Neighborhood characteristics have consistently been linked to physical and mental health outcomes and overall mortality (1, 2). Specifically, individuals living in neighborhood environments of lower socioeconomic status and/or with higher levels of adverse characteristics (e.g., neighborhood disorder, or lower levels of safety or social cohesion) have been found to have higher body mass index (BMI) (3, 4), diabetes (5), and hypertension (6, 7), among other risk factors. However, the specific mechanisms linking neighborhood characteristics to residents’ health outcomes are not fully understood.
In complementary research on sleep quality and duration, the role of sleep has been recognized as an important risk factor for a host of adverse health outcomes including obesity, poor self-reported health, physical limitations, poorer immune functioning, and cardiometabolic dysregulation (8–11). Because of its influence on metabolic and cardiovascular processes (12) and links to depressive symptoms and suicide (13, 14), sleep could also serve as an important, understudied mechanism through which neighborhood contexts influence poorer physical and mental health (15–18).
In fact, several recent studies found that more negative assessments of perceived neighborhood characteristics were associated with poorer sleep quality (15–17, 19, 20). For example, one six-country study found that lower perceived neighborhood safety was associated with poorer sleep quality, insomnia, and sleepiness (21). Several prior studies have analyzed associations of noise/traffic (22–25) with both subjective and objective sleep measures and exposure to violence (26) as contributors to poorer self-reported sleep quality and/or decreased sleep duration.
Most prior studies have examined a single aspect of neighborhoods (e.g., disorder or social cohesion), and have focused on either perceived or objective assessments of neighborhood characteristics, but not both. In addition, the existing literature has utilized samples with limited racial/ethnic diversity, with scant research focused on the most high-risk populations, such as African Americans in lower SES neighborhoods. Yet African Americans face disproportionate risk for sleep problems, including obstructive sleep apnea, worse sleep quality, shorter sleep duration, and decreased sleep efficiency (27–30), as well as cardiometabolic disorders (31, 32), and are at greater risk of residing in impoverished neighborhoods compared to non-Hispanic Whites, even after accounting for individual-level socioeconomic status (SES) (33). Finally, the extant literature has not evaluated potential mechanisms that may account for associations between neighborhood characteristics and sleep.
The current analysis addressed several of the limitations in prior literature on associations of neighborhood characteristics and sleep quality by: 1.) examining associations of multiple indicators of neighborhood characteristics, including both perceived and objective measures; 2.) enrolling a large sample of African Americans in neighborhoods of lower SES; and 3.) exploring a potential mechanism that may link neighborhood characteristics to sleep. Specifically, consistent with prevailing theories concerning potential pathways linking neighborhood contexts with sleep(17), we examined psychological distress as a potential mediator of observed associations.
We hypothesized that lower perceived levels of neighborhood safety, social cohesion, satisfaction, and infrastructure (e.g., sidewalks present, streets well-lit at night), as well as more negative objectively-measured neighborhood characteristics (e.g., crime rates, pedestrian safety measures, land use) are associated with poorer perceived sleep quality (assessed by participant diaries), after adjustment for potential confounds, including individual-level SES. We further hypothesized that associations between higher levels of adverse neighborhood characteristics and poorer sleep quality would be mediated by psychological distress.
Methods
The data for the current analyses come from the PHRESH Zzz Study (Pittsburgh Hill/Homewood Research on Neighborhoods, Sleep, and Health), which was designed to investigate to what extent changes in the neighborhood built and social environment result in changes in health behaviors and risk factors relevant to obesity-related morbidity in two lower-income neighborhoods in Pittsburgh over time. The sample includes randomly selected households from two socioeconomically similar urban neighborhoods, in which more than 90% of residents were African American in the 2000 Census. One neighborhood is scheduled to undergo various neighborhood revitalization initiatives, including increased retail and business development, and renovation of green space for recreational activities. Data for the current analyses were collected before major renovations took place and included an in-person household survey (e.g., sociodemographics, psychological distress, perceived neighborhood characteristics), sleep diaries, and objective “audits” of neighborhood street segments and crime data from the Pittsburgh Police Department.
Sleep
Participants were asked to complete a paper sleep diary each morning after waking up for a 7-day period in which they rated their sleep quality, our primary outcome of interest, on a 5-point Likert-scale from “very bad” to “very good.” These subjective ratings were used to assess sleep quality. Information on use of medications that may affect sleep was also assessed using as part of the sleep diary component of the study, and was analyzed in sensitivity analyses which excluded individuals who were using any medications that could affect sleep. Specifically, they were asked, “Did you take any sleep medication to help you fall asleep tonight? (yes or no).” To be included in the analytic sample, participants were required to have at least four days of reporting on sleep quality, which were averaged over the total days of recording.
Sociodemographic characteristics
Participants provided information on their individual-annual household income, which served as the indicator and included as a covariate in all models. Race/ethnicity was derived from two self-reported items, one on race and the other on ethnicity (i.e., Hispanic, non-Hispanic). Additional demographic measures included: age (date of birth), gender, marital/cohabitation status, and presence of any children in the home. Interviewers measured height to the nearest eighth-inch using a carpenter’s square (triangle) and an eight-foot folding wooden ruler marked in inches. Interviewers measured weight to the nearest tenth-pound using a Seca Robusta 813 digital scale. BMI (kg/m2) was calculated from participants’ height and weight.
Psychological distress
The Kessler 6 (K6) is a well-validated self-report instrument to measure psychological distress. It was included in the current study because it is well-validated instrument that assesses general distress symptoms, rather than specific clinical symptoms associated with a particular disorder (34). Moreover, the measure has previously been found to be strongly associated with socioeconomic status and other demographic characteristics, as well as a host of adverse physical and mental health outcomes (35). The questionnaire asked respondents, “During the last 30 days, about how often did …” “…you feel hopeless?”; “…you feel restless or fidgety?”; “…you feel that everything was an effort?” “…you feel nervous?”; “… you feel worthless?” Responses included: “most of the time,” “some of the time,” “a little of the time,” and “none of the time.” K6 scores were added to models to determine the extent to which psychological distress explains observed associations between neighborhood characteristics and sleep quality.
Perceived neighborhood characteristics
We included four measures of perceived neighborhood characteristics: social cohesion, perceived safety, neighborhood satisfaction, and neighborhood infrastructure. Social cohesion was assessed with a five-item Likert-scale, ranging from 1 (strongly agree) to 5 (strongly disagree). This scale has been validated previously (36), and is coded such that higher scores reflect greater social cohesion. Participants were asked how strongly they agree or disagree with various statements (e.g., “People around here are willing to help their neighbors;” “This is a close-knit neighborhood;” “People in this neighborhood can be trusted;” “People in this neighborhood generally don’t get along with each other” (reverse-coded); “People in this neighborhood do not share the same values” (reverse-coded) (Cronbach’s α = .85) (36).
Perceived safety was measured using four items rated on 5-point Likert scales, ranging from 1 (strongly agree) to 5 (strongly disagree). Scores were coded such that higher scores reflected perceptions of greater safety. Questions included: “You feel safe walking in your neighborhood during the day,” “You feel safe walking in your neighborhood during the evening,” “Your neighborhood is safe from crime,” and “Violence is a problem in your neighborhood” (reverse-coded) (Cronbach’s α = .85) (36).
Neighborhood satisfaction was assessed by asking participants, “All things considered, would you say you are very satisfied, satisfied, dissatisfied, very dissatisfied or neutral - neither satisfied nor dissatisfied with your neighborhood as a place to live?”
Assessments of perceived neighborhood infrastructure were evaluated by asking respondents to rate, on a 5-point scale (strongly disagree to strongly agree) five aspects of neighborhood infrastructure, such as, “There are sidewalks on most of the streets in your neighborhood,” “Your neighborhood streets are well lit at night,” and “Crosswalks/pedestrian signals to help people walking cross busy streets in your neighborhood,” etc. (Cronbach’s α = .61) (36).
Objective neighborhood characteristics
In both neighborhoods, trained data collectors conducted audits on 613 street segments. Segments (both sides of a street between two cross streets) were randomly selected, with an oversampling of segments where there was anticipated change. Data collectors walked the length of each segment to complete the audits, adapted from the Bridging the Gap Street Segment Tool (37, 38). Data were collected at the street-level, and factor analyses were conducted at the level of the individual, by examining street segment data from within a 0.25-mile network distance of each participant’s home. Aspects of neighborhoods that are relevant to sleep were selected for inclusion in principal components analyses (PCA), with varimax rotation. We restricted factors to include those that had Eigen values greater than one and that contained at least two items. Results of the PCA produced three distinct factors that met these criteria: (1) neighborhood disorder (e.g., barred or broken windows, vacant lots, litter); (2) pedestrian safety (e.g., presence of sidewalks, traffic signs); and (3) land use (e.g., public spaces, services, retail stores, restaurants).
Crime
Using incident-level crime data provided by the City of Pittsburgh police department and ArcGIS 10.2 software, we calculated street network distances from each household to each approximate crime location. We were able to geocode 95% of the incidents using the address information from the raw data. For each household, we summed the total number of 2013 crimes that occurred within a 1-km network distance, to arrive at the household buffer for crime in 2013. The 1-km distance was chosen because this has been used in prior neighborhoods research (39, 40) and because this is considered “walking distance” (or within 10 minutes by walking). We also believed that crimes committed within a more proximal distance to the participant’s home would be more strongly associated with sleep. Violent crimes include incidents categorized as aggravated assault, simple assault, rape, and homicide. Property crimes include incidents categorized as arson, motor vehicle theft, burglary, robbery, stolen property, theft, and vandalism. Because violent crimes and property crimes were highly correlated at (r = 0.90), these were summed to create a total crime index, which served as the crime variable used in the analyses.
Analytic Strategy
Multivariable regressions were first estimated to investigate associations of neighborhood characteristics with sleep, adjusting for demographic covariates (age, gender, education, household income, marital status, presence of children in the home, BMI). Models included a dummy-coded variable for neighborhood (Hill District and Homewood) to account for any neighborhood-level differences at baseline. For significant associations between neighborhood characteristics and sleep quality, we also examined whether psychological distress statistically mediated the effects.
Specifically, we tested whether psychological distress statistically mediated the significant associations between neighborhood characteristics and sleep quality. Following Baron & Kenny’s recommendations for testing statistical mediation, the following criteria must be met: (1) the association between the independent variable (IV; perceived neighborhood characteristic) and the dependent variable (DV; sleep quality) must be demonstrated; (2) a relationship between the IV and the proposed mediator (psychological distress) must be demonstrated; and (3) mediation would be demonstrated if the association between the IV and the DV were significantly reduced after statistically controlling for the proposed mediator (41). In addition, to confirm whether the mediation effects were statistically significant, we conducted Sobel tests (42, 43) to determine whether the reduction in the effect of the independent variable, after including the mediator in the model, was a statistically significant reduction. In addition to controlling for neighborhood in all analyses, we also included the interaction terms for neighborhood (Hill District or Homewood) and each of the neighborhood characteristics, to determine if differential associations would emerge between neighborhood characteristics and sleep quality in the two neighborhoods. There were no significant interaction terms (analyses not shown). Therefore, for parsimony, models are presented without the interaction terms included. Finally, in sensitivity analyses, we re-estimated all analyses of the final models after excluding participants using sleep medications (n = 136).
Results
Sample characteristics
By study design, thirty-six percent (n = 310) of the sample was from the Homewood neighborhood, and the remaining 64% (n = 563) resided in the Hill District neighborhood (Table 1). Women constituted 77% of the sample. Approximately 26% of the sample had household incomes below $5,000; and an additional 25% had household incomes between $5000 and $9,900. Married and cohabiting persons made up 20.5% of the sample, and 28.1% of participants had children in the home. Participants were 55.4 years old on average, and the average body mass index (BMI) of the sample was 31.2 (class 1 obesity). Sleep quality scores ranged from 1 to 5 and averaged 3.7, indicating fair to good sleep.
Table 1.
Study characteristics for the total sample
| Mean (SD) or Percent | Range | |
|---|---|---|
|
|
||
| Female | 77.3% | |
| Hill District neighborhood | 64% | |
| Mean Age (years) | 55.4 (16.3) | 19–100 |
| Education | ||
| Less than high school | 12.7% | |
| High school | 41.9% | |
| Some college | 30.6% | |
| College | 14.8% | |
| Per capita annual household income in $1000s | 13.3 (13.5) | 0.2–87.5 |
| Married or living with partner | 20.5% | |
| Household with children | 28.1% | |
| Mean BMI (kg/m2) | 31.2 (7.5) | 14.6–56.2 |
| Sleep medication use | 16.3% | |
| Kessler psychological distress scale (K6) | 4.3 (4.5) | 0.0–24.0 |
| Mean Sleep Quality Rating | 3.7 (0.8) | 1.0–5.0 |
| Perceived Neighborhood Measures | ||
| Neighborhood Safety | 2.9 (0.8) | 1.0–4.8 |
| Neighborhood Satisfaction | 3.5 (1.2) | 1.0–5.0 |
| Neighborhood Infrastructure | 3.2 (0.7) | 1.2–5.0 |
| Social Cohesion | 3.1 (0.8) | 1.0–5.0 |
| Objective Neighborhood Measure | ||
| Neighborhood Disorder | 0.0 (1.0) | −2.8–1.8 |
| Pedestrian Safety | 0.0 (1.0) | −2.1–5.9 |
| Public Space/Land Use | 0.0 (1.0) | −4.6–2.5 |
| Total Crimes1 | 514.6 (235.3) | 0.0–996.0 |
Total Crimes refers to the total number of property and violent crimes committed within 1 km of participants’ homes.
Levels of perceived neighborhood characteristics for safety averaged 2.9, which indicates a neutral perception of level of safety (range = 1 to 4.8; SD = 0.8); 3.2 for infrastructure (range = 1.2 to 5.0; SD = 0.7), indicating a moderate level of quality of infrastructure; 3.1 for social cohesion (range = 1.0 to 5.0; SD = 0.8), indicating a moderate level of social cohesion; and 3.5 for level of satisfaction (range = 1 to 5; SD = 1.2), indicating residents’ perceptions of neighborhoods are between neutral to satisfied in the full sample. We examined outliers and skewness for all primary study variables. There were no extreme values or exceptionally skewed variables.
Correlations among neighborhood characteristics
We next examined correlations among all perceived and objective neighborhood characteristics (Table 2). There were significant correlations among neighborhood infrastructure with all other perceived characteristics, as well as neighborhood disorder (inversely correlated). Perceived safety, satisfaction, and social cohesion were all significantly correlated with one another (r’s range from 0.30 to 0.49). Correlations among objectively measured characteristics were not as strong (r’s range from −0.16 to 0.11). Total crime was inversely correlated with perceived safety and pedestrian safety, and positively correlated with disorder.
Table 2.
Correlations among neighborhood characteristics
| Social Cohesion | Perceived Safety | Satisfaction | Disorder | Pedestrian Safety | Land Use | Total Crime | |
|---|---|---|---|---|---|---|---|
|
|
|||||||
| Infrastructure | 0.30** | 0.39** | 0.37** | −0.1947 | −0.03 | −0.02 | −0.02 |
| Social Cohesion | 0.47** | 0.44** | −0.05 | −0.01 | 0.02 | −0.06+ | |
| Perceived Safety | 0.49** | −0.26** | −0.03 | 0.06 | −0.16** | ||
| Satisfaction | −0.20** | −0.06+ | 0.04 | −0.04 | |||
| Disorder | 0.01 | −0.03 | 0.11** | ||||
| Pedestrian Safety | −0.00 | −0.08* | |||||
| Land Use | 0.04 | ||||||
Note:
p <0.01;
p <0.05;
p <0.10.
Regression analyses
Perceived neighborhood characteristics and sleep quality
In the regression analyses (Table 3), we observed that higher levels of perceived neighborhood safety were associated with higher sleep quality. For each 1-SD unit increase in perceived safety, residents reported 0.13-unit higher level of sleep quality (p < 0.001), adjusting for age, gender, marital status, SES, BMI, presence of children in the home, and neighborhood indicator.
Table 3.
Results of linear regression models predicting sleep quality from perceived and objective neighborhood characteristics (N = 873).
| β | SE | Adj. R-sq. | |
|---|---|---|---|
|
|
|||
| Perceived Characteristics | |||
| Neighborhood Safety | 0.13*** | 0.04 | 0.03 |
| Neighborhood Satisfaction | 0.14*** | 0.02 | 0.03 |
| Neighborhood Infrastructure | 0.07* | 0.04 | 0.02 |
| Social Cohesion | 0.08* | 0.03 | 0.02 |
| Objective Characteristics | |||
| Neighborhood Disorder | −0.03 | 0.03 | 0.01 |
| Pedestrian Safety | 0.01 | 0.03 | 0.01 |
| Public Space/Land Use | −0.03 | 0.03 | 0.01 |
| Total Crime | 0.01 | 0.00 | 0.01 |
Note: Each of the neighborhood characteristics are entered into separate models. Each model includes covariates: neighborhood, age, male, married, household income, children in home, and BMI.
p <0.001;
p <0.01;
p <0.05.
Higher levels of neighborhood satisfaction were also associated with higher levels of sleep quality (standardized β = 0.14, p < 0.001). Measures of perceived social cohesion and neighborhood infrastructure were both positively associated with sleep quality (standardized β = 0.08 and 0.07, respectively, p-values < 0.05 for each, after adjusting for covariates). Neighborhood satisfaction and safety explain about 3% of the variance in sleep quality; while neighborhood infrastructure and social cohesion each explain about 2%. These effect sizes are small (44), but consistent with effect size magnitudes reported in prior research on neighborhood influences on sleep (15). Further, these associations are robust to adjustment for individual-level SES and BMI.
Objective neighborhood characteristics and sleep quality
As shown in Table 3, none of the objective neighborhood characteristics included in these analyses were associated with sleep quality.
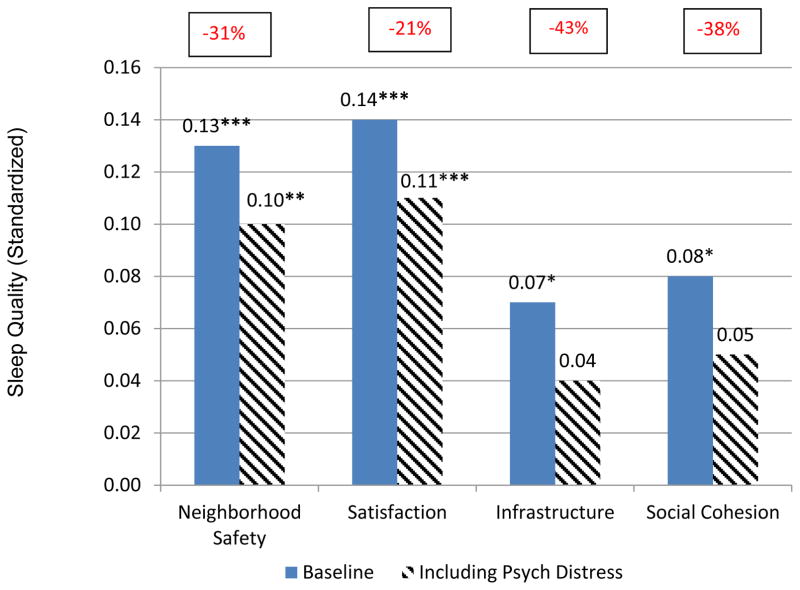
Mediation analyses
For significant associations between perceived neighborhood characteristics and sleep quality, we tested whether associations were mediated by psychological distress. In support of statistical criteria for identifying a potential mediator, psychological distress was significantly associated with perceived levels of: neighborhood satisfaction (β = 0.11; p < 0.01), safety (β = 0.14; p < 0.01), infrastructure (β = 0.10; p < 0.05) and social cohesion (β = 0.10; p < 0.01), as well as sleep quality (β = 0.10; p < 0.01). Associations of both social cohesion and neighborhood infrastructure with sleep were reduced to non-significance after adjusting for psychological distress. Specifically, coefficients for social cohesion and neighborhood infrastructure were reduced from 0.08 to 0.05 (38%) and from 0.07 to 0.04 (43%), respectively, after adding psychological distress to the models Figure 1. Sobel tests confirmed that psychological distress significantly mediated both of these associations.
Figure 1.
Plot of sleep quality according to perceived neighborhood characteristics: Mediation (N = 873).
In contrast, the association of perceived neighborhood safety with sleep quality was reduced from β 0.13 to β = 0.10 (31%) but remained statistically significant with the inclusion of psychological distress in the model, which is consistent with partial mediation. Similarly, the association of neighborhood satisfaction with sleep quality did not change substantially from β = 0.14 (p < 0.001) after adjusting for psychological distress (β = 0.11, p < 0.001) for a reduction of 21%. Sobel tests indicated that although psychological distress partially mediated associations with these neighborhood characteristics, there were also significant direct associations of these neighborhood characteristics with sleep quality, after accounting for psychological distress.
Discussion
The current study makes several contributions that fill important gaps in the literature on the association between neighborhoods and sleep. Specifically, we investigated multiple disparate perceived and objective neighborhood characteristics, included objectively measured crime data. focused on a large urban, low-income, predominantly African American population, who are known to be at increased risk of experiencing poorer sleep quality (45), and explored an important potential mediating pathway linking neighborhoods to sleep (psychological distress).
Consistent with prior research, we found important associations between neighborhood characteristics and sleep quality among our cohort who lived in two low-income predominantly African American neighborhoods. Specifically, perceived safety, social cohesion, perceptions of neighborhood infrastructure, and overall satisfaction with the neighborhood were associated with sleep quality. In light of the known links between sleep and health (8–11), and the substantial racial/ethnic and socioeconomic health disparities for various conditions (31, 32), the current findings suggest that differences in neighborhood characteristics may play a role in health disparities, via reduced sleep quality among lower income African Americans.
Moreover, our study investigated psychological distress as a potential pathway mediating neighborhood characteristics and sleep. Low levels of neighborhood safety and social cohesion have previously been hypothesized to impair sleep as a result of increased psychological stress, which could lead to states of vigilance or increased arousal, and/or increased level of depressive symptoms (17, 26). As a test of this theory, we further examined whether psychological distress served as a potential mediator of neighborhood-sleep associations. Associations between two perceived neighborhood characteristics (infrastructure and social cohesion) and sleep quality in the current study were largely attenuated by psychological distress, although the associations of perceived neighborhood safety and satisfaction with sleep quality persisted even after adjusting for psychological distress and other covariates.
In contrast to the significant associations we observed between perceived neighborhood characteristics and sleep quality, we did not observe significant associations between any of the objective neighborhood characteristics and sleep. These findings are consistent with prior work which has failed to find associations between objective neighborhood characteristics and health behaviors and outcomes (46, 47). For instance, Frei and colleagues found that greater subjectively assessed noise annoyance, but not objectively measured noise exposure, was significantly associated with subjective sleep quality (25). Such findings may be indicative of common method variance and/or that perceptions of neighborhood characteristics may be more proximally linked to perceptions of sleep quality. Nevertheless, given that this is one of the few studies to consider objectively measured neighborhood characteristics and sleep, further research is needed to identify other objectively measured neighborhood factors (e.g., crowding) that could influence sleep.
These findings must be considered in light of study limitations. First, although we included a broad range of potentially relevant objective neighborhood measures, we did not include others that may be particularly salient for sleep, such as noise levels (22–25). Moreover, we assessed only one dimension of sleep, sleep quality, via a single-item assessed via daily diary. Including a more extensive battery of questions and/or objective sleep measures would provide a more comprehensive profile of sleep, including sleep fragmentation and timing, which may show unique associations with neighborhood characteristics and have also been linked with health outcomes (48). Further, although we included a well-validated measure of psychological distress, other unmeasured psychosocial pathways (e.g., depression, anxiety) were not assessed in the current study in an effort to limit participant burden, but may also be relevant to neighborhood-health associations. In addition, the current study was conducted in an urban area, and findings may differ in suburban or rural environments. Moreover, although we consider the fact that we include a mostly African American population a strength, the results may not be generalizable to White or other racial/ethnic populations. Finally, because the data are cross-sectional, we cannot assess potentially causal relationships based on these data alone. Some portion of the association of sleep with perceived measures may be partially attributable to same-source bias, in that certain individuals may be inclined toward negative versus positive perspectives across different aspects of their lives. We note, however, that our results linking neighborhood safety and satisfaction to sleep quality were robust, even after adjustment for psychological distress.
Conclusions
Our findings are consistent with the theory that unfavorable neighborhood characteristics may contribute to poorer sleep quality in a low-income high risk African American population. In particular, one’s perceptions of the quality of various aspects of the neighborhood may specifically contribute to poorer sleep; whereas objectively measured characteristics are not significantly associated. Our findings further suggest that psychological distress may, at least in part, mediate associations between perceived neighborhood characteristics and sleep quality. Community-based interventions that serve to build or maintain social cohesion, satisfaction, and perceived safety in neighborhoods may provide a novel target of prevention and intervention efforts to reduce sleep problems and downstream health consequences in at-risk communities. In future analyses within this sample, we will have the unique ability to investigate whether, and to what extent, changes in the neighborhood characteristics as a result of neighborhood revitalization efforts affects sleep.
Acknowledgments
Support for the study which serves as the source of these data was provided by the National Heart, Lung & Blood Institute (R01HL122460) and the National Cancer Institute (R01CA164137).
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Diez Roux AV, Mair C. Neighborhoods and health. Annals of the New York Academy of Sciences. 2010;1186(1):125–45. doi: 10.1111/j.1749-6632.2009.05333.x. [DOI] [PubMed] [Google Scholar]
- 2.White K, Borrell LN. Racial/ethnic residential segregation: framing the context of health risk and health disparities. Health & place. 2011;17(2):438–48. doi: 10.1016/j.healthplace.2010.12.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Fish JS, Ettner S, Ang A, Brown AF. Association of perceived neighborhood safety on body mass index. American journal of public health. 2010;100(11):2296–303. doi: 10.2105/AJPH.2009.183293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Burdette HL, Wadden TA, Whitaker RC. Neighborhood safety, collective efficacy, and obesity in women with young children. Obesity. 2006;14(3):518–25. doi: 10.1038/oby.2006.67. [DOI] [PubMed] [Google Scholar]
- 5.Auchincloss AH, Roux AVD, Mujahid MS, Shen M, Bertoni AG, Carnethon MR. Neighborhood resources for physical activity and healthy foods and incidence of type 2 diabetes mellitus: the Multi-Ethnic study of Atherosclerosis. Archives of internal medicine. 2009;169(18):1698–704. doi: 10.1001/archinternmed.2009.302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Morenoff JD, House JS, Hansen BB, Williams DR, Kaplan GA, Hunte HE. Understanding social disparities in hypertension prevalence, awareness, treatment, and control: the role of neighborhood context. Social science & medicine. 2007;65(9):1853–66. doi: 10.1016/j.socscimed.2007.05.038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Mujahid MS, Roux AVD, Morenoff JD, Raghunathan TE, Cooper RS, Ni H, et al. Neighborhood characteristics and hypertension. Epidemiology. 2008;19(4):590–8. doi: 10.1097/EDE.0b013e3181772cb2. [DOI] [PubMed] [Google Scholar]
- 8.Jennings J, Muldoon M, Hall M. Self-reported sleep quality is associated with the metabolic syndrome. Sleep. 2007;30:219–23. doi: 10.1093/sleep/30.2.219. [DOI] [PubMed] [Google Scholar]
- 9.Nock NL, Li L, Larkin EK, Patel SR, Redline S. Empirical evidence for “syndrome Z”: a hierarchical 5-factor model of the metabolic syndrome incorporating sleep disturbance measures. Sleep. 2009;32(5):615–22. doi: 10.1093/sleep/32.5.615. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Gallicchio L, Kalesan B. Sleep duration and mortality: a systematic review and meta-analysis. Journal of sleep research. 2009;18(2):148–58. doi: 10.1111/j.1365-2869.2008.00732.x. [DOI] [PubMed] [Google Scholar]
- 11.Irwin MR. Why sleep is important for health: a psychoneuroimmunology perspective. Psychology. 2015;66(1):143. doi: 10.1146/annurev-psych-010213-115205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Patel SR, Hu FB. Short sleep duration and weight gain: a systematic review. Obesity. 2008;16(3):643–53. doi: 10.1038/oby.2007.118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Bernert RA, Nadorff MR. Sleep disturbances and suicide risk. Sleep medicine clinics. 2015;10(1):35–9. doi: 10.1016/j.jsmc.2014.11.004. [DOI] [PubMed] [Google Scholar]
- 14.Lopresti AL, Hood SD, Drummond PD. A review of lifestyle factors that contribute to important pathways associated with major depression: diet, sleep and exercise. Journal of affective disorders. 2013;148(1):12–27. doi: 10.1016/j.jad.2013.01.014. [DOI] [PubMed] [Google Scholar]
- 15.Hale L, Hill TD, Burdette AM. Does sleep quality mediate the association between neighborhood disorder and self-rated physical health? Preventive medicine. 2010;51(3):275–8. doi: 10.1016/j.ypmed.2010.06.017. [DOI] [PubMed] [Google Scholar]
- 16.Hale L, Hill TD, Friedman E, Nieto FJ, Galvao LW, Engelman CD, et al. Perceived neighborhood quality, sleep quality, and health status: Evidence from the Survey of the Health of Wisconsin. Social Science & Medicine. 2013;79:16–22. doi: 10.1016/j.socscimed.2012.07.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Hill TD, Burdette AM, Hale L. Neighborhood disorder, sleep quality, and psychological distress: testing a model of structural amplification. Health & place. 2009;15(4):1006–13. doi: 10.1016/j.healthplace.2009.04.001. [DOI] [PubMed] [Google Scholar]
- 18.Johnson DA, Brown DL, Morgenstern LB, Meurer WJ, Lisabeth LD. The association of neighborhood characteristics with sleep duration and daytime sleepiness. Sleep Health. 2015;1(3):148–55. doi: 10.1016/j.sleh.2015.06.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Brouillette RT, Horwood L, Constantin E, Brown K, Ross NA. Childhood sleep apnea and neighborhood disadvantage. The Journal of pediatrics. 2011;158(5):789–95. e1. doi: 10.1016/j.jpeds.2010.10.036. [DOI] [PubMed] [Google Scholar]
- 20.Chambers EC, Pichardo MS, Rosenbaum E. Sleep and the housing and neighborhood environment of urban Latino adults living in low-income housing: the AHOME study. Behavioral sleep medicine. 2016;14(2):169–84. doi: 10.1080/15402002.2014.974180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Hill TD, Trinh HN, Wen M, Hale L. Perceived neighborhood safety and sleep quality: a global analysis of six countries. Sleep medicine. 2014 doi: 10.1016/j.sleep.2014.12.003. [DOI] [PubMed] [Google Scholar]
- 22.Basner M, Müller U, Elmenhorst E-M. Single and combined effects of air, road, and rail traffic noise on sleep and recuperation. Sleep. 2011;34(1):11–23. doi: 10.1093/sleep/34.1.11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Muzet A. Environmental noise, sleep and health. Sleep medicine reviews. 2007;11(2):135–42. doi: 10.1016/j.smrv.2006.09.001. [DOI] [PubMed] [Google Scholar]
- 24.Pirrera S, De Valck E, Cluydts R. Nocturnal road traffic noise: A review on its assessment and consequences on sleep and health. Environment international. 2010;36(5):492–8. doi: 10.1016/j.envint.2010.03.007. [DOI] [PubMed] [Google Scholar]
- 25.Frei P, Mohler E, Röösli M. Effect of nocturnal road traffic noise exposure and annoyance on objective and subjective sleep quality. International journal of hygiene and environmental health. 2014;217(2):188–95. doi: 10.1016/j.ijheh.2013.04.003. [DOI] [PubMed] [Google Scholar]
- 26.Johnson SL, Solomon BS, Shields WC, McDonald EM, McKenzie LB, Gielen AC. Neighborhood violence and its association with mothers’ health: assessing the relative importance of perceived safety and exposure to violence. Journal of Urban Health. 2009;86(4):538–50. doi: 10.1007/s11524-009-9345-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Adenekan B, Pandey A, McKenzie S, Zizi F, Casimir GJ, Jean-Louis G. Sleep in America: role of racial/ethnic differences. Sleep medicine reviews. 2013;17(4):255–62. doi: 10.1016/j.smrv.2012.07.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Baldwin CM, Ervin A-M, Mays MZ, Robbins J, Shafazand S, Walsleben J, et al. Sleep disturbances, quality of life, and ethnicity: the Sleep Heart Health Study. J Clin Sleep Med. 2010;6(2):176–83. [PMC free article] [PubMed] [Google Scholar]
- 29.Hall MH, Matthews KA, Kravitz HM, Gold EB, Buysse DJ, Bromberger JT, et al. Race and financial strain are independent correlates of sleep in midlife women: the SWAN sleep study. Sleep: Journal of Sleep and Sleep Disorders Research. 2009 [PMC free article] [PubMed] [Google Scholar]
- 30.Olafiranye O, Akinboboye O, Mitchell JE, Ogedegbe G, Jean-Louis G. Obstructive sleep apnea and cardiovascular disease in blacks: a call to action from the Association of Black Cardiologists. American heart journal. 2013;165(4):468–76. doi: 10.1016/j.ahj.2012.12.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Beckles GL, Zhu J, Moonesinghe R. Diabetes-United States, 2004 and 2008. MMWR Surveill Summ. 2011;60(Suppl):90–3. [PubMed] [Google Scholar]
- 32.Freedman DS. Obesity—United States, 1988–2008. MMWR Surveill Summ. 2011;60(01):73–7. [PubMed] [Google Scholar]
- 33.Pattillo M. Black middle-class neighborhoods. Annual Review of Sociology. 2005:305–29. [Google Scholar]
- 34.Kessler RC, Andrews G, Colpe LJ, Hiripi E, Mroczek DK, Normand S-L, et al. Short screening scales to monitor population prevalences and trends in non-specific psychological distress. Psychological medicine. 2002;32(06):959–76. doi: 10.1017/s0033291702006074. [DOI] [PubMed] [Google Scholar]
- 35.Weissman J, Pratt LA, Miller EA, Parker JD. Serious psychological distress among adults: United States, 2009–2013. NCHS data brief. 2015:203. [PubMed] [Google Scholar]
- 36.Sampson RJ, Raudenbush SW, Earls F. Neighborhoods and violent crime: A multilevel study of collective efficacy. Science. 1997;277(5328):918–24. doi: 10.1126/science.277.5328.918. [DOI] [PubMed] [Google Scholar]
- 37.Kelly CM, Schootman M, Baker EA, Barnidge EK, Lemes A. The association of sidewalk walkability and physical disorder with area-level race and poverty. Journal of epidemiology and community health. 2007;61(11):978–83. doi: 10.1136/jech.2006.054775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Slater SJ, Nicholson L, Chriqui J, Barker DC, Chaloupka FJ, Johnston LD. Walkable communities and adolescent weight. American journal of preventive medicine. 2013;44(2):164–8. doi: 10.1016/j.amepre.2012.10.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Boone-Heinonen J, Diez-Roux AV, Goff DC, Loria CM, Kiefe CI, Popkin BM, et al. The neighborhood energy balance equation: does neighborhood food retail environment+ physical activity environment= obesity? The CARDIA study. PLoS One. 2013;8(12):e85141. doi: 10.1371/journal.pone.0085141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Rundle AG, Sheehan DM, Quinn JW, Bartley K, Eisenhower D, Bader MM, et al. Using GPS data to study neighborhood walkability and physical activity. American journal of preventive medicine. 2016;50(3):e65–e72. doi: 10.1016/j.amepre.2015.07.033. [DOI] [PubMed] [Google Scholar]
- 41.Baron RM, Kenny DA. The moderator–mediator variable distinction in social psychological research: Conceptual, strategic, and statistical considerations. Journal of personality and social psychology. 1986;51(6):1173. doi: 10.1037//0022-3514.51.6.1173. [DOI] [PubMed] [Google Scholar]
- 42.Sobel ME. Asymptotic confidence intervals for indirect effects in structural equation models. Sociological methodology. 1982;13(1982):290–312. [Google Scholar]
- 43.Sobel ME. Some new results on indirect effects and their standard errors in covariance structure models. Sociological methodology. 1986;16:159–86. [Google Scholar]
- 44.Cohen J. Statistical Power Analysis for the Behavioral Sciences. 2. Hillsdale, New Jersey: L. Erlbaum; 1988. [Google Scholar]
- 45.Patel NP, Grandner MA, Xie D, Branas CC, Gooneratne N. “ Sleep disparity” in the population: poor sleep quality is strongly associated with poverty and ethnicity. BMC Public Health. 2010;10(1):1. doi: 10.1186/1471-2458-10-475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Block JP, Christakis NA, O’malley AJ, Subramanian S. Proximity to food establishments and body mass index in the Framingham Heart Study offspring cohort over 30 years. American Journal of Epidemiology. 2011:kwr244. doi: 10.1093/aje/kwr244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Thornton LE, Bentley RJ, Kavanagh AM. Fast food purchasing and access to fast food restaurants: a multilevel analysis of VicLANES. International journal of behavioral nutrition and physical activity. 2009;6(1):28. doi: 10.1186/1479-5868-6-28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Matthews KA, Dahl RE, Owens JF, Lee L, Hall M. Sleep duration and insulin resistance in healthy black and white adolescents. Sleep. 2012;35(10):1353–8. doi: 10.5665/sleep.2112. [DOI] [PMC free article] [PubMed] [Google Scholar]