Abstract
Background/Objective:
There is little randomised evidence using a whole food plant-based (WFPB) diet as intervention for elevated body mass index (BMI) or dyslipidaemia. We investigated the effectiveness of a community-based dietary programme. Primary end points: BMI and cholesterol at 6 months (subsequently extended).
Subjects:
Ages 35–70, from one general practice in Gisborne, New Zealand. Diagnosed with obesity or overweight and at least one of type 2 diabetes, ischaemic heart disease, hypertension or hypercholesterolaemia. Of 65 subjects randomised (control n=32, intervention n=33), 49 (75.4%) completed the study to 6 months. Twenty-three (70%) intervention participants were followed up at 12 months.
Methods:
All participants received normal care. Intervention participants attended facilitated meetings twice-weekly for 12 weeks, and followed a non-energy-restricted WFPB diet with vitamin B12 supplementation.
Results:
At 6 months, mean BMI reduction was greater with the WFPB diet compared with normal care (4.4 vs 0.4, difference: 3.9 kg m−2 (95% confidence interval (CI)±1), P<0.0001). Mean cholesterol reduction was greater with the WFPB diet, but the difference was not significant compared with normal care (0.71 vs 0.26, difference: 0.45 mmol l−1 (95% CI±0.54), P=0.1), unless dropouts were excluded (difference: 0.56 mmol l−1 (95% CI±0.54), P=0.05). Twelve-month mean reductions for the WFPB diet group were 4.2 (±0.8) kg m−2 BMI points and 0.55 (±0.54, P=0.05) mmol l−1 total cholesterol. No serious harms were reported.
Conclusions:
This programme led to significant improvements in BMI, cholesterol and other risk factors. To the best of our knowledge, this research has achieved greater weight loss at 6 and 12 months than any other trial that does not limit energy intake or mandate regular exercise.
Introduction
Background
Globally, the obesity epidemic worsens.1, 2 In 2014 more than 600 million adults were obese and a further 1.9 billion adults were overweight.3 In New Zealand, 31% of adults are obese and 35% are overweight.4 A raised body mass index (BMI) is associated with many forms of cancers; type 2 diabetes (T2DM); osteoarthritis; obstructive sleep apnoea; a shorter life expectancy; a lower quality of life and cardiovascular disease.2, 3, 5, 6 Additionally, these diseases impose a significant financial burden on both the health-care system and the wider economy.7
Many individuals attempt to lose weight by making changes to their diet, and commercial weight loss programmes are part of a multibillion-dollar market.8 Reviews of dietary interventions for weight loss fail to demonstrate superiority of one diet over another.8, 9, 10 In one review of 48 trials comparing commercial interventions, both low-carbohydrate and low-fat diet approaches were deemed effective at 6 months; participants lost on average 8 kg, with 1–2 kg regained at 12 months.10 Massive weight loss has also been achieved through a very high carbohydrate (⩾90 % dietary energy), calorie-restricted 'Rice Diet' as far back as 1940. This extremely restrictive approach has shown in one case series an average 63.9 (SD±17.2) kg weight loss for 106 patients.11, 12
The whole food plant-based (WFPB) diet is high in micronutrient density and the most frequently researched iterations are low in fat, which comprises approximately 7–15% of total energy.13, 14, 15 Interventions using the WFPB diet (alone, or with exercise and stress reduction) have demonstrated: reversal of ischaemic heart disease, improvements in glycaemic control, weight loss, long-term acceptability and sustainability, and reduction of prostate-specific antigen in biopsy-proven low-grade prostate cancer.16, 17, 18, 19, 20, 21, 22
Other nonclinical implications deserve attention. A WFPB diet generally requires less land, energy, and water than a diet high in animal products.23 On a per calorie basis, a high-meat diet (>100 g per day) produces 2.5 times more greenhouse gas emissions than a vegan diet.24 Farming the estimated 70 billion land animals consumed annually contributes between 14.5 and 51% of total human-induced greenhouse gas emissions, more than all of transportation.23, 25, 26, 27, 28
Objective
We aimed to investigate the effectiveness of our community-based WFPB dietary programme in a population of New Zealanders. Our programme was unique because we focused on creating long-term behavioural changes through developing practical skills (especially cooking).13, 16, 17, 19
Subjects and methods
Study overview
The BROAD study was a prospective, two-arm, parallel, superiority study run from August 2014 to initially February 2015 (subsequently extended). We compared standard medical care (control) with standard medical care plus a diet change programme (intervention).
Recruitment of participants
The intervention involved patients from a group general practice in Gisborne, the region with New Zealand's highest rates of socioeconomic deprivation, obesity and type 2 diabetes.29, 30 Inclusion criteria were age 35–70 and either obese (BMI⩾30 kg m−2) or overweight (BMI⩾25 kg m−2), with a diagnosis of one of type 2 diabetes, ischaemic heart disease, or the cardiovascular risk factors of hypertension or hypercholesterolaemia (for definitions see Table 1, baseline characteristics). Participant exclusion criteria were diagnoses of life-threatening comorbidities; thyroid disease; coronary artery bypass grafting within 6 weeks; myocardial infarction within 1 month; angioplasty within 6 months; >50% stenosis of the left main coronary artery; unresponsive congestive heart failure; malignant uncontrolled arrhythmias; homozygous hypercholesterolaemia; severe mental health disorders; current alcohol or drug misuse; currently smoking; currently pregnant or breastfeeding women, prior bariatric surgery, other conditions that directly affect weight (e.g. lead toxicity, malignancy).
Table 1. Participant characteristics at baseline according to study arm (n=65).
| Characteristic | Intervention (n=33) | Control (n=32) |
|---|---|---|
| Sex, n (%) | ||
| Female | 22 (67) | 17 (53) |
| Male | 11 (33) | 15 (47) |
| Age, years (±SD) | 56±9.9 | 56±9.5 |
| Ethnicity,a n (%) | ||
| NZ European | 30 (90.9) | 21 (65.6) |
| Māori | 3 (9.1) | 5 (15.6) |
| Other | 6 (18.7) | |
| Diagnosesa | ||
| BMIb (kg m−2) | ||
| Obesity, ⩾30 | 29 (88) | 30 (94) |
| Overweight, 25–29.9 | 4 (12) | 2 (6) |
| Type 2 diabetes mellitusc | 7 (21) | 2 (6) |
| Cardiovascular pathology | 20 (61) | 20 (63) |
| Ischaemic heart diseased | 4 (12) | 3 (9) |
| Hypertensione | 19 (58) | 17 (52) |
| Hypercholesterolaemiaf | 17 (52) | 15 (47) |
| Clinical measures—values are means (95% CI) | ||
| Weight (kg) | 94.8 (6.4) | 96.9 (7.4) |
| BMI (kg m−2) | 34.5 (1.6) | 34.2 (2.3) |
| Cholesterolg (mmol l−1) | ||
| Total | 5.4 (0.5) | 5.5 (0.6) |
| Triglycerides | 1.6 (0.3) | 1.4 (0.3) |
| LDL | 3.4 (0.4) | 3.5 (0.5) |
| HDL | 1.3 (0.1) | 1.4 (0.2) |
| Waist circumference (cm) | 108 (4) | 110 (5) |
| Systolic BP (mm Hg) | 133 (6) | 132 (7) |
| Diastolic BP (mm Hg) | 81 (3) | 78 (3) |
| HbA1c (mmol mol−1) | 42 (3) | 37 (2) |
| CVD RA (% 5-year risk)h | 11.7 (2.5) | 12.2 (1.9) |
| Questionnairesi | ||
| SF-36 Physical component summary | 47 (3) | 49 (3) |
| SF-36 Mental component summary | 52 (2) | 54 (3) |
| Dietary indiscretions | 26 (3) | 22 (4) |
| Exercise | 20 (9) | 47 (23) |
| Food enjoyment | 12 (1) | 13 (1) |
| Food cost | 23 (5) | 22 (3) |
| General self-efficacy | 32 (1) | 32 (2) |
| Nutritional self-efficacy | 15 (1) | 16 (1) |
| Self-esteem | 2.4 (0.3) | 2.3 (0.3) |
| Big Five Inventory Multidimensional Personality Assessment | ||
| Extraversion | 3.1 (0.3) | 3.3 (0.3) |
| Agreeableness | 4 (0.2) | 4 (0.3) |
| Conscientiousness | 3.9 (0.2) | 4.2 (0.2) |
| Neuroticism | 2.7 (0.2) | 2.4 (0.3) |
| Openness | 3.6 (0.3) | 3.5 (0.3) |
| Readiness for change | ||
| Question 1 | 3.3 (0.2) | 3.4 (0.2) |
| Question 2 | 3.3 (0.2) | 3.3 (0.2) |
| Question 3 | 3.4 (0.2) | 3.3 (0.2) |
From information on electronic medical records (EMR) system.
Body mass index is calculated as the weight in kilograms divided by the square of the height in metres.
Type 2 diabetes mellitus was defined by the New Zealand standard, HbA1c ⩾50mmol mol−1 cutoff.
Ischaemic heart disease included prior coronary stenting; prior coronary artery bypass grafting (CABG); prior cardiovascular ischaemic event; or antianginal medication use.
Hypertension included pre-treatment BP>140/90 mm Hg or current antihypertensive medication prescription.
Hypercholesterolaemia included those with pre-treatment total cholesterol >6mmol l−1 or current cholesterol-lowering medication prescription.
To convert values for total, low-density lipoprotein cholesterol (LDL) and high-density lipoprotein cholesterol (HDL) from mmol l−1 to mg dl−1, multiply by 38.67, for triglycerides multiply mmol l−1 by 88.57.
The cardiovascular disease risk calculator estimates the risk of a cardiovascular event occurring within a 5-year period, using age, current HbA1c, duration of type 2 diabetes, sex, smoking status, ethnicity, total cholesterol to HDL-cholesterol ratio, systolic BP and status regarding use of BP lowering medication.
We used the Short Form 36 Health Survey (SF-36) for quality of life assessment and responses were scored using Optum Scoring Software v4.5. For 3-day food recall each ‘red category' or ambiguous food item scored one point, e.g. pasta with meat (1) and cheese (1)=2, values reflect total over 3 days. Exercise units were average for 3 days using minutes of exercise × rated perceived exertion, where value shown is in hundreds, that is, 32 in table=3200. Food enjoyment, self-efficacy and readiness for change used a 1–4 Likert scale, with 4 being highest. Pooled answers had maximum score: 16 for food enjoyment, 40 for general self-efficacy and 20 for nutritional self-efficacy. Self-esteem was a single question using a 1–5 Likert scale, with 1 as highest.
Enrolment
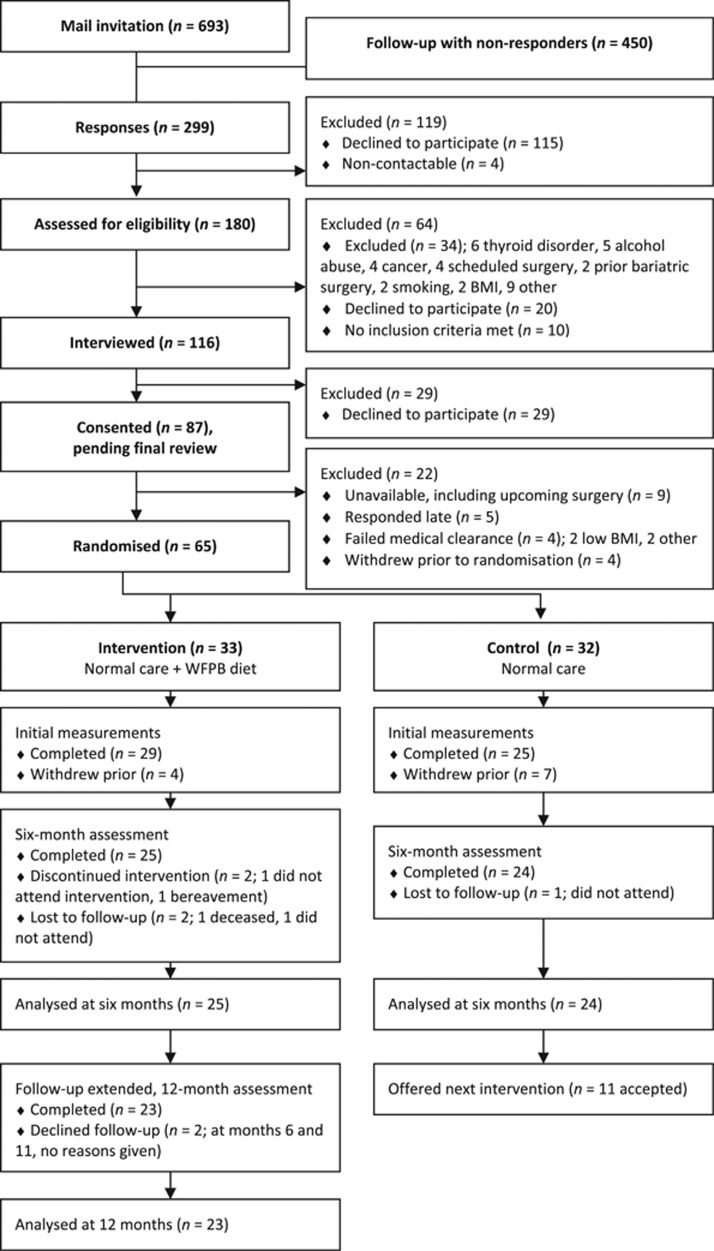
We invited 693 candidates by letter in May 2014 and sent a reminder to 450 non-responders 1 month later. The letter included consent for EMR screening, general and nutritional self-efficacy questionnaires, a question on self-esteem, and three questions on readiness for change.31, 32, 33 Doctors reviewed the EMR and confirmed eligibility. The research coordinator conducted 116 interviews, and explained randomisation, the WFPB diet and showed examples of appropriate meals. Candidates listed the benefits and downsides of allocation to either trial group before providing written consent. We randomised 65 participants total (Figure 1).
Figure 1.
Patient flow.
Intervention
Intervention participants followed a low-fat plant-based diet (approximately 7–15% total energy from fat).13 We chose a low-fat iteration of the plant-based diet as this has been shown with previous research to achieve optimal outcomes, especially for heart disease and weight loss.13, 14, 17, 18 This dietary approach included whole grains, legumes, vegetables and fruits. Participants were advised to eat until satiation. We placed no restriction on total energy intake. Participants were asked to not count calories. We provided a ‘traffic-light' diet chart to participants outlining which foods to consume, limit or avoid (Supplementary Table S1). We encouraged starches such as potatoes, sweet potato, bread, cereals and pasta to satisfy the appetite. Participants were asked to avoid refined oils (e.g. olive or coconut oil) and animal products (meat, fish, eggs and dairy products). We discouraged high-fat plant foods such as nuts and avocados, and highly processed foods. We encouraged participants to minimise sugar, salt and caffeinated beverages. We provided 50 μg daily vitamin B12 (methylcobalamin) supplements. The intervention group attended 2-h evening sessions twice-weekly for 12 weeks. We ran sessions at a local polytechnic, incorporating a chef-guided cooking tutorial and presentation by doctors, with a discussion. Programme outline provided (Supplementary Table S2). Special events included screening the documentary 'Forks Over Knives' and an accompanying film endorsing the WFPB diet; discussion sessions; restaurant meals; quiz night; potlucks; and graduation ceremony. Both intervention and control group participants received $40 petrol vouchers to cover travel costs and received a birthday card along with a voucher redeemable for a native plant.
Data collection and measurements
After enrolment was completed, both groups completed the same questionnaires. We used the Big Five Inventory (BFI 44) personality assessment for traits associated with adherence.34, 35 We used the Short Form 36 health survey version 2 (SF-36v2) to measure self-perceived health status. For diet and exercise, we used 3-day recall forms to track dietary indiscretions and exercise. We averaged daily exercise scores using participant reported exertion (Borg Rating of Perceived Exertion scale) multiplied by minutes of exercise.36 We asked four questions to assess food enjoyment, and calculated food spending by amount divided by frequency to get the cost per day. We counted regular medications from the EMR, excluding as needed (PRN) medications except for glyceryl trinitrate. We discussed prescribing with general practitioners, but general practitioners made all prescribing decisions. We used an online risk assessment (CVD RA) calculator to estimate the 5-year risk of a cardiovascular event.37, 38 We used the Behavior Change Technique Taxonomy to classify aspects of the intervention (Supplementary Table S3).39 The research coordinator performed measurements using the same clinic and equipment, with intervention and control measured 1 week apart. Participants removed shoes and outer clothing. We measured blood pressure (BP) after 5 min seated using the automated digital Pro 3400 BP device (Welch Allyn, Auckland, New Zealand) on the left arm. We then measured height, weight, waist circumference (WC) and a second BP reading. We measured height standing using a wall-mounted stadiometer and weighed participants using a calibrated medical scale (Wedderburn model WM202, Napier, New Zealand). We measured WC standing beside the participant, pulled snug at the height of the navel. T-Lab Gisborne conducted all blood testing. We asked participants to fast for 12 h prior. General chemistry and lipids were measured on the COBAS c6000 (Roche Diagnostics, Auckland, New Zealand), and HbA1c on the D-10 (Bio-Rad Laboratories, Auckland, New Zealand).
Outcomes
The primary outcomes were BMI and cholesterol. Secondary outcomes included changes in medication usage, quality of life, cardiovascular risk factors, cardiovascular events, or progression to surgery, and transfer to a higher level of care. The initial end point was 6 months. We measured personality inventory for factors associated with adherence, and collected data on any harms.
Minor changes to trial design
At the 6-month end point, we observed significant differences between the intervention and control groups, and we offered the intervention to the control group. Ethics approval was obtained to extend follow-up to 3 years total, and the protocol was updated.
Randomisation
We randomised participants in the order of interview by 1:1 sequence from random.org. The allocation was passed to another researcher who assigned groups. We randomised five married, partnered and related pairs together.
Blinding
It was not feasible to blind participants. The researcher performing measurements was aware of allocation. The participants' usual health-care providers were not informed of allocation, although they could ask participants. The statistician was blinded.
Sample size and analysis
We assumed an 80% chance of demonstrating an effect on cholesterol and BMI at a confidence level of 95% (P<0.05), based on previous research.40 Sample size calculation indicated 30 participants per group. Allowing for a 30% dropout rate, we sought 40 participants per group. However, due to time constraints we started with 33 intervention and 32 control group participants. All predefined outcomes were analysed using the pairwise deletion method. We additionally analysed a subgroup that excluded intervention dropouts for between-group differences in total cholesterol. All t-tests were two-tailed. Comparison of results between the two groups were analysed using unpaired t-test, after performing an f-test to determine whether the groups of results had variances that were not significantly different. One set of intergroup differences came close to an unequal variance; however, analysis on the basis of an unequal variance did not change the significance of the result. Statistics were analysed using an external blinded statistician, not otherwise involved in the study, using Stata (College Station, TX, USA).
Results
Losses and exclusions
During the research, one intervention participant died in a motor vehicle accident at week 19. One control group participant reportedly began a plant-based diet from week 6 and continued in the control group.
Results
Of the 693 total people invited by mail, 65 (9.4%) were randomised to either intervention or control. At the 6-month assessment 49 of 65 (75.4%) participants were followed up: 25 (76%) of the intervention group and 24 (75%) of the control. From the intervention group 23 (70%) were followed up at 1 year (Figure 1). Baseline characteristics are available in Table 1.
BMI end point
The primary outcome of BMI change was available for 25 (76%) participants in the intervention group and 24 (75%) in the control at 6 months. Individual BMI changes over time are shown in Supplementary Figure S1. Intervention and between-group reductions in BMI and weight were statistically significant at all measurement points (all P<0.0001, unless stated) (Tables 2 and 4). At 6 months mean intervention BMI reduction was 4.4 (range 0.4–7.4, 95% confidence interval (CI) 3.7–5.1) kg m−2, and at 12 months this was 4.2 (range 0.5–8.3, 95% CI 3.4–5) kg m−2. From 6 to 12 months intervention BMI increased non-significantly by 0.4 (range −1.3 to 4, 95% CI −0.1 to 0.9, P=0.12) kg m−2. For weight, intervention reduction at 6 months was 12.1 (range 1.4–27.3, 95% CI 9.9–14.3) kg, and at 12 months was 11.5 (range 1.6–28.3, 95% CI 9–14) kg. Within the control group, there were no significant reductions in BMI at 3 (P=0.2) or 6 months (P=0.18) (Table 3). At 6 months the between-group analyses showed differences of 3.9 (95% CI±1) kg m−2, and 10.6 (95% CI±2.9) kg, which favoured the intervention.
Table 2. Intervention group differences in outcomes at 3 (programme end), 6 and 12 months, n=33 a.
| Measurement time (months) |
Mean value |
Within-group difference |
P-value |
|||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Baseline | 3 | 6 | 12 | 0–3 | 0–6 | 0–12 | 0–3 | 0–6 | 0–12 | |
| Clinical measures | ||||||||||
| Weight (kg) | 94.8 (6.4) | 86.7 (6) | 82.9 (6.1) | 82.7 (6.8) | −8.6 (1.2)**** | −12.1 (2.2)**** | −11.5 (2.5)**** | <0.0001 | <0.0001 | <0.0001 |
| BMI (kg m−2) | 34.5 (1.6) | 31.5 (1.7) | 30.2 (1.6) | 30.2 (1.7) | −3.1 (0.3)**** | −4.4 (0.7)**** | −4.2 (0.8)**** | <0.0001 | <0.0001 | <0.0001 |
| Cholesterol (mmol l−1) | 5.4 (0.5) | 4.5 (0.4) | 4.7 (0.4) | 5 (0.6) | −1 (0.4)*** | −0.7 (0.4)** | −0.5 (0.5)* | <0.001 | <0.01 | 0.05 |
| Triglycerides | 1.6 (0.3) | 1.8 (0.4) | 1.9 (0.5) | 1.8 (0.5) | 0.2 (0.3) | 0.3 (0.3)* | 0.3 (0.5) | 0.18 | 0.05 | 0.24 |
| LDL | 3.4 (0.4) | 2.5 (0.3) | 2.6 (0.3) | 3 (0.5) | −0.9 (0.4)**** | −0.8 (0.3)*** | −0.6 (0.4)* | <0.0001 | <0.001 | 0.01 |
| HDL | 1.3 (0.1) | 1.1 (0.1) | 1.2 (0.1) | 1.3 (0.1) | −0.2 (0.1)**** | −0.2 (0.1)** | −0.1 (0.2) | <0.0001 | <0.01 | 0.38 |
| Total:HDL (ratio) | 4.3 (0.4) | 4.6 (0.5) | 4.6 (1.1) | 3.9 (0.6) | 0.1 (0.5) | 0.3 (1) | −0.3 (0.5) | 0.67 | 0.49 | 0.33 |
| Waist circumference (cm) | 108 (4) | 101 (4) | 98 (4) | 99 (4) | −7 (2)**** | −10 (2)**** | −9 (3)**** | <0.0001 | <0.0001 | <0.0001 |
| Systolic BP (mm Hg) | 133 (6) | 130 (5) | 132 (6) | 142 (8) | -4 (6) | −2 (6) | 7 (8) | 0.19 | 0.44 | 0.06 |
| Diastolic BP (mm Hg) | 81 (3) | 81 (3) | 82 (3) | 83 (4) | −1 (3) | 0 (3) | 1 (4) | 0.67 | 0.79 | 0.51 |
| HbA1c (mmol mol−1) | 42 (3) | 38 (3) | 39 (3) | 37 (4) | −4 (2)**** | −3 (2)** | −5 (2)**** | <0.0001 | <0.01 | <0.0001 |
| Creatinine (μmol l−1) | 73 (6) | 66 (5) | 63 (5) | 64 (6) | −7 (3)*** | −11 (4)**** | −9 (4)**** | <0.001 | <0.0001 | <0.0001 |
| CVD RA (% 5-year risk) | 11.7 (2.5) | 11.1 (2.4) | 11.2 (2.4) | 11.7 (2.8) | −0.4 (0.3)* | −0.3 (0.4) | 0 (0.4) | 0.02 | 0.08 | 0.85 |
| Questionnaires | ||||||||||
| SF-36 Physical component summary | 47 (3) | 55 (2) | 55 (2) | 55 (2) | 7 (3)*** | 7 (3)**** | 8 (3)*** | <0.001 | <0.0001 | <0.001 |
| SF-36 Mental component summary | 52 (2) | 55 (2) | 56 (2) | 54 (2) | 4 (2)** | 4 (3)** | 3 (3)* | <0.01 | <0.01 | 0.02 |
| Dietary indiscretions | 26 (3) | 1 (1) | 3 (1) | 5 (1) | −26 (4)**** | −24 (3)**** | −22 (4)**** | <0.0001 | <0.0001 | <0.0001 |
| Exercise | 20 (9) | 35 (13) | 23 (10) | 32 (18) | 14 (15) | 3 (12) | 13 (20) | 0.06 | 0.64 | 0.18 |
| Food enjoyment | 12 (1) | 13 (1) | 13 (1) | 13 (1) | 0 (1) | 1 (1)* | 1 (1) | 0.43 | 0.02 | 0.14 |
| Food cost | 23 (5) | 24 (6) | 22 (4) | 20 (6) | 2 (8) | −1 (4) | −3 (5) | 0.53 | 0.54 | 0.19 |
| General self-efficacy | 32 (1) | 33 (3) | 34 (1) | 34 (2) | 1 (3) | 2 (2)* | 2 (2)* | 0.53 | 0.03 | 0.05 |
| Nutritional self-efficacy | 15 (1) | 17 (1) | 17 (1) | 16 (1) | 2 (1)*** | 2 (1)** | 1 (1)* | <0.001 | <0.01 | 0.05 |
| Self-esteem | 2.4 (0.3) | 2.1 (0.4) | 2 (0.3) | 2.1 (0.4) | −0.3 (0.4) | −0.4 (0.4)* | −0.2 (0.5) | 0.09 | 0.04 | 0.31 |
Abbreviations: HDL, high-density lipoprotein cholesterol; LDL, low-density lipoprotein cholesterol.
Values are means (95% CI). Paired, two-tailed t-tests were performed for within-group comparisons; ****P<0.0001, ***P<0.001, **P<0.01, *P<0.05.
Table 4. Differences in outcomes between intervention and control groups at 3 and 6 monthsa.
| Measurement time (months) |
Differences in change, mean |
P-value |
||
|---|---|---|---|---|
| 0–3 | 0–6 | 0–3 | 0–6 | |
| Clinical measures | ||||
| Weight (kg) | −7.5 (2) **** | −10.6 (2.9) **** | <0.0001 | <0.0001 |
| BMI (kg m−2) | −2.7 (0.7) **** | −3.9 (1) **** | <0.0001 | <0.0001 |
| Cholesterol (mmol l−1) | −0.7 (0.5) * | −0.5 (0.5) | 0.01 | 0.10 |
| Triglycerides | 0.2 (0.4) | 0.2 (0.5) | 0.29 | 0.32 |
| LDL | −0.4 (0.5) | −0.4 (0.5) | 0.15 | 0.12 |
| HDL | −0.3 (0.1) **** | −0.2 (0.1) **** | <0.0001 | 0.001 |
| Total:HDL (ratio) | 0.4 (0.6) | 0.6 (1.1) | 0.18 | 0.28 |
| Waist circumference (cm) | −7 (2) **** | −10 (4) *** | <0.0001 | <0.0001 |
| Systolic BP (mm Hg) | −2 (9) | 2 (8) | 0.57 | 0.63 |
| Diastolic BP (mm Hg) | −3 (4) | 0 (4) | 0.18 | 0.84 |
| HbA1c (mmol mol−1) | −6 (2) **** | −5 (3) **** | <0.0001 | <0.001 |
| Creatinine (μmol l−1) | −5 (4) * | −9 (6) ** | 0.01 | <0.01 |
| CVD RA (% 5-year risk) | −0.6 (0.4) * | −0.5 (0.5) | 0.02 | 0.06 |
| Questionnaires | ||||
| SF-36 Physical component summary | 6 (4) ** | 4 (4) * | <0.01 | 0.03 |
| SF-36 Mental component summary | 4 (4) | 6 (4) ** | 0.08 | <0.01 |
| Dietary indiscretions | −23 (5) **** | −20 (4) **** | <0.0001 | <0.0001 |
| Exercise | 15 (29) | 12 (20) | 0.29 | 0.23 |
| Food enjoyment | 0 (1) | 1 (1) | 0.90 | 0.26 |
| Food cost | 2 (9) | 4 (6) | 0.69 | 0.21 |
| General self-efficacy | 2 (4) | 3 (3) * | 0.23 | 0.01 |
| Nutritional self-efficacy | 4 (1) **** | 4 (2) **** | <0.0001 | <0.0001 |
| Self-esteem | −0.5 (0.4) * | −0.8 (0.5) ** | 0.03 | <0.01 |
Values are presented as means (95% CI). Unpaired t-tests were performed for between-group differences (P-values). Asterisks for P-values; ****P<0.0001, ***P<0.001, **P<0.01, *P<0.05. Calculated as (differences in intervention compared with baseline)–(differences in control compared with baseline), i.e. negative difference represent greater intervention reduction compared with control. Negative scores for dietary indiscretions and self-esteem favour intervention. Positive scores for SF-36 summaries, exercise, food enjoyment, general self-efficacy and nutritional self-efficacy favour intervention. Abbreviations: HDL, high-density lipoprotein cholesterol; LDL, low-density lipoprotein cholesterol.
Table 3. Control group differences in outcome at 3 and 6 months, n=32 a.
| Measurement time (months) |
Mean value |
Within-group difference |
P-value |
||||
|---|---|---|---|---|---|---|---|
| Baseline | 3 | 6 | 0 –3 | 0–6 | 0–3 | 0–6 | |
| Clinical measures | |||||||
| Weight (kg) | 96.9 (7.4) | 95.3 (7.7) | 94.1 (7) | −1.2 (1.7) | −1.6 (2.1) | 0.16 | 0.13 |
| BMI (kg m−2) | 34.2 (2.3) | 33.5 (2.4) | 33.2 (2.2) | −0.4 (0.6) | −0.5 (0.8) | 0.2 | 0.18 |
| Cholesterol (mmol l−1) | 5.5 (0.6) | 5.3 (0.8) | 5.2 (0.7) | −0.3 (0.2)* | −0.3 (0.4) | 0.02 | 0.15 |
| Triglycerides | 1.4 (0.3) | 1.3 (0.5) | 1.5 (0.5) | 0 (0.2) | 0.1 (0.3) | 0.88 | 0.43 |
| LDL | 3.5 (0.5) | 3.1 (0.7) | 3.1 (0.6) | −0.5 (0.4)** | −0.4 (0.3)* | <0.01 | 0.02 |
| HDL | 1.4 (0.2) | 1.5 (0.3) | 1.5 (0.2) | 0.1 (0.1) | 0.1 (0.1) | 0.07 | 0.11 |
| Total:HDL (ratio) | 4.2 (0.5) | 4.1 (1) | 4.2 (0.8) | −0.3 (0.4) | −0.2 (0.4) | 0.13 | 0.21 |
| Waist circumference (cm) | 110 (5) | 110 (5) | 110 (5) | −1 (2) | 0 (3) | 0.37 | 0.96 |
| Systolic BP (mm Hg) | 132 (7) | 131 (6) | 127 (7) | −1 (7) | −4 (7) | 0.7 | 0.21 |
| Diastolic BP (mm Hg) | 78 (3) | 81 (3) | 78 (3) | 2 (3) | 0 (3) | 0.13 | 0.99 |
| HbA1c (mmol mol−1) | 37 (2) | 39 (3) | 39 (3) | 2 (1)* | 2 (1)** | 0.01 | <0.01 |
| Creatinine (μmol l−1) | 75 (4) | 73 (6) | 72 (6) | −1 (3) | −2 (4) | 0.35 | 0.32 |
| CVD RA (% 5-year risk) | 12.2 (1.9) | 12 (2.4) | 12.2 (2.1) | 0.1 (0.3) | 0.2 (0.4) | 0.42 | 0.38 |
| Questionnaires | |||||||
| SF-36 Physical component summary | 49 (3) | 50 (4) | 52 (3) | 0 (3) | 3 (2)* | 0.77 | 0.03 |
| SF-36 Mental component summary | 54 (3) | 55 (4) | 53 (3) | 0 (4) | −2 (3) | 0.97 | 0.33 |
| Dietary indiscretions | 22 (4) | 19 (3) | 18 (4) | −3 (4) | −4 (3)* | 0.1 | 0.01 |
| Exercise | 47 (23) | 39 (16) | 36 (24) | −1 (26) | −9 (17) | 0.93 | 0.26 |
| Food enjoyment | 13 (1) | 13 (1) | 13 (1) | 0 (1) | 0 (1) | 0.25 | 0.62 |
| Food cost | 22 (3) | 24 (5) | 19 (5) | 1 (6) | −5 (5)* | 0.84 | 0.03 |
| General self-efficacy | 32 (2) | 31 (3) | 30 (3) | −1 (2) | −1 (2) | 0.25 | 0.19 |
| Nutritional self-efficacy | 16 (1) | 14 (1) | 14 (1) | −2 (1)*** | −2 (1)* | <0.001 | 0.01 |
| Self-esteem | 2.3 (0.3) | 2.3 (0.3) | 2.5 (0.4) | 0.2 (0.3) | 0.3 (0.3)* | 0.16 | 0.04 |
Abbreviations: HDL, high-density lipoprotein cholesterol; LDL, low-density lipoprotein cholesterol.
Values are presented as means (95% CI). Paired, two-tailed t-tests were performed for within-group comparisons; ****P<0.0001, ***P<0.001, **P<0.01, *P<0.05.
Cholesterol end point
The primary outcome of cholesterol change was available for 25 (76%) participants in the intervention group and 23 (72%) in the control at 6 months. Individual cholesterol changes over time are shown in Supplementary Figure S2. Within the intervention group mean reduction in total cholesterol was statistically significant at all time periods, although there was a smaller effect size with time: at month 3 it was 0.95 (95% CI 0.51–1.39, P<0.001) mmol l−1; at month 6 it was 0.71 (95% CI 0.28 to 1.14, P<0.01) mmol l−1; and at month 12 it was 0.55 (95% CI 0.01–1.09, P=0.05) mmol l−1. In the control group we observed a statistically significant mean reduction in total cholesterol at month 3, at 0.28 (95% CI 0.05–0.52, P=0.03) mmol l−1, but this was not significant by month 6, at 0.26 (95% CI −0.10 to 0.62, P=0.15) mmol l−1. Comparing standard care plus dietary programme (intervention) to standard care (control) at month 6, our analysis showed a nonsignificant reduction in total cholesterol at 0.45 (95% CI −0.09 to 1.00, P=0.10). Post hoc subgroup analysis for total cholesterol difference excluding intervention group dropouts showed a significant reduction of 0.56 (95% CI±0.54, P=0.05) mmol l−1, which favoured the intervention. Statistically significant between-group HDL-cholesterol differences were seen from baseline to 6 months at 0.25 (95% CI±0.15, P<0.0001) mmol l−1.
Secondary end points
Medication data were available at 6 months for 62 of 65 (95%) participants via the GP EMR. Control group medications increased from 74 to 80 over 6 months, an 8% increase, and intervention group medication usage decreased from 94 to 74 at 6 months, and to 67 over 12 months: a 29% decrease (Supplementary Table S4).
Cardiovascular risk factors
The CVD RA within the intervention group decreased slightly from baseline to 3 months; 0.4% (95 CI±0.3, P=0.02), and the between-group difference was significant 0.6% (95% CI±0.4, P=0.02). There were no other significant differences observed for CVD RA. The HbA1c between-group differences favoured the intervention, with a reduction of 5 (95% CI±3, P<0.001) mmol mol−1 at 6 months. From baseline to 12 months the intervention average HbA1c reduced by 5 (range −1 to 15, 95% CI±2, P<0.0001) mmol mol−1. For the intervention group, two people with diabetes no longer met diagnostic criteria (i.e. HbA1c ⩾50 mmol mol−1) at both 6 and 12 months. Higher starting HbA1c correlated with a larger subsequent reduction to 3, 6 and 12 months (correlation tests, P<0.01 or less). Intervention WC reduced compared with baseline at all time periods (Table 2). No changes were seen in the control group (Table 3), and between-group differences demonstrated 10 (95% CI±4, P<0.0001) cm greater mean intervention reduction at 6 months. There were no transfers to higher-level care or acute admissions for cardiac-related care for any participant during the first 12 months of the research.
Quality of life and other variables
Quality of life showed significant improvements in the intervention group for all measurement periods in both the ‘physical component summary' and the ‘mental component summary' (Table 2). The control group showed significant improvement to 6 months with the physical component summary (P=0.03) (Table 3). Between-group differences favouring intervention were significant at 6 months for both the physical component summary (P=0.03) and the mental component summary (P<0.01) (Table 4). At 6 months no significant between-group differences were seen for: average daily exercise, food enjoyment or food costs (Table 4). Statistically significant differences favouring the intervention were seen at 6 months for general self-efficacy (P=0.01), nutritional self-efficacy (P<0.0001) and self-esteem (P<0.01).
Adherence
Average attendance for intervention evening sessions was 79%. Dietary indiscretions (diet) over 3 days were used as adherence measure, and intervention BMI change from 0 to 12 months was correlated with diet at 3, 6 and 12 months (correlation tests: P<0.0001, P=0.04, P<0.001, respectively). Baseline diet was not related to 12-month BMI change (correlation test, P=0.84). In the intervention group, indiscretions increased significantly from 1 (95% CI±1) at 3 months to 3 (±1) at 6 months (paired t-test; P<0.0001), and then increased significantly to 5 (±1) at 1 year (6–12 month increase paired t-test; P=0.001). Intervention adherence vs BMI reduction from 0 to 12 months is shown in Supplementary Figure S3. In the control group, we observed a significant decrease in dietary indiscretions from baseline to 6 months (Table 3), although these were much smaller than the intervention group (Table 2). In the control group there was no correlation between BMI change from baseline to 6 months and dietary indiscretions at 0, 3 or 6 months (correlation tests: P=0.38; 0.88 and 0.57, respectively).
Harms
No serious harms relating to the intervention were reported. One intervention participant with a diagnosis of type 2 diabetes reported hypoglycaemia from week 1 consuming the WFPB diet, and his general practitioner reduced, and then later stopped his insulin. Two intervention participants developed low serum vitamin B12, which normalised with supplementation. At month 5, an intervention group participant underwent cholecystectomy for cholecystitis.
Discussion
This randomised controlled trial compared a 12-week WFPB dietary programme to normal care alone. The intervention led to significant and sustained BMI and weight reduction at all measurement points compared with the control group. To the best of our knowledge, there are no randomised controlled trials that have achieved a greater average weight loss over a 6- or 12-month period, without mandating regular exercise or restricting total caloric intake.9, 10, 41 The key difference between this trial and other approaches to weight loss was that participants were informed to eat the WFPB diet ad libitum and to focus efforts on diet, rather than increasing exercise. The mechanism for this is likely the reduction in the energy density of the food consumed (lower fat, higher water and fibre).42 Multiple intervention participants stated 'not being hungry' was important in enabling adherence. Intervention participants were highly adherent with the dietary changes, although this decreased with time. Diet at 3 months correlated with weight loss at 12 months, but starting diet did not. These findings suggest an audited diet diary may be useful to predict success with a WFPB diet, and that those starting from a typical Western diet could expect similar results.
Our results show a reduction in cholesterol for the intervention group at all measurement points, and in the control at 3 months only. Between-group analysis showed statistically significant differences in cholesterol at 3 months, and at 6 months with subgroup analysis. The ability to detect differences is potentially reduced by intervention group reduction in medications, and a decrease in dietary adherence over time. HbA1c reductions favoured the intervention and all intervention patients with a diabetes diagnosis improved while adherent, and two resolved their condition by HbA1c. At 6 months, the intervention compared with the control had an increased quality of life (SF-36v2), general and nutritional self-efficacy, and self-esteem, without significant changes in food enjoyment, cost or exercise. Total regular medication usage decreased in the intervention group (94 at baseline, 74 at 6 months, 67 at 12 months), and increased in the control group (74 at baseline, 80 at 6 months). CVD RA tools are widely used in New Zealand, and although we saw intervention WC, BMI and HbA1c improve, the between-group CVD RA (which does not account for some of these) did not change significantly. Also, HDL-cholesterol tends to decrease on a plant-based diet, and previous research had shown this 'may not be helpful for predicting cardiovascular risk in individuals consuming a low-fat, plant-based diet'.43 Our analysis corroborates that this tool is not particularly appropriate for those consuming a WFPB diet.
Strengths of this research include randomisation, and the ‘real world' nature of the programme, which involved community-dwelling adults who were provided skills and education but were responsible for their own food choices. A previous survey identified a lack of information as the main barrier to beginning a WFPB diet, and information provision formed a large part of our programme.44 Factors promoting success in the intervention group included the 2-week preparation period, individualised feedback and rapid initial weight loss. Reports from intervention participants suggest family and acquaintances themselves benefitted from exposure to the WFPB diet.
Limitations include necessarily explaining the WFPB diet to all participants during informed consent, and perhaps as a consequence, we observed a significant improvement with control group dietary indiscretions. Increased testing for normal care participants may have led to more focused treatment, and the observed lipid reductions, and a reduction in effect size. In our research, 7 of 65 (11%) participants had a diagnosis of ischaemic heart disease, and we included participants without a necessarily elevated HbA1c or cholesterol, so collectively these could have lessened effect size. As it stands, our average cholesterol reductions were not necessarily as large as those seen with previous research. Other research has also evaluated dietary records in more depth, or used a WFPB diet programme in combination with exercise or relaxation.17, 19, 40 Weaknesses for this research include that the intervention group was not perfectly adherent. The intervention cholesterol drop was largest at measurement points when adherence was highest, and as adherence decreased, cholesterol increased, suggesting a dose–response relationship. Consumption of ‘green' category foods was encouraged, but not monitored, although this could be of benefit. Our questions for exercise, food costs and dietary indiscretions involved self-reporting and recall, which could have introduced error. Another source for introducing inaccuracy was using EMR ethnicity data, which may have underrepresented rates of Māori participants. Finally, participant dropouts may have affected results, although they were roughly equal in both groups.
Our programme contrasts with other commonly used approaches: exercise and very-low-calorie diets, or bariatric surgery. Very-low-calorie diets have achieved equal or greater mean weight loss to that seen in our research.45, 46 However, medically supervised liquid ‘meal replacements' are not intended for ongoing use and are associated with 'high costs, high attrition rates, and a high probability of regaining 50% or more of lost weight in 1 to 2 years'.47 Increased risks include gallstones, cold intolerance, hair loss and constipation.46 This contrasts with our research, whereby many in the WFPB diet group improved in the 9 months following the 12-week intervention. The Cochrane review of bariatric surgery shows both greater and lesser reduction in BMI at 12 months compared with our results, although it tends to favour bariatric surgery.48 One recent study with Roux-en-Y gastric bypass showed an increased quality of life after bariatric surgery, but hospitalisation rates were 4–5 times higher than the comparison group.49 The Cochrane review states bariatric surgery studies tend to include young, 'low-risk', mainly female patients and that the 'longer-term impact of surgery on weight loss or comorbidities is unclear'. Because bariatric surgery candidates are motivated for change, they could also be suitable for a WFPB dietary programme. This approach poses no risk of surgical morbidity or mortality but does require more time with patients. A WFPB dietary programme can be utilised in centres where surgery is unavailable, and we estimate cost per patient to be substantially less than surgery.
Reviews comparing the WFPB approach to other diets show similar weight loss at 12 months for low-carbohydrate and low-fat diet approaches.10, 50 Individual studies that combine regular exercise with either unrestricted or energy-restricted low-carbohydrate diets have observed similar weight loss to our intervention at 6 months: 12.0 (95% CI±1.8) kg;51 and at 1 year: 10.9 (95% CI±1.2) kg,52 and 12.2 (includes telemonitoring, 95% CI±1.3) kg reductions.53 However, studies on the effects of low-carbohydrate diets have shown higher rates of all-cause mortality,54 decreased peripheral flow-mediated dilation,55 worsening of coronary artery disease,56 and increased rates of constipation, headache, halitosis, muscle cramps, general weakness and rash.10 Other energy-restricted diets can be effective for weight loss, for example, one study using a 1 500 kcal daily intake, with 50% carbohydrate, 30% fat and 20% protein achieved an average 17.3 (95% CI±1.6) kg reduction in weight at 36 weeks, which is significantly more than our results.57 However, by restricting amount of food eaten, patients are likely to feel hungry, and hunger scores have been shown to predict those at risk of weight regain.58 Low-fat interventions that encourage regular exercise have shown equal weight loss at 1 year with energy-restricted and non-energy-restricted approaches: 10.8 kg (95% CI not available and±1.6, respectively).17, 52
Generalising our results to the community, we felt there were several key differences. Our study population had a higher number of females and a higher mean age. Our rates of Māori participants were less than the Gisborne community and similar to the national average. We would estimate our participants to have a higher than average health literacy. To provide longer-term data, we have extended follow-up to observe the intervention group for 3 years total.
Conclusion
Many patients are interested in making dietary changes, and the WFPB diet can be offered as a safe and effective option for losing weight and obtaining some reduction in cholesterol, without necessarily increasing exercise. The main advantage is in eating to satiation without restricting the amount of food eaten. This small study also showed several improvements with chronic disease risk factors and quality of life, which were largely maintained to 12 months. Future research could identify participants who are currently likely to succeed with a diet change, which could reduce dropout rates and increase effectiveness. Given the low cost of this intervention and the relative benefits of this dietary approach, this could be offered by policy makers and practitioners as promoting weight loss, and suitable for consumption in hospitals.
Acknowledgments
All funding for this research was provided by the following charitable trusts: Tairāwhiti Traditional and Complementary Therapies Research Trust (TTCTRT), the Tairāwhiti Community Services Trust and the J N Williams Memorial Trust. One researcher and author (PMH) is a trustee on TTCTRT, otherwise the funders had no role in study design and conduct; data collection and analysis; decision to publish; or preparation, review and approval of the manuscript. We are indebted to T-lab for substantial reductions in blood tests costs. We gratefully acknowledge Dr McDougall for his support and contribution with ‘The Starch Solution' books. We give thanks to James Cameron and Suzy Amis Cameron for their support and video endorsement. Many thanks to Professor Ross Lawrenson, University of Auckland, for assistance with peer review of the initial ethics application. We thank Patricia Sheehan, clinical librarian at Hauora Tairāwhiti, and Wellington school of Medicine library for research assistance, John Roy and Stephanie Sheppard for statistical analyses, Phil Watson for assisting with an evening session, Gavin Moloney for dietetic advice, Down to Earth Health 2000 and Clinicians for discounted vitamin B12 supplements, and City Medical. We thank EIT Polytechnic, especially staff Karen Johnston, Mark Morrell, Sue Matthews and Jan Mogford. We thank Larry Robb for his contributions as group mentor. We thank Craig Hagan and Jon Rush of Farmhouse Films for their video productions. Thanks to restaurants providing WFPB meals; Morrell's Artisan Bakery, Sofra café, Thai sunshine, Yoko sushi, The Works, and Café 84. NW thanks Health Workforce New Zealand. The New Zealand Northern B Health and Disability Committee approved this study: 14/NTB/37. It was registered prospectively with the Australian New Zealand Clinical Trials Registry: protocol available, trial ID ACTRN12614000395639.
Author contributions
All authors contributed to trial design, monitoring of data collection, and drafting and revision of the paper. NW and LW designed data collection, performed individual patient consults, reviewed EMR and co-founded the research. NW, LW and MS implemented trial and presented group information sessions. MS performed recruitment, performed data collection, cleaned data and checked references. NW and BD contributed to the statistical analysis. NW is the guarantor for the study. All authors had full access to all of the data in the study. NW takes responsibility for the integrity of the data and the accuracy of the data analysis.
Footnotes
Supplementary Information accompanies this paper on the Nutrition & Diabetes website (http://www.nature.com/nutd)
NW is employed by the Royal NZ college of GPs, which is a position funded by Health Workforce New Zealand. MS and NW report being directors/shareholders in Plant Based Lifestyles Ltd, which was initiated after the completion of the BROAD study. BD, NW, MS and PMH report being trustees of the Plant Based New Zealand Health Charitable Trust. PMH reports he is a trustee on the Tairāwhiti Traditional and Complementary Therapies Research Charitable Trust (TTCTRT). LW reports being director/shareholder in Two Zesty Bananas Ltd, which was initiated after the intervention.
Supplementary Material
References
- Finucane MM, Stevens GA, Cowan MJ, Danaei G, Lin JK, Paciorek CJ et al. National, regional, and global trends in body-mass index since 1980: systematic analysis of health examination surveys and epidemiological studies with 960 country-years and 9·1 million participants. Lancet 2011; 377: 557–567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mitchell N, Catenacci V, Wyatt HR, Hill JO. Obesity: overview of an epidemic. Psychiatr Clin N Am 2011; 34: 717–732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- WHO. Obesity and Overweight [Internet]. WHO [cited 19 March 2015]. Available at www.who.int/mediacentre/factsheets/fs311/en/.
- Obesity data and stats [Internet]. Ministry of Health NZ [cited 3 December 2015]. Available at www.health.govt.nz/nz-health-statistics/health-statistics-and-data-sets/obesity-data-and-stats.
- WHO. NCD mortality and morbidity [Internet]. WHO [cited 19 March 2015]. Available at www.who.int/gho/ncd/mortality_morbidity/en/.
- Sarwer DB, Moore RH, Diewald LK, Chittams J, Berkowitz RI, Vetter M et al. The impact of a primary care-based weight loss intervention on quality of life. Int J Obes (Lond) 2013; 37: S25–S30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wider economic and social costs of obesity to New Zealand. 12 February 2015 [cited 19 March 2015]. Available at www.superu.govt.nz/publication/wider-economic-and-social-costs-obesity-new-zealand-discussion-non-health-impacts.
- Atallah R, Filion KB, Wakil SM, Genest J, Joseph L, Poirier P et al. Long-term effects of 4 popular diets on weight loss and cardiovascular risk factors: a systematic review of randomized controlled trials. Circ Cardiovasc Qual Outcomes 2014; 7: 815–827. [DOI] [PubMed] [Google Scholar]
- Makris A, Foster GD. Dietary approaches to the treatment of obesity. Psychiatr Clin N Am 2011; 34: 813–827. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnston BC, Kanters S, Bandayrel K, Wu P, Naji F, Siemieniuk RA et al. Comparison of weight loss among named diet programs in overweight and obese adults: a meta-analysis. JAMA, 2014; 312: 923–933. [DOI] [PubMed] [Google Scholar]
- Newborg B. Walter Kempner and the Rice Diet: Challenging Conventional Wisdom. Carolina Academic Press: Durham, NC, 2011, p 274. [Google Scholar]
- Kempner W, Newborg BC, Peschel RL, Skyler JS. Treatment of massive obesity with rice/reduction diet program. An analysis of 106 patients with at least a 45-kg weight loss. Arch Intern Med 1975; 135: 1575–1584. [PubMed] [Google Scholar]
- McDougall J, Thomas LE, McDougall C, Moloney G, Saul B, Finnell JS et al. Effects of 7 days on an ad libitum low-fat vegan diet: the McDougall Program cohort. Nutr J 2014; 13: 99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Esselstyn CB Jr. Prevent and Reverse Heart Disease: The Revolutionary, Scientifically Proven, Nutrition-Based Cure. Penguin Group, 2008; , p 65. [Google Scholar]
- Tuso PJ, Ismail MH, Ha BP, Bartolotto C. Nutritional update for physicians: plant-based diets. Perm J 2013; 17: 61–66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Esselstyn CB, Gendy G, Doyle J, Golubic M, Roizen MF. A way to reverse CAD? J Fam Pract 2014; 63: 356–364b. [PubMed] [Google Scholar]
- Ornish D, Scherwitz LW, Billings JH, Brown SE, Gould KL, Merritt TA et al. Intensive lifestyle changes for reversal of coronary heart disease. JAMA 1998; 280: 2001–2007. [DOI] [PubMed] [Google Scholar]
- Ferdowsian HR, Barnard ND, Hoover VJ, Katcher HI, Levin SM, Green AA et al. A multicomponent intervention reduces body weight and cardiovascular risk at a GEICO corporate site. Am J Health Promot 2010; 24: 384–387. [DOI] [PubMed] [Google Scholar]
- Kent L, Morton D, Hurlow T, Rankin P, Hanna A, Diehl H. Long-term effectiveness of the community-based Complete Health Improvement Program (CHIP) lifestyle intervention: a cohort study. BMJ Open 2013; 3: e003751. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Turner-McGrievy GM, Barnard ND, Scialli AR. A two-year randomized weight loss trial comparing a vegan diet to a more moderate low-fat diet. Obesity (Silver Spring) 2007; 15: 2276–2281. [DOI] [PubMed] [Google Scholar]
- Berkow SE, Barnard N, Eckart J, Katcher H. Four therapeutic diets: adherence and acceptability. Can J Diet Pract Res 2010; 71: 199–204. [DOI] [PubMed] [Google Scholar]
- Ornish D, Weidner G, Fair WR, Marlin R, Pettengill EB, Raisin CJ et al. Intensive lifestyle changes may affect the progression of prostate cancer. J Urol 2005; 174: 1065–1069. [DOI] [PubMed] [Google Scholar]
- Oppenlander RA. Food Choice and Sustainability: Why Buying Local, Eating Less Meat, and Taking Baby Steps Won't Work. Langdon St Press: Minneapolis, MN, 2013; p 470. [Google Scholar]
- Scarborough P, Appleby PN, Mizdrak A, Briggs ADM, Travis RC, Bradbury KE et al. Dietary greenhouse gas emissions of meat-eaters, fish-eaters, vegetarians and vegans in the UK. Clim Change 2014; 125: 179–192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- FAO. News Article: Key facts and findings [Internet]. [cited 16 November 2015]. Available at www.fao.org/news/story/en/item/197623/icode/.
- Goodland R, Anhang J. Livestock and Climate Change [Internet]. World Watch Institute, 2009 [cited 4 December 2015]. Available at http://www.worldwatch.org/files/pdf/Livestock%20and%20Climate%20Change.pdf.
- Steinfeld H, Gerber P, Wassenaar T, Castel V, Rosales M, de Haan C Livestock's long shadow —environmental issues and options [Internet]. Food and Agriculture Organization of the United Nations, 2006 [cited 29 March 2015]. Available at ftp.fao.org/docrep/fao/010/A0701E/A0701E00.pdf.
- Springmann M, Godfray HCJ, Rayner M, Scarborough P. Analysis and valuation of the health and climate change cobenefits of dietary change. Proc Natl Acad Sci USA 2016; 113: 4146–4151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Atkinson J, Salmond C, Crampton P. NZDep2013 Index of Deprivation [Internet]. Socioeconomic Deprivation Indexes: NZDep and NZiDep, Department of Public Health [cited 18 April 2015]. Available at www.otago.ac.nz/wellington/departments/publichealth/research/hirp/otago020194.html.
- Parliamentary Library Parliament L and P. Obesity and diabetes in New Zealand [Internet]. 2014 Oct [cited 25 June 2015]. Available at www.parliament.nz/en-nz/parl-support/research-papers/00PLLawRP2014041/obesity-and-diabetes-in-new-zealand.
- Schwarzer R, Jerusalem M. Causal and Control Beliefs. Measures in Health Psychology: A User's Portfolio. NFER-Nelson: Windsor, England, 1995, pp; 35–37. [Google Scholar]
- Schwarzer R, Renner B. Social-cognitive predictors of health behavior: action self-efficacy and coping self-efficacy. Health Psychol 2000; 19: 487–495. [PubMed] [Google Scholar]
- Bandura A. Self-efficacy: toward a unifying theory of behavioral change. Psychol Rev 1977; 84: 191–215. [DOI] [PubMed] [Google Scholar]
- John OP, Naumann LP, Soto CJ. Paradigm shift to the integrative big-five trait taxonomy: history, measurement, and conceptual issues. Handbook of Personality: Theory and Research. Guilford Press: New York, NY, 2008, pp; 114–158. [Google Scholar]
- John OP, Donahue EM, Kentle RL. The Big Five Inventory-Versions 4a and 54. University of California, Berkeley, Institute of Personality and Social Research: Berkeley, CA, 1991. [Google Scholar]
- Impellizzeri FM, Rampinini E, Coutts AJ, Sassi A, Marcora SM. Use of RPE-based training load in soccer. Med Sci Sports Exerc 2004; 36: 1042–1047. [DOI] [PubMed] [Google Scholar]
- The New Zealand Society for the Study of Diabetes. CVD risk assessment for people with type 2 diabetes in New Zealand [Internet] [cited 1 June 2016]. Available at http://www.nzssd.org.nz/cvd/.
- New Zealand Primary Care Handbook 2012 [Internet]. Ministry of Health NZ [cited 8 April 2016]. Available at www.health.govt.nz/publication/new-zealand-primary-care-handbook-2012.
- Michie S, Richardson M, Johnston M, Abraham C, Francis J, Hardeman W et al. The behavior change technique taxonomy (v1) of 93 hierarchically clustered techniques: building an international consensus for the reporting of behavior change interventions. Ann Behav Med 2013; 46: 81–95. [DOI] [PubMed] [Google Scholar]
- Esselstyn CB, Ellis SG, Medendorp SV, Crowe TD. A strategy to arrest and reverse coronary artery disease: a 5-year longitudinal study of a single physician's practice. J Fam Pract 1995; 41: 560–568. [PubMed] [Google Scholar]
- Barnard ND, Levin SM, Yokoyama Y. A systematic review and meta-analysis of changes in body weight in clinical trials of vegetarian diets. J Acad Nutr Diet 2015; 115: 954–969. [DOI] [PubMed] [Google Scholar]
- Ello-Martin JA, Roe LS, Ledikwe JH, Beach AM, Rolls BJ. Dietary energy density in the treatment of obesity: a year-long trial comparing 2 weight-loss diets. Am J Clin Nutr 2007; 85: 1465–1477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kent L, Morton D, Rankin P, Ward E, Grant R, Gobble J et al. The effect of a low-fat, plant-based lifestyle intervention (CHIP) on serum HDL levels and the implications for metabolic syndrome status – a cohort study. Nutr Metab (Lond) 2013; 10: 58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lea EJ, Crawford D, Worsley A. Public views of the benefits and barriers to the consumption of a plant-based diet. Eur J Clin Nutr 2006; 60: 828–837. [DOI] [PubMed] [Google Scholar]
- Johansson K, Neovius M, Hemmingsson E. Effects of anti-obesity drugs, diet, and exercise on weight-loss maintenance after a very-low-calorie diet or low-calorie diet: a systematic review and meta-analysis of randomized controlled trials. Am J Clin Nutr 2014; 99: 14–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tsai AG, Wadden TA. The evolution of very-low-calorie diets: an update and meta-analysis. Obesity (Silver Spring) 2006; 14: 1283–1293. [DOI] [PubMed] [Google Scholar]
- Tsai AG, Wadden TA. Systematic review: an evaluation of major commercial weight loss programs in the United States. Ann Intern Med 2005; 142: 56–66. [DOI] [PubMed] [Google Scholar]
- Colquitt JL, Pickett K, Loveman E, Frampton GK. Surgery for weight loss in adults. Cochrane Database Syst Rev 2014; 8: CD003641. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gribsholt SB, Pedersen AM, Svensson E, Thomsen RW, Richelsen B. Prevalence of self-reported symptoms after gastric bypass surgery for obesity. JAMA Surg 2016; 6: 1–9. [DOI] [PubMed] [Google Scholar]
- Nordmann AJ, Nordmann A, Briel M, Keller U, Yancy WS, Brehm BJ et al. Effects of low-carbohydrate vs low-fat diets on weight loss and cardiovascular risk factors: a meta-analysis of randomized controlled trials. Arch Intern Med 2006; 166: 285–293. [DOI] [PubMed] [Google Scholar]
- Yancy WS, Olsen MK, Guyton JR, Bakst RP, Westman EC. A low-carbohydrate, ketogenic diet versus a low-fat diet to treat obesity and hyperlipidemia: a randomized, controlled trial. Ann Intern Med 2004; 140: 769–777. [DOI] [PubMed] [Google Scholar]
- Foster GD, Wyatt HR, Hill JO, Makris AP, Rosenbaum DL, Brill C et al. Weight and metabolic outcomes after 2 years on a low-carbohydrate versus low-fat diet. Ann Intern Med 2010; 153: 147–157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Luley C, Blaik A, Götz A, Kicherer F, Kropf S, Isermann B et al. Weight loss by telemonitoring of nutrition and physical activity in patients with metabolic syndrome for 1 year. J Am Coll Nutr 2014; 33: 363–374. [DOI] [PubMed] [Google Scholar]
- Noto H, Goto A, Tsujimoto T, Noda M. Low-carbohydrate diets and all-cause mortality: a systematic review and meta-analysis of observational studies. PLoS ONE 2013; 8: e55030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schwingshackl L, Hoffmann G. Low-carbohydrate diets impair flow-mediated dilatation: evidence from a systematic review and meta-analysis. Br J Nutr 2013; 110: 969–970. [DOI] [PubMed] [Google Scholar]
- Fleming RM. The effect of high-protein diets on coronary blood flow. Angiology 2000; 51: 817–826. [DOI] [PubMed] [Google Scholar]
- Andreou E, Philippou C, Papandreou D. Effects of an intervention and maintenance weight loss diet with and without exercise on anthropometric indices in overweight and obese healthy women. Ann Nutr Metab 2011; 59: 187–192. [DOI] [PubMed] [Google Scholar]
- Pasman WJ, Saris WH, Westerterp-Plantenga MS. Predictors of weight maintenance. Obes Res 1999; 7: 43–50. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.