η2=0.79], live-instruction [F (1,14)=40.2, p<0.001, partial η2=0.74], and self-guided intervention [F(1,14)=37.9, p < 0.001, partial η2=0.73]. Post hoc testing revealed a mean increase of approximately 150 kPa (p<0.001) from pretest to posttest for all three groups (Table 3).
Between Group Comparison
Statistical analysis revealed no significant difference between groups for knee flexion ROM [F (2,42)=1.44, p=0.25, partial η2=0.25] and pressure pain threshold [F (2,42)=1.45, p=0.25, partial η2=0.06].
DISCUSSION
This investigation sought to compare the efficacy of a video-guided, live instructed, and self-guided (control) foam roll intervention in healthy adults. The results suggest that foam rolling interventions produce short-term gains in knee flexion ROM and can increase pressure pain threshold levels (improve individual tolerance to pain) in the target muscle group regardless of instructions given for performance. These short-term gains have been observed in prior research.1,5 Perhaps, the effects that occur from foam rolling are independent of the type of instruction and may occur from the physical force applied by the body's weight on the foam roller.
Two proposed theories suggest that foam rolling can cause a mechanical or neurophysiological effect.22,23 Mechanical theory suggests that the viscoelastic properties of fascia are affected by the pressure of the foam roll. Other mechanisms involved may include reduced thixotrophy, alteration in myofascial restriction and trigger points, fluid changes, cellular responses, and fascial inflammation.22,23 Neurophysiological theory suggests that mechanical pressure from the foam roll influences tissue relaxation and pain reduction through central nervous system afferent input from the Golgi tendon reflex, mechanoreceptors (e.g. Golgi tendon organ), and nocioceptors. 22,23 These hypotheses still need further investigation. Lastly, the lack of between group differences do indeed have practical implications, as it seems that individualized instruction may not be necessary if indeed other instructional methods are available.
Clinicians must consider that the results of this investigation suggest that the two instructional methods (video and live instruction) and the self-guided method produced similar outcomes and can be used interchangeably. Clinically, live instruction may be more practical since the clinician can teach and observe the patient performing the foam rolling technique and provide any corrections as needed. The clinician could reinforce the technique taught by recommending an instructional internet video for the patient to follow or follow up with the patient after they have attempted the technique themselves. Clinicians often use live-instruction to teach the patient an exercise technique. This traditional method has been shown to have limitations due to poor patient compliance. Researchers have suggested that up to 70% of patients do not adhere to a home exercise program.24 Patients often have better adherence with a structured and monitored home exercise program.25–28 The use of Internet based video instruction may enhance the patient's understanding of the technique. The most recent statistics from 2012 report that 71% of all Internet users had accessed the Internet to search for health related information or interact with a health professional and that 35% of adults in the United States report having used the Internet to specifically diagnose a health condition.29,30 This growing trend may eventually become the standard way patients access information. Clinicians may need to utilize current technology in order to provide their patients with the best care.
Limitations
Several limitations need to be discussed in relation to this investigation. First, this investigation tested only healthy subjects which limits the generalizability of these results to other populations. Second, the short-term effects of each instructional foam roll method were studied, thus, similar results may not be present in the long-term. This may specifically be a concern to those who used the self-guiding method as a divergence in technique may occur over time. Third, the video-guided intervention and live instruction only demonstrated only a single foam rolling technique on the quadriceps group for a short duration. This must be considered for clinical practice or prescription of a video based instructional program provided in a static format. Fourth, the GRID foam roll was used in this study, which is a rigid cylinder with an outer foam layer. Foam rollers with different densities may have produced different results.
Future research
Future research should attempt to determine the optimal teaching strategy for different patient populations and among various cohorts of the general population such as distance runners and recreational athletes. Specifically, determining whether any teaching strategy is more effective for patients with different medical conditions and at different stages in the rehabilitation process. Future research should also focus on determining the optimal foam rolling treatment including: cadence, technique, amount of force, and optimal type of foam roller for different musculoskeletal conditions.
Conclusion
This investigation compared an Internet based instructional video to live-instruction and no instruction for a common foam rolling intervention. All intervention groups showed gains in ROM and pressure pain thresholds, indicating no difference attributable to instructional strategy. The research on foam rolling is still developing with no current consensus on the most optimal instructional strategy. This investigation provides some insight into options for teaching techniques to healthy individuals. Individuals can benefit from various types of instruction and in cases of limited resources video may offer an alternative or adjunct to live instruction or an existing self-guided program. Future research should focus on determining the optimal teaching strategy for different patient populations.
References
- 1.Cheatham SW, Kolber MJ, Cain M, et al. The effects of self-myofascial release using a foam roll or roller massager on joint range of motion, muscle recovery, and performance: A systematic review. Int J Sports Phys Ther. 2015;10(6):827-838. [PMC free article] [PubMed] [Google Scholar]
- 2.Beardsley C, Skarabot J. Effects of self-myofascial release: A systematic review. J Bodyw Mov Ther. 2015;19(4):747-758. [DOI] [PubMed] [Google Scholar]
- 3.Curran PF, Fiore RD, Crisco JJ. A comparison of the pressure exerted on soft tissue by 2 myofascial rollers. J Sport Rehabil. 2008;17(4):432-442. [DOI] [PubMed] [Google Scholar]
- 4.Schroeder AN, Best TM. Is self myofascial release an effective preexercise and recovery strategyϿ. A literature review. Curr Sports Med Rep. 2015;14(3):200-208. [DOI] [PubMed] [Google Scholar]
- 5.Aboodarda SJ, Spence AJ, Button DC. Pain pressure threshold of a muscle tender spot increases following local and non-local rolling massage. BMC Musculoskelet Disord. 2015;16:265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Okamoto T, Masuhara M, Ikuta K. Acute effects of self-myofascial release using a foam roller on arterial function. J Strength Cond Res. 2014;28(1):69-73. [DOI] [PubMed] [Google Scholar]
- 7.Roach S, San Juan JG, Suprak DN, et al. Concurrent validity of digital inclinometer and universal goniometer in assessing passive hip mobility in healthy subjects. Int J Sports Phys Ther. 2013;8(5):680-688. [PMC free article] [PubMed] [Google Scholar]
- 8.Romero-Franco N, Montano-Munuera JA, Jimenez-Reyes P. Validity and reliability of a digital inclinometer to assess knee joint position sense in a closed kinetic chain. J Sport Rehabil. 2016:1-16. [DOI] [PubMed] [Google Scholar]
- 9.Konor MM, Morton S, Eckerson JM, et al. Reliability of three measures of ankle dorsiflexion range of motion. Int J Sports Phys Ther. 2012;7(3):279-287. [PMC free article] [PubMed] [Google Scholar]
- 10.Gnat R, Kuszewski M, Koczar R, et al. Reliability of the passive knee flexion and extension tests in healthy subjects. J Manipulative Physiol Ther. 2010;33(9):659-665. [DOI] [PubMed] [Google Scholar]
- 11.Chesterton LS, Sim J, Wright CC, et al. Interrater reliability of algometry in measuring pressure pain thresholds in healthy humans, using multiple raters. Clin J Pain. 2007;23(9):760-766. [DOI] [PubMed] [Google Scholar]
- 12.Nussbaum EL, Downes L. Reliability of clinical pressure-pain algometric measurements obtained on consecutive days. Phys Ther. 1998;78(2):160-169. [DOI] [PubMed] [Google Scholar]
- 13.Walton DM, Macdermid JC, Nielson W, et al. Reliability, standard error, and minimum detectable change of clinical pressure pain threshold testing in people with and without acute neck pain. J Orthop Sports Phys Ther. 2011;41(9):644-650. [DOI] [PubMed] [Google Scholar]
- 14.Skarabot J, Beardsley C, Stirn I. Comparing the effects of self-myofascial release with static stretching on ankle range-of-motion in adolescent athletes. Int J Sports Phys Ther. 2015;10(2):203-212. [PMC free article] [PubMed] [Google Scholar]
- 15.Lee SY, Sung KH, Chung CY, et al. Reliability and validity of the Duncan-Ely test for assessing rectus femoris spasticity in patients with cerebral palsy. Dev Med Child Neurol. 2015;57(10):963-968. [DOI] [PubMed] [Google Scholar]
- 16.Marks MC, Alexander J, Sutherland DH, et al. Clinical utility of the Duncan-Ely test for rectus femoris dysfunction during the swing phase of gait. Dev Med Child Neurol. 2003;45(11):763-768. [DOI] [PubMed] [Google Scholar]
- 17.Peeler J, Anderson JE. Reliability of the Ely's test for assessing rectus femoris muscle flexibility and joint range of motion. J Orthop Res. 2008;26(6):793-799. [DOI] [PubMed] [Google Scholar]
- 18.Pearcey GE, Bradbury-Squires DJ, Kawamoto JE, et al. Foam rolling for delayed-onset muscle soreness and recovery of dynamic performance measures. J Athl Train. 2015;50(1):5-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Portney LG, Watkins MP. Foundations of Clinical Research: Applications to Practice. Pearson/Prentice Hall; 2009. [Google Scholar]
- 20.Balaguier R, Madeleine P, Vuillerme N. Intra-session absolute and relative reliability of pressure pain thresholds in the low back region of vine-workers: Effect of the number of trials. BMC Musculoskelet Disord. 2016;17(1):350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Balaguier R, Madeleine P, Vuillerme N. Is one trial sufficient to obtain excellent pressure pain threshold reliability in the low back of asymptomatic individualsϿ. A test-retest study. PLoS One. 2016;11(8):e0160866. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Jay K, Sundstrup E, Sondergaard SD, et al. Specific and cross over effects of massage for muscle soreness: randomized controlled trial. Int J Sports Phys Ther. 2014;9(1):82-91. [PMC free article] [PubMed] [Google Scholar]
- 23.Kelly S, Beardsley C. Specific and cross-over effects of foam rolling on ankle dorsiflexion range of motion. Int J Sports Phys Ther. 2016;11(4):544-551. [PMC free article] [PubMed] [Google Scholar]
- 24.Sluijs EM, Kok GJ, van der Zee J. Correlates of exercise compliance in physical therapy. Phys Ther. 1993;73(11):771-782; discussion 783-776. [DOI] [PubMed] [Google Scholar]
- 25.Picorelli AM, Pereira LS, Pereira DS, et al. Adherence to exercise programs for older people is influenced by program characteristics and personal factors: A systematic review. J Physiother. 2014;60(3):151-156. [DOI] [PubMed] [Google Scholar]
- 26.Anwer S, Alghadir A, Brismee JM. Effect of home exercise program in patients with knee osteoarthritis: A systematic review and meta-analysis. J Geriatr Phys Ther. 2016;39(1):38-48. [DOI] [PubMed] [Google Scholar]
- 27.Gallagher KM. Helping older adults sustain their physical therapy gains: A theory-based intervention to promote adherence to home exercise following rehabilitation. J Geriatr Phys Ther. 2016;39(1):20-29. [DOI] [PubMed] [Google Scholar]
- 28.Jordan JL, Holden MA, Mason EE, et al. Interventions to improve adherence to exercise for chronic musculoskeletal pain in adults. Cochrane Database Syst Rev. 2010(1):Cd005956. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Silver MP. Patient perspectives on online health information and communication with doctors: A qualitative study of patients 50 years old and over. J Med Internet Res. 2015;17(1):e19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Fredericks S MG. Delivering a patient education intervention using both the internet and telephone – A discursive presentation. Can J Nurs Inform. 2013;7(3):1-6. [Google Scholar]