Abstract
The potential of the skin immune system to generate immune responses is well established, and the skin is actively exploited as a vaccination site. Human skin contains several antigen-presenting cell subsets with specialized functions. In particular, the capacity to cross-present exogenous antigens to CD8+ T cells is of interest for the design of effective immunotherapies against viruses or cancer. Here, we show that primary human Langerhans cells (LCs) were able to cross-present a synthetic long peptide (SLP) to CD8+ T cells. In addition, modification of this SLP using antibodies against the receptor langerin, but not dectin-1, further enhanced the cross-presenting capacity of LCs through routing of internalized antigens to less proteolytic early endosome antigen 1+ early endosomes. The potency of LCs to enhance CD8+ T-cell responses could be further increased through activation of LCs with the toll-like receptor 3 ligand polyinosinic:polycytidylic acid (pI:C). Altogether, the data provide evidence that human LCs are able to cross-present antigens after langerin-mediated internalization. Furthermore, the potential for antigen modification to target LCs specifically provides a rationale for generating effective anti-tumor or anti-viral cytotoxic T lymphocyte responses.
Keywords: antigen cross-presentation, dectin-1, early endosomes, human Langerhans cells, langerin
Introduction
Antigen-presenting cells (APCs), and in particular, dendritic cells (DCs), induce adaptive immune responses through the presentation of endogenous peptides in the context of major histocompatibility complex (MHC) class I molecules and exogenous peptides in the context of MHC class II molecules to CD8+ and CD4+ T cells, respectively. In addition, DCs are able to capture and present exogenously derived antigens via MHC class I molecules, a process known as cross-presentation.1 Antigen cross-presentation plays an important role in the priming of cytotoxic T cells against viruses and tumors, but it is also important in maintaining self-tolerance.2 However, not all DC subsets have identical cross-presentation capacities, and some DC subsets appear to be better equipped for this task. Therefore, careful selection of the DC subset is of utmost importance in the design of anti-tumor or anti-viral DC-targeting vaccination strategies.
Langerhans cells (LCs) are a subset of DCs present in mucosal tissues and stratified epithelium, such as the epidermis of the skin. Human LCs are characterized by the expression of CD1a and the C-type lectin receptor (CLR) langerin and the presence of Birbeck granules, which are associated with langerin expression.3 Langerin mediates recognition through interaction with glycoconjugates such as the high-mannose structure mannan or the β-glucans expressed on the surface of pathogens.4 Langerin mediates ligand internalization for antigen processing and presentation, and therefore it has the potential to be used to specifically deliver antigens conjugated to glycans or α-langerin antibodies to LCs. Although capture of exogenous antigens by human LCs results in the induction of CD4+ T-cell responses,5,6 it still remains under debate whether human LCs are able to cross-present exogenous antigens. In vitro-derived LCs cultured from CD34+ progenitor cells efficiently promote CD8+ T-cell proliferation after internalization of soluble peptides.7 Additionally, LCs pulsed with a short Epstein–Barr virus (EBV) peptide or a 39 amino acid-long peptide containing the EBV minimal epitope, were more efficient than pulsed dermal DCs (dDCs) in cross-presentation of the EBV antigen to memory CD8+ T cells.8 This enhanced CD8+ T-cell activation by LCs was dependent on the interaction between CD70 and CD278 but did not rely on specific, receptor-mediated uptake of antigens. However, others reported that isolated human LCs were unable to cross-present heat-inactivated measles virus (MV), which was specifically recognized and internalized by langerin.9 In addition, studies performed in mice also suggest that LCs may have lower cross-presenting capacity.10 Using a murine model of Candida albicans skin infection, the authors showed that LCs were dispensable in the generation of cytotoxic T cells.10 Instead, langerin+ dDCs were required for the generation of antigen-specific CTLs and Th1 cells against C. albicans. Other studies have recently suggested that cross-presentation is mainly an attribute of the langerin+ dDC subpopulation and not of the LCs in murine skin.11,12 However, the existence of an equivalent of this langerin+ dDC subpopulation in human skin has been questioned,13 although very recently, a langerin+ APC subpopulation has also been detected in the human dermis.14
Because of their APC-restricted expression pattern and their function as antigen-uptake receptors for processing and presentation, CLRs have often been studied as targeting receptors for vaccination.15,16 Antigen targeting to DEC-205, DCIR, CLEC9a, dectin-1, and DC-SIGN on DCs results in receptor internalization and enhanced antigen-specific CD4+ and CD8+ T-cell responses.17,18,19,20 Because CLRs are expressed by specific DC subsets, the choice of a CLR for targeting not only determines the antigen internalization pathway but also to which DC subset the antigen is targeted. Various pathways involved in cross-presentation after CLR-mediated antigen internalization of antigens have been proposed. One mechanism involves the translocation of antigen into the cytoplasm for proteosomal degradation, followed by transporter associated with antigen processing (TAP)-mediated peptide transport in the endoplasmatic reticulum and loading onto MHC class I molecules.21,22 Antigenic peptides can also be generated in the endocytic pathway in a proteosome-independent manner and subsequently bind to the recycling MHC class I molecules present within endosomal compartments.23,24,25 Recently, it was shown that antigen targeting to specific intracellular compartments, either to early endosomes via CD40 and mannose receptor antibody conjugates or to late lysosomal compartments via DEC-205, resulted in antigen cross-presentation.26 Targeting antigens to early endosomes has been shown to result in the most efficient antigen cross-presentation, suggesting that the endocytic compartments to which antigens are delivered determine the efficiency of cross-presentation.
In this study, we set out to investigate the role of human LCs in the cross-presentation of a synthetic long peptide (SLP) conjugated to antibodies specific for the CLRs langerin and dectin-1, which gave us the opportunity to study the role of each receptor in the processing and shuttling of antigens to MHC class I-loading compartments. To determine whether antigen uptake via langerin and dectin-1 by human LCs result in different intracellular routing and antigen cross-presentation, we analyzed the co-localization of both receptors with the early endosome marker early endosome antigen-1 (EEA-1) and the lysosome marker Lysosomal-associated membrane protein 1 (LAMP-1) in pulse–chase experiments. Here, we report that targeting langerin, but not dectin-1, with either antibody resulted in enhanced cross-presentation. Altogether, these results provide a rationale for developing vaccines that specifically target langerin on human LCs to induce anti-tumor CD8+ T-cell responses.
Materials and methods
Cells
Primary human LCs were isolated from abdominal resections from healthy donors undergoing cosmetic surgery (Bergman Clinics, Bilthoven, the Netherlands) and obtained with informed consent within 24 h after surgery as previously described.27 Briefly, 5 mm-thick slices of skin, containing the epidermis and dermis, were cut using a dermatome. The slices were incubated in dispase II (1 mg mL–1, Roche Diagnostics, Basil, Switzerland) in Iscove's modified Dulbecco's medium (IMDM; Invitrogen, Waltham, MA, USA) supplemented with 10% fetal calf serum (FCS; BioWhittaker, Walkersville, MD, USA), 50 U mL–1 penicillin (Lonza, Basil, Switzerland), 50 μg mL–1 streptomycin (Lonza), and 10 μg mL–1 gentamicin (Lonza) overnight at 4 °C, followed by mechanical separation of the dermis and the epidermis using tweezers. The epidermis was washed in phosphate-buffered saline (PBS), cut into small pieces and incubated in PBS-containing DNase I (200 U mL–1, Roche Diagnostics) and trypsin (0.05%, Invitrogen) for 30 min at 37 °C. After incubation, a single-cell suspension was generated using 100 μm nylon cell strainers (BD Falcon, Corning, NY, USA), and cells were layered onto a Ficoll gradient. An average of 1 × 104 LCs per cm2 of tissue with a purity higher than 90% was obtained and characterized as CD1a+ langerin+ cells by flow cytometry as described below. LCs were cultured in IMDM supplemented with 10% FCS, 50 U mL–1 penicillin, 50 μg mL–1 streptomycin, and 10 μg mL–1 gentamicin. Where indicated, 5 × 104 LCs were cultured for 24 h in 200 µL–1 medium supplemented with 20 μg mL–1 polyinosinic:polycytidylic acid (pI:C; Invivogen, Carlsbad, CA, USA), 20 ng mL–1 lipopolysaccharide (LPS; derived from E. coli, Sigma, St Louis, MO, USA), 5 μg mL–1 R837 (Invivogen), or 5 μg mL–1 R848 (Invivogen) to induce maturation. In the indicated experiments, LCs were obtained by spontaneous migration. Briefly, the epidermis and dermis were separated as described above. The epidermis was washed in PBS and cultured for 2 days in a 25 cm2 culture dish (Greiner, Alphen aan den Rijn, The Netherlands) containing 40 mL of IMDM supplemented with 10% FCS, 50 U mL–1 penicillin, 50 μg mL–1 streptomycin, and 10 μg mL–1 gentamicin to allow for the spontaneous migration of LCs. After 2 days, cells present in the supernatant were harvested and layered onto a Ficoll gradient and further cultured as described above.
Tap-deficient T2 cell line
The TAP-negative B × T hybrid cell line 1.74 × CEM (referred to as T2) was used for peptide stabilization assays.28 T2 cells (1 × 105) were incubated overnight with peptide in RPMI-1640 medium at 37 °C, washed twice in PBS, and assayed for surface MHC class I expression by flow cytometry (FACSCalibur, Becton Dickinson, San Jose, CA, USA) using an human leukocyte antigen (HLA)-A2-specific monoclonal antibody (mAb; Becton Dickinson).
Flow cytometry
Phenotypic analysis of isolated LCs was performed by flow cytometry. Cells were washed in PBS supplemented with 1% bovine serum albumin (BSA) and 0.02% NaN3 and incubated for 30 min at 4 °C in the presence of the appropriate dilutions of fluorescent-conjugated mAbs to CD1a (APC, clone HI149, Becton Dickinson), CD14 (FITC, clone MoP9, Becton Dickinson), CD70 (PE, clone Ki-24, Becton Dickinson), CD86 (PE, clone 2331, Becton Dickinson), HLA-DR (PerCP, clone L203, Becton Dickinson), HLA-ABC (FITC, clone W6/32, ImmunoTools, Friesoythe, Germany) CD83 (PE, clone HB15e, Beckman Coulter Immunoteck, Bubeneč, Czeck Republic), or the corresponding isotype-matched control mAbs (Becton Dickinson). The HLA-A2 status of the cells was determined using a specific mAb (Becton Dickinson). The cells were subsequently analyzed using the FACSCalibur and FlowJo software (Tree Star Inc., Ashland, OR, USA).
Imaging flow cytometry
Approximately 0.1 × 106 primary human LCs, which migrated spontaneously from human skin, were incubated for 3 h at 37 °C in culture medium with or without 20 μg mL–1 pI:C to induce maturation. Cells were then washed twice and incubated in ice-cold culture medium. As indicated, AF647-labeled anti-dectin-1 (AbD Serotec, Puchheim, Germany) and PE-labeled anti-langerin (R&D Systems, Minneapolis, MN, USA) were added, and cells were incubated for 15 min at 37 °C to allow binding to cell surface-expressed langerin and dectin-1. Cells were then washed in ice-cold medium and transferred to a 37 °C incubator, and samples were obtained at the indicated time points. Cells were subsequently washed in ice-cold PBS and fixed in ice-cold 4% paraformaldehyde in PBS for 20 min. To prevent cell loss during the staining procedure, LCs were mixed with monocyte-derived DCs. Cells were then permeabilized in 0.1% saponin (Sigma) in PBS for 30 min at room temperature (RT) and subsequently blocked using PBS-containing 0.1% saponin and 2% BSA for 30 min at RT. Staining was performed at RT in PBS supplemented with 0.1% saponin and 2% BSA. After staining, cells were washed twice in PBS, resuspended in PBS-containing 1% BSA and 0.02% NaN3, and stored at 4 °C until analysis. Cells were acquired on an ImageStream X (Amnis, Merck Millipore, Darmstadt, Germany) imaging flow cytometer. A minimum of 15 000 cells was acquired per sample at a flow rate ranging between 50 cells/second and 100 cells/second at 60× magnification. At least 2000 cells were acquired from single-stained samples to allow for compensation (Supplementary Figure S1). Analysis was performed using IDEAS v6.1 software (Amnis). Cells were gated based on the Gradient RMS (brightfield) feature, which was used to select for cells in focus (Supplementary Figure S2a), and langerin expression (Supplementary Figure S2b). Co-localization (Supplementary Figure S3) was calculated using bright detail similarity R3 (for 2-color co-localization) or bright detail co-localization 3 (for 3-color co-localization).
Antibody degradation assay western blot
LCs were incubated in serum-free IMDM for 30 min, incubated with 50 µg mL–1 anti-langerin (10E2) or anti-Dectin-1 (AbD Serotec) for 45 min on ice to ensure binding. Cells were washed twice in ice-cold medium to remove unbound antibody, and internalization was assessed after 0-, 15-, and 45-min incubations at 37 °C. Following the indicated incubation times, cells were lysed in NP-40 lysis buffer for 30 min on ice. Nuclei were removed by spinning cells at 14 000 r.p.m. for 10 min and the supernatant, which contained the cell lysate, was used for western blot (WB). Cell lysates were denatured in sodium dodecyl sulfate (SDS) sample buffer (Bio-Rad, Hercules, CA, USA) and reducing agent and boiled for 5 min. Samples were loaded and separated on a 10% SDS–polyacrylamide gel in electrophoresis buffer (3 g Tris, 14.4 g glycine, 1 L MQ, 0.1% SDS) before transferring to a nitrocellulose membrane (Bio-Rad) for 2 h at 250 mV for immunoblotting. The blot was blocked in blocking solution (Carl Roth, Karlsruhe, Germany) for 1 h at RT, followed by incubation with a polyclonal goat anti-mouse Ig horseradish peroxidase (HRP) conjugate (Dako, Glostrup, Denmark) for 1 h at RT. After extensive washing with PBS plus 0.05% Tween, antibody binding was visualized using enhanced chemiluminescence (Bio-Rad). Antibody staining was removed by incubating the blot in stripping buffer for 1 h at 60 °C, followed by blocking for 1 h at RT. Actin was stained using goat polyclonal anti-actin IgG (Santa Cruz Biotechnology, Dallas, Texas, USA) and the corresponding HRP-coupled secondary antibody.
Immunofluorescence microscopy
Human tissue sections (7 µm) were fixed in acetone and blocked with goat serum prior to staining. Antibodies directed against CD14, CD1a, or langerin were added at 10 µg mL–1 in PBS-containing 1% BSA for 60 min at 37 °C, followed by secondary Alexa 488-conjugated rabbit anti-mouse IgG2A, Alexa 546-conjugated rabbit anti-mouse IgG2B, or Alexa 647-conjugated rabbit anti-mouse IgG1-specific antibodies (Molecular Probes, Waltham, MA, USA) for 30 min at RT. Sections were counterstained using Hoechst 33342 (Thermo Fisher Scientific, Waltham, MA, USA) and analyzed by fluorescence microscopy (Leica Microsystems).
Modification of MART-1 peptide with antibodies
The SLP melanoma antigen recognized by T-cells 1 (MART-1) (C-YTTAEELAGIGILTV) was produced by solid-phase peptide synthesis using Fmoc-chemistry with a Symphony peptide synthesizer (Protein Technologies Inc., Tucson, AZ, USA) Peptide was conjugated to antibodies on the N-terminal cysteine through a thiol-maleimide reaction. To this end, antibodies were activated by reaction with SMCC (succinimidyl 4-(N-maleimidomethyl) cyclohexane-1-carboxylate, Thermo Scientific, Waltham, MA, USA). Peptide was conjugated to antibodies using the bifunctional crosslinker succinimidyl-4-(N-maleimidomethyl) cyclohexane-1-carboxylate (SMCC, Thermo Scientific). Briefly, antibodies were activated with SMCC (8 eq.) in phosphate buffer (pH 8.2) for 30 min at RT. After desalting over a G-25 10 × 100 mm single-use desalting gel filtration column (Amersham Biotech, Amersham, UK), peptide was dissolved in dimethylsulphoxide and added to the vial containing the antibody. After performing the coupling reaction at RT for 2 h, unconjugated peptide was removed by size-exclusion chromatography using a Superdex 75 column (30 × 100 mm, Amersham Biotech), and antibody-peptide constructs were eluted with 50 mM ammonium formate buffer (pH 6.8). The fractions containing the antibody-peptide constructs were pooled and lyophilized.
Generation of langerin-Fc constructs
The binding capacity of langerin to various Lewis-type glycans was determined using langerin-Fc molecules. Langerin-Fc was generated by amplifying LC RNA encoding the extracellular domains of langerin (aa 63–328) by PCR. The product was confirmed by sequence analysis and fused at the C-terminus to human IgG1-Fc in the Sig-pIgG1-Fc vector. Langerin-Fc was produced by stable transfection of Chinese hamster ovary cells, and langerin-Fc concentrations were determined by ELISA.
ELISA-based langerin-binding assay
The conjugation of the Leb, LeX, and LeY glycans to the MART-1 peptide was confirmed by ELISA using anti-Leb, -LeX, and -LeY antibodies (Calbiochem, San Diego, CA, USA).18 Briefly, glycopeptides were dissolved in PBS-containing 0.05% BSA, coated onto NUNC MaxiSorp plates (Nunc, Roskilde, Denmark), and incubated overnight at 4 °C. Plates were blocked with 1% BSA in PBS to avoid non-specific binding. After extensive washing, the glycopeptides were incubated with langerin-Fc for 90 min at RT. Binding was detected using a peroxidase-labeled F(ab′)2 goat anti-human IgG/Fcγ-specific antibody. Signal detection was achieved by incubation with 1.3 mM H2O2 in the presence of TMB (3,3′,5,5′-tetramethylbenzidine) in 0.1 M sodium acetate-citrate buffer until the development of the reaction. The reaction was then stopped using 1 M H2SO4, and absorbance was measured at 450 nm using a colorimeter (Bio-Rad). As a positive control, biotin-labeled Leb, LeX, and LeY conjugated to polyacrylamide (PAA; Lectinity, Moscow, Russia) were used.
Quantitative real-time RT-PCR
Cells were lysed, and mRNA was isolated using the mRNA Capture Kit (Roche). Complimentary DNA was synthesized using the Reverse Transcription System Kit (Promega) according to the manufacturer's guidelines. Each experiment contained cells isolated from at least five skin donors to obtain sufficient cell numbers for analysis. Oligonucleotides were designed using Primer Express 2.0 software (Applied Biosystems, Waltham, MA, USA) and synthesized by Invitrogen Life Technologies, Waltham, MA, USA. Real-time PCR analysis was performed as previously described using the SYBR Green method with an ABI 7900HT Sequence Detection System (Applied Biosystems).29 GAPDH was used as an endogenous reference gene.
Antigen presentation to human CD8+ T-cell clones specific for MART-1
A CD8+ T-cell clone specific for MART-126-35 was generated and cultured as previously described.30 The modified 16 aa-long MART-121-35 peptide (C-YTTAEELAGIGILTV) was added to 20 000 HLA-A2+ LCs per well obtained after migration from the skin, at the indicated concentrations together with poly I:C (20 μg mL–1) for 3 h at 37 °C. After extensive washing, HLA-A2+ MART-1-specific CD8+ T cells (100 000/well) were added to the wells. After 24 h, supernatants were collected and interferon-gamma (IFN-γ) levels were measured by sandwich ELISA, using specific antibody pairs from Biosource and according to the manufacturer's guidelines.
Statistical analysis
Results were analyzed using either a one-way analysis of variance (ANOVA) followed by Bonferrroni multiple comparison test or a two-way ANOVA followed by Bonferroni multiple comparison test using GraphPad Prism software (GraphPad Software, San Diego, CA, USA). Results were considered to be statistically significant when p < 0.05.
Results
LCs are the main langerin+ cells in the human skin
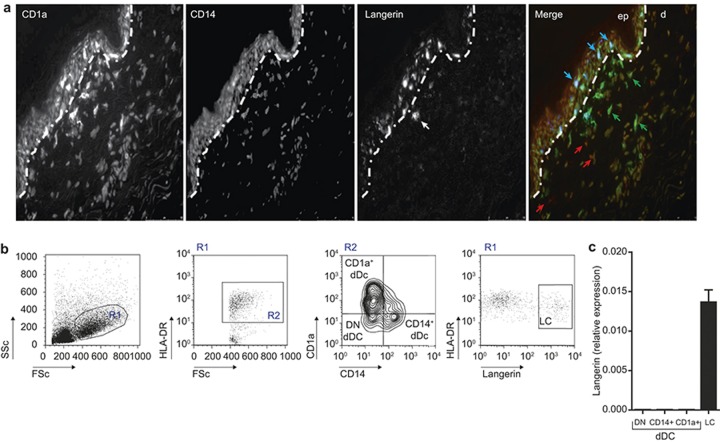
Although langerin has been classically reported to be exclusively expressed on epidermal LCs in the human skin,31,32 recent publications have challenged this knowledge by reporting the existence of langerin+ CD1a+ dDCs in human dermis, lung, liver, and lymphoid tissue.14 To analyze whether langerin expression is restricted to epidermal LCs, human skin sections were stained for CD14, CD1a, and langerin. As shown in Figure 1a, the great majority of langerin staining was observed in epidermal LCs, which were also positive for CD1a, and only rare CD1a+ langerin+ cells could be observed in the dermis in close proximity with the dermo-epidermal junction (Figure 1a). These cells could simply represent activated LCs that migrate through the dermis to the lymph nodes.14 In addition, it was recently demonstrated that these cells could also be dDCs that have been in contact with transforming growth factor beta leaked from the epidermis, resulting in upregulation of langerin.33 Nevertheless, the frequency of these cells is extremely low, and it is questionable whether their presence in the dermis has any functional relevance. Indeed, most of the dermal CD1a+ DCs we observed were devoid of langerin expression (Figure 1). Additionally, we confirmed the data by quantitative RT-PCR analysis of langerin expression on FACS-sorted HLA-DR+ APCs isolated from the dermis and epidermis (Figure 1b). Figure 1c confirms that langerin was exclusively expressed by LCs and not by dermal CD1a+ DCs, CD14+ DCs, or the HLA-DR+CD1a-CD14-dDC subset, which may consist of macrophages and BDCA3+ skin DCs, among other cell types. Thus, LCs are the main langerin+ cells in the human skin.
Figure 1.
Langerin is exclusively expressed by human LCs. (a) Staining of a section of steady-state human skin for langerin (blue), CD1a (green), CD14 (red), and Hoechst (yellow), and analysis by fluorescence microscopy. (b) Gating strategy for FACS-sorted LCs, CD14+, CD1a+, and double-negative dermal DCs. (c) Langerin mRNA is exclusively expressed in primary, FACS-sorted LCs and not by the other skin DC subsets. N = 3; each experiment contained sorted cells from at least five skin donors. mRNA values are normalized to GAPDH levels.
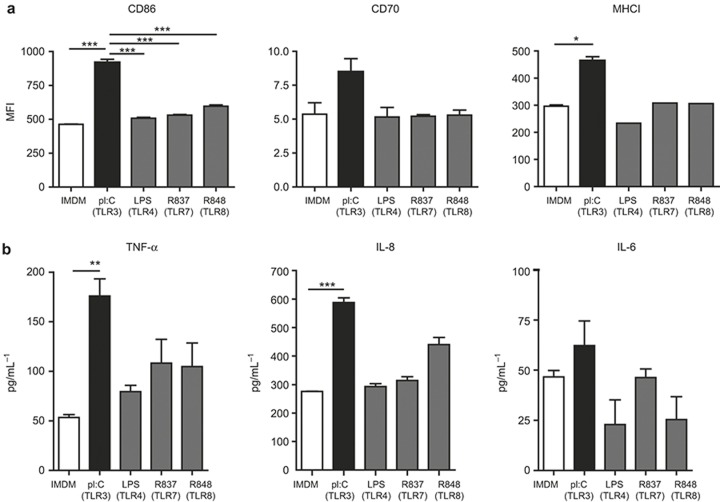
Human LCs mature in vitro upon stimulation with pI:C but are not affected upon stimulation with other TLR ligands
We wanted to investigate whether human LCs are able to cross-present antigens and induce CD8+ T-cell responses. Because cross-presentation has been described to be dependent on the maturation status of DCs,34,35 we investigated the effects of various TLR-specific compounds on the maturation of LCs and their cytokine responses. As shown in Figure 2a, only the TLR3 ligand pI:C induced an upregulation of the co-stimulatory molecules CD86 and CD70 and MHC class I, while the TLR4 ligand LPS and the TLR7/8 ligands R837 and R848 had no effects (Figure 2a). In addition, only pI:C induced an enhanced production of the pro-inflammatory cytokines TNF-α, IL-6, and IL-8 (Figure 2b). LCs did not secrete the anti-inflammatory cytokine IL-10 either in the presence or absence of pI:C, LPS, R837, or R848 (levels below 10 pg mL–1; data not shown). Therefore, human LCs matured upon stimulation with the TLR3 ligand pI:C, which can be explained by the abundant expression of TLR3 by LCs as described in the literature.36,37
Figure 2.
Maturation of LCs in vitro upon stimulation with the TLR3 ligand pI:C. (a) Phenotypic characterization of human LCs after 16 h of culture in the presence of the indicated TLR ligands. The mean fluorescence intensity is depicted for MHC class I, CD86, and CD70. The data represent the average ± SEM for three independent skin donors. (b) Cytokines produced by human LCs cultured for 16 h in the presence or absence of the indicated TLR ligands. The data represent the average ± SEM for three independent skin donors. *p < 0.05; **p < 0.01; ***p < 0.001.
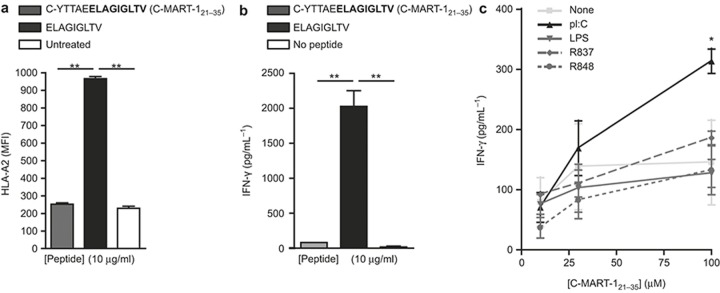
pI:C treatment enhances the cross-presentation capacity of LCs
In order to investigate the capacity of LCs to cross-present SLPs, we pulsed human LCs with a titration of a 16 aa MART-1 peptide (C-YTTAEELAGIGILTV) containing an HLA-A2-restricted epitope (ELAGIGILTV) recognized by an MART-1-specific CD8+ T-cell clone in the presence of various TLR ligands. This clone responds to specific peptide-MHC-I complexes by producing IFN-γ. To verify that the 16-aa SLP requires antigen processing before loading on MHC class I molecules, a T2 assay was performed. The data presented in Figure 3a excluded the possibility of direct external loading because the SLP did not stabilize HLA-A2 molecules on the surface of the TAP-deficient T2 cell line (Figure 3a). As a positive control, T2 cells were incubated with the minimal MART-1 epitope that can directly bind and stabilize HLA-A2 on the surface of T2 cells (Figure 3a). In addition, HLA-A2+ human LCs were loaded with the 16-aa MART-1 SLP or the 10-aa minimal MART-1 epitope for 30 min, washed and then co-cultured with the MART-1-specific CD8+ T-cell clone. Only when the LCs were loaded with the minimal epitope, did the CD8+ T cells respond by secreting IFN-γ (Figure 3b). No T-cell activation was observed when the LCs were incubated with the 16-aa SLP, indicating that this peptide requires processing before it can be presented on HLA-A2 molecules (Figure 3b).
Figure 3.
pI:C stimulation of LCs results in superior antigen cross-presentation. (a) 1 × 105 T2 cells were incubated with a 16 aa MART-1 peptide, the minimal CD8 epitope or no peptide, after which cells were analyzed for surface HLA-A2 expression by flow cytometry. The data represent the average of three experiments ± SD. **p < 0.01. (b) In total, 2 × 104 HLA-A2+ LCs were incubated with a 16 aa MART-1 peptide, the minimal CD8 epitope or no peptide for 30 min, washed and co-cultured with 1 × 105 MART-1-specific CD8+ T cells. After 24 h of co-culture, T-cell activation was measured by IFN-γ ELISA analysis of the supernatants. The data represent the average of two experiments ± SD. **p < 0.01. (c). Human LCs were incubated with the synthetic long MART-1 peptide and indicated TLR ligands for 3 h, washed and co-cultured with a MART-1-specific CD8+ T-cell clone. After 24 h of co-culture, T-cell activation was measured by IFN-γ ELISA analysis of the supernatants. The data from one representative experiment measured in triplicate is shown, n = 3. *p < 0.05.
As demonstrated in Figure 3c, human LCs were able to cross-present to the MART-1-specific CD8+ T-cell clone after 3 h of antigen internalization, as measured by the secretion of IFN-γ. Moreover, the simultaneous administration of MART-1 peptide and pI:C resulted in a significant increase in the activation of CD8+ T cells, whereas the addition of LPS, R837, or R848 did not enhance cross-presentation (Figure 3c). Thus, human LCs were able to cross-present a soluble SLP, which could be further enhanced in the presence of pI:C.
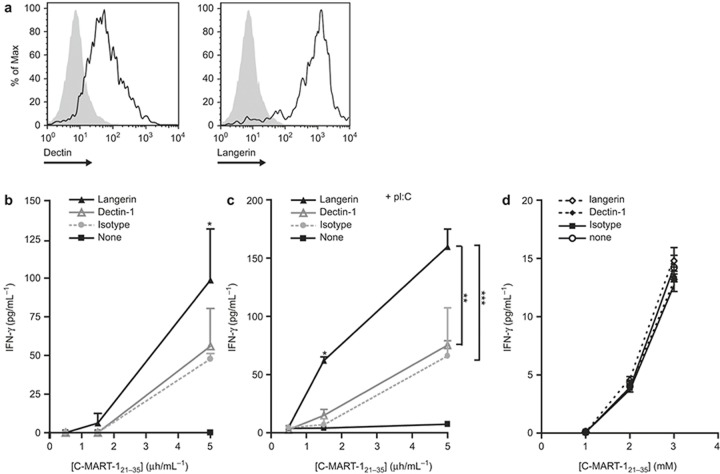
Targeting langerin, but not dectin-1, using SLP-antibody conjugates enhanced antigen cross-presentation in LCs
Because human LCs have the capacity to cross-present an MART-1 SLP, which was presumably internalized by pinocytosis, we next investigated whether receptor-mediated internalization would enhance cross-presentation by altering the endocytic routing of the antigens. To investigate this, anti-langerin or anti-dectin-1 mouse mAbs were conjugated to the MART-1 SLP via maleimide-thiol coupling through the N-terminal cysteine on the SLP. Both langerin and dectin-1 are expressed on human LCs (Figure 4a), and, as shown in Figure 1, langerin is a specific marker of human LCs, making this receptor a suitable target for LC-targeting immunotherapy. Conjugation of SLPs to anti-langerin antibodies resulted in a significantly higher activation of the CD8+ T-cell clone (Figure 4b) compared to a SLP alone or a SLP conjugated to the anti-dectin-1 antibody or an isotype control, indicating that langerin targeting enhances cross-presentation by human LCs. Furthermore, langerin-specific responses were further increased when LCs were simultaneously exposed to pI:C (Figure 4c). Interestingly, although both dectin-1 and langerin were expressed on LCs (Figure 4a), we could not detect any dectin-1-specific enhancement of cross-presentation compared to the isotype control (Figure 4b and c), suggesting that antigens endocytosed via dectin-1 followed an intracellular routing that did not result in proper processing and/or loading to MHC class I. In addition, the effect of pI:C was not related to enhanced co-stimulation, as can be deduced from Figure 4d, where no additional effect on IFN-γ production could be observed when MART-1-loaded LCs were stimulated with pI:C. Seemingly, dectin-1 or langerin targeting did not have any co-stimulation-related effects on IFN-γ production (Figure 4d). Together, these data show that only langerin targeting of MART-1 SLP allowed antigen routing to a cross-presentation compartment, which could be enhanced by the simultaneous triggering of TLR3.
Figure 4.
SLP conjugated to langerin results in enhanced cross-presentation to antigen-specific CD8+ T cells. (a) Dectin-1 and langerin are highly expressed by human LCs as measured by flow cytometry. Open histograms: specific antibody; filled histograms: isotype control. The data are representative of three donors. (b and c) MART-1 (C-YTTAEELAGIGILTV) peptide was conjugated to anti-langerin and anti-dectin-1 or mIgG1 isotype control mAbs, incubated with human LCs for 3 h in the presence (c), or absence (b) of 20 μg mL–1 pI:C and co-cultured with an MART-1-specific CD8+ T-cell clone. The activation of the T cells was measured by IFN-γ ELISA analysis of the supernatants taken after 24 h of co-culture. The data are representative of two independent experiments and depict the average ± SEM of triplicates. (d) Human LCs were incubated with MART-1 (C-YTTAEELAGIGILTV) peptide in the presence or absence of anti-langerin, anti-dectin-1, or 20 μg mL–1 pI:C for 3 h, and then washed and co-cultured with an MART-1-specific CD8+ T-cell clone. The activation of the T cells was measured by IFN-γ ELISA analysis of the supernatants taken after 24 h of co-culture.
Langerin routes antigens to specific early endosomes
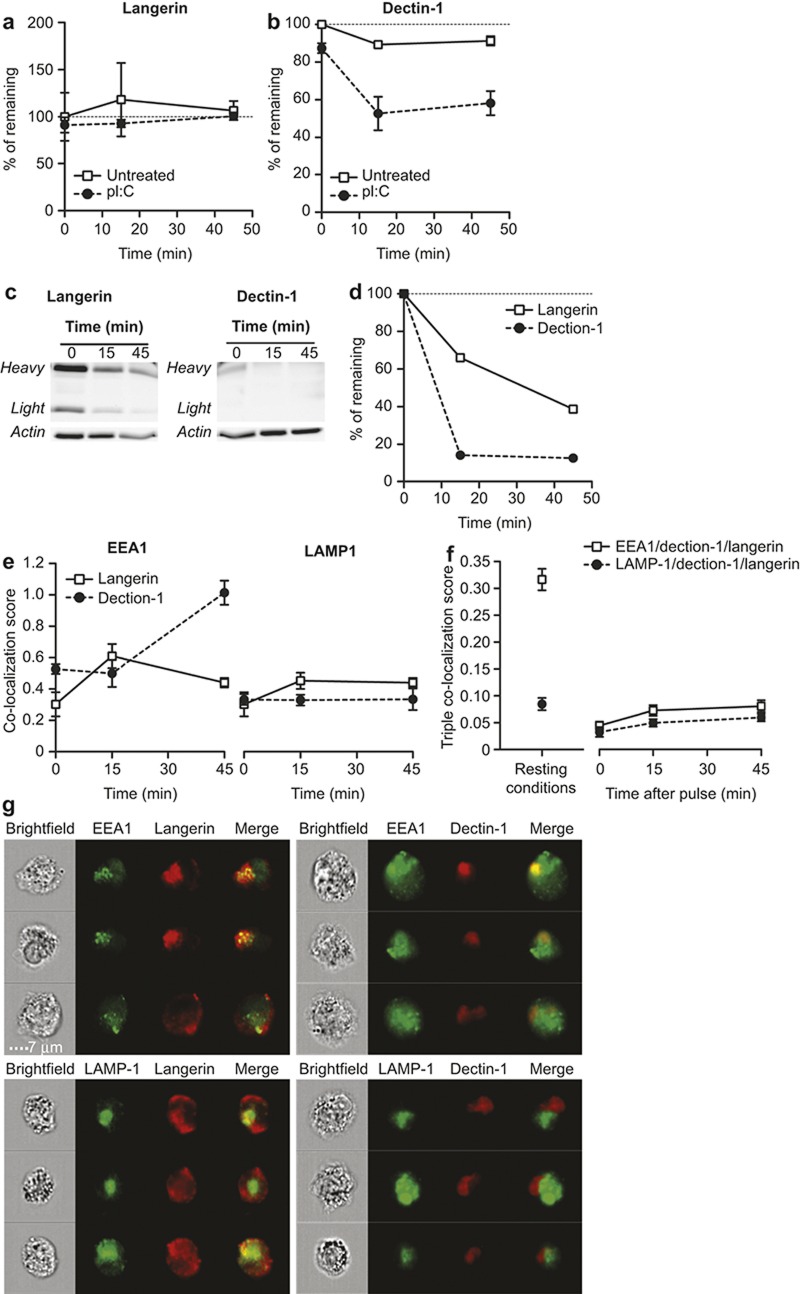
To investigate the differences in antigen cross-presentation after langerin and dectin-1 targeting, we pulsed LCs using fluorescently labeled antibodies and followed their intracellular localization using the early endosomal marker EEA-1 and the lysosomal marker LAMP-1 by imaging flow cytometry. The fluorescence associated with the anti-langerin antibody hardly decreased over time (Figure 5a), while that of the anti-dectin-1 antibody rapidly decreased (Figure 5b), suggesting that langerin routes antigens to a less degradative compartment compared to dectin-1. To further confirm this point, we investigated antibody degradation by WB in LC lysates obtained at the above-mentioned time points. Our data indeed confirmed a faster degradation of anti-dectin antibodies compared to anti-langerin (Figure 5c). We then investigated the co-localization of each of the CLR-specific antibodies with EEA-1+ compartments and observed that dectin-1 had a longer and stronger association with EEA-1+ compartments compared to langerin based on a co-localization score close to 1 (Figure 5e and g). The co-localization between langerin and LAMP-1+ compartments or dectin-1 and LAMP-1+ compartments was poor and did not differ in time and intensity (Figure 5e and g).
Figure 5.
Langerin routes to less degradative endosomal compartments in LCs after antigenic pulse compared to dectin-1 A+B. The remaining fluorescence of anti-langerin (a) and anti-dectin-1 antibodies (b) in a pulse–chase in the presence or absence of pI:C. C+D. Pulse–chase of anti-langerin and anti-dectin-1 antibody degradation in LCs by western blotting using an anti-mouse Fc peroxidase-labeled antibody. Staining is shown in (c), and band intensity quantification in (d). (e) Co-localization of langerin and dectin-1 with the intracellular compartments EEA-1 and LAMP-1 after receptor binding and internalization at the cell surface. (f) Three-color co-localization score of langerin, dectin-1 and EEA-1, or LAMP-1 in resting conditions (left panel) or after receptor triggering at the cell surface (right panel) measured by imaging flow cytometry (representative images are shown in Supplementary Figure S4). (g) Randomly selected LCs representing the data depicted in e (15-min time point).
Because there was a divergence in the degradation of the fluorescence signal and the localization to early endosomes, we speculated that dectin-1 and langerin routed to different types of early endosomes with differing degradative capacities. To investigate this, we used a 3-color co-localization feature and addressed the co-localization of either EEA1 or LAMP1 with dectin-1 and langerin simultaneously. In resting LCs, both dectin-1 and langerin were expressed on the membrane of LCs, as shown in Figure 4a. However, a significant proportion of both receptors localized to an intracellular compartment, which appeared to be EEA1+ (Figure 5s and Supplementary Figure S4). Presumably, this compartment served as an intracellular depot for the rapid upregulation of both receptors on the membrane of LCs. Interestingly, upon triggering dectin-1 and langerin, 3-color co-localization with EEA1 dramatically decreased, suggesting that, although both receptors were internalized and routed to early endosomes (as shown in Figure 5e), they did not coincide with the same endosomes (Figure 5f and Supplementary Figure S4). These data indicate that langerin routes to specific EEA-1+ early endosomes that presumably are better equipped to facilitate cross-presentation than the early endosomes to which dectin-1 routes.
Discussion
Within the human skin, at least three main and distinct populations of DCs can be identified, namely, LCs, CD14+ dDCs, and CD1a+ dDCs. After activation, the langerin+ LCs and dDC subsets are able to migrate to the skin-draining lymph nodes, where they activate CD4+ and CD8+ T-cell responses.38,39 The precise function of each subset is still under debate, especially with regard to antigen cross-presentation. Recently, a minor population of BDCA3+ myeloid DCs has been described as homologues of mouse CD8+ DCs and has been shown to have superior cross-presentation capacity.40,41,42 Antigen targeting to CLEC9a, a CLR expressed on BDCA3+ DCs, results in antigen uptake and (cross-)presentation.43 However, it has also been shown that human skin resident BDCA3+ DCs can produce IL-10 and induce regulatory T cells (Tregs).44 In addition, the low numbers of these cells also make them less favorable to target for the induction of anti-tumor immune responses.
In this study, we investigated the cross-presentation capacity of human LCs when an SLP was targeted to distinct CLRs. Specific targeting of SLP to the LC-specific receptor langerin using modification by either antibody resulted in the enhanced activation of effector CD8+ T cells. These results imply that human LCs are a suitable candidate for the in vivo targeting of vaccines. Although LCs are located in the epidermis of the human skin, the administration of an LC-targeting vaccine can also be applied intradermally because intradermally deposited DEC-205 or langerin antibodies have been shown to be rapidly captured by LCs.45
In our studies, the use of mAbs to target peptides or proteins to langerin46 resulted in efficient antigen cross-presentation. In contrast, antigens internalized via the CLR dectin-1 did not allow enhanced cross-presentation, showing that the intracellular routing of antigens internalized via dectin-1 was different from that of antigens internalized via langerin in LCs. This is supported by our imaging flow cytometry data, which demonstrate that dectin-1 routed to more degradative intracellular compartments that also did not co-localize with langerin+ EEA-1+ compartments. However, it has been shown for in vitro-generated moDCs that dectin-1 allows binding and internalization of CMV pp65-expressing apoptotic cells and that this interaction results in cross-presentation to CMV pp65-specific CD8+ T cells,19, showing the potential of dectin-1 to facilitate routing of antigen to MHC class I loading compartments when expressed on DCs. The discrepancy between these results and the findings presented in this study concerning cross-presentation after dectin-1 targeting might be explained by the difference in cell types, i.e., primary LCs versus in vitro-generated DCs. Alternatively, it may also be attributed to the mode of antigen delivery. In the experiments described here, dectin-1 was targeted using mAbs conjugated to a soluble MART-1 peptide, whereas in the study by Weck et al., dectin-1 facilitated the uptake of total apoptotic cells.19
Dectin-1 is not the only CLR in which the capacity to cross-present is in part determined by the mode of antigen delivery. Van der Vlist et al. reported that human LCs are not able to cross-present antigens derived from whole MV or MV-infected apoptotic cells taken up via langerin.9 We have recently demonstrated that differences in the size of the antigen influence langerin-mediated antigen internalization and cross-presentation in LCs.47 Bigger nanoparticles are less well internalized and cross-presented by LCs compared to small, soluble peptides.29 These findings might explain the discrepancy found between the Van der Vlist study and the data presented here. In their study, the authors used relatively large MV particles and MV-infected cells that were not cross-presented in a langerin-dependent fashion, whereas we did show langerin-mediated internalization and cross-presentation of a small SLP in our studies.
This study also showed that cross-presentation by human LCs was enhanced in the presence of the TLR3 agonist pI:C. The combined administration of antigens and TLR agonists is reported to be necessary to prevent the induction of T-cell tolerance. Recently, the requirement for a potent activator to overcome the tolerogenic state of LCs that selectively and specifically induces the activation and proliferation of skin-resident Tregs has been described.48 Similar to DCs, in the presence of danger signal derived from pathogens, LCs become activated and induce the proliferation of effector memory T cells that are present in the skin and reduce the activity of Tregs.48 It seems likely that the precise function of LCs in vivo might be determined by danger stimuli derived from the microenvironment.49
Altogether, we have shown the capacity of human primary LCs to cross-present a soluble, synthetic long MART-1 peptide. Additionally, cross-presentation by LCs was enhanced when cells were concomitantly matured using the TLR3 agonist pI:C. Targeting of MART-1 SLP to anti-langerin antibodies resulted in further enhancement of the activation of MART-1-specific CD8+ T cells through the langerin-mediated routing of antigens to less-proteolytic early endosomes compared to dectin-1-mediated antigen internalization. These results provide a rationale for the development of new in vivo vaccines that target human LCs via langerin for the induction of effective anti-tumor or anti-viral CTL responses.
Acknowledgments
We would like to thank the personnel of the Bergman clinic in Bilthoven, the Netherlands for providing healthy donor skin. We would like to thank Tom O'Toole for the technical assistance with imaging flow cytometry. The present work was funded by KWF (VU2009-2598), the Dutch Science Foundation (NWO, VENI Grant NO 863.10.017), the European Research Council (ERCAdvanced339977), and NanoNext 3D01.
Footnotes
Supplementary information of this article can be found on the Cellular & Molecular Immunology's website (http://www.nature.com/cmi).
Supplementary Information
References
- Heath WR, Belz GT, Behrens GM, Smith CM, Forehan SP, Parish IA et al. Cross-presentation, dendritic cell subsets, and the generation of immunity to cellular antigens. Immunol Rev 2004; 199: 9–26. [DOI] [PubMed] [Google Scholar]
- Joffre OP, Segura E, Savina A, Amigorena S. Cross-presentation by dendritic cells. Nat Rev Immunol 2012; 12: 557–569. [DOI] [PubMed] [Google Scholar]
- Valladeau J, Dezutter-Dambuyant C, Saeland S. Langerin/CD207 sheds light on formation of birbeck granules and their possible function in Langerhans cells. Immunol Res 2003; 28: 93–107. [DOI] [PubMed] [Google Scholar]
- Feinberg H, Taylor ME, Razi N, McBride R, Knirel YA, Graham SA et al. Structural basis for langerin recognition of diverse pathogen and mammalian glycans through a single binding site. J Mol Biol 2011; 405: 1027–1039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Furio L, Briotet I, Journeaux A, Billard H, Peguet-Navarro J. Human Langerhans cells are more efficient than CD14(-)CD1c(+) dermal dendritic cells at priming naive CD4(+) T cells. J Invest Dermatol 2010; 130: 1345–1354. [DOI] [PubMed] [Google Scholar]
- Furio L, Billard H, Valladeau J, Peguet-Navarro J, Berthier-Vergnes O. Poly(I:C)-Treated human Langerhans cells promote the differentiation of CD4+ T cells producing IFN-gamma and IL-10. J Invest Dermatol 2009; 129: 1963–1971. [DOI] [PubMed] [Google Scholar]
- Klechevsky E, Morita R, Liu M, Cao Y, Coquery S, Thompson-Snipes L et al. Functional specializations of human epidermal Langerhans cells and CD14+ dermal dendritic cells. Immunity 2008; 29: 497–510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Polak ME, Newell L, Taraban VY, Pickard C, Healy E, Friedmann PS et al. CD70-CD27 interaction augments CD8+ T-cell activation by human epidermal Langerhans cells. J Invest Dermatol 2012; 132: 1636–1644. [DOI] [PubMed] [Google Scholar]
- van der Vlist M, de Witte L, de Vries RD, Litjens M, de Jong MA, Fluitsma D et al. Human Langerhans cells capture measles virus through Langerin and present viral antigens to CD4(+) T cells but are incapable of cross-presentation. Eur J Immunol 2011; 41: 2619–2631. [DOI] [PubMed] [Google Scholar]
- Igyarto BZ, Haley K, Ortner D, Bobr A, Gerami-Nejad M, Edelson BT et al. Skin-resident murine dendritic cell subsets promote distinct and opposing antigen-specific T helper cell responses. Immunity 2011; 35: 260–272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bedoui S, Whitney PG, Waithman J, Eidsmo L, Wakim L, Caminschi I et al. Cross-presentation of viral and self antigens by skin-derived CD103+ dendritic cells. Nat Immunol 2009; 10: 488–495. [DOI] [PubMed] [Google Scholar]
- Henri S, Poulin LF, Tamoutounour S, Ardouin L, Guilliams M, de Bovis B et al. CD207+ CD103+ dermal dendritic cells cross-present keratinocyte-derived antigens irrespective of the presence of Langerhans cells. J Exp Med 2010; 207: 189–206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Igyarto BZ, Kaplan DH. Antigen presentation by Langerhans cells. Curr Opin Immunol 2013; 25: 115–119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bigley V, McGovern N, Milne P, Dickinson R, Pagan S, Cookson S et al. Langerin-expressing dendritic cells in human tissues are related to CD1c+ dendritic cells and distinct from Langerhans cells and CD141 high XCR1+ dendritic cells. J Leukoc Biol 2015; 97: 627–634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Robinson MJ, Sancho D, Slack EC, LeibundGut-Landmann S, Reis E Sousa C. Myeloid C-type lectins in innate immunity. Nat Immunol 2006; 7: 1258–1265. [DOI] [PubMed] [Google Scholar]
- Tacken PJ, de Vries I, Torensma R, Figdor CG. Dendritic-cell immunotherapy: from ex vivo loading to in vivo targeting. Nat Rev Immunol 2007; 7: 790–802. [DOI] [PubMed] [Google Scholar]
- Tel J, Sittig SP, Blom RA, Cruz LJ, Schreibelt G, Figdor CG et al. Targeting uptake receptors on human plasmacytoid dendritic cells triggers antigen cross-presentation and robust type I IFN secretion. J Immunol 2013; 191: 5005–5012. [DOI] [PubMed] [Google Scholar]
- Unger WW, van Beelen AJ, Bruijns SC, Joshi M, Fehres CM, van Bloois L et al. Glycan-modified liposomes boost CD4+ and CD8+ T-cell responses by targeting DC-SIGN on dendritic cells. J Control Release 2012; 160: 88–95. [DOI] [PubMed] [Google Scholar]
- Weck MM, Appel S, Werth D, Sinzger C, Bringmann A, Grunebach F et al. hDectin-1 is involved in uptake and cross-presentation of cellular antigens. Blood 2008; 111: 4264–4272. [DOI] [PubMed] [Google Scholar]
- Bonifaz LC, Bonnyay DP, Charalambous A, Darguste DI, Fujii S, Soares H et al. In vivo targeting of antigens to maturing dendritic cells via the DEC-205 receptor improves T cell vaccination. J Exp Med 2004; 199: 815–824. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kovacsovics-Bankowski M, Rock KL. A phagosome-to-cytosol pathway for exogenous antigens presented on MHC class I molecules. Science 1995; 267: 243–246. [DOI] [PubMed] [Google Scholar]
- Rodriguez A, Regnault A, Kleijmeer M, Ricciardi-Castagnoli P, Amigorena S. Selective transport of internalized antigens to the cytosol for MHC class I presentation in dendritic cells. Nat Cell Biol 1999; 1: 362–368. [DOI] [PubMed] [Google Scholar]
- Shen L, Sigal LJ, Boes M, Rock KL. Important role of cathepsin S in generating peptides for TAP-independent MHC class I crosspresentation in vivo. Immunity 2004; 21: 155–165. [DOI] [PubMed] [Google Scholar]
- Di PT, Chatterjee B, Smed-Sorensen A, Clayton S, Palazzo A, Montes M et al. Direct proteasome-independent cross-presentation of viral antigen by plasmacytoid dendritic cells on major histocompatibility complex class I. Nat Immunol 2008; 9: 551–557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gromme M, Uytdehaag FG, Janssen H, Calafat J, van Binnendijk RS, Kenter MJ et al. Recycling MHC class I molecules and endosomal peptide loading. Proc Natl Acad Sci USA 1999; 96: 10326–10331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chatterjee B, Smed-Sorensen A, Cohn L, Chalouni C, Vandlen R, Lee BC et al. Internalization and endosomal degradation of receptor-bound antigens regulate the efficiency of cross presentation by human dendritic cells. Blood 2012; 120: 2011–20. [DOI] [PubMed] [Google Scholar]
- de Witte L, Nabatov A, Pion M, Fluitsma D, de Jong MA, de Gruijl TD et al. Langerin is a natural barrier to HIV-1 transmission by Langerhans cells. Nat Med 2007; 13: 367–371. [DOI] [PubMed] [Google Scholar]
- Salter RD, Cresswell P. Impaired assembly and transport of HLA-A and -B antigens in a mutant TxB cell hybrid. EMBO J 1986; 5: 943–949. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fehres CM, Bruijns SC, van Beelen AJ, Kalay H, Ambrosini M, Hooijberg E et al. Topical rather than intradermal application of the TLR7 ligand imiquimod leads to human dermal dendritic cell maturation and CD8+ T-cell cross-priming. Eur J Immunol 2014; 44: 2415–2424. [DOI] [PubMed] [Google Scholar]
- Hooijberg E, Ruizendaal JJ, Snijders PJ, Kueter EW, Walboomers JM, Spits H. Immortalization of human CD8+ T cell clones by ectopic expression of telomerase reverse transcriptase. J Immunol 2000; 165: 4239–4245. [DOI] [PubMed] [Google Scholar]
- Angel CE, Lala A, Chen CJ, Edgar SG, Ostrovsky LL, Dunbar PR. CD14+ antigen-presenting cells in human dermis are less mature than their CD1a+ counterparts. Int Immunol 2007; 19: 1271–1279. [DOI] [PubMed] [Google Scholar]
- Eisenwort G, Jurkin J, Yasmin N, Bauer T, Gesslbauer B, Strobl H. Identification of TROP2 (TACSTD2), an EpCAM-like molecule, as a specific marker for TGF-beta1-dependent human epidermal Langerhans cells. J Invest Dermatol 2011; 131: 2049–2057. [DOI] [PubMed] [Google Scholar]
- Bigley V, McGovern N, Milne P, Dickinson R, Pagan S, Cookson S et al. Langerin-expressing dendritic cells in human tissues are related to CD1c+ dendritic cells and distinct from Langerhans cells and CD141 high XCR1+ dendritic cells. J Leukoc Biol 2015; 97: 627–634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Crespo MI, Zacca ER, Nunez NG, Ranocchia RP, Maccioni M, Maletto BA et al. TLR7 triggering with polyuridylic acid promotes cross-presentation in CD8alpha+ conventional dendritic cells by enhancing antigen preservation and MHC class I antigen permanence on the dendritic cell surface. J Immunol 2013; 190: 948–960. [DOI] [PubMed] [Google Scholar]
- Bonifaz L, Bonnyay D, Mahnke K, Rivera M, Nussenzweig MC, Steinman RM. Efficient targeting of protein antigen to the dendritic cell receptor DEC-205 in the steady state leads to antigen presentation on major histocompatibility complex class I products and peripheral CD8+ T cell tolerance. J Exp Med 2002; 196: 1627–1638. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Flacher V, Bouschbacher M, Verronese E, Massacrier C, Sisirak V, Berthier-Vergnes O et al. Human Langerhans cells express a specific TLR profile and differentially respond to viruses and Gram-positive bacteria. J Immunol 2006; 177: 7959–7967. [DOI] [PubMed] [Google Scholar]
- van der Aar AM, Sylva-Steenland RM, Bos JD, Kapsenberg ML, de Jong EC, Teunissen MB. Loss of TLR2, TLR4, and TLR5 on Langerhans cells abolishes bacterial recognition. J Immunol 2007; 178: 1986–1990. [DOI] [PubMed] [Google Scholar]
- Segura E, Valladeau-Guilemond J, Donnadieu MH, Sastre-Garau X, Soumelis V, Amigorena S. Characterization of resident and migratory dendritic cells in human lymph nodes. J Exp Med 2012; 209: 653–660. [DOI] [PMC free article] [PubMed] [Google Scholar]
- van de Ven R, van den Hout MF, Lindenberg JJ, Sluijter BJ, van Leeuwen PA, Lougheed SM et al. Characterization of four conventional dendritic cell subsets in human skin-draining lymph nodes in relation to T-cell activation. Blood 2011; 118: 2502–2510. [DOI] [PubMed] [Google Scholar]
- Bachem A, Guttler S, Hartung E, Ebstein F, Schaefer M, Tannert A et al. Superior antigen cross-presentation and XCR1 expression define human CD11c+CD141+ cells as homologues of mouse CD8+ dendritic cells. J Exp Med 2010; 207: 1273–1281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jongbloed SL, Kassianos AJ, McDonald KJ, Clark GJ, Ju X, Angel CE et al. Human CD141+ (BDCA-3)+ dendritic cells (DCs) represent a unique myeloid DC subset that cross-presents necrotic cell antigens. J Exp Med 2010; 207: 1247–1260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Poulin LF, Salio M, Griessinger E, Anjos-Afonso F, Craciun L, Chen JL et al. Characterization of human DNGR-1+ BDCA3+ leukocytes as putative equivalents of mouse CD8alpha+ dendritic cells. J Exp Med 2010; 207: 1261–1271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schreibelt G, Klinkenberg LJ, Cruz LJ, Tacken PJ, Tel J, Kreutz M et al. The C-type lectin receptor CLEC9A mediates antigen uptake and (cross-)presentation by human blood BDCA3+ myeloid dendritic cells. Blood 2012; 119: 2284–2292. [DOI] [PubMed] [Google Scholar]
- Chu CC, Ali N, Karagiannis P, Di MP, Skowera A, Napolitano L et al. Resident CD141 (BDCA3)+ dendritic cells in human skin produce IL-10 and induce regulatory T cells that suppress skin inflammation. J Exp Med 2012; 209: 935–945. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Flacher V, Tripp CH, Stoitzner P, Haid B, Ebner S, Del FB et al. Epidermal Langerhans cells rapidly capture and present antigens from C-type lectin-targeting antibodies deposited in the dermis. J Invest Dermatol 2010; 130: 755–762. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Klechevsky E, Flamar AL, Cao Y, Blanck JP, Liu M, O'Bar A et al. Cross-priming CD8+ T cells by targeting antigens to human dendritic cells through DCIR. Blood 2010; 116: 1685–1697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fehres CM, Kalay H, Bruijns SCM, Musaafir SAM, Ambrosini M, van Bloois L et al. Cross-presentation through langerin and DC-SIGN targeting requires different formulations of glycan-modified antigens. J Control Release 2015; 203: 67–76. [DOI] [PubMed] [Google Scholar]
- Seneschal J, Clark RA, Gehad A, Baecher-Allan CM, Kupper TS. Human epidermal Langerhans cells maintain immune homeostasis in skin by activating skin resident regulatory T cells. Immunity 2012; 36: 873–884. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Romani N, Brunner PM, Stingl G. Changing views of the role of Langerhans cells. J Invest Dermatol 2012; 132: 872–881. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.